Soft contact lenses continue to dominate the global contact lens market, accounting for around 90 per cent of all fits worldwide.1 Materials, optical designs and additional features continue to evolve in an attempt to reach ever increasing levels of comfort, vision and health for patients. As efforts to improve long-term contact lens success continue, attention to lens selection and optimisation of fit should not be ignored. Although there are fewer parameters to consider when fitting a soft lens compared to rigid gas permeable lens for example, it is still of utmost importance to assess the fitting accurately and monitor the ocular response to contact lens wear.
Contact lenses should interfere minimally with corneal metabolism and provide crisp, clear stable vision while being comfortable at all times. Prescribing the right material, lens dimensions and wearing modality to match the wearer’s ocular surface and lifestyle, should be the goal of every contact lens practitioner. Sub-optimal fit or inappropriate lens selection can result in discomfort and/or have potential physiological impact. In turn, this has shown to contribute significantly to contact lens wear discontinuation if not addressed appropriately.2
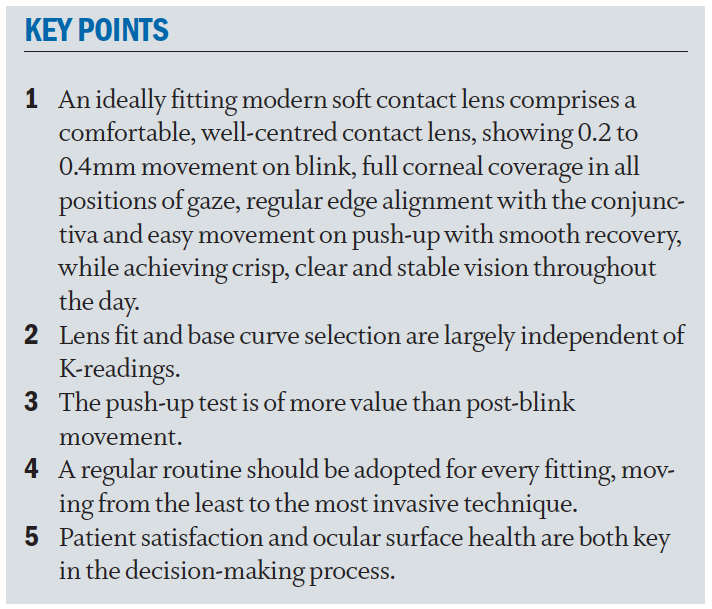
An ideally fitting soft contact lens comprises a well-centred contact lens, showing 0.2 to 0.4mm movement on blink, full corneal coverage in all positions of gaze, regular edge alignment with the conjunctiva and easy movement on push-up. Furthermore, the patient should report high levels of comfort and crisp, stable vision. Although it can be argued that the skill of achieving an ideal fit is relatively straightforward, its success relies very much on making correct decisions based on clinical judgements when monitoring the ocular physiology of the patient over time. In addition, an ‘acceptable fit’ is not necessarily the most optimal fit for that individual, so communication with your patient remains paramount. This article provides a practical overview of the key aspects and principles associated with spherical soft contact lens fitting, and can be applied to both hydrogel and silicone hydrogel contact lenses. Future articles in this series will address toric and multifocal soft contact lens fitting separately.
Establishing a routine
Good clinical practice does not involve viewing one observation in isolation. Therefore, clinicians are encouraged to follow a structured routine, and act on sub-optimal findings taking all results into account. A schematic overview of a soft contact lens fitting routine is shown in table 1. Each element of the fitting process is described in more detail in the following sections.
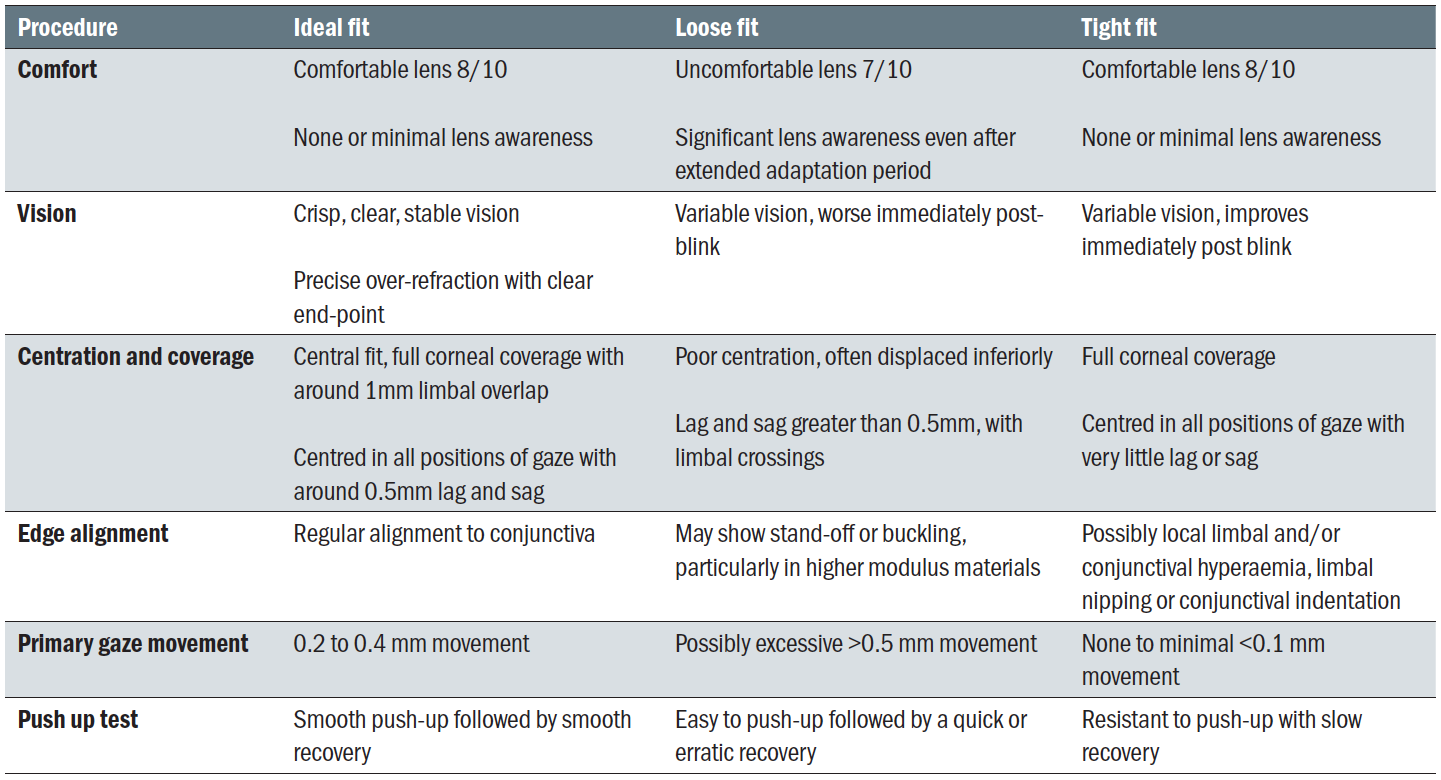
Table 1: Schematic flow chart of soft contact lens fitting procedures
Initial trial lens selection
Although contact lens practitioners have relatively little control over the available lens designs, the first trial lens should be selected using the following criteria as closely as possible. In order of importance, these are:
- Material; the selection of the soft lens material is considered the most important factor in achieving excellent contact lens comfort and subsequent patient satisfaction. It can also be argued that lens material is the first parameter to be modified when attempting to optimise a lens fitting. Material properties should allow sufficient oxygen transmission to maintain ocular health, be resistant to deposits, and attain high surface wettability. The two principal material choices are hydrogel and silicone hydrogel, each with their own advantages and disadvantages,3,4 as discussed in the previous article in this series (see Optician 06.03.2020).
- Back vertex power (BVP); should be as close as possible to the patient’s prescription to allow them to judge the visual benefits of contact lens wear correctly and to facilitate adaptation. If the exact power is not available, it is preferable that the lens is chosen to under-correct rather than over-correct, to avoid unnecessary accommodative effort that would influence the over-refraction. If the spectacle power is above ±4.00DS in any meridian, adjustments should be made to account for the change in back vertex distance.
- Total diameter; must be larger than the horizontal visible iris diameter (HVID) by approximately 2 to 3mm to allow for full corneal coverage. The majority of spherical soft lenses are manufactured in diameters between 14.0 to 14.5mm; consequently, the choice is very much dependent on availability.
- Back optic zone radius (BOZR); sometimes referred to as the base curve (BC), the historic general rule of thumb describes a choice of BOZR within the range of flattest keratometry readings plus 0.7 to 1.0 mm, however, little correlation has been seen between BOZR and optimal fitting.5 The underlying assumption of this rule is that steeper corneas have a greater sagittal height, therefore requiring a lens of greater sagittal depth, in the form of a steeper base curve. However, sagittal height is a function of not only the corneal curvature, but also the corneal asphericity, corneal diameter and curvature of the paralimbal sclera.6 As such, when a choice of BC is available within the same lens, follow the manufacturer’s guidelines to decide which lens to try first, without regard to keratometry readings.
Adaptation period
Once the lenses have been applied, the fit has to be assessed after a suitable settling period. Once placed on the eye, soft contact lenses will lose water, which will cause a subsequent change in parameters including diameter and base curve, which in turn may have an effect on the fitting characteristics. Other parameters that have been shown to change following application of a contact lens are pH, temperature, and osmolarity.7 Intuitively, it is therefore important that the fit is assessed once the lens is in equilibrium with the tear film.
It has been shown that lens movement significantly decreases within the first 30 minutes of wear, independent of the water content of the contact lens material.8 The same study also reported that in 75% of patients, the most effective time to predict the final fitting characteristics is approximately five minutes after the lens has been applied. Another study has shown that contact lens fitting characteristics after 10 to 20 minutes of initial lens wear is predictive of eight hours contact lens wear.9 As such, common clinical practice would involve selecting an alternative trial lens if the contact lens fit is unacceptable after a settling period of 10 minutes.9
While 10 minutes may be enough to assess lens stabilisation, it is clearly insufficient to judge the ocular physiological response to the lens, or for the patient to appreciate what wearing contact lenses entails, and to experience a more real world beyond the consulting room chair. Ultimately, this is the objective of ongoing aftercare, enabling the practitioner to monitor not only the physiological response to lenses, but also any changes in a person’s routine, including wearing time, work environment, and evening and weekend activities.
Patient subjective responses
Once the contact lens has been applied to the eye, the patient response to the contact lens in respect to comfort and vision should be ascertained. In contrast to a rigid contact lens, a soft lens should feel virtually indiscernible on the eye. Any initial discomfort due to differences between the osmolarity and pH of the lens storage solution and the patient’s tears should be quick to resolve. Lens sensation should be consistent, with no significant differences on versions or following blink. As a general rule, comfort should be reported as eight out of 10, on a 10-point scale, or better. Should comfort be reported as lower than this, an alternative lens material and/or fit should be considered.
Assuming the correct prescription has been selected, vision should be reported as stable and clear, although patients with higher refractive errors may notice peripheral distortion and could encounter some initial difficulty in judging distances due to magnification changes. These should, however, soon resolve. If vision is reported as fluctuating between blinks, this could indicate a poorly fitting and/or poorly wetting lens.
Vision assessment
Distance and near visual acuity should now be assessed, and a standard over-refraction performed, including binocular balancing as appropriate. For single vision spherical lenses, a trial frame of phoropter can be used. The refraction should have a clear endpoint and visual acuity should be stable and crisp. Fluctuations in acuity could indicate a poor lens fit. Unstable vision tends to indicate a loose fit; however, if this becomes clearer following a blink it may indicate a tight fitting. The use of the retinoscope is recommended to exclude uncorrected refractive power and confirm that the optic zone covers the pupil, especially in high-powered lenses.
Slit lamp examination
The lens fit should be assessed using the slit lamp biomicroscope to allow for sufficient magnification, and assessment should be based on moving from the least to the most invasive technique. Diffuse direct illumination and medium to high magnification is recommended to visualise the whole of the contact lens on-eye.
The following assessments should be made:
- Lens surface quality
Before any of the fitting characteristics are evaluated, the lens surface quality should be recorded. Scan the lens surface using a parallelepiped beam at medium magnification (16x) or observe the 1st Purkinje image to assess initial wettability of the lens (figure 1). A Placido ring topographer (figure 2) or a one-position keratometer can alternatively be used. The lens surface is expected to be excellent after the initial adaptation period, although this depends on the quality and composition of the tear film as well as compatibility with the contact lens material. - Corneal coverage and centration
With the eye in primary position, the lens should show full corneal coverage before, during and after the blink (figure 3) and ideally display around 1 mm of limbal overlap. Incomplete corneal coverage can lead to more lens awareness, corneal desiccation staining (figure 4), and mechanical stress on the peripheral cornea. - Movement on excursions
As well as assessing coverage in the primary position, coverage and movement should also be assessed on excursions, to ensure full coverage in all directions of gaze. Although traditional training and fitting guides recommend assessing lens movement on right and left gaze (known as lag, figure 5) and on up gaze (known as sag, figure 6), studies indicate that these measures have little predictive value in deciding if a lens fit is ideal or not,8,10 though movement on horizontal gaze may be more useful of the two.11 Movement should be quantified in millimetres and can be assessed by comparing the amount of movement to the limbal overlap, which ‘is expected to be’ around 1mm. Alternatively, movement can be quantified by comparing to a known beam width as measured by the slit lamp graticule. - Edge alignment
The edge of the contact lens should be aligned with the conjunctiva, and not indent the conjunctival vessels. Failure to achieve a smooth transition could result in local limbal or conjunctival hyperaemia and/or limbal nipping. Indentation would indicate stagnation of tears in this region and reduced oxygen supply to the limbus. If available, a flatter base curve could be trialled, or a different lens design with a different edge profile. Signs of indentation are more commonly observed with high modulus silicone hydrogel lenses. Similarly, the lens should also show no edge stand-off (lens buckling, or fluting, figure 7), which could lead to discomfort. This aspect of the lens fitting is often overlooked, as higher magnification is needed to observe this finding. Even slight edge stand-off in an otherwise optimal lens fit can cause discomfort due to its interaction with the eye lid. If available, a steeper base curve should be trialled and assessed. Otherwise, a different lens design or material will be required. - Primary gaze post-blink movement
This should ideally be measured with a graticule, by looking at the bottom of the lens during the blink or, if the lower lid obscures the inferior lens edge, at four or eight o’clock. In absence of a graticule, the movement can be measured in relation to a fixed beam height, of 1 to 3mm, for example. In addition, it is helpful to watch the lens border move in relation to an underlying conjunctival or scleral blood vessel.
The ideal lens movement should be 0.2mm to 0.4mm; however, this depends on the lens material. In modern, thin, high water content and low elastic modulus lens designs, the movement is often less compared to older, thicker, lower water content designs. Even less movement can be observed with silicone hydrogel lenses.12 In some cases, the lens shows no or hardly any movement, even though the lens exhibits a good fit otherwise. As such, it is difficult to judge the fit on movement alone, and a better assessment of lens dynamics can be made using the push-up test. - Push-up test
The push-up test is considered the most effective way to judge the dynamic fit of a contact lens. To perform this assessment, the practitioner moves the lens vertically, through pressure on the lower eyelid using their finger (figure 8), then allows the lens to re-centre naturally. The tightness of the lens is determined by evaluating the relative force required to move the lens upwards, together with the speed of its recovery to its original position. A percentage grade can be used for record keeping, with 100 per cent representing a lens that is impossible to move and zero per cent a lens that falls away from the cornea without lid support. An optimum fitting lens would be recorded as 50 per cent.13
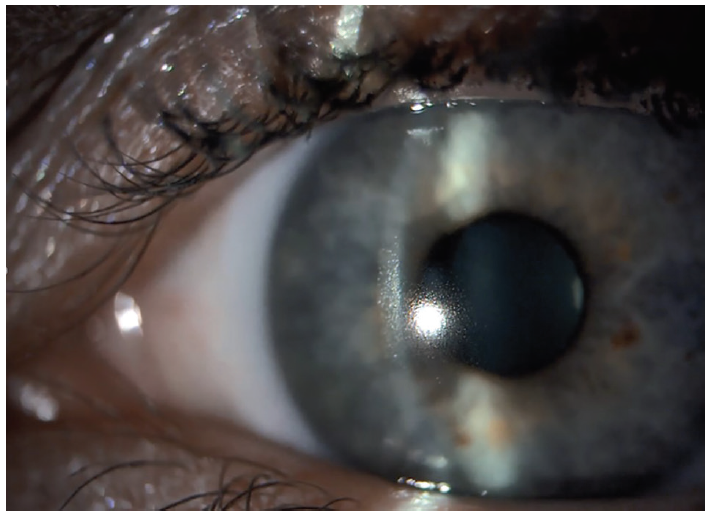 Figure 1: Assessment of contact lens wettability through observation of the 1st Purkinje image, with time to scatter following blink noted as the pre-lens thinning time
Figure 1: Assessment of contact lens wettability through observation of the 1st Purkinje image, with time to scatter following blink noted as the pre-lens thinning time
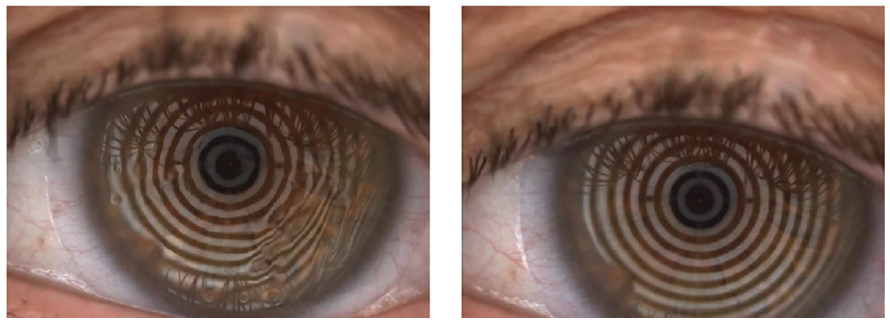 Figure 2: Assessment of pre-lens tear film break up time to provide information on contact lens wettability. Poor contact lens wetting is observed as distortion of Placido rings (left), versus good wetting (right)
Figure 2: Assessment of pre-lens tear film break up time to provide information on contact lens wettability. Poor contact lens wetting is observed as distortion of Placido rings (left), versus good wetting (right)
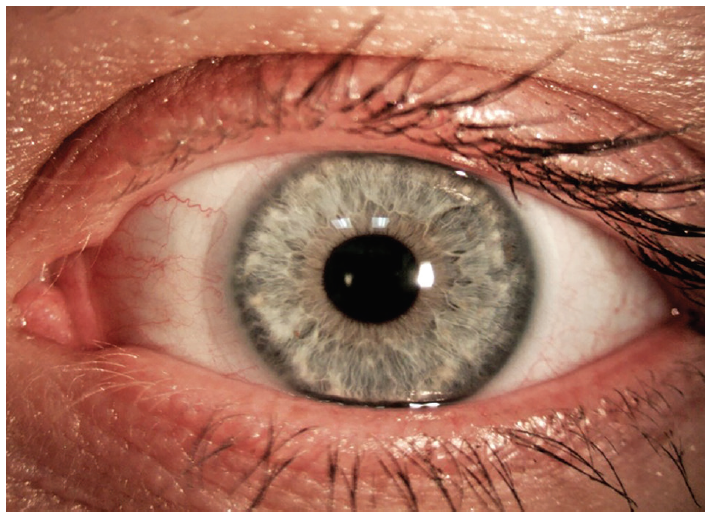 Figure 3: Soft contact lens centration and coverage in primary position, showing 1mm limbal overlap
Figure 3: Soft contact lens centration and coverage in primary position, showing 1mm limbal overlap
 Figure 4: Incomplete corneal coverage (left), can lead to corneal desiccation straining (right)
Figure 4: Incomplete corneal coverage (left), can lead to corneal desiccation straining (right)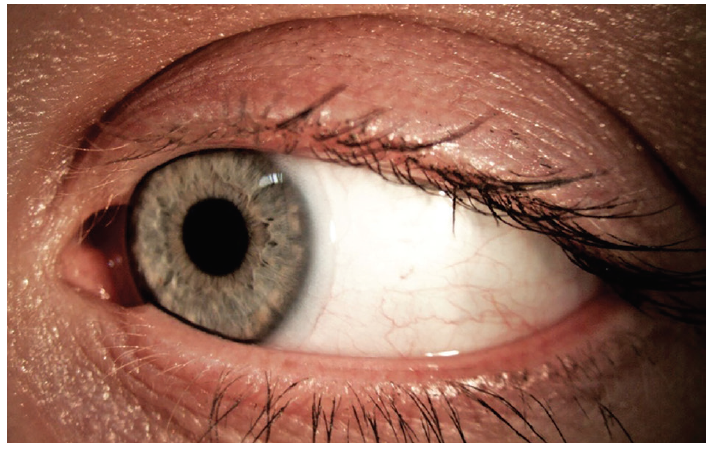 Figure 5: Soft contact lens lag, examined on left and right gaze
Figure 5: Soft contact lens lag, examined on left and right gaze Figure 6: Soft contact lens sag, examined on upward gaze
Figure 6: Soft contact lens sag, examined on upward gaze
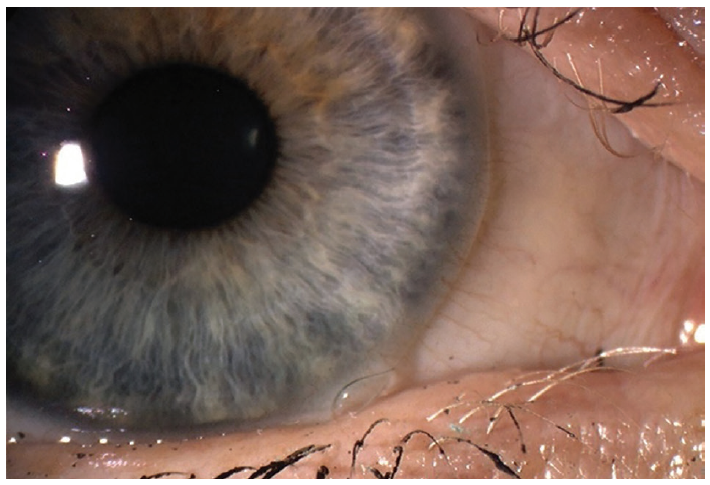 Figure 7: Edge fluting seen in a flat fitting contact lens
Figure 7: Edge fluting seen in a flat fitting contact lens
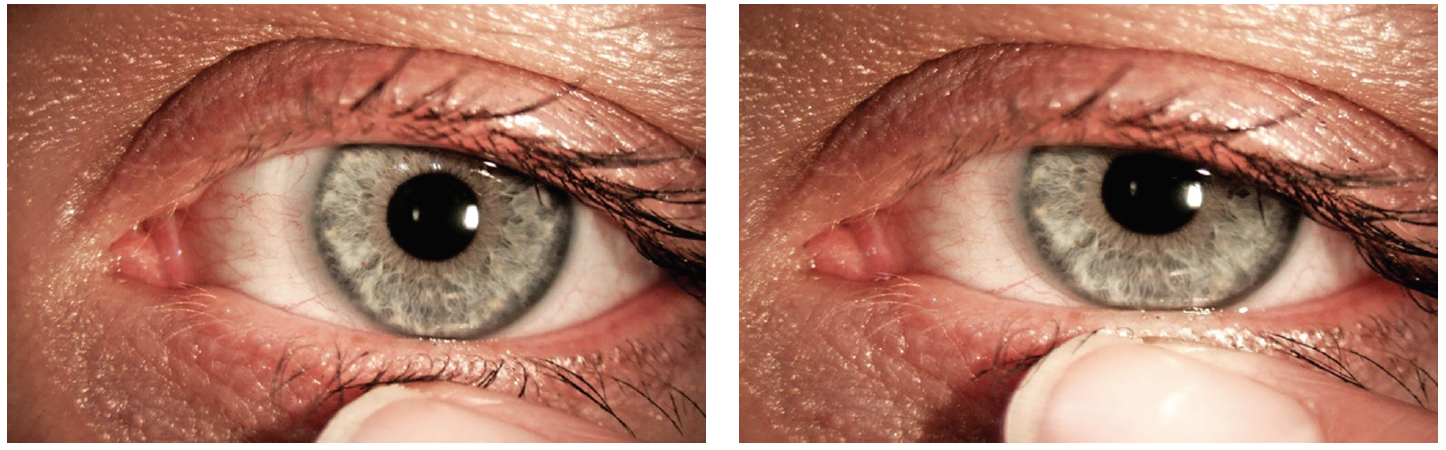
Figure 8: The push up test. The lens is manually moved by pushing the bottom of the lens (left) up vertically (right) using the lower lid, before being released and recovery observed
Interpretations of findings
Accurately assessing the fit of a soft contact lens involves evaluating both static and dynamic criteria, and consistent with good clinical practice, one observation should not be used in isolation to make conclusions. Table 2 reviews both the physical fit and performance requirements of an ideal lens fit, as well as the characteristics of loose and tight fits.
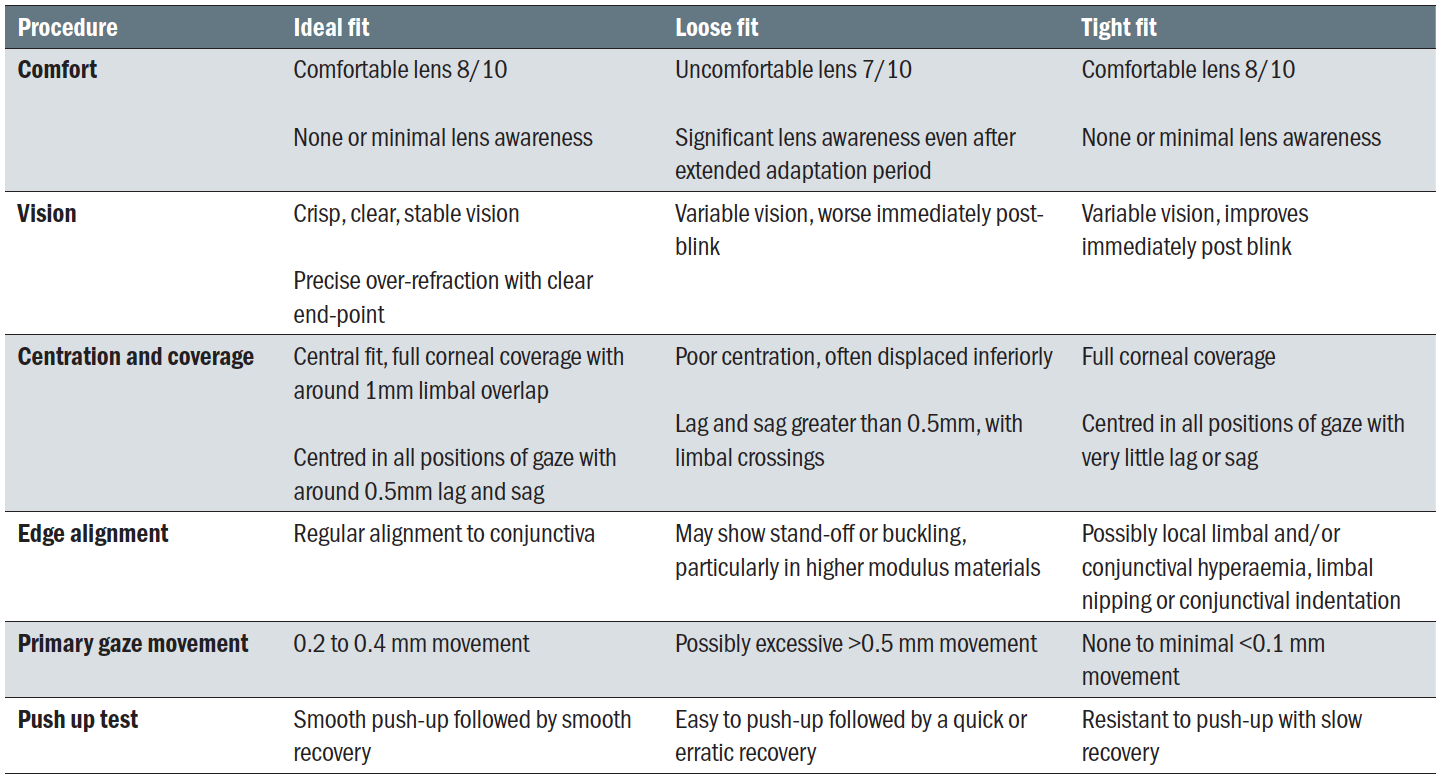 Table 2: Characteristics of ideal, loose and tight soft contact lens fittings
Table 2: Characteristics of ideal, loose and tight soft contact lens fittings
Ocular factors affecting soft contact lens fit
Factors which could affect a soft contact lens fit and subsequently the subjective performance of a lens on-eye are discussed in more detail here. As previous, interpretation of these should not be viewed or managed in isolation.
- Ocular sag. The sagittal height or sag of the cornea is a function of the corneal shape factor, diameter, and radius, as well as the scleral shape factor and radius. So corneal geometry, including sagittal height, is determined by the corneal
asphericity and diameter as well as the corneal curvature. Although ocular sag plays a significant role in the optimal soft contact lens fitting, it is not considered a key parameter because it is difficult to measure. As a result, diagnostic lens fitting using trial lenses is the only way to judge the effect of the sag on the lens fit. - Corneal apex. A displaced corneal apex will typically lead to a decentred lens. To ensure full corneal coverage, opting for a lens with a larger total diameter should prevent exposure and subsequent desiccation of the cornea. In cases of a displaced corneal apex, changes in the base curve will have little effect on centration.
- Lid pressure. Tight lids may result in high-riding lenses and possibly, excessive lens movement. This can be managed by refitting with a thin lens design and/or increasing the lens diameter. Loose lids generally have less effect on the lens
fitting. - Tear morphology. Both pH and osmotic pressure can change lens parameters and affect the fit of the lens. A reduction in pH leads to steepening parameters of ionic contact lenses, and it has been shown that both ionic and non-ionic lenses tighten in fit as the tonicity of the tear film is reduced.14 This is clinically significant because if a satisfactory fit cannot be obtained with one contact lens material, then it might be worth refitting with a material of a different ionicity or water content.
Lens variables affecting soft contact lens fit
In addition to ocular factors, lens variables can also influence the performance and fitting characteristics of soft contact lenses. The key lens factor variables that can affect fit are as follows:
- Back optic zone radius. Although traditionally one would choose a larger back optic zone radius to increase lens movement, it is now well established that the base curve has no predictive value on lens movement.15,16 This does not imply that a change in base curve has no effect on lens movement at all, only that a steeper base curve would not automatically result in a tighter fit, as one would predict. In addition, practitioners should be aware that changing to a different contact lens brand with identical base curve and total diameter will not guarantee the lens behaves identically on the eye. This is due to the variations in peripheral lens design between contact lens brands, which informs the relationship between the front and back peripheral curves. As well as having a marked effect on the lens fitting characteristics, the peripheral design influences lens handling characteristics and comfort.17
- Total diameter. Increasing the total diameter will expand the sagittal height of the lens and tighten the fit, whereas reducing it will have the opposite effect. Total diameter should also be increased to improve corneal coverage in a lens fitted onto a cornea with a displaced apex. Changes to the lens diameter tend to have a greater impact on the fit of a soft contact lens compared to changes to the BOZR.
Adaptation advice
Traditionally, practitioners would instruct all new contact lens wearers to adhere to an adaptation schedule to ‘ease’ into lens wear in an attempt to maximise the clinical performance of the contact lenses over the first few days of wear. However, it was recently shown that this is not required with current modern soft daily disposable contact lens materials, whether these were hydrogel or silicone hydrogel lenses. The lack of clinical benefit for a gradual adaptation schedule supports the adoption of a ‘no need to adapt’ approach for neophyte daily disposable lens wearers, and is likely to improve compliance. A study investigating the need for an adaptation schedule for bi-weekly or monthly soft contact lenses is currently under way.
Conclusions
As soft contact lenses continue to dominate the global contact lens market, it is essential that soft contact lenses are accurately fitted and assessed to ensure maximum success. Patient subjective response, vision and slit lamp examination should all be taken into account when determining whether the fit of a lens is optimal. Of course, the process for assessing soft contact lens fit does not cease after the initial assessment. The effects of factors such as wearing time, environmental conditions and ocular physiology, including dry eye, must be monitored constantly. Ongoing aftercare is key to continued contact lens success.
Dr Byki Huntjens is a senior lecturer at City, University of London and a paid consultant for Johnson & Johnson Vision.
Dr Rachel Hiscox is a Professional Education & Development Manager, UK & Ireland for Johnson & Johnson Vision Care.
- This article is part of a revised and updated ‘Essential Contact Lens Practice’ series, originally authored by Jane Veys, John Meyler and Ian Davies. This article was produced without further input or review from the original authors.
References
- Morgan PB, et al. International contact lens prescribing in 2019. Contact Lens Spectrum. Accessed 8 February 2020. https://www.clspectrum.com/issues/2020/january-2020/international-contact-lens-prescribing-in-2019
- Sulley A, Young G, Hunt C. Factors in the success of new contact lens wearers. Contact Lens and Anterior Eye. 2017;40(1):15-24
- Stapleton F, Stretton S, Papas E, Skotnitsky C, Sweeney DF. Silicone hydrogel contact lenses and the ocular surface. The ocular surface. 2006;4(1):24-43.
- Bhamra TS, Tighe BJ. Mechanical properties of contact lenses: The contribution of measurement techniques and clinical feedback to 50 years of materials development. Contact Lens and Anterior Eye. 2017;40(2):70-81.
- Young G, Schnider, Hunt C, Efron S. Corneal topography and soft contact lens fit. Optom Vis Sci, 2010;87:358-366
- Young G . Ocular sagittal height and soft contact lens fit. J BCLA, 1992; 15:1 45-49.
- Fonn D. Targeting contact lens induced dryness and discomfort: what properties will make lenses more comfortable. Optometry and Vision Science. 2007;84(4):279-85.
- Brennan NA, Lindsay RG, McCraw KA, Young L, Bruce AS, Golding TR. Soft lens movement: temporal characteristics. Optometry and vision science. 1994;71(6):359-63.
- Boychev N, Laughton DS, Bharwani G, Ghuman H, Wolffsohn JS. How should initial fit inform soft contact lens prescribing. Contact Lens and Anterior Eye. 2016;39(3):227-33
- Young G. Evaluation of soft contact lens fitting characteristics. Optometry and vision science. 1996;73(4):247-54.
- Wolffsohn JS, Hunt OA, Basra AK. Simplified recording of soft contact lens fit. Cont Lens Anterior Eye. 2009;32(1):37–42
- Brennan NA, Coles ML, Ang JH. An evaluation of silicone-hydrogel lenses worn on a daily wear basis. Clinical and Experimental Optometry. 2006 Jan;89(1):18-25.
- Chalmers R. Overview of factors that affect comfort with modern soft contact lenses. Contact Lens and Anterior Eye. 2014;37(2):65-76.
- Stahl U, Willcox M, Stapleton F. Osmolality and tear film dynamics. Clinical and Experimental Optometry. 2012;95(1):3-11
- Young G. Evaluation of soft contact lens fitting characteristics. Optometry and vision science. 1996;73(4):247-54.
- Roseman MJ, Frost A, Lawley ME. Effects of base curve on the fit of thin, mid-water contact lenses. International Contact Lens Clinic. 1993;20(5-6):95-101
- Young G, Holden BR, Cooke GE. Influence of soft contact lens design on clinical performance. Optometry and vision science. 1993;70(5):394-403.
- Wolffsohn JS, et al. Fast versus gradual adaptation of soft daily disposable contact lenses in neophyte wearers. Contact Lens and Anterior Eye. 2019;20. (Article in press)
