The optical, physical and mechanical properties of lens materials are important considerations in terms of the compatibility of the material to the chosen frame and the performance of the finished spectacles in terms of vision, comfort and cosmetic appearance.
In an ideal world, opticians and optometrists would provide every patient with a spectacle lens that is thin, light, impact and abrasion resistant, as well as maintaining the highest possible standard of vision. In practice, it is often necessary to compromise some aspect of lens performance because as one parameter improves others often fall short of the ideal. Careful consideration by the practitioner is needed to balance the spectacle prescription against the patient’s needs, so determining which lens property is most important to the patient.
Optical dispensing staff and manufacturers’ lens catalogues often focus on one key lens feature, usually the refractive index. However, all optical and mechanical properties must be considered if patients are to make an informed choice. Being able to scrutinise technical data is essential if the properties of one lens are to be accurately compared to another. For example, the authors have in the past been offered 1.6 index plastic lenses at a fraction of the price of the mainstream manufacturers. However, once a few pairs had been dispensed and a number of patients disappointed, the full technical information was obtained and the reasons for the price difference became apparent; namely, a much lower Abbe number and poor mechanical strength rendering it unsuitable for rimless frames.
Lens properties to be considered include:
- Refractive index (n)
- Abbe number (υ)
- Specific gravity
- Lens form
This article concentrates on lens material properties. Lens form will be considered in a future article.
Refractive index (n)
The refractive index is the ratio of the velocity of monochromatic light for a specified wavelength (λ) in a vacuum to the velocity of light in the considered lens material.1 For technical applications such as ophthalmic lenses, it is measured in air (relative refractive index).
Monochromatic light is specified, as values for n vary according to wavelength.
Reference wavelengths used for the determination of refractive index are as follows:2
- mercury e-line λe = 546.07 nanometres (nm)
- helium-d line λd = 587.56nm
It is important to note which wavelength has been used when comparing lenses from different manufacturers as, when ne rather than nd is used, the refractive index will have a slightly higher value.
These lines are used out of convention because they are close to the middle of the visible spectrum, and because accurate sources of monochromatic light of the required wavelength are readily available to the scientific laboratories that assess lens materials and have since become enshrined in international standards. Historically, different countries have preferred one or other method; for example, the United Kingdom used nd and Germany ne. The globalisation of lens manufacture now means the boundaries have been blurred, and in real terms it makes very little difference. For example, for CR39, nd = 1.498 and ne = 1.501, both of which round to 1.50 at two decimal places. Nevertheless, it has not been unknown for unwitting or deceitful sales representatives to claim a slight superiority over a competitor product when no such advantage exists.
The velocity of light in a vacuum is approximately 186,000 miles or 300,000 kilometres per second. Its velocity through differing lens materials varies as some materials offer more resistance than others, the higher the refractive index the greater its resistance or slower its speed. The velocity of light in air is generally taken to be 2.98x108ms-1.
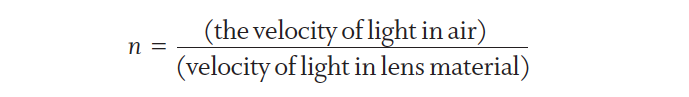
The higher the refractive index the flatter and usually thinner the lens will be, and the classification of refractive index is clearly described within BS 7394-2:2007 from normal to very high index (table 1).3 At all times, using correct terminology with patients is essential to avoid any misrepresentation of facts and for ensuring informed choice and valid consent is obtained. Non-registered dispensing staff can often be overheard using the term ‘high index’ for any refractive index above 1.5 and superlatives like ‘extra-’, ‘super-’ and ‘ultra-thin’ are only helpful if they are applied consistently by manufacturers and retailers alike. 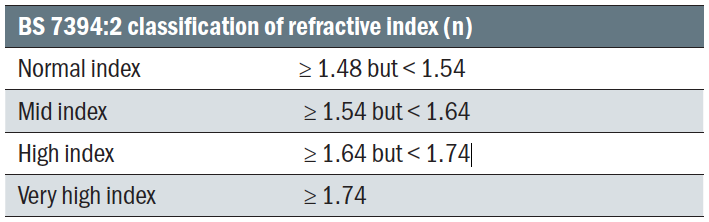 Table 1: BS 7394:2 classification of refractive index (n)
Table 1: BS 7394:2 classification of refractive index (n)
Transparency and clarity when making direct lens product comparisons is key to maintaining patient confidence and trust. Properties of lenses of differing refractive indices can be seen in table 2. 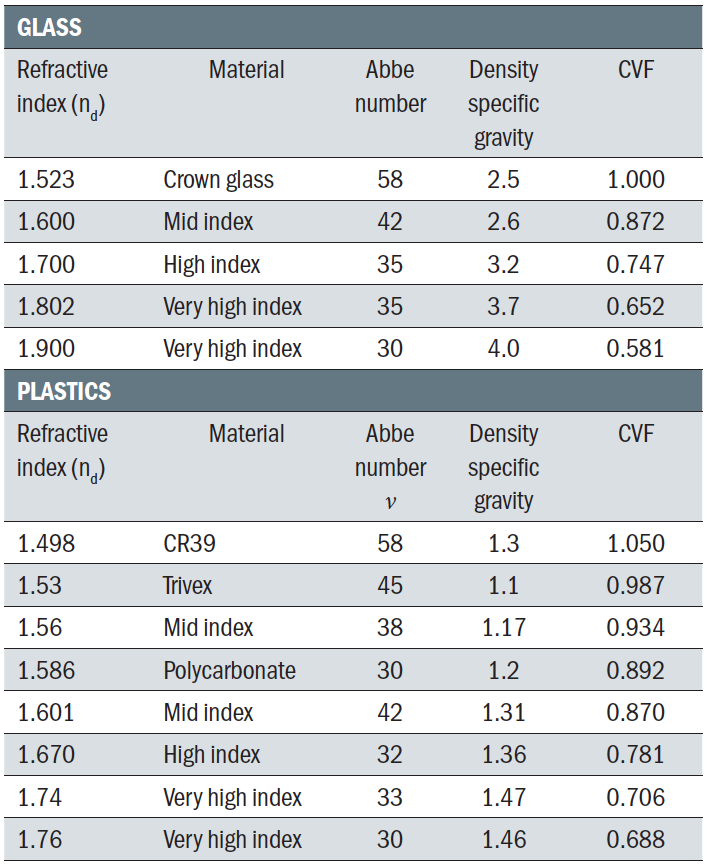 Table 2: Properties of lenses of differing refractive indices
Table 2: Properties of lenses of differing refractive indices
Lens thickness and sags
With minus power prescriptions when assuming equal centre thickness, an increase in refractive index always produces a thinner lens, even when using stock lenses of similar form. However, it is by no means assured that two lens materials of the same index will have similar centre substance. For example, glass lenses are more rigid, and it may be that a plastic lens of the same refractive index requires a thicker centre substance in order to have sufficient mechanical strength to avoid it buckling under the tension imposed during glazing the lens to a frame.
With plus lenses, differing minimum edge thicknesses can mean that any anticipated saving due to increased refractive index is not as great as expected, especially if the lower index lens was aspheric and the new higher index lens is not. Patients are most frequently disappointed when they are dispensed higher refractive index lenses from stock (with the promise that higher index means thinner, lighter lenses) when they have previously had a lower index lens surfaced to minimum size uncut (MSU). This is particularly apparent when small frame sizes are used, as with small children, and the practice uses stock lenses to save on costs.
The thickness of lenses can easily be calculated using sags. Most practitioners will have been taught the approximate sag formula: 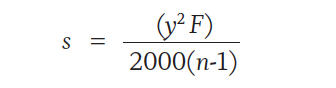
This was certainly useful as an easy and more convenient calculation in the days before scientific calculators and computers. In an age when most people have a smart phone and can calculate a square root with ease, it is probably easier to use the accurate formula, which can also be easily derived from the diagram shown (figure 1).
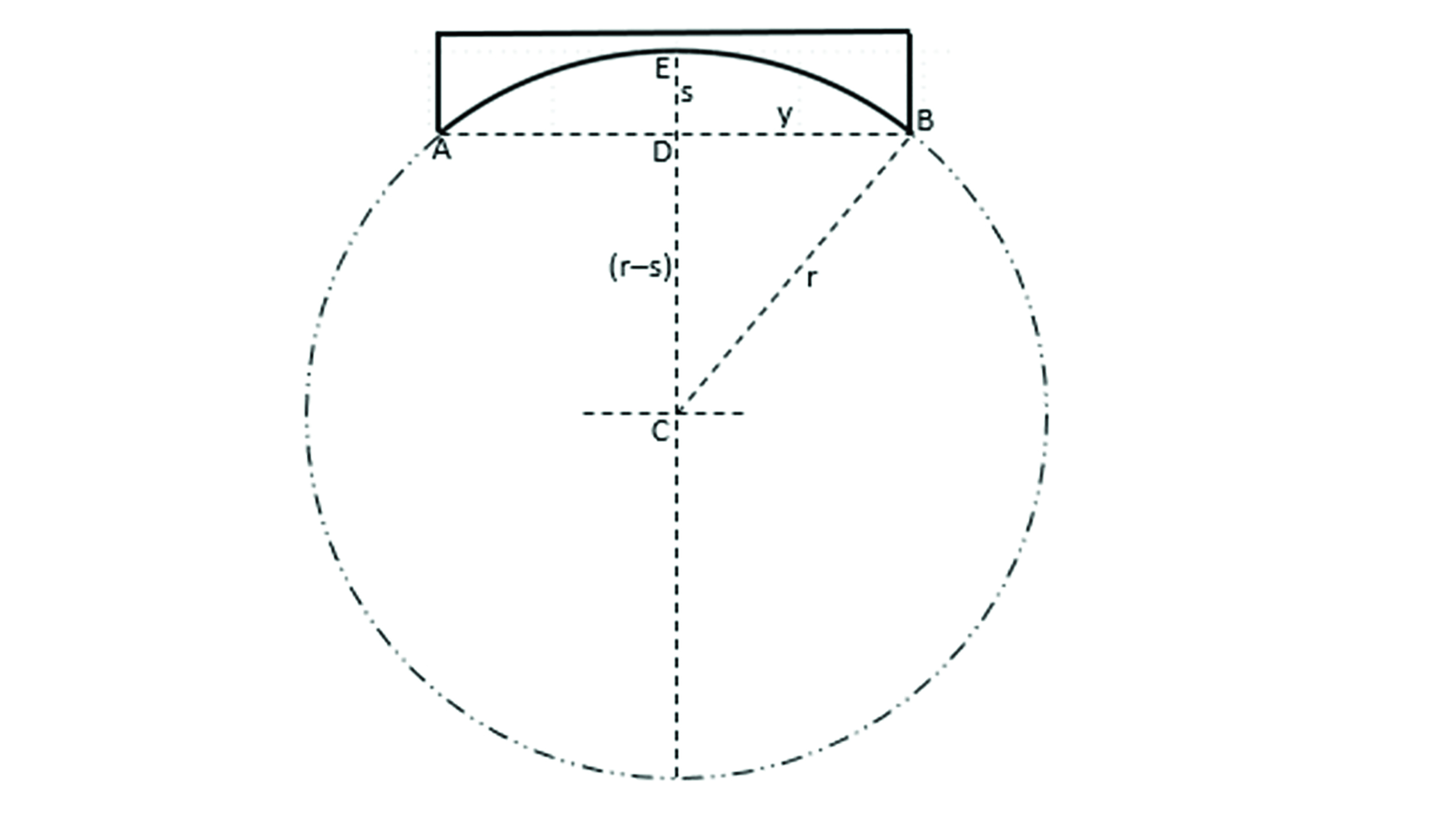
Figure 1: A negative lens surface of diameter AB
From figure 1, it can be seen that AB = 2y and radius of curvature BC = r. The sagitta, or sag, s, is the distance from the chord AB to the apex of the lens surface, marked by the distance ED. EC is also the radius of curvature, r, so DC is equal to (r – s).
Using Pythagoras’ theorem:
(r – s)2 = r2 – y2
Then, taking the square root of each side of the equation:
r – s = √(r2 – y2)
Which can easily be rearranged to:
s = r – √(r2 – y2 )
Returning to the problem of a stock mid-index lens working out thicker and heavier than a standard lens material that has been surfaced to MSU, consider the following example of a plano-convex lens with a +6.00DS front surface made from either CR39 (n=1.498, diameter 52mm uncut) or polycarbonate (n=1.586, 65mm diameter).
For the CR39 lens:

For the polycarbonate lens:

It can thus be seen that a stock mid-index lens has a thicker centre substance than a surfaced CR39 lens. However, the actual thickness as perceived by the wearer is even worse once a stock lens has been edged down to fit the frame.
Now consider substituting the calculated centre thickness and using a new semi-diameter value.

Substituting the calculated centre thickness and with a new semi-diameter, y = 26mm, the edge thickness of the cut lens can easily be calculated;
 It is common to see children whose lenses have been cut from stock lenses rather than surfaced to their requirements (despite their being an NHS supplement available for this). Sometimes this happens despite an increase in refractive index and where parents have been promised lenses that are thinner, flatter and lighter; only to be disappointed. This example demonstrates how, if the patient has previously had surfaced CR39 lenses, stock polycarbonate lenses may be of no real benefit. Indeed, the patient has potentially been mis-sold as the apparent thickness that the patient perceives, namely the edge thickness, has more than doubled.
It is common to see children whose lenses have been cut from stock lenses rather than surfaced to their requirements (despite their being an NHS supplement available for this). Sometimes this happens despite an increase in refractive index and where parents have been promised lenses that are thinner, flatter and lighter; only to be disappointed. This example demonstrates how, if the patient has previously had surfaced CR39 lenses, stock polycarbonate lenses may be of no real benefit. Indeed, the patient has potentially been mis-sold as the apparent thickness that the patient perceives, namely the edge thickness, has more than doubled.
Curve variation factor (CVF)
Currently, with the availability of software able to calculate lens thicknesses, the curve variation factor is often overlooked. The CVF demonstrates the variation in surface power of a lens material when compared to crown glass, so providing an indication of the change in thickness. It can also be used in tool power calculation. For glass lenses:
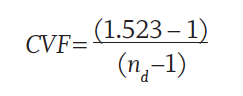
If we compare two lenses of the same power:
CVF for crown glass = 1
CVF for 1.802 glass = 0.652
So, the 1.802 glass would offer a 35% reduction in thickness
There are many reasons for altering lens material and selecting a higher refractive index. The General Optical Council (GOC) standards 1.2, 2.1 and 5.3 clearly set out registrants’ responsibilities regarding effective communication, informed consent and keeping knowledge and skills up to date.4 Patients are often very well informed these days as the internet offers an easy way to access information. So, more than ever, the knowledge and product awareness of the optometrist and dispensing optician is essential.
Of course, refractive index is not the only consideration. Impact resistance and safety may also be of interest, and so too should the dispersive power of the lens.
Abbe Number
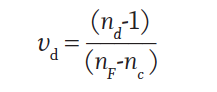
The Abbe number, denoted by the lower case Greek letter nu (υ), is often referred to as the V-value or constringence. However, these terms are now superseded by the term Abbe number.
Abbe number expresses the chromatic dispersion of a lens and according to BS EN ISO 13666:20191 is calculated as follows:
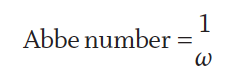
Abbe number is the reciprocal of the dispersive power (ω), therefore:
British standards BS 7394-2:20073 once again clearly sets out the correct terminology for classification by Abbe number as shown in table 3.  Table 3: Classification by Abbe number
Table 3: Classification by Abbe number
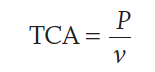
Chromatic aberration is inversely proportional to the Abbe number, so the greater the Abbe number the less the chromatic aberration. Transverse chromatic aberration (TCA) is more important for spectacle lens design and is expressed in prism dioptres (∆). Longitudinal chromatic aberration will be covered in aberrations of spectacle lenses in a subsequent article.
 F is the dioptric power of the lens and c is the distance in centimetres (cm) from the optical centre. The threshold of TCA <0.1Δ is accepted as unlikely to be detected by the human eye.
F is the dioptric power of the lens and c is the distance in centimetres (cm) from the optical centre. The threshold of TCA <0.1Δ is accepted as unlikely to be detected by the human eye.
If we take a prescription of R +4.50DS L +4.50DS made in CR39 (nd = 1.498), and Abbe number of 58 at 10mm (1cm) below the optical centre:

Now, consider the same lens made in polycarbonate (nd= 1.586, Abbe number 30):
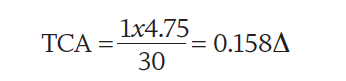
Here we can see that the TCA for polycarbonate is >0.1Δ meaning that, depending on illumination, the patient is likely to notice colour fringes (around high contrast objects) or off axis blurring (low contrast objects).5 If the first time these aberrational effects are mentioned is at the point when the patient returns to complain, then confidence will have already been lost.
Meslin and Obrecht6 use a graph (figure 2) to show the relative visual acuity as a function of the prismatic effect for nine different lens materials of differing Abbe numbers, varying from 20 to 60. It can be seen that chromatic aberration has a marked impact on visual acuity. Because there is no chromatic aberration when looking through the optical centre of any lens, the relative visual acuity is 1 when the prismatic effect is 0. At any point away from the optical centre the prismatic effect can be calculated using Prentice’s Rule:
P=cF
where P is the prismatic effect (in prism dioptres Δ), c is the distance from the optical centre (in cm) and F is the focal power of the lens (in dioptres, D).
 Figure 2: The relative visual acuity compared to prismatic effect for 9 lens materials with Abbe values from 20 to 60.
Figure 2: The relative visual acuity compared to prismatic effect for 9 lens materials with Abbe values from 20 to 60.
Interestingly, many further studies point to the importance of TCA being underestimated.7,8 Calculating TCA is not difficult and should be considered appropriately.
Chromatic aberration causes colour fringing around high contrast objects but also causes a degradation of vision in low contrast environments that patients may struggle to articulate. Patients whose spectacles ‘just don’t feel right’ may well be noticing reduced visual acuity caused by a lower Abbe number in their new spectacles than in their old ones. Practical experience would suggest that few patients complain of issues relating to colour fringing or chromatic aberration when the Abbe number is of a value relating to low or medium dispersion. However, high dispersion lens materials can cause issues even in low powers. This is especially so with progressive lenses, where the patient has no choice but to use a part of the lens significantly distant from the distance optical centre when reading.
Many patients, particularly high myopes, are prepared to sacrifice optical performance for the improved cosmetic appearance and comfort that thinner, lighter lenses with a high or very high refractive index allow. However, before gaining consent from a patient to dispense lenses with a low Abbe number (high dispersion), it is important to spell out the advantages and disadvantages.
It is particularly important to explain the downside of high dispersion lenses. If the patient is unclear about any compromise, they may not have chosen them. For example, patients with high prescriptions are usually made aware that thinner lenses come with adaptation requirements and may be warned to look directly at objects to maximise their visual acuity. Brooks and Borish9 set out important dispensing factors when using lenses with high dispersion, as follows:
- Always use monocular pupillary distances
- Take into account the pantoscopic angle
- Keep back vertex distance to a minimum
- For high lens powers, avoid pantoscopic angles >10 degrees
- Consider the position of the optical centres in relation to horizontal centre line and edge thickness differences
However, there is an increasing trend to supply lenses with the lowest available Abbe number without properly informing the patient (or those with legal responsibility for the patient) of the potential downsides. Polycarbonate lenses (ν=30) are often offered to as standard for children and for all patients selecting rimless mounts, regardless of prescription, on the grounds of increased impact resistance and safety. However, just as often there is no mention of decreased optical performance. Under such circumstances, the patient is not being offered enough information to make an informed choice and give informed consent as required under GOC standards 3.1.4,4 and so the dispense is unlikely to be valid and would not be supported were there later to be any complaint made.
Winter et al7 found that the peripheral retina is more sensitive to TCA than foveal vision. These effects, combined with the spectacle lens induced TCA of higher dispersive lenses, could lower peripheral acuity. This underlines the importance of evaluation of lens properties, particularly for visually impaired patients with maculopathy who rely on eccentric viewing techniques, or patients with nystagmus depending upon a null point to maximise their functional vision.
Chromatic aberration of less than 0.1Δ cannot be detected, and greater amounts can be tolerated by most patients. Wilson and Daras (citing Torgersen)10 state that 0.16Δ is the level below which problems are unlikely to occur. So:

where F is the dioptric power of the lens and c is the distance in centimetres (cm) from the optical centre.
From, P=cF (Prentice’s Rule), we can say:
By re-arranging this, the maximum amount of prism that can be experienced for a given lens material can be calculated and then, using P=cF, the off-axis distance the patient can view without encountering problems.
For example, where P = 0.16 ν, the amount of prism tolerated in a lens, where ν=30) is 4.8Δ and where ν=58, it is 9.28Δ. Put another way, on a +2.50D lens where the near vision point is 20mm below the distance optical centre, an Abbe number of 30 would cause noticeable TCA that would not be a concern with most other lens materials. So remember, a low Abbe value is not just an issue for high powered prescriptions.
Reflectance
A proportion of light incident upon a surface of a lens will be reflected, meaning that <100% will enter the lens material. For light incident normally at the lens surface, the amount of reflected light is the reflection factor (ρ) and expressed as a percentage:
 From this equation, it can easily be seen that as n increases, so does ρ.
From this equation, it can easily be seen that as n increases, so does ρ.
So, a glass lens of refractive index n = 1.9 will lose nearly 10% of light to reflection from each surface and for this reason anti-reflection coatings are essential on high and very high refractive index lenses. This is why they are usually supplied as standard.
BS 7394-2-20073 states that, for lenses to classified as anti-reflective, the reflectance has to be <2.5%, and to be classified as multi or broadband anti-reflective coated, reflectance has to be <1.5%.
Abrasion resistance
It is difficult to obtain robust technical data on the scratch resistance of alternative lens materials. Glass lenses are roughly 10 times more scratch resistant than plastic materials. However, coating usually reduces the scratch resistance of glass and improves the scratch resistance of plastic.
Impact resistance
The robustness of lenses in terms of their resistance to breakage will be covered in a future article on protective eyewear. However, patients considering glass lenses must be told of the risk they are subjecting themselves to so that they can consider the implications. Highly myopic patients will often be very happy with 1.8 or 1.9 glass lenses for general use, but purchase separate spectacles for high risk activities such as sport, DIY or occupational use.
It is important to be realistic when discussing safety; life is never without risk. However, there are downsides to materials like polycarbonate, as already discussed, that may negate any safety benefit, especially when the lenses are to be glazed to a frame that does not conform to any recognised safety standards itself.
In the author’s experience, young children are very unlikely to be involved in high risk activities that make polycarbonate a better alternative to CR39. That said, there is evidence that reducing visual acuity unnecessarily is counterproductive to the treatment of amblyopia.
Asking thousands of eye care professionals at CET events, the author and colleagues have found only one who has come across a child who has broken a lens while the spectacles were in situ. A Google search reveals just two such cases, though sadly one resulting in the enucleation of the left eye, over the past decade in the UK. The teenage boy who lost his left eye should have been wearing sports goggles (or contact lenses) for football, and the other child had been subject to a vicious assault which an optician could not reasonably foresee. The use of low Abbe number lenses as standard, especially for patients whose visual system is not yet fully developed, is a topic worthy of further debate and clinical research.
Density
The wearing comfort of a pair of spectacles is, assuming the frame fits well, largely determined by their weight. The evolution from glass to plastic lenses has meant lenses are typically much lighter in weight than they used to be. To make accurate comparisons for your patient between, say, their existing high index glass lenses and a high index or very high index plastic alternative, it is necessary to know the density or specific gravity.
Density (ρ) is a measure of how heavy a substance is in a given volume and derived as follows;
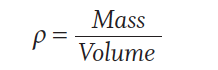
Relative density or specific gravity is the ratio of the density of a material to the density of a reference substance at a specified temperature and pressure. The reference substance used is water at 4°C and 760 torr (or mmHg).11,12 As 1cm3 of water weighs 1 gram (g), a specified volume of crown glass with a specific gravity of 2.5 is 2.5 times heavier than water. While this provides another tool for comparison of lens materials, it needs to be remembered that, due to the higher refractive index of some materials, surface curves will be flatter and so have less overall volume/mass. So, for direct comparison more information will be needed.
Different lens materials can also be surfaced to differing minimum centre/edge substances, and so this also needs to be taken into account. Nevertheless, assuming a similar centre substance, the weight of lenses of the same refractive index can be compared accurately. It can therefore be seen from table 2 that 1.6 glass is almost exactly twice the weight of 1.6 plastic, which is itself nearly 10% heavier than polycarbonate.
Conclusion
It is the role of the dispensing optician or optometrist (and the optical dispensing assistants under their clinical supervision) to ensure that all patients are offered all the information appropriate to make an informed choice and to ensure that the offered consent is valid for the supply of their ophthalmic lenses. Even the simplest of prescriptions can present a complex challenge for decision-making process once the frame, patient lifestyle and various complicating factors, such as the treatment of amblyopia and the need to maximise visual acuity, are brought into play.
Physical as well as optical properties need to be taken into account. A lens material will require a certain thickness to withstand being fitted to a frame without warping, and this combined with the curve variation factor needs to be taken into account when comparing the overall thickness of different lens materials. Often the greatest impact upon lens thickness and weight is achieved by minimising decentration, and therefore uncut lens size, rather than increasing refractive index. However, both options can produce stunning results, especially noticed if a patient has been dispensed poorly in the past.
This article has demonstrated that a high index lens may actually be thicker than a lower refractive index if a large diameter lens is used or required. It is not sufficient for dispensing staff to simply trot out average percentage savings when ‘upgrading’ patients without first establishing and explaining any factors that might counteract these savings, such as a larger frame and increased decentration.
Practitioners are encouraged to determine accurately the lens thickness and weight using one of the many computer programmes available for this, rather than using estimates that are often inaccurate, so that patients are as fully informed as possible.
Finally, practitioners must consider the wellbeing of their patients when helping them to make a decision on lens material. The recent move to provide certain categories of patient with polycarbonate lenses as standard, notionally on grounds of impact resistance, needs to be balanced against the downside of reduced optical quality and poor durability due to inferior scratch resistance or resistance to chemical attack. This is particularly the case for lenses to be glazed into rimless mounts.
It has been shown that the difference in off-axis decimal Snellen visual acuity between a lens with an Abbe value of around 30 (such as one made from polycarbonate, or a typical 1.67 plastic) is around 0.1 lower (approximately one line of acuity) than an alternative product (such as Trivex or a high quality 1.6 lens). The difference in optical quality, and corresponding loss of off-axis visual acuity between high dispersion lenses and low dispersion lenses (such as CR39) is even more pronounced. This should encourage a practitioner to evaluate the risks and benefits of alternative lens materials and explain the compromises that may accompany the benefits of the lenses they are recommending. Only then can they be confident of ensuring the patient is able to make an informed choice and valid consent given. •
Tina Arbon Black BSc (Hons) FBDO CL is director of accredited CET provider Orbita Black Limited, an ABDO practical examiner, practice assessor and exam script marker, and a distance learning tutor for ABDO College.
References
- British Standards Institution BS EN ISO 13666:2019 (TC): Ophthalmic optics – Spectacle lenses – Vocabulary. London: BSI; 2019.
- British Standards Institution (1998) BS EN ISO 7944:1998: Optics and optical instruments-Reference wavelengths. London: BSI; 1998.
- British Standards Institution BS 7394-2:2007 Complete spectacles part 2: Specification for prescription spectacles. London BSI; 2007
- The General Optical Council (2016) Standards of Practice for Optometrists and dispensing Opticians. Available at: https://standards.optical.org/the-standards/optometrists-and-dispensing-opticians/ Accessed 28th May 2020.
- Jalie M (2019) Modern spectacle Lens Design, Clinical and Expermental Optometry, 103(1) pp 1-2 Available at: https://www.optometry.org.au/wp-content/uploads/Publications/CXO/Issues/cxo_v103_i1_Jan.pdf#page=5 Accessed 28th May 2020
- Meslin D and Obrecht G (1988) Effect of Chromatic dispersion of a lens on Visual Acuity. American Journal of Optometry & Physiological Optics 65(1) pp. 25-28 Available at: http://www.essiloracademy.eu/sites/default/files/American%20Journal%20of%20Optometry.pdf Accessed 1st June 2020
- Winter S, Fathi M, Venkataraman A, Rosen R, Seidemann A, Esser G, Lundstrom L, and Unsbo P (2015) Effect of induced transverse chromatic aberration on peripheral vsion. Journal of the Optical Society of America, 32(10). Available at: https://www.osapublishing.org/DirectPDFAccess/641260E2-90BE-006B-513B8ED3DC81C784_326495/josaa-32-10-1764.pdf?da=1&id=326495&seq=0&mobile=no Accessed 1st June 2020
- Tang C and Charman W (1992) Effects of monochromatic and chromatic oblique aberrations on visual performance during spectacle wear. Ophthalmic and Physioloical Optics 12(3) Available at: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1475-1313.1992.tb00407.x Accessed 1st June 2020
- Brooks C and Borish I (2007) System for Ophthalmic Dispensing 3rd Edn. America: Butterworth Heinemann p. 407
- Wilson D and Daras S (2014) Practical Optical Dispensing 3rd Edn. Australia: The Open Training and Education Network. p.66
- Wilson D and Daras S (2014) Practical Optical Dispensing 3rd Edn. Australia: The Open Training and Education Network. p.63
- Jalie M (2016) The Principles of Ophthalmic Lenses 5th Edn. London: Association of British Dispensing Opticiand. P.92-93
