Why is informed consent a benefit to contemporary ophthalmic practice?
There are two fundamental reasons why informed consent is beneficial in practice. One is from the patient’s perspective and the other from the practitioner’s perspective as follows:
- It empowers patients to decide what is (or is not) going to be done to them, weigh up the risks and benefits of options available, and choose a particular course of action.
- It provides practitioners with a defence to any criminal charge of assault, battery, trespass to the person, or a civil claim.
‘An assault is intentionally or recklessly causing another to apprehend immediate and unlawful violence, whereas battery is the intentional or reckless infliction of unlawful force or recklessly applying unlawful force to another.’1 In practice, this means interacting (for example, touching the patient) or conducting an ‘invasive’ procedure without consent, or undertaking an incorrect procedure (such as administering an eye-drop in the wrong eye) with consent.
The evolution from peer-view ‘consent’ into patient-centred ‘informed consent’ over a period of 58 years in the UK, as a result of court judgements on landmark cases from 1957 onwards, has fundamentally changed practitioner obligations and patient rights regarding the standard of care, for clinical diagnosis, treatment and disclosure.
In its guidance2 on the legal framework that healthcare practitioners need to take account of in obtaining valid consent to examination, treatment or care, the Department of Health states that consent is only valid if the patient:
- Has capacity to give consent.
- Gives consent voluntarily.
- Has received sufficient information to decide upon consent.
Has capacity to give consent
Much of what is meant by ‘capacity’ is enshrined in law. Adults are presumed to have capacity to make decisions regarding their own healthcare needs, such as examination and treatment interventions, in the absence of evidence to suggest otherwise (figure 1).3,4 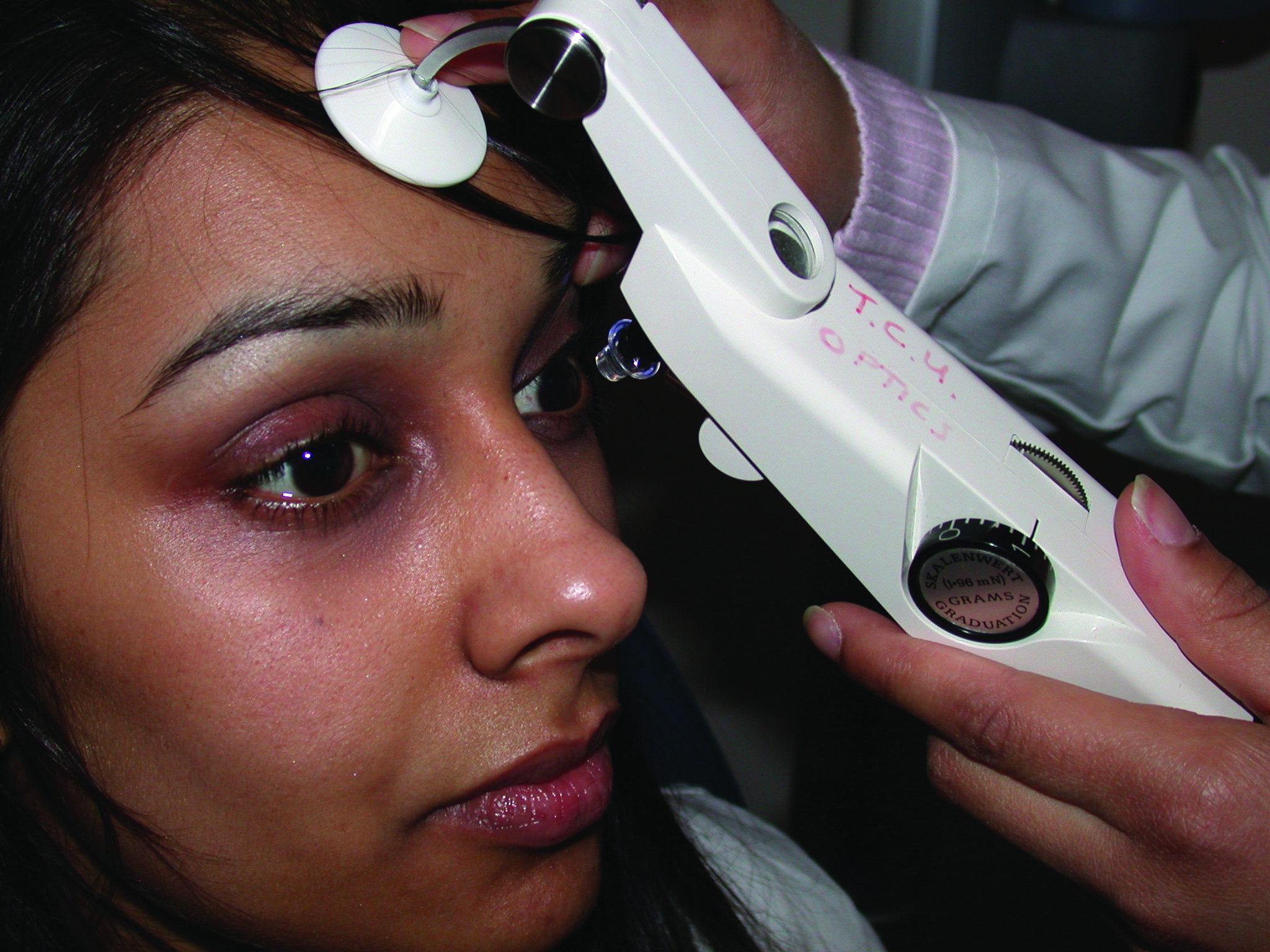 Figure 1: An adult patient presumed to have capacity to make decisions regarding clinical procedures
Figure 1: An adult patient presumed to have capacity to make decisions regarding clinical procedures
A patient is deemed to lack capacity if ‘in relation to a matter, if at the material time he is unable to make a decision for himself in relation to the matter because of an impairment of, or a
disturbance in the functioning of, the mind or brain. It does not matter whether the impairment or disturbance is permanent or temporary. A lack of capacity cannot be established merely by reference to the following:
- A person’s age or appearance.
- A condition of his, or an aspect of his behaviour, which might lead others to make unjustified assumptions about his
capacity’.4
Impairment, or a disturbance in functioning of the mind or brain, can include any of the following (though this list is not exhaustive):
- Mental health conditions, such as schizophrenia or bipolar disorder.
- Dementia states.
- Severe learning disabilities.
- Brain damage, such as caused by stroke or other brain injury.
- Physical or mental conditions that cause confusion, drowsiness or a loss of consciousness.
- Intoxication caused by substance misuse.
A person’s capacity can also be temporarily affected by the
following (again, not an exhaustive list):
- Shock
- Panic
- Extreme tiredness or fatigue
- Medication
- Distraction
- Stress
Healthcare practitioners are expected to take all reasonable steps to support the patient in making a decision themselves before concluding that they cannot. This may involve taking extra time with the patient and using language appropriate to their level of understanding. This may involve using interpreters, sign language, visual materials, communication aids, and so on (figure 2). The patient’s carers may be able to help in this regard, but they cannot give valid consent on behalf of the patient.
 Figure 2: A wide range of techniques, from signing to written instruction to visual aids, might need to be employed to enable a patient to give informed consent
Figure 2: A wide range of techniques, from signing to written instruction to visual aids, might need to be employed to enable a patient to give informed consent
The patient is generally deemed to have capacity if they are able to:
- Understand the information given.
- To retain and evaluate this information.
- Make a decision.
- Communicate that decision.
It is reasonable to conclude, on the balance of probability, that the patient lacks capacity to make a specific decision if they lack one or more of these traits.4 No one can consent on behalf of a person lacking capacity. In such a situation, if the patient has not made an advance decision (something only used for refusal of, or request for specific treatments) or has a formally appointed person to make decisions for them (such as an attorney for health and welfare, or a deputy appointed by the Court of Protection – figure 3), the patient’s ‘best interests’ become the drivers in the decision-making process taking into account factors detailed in the Mental Capacity Act 20054 and the Mental Act 2005 Code of Practice.5 This may well mean that the practitioner has to delay or postpone the intervention if more time is needed to obtain valid consent.  Figure 3: An attorney for health and welfare may make decisions on behalf of the patient
Figure 3: An attorney for health and welfare may make decisions on behalf of the patient
The situation for young persons aged 16 to 17 years is the same as that for adults, with some restrictions. These include decisions about blood and/or organ donation, agreement in participating in research and refusal of treatment.3 As for children (under 16 years), either parent can consent as long as they have capacity and as long as they were married when the child was born. If not, only the mother can consent.
There are some circumstances when others can consent for children (such as guardians and others with parental responsibility), and these are set out in detail in the Children Act 1989.6 Children under 16 years may give consent to examination and treatment in their own right if they are deemed to have capacity. This would be a sufficient understanding to grasp fully what is involved in a proposed intervention, including its purpose, nature, and implications, to make a decision, and to communicate that decision. In such a case they would be described as being Gillick competent.7
Gives consent voluntarily
Although self-evident, for consent to be valid, it must be given freely and without coercion. While patients may at times want to seek support from others, subtle (or otherwise) pressure to adopt a particular treatment option may come from partners, family members, friends, employers, carers or even other healthcare practitioners. It may seem obvious, but it is worth mentioning that discussing examination or treatment options with patients on their own may indeed elicit their bona fide choice. This may further be helped by giving the patient some time to consider their options before finally deciding; a so-called cooling off period.
Sufficient Information
In 1957, this was decided by the landmark case of Bolam v Friern Hospital Management Committee8 which established the Bolam test and the principle that a healthcare practitioner ‘is not guilty of negligence if he has acted in accordance with a practice accepted as proper by a responsible body of medical men skilled in that particular art. Putting it another way round, a doctor is not negligent if he is acting in accordance with such a practice, merely because there is a body of opinion that takes a contrary view.’ This became the litmus test for all future cases where the standard of care for diagnosis, treatment and disclosure, including consent information and advice given, was in question. It is also sometimes referred to as the peer-view.
To understand the metamorphosis of consent from peer view to patient-view informed consent, it is important to appreciate the concept of a disclosure claim. This arises when a patient alleges that, had they been informed about the risks associated with a particular procedure, intervention or treatment option, they would have declined it, would have delayed it, or would have selected an alternative if given the choice. This is different to other clinical negligence claims in that determining what information to provide to the patient does not involve the use of clinical skills.
Subsequently, the case of Bolitho v City and Hackney Health Authority9 refined the Bolam test, moving away from simply peer view to expert views that must withstand logical judicial analysis and greater scrutiny. In Pearce v United Bristol Healthcare NHS Trust,10 the Bolam test was applied and, though the Pearces were not successful in their claim for negligence, there was an explicit departure from the Bolam test towards the patient’s prerogative regarding risk disclosure.
In Chester v Afshar,11 the surgeon was held negligent in failing to warn the patient of the 1 to 2% risk of nerve injury and possible motor and sensory impairment inherent in her back surgery, even if correctly completed. This was an unequivocal judgement made by the Court of Appeal in May 2002, that even small risks must be declared, and that it was for the patient to weigh up the importance of that risk to them – not the practitioner. This judgement also made it clear that a failure to recognise that the patient has the right to make decisions about their treatment would attract liability even if that failure has not caused any harm.
In Birch v University Hospital NHS Foundation Trust,12 Justice Cranston, applying the Bolam test modified by Bolitho, found for the claimant. This judgement obliges practitioners to disclose benefits and risks of alternative procedures, treatments or interventions, so that patients can make informed decisions about all the options available.
This approach was then ratified in the landmark case of Montgomery v Lanarkshire Health Board13 concerning Mrs Montgomery, an insulin dependent diabetic, who, in 1999, was expecting her first baby. As a result of her diabetes, it was likely that her baby was going to be large (macrosomia). The risk of shoulder dystocia (the situation where, after delivery of the head, the baby’s anterior shoulder gets caught above the mother’s pubic bone) is 9 to 10% in diabetic mothers. However, in this instance, the consultant obstetrician and gynaecologist failed to warn Montgomery on the grounds that the probability of a grave complication for the baby was just a 0.2% risk of a brachial plexus injury, and less than 0.1% of the umbilical cord becoming trapped and occluded and causing prolonged hypoxia, resulting in cerebral palsy or death of the baby. The same consultant also failed to give Mrs Montgomery the choice of a caesarean section. Complications during the delivery ensued and the baby was born with severe disabilities. The Supreme Court ruled that it was incumbent on the consultant obstetrician and gynaecologist to advise Mrs Montgomery of the common14 risk of shoulder dystocia, and the very small risk of catastrophic injury resulting from the deprivation of oxygen if a vaginal delivery were attempted, and to discuss with her the alternative of a caesarean section. The Bolam test was regarded as inappropriate with respect to consent and disclosure in this case and, after the appeal went to the Supreme Court and was allowed, Montgomery was awarded £5.25 million in damages.
With the Montgomery judgement, the principle of patient-view informed consent finally arrived unequivocally into UK law in 2015, with risk disclosure becoming entirely patient-centred and the situation regarding ‘sufficient information’ in law updated.
Practitioner obligations and patient’s rights
The Bolam principle still continues to be the litmus test for the standard of treatment – but not for disclosure. That is to say, when clinical skills are challenged, expert opinions will still normally be sought and decisions made based on what is considered to be the standard of treatment that would be delivered by a ‘prudent practitioner’ in the relevant field. Professional guidelines often come into play in such situations.
The Montgomery principle replaces the Bolam principle for disclosure and consequently consent. This means that the duty of care now obliges practitioners to provide patients with
information about all aspects that may have an impact on the patient’s decision (figure 4). This includes:
- Treatment options
- Alternatives
- Advantages and disadvantages of each
- Risks of each
- Answers to all the patient’s questions
 Figure 4: The Montgomery principle obliges the practitioner to provide patients with information about all aspects that may have an impact on the patient’s decision
Figure 4: The Montgomery principle obliges the practitioner to provide patients with information about all aspects that may have an impact on the patient’s decision
The practitioner is required to ensure that all ‘material’ risks are understood by the patient. In law, a risk is deemed material ‘if, in the circumstances of the particular case, a reasonable person in the patient’s position, if warned of the risk, would be likely to attach significance to it or if the doctor is or should reasonably be aware that the particular patient, if warned of the risk, would be likely to attach significance to it.’13 The proviso being that the material risk should be well known and a reasonable practitioner would be aware of it,14 and any reasonable alternative treatment should be widely known about or commonly accepted practice.15 This is necessary before it is possible to be satisfied that the patient has proper and complete information to consent, or decline a particular course of clinical intervention. For example, one patient may not consent to wearing extended-wear contact lenses which carry the potential, though rare,16 risk of sight threatening microbial keratitis of 19.5 per 10000 wearers per year17 while another may indeed consent notwithstanding the risk.
Although it has no binding authority in UK, it is worth noting that the attending ophthalmologist in Rogers v Whitaker,18 failed to warn the patient with sight loss in one eye of the very rare16 (1 in 14000 or 0.0071%) chance of developing sympathetic ophthalmitis (a diffuse granulomatous inflammation of the uveal layer in both eyes following trauma to one eye that can cause total blindness) in the good eye with the blind eye undergoing elective surgery. As a result, the Supreme Court of New South Wales, Australia, determined that there was a duty to warn patients of any material risks involved in a proposed clinical intervention. In this case, Mrs Maree Whitaker was awarded AU$808,564.38 for negligence with regards to consent.
The point is, risk cannot be condensed to just percentages. A material risk to one patient may not be such to another. Risk will vary from patient to patient, and this has to be discussed between practitioner and patient before valid informed consent can be realised.
Practitioners may contend that disclosing rare16 or uncommon, but more serious, risks of some diagnostic and treatment options might unduly alarm patients and may even put them off agreeing to something that might be considered in their best interest. However, the Montgomery judgement means that it is no longer up to the practitioner to decide if a risk or a question is relevant. It is the patient’s right. Some risks are very rare and may never come to pass in the patient’s or the practitioner’s lifetime, but nevertheless they have to be raised.
Establishing consent
There are very few instances where written consent is required by law. Examples of this include with relation to the storage and use of gametes and embryos in fertility treatment. In general, verbal consent is as valid as written consent. The important thing is that consent is a process based on a dialogue between the patient and the practitioner, and not just a ‘tick in a box’ exercise or a signature on a form. While tick boxes and signatures on forms do provide evidence that the practitioner has paid some attention to patient consent, they do no more than that. If there is any question over whether valid consent was obtained, the key issue will not be whether a box was ticked by the practitioner or not, nor whether the patient had signed a form or not, but whether the patient was given all the information they needed to make an informed decision and they understood it. For example, patients considering contact lens wear, should be told about the actual risks of microbial keratitis with differing types of contact lenses and modalities of wear, and that contact lens wear is not a risk-free intervention. It should be established that it is possible to suffer an adverse event related to non-modifiable risk factors,17 even if the patient follows the practitioner’s advice and has regular check-ups. Discussions with patients have to cover key up-to-date facts, together with the known risks of adverse effects, of any diagnostic techniques or interventions to be undertaken, along with any alternatives. Only then can they decide if a risk is material, and it is the patient’s right to be able to do so.
Many practitioners use patient information leaflets to help with explanations and to give information to patients (figure 5). Often produced by suppliers, professional organisations, and some practices themselves, they are intended to inform patients in understanding ocular conditions and to making informed decisions regarding treatment choices. Unfortunately, some may be ‘out of date’ and some more ‘point-of-sale’ material and somewhat biased towards a particular product or service – these are best avoided. Should the information in the patient information leaflets used not be correct, up-to-date or be misleading, the practitioner who hands them out is liable even if they are not the author.19 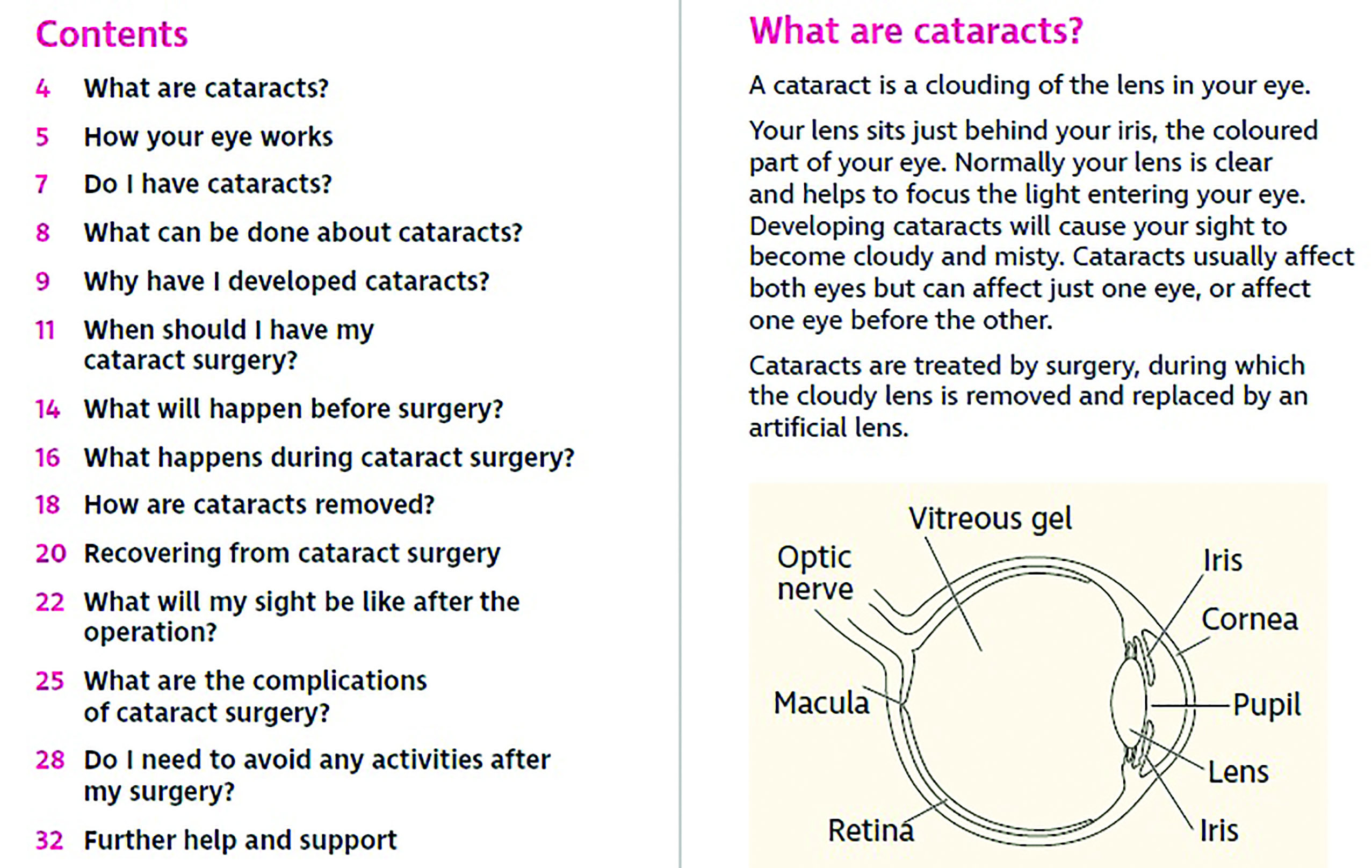 Figure 5: Many practitioners use patient information leaflets to help with explanations
Figure 5: Many practitioners use patient information leaflets to help with explanations
Patient information leaflets are not intended to be a substitute for dialogue between patient and practitioner, but instead are intended to complement the discussions. As such, they have to be carefully checked regularly to ensure that they are up-to-date, accurate, and contain information that is apposite. It is best practice to keep a copy of the information leaflet, annotated as appropriate and as provided to the patient, in the records of the recipient for future reference should there be a question regarding information supplied to the patient.
Patient information leaflets could be used more creatively in practice as part of the informed consent process. They could, for example, be used to give patients clear information about a variety of ophthalmic practice activities, such as personal data handling and processing by the practice, examination or diagnostic procedures, treatment intervention options, associated risks and so on. Patients could be supplied with these leaflets to ‘pre-read’ and then be given an opportunity to ask questions. They could also then discuss opting out, if they so wish, from parts of the examination and/or interventions that they consider to be unacceptable to them before, or during, any formal consultation or attendance at the practice.
It is important however, that patients are not inundated with technical information but, instead, are provided with information that they can easily digest. This means that it is best to use terminology that the patient can relate to when obtaining consent. For example, consider the very low risk of precipitating an angle closure attack (approximately 1 in 20,000 or 0.005%20) when using topical mydriatics for diagnostic purposes. This could be explained as ‘perhaps two or three people out of a full Villa Park stadium in Birmingham, around 43,000 people in all, might get a pressure reaction with these dilating drops.’ The author would contend that this more informative and accurate than simply stating that it is an ‘unlikely’ or a ‘highly unlikely’ adverse event and leave it to the patient to decide if this risk is material to them based on that. Risks of adverse effects from diagnostic or clinical interventions should be stated with an indication of what the frequency of the risk is (very common, common, uncommon, rare, very rare or frequency not known)16 where known.
Record-keeping
Informed consent is a process, and good record keeping is part of the process. It is essential to keep clear, relevant, unambiguous, contemporaneous notes of consent discussions between patient and practitioner regarding risks and adverse effects. This is particularly so where any intervention carries the risk of a grave adverse effect, however small, ensuring that the patient has understood this. Practitioners might use tick boxes as an aide memoire to ensure discussion on a particular aspect is covered; but that is all tick boxes are in the eyes of the law. They are not necessarily proof of informed consent.
Similarly, consent forms that contain key up-to-date facts, together with known risks and adverse effects, of diagnostic techniques or treatments and their alternatives may be used. But again, they are not necessarily proof that consent was indeed informed, or that risks were fully understood by the patient, and therefore valid. This has been reiterated in the case of Hassell v Hillingdon Hospitals NHS Foundation Trust,21 where Mrs Hassell underwent spinal surgery having signed a consent form on the day of the surgery when her mind was not engaged. She was paralysed as a result of the surgery and the court found that the claimant, under the circumstances, had not given informed consent despite having signed a consent form, and was awarded the sum of £4.4 million.
More guidance on informed consent for health professionals and practices is available from a number of organisations and readers are advised to consult these.22-25
NB – It is essential to remember that every case turns on its own merits and that any views expressed here are not a substitute for formal legal counsel.
Dr Nizar Hirji is Optometrist Consultant, Hirji Associates, Birmingham.
References
- Halsbury’s Laws of England, Criminal Law, V.25 (2010), Paras 1-426; V.26 (2010), Paras 427-792, 2.Offences against the person, 3 Non-Fatal offences against the person (x) Assault, A. Common assault and battery, 157. Assault and battery.
- ‘Reference guide to consent for examination or treatment’ (second edition) https://www.gov.uk/government/publications/reference-guide-to-consent-for-examination-
or-treatment-second-edition last accessed March 2020 - Family Law Reform Act 1969 http://www.legislation.gov.uk/ukpga/1969/46 (last accessed March 2020)
- Mental Capacity Act 2005 https://www.legislation.gov.uk/ukpga/2005/9/section/2 (last accessed March 2020)
- Mental Capacity Act 2005 – Code of Practice. The Stationary Office ISBN 978 0 11 7037465 This document can be viewed at www.publicguardian.gov.uk (last accessed Apr 2020)
- Children Act 1989 http://www.legislation.gov.uk/ukpga/1989/41/section/5 (last accessed March 2020)
- Gillick v West Norfolk and Wisbech AHA [1985] UKHL 7 (17 October 1985) https://www.bailii.org/uk/cases/UKHL/1985/7.html (last accessed March 2020)
- Bolam v Friern Hospital Management Committee [1957] 1 WLR. 582
- Bolitho v City and Hackney Health Authority [1997] 3 WLR. 1151
- Pearce v United Bristol healthcare Trust [1998] EWCA Civ 865.
- Chester v. Afshar [2004] UKHL 41.
- Birch v University College London Hospital NHS Foundation Trust [2008] EWHC 2237 (QB); (2008) 104 BMLR. 168
- Montgomery v Lanarkshire Health Board [2015] UKSC 11
- Duce v Worcestershire Acute Hospitals NHS Trust [2018] EWCA Civ 1307
- Bayley v George Eliot Hospital Trust [2017] EWC 3398 (QB)
- British National Formulary (2020) Adverse reactions to drugs, Description of the frequency of side effects https://bnf.nice.org.uk/guidance/adverse-reactions-to-drugs.html (last accessed March 2020)
- Stapleton,F; Keay, L; Edwards,K; Naduvilath, T; Dart, JK; Holden,BA (2008) ‘The Incidence of Contact Lens-Related Microbial Keratitis in Australia’ Ophthalmology Volume 115, Number 10, October 1655-1662
