With continuing advances in technology, eye care professionals now have a larger range of contact lens products to choose from than ever before. So, how can we be sure we are prescribing our patients with the right product to meet their needs?
This article uses patient examples to explore the contact lens selection decision-making process, with the aim to ensure we are making personalised contact lens recommendations for each of our patients based not only on their contact lens requirements, but also on their ocular health. In ensuring we provide patients with personalised recommendations, we hope to optimise our patient satisfaction and increase contact lens wearer retention. This practice will also ensure we are meeting the General Optical Council (GOC) Standards of Practice, treating our patients as individuals, taking into account their views and preferences when making decisions about their care.1
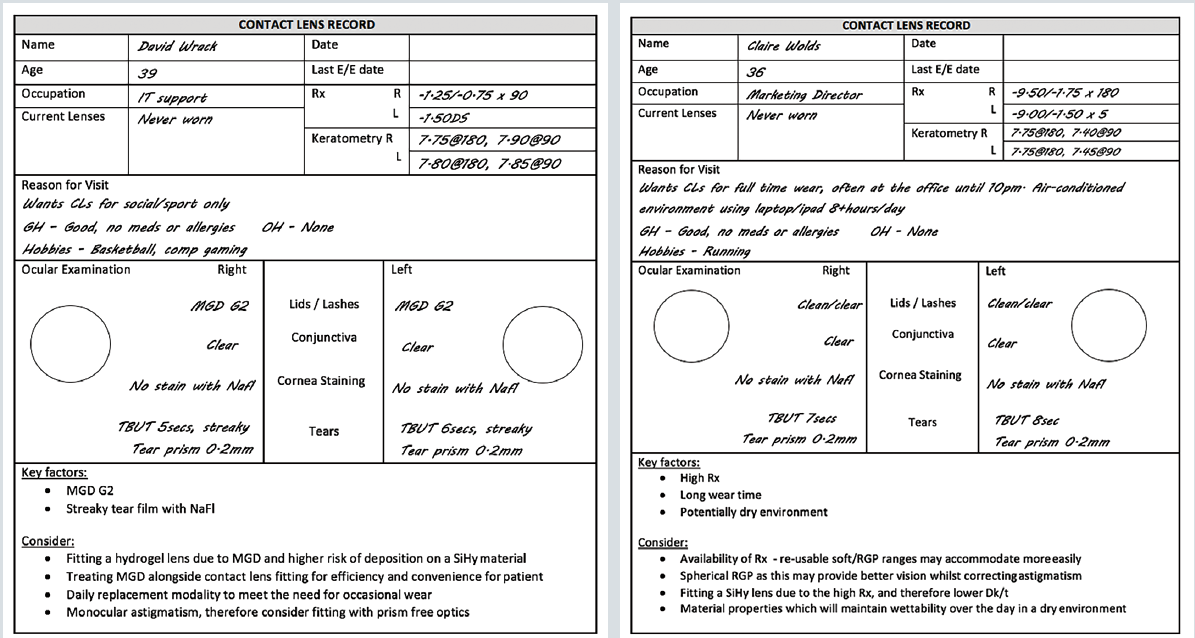
Patient examples
In creating a personalised contact lens recommendation for each patient, we need to consider the attributes of the lens we select to ensure it can provide our patient with optimum vision and comfort, while delivering safe and healthy wear. The following detailed contact lens properties should always be considered; material, optical design, material properties and modality. These elements, together with the patient’s lifestyle, ocular health and prescription requirements will help to inform our ideal contact lens choice.
Material Properties
The first decision to consider here is the material of the contact lens; should you fit a hydrogel or silicone hydrogel (SiHy) soft contact lens, or would a rigid gas permeable (RGP) contact lens better meet the patient’s needs?
Soft contact lenses continue to dominate most of the contact lens market, accounting for 87% of all fits worldwide.2 Options available to the practitioner continue to evolve, covering a wider range of parameters, designs and replacement frequencies. Historically, prescription of either daily disposable (DD) or re-usable (RU) hydrogel exceeded that of SiHy lenses, however, increasing preference for SiHy lenses led to a higher proportion of SiHy lenses being prescribed from 2015 onwards. While SiHy lenses continue to grow in popularity, the most prescribed brand of DD contact lenses worldwide remains a hydrogel.*
While there is a shift towards use of SiHy lenses due to their higher oxygen permeability, hydrogel contact lenses, with their naturally hydrophilic nature, low modulus and reduced tendency to attract lipid deposits,3 remain a good choice, particularly for patients who have marginal tear films and excess lipid contamination of the tears due to meibomian gland dysfunction.4 Oxygen transmissibility should of course be a consideration for each patient, however, recent clinical insights show us that at a Dk/t of approximately 20 units, the central cornea receives the oxygen it requires for normal oxygen consumption in the open eye state5 and many modern hydrogels fit within this range. There is also considerable evidence that market leading high-water content hydrogel lenses made of etafilcon A do not produce clinically significant levels of corneal oedema,6 or show any difference in central corneal oxygen consumption compared to a SiHy material, lotrafilcon A.
SiHy contact lenses, first introduced to market in the late 1990s, are again available in both DD and RU modalities and now make up 57% of fits worldwide and 76% of fits in the UK.2 Incorporation of silicone into the contact lens, produces a material with significantly increased oxygen permeability, meaning oxygen consumption for SiHy lenses is 98-100%,7 irrespective of make or model. When SiHy contact lenses first came to the market it was thought that greater oxygen transmissibility would also result in improved comfort levels and a reduction in adverse events, however, a comfort advantage with SiHy lenses has been hard to prove due to confounding factors8 and research has shown no relationship between Dk/t and comfort.9 This is likely due to the inherent hydrophobicity and stiff nature of silicone which meant that first generation SiHy lenses had a higher modulus and poorer wettability10 compared to their hydrogel counterparts. More modern SiHy materials have dealt with these concerns and now are available with highly desirable levels of comfort and tear film interaction.11 With regards to adverse events, despite SiHy lenses causing a reduction in hypoxic events, they have not brought about a reduction in risk of microbial keratitis as was anticipated12,13 and several studies have in fact shown a nearly two-fold increase in relative risk for infiltrative keratitis.14-16 These challenges aside, where consideration of oxygen transmissibility is important, for example, in patients who are predisposed to vascularisation secondary to the thicker designs of some toric lenses or higher spherical refractive errors, a SiHy would be the desired material of choice.
While RGP lenses only account for 10% of contact lens fits worldwide,2 their value should not be forgotten. RGP contact lenses can offer practitioners a larger prescription range, can correct corneal astigmatism up to 2.50DC with a simple spherical lens and are also available in toric and multifocal designs. Due to its rigid surface, RGP contact lenses have been shown to provide patients with preferable vision compared to soft contact lenses,17,18 likely due to neutralisation of corneal irregularities by the pre-corneal tear lens. As such, RGP lenses are included for the correction of corneal irregularity, such as keratoconus, post corneal graft and post-refractive surgery, as well as for high levels of ametropia or astigmatism. In addition to excellent vision, RGP lenses can support excellent corneal health due to incomplete corneal coverage and retro-lens tear exchange, resulting in an excellent safety record and a very low risk of microbial keratitis.19 However, these benefits come at a much longer adaptation period compared to soft contact lenses,18 which may account for the reduced prescribing of these lenses in mainstream practice over the past 20 years.2
It is clear from the information above that RGP, hydrogel and SiHy contact lenses all have a solid place in modern contact lens practice and practitioners should always select the best contact lens material for patients based on overall comfort, visual performance, safety and clinical need. As soft contact lenses make up 95% of contact lenses prescribed in the UK,2 the rest of the article will concentrate on the material properties associated with soft contact lenses only.
Deposition
Hydrogel and SiHy lenses differ in their deposition profiles, with wide variations also occurring within these lens types, depending upon the International Organisation for Standardization (ISO) classification as described in table 1 and figure 1. Both research and clinical experience recognise that, broadly, Hy contact lenses deposit more protein (figure 2 upper) compared to lipid (figure 2 lower), while the converse is true of SiHy. Furthermore, higher water content, ionic hydrogel materials have a tendency to attract greater amounts of protein compared to non-ionic lower water content hydrogel lenses. Once deposited on the contact lens surface, the protein can become denatured, triggering the release of inflammatory biomarkers which could result in irritation.20 However, if the proteins are simply taken into the lens and not denatured, as has been demonstrated in etafilcon A, a group IV hydrogel, they can support the maintenance of low levels of inflammatory biomarkers, that could result in less irritation.21
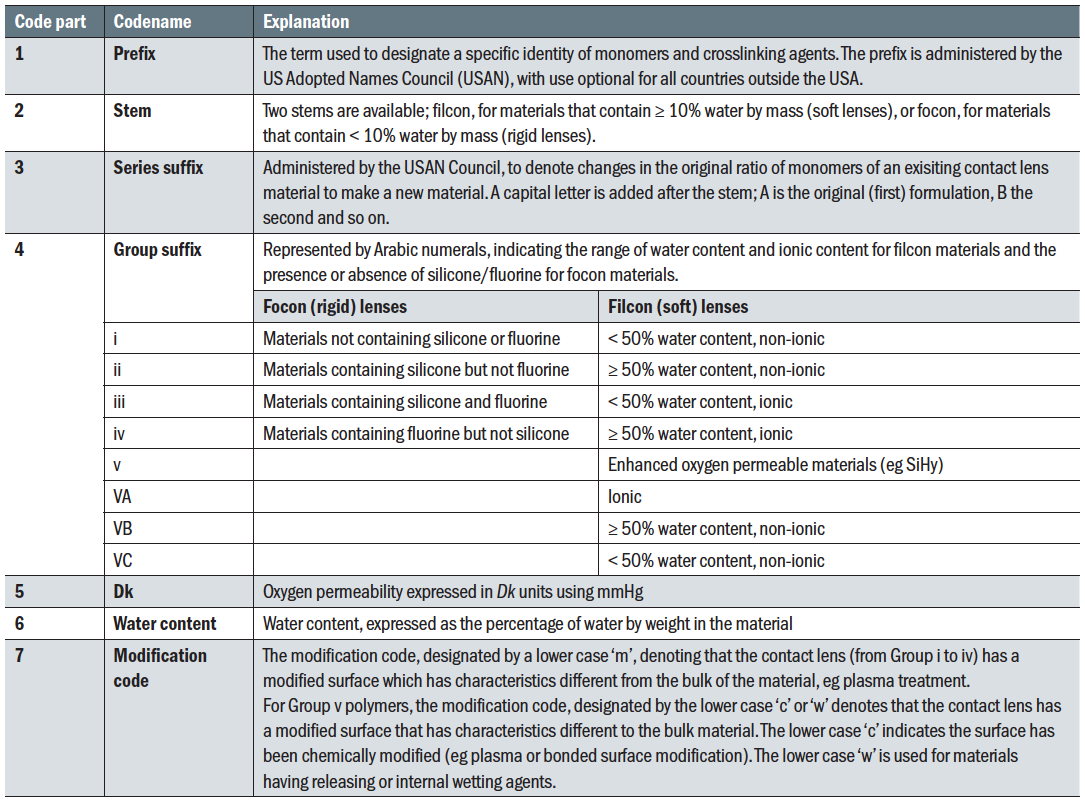 Table 1: ISO System of Contact Lens Materials Classification in a seven-part code23
Table 1: ISO System of Contact Lens Materials Classification in a seven-part code23
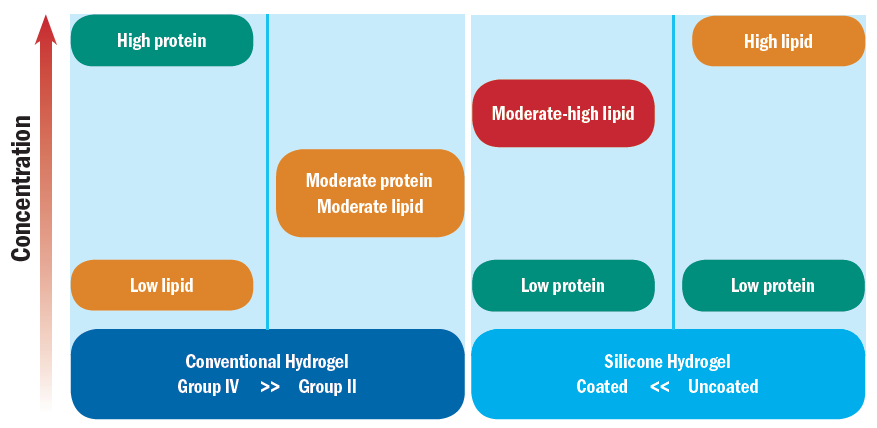
Figure 1: Schematic illustration of trends in lipid and protein deposits on different contact lens materials (After Mann A and Tighe B. Contact lens interactions with the tear film. Experimental Eye Research, 2013;117:88-98) 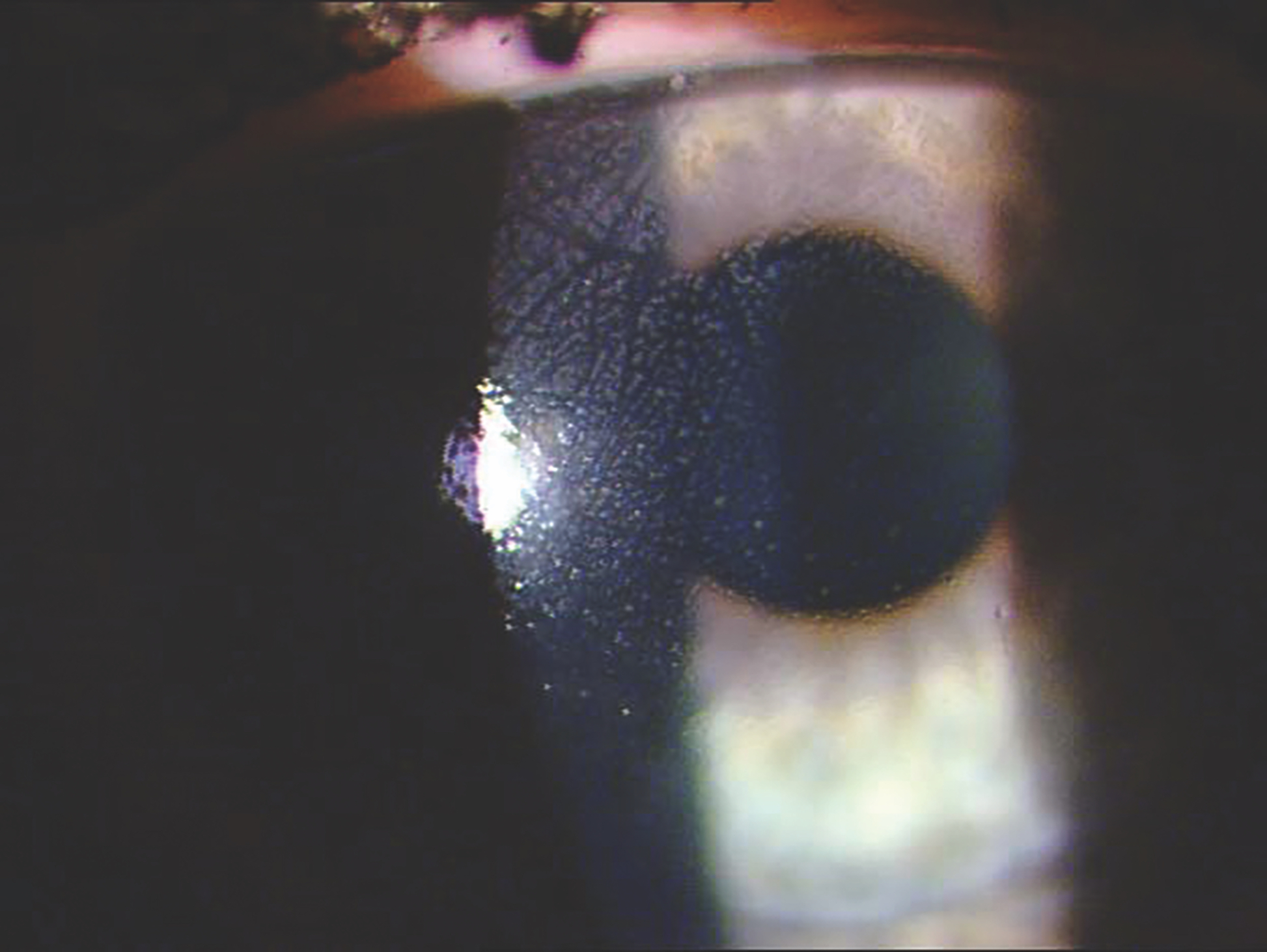
Figure 2: Deposition of protein (above) is more common with hydrogel lenses compared to lipid (below) with SiHy lenses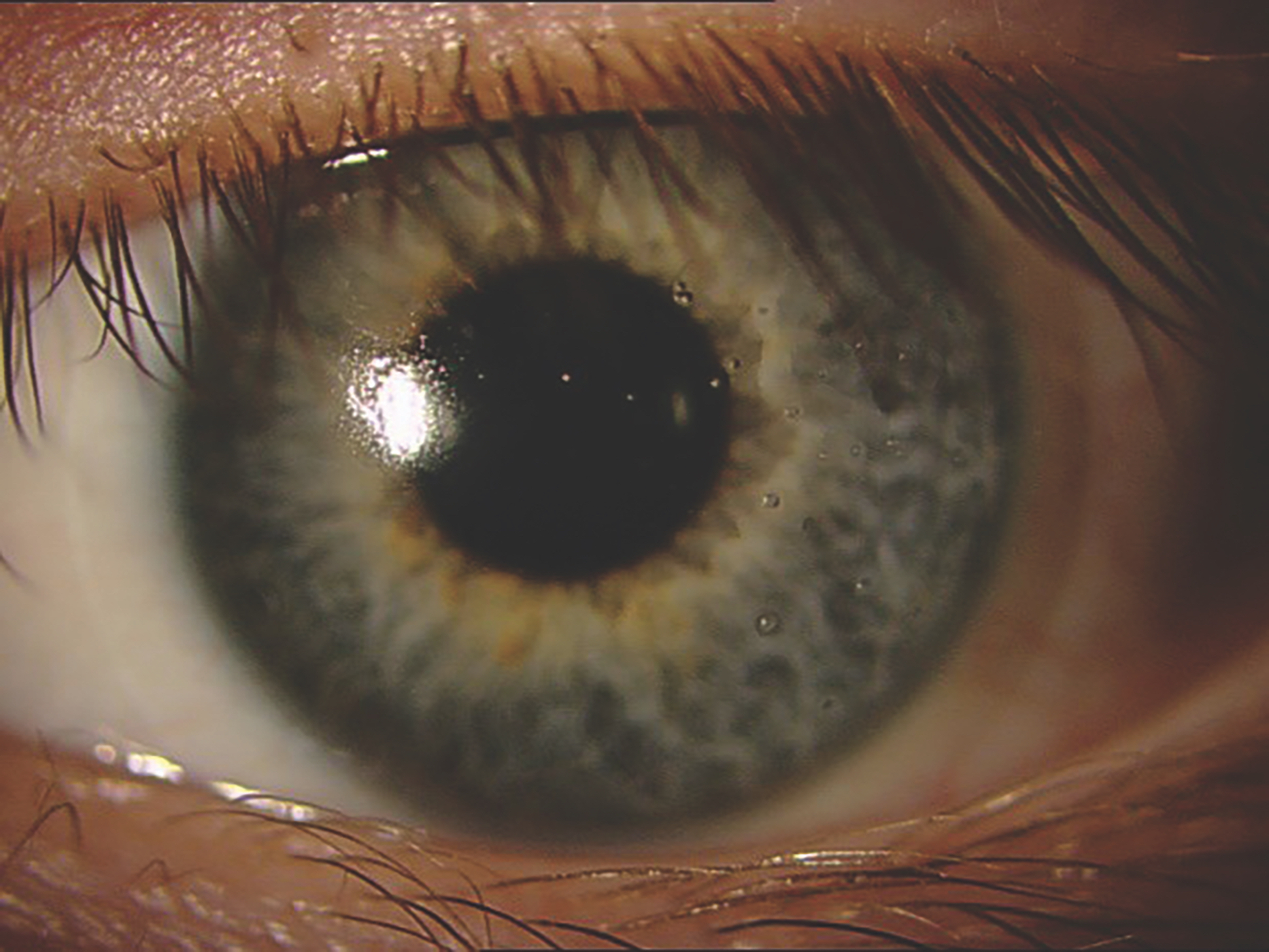
Knowledge of the differences in deposition profile can be useful when considering matching a contact lens material to a patient’s ocular surface. For example, a patient with meibomian gland dysfunction who is prone to exhibiting high levels of cholesterol in their tears, may benefit from being fitted with a hydrogel material where possibility of lipid deposition is lower.22
Modulus
When considering matching a contact lens to a patient, the modulus of the lens is one of the material properties that should be considered. The modulus, a mechanical property of the lens, describes the tensile, or elastic, strength of the lens, and together with the lens thickness denotes how easily the lens will drape over the cornea. Where the thickness of a lens remains constant, a reduction in the material modulus will create a lens which more easily drapes over anterior surface. While researching the effect of modulus on contact lens comfort is challenging due to confounding material factors, research suggests that a negative correlation exists between modulus and patient comfort, that is, as modulus increases, patient reported comfort decreases.10 This was evident when fitting patients into first generation SiHy lenses where the tensile modulus was significantly higher than typical hydrogel lenses and an adaptation time was needed.24 Risk of mechanically induced ocular complications, such as superior epithelial arcuate lesion (SEAL) stain (figure 3) or contact lens induced papillary conjunctivitis (CLPC) (figure 4), were also high in first generation SiHy lenses, a complication which is rarely seen with more modern SiHy materials where the modulus is much lower.25,26 While a lower modulus may have a beneficial impact on comfort, it can cause problems with handling, so could cause challenges for patients with poor dexterity. Without a standard method for calculation of modulus, the values reported through different studies cannot be directly compared. The modulii values of a range of daily disposable contact lenses are shown in figure 5, as reported by Sulley et al, as measured using one technique.27
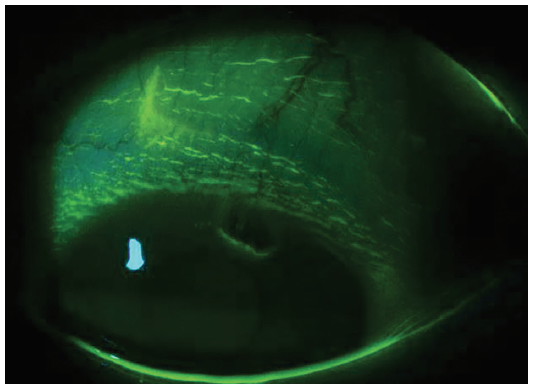 Figure 3: Superior epithelial arcuate lesion, a mechanical complication associated with high modulus contact lenses
Figure 3: Superior epithelial arcuate lesion, a mechanical complication associated with high modulus contact lenses
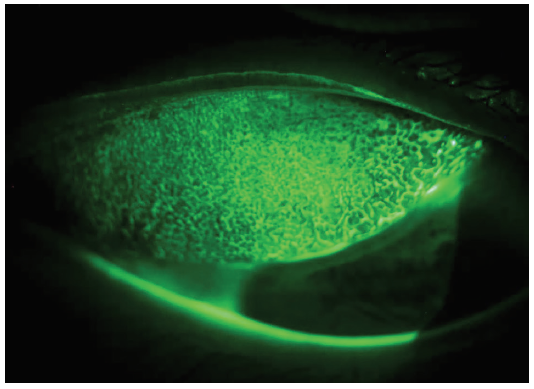 Figure 4: Contact lens papillary conjunctivitis (CLPC), a complication associated with high modulus contact lenses
Figure 4: Contact lens papillary conjunctivitis (CLPC), a complication associated with high modulus contact lenses
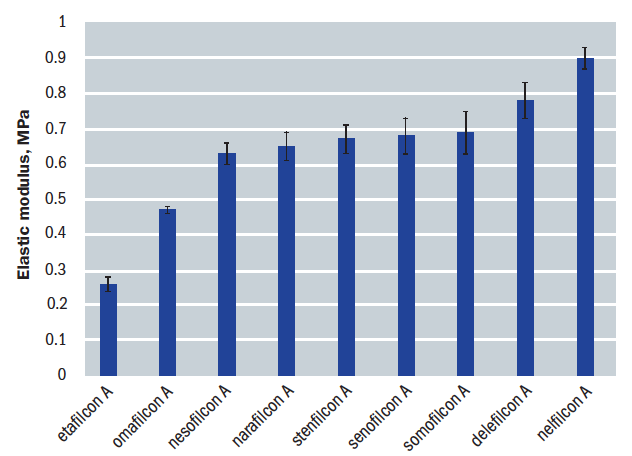
Figure 5: Mean modulus of elasticity values for a range of daily disposable contact lenses, investigated by Sulley et al.27 Error bars represent the standard deviation of the mean.
Coefficient of friction
The coefficient of friction of the lens material is another vital material property to consider. Defined as the force required to move an object divided by its mass, it indicates the resistance the upper lid will have when passing over the contact lens surface when blinking.18 A low coefficient of friction (or high lubricity) relates to the ability of the eyelid to travel smoothly across the front surface of the contact lens without irritation. There is considerable evidence showing a strong correlation between coefficient of friction and mean comfort, where comfort increases as coefficient of friction decreases.28,29
No standard method has been developed or adopted by the industry to measure coefficient of friction, therefore contact lens companies may use different methods, yielding different results, making comparison between companies challenging. The dynamic coefficient of friction of several different contact lens materials, measured using the same technique, are shown in figure 6.
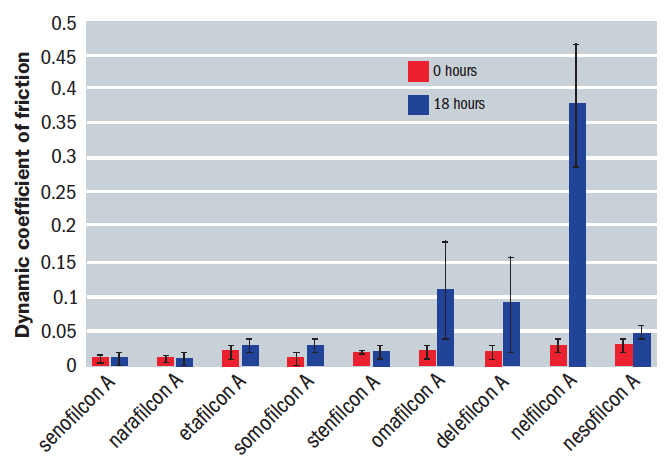
Figure 6: Mean dynamic coefficient of friction for a range of daily disposable contact lens materials at 0 hours (grey bars) and 18 hours (blue bars) simulated wear.32,33 Error bars represent the standard deviation of the mean
Lid-parallel conjunctival folds (LIPCOF, figure 7) and lid wiper epitheliopathy (LWE, figure 8) are thought to be clinical indicators of friction and are associated with increased contact lens discomfort.30,31 Examination of the ocular adnexa for signs LIPCOF and LWE is therefore advised during contact lens aftercare, with presence indicating potential need to move the patient into a more lubricious material.
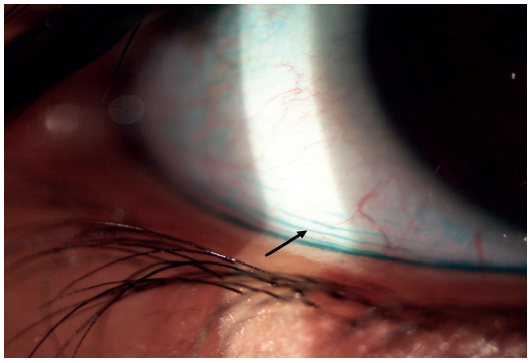 Figure 7: Lid parallel conjunctival folds (LIPCOF), visibility enhanced with Lissamine Green Dye (black arrow)
Figure 7: Lid parallel conjunctival folds (LIPCOF), visibility enhanced with Lissamine Green Dye (black arrow)
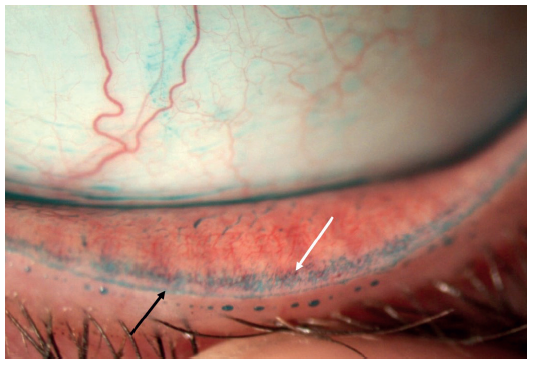
Figure 8: Lid wiper epitheliopathy (LWE) stained with Lissamine Green, showing stain (white arrow) extending beyond Marx line (black arrow)
Wettability
The term ‘wettability’ describes the ability of the tear film to spread across and remain on a contact lens surface. The more wettable the contact lens material is, the better the tear film forms a cohesive film across the lens surface and does not dry or thin between blinks. Wettability is intrinsically linked to the coefficient of friction of a lens, in that as wettability reduces, coefficient of friction will increase.
Traditionally, wettability has been assessed in vitro by measuring the contact angle of a sessile droplet of water or saline on the contact lens,34,35 with a lower contact angle indicating better wetting. However, these in vitro measurements do not appear to show any relationship to on-eye clinical wetting, therefore are of limited value. In vivo wettability is perhaps more useful, though the link between in vivo wettability and comfort is yet to be fully understood. In vivo wettability has been assessed in research using a variety of simple techniques which can be translated into clinical practice, including measurement of pre-lens non-invasive tear break up time (NITBUT)36,37 and assessment using specular reflection.38 Wettability can easily be assessed in practice using either of these techniques, as demonstrated in figure 9.
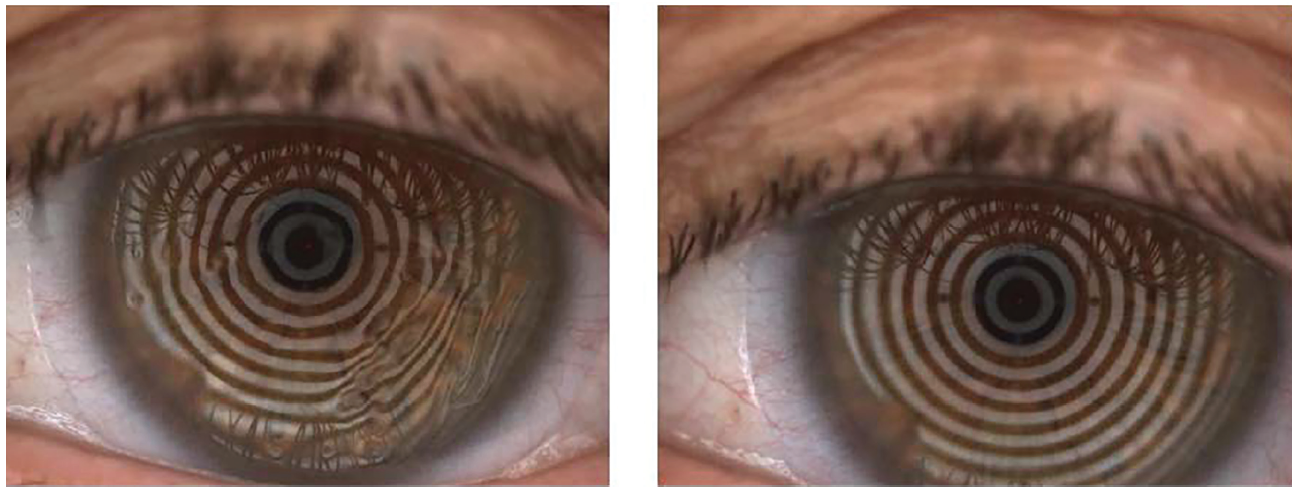 Figure 9: Assessment of pre-lens tear film break up time to provide information on contact lens wettability. Poor contact lens wetting is observed as distortion of Placido rings (left), versus good wetting (right)
Figure 9: Assessment of pre-lens tear film break up time to provide information on contact lens wettability. Poor contact lens wetting is observed as distortion of Placido rings (left), versus good wetting (right)
Design
All contact lenses are designed differently, with a range of base curves, diameters and edge profiles available and it is recognised that the comfort of the lens can potentially be affected by these differing design features.24 Certainly, the design of a lens can influence how the lens fits the patient and the comfort this brings. Eye care professionals who regularly fit soft contact lenses know to assess movement of the lens on eye39,40 and corneal coverage41 to determine if we think the fit may be successful, as both of these elements are believed to impact patient comfort. Likewise, with RGP fitting we look at how the lens edge interacts with the lids on blink to consider optimum wearer comfort. The edge profile of a lens is another design element that can have an impact on comfort and that does vary between lenses. The edge profile of a lens can be classified as either tapered, edge-on-eye design, or as rounded/block, edge-off-eye design (figure 10). The Tear Film and Ocular Surface (TFOS) International Workshop on Contact Lens Discomfort24 reported that studies have shown that lenses with a rounded, edge-off-eye design tend to provide poorer comfort compared to lenses with tapered, edge-on-eye designs,42 with the tapered designs providing a smoother transition between the conjunctiva and the lens surface,43 with less movement.24
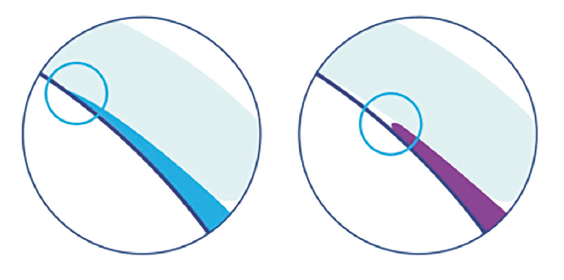
Figure 10: Diagrams showing a tapered, edge-on-eye design (left) and a rounded/block, edge-off-eye design (right). (Image supplied by Johnson & Johnson Vision)
It is worth educating our patients to know that contact lens designs do vary and can bring wearer benefits. They will recognise and appreciate our clinically advised product recommendation even more if we are able to articulate to them the features and benefits of the specific lenses we are recommending. It makes sense to speak to your contact lens manufacturers to obtain detailed design information regarding the products you routinely fit or have access to, having knowledge of the features and benefits of each design will again lead to more successful fitting and less potential for trial and error.
Recognising and fully considering these design differences as part of the fitting process for our presbyopic patients will ensure a much more likely first time successful fit.
Modality
Modality, or frequency of lens replacement, also needs to be considered when selecting a lens for patients. In the UK, practitioners now prescribe daily lenses 62% of the time,24 with this shift likely driven by convenience and reduced risk of infection.44 Re-usable lenses typically offer a wide range of prescription parameters and may well be the only option for some patients, while also offering a more cost-effective solutions for patients who are price conscious. While there is no strong evidence showing a direct link between the modality of a lens and comfort,22 it is widely recognised that build-up of deposits on certain lens materials can lead to higher discomfort in wearers of some re-usable contact lens materials on the market. It should also be noted that comfort in monthly lenses is likely to reduce over the month,45 so patient satisfaction should be carefully assessed at each aftercare to avoid the patient ceasing lens wear due to comfort issues.
Cost
Once we have fully considered the patient’s lifestyle needs, their ocular health and the material properties of the lenses available to create the perfect match, the appropriate lens should be recommended to the patient with clear reasons as to why this lens best meets their requirements. Price is shown in studies to be a secondary consideration46 for most patients (figure 11), especially when you consider cost per wear which often equates to a difference of just a few pence per day. However, once the patient is informed of the cost of the recommended lens, if it is not suitable, then you can work together to see if a more cost-effective option is available and advise them of the loss of benefit that this contact lens option may deliver.
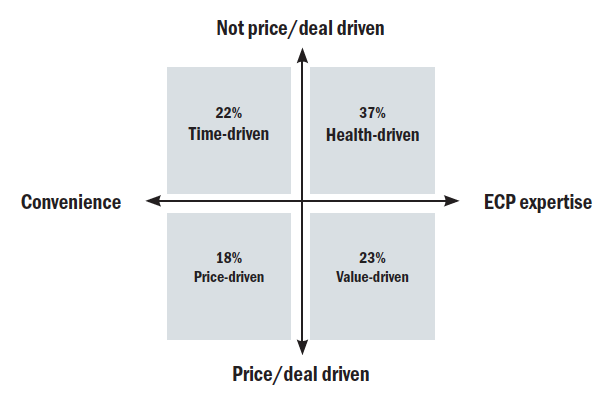
Figure 10: Patient motivations to healthcare in the UK46
Additional considerations for maximum success
While it is paramount that eye care professionals stay fully up to date with new innovations in terms of design and material properties, it is the ability to apply these elements to each individual patient, that will ultimately lead to successful, long-term contact lens wear. If, for example, ocular examination revealed hyperaemia and papillae on lid eversion, and the patient reported suffering seasonal hay fever, we may wish to recommend daily disposable contact lenses as a matter of course. Daily disposable contact lenses would best serve the patient by minimising the build-up of both deposits and allergens, with research showing that hydrogel daily disposables provide both increased comfort and a protective element for such individuals.47,48 Environmental factors and previous patient history should also be taken into account when considering an appropriate contact lens recommendation. A patient with a history of infection would undoubtedly benefit from a daily disposable modality, where risk of infection is lower,49 as would patients who smoke, due to the increased risk of corneal infiltrative events and microbial keratitis.50
Summary
In making tailored contact lens recommendations for patients, we must ensure we match our patient’s needs and ocular health with the most appropriate contact lens, taking into account material properties and design in doing so. This personalised recommendation should then be clearly communicated with the patient, so that they are able to understand the importance of the contact lens fitting process and indeed aftercare in ensuring they have successful contact lens wear. The key to optimum recommendation for maximum success is to be knowledgeable about the products that are available and able to apply this knowledge when factors affecting suitability come in to play. Prescribing contact lenses is both a science and an art and can be very rewarding to both ourselves and our patients when we get it right.
Robyn Marsden is an optometrist and a paid consultant faculty member for the Johnson & Johnson Institute, UK and a Professional Affairs Consultant for Johnson & Johnson Vision. Dr Rachel Hiscox is a Professional Education & Development Manager, UK & Ireland for Johnson & Johnson Vision Care.
• This article is part of a revised and updated ‘Essential Contact Lens Practice’ series, originally authored by Jane Veys, John Meyler and Ian Davies. This article was produced without further input or review from the original authors.
*Source: Euromonitor International Limited; based on research conducted in August 2019; “world” and “globally” represent markets accounting for 80.8% of total daily disposable contact lenses in 2018 (retail sales). Claim effective starting August 10, 2019
References
- GOC: Standards of practice for Optometrists and Dispensing Opticians April 2016
- Morgan P et al, International Contact Lens Prescribing in 2019. Contact Lens Spectrum, 2020;35:26-32
- Nichols JJ. Deposition on silicone hydrogel lenses. Eye Contact Lens. 2013 Jan;39(1):20-23
- Ghormley N, Jones L. Managing lipid deposition on silicone hydrogel lenses. Contact Lens Spectrum 2006;21(1):21
- Brennan NA. Beyond flux: total corneal oxygen consumption as an index of corneal oxgenation during contact lens wear. Optom Vis Sci 2005;82:6 467-72
- Szczotka-Flynn LB, Raghupathy S, Debanne S et al. Daily wear central corneal swelling with etafilcon A is non-inferior to two silicone hydrogel lens types. Optom Vis Sci 2015; 92
- Brennan, Noel and Morgan, Philip. Part I: Clinical Highs & Lows of Dk/t. Has oxygen run out of puff? Optician, 2009, Vol 238, No 6209, 16–20
- Guillon M. Are silicone hydrogel contact lenses more comfortable than hydrogel contact lenses? Eye Contact Lens 2013;39(1):86-92
- Brennan N. Contact lens based correlates of soft contact lens wearing comfort. Optom Vis Sci, 2009;86:E-abstract 90957
- Jones L, Subbaraman LN, et al. Surface treatment, wetting and modulus of silicone hydrogels. Optician 2006;232(6067):28-34
- McParland M, Pall B, Schnider C. New lens for demanding days. Optician 2016 251; 6555: 24-28
- Dart JK, Radford CF, et al. Risk factors for microbial keratitis with contemporary contact lenses: a case-control study. Ophthalmology 2008;115(10):1647-54, 1654 e1-3
- Stapleton F, Keay L, et al. The incidence of contact lens-related microbial keratitis in Australia. Ophthalmology 2008;115(10):1655-62
- Chalmers RL, Keay L, et al. Multicenter case-control study of the role of lens materials and care products on the development of corneal infiltrates. Optom Vis Sci 2012;89(3):316-25
- Chalmers RL, Wagner H, et al. Age and other risk factors for corneal infiltrative and inflammatory events in young soft contact lens wearers from the Contact Lens Assessment in Youth (CLAY) study. Invest Ophthalmol Vis Sci 2011;52(9):6690-6
- Radford CF, Minassian D, et al. Risk factors for nonulcerative contact lens complications in an ophthalmic accident and emergency department: a case-control study. Ophthalmology 2009;116(3):385
- Fonn D, Gauthier CA, Pritchard N. Patient preferences and comparative ocular responses to rigid and soft contact lenses. Optom Vis Sci. 1995;72(12):857–863
- Fonn D, Holden BA. Rigid gas-permeable vs. hydrogel contact lenses for extended wear. Am J Optom Physiol Opt. 1988;65(7):536–544
- Stapleton F, Keay L, Edwards K, et al. The incidence of contact lens-related microbial keratitis in Australia. Ophthalmology. 2008;115(10):1655–166
- Omali NB, Subbaraman LN, Coles-Brennan C et al. Biological and clinical implications of lysozyme deposition on soft contact lenses. Optom Vis Sci 2015;92:7 750-7
- Omali NB, Subbaraman LN, Coles-Brennan C, Fadli Z, Jones LW. Biological and Clinical Implications of Lysozyme Deposition on Soft Contact Lenses. Optom Vis Sci. 2015;92(7):750–757
- Sulley A. Getting comfortable with deposits. Optician 2015;250:6522 20-22
- BS EN ISO 18369-1:2017. Ophthalmic Optics. Contact Lenses. Vocabulary, classification system and recommendations for labelling specifications
- Jones L, Brennan NA, González-Méijome J, et al. The TFOS International Workshop on Contact Lens Discomfort: report of the contact lens materials, design, and care subcommittee. Invest Ophthalmol Vis Sci. 20 13;54(11):TFOS37–TFOS70
- Dumbleton K. Adverse events with silicone hydrogel continuous wear. Cont Lens Anterior Eye. 2002;25:137–146
- Lin MC, Yeh TN. Mechanical complications induced by silicone hydrogel contact lenses. Eye Contact Lens. 2013;39: 115–124
- Sulley et al. Daily disposable and reusable contact lens moduli – Are they really different? CLAE, 2018;41:S54
- Brennan NA. Contact lens based correlates of soft lens wearing comfort. Optom Vis Sci, 2009;86:e-abstract 90957
- Coles CML, Brennan NA. Coefficient of friction and soft contact lens comfort. Optom Vis Sci, 2012;88:e-abstract 125603
- Pult H, Purslow C, Berry M, Murphy PJ. Clinical tests for successful contact lens wear; relationship and predictive potential. Optom Vis Sci, 2008;85:E924-9
- Korb DR, Greiner JV, Herman JP, et al. Lid-wiper epitheliopathy and dry-eye symptoms in contact lens wearers. CLAO J. 2002;28:211–216
- Sterner O, Aeschlimann R, Zurcher S, Osborn Lorenz K, Kakkassery J, Spencer ND, Tosatti S. Friction Measurements on Contact Lenses in Their Operating Environment: Effect of Testing Conditions on Friction. IOVS 2016 Oct;57(13):5383-5392
- JJV Data on File 2018. Material Properties: 1-DAY ACUVUE® MOIST, 1-DAY ACUVUE® TruEye® and ACUVUE OASYS® 1-Day with HydraLuxe Technology Brand Contact Lenses and other daily disposable contact lens brands
- Read ML, Morgan PB, Kelly JM, Maldonado-Codina C. Dynamic contact angle analysis of silicone hydrogel contact lenses. J Biomater Appl. 2011;26:85–99
- Lin MC, Svitova TF. Contact lenses wettability in vitro: effect of surface-active ingredients. Optom Vis Sci. 2010;87:440– 447
- Guillon M, Styles E, Guillon JP, Ma¨ıssa C. Preocular tear film characteristics of nonwearers and soft contact lens wearers. Optom Vis Sci. 1997;74:273–279
- Guillon JP. Non-invasive Tearscope-Plus routine for contact lens fitting. Cont Lens Anterior Eye. 1998;21(suppl 1):S31– S40
- Shiobara M, Schnider CM, Back A, Holden BA. Guide to the clinical assessment of on-eye wettability of rigid gas permeable lenses. Optom Vis Sci. 1989;66:202–206
- Hoekel JR, Maydew TO, Bassi CJ, Bennett ES, Henry VA. An evaluation of the 8.4 mm and the 8.8 mm base curve radii in the Ciba NewVue vs the Vistakon Acuvue. Int Contact Lens Clin. 1994;21:14–18
- Young G. Evaluation of soft contact lens fitting characteristics. Optom Vis Sci. 1996;73:247–254
- McNamara NA, Polse KA, Brand RJ, Graham AD, Chan JS, McKenney CD. Tear mixing under a soft contact lens: effects of lens diameter. Am J Ophthalmol. 1999;127:659–665
- Maissa C, Guillon M, Garofalo RJ. Contact lens-induced circumlimbal staining in silicone hydrogel contact lenses worn on a daily wear basis. Eye Contact Lens. 2012;38:16– 26
- Shen M, Cui L, Riley C, Wang MR, Wang J. Characterization of soft contact lens edge fitting using ultra-high resolution and ultra-long scan depth optical coherence tomography. Invest Ophthalmol Vis Sci, 2011;52:4091– 4097
- Stapleton F. et al. Risk factors for moderate and severe microbial keratitis in daily wear contact lens users. Ophthalmology, 2012; 119(8):1616-21
- Frangie J, Schiller S, Hill LA. Understanding lens performance for wearers of monthly replacement contact lenses. Optom Today. 2008;48:39–42
- JJV Data on File 2017. Independent market research, 2017, UK, CL Wearers (n=493)
- Hayes VY, Schnider CM, Veys J: An evaluation of 1-day disposable contact lens wear in a population of allergy sufferers. Cont Lens Anterior Eye 2003; 26: 85-93
- Wolffsohn JS, Emberlin JC: Role of contact lenses in relieving ocular allergy. Cont Lens Anterior Eye 2011; 34: 169- 72.
- Chalmers RL, Hickson-Curran SB, Keay L, Gleason WJ, Albright R: Rates of adverse events with hydrogel and silicone hydrogel daily disposable lenses in a large postmarket surveillance registry: The TEMPO Registry. Invest Ophthalmol Vis Sci 2015; 56: 654-63
- McNally JJ, Chalmers RL, McKenney CD, Robirds S: Risk factors for corneal infiltrative events with 30-night continuous wear of silicone hydrogel lenses. Eye Contact Lens 2003; 29: S153-6; S166, S192-4
