There are several key areas where the role of blue light has been implicated as having an impact upon ocular and visual health.
Ocular Tissue Damage and Macular Degeneration
In recent years, shorter wavelength blue light has been a major topic of discussion by eye care professionals. Much of the concern has been related to the ageing demographic of the population and the implication of blue light in ocular tissue damage, 1a such as may occur in the retinal pigment epithelium through photo-oxidative stress,1 potentially contributing to age-related macular degeneration (AMD, figure 1).2-7
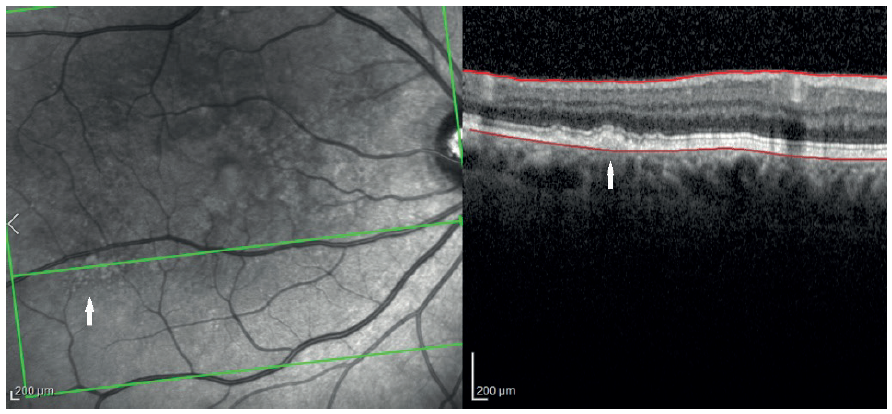 Figure 1: Early build-up of lipofuscin (white arrows) as an indication of future age-related macular degeneration. Can blue light exacerbate this process?
Figure 1: Early build-up of lipofuscin (white arrows) as an indication of future age-related macular degeneration. Can blue light exacerbate this process?
In vitro studies have shown that blue light with a wavelength of 440nm has the most potential for photo-oxidative stress damage at the macula,9 and in addition there is extensive peer-reviewed research from animal studies that suggests there is a ‘blue light hazard’ (so may have the potential for damage) in the range of 415nm through to 455nm.25 -33 It is, however, recognised that the lens of the eye yellows with age (brunescence) and the transmission of these wavelengths is reduced, particularly in the over-60 age group (figure 2).10-13 The yellow macular pigment composed principally of the three isomeric carotenoids meso-zeaxanthin, lutein, and zeaxanthin may also help protect the macula from blue light.59
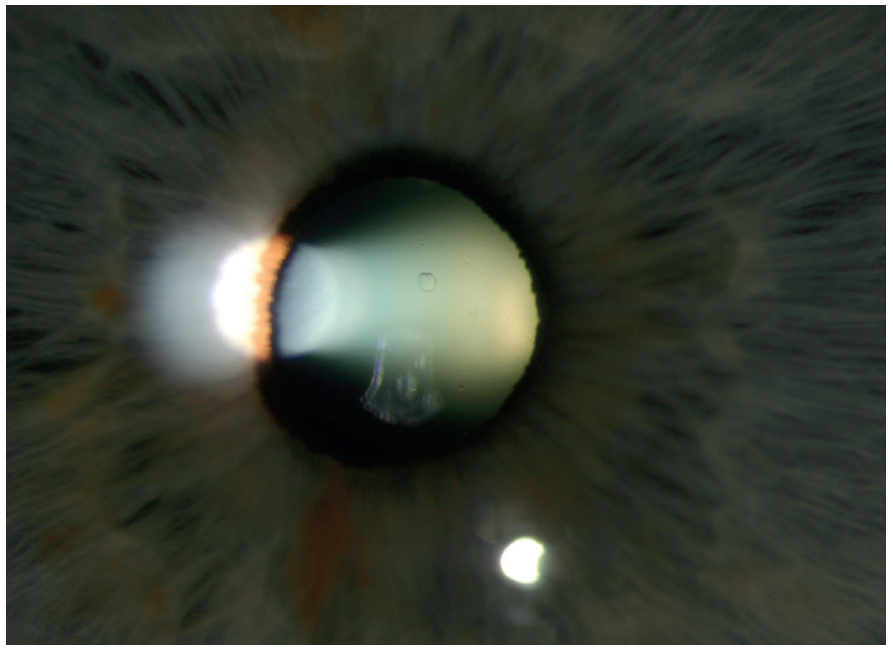 Figure 2: Lens brunescense – a natural barrier to short wavelength visible light
Figure 2: Lens brunescense – a natural barrier to short wavelength visible light
This said, the metabolic by-products formed in the retina by continual photoreception activity accumulate with age. If phototoxicity is more likely to occur in an already compromised retina, then the yellowing crystalline lens should have a protective effect. Indeed, it may be that blue attenuation spectacle lenses may be more helpful to the elderly in reducing crystalline lens fluorescence than in protecting the retina.
It should be noted that AMD is a multifactorial condition and the aetiology and pathogenesis of AMD are not well understood and remain a major challenge to understand.8 Although age, genetic inheritance and smoking are much greater risk factors than blue light, this does not prevent us trying to reduce any potential harmful effects. Also, if blue light exposure is a risk factor, it will be a modifiable one like smoking, so something that could be ameliorated.
Modern Lifestyle Exposure and Indoor Exposure
While the primary source of blue light is from sunlight, over the past 10 years or so our exposure indoors to bluer light has increased many times over as we embrace contemporary living environments, modern communication technology and ‘digital lifestyles’.
Indoor blue light sources include the following to varying degrees:
- Light-emitting diodes (LEDs)
- Lower energy light sources
- OLED screens – these use a light-emitting diode containing thin flexible sheets of an organic electroluminescent material and are used mainly in digital display screens televisions, computers, personal digital assistants and smart phones.
Many screen devices are inevitably used at closer viewing distances which result in higher levels of their light output impacting upon the eye. However, blue light screen emissions are at such low levels that they do not in any way represent a biohazard.14 So, although these devices generate blue light in the 380 to 450nm range, the radiant energy is extremely low.
In tests measuring at 450nm, the absolute irradiance of a phone with a white screen at its brightest setting produces an intensity of only 0.05µW/cm²/nm, whereas the blue sky at 90 degrees to the sun at 4pm produces an intensity 400 times greater, at 20µW/cm²/nm, and sunlight reflecting from white paper produces an intensity at 450nm of 60µW/cm²/nm, a thousand times greater than the phone. This means that, to be exposed to the same amount of dangerous high energy photons as during a 20-minute walk or drive to work, you would need to spend 133 hours looking at your phone or computer screen continuously.15
By contrast, current white LEDs have much higher spectral emissions in the blue wavelengths than tungsten or tungsten-halide lamps and at levels that may require attention over cumulative exposures during a human lifetime.16,17 Such light sources are used in ophthalmic instruments.
Circadian Rhythm
The circadian rhythm or the sleep-wake cycle is controlled by melatonin release, a hormone secreted by the pineal gland located behind the third ventricle of the brain. When the retina of a sleeping individual is exposed to light with a blue component, melatonin production is suppressed and the individual wakes up. By contrast, switching off blue-light or switching on absorption at night up-regulates melatonin production and the individual goes to sleep.40 The photosensitive retinal ganglion cells are most sensitive to blue light wavelengths around 470nm (blue turquoise). Disruption of these rhythms has been linked to a wide range of conditions such as sleep disorders, depression, anxiety, obesity and diabetes.41-46 It has also been shown that exposure to commercially available 6500K fluorescent lighting for 90 minutes before bedtime strongly suppresses melatonin release by up to 40%.47 However, it should be borne in mind that it is highly unlikely that 6500K fluorescent lighting (which is cold white) would be used in the home and particularly before bedtime, though some agricultural workers may have such exposure. Home lighting is more likely to be within the 2700 to 3000K warm white range, whether fluorescent, LED or halogen.
Using blue light-emitting LED smartphones and e-readers at night may also negatively influence sleep.48,49 This is difficult to quantify, however, as other contributory factors including having a phone placed by the bed,60 the viewing of content of heightened impact, and poor sleep discipline may ultimately be more powerful triggers.
Digital Eyestrain
Computer vision syndrome, also referred to as digital eye strain, describes a group of eye and vision-related problems that result from prolonged computer, tablet, e-reader and smartphone use. Many individuals experience eye discomfort and vision problems when viewing digital screens for extended periods. The level of discomfort appears to increase with the amount of digital screen use.18,19
The Vision Council of America defines digital eye strain as ‘physical discomfort after screen use for longer than two hours at a time.’ Symptoms may include the following:
- Headaches
- Sore or tired eyes (eye strain)
- Blurred near vision
- Glare (light) sensitivity
- Blurred distance vision
- Dry or watery eyes
- Burning, itching or red eyes
- Back pain
- Neck and shoulder pain
- Double vision
According to The Vision Council Digital Eyestrain Report (June 2017), 83.6% of Americans aged 18 and older typically use computers and other digital devices at least two hours per day, and 50.3% use these devices at least six hours per day. Among parents surveyed, 72.9% reported that their children spend at least two hours per day in front of a digital device screen.1 Also, 62.2% of survey respondents said they were either ‘very concerned’ or ‘somewhat concerned’ about the impact of digital device usage on their eyes, and 77.1% were ‘very concerned’ or ‘somewhat concerned’ about the impact of digital devices on their children’s developing eyes.21
One factor that potentially contributes to digital eye strain is chromatic aberration. This occurs even if vision is corrected as well as possible with prescription eyewear. This is because the refractive indices of ocular tissues vary with wavelength. The eye’s optical power is therefore different for different colours, leading to a chromatic difference in refraction, or longitudinal chromatic aberration (figure 3). Measured values of chromatic aberration are very consistent across subjects. From the red to blue ends of the spectrum, as much as two dioptres of focus difference occurs.22 Additionally, blue light scatters more within the eye, reducing contrast which can affect visual quality and comfort.23
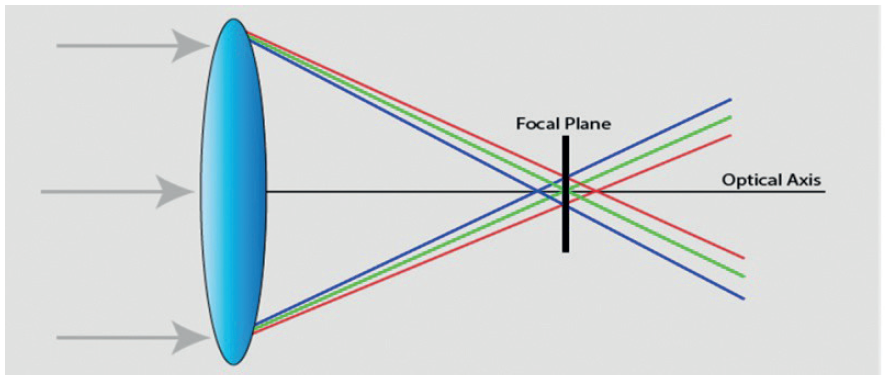
Figure 3: Longitudinal chromatic aberration occurs as longer wavelengths are refracted less than shorter wavelengths of visible light
A recent clinical study also suggested that blue light exposure was linked to a reduction in visual quality in subjects with dry eye resulting from poor tear film stability24 and increased glare sensation.34,35
Dry eye has been cited as a major contributor to computer vision syndrome36 and long periods of computer work are associated with a high prevalence of dry eye37 because of a reduced blink rate which ultimately affected tear film stability.38,39
Blue Filtering Lenses
In 2017, the clinical performance (contrast sensitivity, with and without glare, and colour discrimination tests) and the subjective perception of different blue-light ophthalmic lenses (BF clear lens with blue-filter anti-reflection coating, BT brown-tinted lenses and AR clear lens with conventional anti-reflection coating acting as a control) was evaluated in a clinical trial on users of digital display screens for a minimum of two hours daily.52 The study sample was divided into two age groups:
- Young (range 18 to 35 years)
- Middle aged adults (range 40 to 55 years)
The researchers reported that blue-light filtering lenses modestly filter short-wavelength light and do not markedly degrade visual performance. Subjectively, more than one-third of subjects involved in the clinical study found that a clear lens with blue filtering coating provided better anti-glare performance and improved their vision for computer and mobile digital screens. The study also found that the young adults preferred the clear lens with conventional anti-reflection coating AR (50.0%) and clear lens with blue-filter anti-reflection coating BF (47.5%) lenses when compared to the brown-tinted lenses BT lens (2.5%). The middle-aged adults, however, preferred the clear lens with the blue-filter anti-reflection coating BF lens (60.0%) as compared to the other two lens types (AR 22.5% and BT 17.5%). The results are summarised in figure 4.
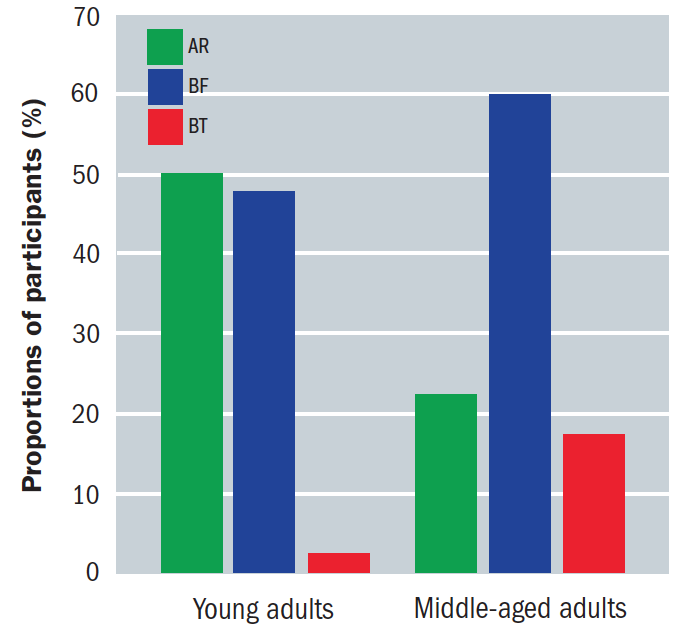
Figure 4: Participant preference of lens type in young and middle-aged adults: (AR) clear lens with conventional anti-reflection coating, (BF) clear lens with blue-filter anti-reflection coating, (BT) brown-tinted lenses
These results could be explained by considering the different eye transmittance between age groups, with a lower transmittance and a higher ocular scattering for blue light in the middle-aged group. In this age group, the use of the blue-light filter can be more useful to reduce the effect of ocular scattering.
Blue filtering spectacle lenses have been available for many years in various guises, from simple tinted lenses through to contrast enhancing lenses, photochromic lenses and mirror coated lenses. However, it is only since around 2013 that blue light reducing lenses were introduced whose mechanism of attenuation was by selective reflection of blue light wavelengths.
The introduction of this type of technology has led to much controversy over the claimed benefits of these lenses resulting in statements being issued in the UK by the College of Optometrists,51 the Association of British Dispensing Opticians52 and the Association of Optometrists.53
Conclusion
The current position of the UK optical bodies is based on the lack of strong clinical evidence for phototoxicity and some concerns over the possible negative effects of reducing blue light on a patient’s wellbeing by disruption of circadian rhythms. The guidance, however, seems to omit the fact that photochromic and light tinted lenses have been available for many years and anecdotal evidence suggests that there has been little or no reported impact on wellbeing with their use.
Interestingly, in an Australian optometrist practitioner survey of 372 respondents, 75.3% indicated prescribing blue light-blocking spectacle lenses in their clinical practice. Forty-four per cent of optometrists considered daily environmental exposure to blue light as a potential cause of retinal damage, and approximately half of respondents thought blue light emitted from computer screens was an important factor in causing computer vision syndrome. About half of optometrists considered placebo effects to potentially play a role, at least sometimes, in patients’ experiences with blue light-blocking lenses.74
There is also a growing body of evidence from in vitro and animal studies2-7 that suggests that both blue and UV light may be risk factors in the development of AMD. UV has been studied for many years and its cumulative effects are well documented, although as little as 1% reaches the retina in adulthood.57 Shorter wavelength blue light continues to pass through to the retina and it is the cumulative effect that gives rise to concern.56
Although there are no long-term studies on humans with regards to ‘the blue light hazard,’ and these are unlikely to be available for many years, we do have the Beaver Dam study which was a 15-year study of the effects of sunlight on population. Its conclusion was that those participants who were exposed to summer sun for more than five hours a day were at a higher risk of development of increased retinal pigment levels and early AMD than those exposed to less than two hours/day during the same period.54 Several other studies also suggest the correlation between sunlight and AMD.61-72
As far as clinical claims are concerned, particularly associated with AMD, patients should be made aware of good eye care regimes, such as wearing sunglasses and limiting their overall UV and blue light exposure.
With regards to circadian rhythm, studies using dark tinted lenses before bedtime have shown that melatonin suppression was significantly reduced although there are no studies directly related to blue attenuating coatings.58
With some degree of certainty, we can say that blue attenuating coatings, particularly for the 40 to 55-year age groups, have been shown to reduce digital eye strain in a clinically validated study by reducing blue light scatter and increasing quality of vision.52
It is recommended that whenever advising blue attenuating lenses, samples should be used to demonstrate the benefits of the lenses when using computer screens and the slight colour shift should be explained.
Andy Sanders is Professional Services Manager for Hoya UK and Ireland, Chair of the FMO Lens Focus Group and Standards Panel
• The author would like to acknowledge the support of Ron Rabbetts and Dr M Wolffe in the writing of this article
References
- a. Behar-Cohen F, et al. Light-emitting diodes (LED) for domestic lighting: Any risk for the eye? Prog. Retin. Eye Res. 2011: 30, 239-257
b. http://iovs.arvojournals.org/article.aspx?articleid=2128327. Blue Light–Induced Oxidative Stress in Human Corneal Epithelial Cells: Protective Effects of Ethanol Extracts of Various Medicinal Plant MixturesJee-Bum Lee; Soo-Hyun Kim; Seung-Chul Lee; Hee-Gu Kim; Ho-Geun Ahn; Zhengri Li; Kyung Chul Yoon - Boulton M, et al. The photoreactivity of ocular lipofuscin. Photochem. Photobiol. Sci. 2004: 3(8), 759-764
- Wang Z, et al. Oxidation of A2E results in the formation of highly reactive aldehydes and ketones. Photochem. Photobiol. 2006: 82(5), 1251-1257
- Parish CA, et al. Isolation and one-step preparation of A2E and iso-A2E fluorophores from human retinal pigment epithelium. Proc. Natl. Acad. Sci. 1998: 95, 14609-14613.
- Ham WT. Ocular hazards of light sources: review of current knowledge. J. Occup. Med. 1983: 25(2), 101-103.
- van Norren D and Schellekens P. Blue light hazard in rat. Vis. Res. 1990: 30(10), 1517-1520.
- Algvere PV, Marshall J and Seregard S. Age-related maculopathy and the impact of blue light hazard. Acta Ophthalmol. Scan. 2006: 84(1), 4-15.
- Sandeep Kumar and Yingbin Fu — Age Related Macular Degeneration: a Complex Pathology austinpublishinggroup.com/genetics-genomic-research/fulltext/ajggr-v1-id1005.php
- Prof J Marshall 2015 pointsdevue.com/article/blue-light-paradox-problem-or-panacea
- Gaillard ER, et al. Age-related changes in the absorption characteristics of the primate lens. Invest. Ophthalmol. Vis. Sci. 2000: 41(6), 1454-1459.
- Bron AJ, et al. The ageing lens. Ophthalmologica. 2000: 214(1), 86-104
- van de Kraats J and van Norren D. Optical density of the aging ocular media in the visible and the UV. J. Opt. Soc. Am. A Opt. Image Sci. Vis. 2007: 24(7), 1842-1857
- Kessel l, et al. Age-related changes in the transmission properties of the human lens and their relevance to circadian entrainment. J. Cataract Refr. Surg. 2010: 36(2), 308-312.
- O’Hagan J B. Low-energy light bulbs, computers, tablets and the blue light hazard. Eye 2016 p230-233
- Dr Shelby Temple Senior Research Associate University of Bristol. Optician, 19th August 2016
- Chamorro E. et al. Effects of Light-emitting Diode Radiations on Human Retinal Pigment Epithelial Cells In Vitro. Photochemistry and Photobiology, 2013, 89
- Krigel A. Light-induced retinal damage using different light sources, protocols and rat strains reveals LED phototoxicity. Neuroscience, 2016, (339): 296-307
- American Optometric society www.aoa.org/patients-and-public/caring-for-your-vision/protecting-your-vision/computer-vision-syndrome
- The Computer-Vision Symptom Scale (CVSS17): development and initial validation.González-Pérez M1, Susi R2, Antona B1, Barrio A1, González E1
- Digital eye strain The Vision council https://www.thevisioncouncil.org/content/digital-eye-strain. (Accessed Dec 15. 2017)
- The Vision Council Digital Eyestrain report June 2017
- http://pabloartal.blogspot.co.uk Pablo Artal. Full Professor of Optics LOUM – Laboratorio de Óptica de la Universidad de Murcia
- http://www.allaboutvision.com/cvs/blue-light.htm Dr Gary Heiting, OD
- Reducing Short-Wavelength Blue Light in Dry Eye Patients with Unstable Tear Film Improves Performance on Tests of Visual Acuity Minako Kaido,1,2,* Ikuko Toda, #3 Tomoo Oobayashi, #3 Motoko Kawashima, #1 Yusaku Katada, #1 and Kazuo Tsubota #1
- Margrain T, et al. Do Blue Light filters confer protection against Age-Related Macular Degeneration? Progress in Retinal and Eye Research. 2004; 23: 523-531
- Shang Y, et al. White Light Emitting Diodes (LEDs) at domestic lighting levels and retinal Injury in a rat model. Environ Health Perspect 2014; 122, 269-276.
- Taylor H, et al. The long-term effects of visible light on the eye. Arch. Ophthalmol.1992; 110: 99-104.
- Cruickshanks K, et al. Sunlight and age-related macular degeneration. The Beaver Dam Eye Study. Arch. Ophthalmol. 1993; 111: 514-518.
- Arnault E, et al. Photoxic Action Spectrum on a Retinal Pigment Epithelium Model of Age-Related Macular Degeneration Exposed to Sunlight Normalized Conditions. PLoS ONE. 2013;8(8): e71398. doi:10.1371/journal.pone.0071398.
- Kuse Y, et al. Damage of photoreceptor-derived cells in culture induced by light emitting diode-derived blue light. Scientific Report 42014., 5223; DOI:10.1038/srep05223,.
- Noell, W et al. Retinal damage by visible light. Invest Ophtalmol. 1966; 5: 450-473
- lgvere P, et al. Age-Related maculopathy and the impact of blue light hazard. Acta Ophtalmol Scand.2006; 84: 4-15.
- Arnault E, et al. Phototoxic Action Spectrum on a Retinal Pigment Epithelium Model of Aged-Related Macular Degeneration Exposed to Sunlight Normalized Conditions. PLoS ONE. 2013; 8(8): e71398. doi:10.10371/journal. pone.0071388
- Sivak M et al. Blue content of LED head lamps and discomfort glare. UMTRI-2005-2
- Gray R, et al. Reduced effect of glare disability on driving performance in patients with blue light-filtering IOLs. J. Cataract Refract. Surg. 2011; 37:38-44
- Rosenfield M. Computer vision syndrome: a review of ocular causes and potential treatments. Ophthalmic Physiol Opt 2011, 31, 502–515. doi: 10.1111/j.1475-1313.2011.00834.x
- Rossignol AM, Morse EP, Summers VM & Pagnotto LD. Visual display terminal use and reported health symptoms among Massachusetts clerical workers. J Occup Med 1987; 29: 112–118.
- Tsubota K & Nakamori K. Dry eyes and video display terminals. N Engl J Med 1993; 328: 584–585
- Patel S, Henderson R, Bradley L et al. Effect of visual display unit use on blink rate and tear stability. Optom Vis Sci 1991; 68: 888–892
- Hatori M, et al. Global rise of potential health hazards caused by blue light-induced circadian disruption in modern aging societies. NPJ Aging Mech Dis. 2017;16: 3:9
- Flo E, et al. Shift-related sleep problems vary according to work schedule. Occup Environ Med 2013;70:238-245.
- Vyas M, et al. Shift work and vascular events: systematic review and meta-analysis. BMJ 2012;345:e4800.
- Kolstad H. Nightshift work and risk of breast cancer and other cancers-a critical review of the epidemiologic evidence. Scand J Work Environ Health 2008;34:5-22
- Bara A, Arber S. Working shifts and mental health-findings from the British Household Panel Survey (1995-2005). Scand J Work Environ Health 2009;35:361-367
- Karlsson B, et al. Is there an association between shift work and having a metabolic syndrome? Results from a population bases study of 27485 people. Occup Environ Med 2001;58:747-752.
- Morikawa Y, et al. Shift Work and the risk of diabetes mellitus among Japanese male factory workers. Scand J Work Environ Health 2005;31:179-183
- Chellappa SL, Steiner R, Blattner P, Oelhafen P, Go¨tz T, et al. (2011) Non-Visual Effects of Light on Melatonin, Alertness and Cognitive Performance: Can Blue-Enriched Light Keep Us Alert? PLoS ONE 6(1): e16429. doi:10.1371/journal.pone.0016429
- J Psychiatr Res. 2017 Apr;87:61-70. doi: 10.1016/j.jpsychires.2016.12.010. Epub 2016 Dec 12 Effects of smartphone use with and without blue light at night in healthy adults: A randomized, double-blind, cross-over, placebo-controlled comparison.
- Chang A, et al. Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proc Natl Acad Sci U S A. 2015; 27;112:1232-1237.
- Lawrenson JG, Hull CC & Downie LE (2017) The effect of blue-light blocking spectacle lenses on visual performance, macular health and the sleep-wake cycle: a systematic review of the literature. Ophthalmic Physiological Optics; 37: 644–654. https://doi.org/10.1111/opo.12406
- https://www.abdo.org.uk/wp-content/uploads/2017/12/ABDO-Blue-Light-Guidance-WEB.pdf
- Blue-Light Filtering Spectacle Lenses: Optical and Clinical Performances Tsz Wing Leung,Roger Wing-hong Li ,Chea-su Kee Published: January 3, 2017 https://doi.org/10.1371/journal.pone.0169114
- https://www.aop.org.uk/advice-and-support/policy/position-statements/visible-blue-light (accessed Feb 2018)
- Ophthalmology. 2007 Feb;114(2):253-62.
- Fifteen-year cumulative incidence of age-related macular degeneration: the Beaver Dam Eye Study. Klein R1, Klein BE, Knudtson MD, Meuer SM, Swift M, Gangnon RE
- www.pointsdevue.com/article/blue-light-paradox-problem-or-panacea
- Voke J. Radiation effects on the eye. Part 3b - Ocular effects of ultraviolet radiation. Optometry Today, 1999: July:37-40.
- van der Lely S. Blue blocker glasses as a countermeasure for alerting effects of evening light-emitting diode screen exposure in male teenagers. J Adolesc Health. 2015;56:113-119
- Verônica Castro Lima, Richard B. Rosen & Michel Farah. Macular pigment in retinal health and disease. International Journal of Retina and Vitreous volume 2, Article number: 19 (2016)
- Prof Russell Foster head of Nuffield Laboratory of Ophthalmology and Director of the Sleep and Circadian Neuroscience Institute at the university of Oxford speaking after presenting at European Society for Paediatric Endocrinology in Vienna 2019[54] Taylor H.R. The long-term effects of visible light on the eye. Arch Ophthalmol. 110(1):99-104, 1992
- Mitchell P. Iris color, skin sun sensitivity, and age-related maculopathy. The Blue Mountains Eye Study. Ophthalmology. 105(8):1359-63, 1998
- Fletcher AE. Sunlight exposure, antioxidants, and age-related macular degeneration. Arch Ophthalmol. 126(10):1396-403, 2008
- Butt AL. Prevalence and risks factors of age-related macular degeneration in Oklahoma Indians: the Vision Keepers Study. Ophthalmology. 118(7):1380-5, 2011
- Vojnikovic B. et al. ( 2010), Epidemiological study of sun exposure and visual field damage in children in Primorsko-Goranska County — the risk factors of earlier development of macular degeneration. Coll Antropol. 34(Suppl 2):57-9
- Huang EJ-C Prevalence and risk factors for age-related macular degeneration in the elderly Chinese population in south-western Taiwan: the Puzih eye study. Eye (2014) 28, February 2014
- Sui GY. Is sunlight exposure a risk factor for age-related macular degeneration? A systematic review and meta-analysis. Br J Ophthalmol. 2013 97: 389-394. November 2012
- Schick T. History of sunlight exposure is a risk factor for Age-Related Macular Degeneration. Retina 36:787–790, 2016
- Lamb LE. Retinyl Palmitate and the Blue-Light-Induced Phototoxicity of Human Ocular Lipofuscin. Archives of Biochemistry and Biophysics, Volume 393, Issue 2, 15 September 2001, 316 – 320
- Delcourt C. Light exposure and the risk of Age-Related Macular Degeneration. Clinical Sciences, October 2001 Arch Ophthalmol. 119(10):1463-1468.
- Taylor H.R. Visible Light and Risk of Age-Related Macular Degeneration. Trans Am Ophthalmol Soc. 1990; 88:163-73; discussion 173-8
- Millen A.E. Association between vitamin D status and age-related macular degeneration by genetic risk. JAMA Ophthalmol. 2015 October; 133(10): 1171–1179
- Werner J.S. Loss of Human Photoreceptor Sensitivity Associated with Chronic Exposure to Ultraviolet Radiation. Ophthalmology. 1989; 96(10): 1552-1558
- ISO TR 20772 - 2018 Ophthalmic optics — Spectacle lenses — Short wavelength visible solar radiation and the eye
- Singh S, Anderson AJ, Downie LE. Insights into Australian optometrists' knowledge and attitude towards prescribing blue light-blocking ophthalmic devices. Ophthalmic Physiol Opt. 2019 May; 39(3):194-204.
