Most of our patients, especially older adults, suffer from systemic pathologies that require various drug treatments. A large number of these substances, however, beside their intended actions, also induce side effects, some of them at the ocular level. Indeed, due to its highly vascularised structure, the eye is particularly vulnerable to any substances that enter the blood stream. Optometrists should at least be aware of the most common such effects. Indeed, alongside knowledge of systemic pathologies for appropriate positive and differential diagnoses, optometrists should also know when to follow up more closely patients taking certain systemic medications. This is especially important when one remembers that some of the side effects of these medications can be toxic and can produce irreversible ocular changes.
The severity of the ocular side effects of various systemic drugs is determined in each patient by several factors:1
- Individual patient characteristics, such as age and gender and history of allergies.
- Individual patient idiosyncrasies (such as abnormal reactions to drugs).
- Other pathologies the patient suffers from. In patients suffering from liver of kidney diseases, drugs will accumulate in higher doses because these disorders will affect the patient’s ability to eliminate toxic substances.
- The nature of the drugs. Side effects occur more often after treatment with drugs that pass easily into the general circulation.
- The quantity of the drug. Side effects occur more often after more prolonged treatments and high dosages.
- The way the drug is administered – topically, orally or by
injections. - The use of multiple drugs – this will increase the risk of
toxicity.
Cholesterol lowering medication
High cholesterol, especially low-density lipoprotein (LDL) cholesterol that binds to artery walls, is a known high-risk factor for cardiovascular disease (CVD). In addition, signs of high levels of cholesterol can also be detected at the eye level. Arcus, xanthelasma, and retinal artery occlusions are such manifestations (figure 1).

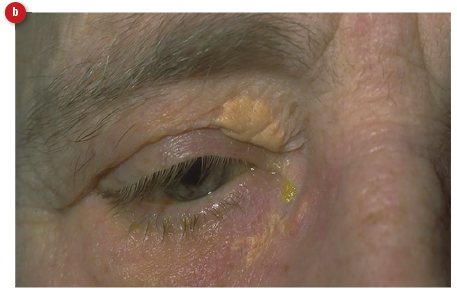
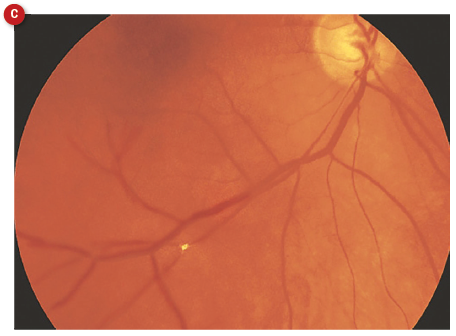 Figure 1: Manifestations of hyperlipidaemia; (a)arcus, (b) xanthelasma, (c) Hollenhorst plaque in a retinal artery branch
Figure 1: Manifestations of hyperlipidaemia; (a)arcus, (b) xanthelasma, (c) Hollenhorst plaque in a retinal artery branch
High levels of cholesterol are treated using a number of drugs, of which the most commonly prescribed are statins. These drugs were first introduced in 1987 and are used in all at-risk patients, those with atherosclerosis and CVD as well as in those suffering from dyslipidaemia.
There are many types of statins on the market, including:
- Atorvastatin (Lipitor)
- Fluvastatin (Lescol)
- Pravastatin (Lipostat)
- Rosuvastatin (Crestor)
- Simvastatin (Zocor)
It is known that statins are associated with a number of systemic side effects, most of which are represented by various muscle pains and weakness. In addition, it has been identified that statins can result in ocular side effects. These include:
- Lid oedema
- Dry eye
- Haemorrhages
- Diplopia
- Myopia
- Blurred vision
- Visual field defects
- Ptosis
- Macular oedema
- Lens opacities
- Ophthalmoplegia
These effects do not appear immediately but after an average of 156 days of treatment and are dose dependent.2 A retrospective study looking at the statin-associated ocular adverse effects, undertaken by the Food and Drug Administration (FDA) and Adverse Drug Reactions Advisory Committee (ADRAC), found that all statins were associated with some ocular side effects but atorvastatin and simvastatin presented the greater risk.2 The authors of this article also mentioned that patients already suffering from muscle or liver diseases were at greater risk of ocular complications after treatment with statins. These usually, however, disappear once the treatment is interrupted. If our patients present with ocular symptoms that affect their daily life, practitioners should first link these to the treatment with statins and then refer the patients to their GP for a possible change in their medication.
Despite the above possible undesirable side effects, treatment with statins can also have positive outcomes for ocular health. Statins have pleiotropic effects and inhibit various signalling proteins that promote processes including inflammation, oxidation, platelet aggregation, increase sympathetic outflow and vasoproliferation. It has also been proposed that the use of statins protects retinal ganglion cells (RGCs) against glaucomatous damage.3 Statins may also increase nitric oxide (NO) production and aqueous outflow which, in turn, result in lower IOP.4,5 In addition, it has also been reported that the use of statins in patients with suspected glaucoma decreased their risk of progressing to primary open angle glaucoma (POAG).6 Moreover, the use of statins in glaucoma patients has resulted in disease stabilisation.
Blood pressure and other CVD medication
Often, during history taking, we come across patients suffering from hypertension or a ‘heart problem’. It is important to establish not only the type of disease they are reporting, but also the treatment they receive because, in some cases, these treatments might have certain ocular side effects with important consequences to their optometric management.
Anti-hypertensives
Systemic hypertension is the most common vascular complication and is associated with advancing age. In the UK, hypertension affects one in four adults and its various related complications cost the NHS more than £2.1 billion every year. Therefore, it is very likely that many of our patients will suffer from this disease and will receive various anti-hypertensive drugs to keep their blood pressure (BP) under control. Sometimes systemic anti-hypertensive medications have an effect on the intraocular pressure (IOP) and, as such, they may mask a high IOP in an undiagnosed POAG patient. In this article, I will mention only the most common anti-hypertensive drugs.
Beta-blockers
Beta-blockers (such as atenolol and bisoprolol) represent a class of drugs that act through blocking the action of adrenaline. This, in turn, will slow down the heart rate and lower the BP. Used as a first line therapy for systemic hypertension in the past, beta-blockers are now considered less effective than the newer classes of anti-hypertensive drugs.
It is well known that systemic beta-blockers also lower IOP and, therefore, could have a protective effect against POAG.7 Beta-blockers are categorised as follows:
- Non-selective beta-blocker
- Cardio-selective beta-1 blocker
- Non-selective beta-blocker with intrinsic sympathomimetic activity (ISA)
Those that have an effect on IOP (atenolol, pindolol and nadolol) belong to the non-selective categories and act in a similar way to their topical equivalents.8
Calcium channel blockers
Calcium channel blockers act by preventing calcium entering cells of the heart and blood vessel walls. As calcium is very important for muscle contraction control, the main effect of calcium channel blockers on lowering the BP is through vasodilation. In addition, these drugs also promote increased oxygenation of heart muscle and, therefore, are also used in treating angina (as discussed later in this article).9 Calcium channel blockers are categorised as follows:
- Dihydropyridines – these include ifedipine, isradipine, felodipine, nicardipine, nisoldipine, lacidipine, amlodipine, and levamlodipine. These drugs are mainly vasodilators and, as such, are used in treating hypertension and chronic angina.10
- Non-dihydropyridines – these include verapamil and diltiazem. They are also used in treating hypertension and chronic angina. As they have an effect on cardiac contractility and electrical conduction, they are also used in treating
arrhythmias.
According to recommendations from the 2017 American College of Cardiology/American Heart Association (ACC/AHA) guideline for the prevention, detection, evaluation, and treatment of high blood pressure, calcium channel blockers are the recommended choice for the initial management of hypertension, either as monotherapy or as part of anti-hypertensive combination therapy. They are also used for stroke prevention.11
Previous research in animals and humans has shown that calcium channel blockers might benefit eyes with glaucoma by increasing blood flow to the optic nerve.12 In addition, it has been proposed that topical calcium channel blockers (verapamil and diltiazem) could reduce the IOP based on animal models.13 That said, other studies have shown that the use of the systemic calcium channel blocker amlodipine was associated with a 26% increased risk of POAG requiring non-pharmacological control.14,15 These contradictory results suggest further research is needed.
Diuretics
Diuretics stimulate renal excretion of water and electrolytes and, hence, reduce the BP. In addition, they promote arteriolar vasodilation. It has been proposed that diuretics, through changes in the body’s water balance, can cause dry eye and a myopic shift.16 Conjunctivitis, corneal epithelial damage and staining secondary to decreased tear production have also been reported. Nevertheless, these effects are rare.
Angiotensin converting enzyme (ACE) inhibitors
ACE inhibitors block angiotensin II production, therefore inducing vasodilation and lower BP. They are also used in the treatment of coronary heart disease (CHD), heart failure, heart attack, diabetes, kidney and skin diseases as well as managing migraine. As well as a beneficial effect on IOP, the use of ACE inhibitors has been reported to be associated with decreased vision, photophobia and conjunctivitis as well as retinal haemorrhaging.17
Anti-anginal drugs
Angina represents chest pain due to cardiac ischaemia through blockage of the coronary arteries. The most commonly prescribed anti-anginal drug is glyceryl trinitrate (nitroglycerin). It can be dispensed in tablet form or as a sublingual spray. The main effect of this drug is vasodilation of the coronary arteries and, hence, an increase to the blood supply to the heart. At the ocular level, it has been reported that nitroglycerin can cause coloured halos, variation in IOP, and may lead to pseudotumour cerebri (raised intracranial pressure and papilloedema – figure 2 – in the absence of a space-occupying lesion). In addition, it has also been reported as a cause of acute glaucoma attacks, although this is rare.
 Figure 2: Glyceryl trinitrate has been associated with papilloedema
Figure 2: Glyceryl trinitrate has been associated with papilloedema
Other side effects reported to be associated with anti-anginal drugs are photosensitivity, amblyopia, oedema around the orbit, haemorrhages and lacrimation.18
Anti-arrhythmics
Heart or cardiac arrhythmia describes the state of having an irregular heartbeat. It can be further divided into slow (bradycardia), fast (tachycardia), irregular (fibrillation, atrial or ventricular) and heart block. Some of these arrhythmias, especially atrial and ventricular fibrillation, are very dangerous and can cause sudden death. There are various causes for each but common culprits are alcohol, smoking, excess of caffeine, certain drugs and viral
infections.
Amiodarone
Amiodarone is used mainly for the treatment of arterial fibrillation (AF) and ventricular tachyarrhythmia (VT). However, due to its high toxicity, it is not used as a first line therapy. At the ocular level, bilateral, asymmetric whorl-like corneal deposits (corneal verticallata – figure 3) are the most common ocular adverse effects of amiodarone and can be found in almost all patients (70 to 100%) after one to four months of treatment. The risk is dose dependant, with doses of 100 to 200mgd-1 having minimal effect and 400 to 1,400 mgd-1 likely to cause more advanced keratopathy.
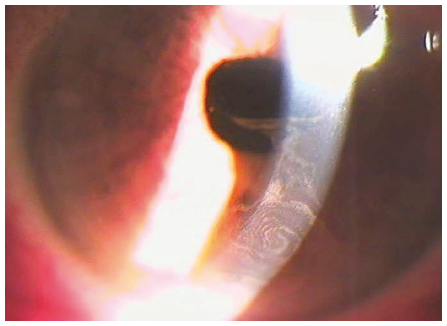 Figure 3: Corneal verticallata
Figure 3: Corneal verticallata
The corneal deposits result from the lipid-binding properties of amiodarone and are classified into four grades, depending on their number, density and extension. The deposits will reduce in number and disappear after the cessation of treatment. In addition, amiodarone can also cause lenticular changes (subcapsular deposits within the pupillary area) and optic neuropathy, all reversible after the treatment is stopped. Usually, patients do not have any symptoms. However, in some cases they can report photophobia, blue-green rings around lights and blurred vision. The optometrist should know the danger and monitor the possible side effects of these drugs. No other measures are usually thought to be necessary, though some have suggested prescribing UV-blocking lenses as useful. A dilated fundus exam, Amsler assessment, and central visual fields testing should be performed (figure 4). If the patient has severe symptoms, the optometrist should refer the patient back to their GP for a possible change in therapy.19
Figure 4: A dilated fundus exam, Amsler grid, and central visual fields testing should be performed upon those taking amiodarone
Digitalis
Digoxin is used to treat arrhythmias and also heart failure. It has been demonstrated that up to 25% of patients that receive treatment with digoxin will experience ocular side effects. These include:
- Changes in colour vision (figure 5)
- Dimming and flickering vision
- Flashes or coloured spots
- Paracentral scotomas20

Figure 5: Digoxin use may cause acquired colour vision defects
It is also believed that digoxin may cause retinal toxicity. Moreover, it can also contribute to reduced aqueous production and, consequently, lowering of IOP.
• Dr Doina Gherghel is an academic ophthalmologist with special interest in inter-professional learning for optometrists.
• The next articles in this series will be dedicated to other common medications, such as hypoglycaemics, hormones, anti-rheumatologic, anti-anxiety, antidepressants and
antipsychotics.
References
- Garg P, Yadav S. Ocular side effects of systemic drugs. Era’s Journal of Medical Research, 2019; 6:1-9
- Mizranita V, Pratisto EM. Statin-associated ocular disorders: the FDA and ADRAC data. Int J Clin Pharm 2015; 37: 844-850
- Pokrovskaya O, Wallace D, O’Brien C. The emerging role of statins in glaucoma pathological mechanisms and therapeutics. Open J Ophthalmol 2014; 4: 124-138)
- Rikitake Y, Liao JK. RhoGTPases, statins and nitric oxide. Circ Res 2005; 97: 1232-1235
- Song J, Deng PF, Stinnett SS et al. Effects of cholesterol-lowering statins on the aqueous humor outflow pathway. Invest Ophthalmol Vis Sci 2005; 46: 2424-2432)
- Stein JD, Newman-Casey PA, Talwar N et al. 2012; 119:2074-2081, Kang JH, Boumenna T, Stein JD et al. Association of statin use and high serum cholesterol levels with risk of primary omen-angle glaucoma. JAMA Ophthalmol, 2019; 137: 756-765
- AP Khawaja, MPY Chan, DC Broadway, et al.Systemic medication and intraocular pressure in a British population: the EPIC-Norfolk Eye Study. Ophthalmology, 2014; 121:1501-1507
- www.healio.com/optometry/glaucoma/news/print/primary-care-optometry-news/%7B5f77d542-900a-479c-83d3-1773b786b4c5%7D/systemic-medications-may-mask-high -intraocular-pressure-in-glaucoma-patients (accessed 3rd March 2020)
- www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/drug-cabinet/calcium-channel-blockers (accessed 3rd March 2020)
- www.uptodate.com/contents/major-side-effects-and-safety-of-calcium-channel-blockers (accessed 3rd March 2020)
- www.ncbi.nlm.nih.gov/pubmed/30520455
- C Mayama. Calcium channels and their blockers in intraocular pressure and glaucoma. Eur J Pharmacol, 739 (2014), pp. 96-105
- (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4741158/
- Müskens RPHM, S de Voogd, RCW Wolfs, et al.S ystemic antihypertensive medication and incident open-angle glaucoma Ophthalmology, 114 (2007), pp. 2221-2226;
- www.sciencedirect.com/science/article/pii/S0161642017309442?via%3Dihub#bib3
- www.oepf.org/sites/default/files/journals/jbo-volume-11-issue-6/11-6%20Valeriewren.pdf
- www.reviewofoptometry.com/article/which-side-effects-are-lurking-in-the-shadows
- Jaanussd, Barlett JD, Hiefr JA. Ocular effects of systemic drugs In :Barlett JD and Jaanus SD. Clinical Ocular pharmacology 3rd ed. Bostan: Butterworth. Heinemann. 1995:957:1006
- www.oepf.org/sites/default/files/journals/jbo-volume-11-issue-6/11-6%20Valeriewren.pdf)
- Muchnick BG. The ocular manifestations of systemic drugs. Optom Today 1998 May:44-52; Garg P, Yadav S. Ocular side effects of systemic drugs. Era’s Journal of Medical Research, 2019; 6:1-9
