While soft toric contact lens fitting had been regarded as a ‘speciality’ until recently, the number of lens designs available has increased and the fitting approach simplified. This is reflected by a continuous increase in toric lens prescribing over a 15-year period observed in an international survey of toric lens prescribing.1 In a 2019 UK contact lens prescribing survey detailing over 1,000 fits, a considerable proportion of new fits and refits were soft toric lenses (31% and 28% respectively).2 Overall, a continued trend of decline in the proportion of soft spherical-only fits was observed due to the increasing popularity of both toric and multifocal designs. Similarly, the popularity of RGP torics is dwindling as practitioners increasingly favour soft lens designs.2
The increasing popularity of soft toric lenses has been fuelled by the release of innovative lens designs, available in a variety of lens materials and with an increasingly wider parameter range, greater even than that for daily disposable lenses. The availability of comprehensive fitting banks now makes trialling astigmatic patients with toric disposable diagnostic lenses as convenient as spherical lens fitting. One of the reasons for this increase in the simplicity of fitting toric lenses has been an advance in manufacturing technology. The advent of new low-cost moulding technology and wet moulding techniques, allowing the lens to remain hydrated throughout manufacture, has led to improvements in contact lens reproducibility and optical quality. This should give practitioners greater confidence that the lenses being dispensed will fit successfully.
Correction of astigmatism
The incidence of astigmatism in the general population is shown in table 1.3 The percentage of prospective lens wearers with ≥0.75DC in at least one eye, and who could be fitted with toric contact lenses, has been estimated at 45.4%4 and, in a more recent study, at 47.4%.5 While the prevalence of with-the-rule and against-the-rule astigmatism has been found to be similar by this later study (≥0.75DC; 15.3% and 14.5% respectively), astigmatism in myopes was found at almost twice the prevalence of that observed in hyperopes (≥0.75DC; 31.7% and 15.7% respectively). It was estimated that 90% of the patients considered in the study could be fitted with a toric lens power range from +6.00DS to -9.00DS, three cylinder powers, and 18 axis values. A separate study suggested that up to 96.4% of 101,973 patient prescriptions analysed could be fitted with the soft toric contact lens power ranges of frequent replacement lenses that are currently available.6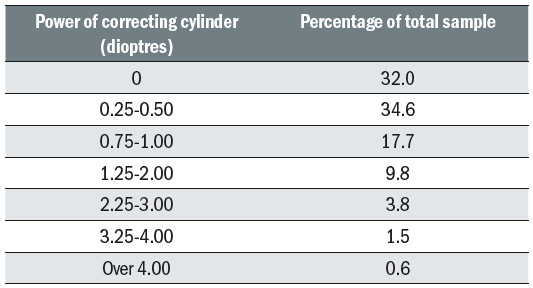 Table 1: Incidence of astigmatism, from Bennett3
Table 1: Incidence of astigmatism, from Bennett3
Despite the increase in soft toric lens prescribing, the level still falls below the prevalence of astigmatism identified in prospective lens wearers. Studies have indicated that patients are often unaware they have astigmatism, were unaware there were lenses for astigmatism or were not offered toric lenses by their practitioner.7,8 Therefore, practitioners should be proactive in these discussions. Practitioners often underestimate the effect on visual performance, of even low levels of astigmatism. A wealth of studies have indicated that visual acuity is significantly improved with toric contact lenses when compared to spherical lenses.8-12 Similar improvements have been observed for low contrast visual acuity,11,12 contrast sensitivity13 and subjective vision.8,11,14 Research data suggests that correcting even low to moderate astigmatism (-0.75DC to -1.75DC) may be important for safety when driving.15 More recently, a study found that correction of astigmatism with toric lenses (-0.75DC to -1.50DC) resulted in significantly improved night driving performance when compared to correction with spherical contact lenses.13
Practitioner concerns about increased chair time should be dispelled; the time taken to fit successfully either toric or spherical lenses during a crossover study was not significantly different (mean fitting time 10.2 and 9.0 minutes, respectively).14 In a clinical evaluation of 200 astigmatic patients, who had not previously worn toric lenses, 88% were successfully fitted at the first attempt with the average fitting appointment taking 22 minutes.8 Patients were fitted with either daily disposable or two-weekly disposable lenses and achieved an overall success rate of 75% following a wearing period of one month. High levels of satisfaction with comfort and vision were also reported (85% and 93% respectively). Similarly, high levels of general satisfaction (96%) have been reported in a recent post-market evaluation study of over 1,200 patients fitted with daily disposable toric lenses.16 
The increased cost of toric lenses compared to spherical lenses may be off-putting to patients. When used on a full time basis, it was reported the annual cost in the UK of monthly disposable toric lenses was 11% greater than a spherical correction.17 Therefore, it is important to demonstrate effectively the benefits of toric correction, not only to neophytes but to existing spherical lens wearers with suitable levels of astigmatism. While this can be easily demonstrated using a trial frame during the consultation, the real-world benefit (such as improved contrast levels and driving performance in both photopic and scotopic conditions) is most effectively demonstrated by dispensing toric lenses for a trial period. While uptake is likely to be dictated by the visual demands and wearing frequency of the individual, this at least allows patients to make an informed choice as to whether toric lens correction is appropriate for them.
Soft Toric Contact Lens Design
While the tear lens formed by a spherical RGP will correct corneal toricity without the need for a toric lens, this is not possible with soft lenses which simply drape over the cornea. Even thick soft lenses or high modulus materials cannot effectively mask corneal astigmatism.18-20 Furthermore, the use of aspheric contact lenses to reduce spherical aberrations do not improve visual acuity for an astigmat as effectively as toric lenses.21
For successful correction of astigmatism, a toric lens needs to maintain the position of the correcting cylinder at the desired axis and the lens needs to maintain rotational stability during and after a blink, as well as during a change in direction of gaze. Manufacturers use a number of methods to achieve this; prism ballast, peri-ballast and thin zone designs (known as double slab-off, dynamic stabilisation and the trademarked Eyelid Stabilised Design).22 The following sections will review each of these designs in turn.
Prism-ballast
This lens design relies on vertical prism to orientate and stabilise the lens. In principle, the lens is produced with an increasingly thicker profile towards its base (figure 1a). The thinner portion of the lens locates under the upper eyelid, which then squeezes the thicker portion of the lens towards the lower lid. This has been described as the ‘watermelon seed’ principle. With more recent lens designs, a thinner inferior lens periphery, or comfort chamfer, is used to reduce the thickness differential and improve oxygen performance.23
Peri-ballast
Although similar to the prism-ballast design, this design utilises eccentric lenticulation and a thinned superior lens edge to produce a prism-like rotational stabilisation effect.24 This modification means that prism is restricted more to the lens periphery, so allowing for a potentially prism-free optic (figure 1b). 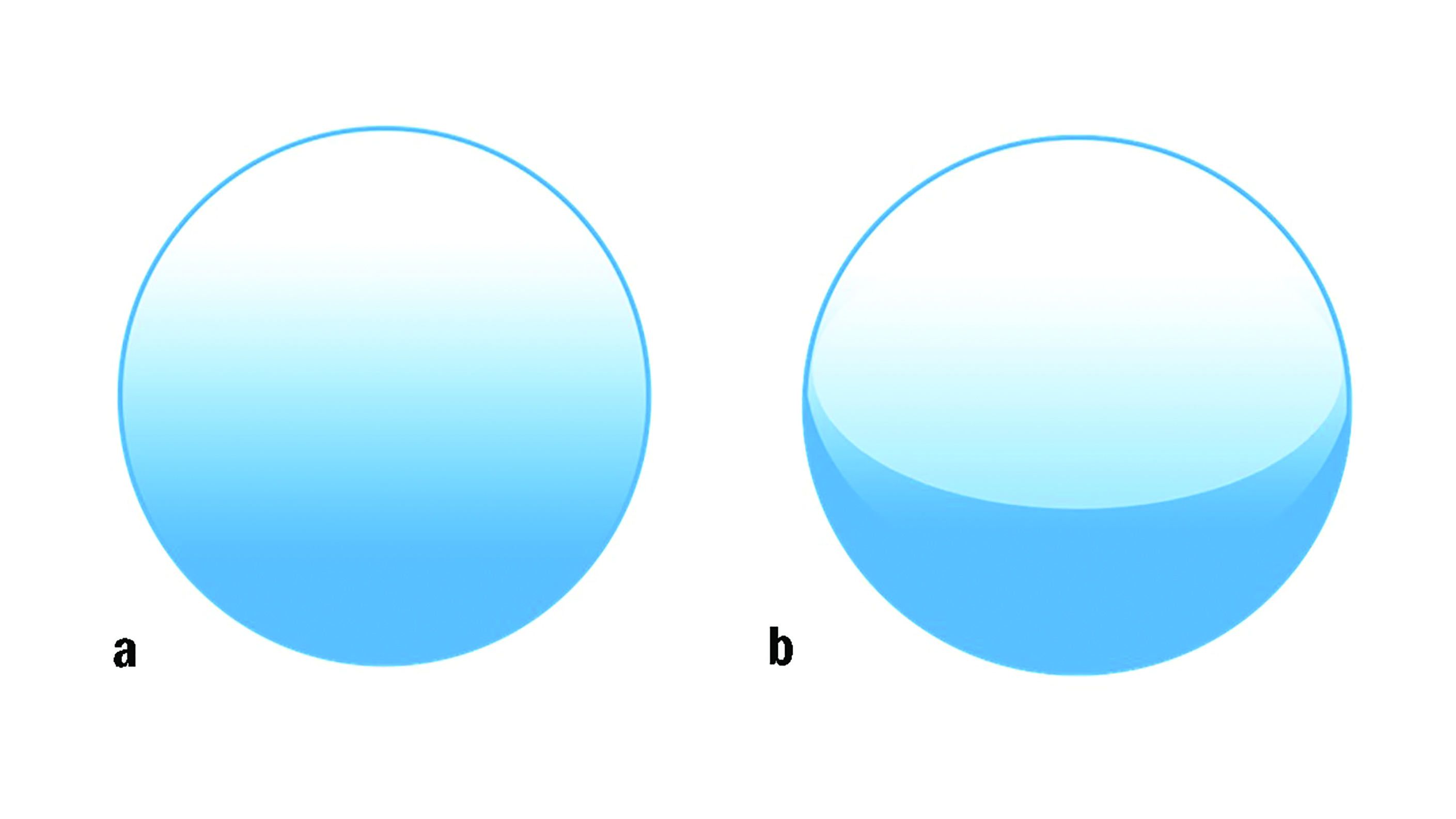 Figure 1: Thickness profiles of a prism ballast (a) and peri-ballast (b) toric soft contact lens, where darker colour indicates great thickness
Figure 1: Thickness profiles of a prism ballast (a) and peri-ballast (b) toric soft contact lens, where darker colour indicates great thickness
Thin zone designs
These designs also rely on the interaction between lids and the lens to achieve stabilisation. Both eyelids play an active role, unlike prism-ballast designs that involve interaction primarily from the upper lid. The design utilises thin zones; the lids squeeze against the thickness differential across the lens aligning the thicker central portion within the palpebral aperture and the thinner zones under the eyelids (figure 2a). Refinement of this stabilisation approach has led to designs that isolate the optical correction within an optic zone resulting in independent stabilisation areas.25 This allows orientation consistency across all powers and a thin overall thickness profile25 (figure 2b). More recently, eyelid stabilised designs have sought to maximise effectiveness by locating thicker ‘stabilisation zones’ within the palpebral apertures while minimising any thickness variation of the lens under the eyelids (figure 2c).
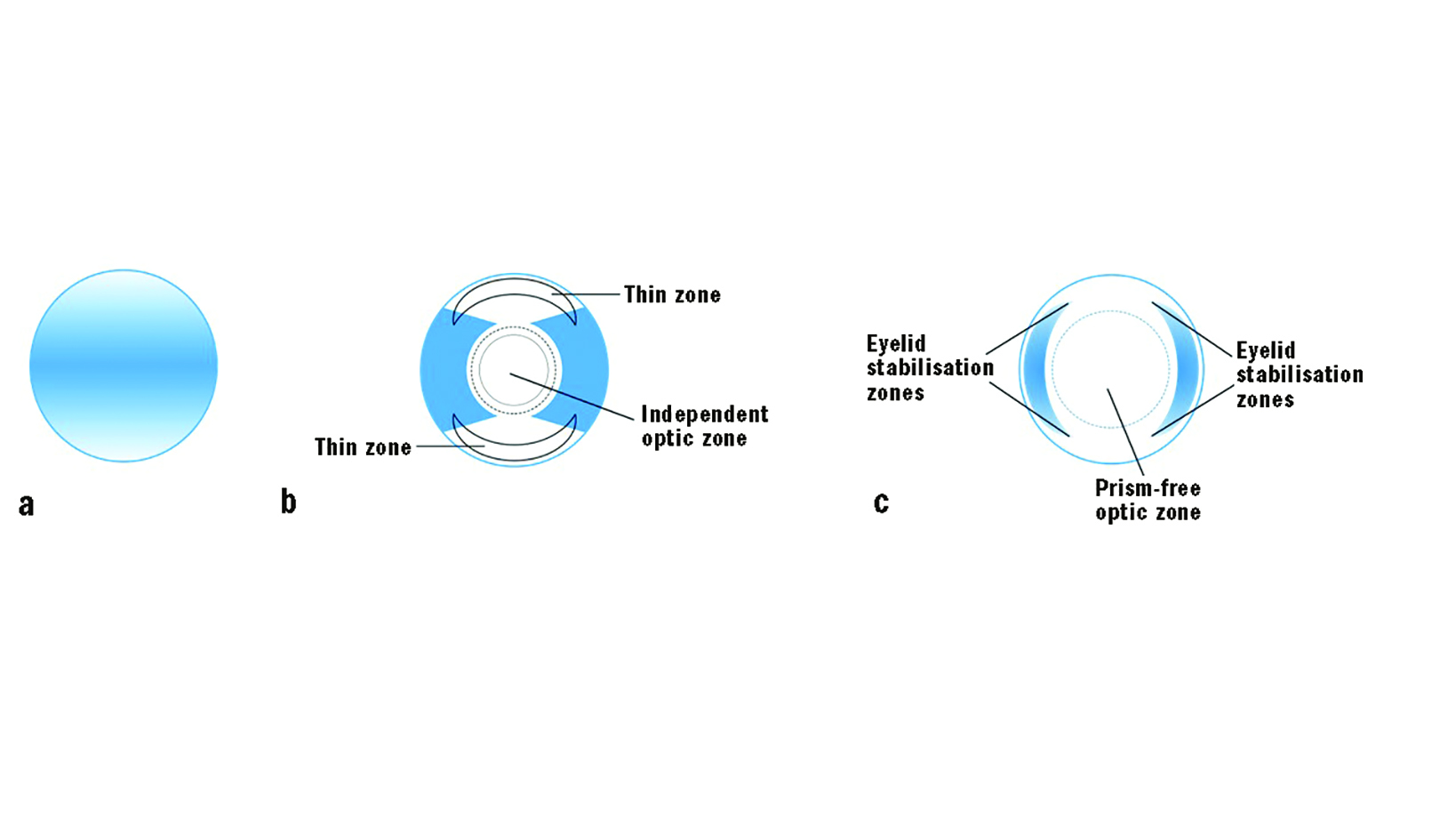 Figure 2: Thickness profiles of thin zone toric contact lens design where darker colour indicates greater thickness in; (a) original designs, (b) refined designs with independent optic zones and (c) in eyelid stabilised designs
Figure 2: Thickness profiles of thin zone toric contact lens design where darker colour indicates greater thickness in; (a) original designs, (b) refined designs with independent optic zones and (c) in eyelid stabilised designs
Toric Lens Performance
When we consider contact lens performance, we must always consider comfort, vision and health. Currently, there are no published trials that have compared the different toric designs on ocular comfort. However, the impact of lens thickness on oxygen performance should be considered when selecting a lens material, particularly for higher prescriptions, as this could have consequences for ocular surface physiology.
The quantity of vertical prism within the central optic zone has been investigated for a variety of stabilisation designs by Sulley et al.26 Despite advances in prism ballast and peri-ballast designs to reduce unwanted prism, significantly higher levels of vertical prism were observed in the prism ballast and peri-ballast designs (range; 0.52Δ to 1.15Δ) compared to the non-prism ballast designs (0.01Δ). The authors concluded that practitioners should consider this factor in particular when fitting monocular astigmats with binocular vision anomalies, as unwanted vertical prism may be present if fitted with a prism ballast or peri-ballast design.*
Stability of lens rotation must also be considered and has been investigated across a number of studies. Rotational stability when performing large saccadic versional tasks was deemed to be superior with an Eyelid Stabilised Design compared to a prism ballast lens, although reading and a visual search task resulted in similar levels of stability.27 In a comparative study of three prism ballast lenses and an Eyelid Stabilised Design lens, both designs showed fast re-orientation speeds after manual rotation by 45 degrees (22 to 25 degrees per minute).28 However, significant differences between lens designs were observed when patients were moved to a recumbent position, with prism ballasted lenses rotating further than the Eyelid Stabilised Design lens (figure 3). Similar findings of increased rotational stability during ocular movements and reduced gravitational effects for Eyelid Stabilised Design lenses compared to other lens designs have also been reported.29 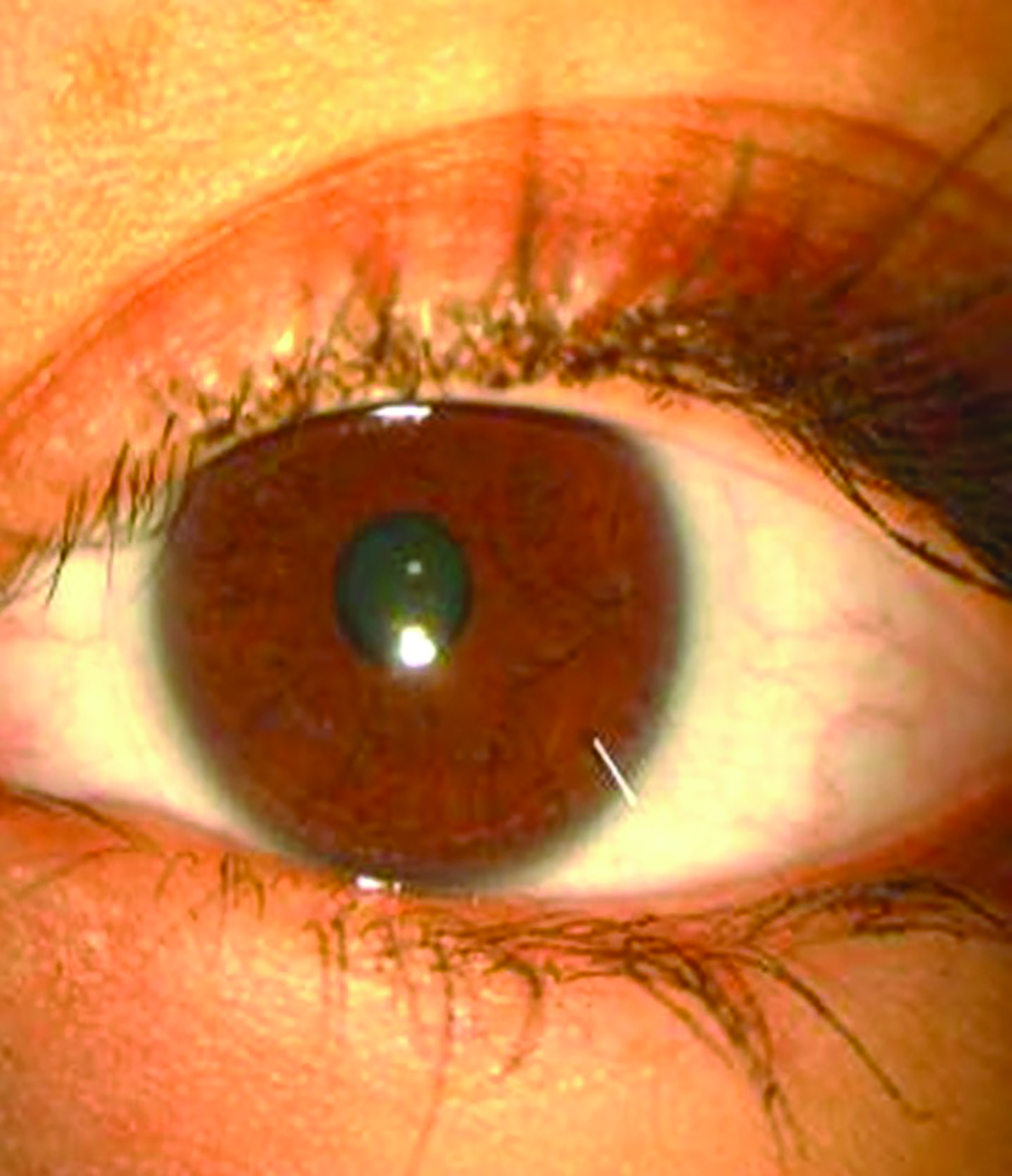 Figure 3: The effect of gravity on a prism ballasted soft toric contact lens while patient’s head is tilted to the side (image courtesy of Graeme Young)
Figure 3: The effect of gravity on a prism ballasted soft toric contact lens while patient’s head is tilted to the side (image courtesy of Graeme Young)
Conversely, in a recent study, an optimised prism ballast lens showed the lowest level of lens rotation from the vertical position and an improved re-orientation speed after manual rotation by 45 degree when compared to four other lenses of differing designs.30λ Lid position, the upward or downward slope of the lids and palpebral aperture size have been shown to be the main patient factors associated with lens orientation and stability.30 Therefore, while it is impossible to predict which lens will offer superior stability for an individual patient it may be preferable to fit Eyelid Stabilised Designs for more dynamic situations (watching or playing sport) or occupations such as dancers or mechanics.
Lens Orientation Marks
Soft toric lenses feature an orientation marking to allow the practitioner to assess the amount of lens rotation and lens stability. It should be noted that the orientation mark does not indicate the cylinder axis. A variety of orientation marks are used by manufacturers, typically either at the six o’clock or the three and nine o’clock positions (figure 4). 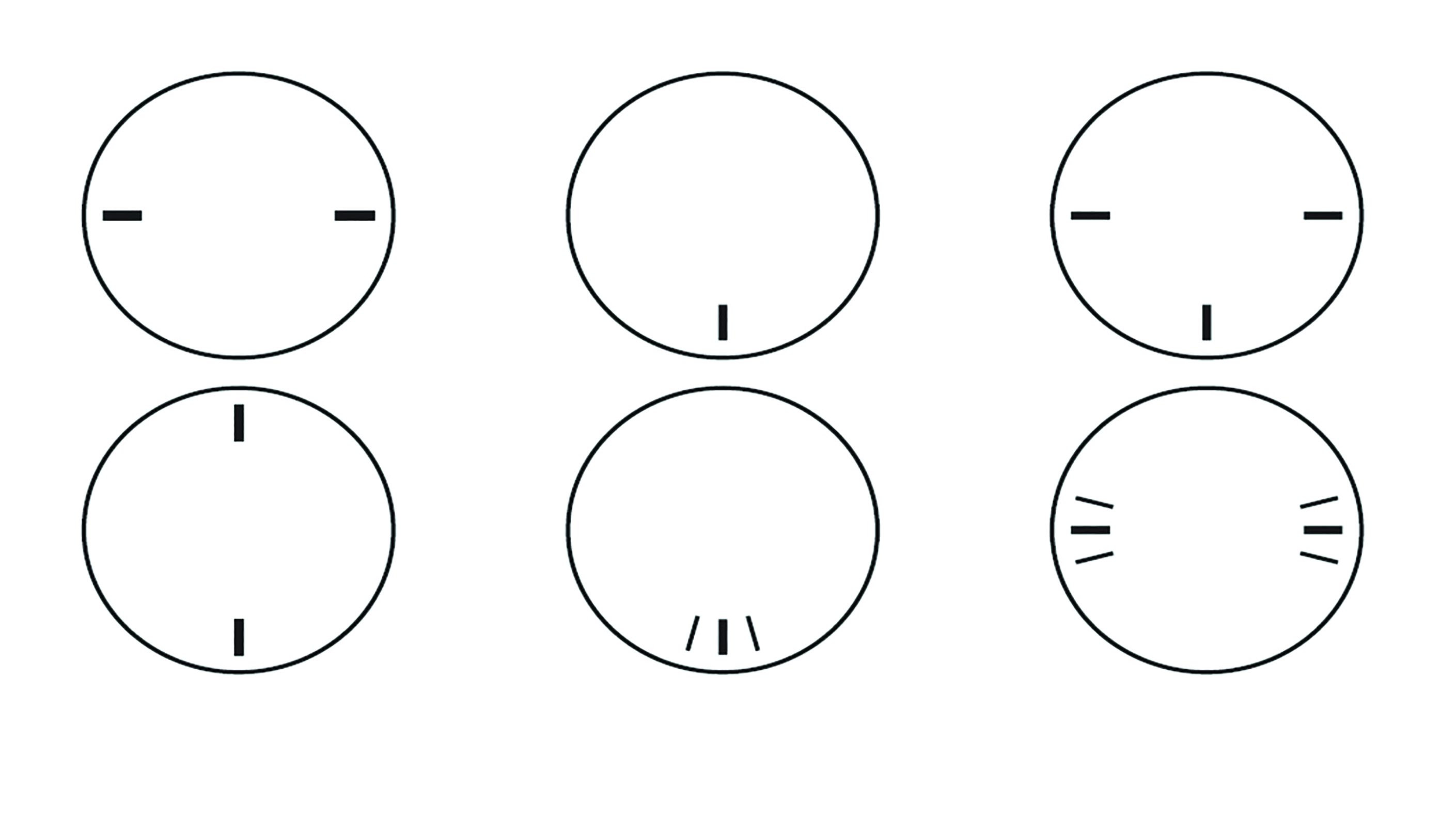 Figure 4: Examples of the different orientation markings used on soft toric contact lenses
Figure 4: Examples of the different orientation markings used on soft toric contact lenses
Lens rotation can either be measured by rotating a fine slit beam to align with the lens orientation marking and reading the axis from the external protractor scale using a graticule (figure 5) or estimated using the orientation marks as a guide (figure 6). An advantage of a toric lens with two markings opposite each other is that by passing a slit-beam through both markings, a more accurate measurement of lens rotation is achieved. Certain orientation markings can be difficult to observe and viewing the markings in indirect or retro-illumination rather than direct illumination can help.
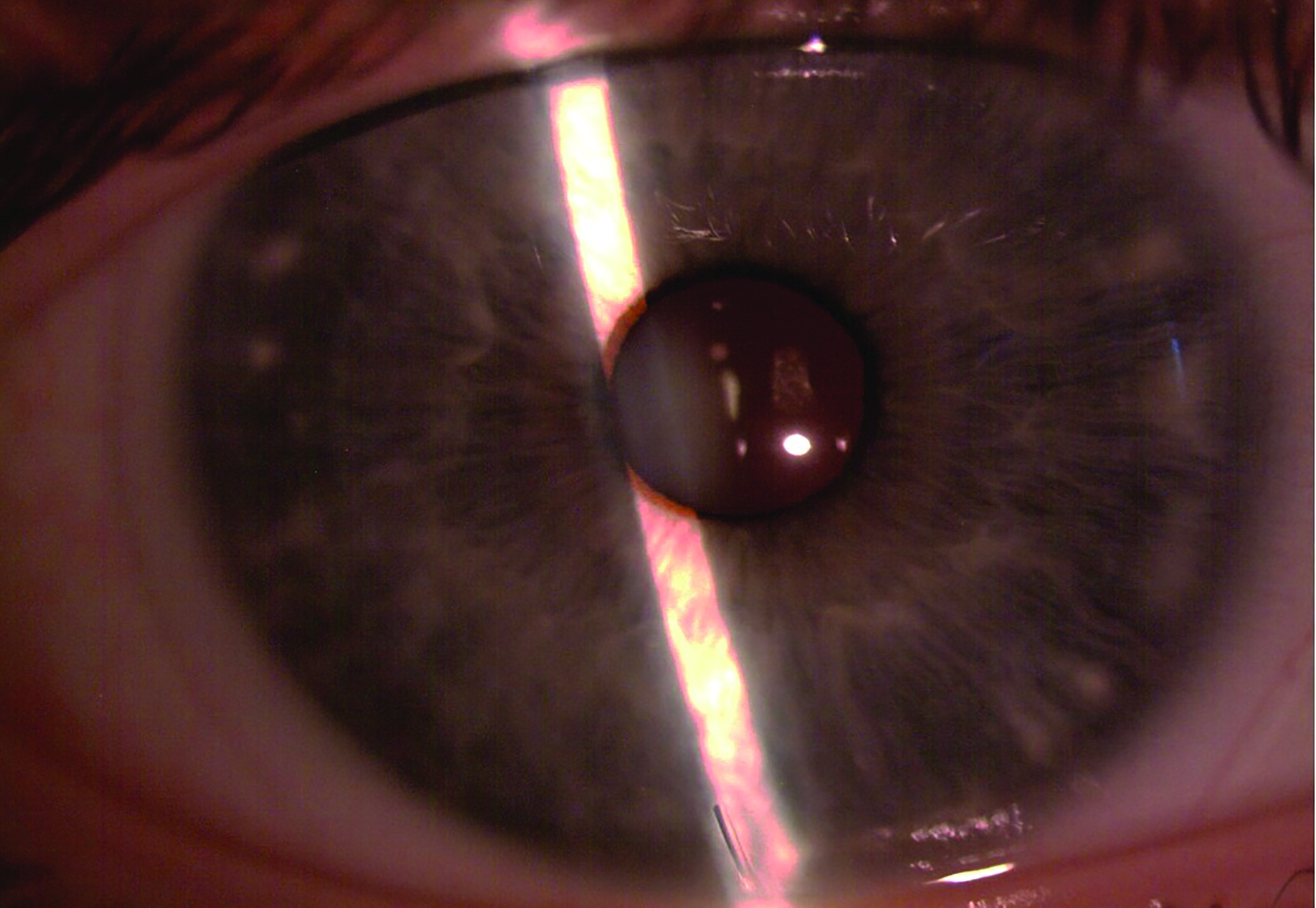 Figure 5: Measurement of soft toric contact lens rotation by rotating a fine slit beam to align with the lens orientation marking and reading the axis from the external protractor scale
Figure 5: Measurement of soft toric contact lens rotation by rotating a fine slit beam to align with the lens orientation marking and reading the axis from the external protractor scale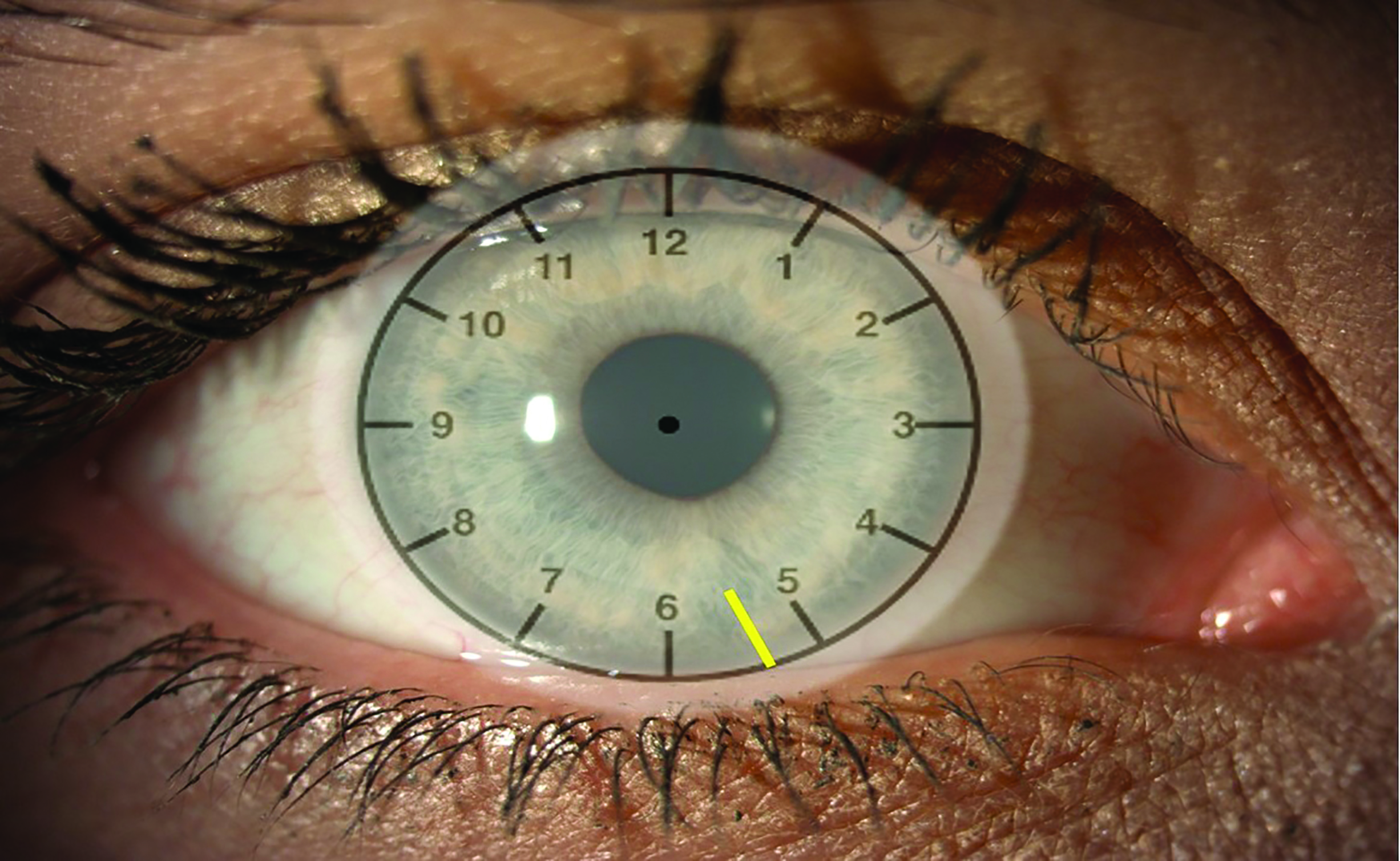 Figure 6: Estimation of rotation using a clock face as a guide, where rotation to the ‘five o’clock’ position would indicate 30 degrees of rotation. In this example, the yellow line indicating the toric marking is sitting approximately two thirds of the way between the five and the six o’clock, indicating rotation of around 20 degrees
Figure 6: Estimation of rotation using a clock face as a guide, where rotation to the ‘five o’clock’ position would indicate 30 degrees of rotation. In this example, the yellow line indicating the toric marking is sitting approximately two thirds of the way between the five and the six o’clock, indicating rotation of around 20 degrees
Adjusting for Rotation
The amount of lens rotation indicates how far the cylinder axis has rotated from the intended position. As long as the lens rotation is stable, the lens can be re-ordered to compensate for this rotation. The axis of the next lens to choose is decided by the following mnemonics:
- LARS; Left rotation = Add and Right rotation = Subtract (figure 7)
- CAAS; Clockwise rotation = Add and Anticlockwise rotation = Subtract (figure 8)
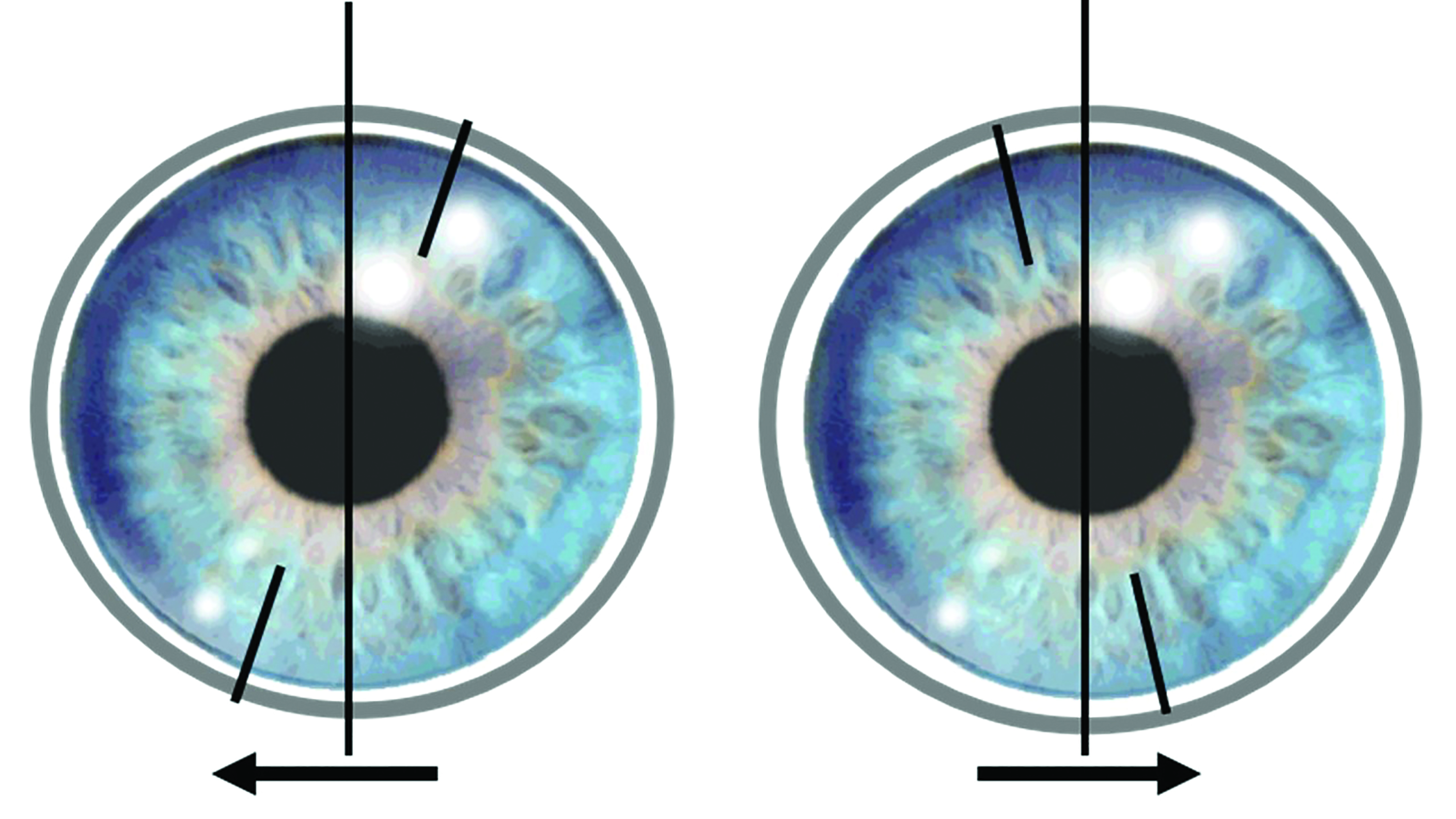 Figure 7: LARS rule where Left rotation (left image) = Add and Right rotation (right image) = Subtract
Figure 7: LARS rule where Left rotation (left image) = Add and Right rotation (right image) = Subtract
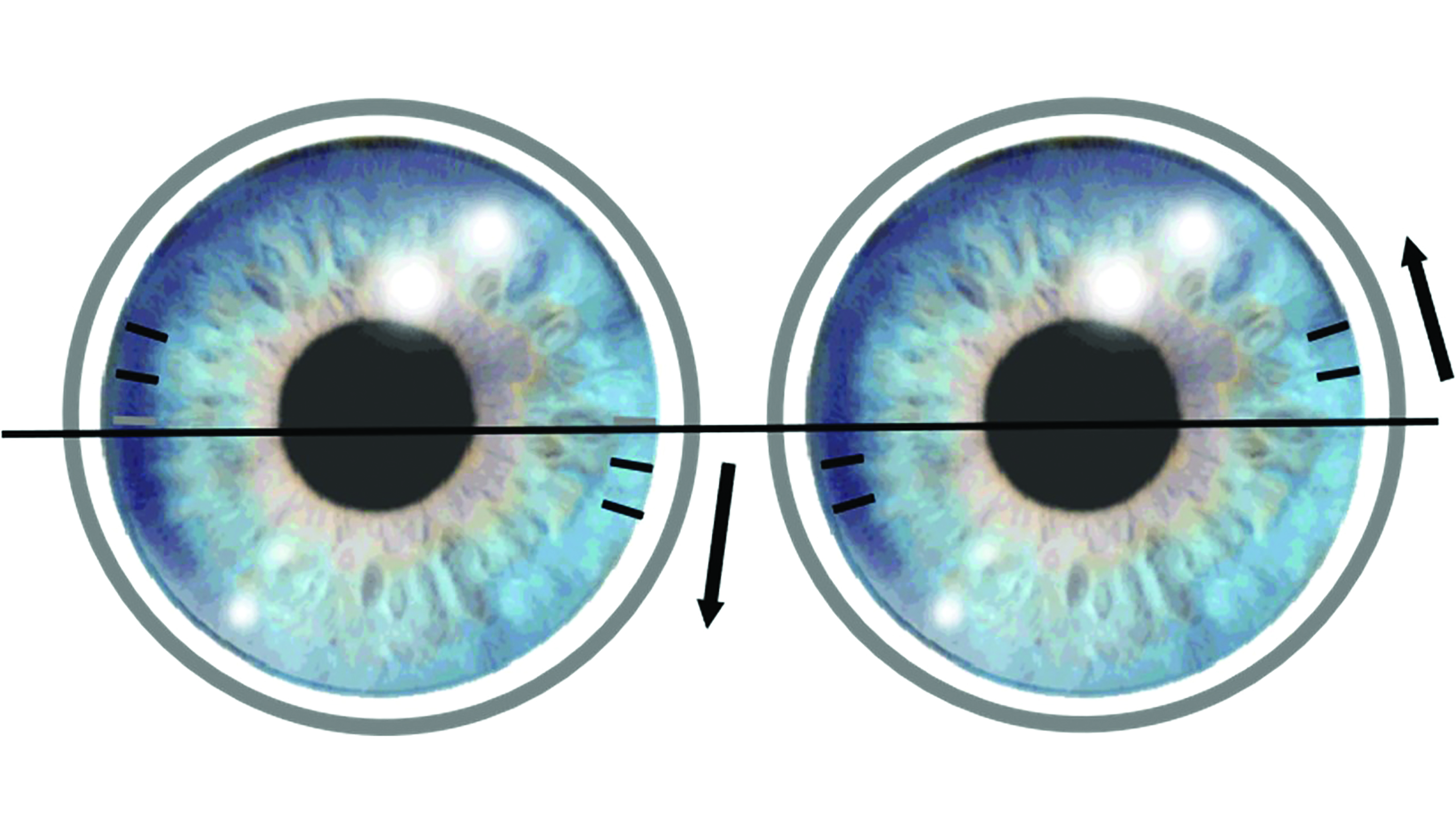 Figure 8: CAAS rule where Clockwise rotation (left image) = Add and Anticlockwise rotation (right image) = Subtract
Figure 8: CAAS rule where Clockwise rotation (left image) = Add and Anticlockwise rotation (right image) = Subtract
Although both mnemonics are useful, LARS may be preferred for lenses with orientation markings at six o’clock and CASS for lenses with orientation markings at the three and nine o’clock positions.
Consider this example:
An initial trial lens of -3.00 / -1.75 x 180 is fitted and rotates anticlockwise, or to the right, by 10 degrees when on the eye. The correction the patient experiences will therefore be -3.00 / -1.75 x 10 and so the vision will be blurred. To compensate for this, using the LARS or CAAS mnemonic, the new trial lens to be ordered will be -3.00 / -1.75 x 170. When the new lens is placed on the eye, the interaction between the lids and lens will be the same as with the first lens, rotating 10 degrees anticlockwise again. This rotation will bring the new axis round to desired 180 degrees and so offer optimal visual correction (figure 9). 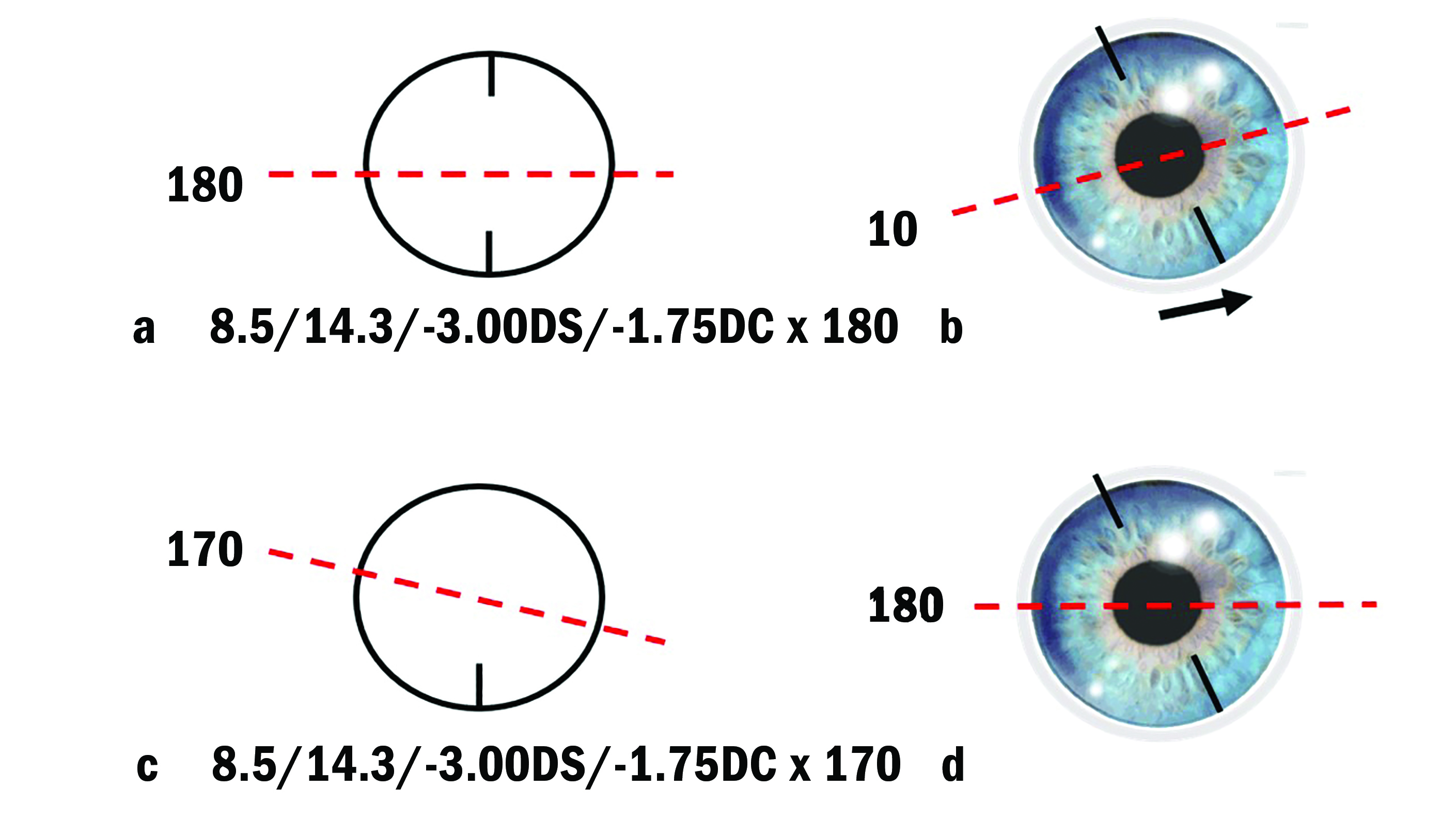 Figure 9: Using LARS and CAAS to manage toric rotation. Here a toric contact lens with a cylinder axis at 180° is ordered (a). Once applied to the eye, the contact lens rotates 10° anticlockwise, or right, meaning the cylinder axis lies at 10° (b). A new trial lens is ordered using the LARS or CAAS calculation with a cylinder axis of 170° (c). Once applied to the eye, the contact lens again rotates by 10° anticlockwise, meaning the cylinder axis is now along the desired 180°
Figure 9: Using LARS and CAAS to manage toric rotation. Here a toric contact lens with a cylinder axis at 180° is ordered (a). Once applied to the eye, the contact lens rotates 10° anticlockwise, or right, meaning the cylinder axis lies at 10° (b). A new trial lens is ordered using the LARS or CAAS calculation with a cylinder axis of 170° (c). Once applied to the eye, the contact lens again rotates by 10° anticlockwise, meaning the cylinder axis is now along the desired 180°
Toric Lens Fitting
The exact fitting procedure for soft toric lenses and for the supply of diagnostic or trial lenses may vary among the different brands and practitioners are encouraged to follow individual manufacturer’s guidelines. A standardised fitting process is described below.
Initial trial lens selection and application
The choice of back optic zone radius (BOZR), lens material and replacement modality for a soft toric lens should be made in the same way as one would select a spherical soft design. The effect of the back vertex difference (BVD) should be carefully considered and calculated empirically for each meridian or determined using manufacturer’s effectivity tables or online calculators. Mistakes can be made by guessing the optimal power, particularly in plus power lenses where practitioners often mistakenly reduce the cylinder power (table 2).
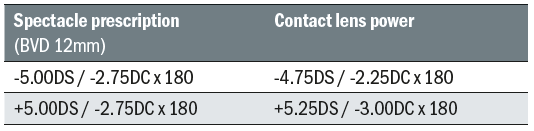 Table 2: Calculated contact lens power for myopic and hyperopic spectacle prescriptions. Note the relative increase in contact lens cylinder power for the hyperopic prescription and the decrease for the myopic prescription
Table 2: Calculated contact lens power for myopic and hyperopic spectacle prescriptions. Note the relative increase in contact lens cylinder power for the hyperopic prescription and the decrease for the myopic prescription
Typically, toric contact lens cylinder powers are only available in 0.50DC steps. Where the desired lens falls between two powers, it is generally advisable to select initially the lower cylinder power. Unwanted lens rotation will have a detrimental impact on visual quality and this can be exacerbated if the cylinder is over-corrected. The cylinder power can be checked during the over-refraction and amended if the higher power is beneficial however. Axis availability for most disposable lenses is in 10-degree steps around the clock, or even five degrees for extended power ranges. Where the desired lens falls between two axes, it can be beneficial to use a trial frame fitted with the patient’s spectacle prescription to determine which axis they prefer.
While a number of patient factors and lens fit characteristics influencing soft toric lens orientation have been identified, the findings fall short of allowing practitioners to accurately predict toric lens orientation. Hence, no initial compensation of the cylindrical axis should be made when choosing the initial trial lens. The patient should be forewarned of an initial increased level of lens awareness with a toric lens, particularly if fitted unilaterally or a spherical lens patient is being refitted with a toric lens. This lens awareness is due to the thickness differential from the lens stabilisation design and typically resolves after a short period of adaptation. Following application, the lens should be allowed to settle, as for a spherical soft lens, before the fit is assessed. While some practitioners prefer to apply toric lenses with the orientation mark in the correct position to optimise the speed of orientation, this is not necessary. With more recent designs, speed of orientation is faster, allowing assessment within one to three minutes following application.8
Lens fit assessment
As for a spherical lens, an optimal lens fit with good centration is desirable; a steep fitting lens is likely to impair re-orientation whereas a flat fitting lens is likely to result in reduced lens stability and increased rotation. The location of the orientation marking should be assessed while the patient fixates in the primary position initially. If the orientation marking is stable in the primary position of gaze, the practitioner should note the position in relation to the intended position and the direction and degree of rotation seen (if any). The method used to measure lens rotation is described earlier in the lens orientation marking section. If the lens position is more than 30 degrees from the intended position, it suggests that there is inadequate stabilisation and an alternative lens design should be considered.
With the patient assuming primary gaze, the lens may show a minimal amount of nasal rotation, typically of up to five degrees either during or immediately after a habitual blink. This is due to the movement of the lower lid during a blink. Excessive rotation following a habitual blink, particularly for higher cylinder powers, is likely to result in unstable vision however and an alternative lens design is indicated. Orientation stability should be assessed further while the patient performs forced blinks and version movements. To simulate real world eye movements, ask the patient to look up, down, left and right, while looking for any significant lens rotation. Provided the lens remains stable, it should provide relatively consistent vision. The efficacy of the lens re-orientation can be assessed by manually rotating the lens off-axis using the lower eyelid. If the stabilisation method is optimal, the lens should return to its original position quickly following a few blinks. As long as the lens is stable, any consistent rotation that impairs the visual performance can be corrected with the LARS or CAAS mnemonic, as described earlier.
Over-refraction
An over-refraction should be carried out to determine the optimal lens power and to provide further information on lens stability. If the patient reports that the vision blurs with each blink, this confirms the lens fit is unsuitable or the rotational stability of the lens is poor. In either case, another lens needs to be applied, either a different parameter (in the case of a poor fit) or stabilisation design (if the lens is rotationally unstable). Visual performance should also be assessed at near.
If the trial lens orientation marking lies within 10 degrees of the intended position, vision can be assessed and a spherical over-refraction carried out to determine whether an alternate spherical power should be ordered. A full sphere-cylinder over-refraction is unnecessary and will over-complicate the process. A cross-cylinder, or a loose cylinder trial lens, held at the appropriate axis can be useful to confirm the correct cylinder power however.
Lenses that position off-axis will produce a residual refractive error, which is a function of the cylinder power and degree of mis-orientation. For example, a toric soft lens of power -3.00DS / -1.75DC x 180 that matches the patient’s ocular prescription but orientates 20 degrees off-axis will result in an over-refraction of +0.50DS / - 1.25DC x 55. The stability of the end-point gives a good indication that lens fit is adequate; however, it is impossible to determine whether the spherical component of the final prescription to be ordered requires adjustment. Consequently, a new trial lens should be applied after compensation of the cylinder axis for lens rotation to allow a meaningful spherical over-refraction.
Troubleshooting
Poor visual performance
The most common reason for reduced visual performance is rotation of the axis or poor lens stability. If the lens has rotated, but remains stable then the degree of rotation should be corrected with the LARS or CAAS mnemonic. If the lens axis has previously been altered to compensate for rotation, it can be beneficial to check the lens is sitting in the expected ‘off axis’ position. Checking the lens power in relation to the spectacle prescription may identify mistakes with back vertex distance compensation or even simple human error. If poor lens stability is observed or the patient reports unstable vision then the lens fit should be optimised. A steep fitting lens is likely to impair re-orientation whereas a flat fitting lens is likely to result in reduced lens stability and increased rotation. Furthermore, a change in the lens stabilisation design is likely to be beneficial where there is inconsistent lens rotation. Figure 10 is a flowchart showing a stepped procedure to tackle poor visual performance. 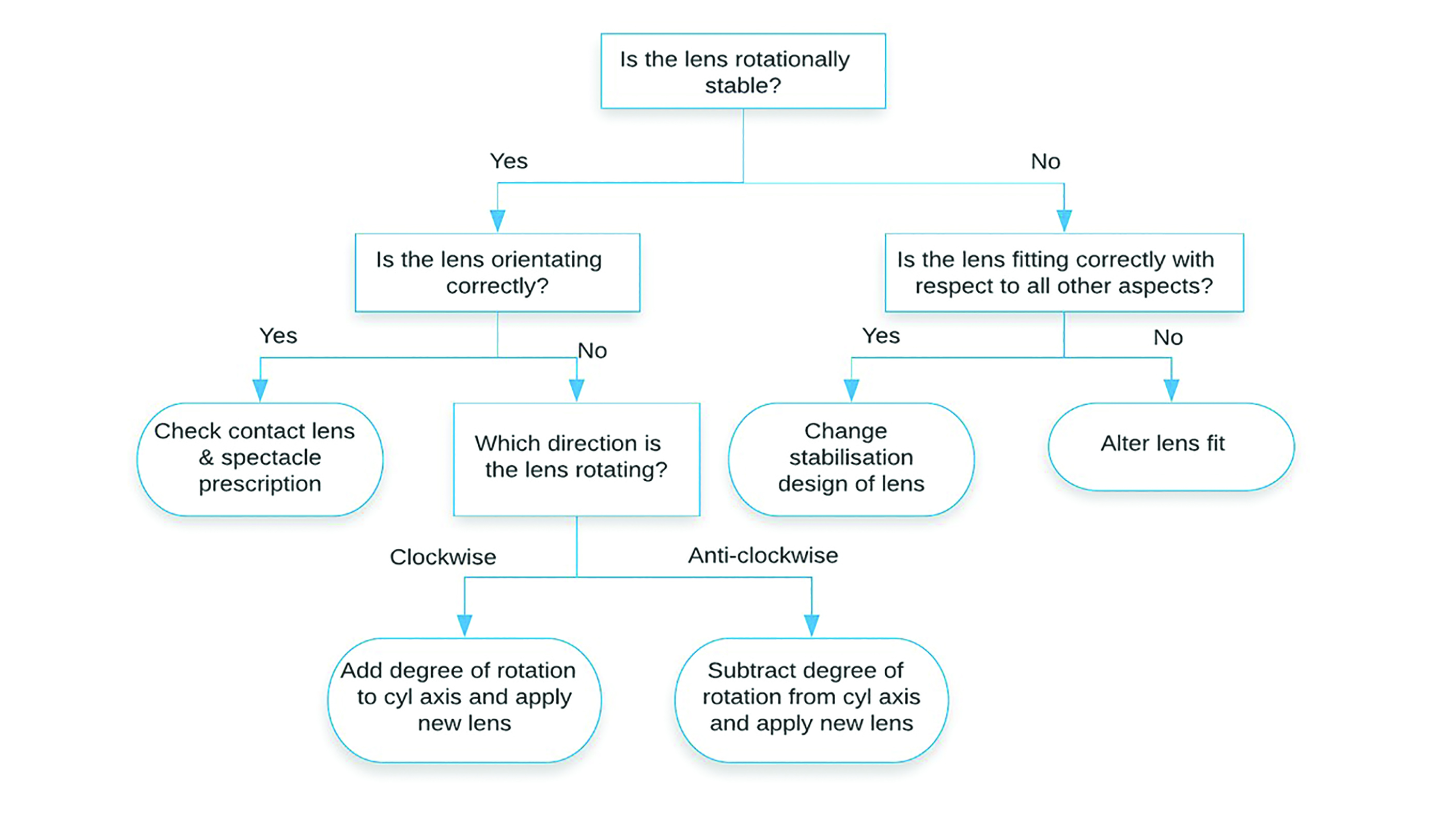 Figure 10: Flowchart to aid problem solving with poor visual acuity
Figure 10: Flowchart to aid problem solving with poor visual acuity
Poor comfort
Discomfort should be managed with the same approach as for a spherical lens. Increasing the lens replacement frequency is likely to be beneficial. While the range of parameters may not be quite as wide in daily disposables as reusables, particularly for the higher cylinder powers, a study has shown that under correction of the cylinder by up 0.50DC, while maintaining the spherical equivalence has no significant adverse effect on visual performance.32 Another factor to consider is the likely thickness differential of the current lens as refitting with a different stabilisation design may be beneficial.
Contact lens wear dropout
Discomfort and poor vision are the primary causes of permanent discontinuation of contact lens wear, or dropout across all lens types.33,34 In a prospective study of retention rates over a 12-month period, the main reason for discontinuation within the toric lens group was poor vision (48%) and expense (19%).34 In a study published in 2011, soft toric lens wearers reported more frequent and intense discomfort and dryness compared to spherical lens wearers.35 More recently, however, a retrospective study by Sulley et al of neophyte wearers found no significant difference in dropout between spherical and toric lens wearers, with 79% and 73% respectively still wearing lenses after 12 months.36 It was suggested this may reflect more recent advances in toric lens design or increased practitioner confidence in fitting such lenses.
The practitioner is key to identifying patients at risk of dropout. Disappointingly, considering the toric lens patients that discontinued lens wear in the study by Sulley, less than a third were offered an alternative lens by their practitioner.36 Real world eye movements are difficult to reproduce on the slit lamp. Therefore, subjective reports of poor lens performance may not correlate with objective measures such as lens rotation and stability. Furthermore, high contrast visual acuity may not indicate the real world visual performance of soft toric lenses. Therefore, practitioners should ask patients about fluctuations in vision during specific activities and in different environments to identify their level of satisfaction.37 To avoid dropout, patients should be proactively refitted and be informed of new lens developments.
Conclusions
With a greater understanding of the forces that influence soft toric lenses on the eye, designs continue to improve with faster orientation when first applied, as well as being more predictable and more stable during more dynamic vision situations. In many ways fitting a soft toric lens today is as straightforward as fitting a spherical lens for the majority of patients and with improving performance and patient satisfaction, should continue to be an integral part of contact lens practice. Practitioners should be proactive in explaining the effects of astigmatism and the possible benefits of toric lenses, encourage trials and identify and refit current wearers at risk of dropout.
Dr Katharine Evans is an Optometrist, Senior Lecturer and Director of Clinics at Cardiff University and is a paid consultant for Johnson & Johnson Vision. Dr Rachel Hiscox is a Professional Education & Development Manager, UK & Ireland for Johnson & Johnson Vision Care.
- This article is part of a revised and updated ‘Essential Contact Lens Practice’ series, originally authored by Jane Veys, John Meyler and Ian Davies. This article was produced without further input or review from the original authors.
*Vertical heterophoria possibly caused by prism dissociation due to the presence of induced optical prism is a relevant factor for practitioners to consider when fitting toric contact lenses for monocular astigmats or those requiring a mix of toric soft contact lens designs.38,39 Clinical studies have not been done to fully characterize the clinical effects of differences in base down prism among different contact lenses.
λ Study contact lenses included: PureVision Toric, Air Optix for Astigmatism, Acuvue Advance for Astigmatism, Biofinity Toric and Proclear Toric.
References
- Morgan PB et al. An international survey of toric contact lens prescribing. Eye Contact Lens 2013;39(2):132-137
- Morgan P. UK contact lens prescribing in 2019. Optician 2019;160(6722):14-16
- Bennett AG and Rabbetts RB. Distribution and ocular dioptrics of ametropia. In: Clinical Visual Optics (London: Butterworths), 1984; 433-444
- Holden BA. The principles and practice of correcting astigmatism with soft contact lenses. Aust J Optom 1975;58:279-299
- Young G, Sulley A, Hunt C. Prevalence of astigmatism in relation to soft contact lens fitting. Eye Contact Lens 2011;37(1):20-25
- Luensmann D. Spectacle prescriptions review to determine prevalence of ametropia and coverage of frequent replacement soft toric contact lenses. Cont Lens Anterior Eye 2018;41(5):412-420
- Astigmatism Consumer Usage and Awareness Study. Bruno & Ridgeway Research Associates, Inc. March 2007
- Sulley et al. Clinical evaluation of fitting toric soft contact lenses to current non-users. Ophthalmic Physiol Opt 2013;33:94-103
- Richdale K et al. Visual Acuity with spherical and toric soft contact lenses in low-to moderate-astigmatic eyes. Optom Vis Sci 2007;84(10)969-975
- Berntsen DA. Higher-order aberrations when wearing sphere and toric contact lenses. Optom Vis Sci 2009;86(2):115-122
- Cho P, Cheung SW, Charm J. Visual outcome of Soflens daily disposable and Soflens daily disposable for astigmatism in subjects with low astigmatism. Clin Exp Optom 2012;95(1):43-47
- Berntsen DA et al. A randomized trial to evaluate the effect of toric versus spherical contact lenses on vision and eyestrain. Eye Contact Lens 2019;45(1)28-33
- Black AA et al. The impact of uncorrected astigmatism on night driving performance. Ophthalmic Physiol Opt 2019;39:350-357
- Cox SM et al. Efficacy of toric contact lenses in fitting and patient-reported outcomes in contact lens wearers. Eye Contact Lens 2018;44:S296-299
- Cox DJ. Does correcting astigmatism with toric lenses improve driving performance? Optom Vis Sci 2015;92(4):404-411
- Saxon J, Rah MJ, Reindel WT. Satisfaction of astigmatic patients with toric nesofilcon A contact lenses. Clin Optom (Auckl) 2019;9(11):1-10
- Efron SE et al. A theoretical model for comparing UK costs of contact lens replacement modalities. Cont Lens Ant Eye 2012;35(1):28-34
- Cho PC and Woo GC. Vision of low astigmats through thick and thin lathe- cut soft contact lenses. Cont Lens Ant Eye 2001;24:153-160.
- Bernstein PR et al. Masking corneal toricity with hydrogels:does it work? Int Contact Lens Clinic 1991;60:728-731.
- Edmondson L et al. Masking astigmatism Ciba Focus Night & Day
vs Focus Monthly, Optom Vis Sci 2003; 80:12 184. - Morgan PB et al. Inefficacy of aspheric soft contact lenses for the correction of low levels of astigmatism. Optom Vis Sci 2005; 82(9):823-828.
- Edrington TB. A literature review: The impact of rotational stabilization methods on toric soft contact lens performance. Cont Lens Ant Eye 2011;34(3):104-110
- Grant R. Toric soft contact lenses: a review. Optician, 1995;209(5483):16-24
- Cox I, Comstock T and Reindel W. A clinical comparison of two soft toric contact lenses. Optician, 1999; 218:5730 32-36.
- Hickson-Curran S, Veys J and Dalton L A new dual-thin zone disposable toric lens. Optician, 2000; 219:5736.
- Sulley A et al. Resultant vertical prism in toric soft contact lenses. Cont Lens Ant Eye 2015;38(4):253-257
- Zeikos GA et al. Rotational stability of toric soft contact lenses during natural viewing conditions. Optom Vis Sci 2007;84(11):1039-1045
- Young G, McIlraith R, Hunt C. Clinical evaluation of factors affecting soft toric lens orientation. Optom Vis Sci 2009;86(11):E1259-1266
- McIlraith R, Young G, Hunt C. Toric lens orientation and visual acuity in non-standard conditions. Cont Lens Ant Eye 2010; 33(1):23-26
- Momeni-Moghaddam H et al. Comparison of fitting stability of the different soft toric contact lenses. Cont Lens Ant Eye 2014; 37(5):346-350
- Young G, Hunt C, Covey M. Clinical evaluation of factors influencing toric soft lens fit. Optom Vis Sci 2002;79(1):11-19
- Sha J et al. Effect of cylinder power and axis changes on vision in astigmatic participants. Clin Optom (Auckl) 2009;19(11):27-38
- Dumbleton K et al. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens 2013;39(1):93-99
- Sulley A et al. Retention rates in mew contact lens wearers. Eye Contact Lens 2018;44(Suppl. 1):S273-282
- Young G et al. Characterizing contact lens-related dryness symptoms in a cross-section of UK soft lens wearers. Cont Lens Ant Eye 2011;34(2):64-70
- Sulley A, Young G, Hunt C. Factors in the success of new contact lens wearers. Cont Lens Ant Eye 2017;40(1):15-24
- Pyzer I. Opening our eyes up to new toric insights. Optometry Today 2009;49(20):40-43
- Jackson D, Bedell HE. Vertical heterophoria and susceptibility to visually induced motion sickness. Strabismus. 2012;20(1):17-23.
- duToit R, Ramke J, Brian G. Tolerance to prism induced by readymade spectacles: setting and using a standard. Optom Vis Sci. 2007;84(11):1053-1059.
