Due to the close embryological and anatomical link between the brain and the eye, many diseases affecting the central nervous system (CNS) also manifest at the ocular level. In addition, the treatment for these disorders may have ocular side effects that need to be recognised and managed
appropriately.
Sedatives, hypnotics and anxiolytics
Although having some significantly different properties, there is a huge overlap between these classes of drugs and, hence, are being presented here in one section. They all have in common the fact that they all ‘slow down’ the brain’s activity in one way or another and to varying degrees. The drugs may be used for the treatment of a large variety of conditions, ranging from insomnia through
to anxiety and even epilepsy. Some are also used to induce anaesthesia.
The most widely known drugs in this complex class are barbiturates and benzodiazepines (table 1).
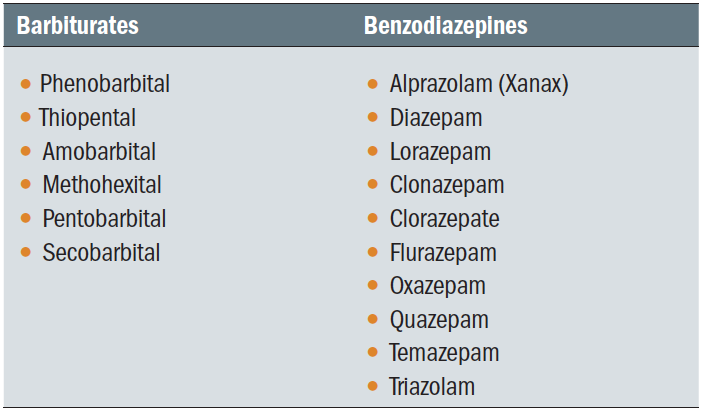 Table 1: Currently prescribed barbiturates and benzodiazepines
Table 1: Currently prescribed barbiturates and benzodiazepines
Barbiturates
Barbiturates were more commonly prescribed in the past, particularly in the 1950s and 1960s where they were commonly used as a sleeping aid. However, due to their high toxicity and dependency, they are today only prescribed occasionally, and very much based on patients’ individual circumstances. For their therapeutic purposes, they are progressively being replaced by benzodiazepines.
Phenobarbital, one of the best-known barbiturates, is used as a short-term sedative and for the treatment of epilepsy. It is also used to treat other types of seizures in both children and adults. It can be administered intravenously (reserved for satus epilepticus, where successive seizures occur before recovery from the preceding one) or orally. Reported ocular side effects associated with phenobarbital are nystagmus and diplopia.
Benzodiazepines
Benzodiazepines are most typically used to treat anxiety and are the most commonly prescribed sedative drugs. Alprazolam (Xanax) and diazepam are maybe the most known and used benzodiazepines.
After dependence and liver toxicity, side effects at the ocular level are the most common reported. The use of benzodiazepine has been linked to decreased contrast sensitivity (figure 1),1 dysfunction of saccades and smooth-pursuits and nystagmus2,3 and retinal toxicity.4 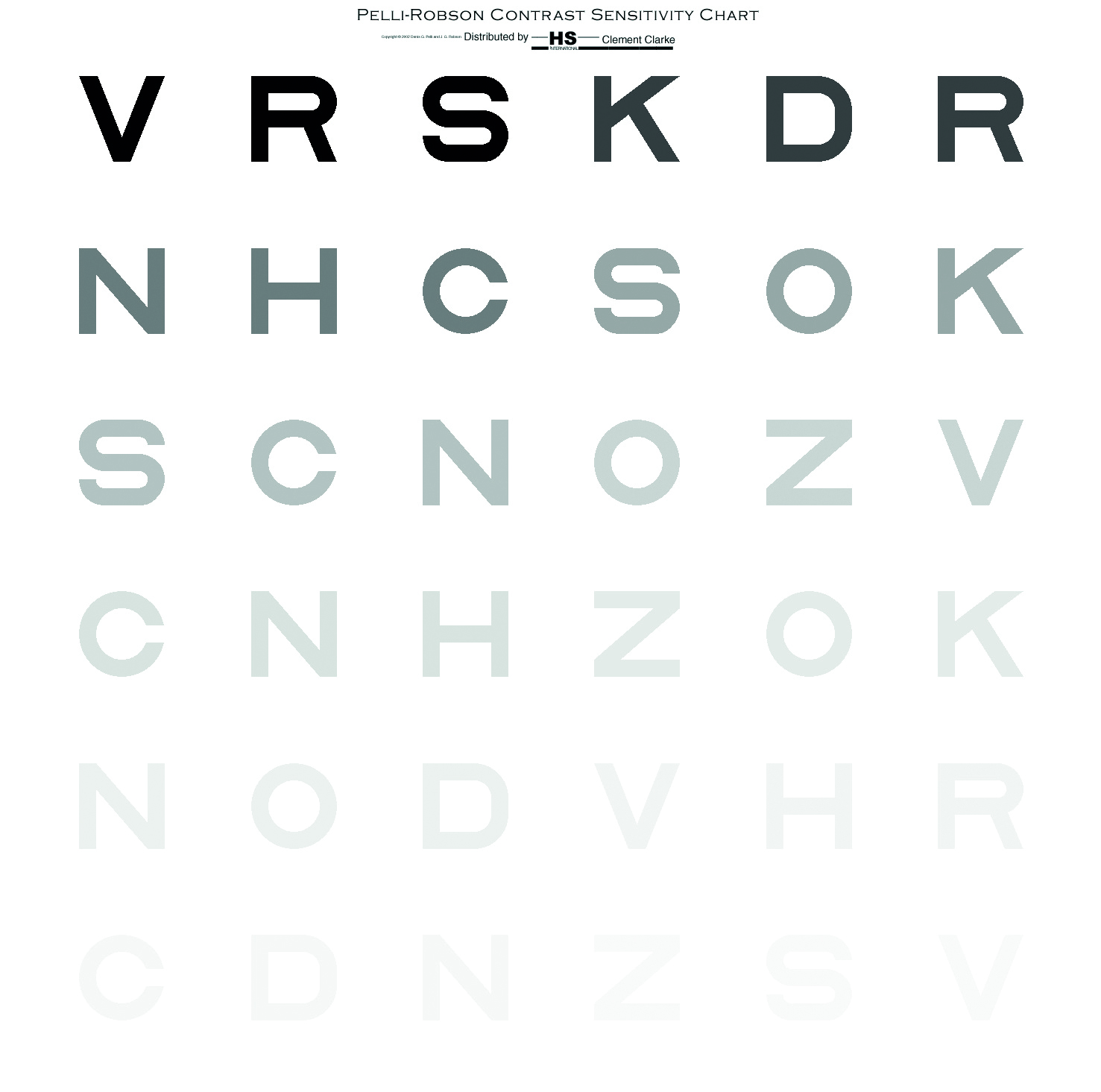 Figure 1: Loss of contrast sensitivity may occur with use of benzodiazepines
Figure 1: Loss of contrast sensitivity may occur with use of benzodiazepines
Antidepressants
Clinical depression, or major depressive disorder (MDD), is one of the most common mental health problem worldwide, being reported as the second leading cause of ‘years lived with a disability.’5 In 2014, 19.7% of people in the UK aged 16 and over showed symptoms of anxiety or depression.5 Risk factors for MDD include:
- Family history
- Existing health conditions (including loss of sight)
- Major life events (bereavement, divorce, job loss, debt)
- Certain prescribed medications
- Drug abuse
Depression is usually treated with counselling, anti-depressants or a combination of therapies.
Anti-depressants are classed into five categories by NHS UK6 as follows:
- Selective serotonin reuptake inhibitors (SSRIs); these are the most commonly used anti-depressants, and have fewest side effects. Examples include fluoxetine (Prozac), citalopram and sertraline (figure 2).
- Serotonin-noradrenaline reuptake inhibitors (SNRIs); examples include duloxetine and venlafaxine.
- Noradrenaline and specific serotonergic antidepressants (NASSAs); these are prescribed for individuals that have contraindications for either SSRIs and SNRIs, and include mirtazapine.
- Tricyclic antidepressants (TCAs); these are used less often and have more side effects. Currently, they are prescribed as a treatment for severe depression, and also for obsessive compulsive disorder (OCD) and bipolar disorders. Examples are amitriptyline, clomipramine, imipramine, lofepramine and nortriptyline.
- Monoamine oxidase inhibitors (MAOIs); these drugs are now rarely used due to the high number of side effects. Examples include tranylcypromine, phenelzine and isocarboxazid.
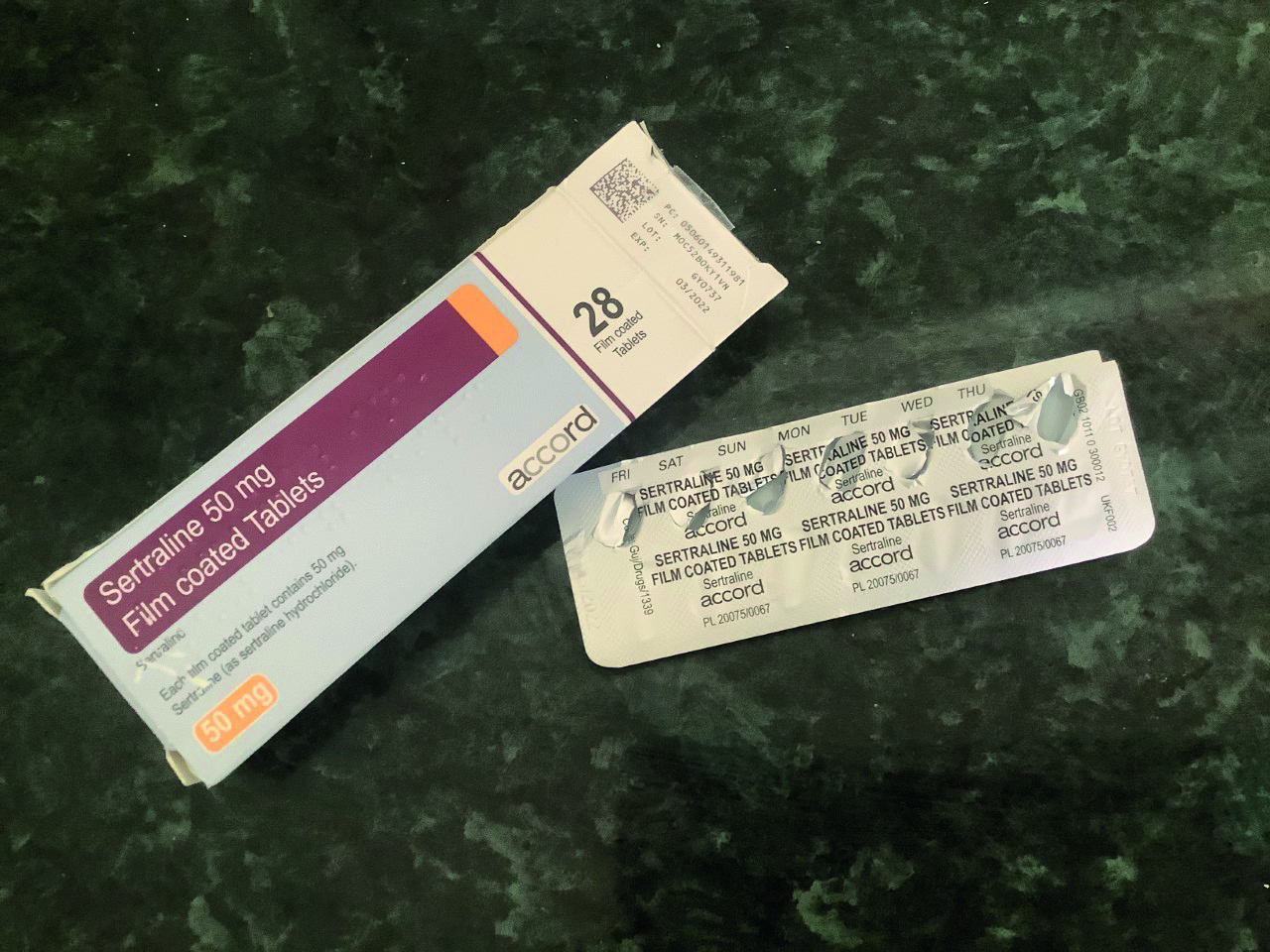 Figure 2: Selective serotonin reuptake inhibitors are commonly prescribed and have the fewest side effects of all antidepressants
Figure 2: Selective serotonin reuptake inhibitors are commonly prescribed and have the fewest side effects of all antidepressants
At the ocular level, the use of antidepressants has been associated with decreased lacrimation and other tear film changes, as well as with accommodative insufficiency and increased intraocular pressure (IOP). In addition, SSRIs and SNRIs can also cause mydriasis and cycloplegia.7 Acute angle closure with pupil block cases in patients with narrow angles have also been reported8 and this reminds eye care practitioners of the importance of recording the presence of narrow angles (figure 3). MAOs work by blocking an enzyme which reduces noradrenaline (NA) levels at neuromuscular junctions in the autonomic nervous system. The resultant impact of raised NA enhances sympathetic activity, and therefore mydriasis and cycloplegia may occur.  Figure 3: Mydriasis may occur with some anti-depressants and so it is important to have identified the presence of a narrow angle
Figure 3: Mydriasis may occur with some anti-depressants and so it is important to have identified the presence of a narrow angle
Antipsychotics
Psychosis is a symptom of many disorders of psychiatric, neurodevelopmental, neurologic and medical nature.9 The American Psychiatric Association’s (APA) publishes the Diagnostic and Statistical Manual of Mental Disorders (DSM) which defines psychosis as ‘the presence of hallucinations (perceptions occurring in the absence of corresponding external or somatic stimuli) without insight into their pathologic nature, delusions (fixed false beliefs), or both hallucinations without insight and delusions.’9
Psychotic disorders can be primary or secondary as outlined in table 2. 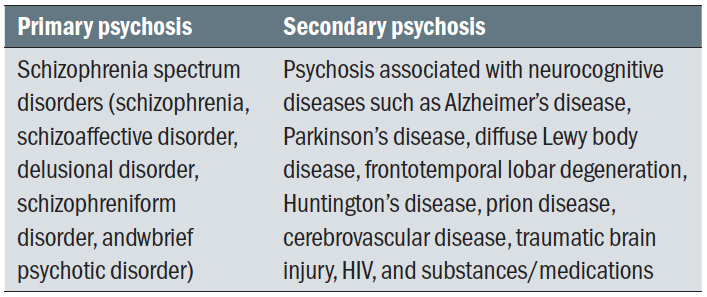 Table 2: Classification of psychotic disorders
Table 2: Classification of psychotic disorders
Medications for psychoses are classified as either typical or atypical antipsychotic drugs, a distinction based mainly on the presence or absence of side effects. Typical antipsychotic medications are the first generation of such drugs and have a multitude of side effects, while the atypical drugs are newer and are better tolerated. The list of available antipsychotic medications in the UK is shown in table 3 and is available from NICE.10 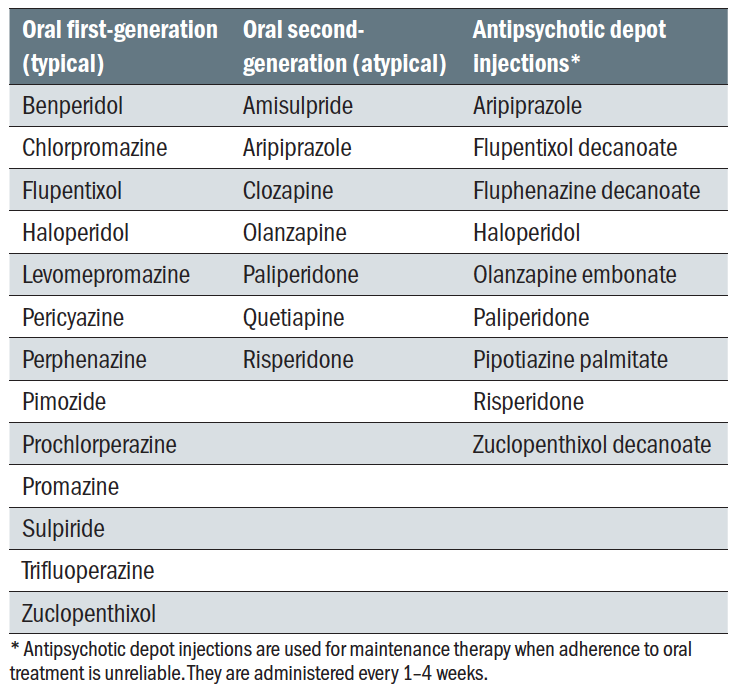 Table 3: Antipsychotic drugs available in the UK
Table 3: Antipsychotic drugs available in the UK
Typical antipsychotic drugs, such as the phenothiazines, have been associated with phototoxic lysis of the corneal endothelium.11 Chlorpromazine, a phenothiazine, cause corneal epithelial keratopathy with a distinctive pattern of swirling lines or fine streaks in the epithelium.12 This does not, however, have any disastrous effect on the patient’s vision and can reverse after reduction or cessation of the drug.
Due to the fact that these drugs have anticholinergic properties, they can also cause:
- Blurred vision
- Decreased accommodation
- Mydriasis
- Dry eye
Pigment deposits can occur on areas of the bulbar conjunctiva that are exposed to UV radiation. In addition, typical antipsychotics can also cause lenticular opacities, and may also lead to other ocular side effects, such as oculogyric crisis, acute angle-closure glaucoma and pigmentary retinopathy.
Atypical antipsychotics have been linked to a higher risk of diabetes and, hence, can increase the risk for diabetic cataract.13
Migraine medication
Migraine represents a very complex and common neurological condition that affects one in seven people. It is reported that, in the UK, there are 190,000 migraine attacks every day, according to the Migraine Trust.14 In 2019, The International Classification of Headache Disorders classified migraine into the following six categories:
- Migraine without aura
- Migraine with aura. This may be further classified into:
- With typical aura (with/without headache)
- With brainstem aura
- Hemiplegic migraine
- Retinal migraine - Chronic migraine
- Complication of migraine
- Probable migraine with/without aura
- Episodic syndromes associated with migraine
Migraine can be associated with various ocular symptoms and abnormalities, such as visual aura, photophobia and glare. Previously, uncorrected refractive errors and binocular vision abnormalities were also associated with migraine; however, newer studies have found little evidence of such associations.16 More interesting is the association between normal tension/open-angle glaucoma and migraine, possibly due to the common vascular systemic risk factors for both type of pathologies.
The recommendations on drug treatment for acute migraine are based on the clinical guidelines, published by NICE as Headaches in over 12s: diagnosis and management.17 During migraine attacks, the usual treatments are ibuprofen, paracetamol and aspirin.18 Other drugs, such as triptan (oral, spray or injection), either used alone or in combination with the pre-mentioned analgesics, are also recommended.
It has been reported that ibuprofen can cause dry eye, blurred vision, refractive changes, diplopia and colour vision changes (figure 4), especially when taken in high dosages (up to 800mg).19 Interestingly, when administered to patients with primary open-angle glaucoma, paracetamol (1000mg taken orally every six hours) reduced the IOP and improved prognosis, possibly due to its indirect action on cannabinoid receptors.20  Figure 4: Dry eye, blurred vision, refractive changes, diplopia and colour vision changes have been reported with high dose use of ibuprofen
Figure 4: Dry eye, blurred vision, refractive changes, diplopia and colour vision changes have been reported with high dose use of ibuprofen
Topiramate, an antiepileptic drug, is also used to treat migraine. Acute angle-closure glaucoma attacks have also been reported in association with use of topiramate.21
Antiepileptic medication
Epilepsy represents a very common neurological disorder of genetic, infectious, metabolic, immune, or unknown aetiology, characterised by recurrent and sudden episodes of seizures due to abnormally excessive electrical brain activity.
Risk factors for epilepsy include:
- History of stroke
- Family history of epilepsy
- Head trauma
- CNS infection
At the moment, there are around 600,000 people with epilepsy in the UK (according to figures from Epilepsy Research UK22) and their care costs the NHS some £1.5 billion annually. Also according to Epilepsy UK, there are 21 epilepsy-related deaths every week.
In 2017, the International League Against Epilepsy (ILAE) classified epilepsy into four main types:23
- Focal
- Generalised
- Combined generalised and focal
- Unknown
During an epileptic seizure, patients usually display various symptoms due to auras experienced before the event, to jerking movements of part or entire body, diminished consciousness and convulsions. The visual system can also be affected by this disease, with manifestations including the following:24
- Visual hallucination (perception of something that is not there)
- Illusions (an altered perception of an existing object)
- Palinopsia (persistent appearance of visual images following removal of the stimulus, also known as visual perseveration)
- Visual field loss (depending on the brain side and area affected)
- Tropia
- Nystagmus
- Eyelid automatism (rhythmic blinking)
- Photosensitivity
- Myokymia (involuntary twitching or myoclonia of the eyelid and eyebrow)
Depending on the form, epilepsy is managed with a large variety of drugs. According to the Medicines and Healthcare products Regulatory Agency (MHRA), these drugs are classified into three categories,25,26 namely:
- Category 1; phenytoin, carbamazepine, phenobarbital, primidone.
- Category 2; valproate, lamotrigine, perampanel, rufinamide, clobazam, clonazepam, oxcarbazepine, eslicarbazepine, zonisamide, topiramate.
- Category 3; levetiracetam, lacosamide, tiagabine, gabapentin, pregabalin, ethosuximide, vigabatrin, brivaracetam.
Some of these drugs are also used sedatives, as previously mentioned. Depending on the dose and the duration of the treatment, many antiepileptics can have various side effects. Most of these are mild, but some can also be life-threatening, such as acute psychotic reactions and suicidal thoughts and behaviours.
The most commonly reported ocular side effects include the following:
- Colour vision defects
- Reduced visual acuity
- Reduced contrast sensitivity
- Visual field defects
- Diplopia
- Nystagmus
- Ocular gaze palsies
Vigabatrin, a category 3 drug prescribed for the treatment of partially epilepsy that is not satisfactorily controlled with other drugs, has also been linked to significant visual field constrictions. This complication can occur in as many as 30 to 40% of the patients treated with this drug. The field loss may be bilateral and heteronymous and sometimes needs to be distinguished from another cause of visual pathway damage (figure 5) such as an aneurysm of the internal carotid artery.
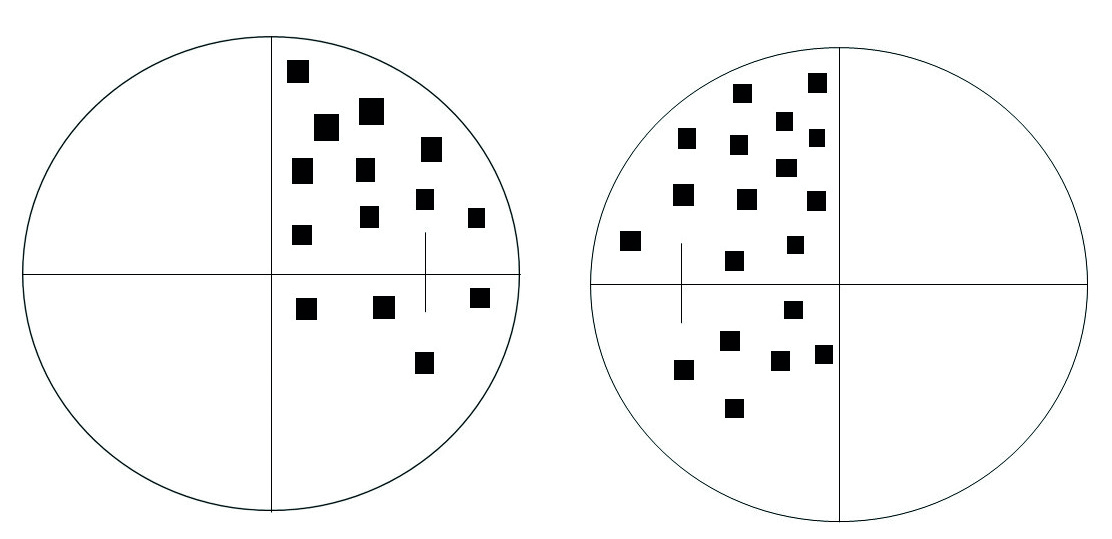
Figure 5: Binasal heteronymous loss due to vigabatrin use should be distinguished from other causes of chiasmal damage
The side effects of vigabatrin use are important to detect as it has been reported that they do not reverse after cessation of the drug. In 2008, the Royal College of Ophthalmologists issued guidelines for screening for visual field defects in patients treated with vigabatrin.27 The RCOphth recommended a baseline assessment of the visual field, followed by six-month follow-up for five years. If the patients do not show a defect, then the screening can be done annually. In addition, patients should also be instructed to report any abnormalities in their vision during the treatment with this drug.
Drugs for multiple sclerosis
Multiple sclerosis (MS) represents a progressive neurodegenerative disorder that, in time, leads to various motor and sensorial deficits manifest at the level of all organs and systems. It is also associated with depression and cognitive dysfunction. MS often first presents as episodes of optic neuritis (where, if retrobulbar, identification of a relative afferent pupil defect is important in primary care diagnosis), but may also present as a new-onset acquired pendular nystagmus or diplopia (due to internuclear ophthalmoplegia) or cranial neuropathy.28 Acute attacks of MS are often treated with corticosteroids as discussed in part two of this series (see Optician 24.04.2020). The most well know of these are:
- Cataract; usually posterior subcapsular
- Increased ocular pressure; this may lead to secondary
glaucoma
Amantadine, an antiviral drug used to treat influenzas, is also used to treat MS-related fatigue and walking difficulties. The mechanism behind the action of this drug in treating MS in uncertain. Use of amantadine has been associated with multiple ocular side effects, including corneal oedema and corneal endothelial dysfunction, and can occur from a few months to years after starting the treatment.29 There are also reports of other side effects, such as visual loss, mydriasis, punctuate subepithelial opacities and oculogyric crisis.30
Other drugs prescribed in MS and their possible ocular side effects are summarised in table 4.
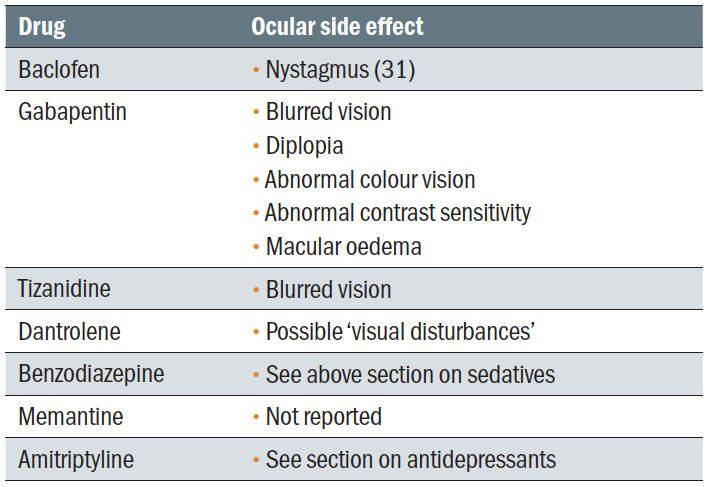 Table 4: Adverse effects of drugs for treating MS
Table 4: Adverse effects of drugs for treating MS
Drug treatments for Alzheimer's disease
Alzheimer’s disease (AD) is the most common form of dementia, the term dementia describing a group of disorders characterised by progressive cognitive decline. Beside its neurological effects, AD also affects the eye and visual system is a multitude of ways (see Optician 21.04.2017).
The main drugs used to treat AD are the acetylcholinesterase inhibitors donepezil, galantamine and rivastigmine (used as monotherapies) or memantine (used when patients are intolerant to the pre-mentioned drugs or suffer from severe AD.32 These drugs are used because it is suggested that cognitive impairment in AD is the result of cholinergic synaptic dysfunction in the hippocampus and neocortex.
Mostly, the adverse effects of these drugs are systemic, ranging from drowsiness to urinary retention, constipation and hallucinations. Blurred vision has also been reported after treatment with these drugs. Nevertheless, as these drugs improve the blood flow at the brain level, and many patients with normal-tension glaucoma have been found to exhibit abnormal cerebral blood flow similar to patients with AD, it could be hypothesised that these drugs may have a beneficial effect for glaucoma patients. In addition, they also lower the IOP, even with oral intake.33 Animal studies have also demonstrated that the drug galantamine protects retinal ganglion cell structure and function in a rat model of glaucoma.34 These effects need further investigation.
Antiparkinsonian drugs
Parkinson’s disease (PD) is a progressive neurodegenerative
disorder characterised by various symptoms that reflect deterioration of the motor system, such as rigidity, shaking, slow movements, and difficulty of walking, all of them classed under the name of parkinsonism. In addition, the visual system is also affected. Indeed, patients may report symptoms such as the
following:
- Photosensitivity
- Reduced visual acuity
- Reduced colour sensitivity
- Reduced contrast sensitivity
Other abnormalities, such as dry eye, blepharospasm, diplopia, convergence insufficiency, apraxia of eyelid opening and visual hallucinations have also been reported. Patients with PD have a characteristic ‘stare’ as their blinking is less frequent.35
The main drug used to treat PD is levodopa. This drug converts into dopamine at the brain level, hence helping with movement control. The use of this medication has been associated with various systemic side effects, some life threatening, such as sudden cardiac arrhythmias.36 Its use was also previously reported to be associated with visual hallucinations.37 Nevertheless, these sort of side effects are rare.
Another class of drugs used to treat PD are the monoamine oxidase B (MAO-B) inhibitors, previously mentioned as an antidepressant. MAO-B represents an enzyme that breaks down dopamine so its inhibition will increase the availability of this vital element. No ocular side effects have been reported after the use of these drugs.
Amantadine (see above) is also been prescribed occasionally in PD, to help with movement control. It is also used to control movement problems that occur as side effects of other antiparkinsonian medications.
A note about pupils
Many prescribed drugs may have some influence upon the autonomic supply to ocular structures, particularly the pupil. Furthermore, many such drugs are used in treating CNS disorders. Table 5 summarises the pupil impact of those most commonly prescribed.
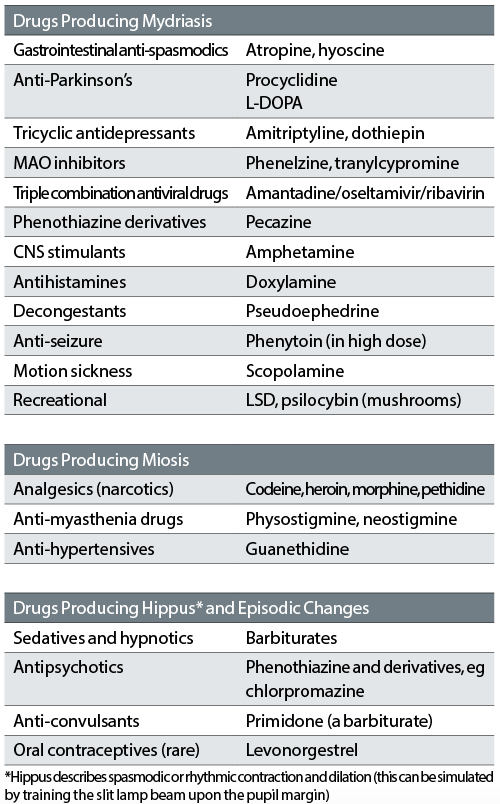 Table 5: Drugs with the potential to affect pupil size
Table 5: Drugs with the potential to affect pupil size
Dr Doina Gherghel is an academic ophthalmologist with a special interest in inter-professional learning for optometrists.
- The 4th article in this series will discuss the ocular side effects of antihistamines, anti-infectives, antimalarial, chemotherapy, interferon, vitamins and herbal supplements
References
- Richa S, Yazbek JC. Ocular adverse effects of common psychotropic agents. CNS Drugs. 2010;24(6):501-26
- Bittencourt PRM, Wade P, Smith AT, Richens A. Benzodiazepines impair smooth pursuit eye movements. Br J Clin Pharmacol. 1983;15:259-62.
- Rucker JC. Current treatment of nystagmus. Curr Treat Options Neurol. 2005;7(1):69-77
- Mateo J. Value of fundus autofluorescence imaging in a rare case of clonazepam associated retinopathy. Acta Ophthalmologica. 2012;90(s249
- https://www.mentalhealth.org.uk/statistics/mental-health-statistics-depression
- https://www.nhs.uk/conditions/antidepressants/
- Lieberman E, Stoudemire A. Use of tricyclic antidepressants in patients with glaucoma: assessment and appropriate precautions. Psychosomatics. 1987;28(3):145-8
- Richa S, Yazbek JC. Ocular adverse effects of common psychotropic agents. CNS Drugs. 2010;24(6):501-26.
- American Psychiatric Association DSM-5 Task Force. Diagnostic and statistical manual of mental disorders, 5th Edition (DSM-5). Washington, DC: American Psychiatric Association, 2013
- https://cks.nice.org.uk/psychosis-and-schizophrenia#!prescribingInfoSub
- Hansen TE, Casey DE, Hoffman WF. Neuroleptic intolerance. Schizophr Bull. 1997;23(4):567-82.
- https://www.reviewofoptometry.com/article/the-minds-eye-ocular-complications-of-psychotropic-medications
- Shahzad S, Suleman MI, Shahab H, et al. Cataract occurrence with antipsychotic drugs. Psychosomatics. 2002;43(5):354-9
- https://www.migrainetrust.org/
- https://ichd-3.org/1-migraine/
- https://onlinelibrary.wiley.com/doi/full/10.1111/j.1475-1313.2004.00212.x?sid=nlm%3Apubmed
- NICE (2012 (last updated November 2015) Headaches in over 12s: diagnosis and management. National Institute for Health and Care Excellence. www.nice.org.uk/
- https://cks.nice.org.uk/migraine#!scenario
- https://www.reviewofcontactlenses.com/article/which-oral-meds-cause-dry-eye
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3564461/
- Abtahi M, Abtahi S, Fazel F, et al. Topiramate and the vision: a systematic review. Clin Ophthalmol. 2012;6:117-131
- https://epilepsyresearch.org.uk/about-epilepsy/epilepsy-statistics/
- Scheffer IE, Berkovic S, Capovilla G, et al. ILAE classification of the epilepsies: position paper of the ILAE Commission for Classification and Terminology. Epilepsia 2017;58(4):512-521
- Bajwa R, Jay WM, Asconapé J. Neuro-ophthalmologic manifestations of epilepsy. Seminars in Ophthalmology2006;21:255-261
- MHRA (2017) Antiepileptic drugs: updated advice on switching between different manufacturers’ products. Medicines and Healthcare products Regulatory Agency. www.gov.uk;
- Joint Formulary Committee (2019) British National Formulary (online). BMJ Group and Pharmaceutical Press. bnf.nice.org.uk
- https://www.rcophth.ac.uk/wp-content/uploads/2015/01/2008-SCI-020-The-Ocular-Side-Effects-of-Vigabatrin-Sabril.pdf
- https://www.reviewofoptometry.com/article/ms-and-the-eye-part-2
- Deogaonkar M, Wilson K, Vitek J. Amantadine induced reversible corneal edema. J Clin Neurosci. 2011;18:298-299
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3096536/
- https://cks.nice.org.uk/multiple-sclerosis#!prescribingInfoSub:7
- https://www.nice.org.uk/guidance/ta217/chapter/1-Guidance
- Estermann S, Daepp GC, Cattapan-Ludewig K, Berkhoff M, Frueh BE, Goldblum D. Effect of oral donepezil on intraocular pressure in normotensive Alzheimer patients. J Ocul Pharmacol Ther. 22(1),62–67 (2006)
- Almasieh M, Zhou Y, Kelly ME, Casanova C, Di Polo A. Structural and functional neuroprotection in glaucoma role of galantamine-mediated activation of muscarinic acetylcholine receptors. Cell Death Dis. 1(2),e27 2010
- https://eyewiki.aao.org/Visual_symptoms_of_Parkinson%E2%80%99s_disease
- https://www.ncbi.nlm.nih.gov/books/NBK482140/
- https://www.ncbi.nlm.nih.gov/pubmed/2692012
