If there is one word to describe the difference between written forms of communication and those that have been discussed in this series to date, it is ‘permanence’. Spoken words take milliseconds to process and are gone. Judgements made on body language are over in seconds. The written word is different. Written words last for as long as the material they are written on lasts, and that can be thousands of years. No one can debate the words used, but, as we will see, without care, words can be taken as meaning different things to different people. A pupil defect does not mean the same to a teacher as it does to an ophthalmologist!
Readability
A body of text is made up of paragraphs, which are made up of sentences, which are made up of phrases, which are made up of words. The core structure within the text is the sentence, and it has been argued that the structure of the sentence is the key component to the readability of the text.1 Within the domain of clinical communication, a second key component which drives readability is the use of specific, medical terms which may not be understood by patients. In a world where communication is more open than it used to be, referral letters often being copied to the patient, care needs to be taken to avoid ambiguity in the written word. While a practitioner may be relieved to know that their patient is ametropic with 1.2 logMAR visual acuity, it is unlikely that most patients will understand what this means.
Readability can be measured. In the 1970s, Kincaid and others, working in the US military, developed the Flesch-Kincaid reading grade level to assess the difficulty of reading technical manuals. The Flesch reading ease test, calculates a numeric value for the readability of a passage of text. The value can be interpreted against levels of educational attainment as shown in table 1.2 The formula for the Flesch reading ease test is complex (figure 1) but it can be easily calculated using freely available online tools. Most versions of Microsoft Word also have the calculation built in as an option under File>Options>Proofing for Windows and through Preferences>Authoring and Proofing tools>Spelling and Grammar for Mac OS.
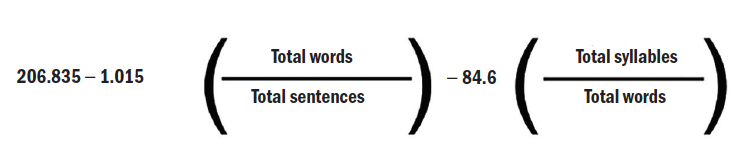 Figure 1
Figure 1
Readability of a whole, or part, of a website can also be assessed using online tools. Figure 2 shows the readability statistics for the portion of six UK optical websites dedicated to explaining the eye examination. As a comparator, the eye examination page of Wikipedia is also shown. While no claim is made that this is a scientific analysis, what is interesting is the consistency in the readability of the three sites managed by large retail chains (M1-M3). That said, none of the sites are able to breach a Flesch readability score of 60, making them ‘fairly difficult to read’ and pitched at a 16 to 18-year-old’s reading ability. The independent practices show much greater variability, with two of the three that I looked at showing negative readability scores. This variance between independent and retail optics is consistent with an analysis previously reported.3 It is quite possible that it is driven by the use of professional agencies to produce the web pages. It also seems that in many cases text is taken from material designed to be read by the eye care practitioner and re-purposed for the patient.

Figure 2: Readability of optical websites
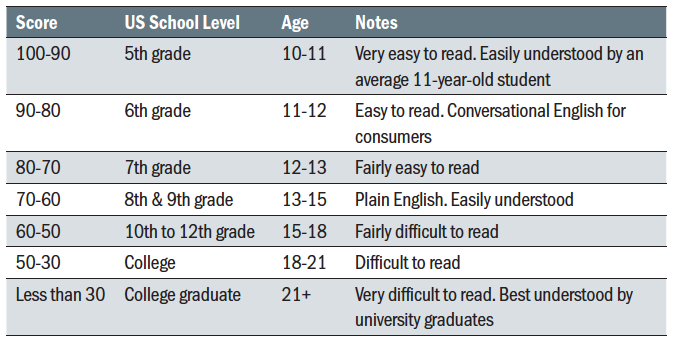 Table 1: Flesch reading ease
Table 1: Flesch reading ease
When designing a website, or indeed developing any patient literature, the practitioner should check its readability and test how understandable it is to a naive reader. If literature on how to handle contact lenses is being designed for those being fitted for myopia control, it should have an average readability in line with the age of the patients to be fitted. In a previous analysis of contact lens literature readability, the average patient handling guide was ‘fairly difficult to read’ and pitched for 16 to 18-year-olds.3
Use of words
One of the factors driving readability is the complexity of the words being used. In figure 2, the number of ‘complex’ words on the websites explaining the eye examination is plotted. It is clear that the sites that are most difficult to read are the ones with the longest words. It is the job of the eye care practitioner to be able to explain what is going on with the patients’ eyes in language that is easily understood.
A good example of this is in the use of the terms ‘eye test’ or ‘sight test’. The profession has, quite correctly, long argued that this is an oversimplification of the work carried out by the optometrist. An ‘eye examination’ is a better descriptor. A ‘comprehensive eye examination’ better still. But consider the words that patients use. Table 2 shows the results of entering the four descriptors into a search engine. If we assume the results are indicative of the language used within the category, the extent by which ‘eye test’ is the common term is overwhelming. Looking then at the top 10 sites that appear when each phrase is used, shows the trend towards the use of the word ‘test’ by optical chains (and the NHS) vs ‘exam’ by the professional bodies and independents. 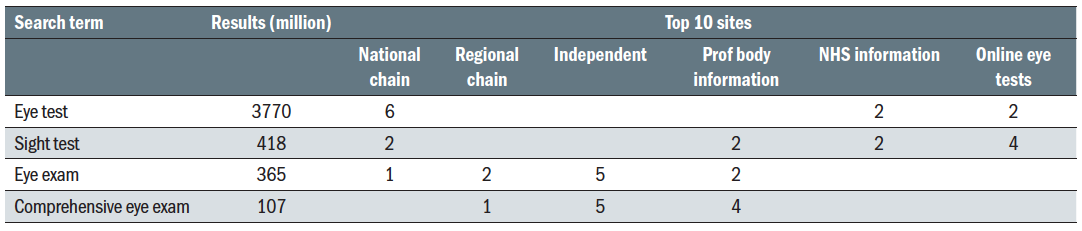 Table 2: Google search results
Table 2: Google search results
This does not mean that the profession should give up on the word ‘exam’. But understanding that ‘test’ is the commonly used language of the patient can help direct the written word. If a patient is scanning text looking for an eye test, they may miss the practices information about eye examinations. Rather than
writing: ‘We offer comprehensive eye examinations to all our patients,’ the practice might consider something along the lines of: ‘Our eye tests provide a comprehensive assessment of your vision and your eye health’. Once the patient is in the practice, then there is an opportunity to educate them on the benefits of the comprehensive eye examination that you offer. If they never come in, you never get this chance.
A universal truth of all businesses is that it is easier to keep existing clients than to gain new ones. In eye care, the reminder letter is one of the most powerful written tools to communicate with patients. Of all the written correspondence, this is probably the one that requires the most care, particularly for the independent practice which does not have the resources to compete with retail advertising. In many cases it is an opportunity which is not optimised.
The reminder letter, or email, is an opportunity for the practice to communicate the unique benefits the patient can expect from booking an appointment. It is an opportunity for the practice to explain what is new and any seasonal offers that may be available. With the increasing availability of advanced diagnostic
equipment, most practices are keen to communicate what they have. Unfortunately, as with web sites, the language used is normally taken from the manufacturer’s literature. There are two issues with this; firstly, the language used is technical, the words complex and the readability difficult. Secondly, there is rarely a benefit statement to the patient. Just saying: ‘Our practice is now equipped with the latest XYZ retinal screening device,’ gives the patient no idea of its benefit. It is important to remember that the primary reason that a patient makes an appointment is to improve or correct their vision. It is the job of the eye care practitioner and practice staff to educate them on the importance of their visual health and how this can be assessed.
Rather than using an expression like: ‘We now do ultra-widefield retinal imaging using our new ABCD system,’ the practice should consider something along the lines of: ‘At your appointment we will take a photograph of the back of your eye using the latest technology. This will help us in assessing the health of your eye. The images that we take will be stored so that we have a record from which any changes can be seen in the future.’
Questionnaires
The use of written patient questionnaires is growing, especially in pre-screening. For some conditions, for example dry eye disease, the questionnaire is a validated element of the diagnosis (figure 3).4 The value of any questionnaire is only going to be as good as its administration and readability. The five-question dry eye questionnaire is good in terms of its structure and readability. If one assumes that it is going to be given to patients with an explanation that it is a valuable tool assisting in the diagnosis of the underlying problem that they are presenting with, then it is likely to be taken seriously and given due consideration.

Figure 3: A questionnaire is a validated element of dry eye disease diagnosis and monitoring
The problem with questionnaires is that they are only as good as the patient’s assessment of them. This in turn will depend on the relative importance the patient places on their accurate completion. Most patients will over-estimate those aspects of their life which would be perceived as being positive by a third party and under-estimate those that would be viewed as negative. The classic case of this is the routine under-reporting of alcohol consumption by people completing a survey.5 If a patient does not see that there is any relevance in a question about their general health when attending, for what they describe as an ‘eye test’, they may well just tick the box that says ‘fine’.
Questionnaires should only be deployed where there is a clear benefit over a face to face discussion. In a research, or data collection setting, they can be used to codify and quantify the variables under investigation. A practice may have an interest, for example, in how many patients presenting with a certain symptom are
taking a particular medication or working in a particular environment. Collection and collation of patient data must be done with due regard to patient confidentiality and data protection.
Questionnaire responses should not be taken in isolation. The paperwork should be given by someone who can explain why the information is being sought and why it is important. The practitioner should then read through the results with the patient and not be afraid of asking supplemental questions and points of clarification. It then goes without saying that all questionnaires should be tested for readability, and, ideally, piloted with a sub-set of patients before being deployed.
Social Media
With 45 million people in the UK being active social media users,6 the written word is more prevalent than ever before. While social media can be a valuable asset in promoting the practice (figure 4),3 its lack of discrimination can also be problematic. When not controlled, social media blurs the boundary between a person’s professional and personal life. Comments which may seem
amusing in one context, could be viewed as trivialising the professionalism of an individual in another. Whether a practice chooses to communicate across social media platforms or not, they should have guidelines on its use for all employees. Ideally these guidelines should be written into employment contracts. Part of the guidelines should be explicit about who is allowed to post material on behalf of the practice and the type of material that is allowed.
 Figure 4: Social media can be a valuable asset in promoting the practice
Figure 4: Social media can be a valuable asset in promoting the practice
Any practice with a social media presence must set up a system to monitor it at least daily. Patient complaints should be managed off line and derogatory remarks investigated and, if appropriate removed. Guidelines on the use of social media in practice are available from the College of Optometrists,7 and the General Medical Council.8
Summary
The written word has a permanence that other forms of communication do not. When writing patient facing material, the practice needs to consider how understandable it is to the target patient. Readability can be quantified using online tools which will give a value based on average reading age and percentage of long words. This can be taken as a guide, but the best way of testing the readability of any text is by asking a selection of those who it is intended for to read it and provide feedback. While questionnaires may seem attractive as an efficient way of capturing patient information, caution should be taken. In isolation, a questionnaire is only as good as the seriousness with which the patient takes it and its readability. Questionnaires should be deployed in conjunction with the verbal and non-verbal communication skills described previously in this series.
Ian Davies is an optometrist now working as an independent motivational speaker, coach and business consultant.
- Look out for interactive CET linked with this series, starting next month.
References
- Moran J. First you write a sentence. 2018.Penguin Random House UK.
- Flesch R. How to write plain English. 2016.University of Canterbury press.
- Davies IP. The use of social media in optometric practice. American Academy of Optometry Meeting, 2019, Orlando.
- Chalmers R, Begley CG, Caffery B. Validation of the 5-Item Dry Eye Questionnaire (DEQ-5): Discrimination across self-assessed severity and aqueous tear deficient dry eye diagnosis. Contact Lens and Anterior Eye, 2009, 33(2):55-60
- Gilligan C, Anderson KG, Ladd BO et al. BMC Public Health, 2019, 19:1639.
- Statista. UK: social media usage 2019 available at https://www.statista.com/statistics/507405/uk-active-social-media-and-mobile-social-media-users/
- The College of Optometrists. Social Media and online behaviour. At https://guidance.college-optometrists.org/guidance-contents/communication-partnership-and-teamwork-domain/social-media/#open:219,220,221
- General Medical Council 2013. Doctors Use of social media. At https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/doctors-use-of-social-media
