The use of high energy pulse application to the skin has been used in dermatology for some years. More recently, application has been found in optometry, in particular the management of meibomian gland disease (MGD) that contributes to dry eye (see Optician 17.03.2017 and 07.12.2018).
The persistent nature of the condition and the need for good compliance with the currently accepted treatment options makes MGD a stubborn condition to address. Any treatment that might be applied by a practitioner and offer a longer-term solution should be viewed with interest. Intense pulsed light (IPL) therapy has been used for some years in the cosmetics industry for removal of skin lesions such as telangiectasia, port-wine stains and haemangiomas. The technique has also been used in the management of severe facial erythema in patients with acne
rosacea. In these patients, it was noticed that there also appeared to be some improvement in their MGD and it is from this serendipitous finding that an IPL treatment tailored for MGD was developed.
Background
IPL has been used for many years in dermatology,1-4 and was FDA approved in the US for the treatment of telangiectasia in 1995.4 These are the abnormal blood vessels found in, for example, rosacea which leak inflammatory mediators that can lead to skin damage. IPL has also found use in the more general treatment for acne as it is also believed to eradicate causative bacteria.1,2
More recently, IPL treatment has been cited in the TFOS DEWSII recommended staged management plan for dry eye disease, and is considered a second stage management option (table 1).
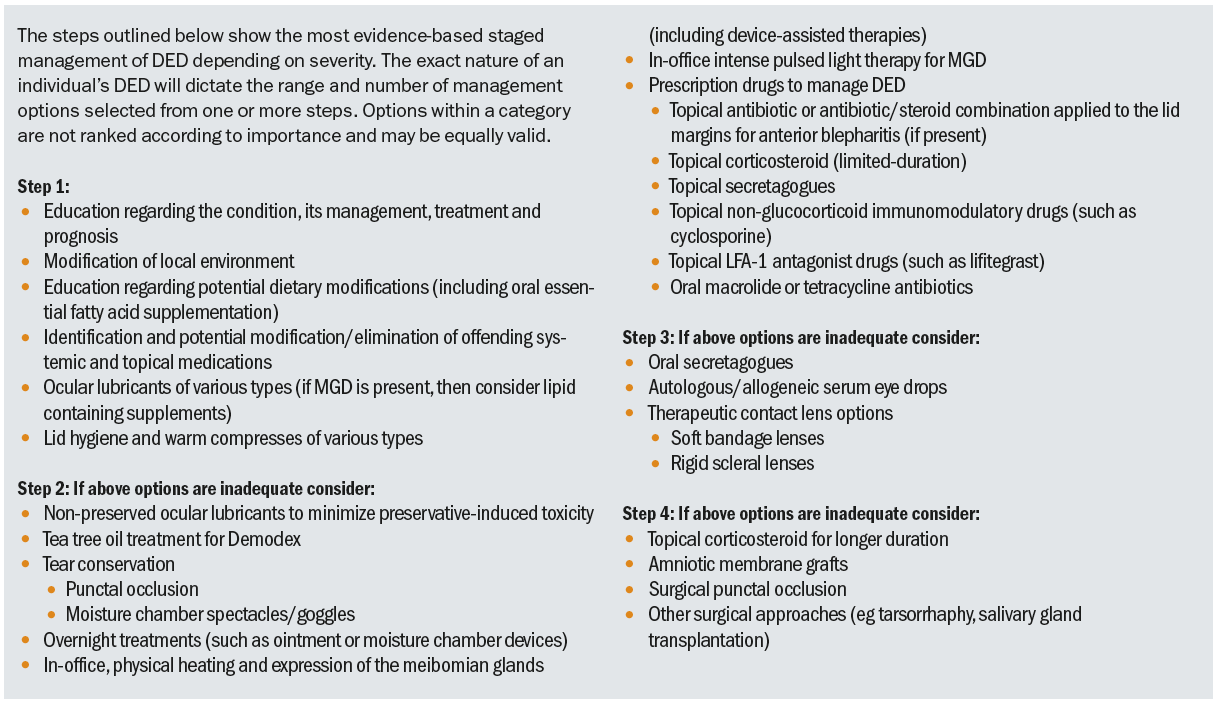 Table 1: IPL is a second stage management option for dry eye disease5,6
Table 1: IPL is a second stage management option for dry eye disease5,6
Practitioners have to deal with meibomian gland dysfunction on a daily basis. It is a major cause of evaporative dry eye symptoms and there are many approaches to its management. These range from the direct expression of meibum from blocked glands in practice, and the use of heat and pressure (typically through a mask) to soften and expel meibum, through to omega-3 supplementation and the use of a variety of drugs such as tetracyclines to reduce the bacterial load or cyclosporine to influence inflammation.
The persistent nature of the condition and the need for good compliance with the currently accepted treatment options makes MGD a stubborn condition to address. Any treatment that might be applied by a practitioner and offer a longer-term solution should be viewed with interest. Intense pulsed light (IPL) therapy has been used for some years in the cosmetics industry for removal of skin lesions such as telangiectasia, port-wine stains and haemangiomas. The technique has also been used in the management of severe facial erythema in patients with acne rosacea. In these patients, it was noticed that there also appeared to be some improvement in their MGD and it is from this serendipitous finding that an IPL treatment tailored for MGD was developed. The IPL treatment leads to intracellular changes at both the gene and protein levels; this is called photo-biomodulation.
IPL photo-biomodulation is being used increasingly by optometrists in the management of patients with evaporative dry eye, blepharitis and acne rosacea. I offer this procedure using the M22 Optima IPL instrument from Lumenis (figure 1). This delivers controlled pulses of intense red and infra-red light of only a few milliseconds duration which are applied to the eyelids and upper face. The M22 uses a band wavelength filter set at 590nm for Dry Eye treatment. The two other systems currently used in the UK are the Topcon Eye-Light system (figure 2) and the E-Eye IRPL (distributed in the UK by Grafton Optical, figure 3).
 Figure 1: M22 Optima IPL
Figure 1: M22 Optima IPL Figure 2: The Topcon Eye-Light system
Figure 2: The Topcon Eye-Light system Figure 3: The E-Eye IRPL
Figure 3: The E-Eye IRPL
How it works
As already stated, IPL was first used in 1995 to treat abnormal blood vessels and inflammation in diseases such as acne rosacea. In 2001, the machine and its treatment parameters were modified specifically to treat dry eye. Its use was pioneered in Nashville by US ophthalmologists Rolando and Melissa Toyos. I have attended IPL training courses run by the Toyos team, both in London and their base in Nashville. I recommend attendance at one of these for anyone new to IPL.
The treatment employs a Xenon flash lamp which will emit light of wavelengths between 400 and 1200nm.1,3,4 When this light passes through a filter cut-off at around 500nm, it causes the blood within telangiectatic blood vessels exposed to the incident light to coagulate, so causing them to close.1,2,4 Toyos et al noted that acne rosacea patients treated with IPL reported a decrease in their dry eye symptoms (80% of people with facial skin rosacea have MGD).1,2
The photo-biomodulation mechanism is due to the red visible and the infra-red invisible IPL light and influences function at a cellular level. The influences were summarised by Dell2 as follows:
- Improved mitochondrial function, potentially ‘activating’ or ‘energising’ the meibomian glands
- Improving calcium channel flow
- Increased collagen synthesis
- Modulation of the secretion of anti-inflammatory molecules
- Suppression of matrix metallopeptidases (MMPs), proteolytic enzymes whose restricted action helps to stabilise the extracellular matrix
All the above effects help normalise the tear film and reduce dry eye irritation. In other specialities, similar wavelength photobiomodulation is being used to treat dry macular degeneration, and diverse conditions such as psoriasis and skeletal problems.
In addition to photo-biomodulation, IPL is thought to exert beneficial effects by several additional mechanisms:
- The abnormal blood vessels in the inflamed lid margin are thrombosed as the IPL light coagulates the oxyhaemoglobin flowing through them (figures 4 and 5). This stops the vessels releasing inflammatory mediators into the meibomian glands in the lid margin.
- Improved nerve function around the meibomian glands.
- The IPL flash heats up and melts the meibum secretions blocking the glands, improving the tear lipids and reducing evaporation.
- The intense light pulse kills Demodex mites living in the vicinity of the meibomian glands. This works because a chromophore in the exoskeleton of the mite absorbs IPL energy. By eradicating Demodex, IPL reduces the consequent bacterial load on the eyelids. This, in turn, reduces chronic inflammation and the consequent conversion of normal melting point meibum to high melting point lipid, thereby improving the fluidity of the lipids secreted and the quality of the lipid layer.
- IPL is thought to stimulate the fibroblasts and up-regulate the synthesis of collagen fibres in the skin. With age, the collagen and elastin fibres relax, reducing skin rigidity and elasticity. IPL is found to counteract this and cause skin tightening.
 Figure 4: Lid margins before and after IPL treatment (image courtesy of Dr Keyur Patel and Tompkins Knight and Son Optometrist practice)
Figure 4: Lid margins before and after IPL treatment (image courtesy of Dr Keyur Patel and Tompkins Knight and Son Optometrist practice)
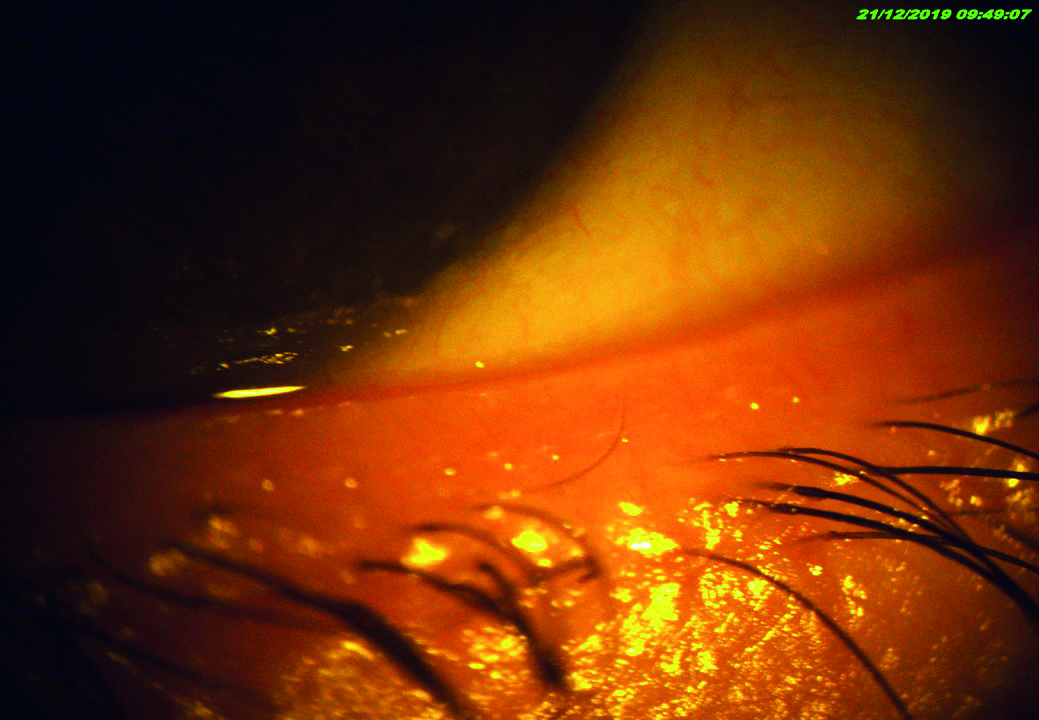 Figure 5: Lid margin appearance after four IPL treatments
Figure 5: Lid margin appearance after four IPL treatments
Figure 5 shows the effect of four treatment sessions on the meibomian secretions of a patient with previously completely blocked glands.
Contraindications for IPL
Contraindications include:
- Systemic use of drugs causing photosensitivity
- A history of high sun exposure or artificial tanning treatment
- Systemic inflammatory connective tissue and skin diseases such as lupus, adnexal ketosis and melanin aggregation
- Skin tattoos
IPL and MGD
In MGD, an inflammatory cycle is created leading to the development of abnormal blood vessels or telangiectasia (figure 6). These, in turn, release pro-inflammatory mediators that cause dilation of the blood vessels and yet further escalate inflammation. Demodex mites and bacteria flourish in the inflamed tissue, leading to clogging of the glands and further irritation and damage to the corneal surface. As evaporation increases once the lipid layer continues to fail, osmolarity increases, so damaging the goblet cells and reducing the quality of the all-important mucous layer. The mucous layer is important to help maintain the aqueous component in its correct place. So, the downward spiral increases. Restoring the lipid layer with omega-3 supplements, lid hygiene and IPL treatment helps to arrest and reverse this process.
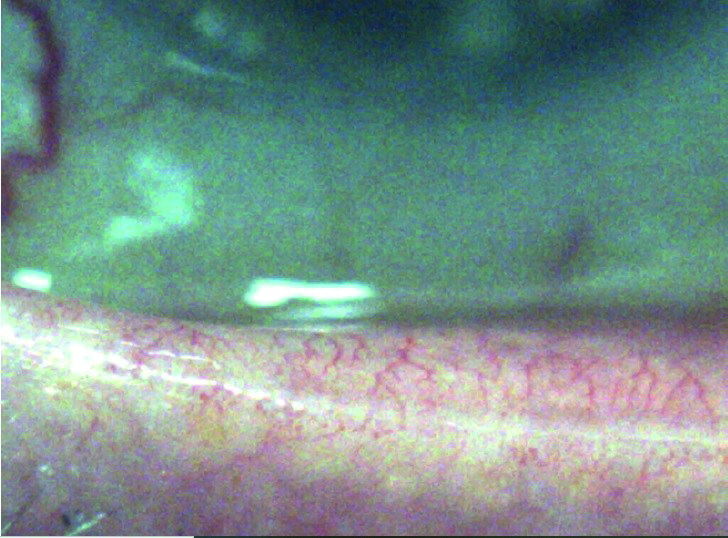 Figure 6: Telangiectasis on the lid margin of a patient with chronic dry eye disease
Figure 6: Telangiectasis on the lid margin of a patient with chronic dry eye disease
Treatment with IPL
The IPL treatment area includes the skin overlying the cheeks and nose in addition to the eyelids. This is because the tiny broken blood vessels in these areas can ‘feed’ the inflammation in the eyelids. Cosmetically, many patients are pleased with the reduction in thread vessels, skin blemishes and wrinkles, which often occur as a beneficial side effect.
Patients should not wear face make-up for at least one day before treatment. They should especially avoid products containing retinoids. Prescribed retinoid skin treatments include tretinoin, tazarotene and adapalene. After treatment, a moisturiser cream is advised as the skin can be sensitive for a few days. High factor sunscreen should be worn afterwards for a few days for the same reason.
Treatment spans four to five sessions, usually scheduled two to four weeks apart. Subsequent maintenance treatment normally consists of one treatment per year. Because IPL is also used to treat facial rosacea, treatment of lower face telangiectasia can be combined with dry eye treatment.
The Optima IPLs OPT feature ensures that the pulses of light are uniform and repeatable. Because the thickness of the skin is so thin close to the lower eyelids, ensuring that the light energy is delivered in a reliable manner is key to safety. In figure 7, you can see a patient having the IPL procedure performed. I treat the entire malar region, from tragus to tragus, across the lower eyelids and bridge of the nose. This protocol allows me to address a large portion of blood supply to the lower lids as well as some of those supplying the upper lids.
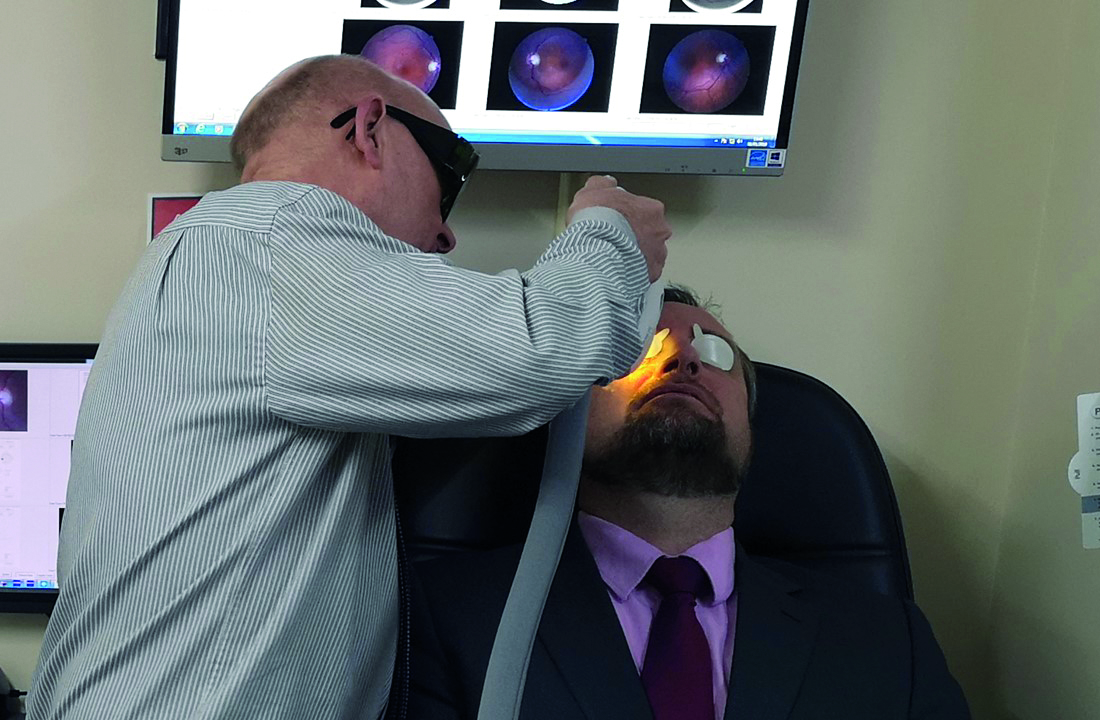 Figure 7: Patient undergoing IPL treatment from the author
Figure 7: Patient undergoing IPL treatment from the author
The procedure requires the following steps:
- Agree consent with the patient
- Apply protective IPL eye patches to the patient (figure 8)
- Optometrist dons the appropriate protective eyewear
- Apply IPL transmission buffer gel to areas to be treated (figure 9)
- Set power setting, pulse duration and pulse frequency
- Test temporal cheek area to confirm setting levels correct
- Make approximately three sweeps from ear to ear for each of around 14 treatment areas (figure 10). Allow a delay of 20 to 60 seconds between each sweep
- Remove treatment gel
- Use a heat expression of meibomian glands
- Apply moisturiser to cheeks
 Figure 8: Eye protection in place
Figure 8: Eye protection in place Figure 9: A transparent buffer gel is applied
Figure 9: A transparent buffer gel is applied Figure 10: Treatment areas
Figure 10: Treatment areas
Before gaining consent, the patient should be counselled and the details of the technique fully explained. They then sign a consent form to say that they understand and are aware of the possibility of side effects, though these are rare and I am pleased to confirm that none have ever occurred in our clinics.
Possible complications include the following:
- Pain
- Reddening of the skin
- Burning sensation
- Oedema
- Temporary discolouration and bruising of the skin
- More long-lasting colour changes, such as hyper-pigmentation (a brown/red discoloration) or hypopigmentation (patches of lighter skin tone)
Unprotected sun exposure in the weeks before and following treatments is contraindicated as it may cause or worsen this condition. A blue-purple bruise (purpura) may appear on the treated area. This can last from a couple of weeks to several months to completely resolve. Scarring and burns have been reported, though this is very uncommon. Careful titration of the power and pulse characteristics usually avoids complications occurring.
It is important that the laser pulse type, flash duration and power settings are tailored to the patient’s skin colour. Ironically, the darker their skin colour, the lower the treatment power settings need to be. The initial setting is based on the Fitzpatrick skin type (figure 11). I usually test a relatively non-visible bit of skin near the tragus at a low setting and work up the power settings till a medium to hot tingle is felt. As the inflammatory vessels recede with each subsequent treatment, the power settings can be gradually increased. The higher the power, the more effective the impact on the meibomian glands, but also the greater chance of skin irritation.
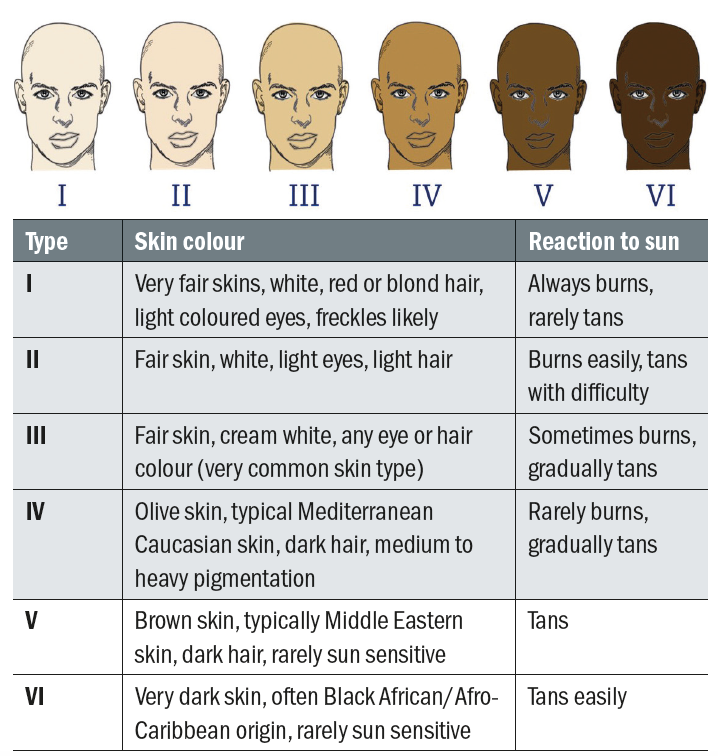
Figure 11: The Fitzpatrick Skin Type Scale
Protective IPL patches are applied to protect the eye itself because, in addition to oxyhaemoglobin, melanin is also heated up by the IPL wavelengths, and so the iris (theoretically) may suffer heat damage. This could result in intraocular inflammation and iris depigmentation. The protective shields are placed just below the lower lash root line or just above the upper lash line, depending on the area being treated. As well as protecting the eye itself, shields also ensure that the eyelashes are not accidentally burned away by mistake.
It is a good idea to increase significantly the ambient room lighting to ensure that you can clearly visualise the areas being treated. As the patient will be wearing a dark protective tint during the treatment process, you can increase lighting to higher levels than might normally be acceptable. This is important, as it ensures that suspicious pigmented lesions or eyebrows are not inadvertently treated.
The purpose of the treatment gel is to protect the skin from the heating effect, and also to ensure that the light reaches the haemoglobin in the telangiectatic vessels (located just below the skin surface) without the need for excess pressure. This would result in flattening of the vessels, thereby occluding the blood flow and reducing oxyhaemoglobin exposure. It is important that the gel used is transparent, as colouring would reduce the light transmission.
The treatment head on the M22 is kept refrigerated. This helps to improve patient comfort and reduces the possibility of thermal skin damage. Reports from the Eye Institute of West Florida told how, when practitioners switched from a previous system that patients had found to be hot and uncomfortable to the cooled head of the M22 Optima IPL, the volume of patients who completed the series of initial and follow-up treatments grew from 80% to 95%.
Patients should be warned that they may smell burning during the process. This is not the skin getting cooked, but merely the downy facial hair going up in smoke. I ensure that, for male patients, I avoid the moustache and beard area during IPL treatment. IPL may interfere with future intentional facial hair growth.
The M22 has three different sizes of treatment head to improve access to difficult areas (figure 12). The fluence emitted has the same energy density whichever head is used.

Figure 12: A range of treatment heads helps to ensure even hard to access areas may be treated
Other IPL Uses
IPL treatment with the M22 is also used for a range of skin
treatments. These include:
- Hair removal
- Thread vein removal
- Treatment of hyperpigmentation (freckle and age spot removal)
- Photo rejuvenation (the treatment of sun damaged skin)
- Acne treatment
The melanin in ‘age-spots’ and freckles is heated up by the IR light and they usually fade with repeated treatments. As you see from figure 13, variable treatment depths can be achieved by selecting different treatment wavelengths.
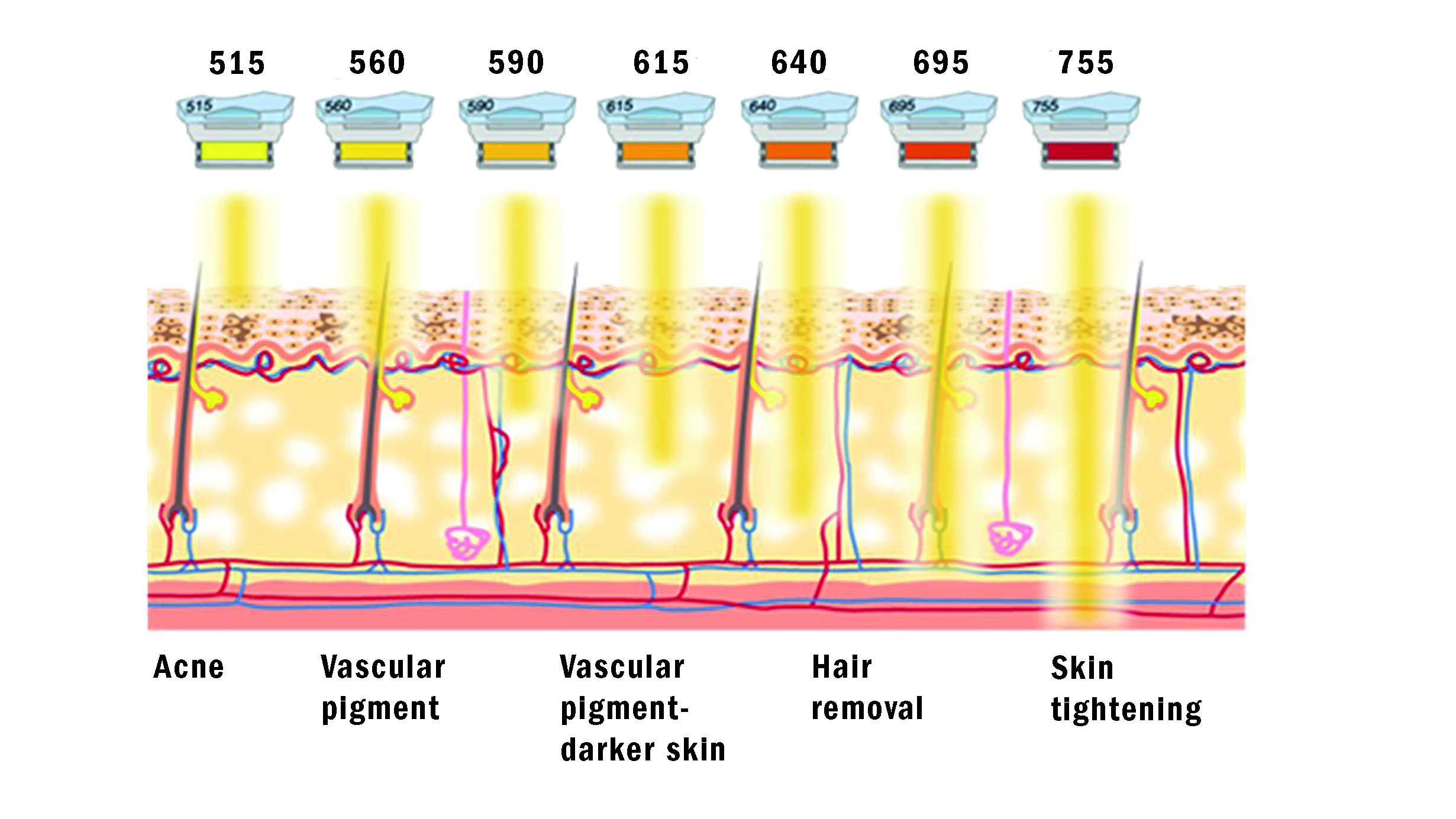 Figure 13: Pre-treatment setting of the incident light will influence the specific depth of tissue treated
Figure 13: Pre-treatment setting of the incident light will influence the specific depth of tissue treated
The M22 unit can be fitted with additional software modules and attachments. This allows other treatments, including YAG laser treatment of deeper vascular lesions and pigmentation, resurfacing laser for skin tightening and wrinkle reduction among others. In the US, many optometrists and ophthalmologists have branched into these aesthetic fields.
Even standard IPL with the M22 device can cause a degree of skin tightening and hair removal. Patients are often very pleased with these ‘bonus’ benefits. It is, I repeat, wise to warn them that they may smell burning hair during the process, and not to worry. During hair removal, the IPL light energy is absorbed by pigment within the hair follicle, heating it up and permanently damaging it so that the hair does not grow back. IPL needs to target the hair follicles during a specific part of their life cycle (during the growth, or ‘anagen’ phase). Not all of the hairs will be in the anagen phase at the same time, so multiple treatments are needed in order to get long-lasting results.
The M22 can also be used to treat conventional acne (vulgaris as opposed to rosacea). This affects over 80% of the population between the ages of 14 and 30 to some extent, but is most prevalent in the teenage years. Often patients with teenage acne are left with disfiguring facial scarring. The main bacterium involved is Propionibacterium acnes. Although it has been found that, in vitro, blue light of 400nm is most effective at destroying P. acnes, its poor penetration depth when applied to skin means that the 590nm broadband of IPL provides more effective penetration into deep blocked skin pores. In addition, it is thought that the thermal effect on the sebaceous glands can support long-term remission from acne. The thermal stimulation of fibroblasts and collagen production can reduce mild acne scarring and accelerate healing.
Andrew Matheson is a specialist therapeutic optometrist involved in medical retina treatments, glaucoma management and providing hospital laser surgery services.
References
- Toyos R, McGill W, Briscoe D. Intense pulsed light treatment for dry eye disease due to meibomian gland dysfunction; a 3-year retrospective study. Photomedical Laser Surgery, 2015; 33: pp41-6.
- Dell SJ. Intense pulsed light for evaporative dry eye disease. Clinical Ophthalmology, 2017; 11: pp 1167-73.
- Rennick S, Adcock L. Intense Pulsed Light Therapy for Meibomian Gland Dysfunction: A Review of Clinical Effectiveness and Guidelines. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health 2018. Available at; www.ncbi.nlm.nih.gov/books/NBK531789/
- Arita R, Fukuoka S, Morishige N. Therapeutic efficacy of intense pulsed light in patients with refractory meibomian gland dysfunction. Ocular Surface. Published Online First: 13 November 2018. doi:10.1016/j.jtos.2018.11.004
- Jones L, Downie L, Korb D, et al. TFOS DEWS II management and therapy report.The Ocular Surface. Published Online First: 1 July 2017. doi:10.1016/j.jtos.2017.05.006
- Farrant S. TFOS DEWS II – part 3; Management. Optician, 17.03.2017
