Voted the third best movie quote of all time, ‘you’re gonna need a bigger boat’ has since become synonymous with situations where there is a stark and frank realisation that the menace is a far greater threat than had earlier been anticipated. In the 1975 film Jaws, the shark makes a sudden, shocking and first full appearance, without any warning, after 81 minutes of gripping cinema tension. The three men sent to manage the dangerous beast immediately realise that theirs will not be a simple or straightforward task.
Optometric primary care during COVID-19
As we move from red to amber across the four nations,1 we are now taking a good look at both the current magnitude and future potential impact of the Covid-19 virus. The aim of this article is to provide practitioners with some considerations and reflections on how to optimise their clinical practice and their practice location a safe, comfortable and inviting place; realistic, pragmatic and thought provoking, but not frightening. We will look carefully at the recent changes in guidance and consider some innovations in clinical practice which may help with the transition to the new phases.
Masks
Updated guidance on the use of face masks was published by the World Health Organisation (WHO) on June 5, 20202 and the UK government made a statement on the use of facemasks in public places, specifically relating to use on public transport, later that same day. The guidance issued was for the wearing of face coverings on buses, trams, trains and the underground, giving a recommendation for immediate public attention and preparation, with a mandatory instruction coming into effect for mask use from June 15, 2020. Prior to this date, guidance had been given by the UK government to allow sufficient stocks of face masks to be procured and purchased for frontline NHS staff and other healthcare workers.
Face coverings and masks may have limited effect if the use, material use or fabric weave is not carefully considered and managed. Importantly, masks must cover the mouth and the nose for a level of effectivity. Figures 1 to 4 show different types of face mask.
 Figure 1: Type 1, 3-ply surgical mask suitable for patient use and non-clinical areas
Figure 1: Type 1, 3-ply surgical mask suitable for patient use and non-clinical areas
For clinical use, a fluid resistant surgical mask (as in figure 2) is the current UK recommendation for procedures at less than 2m, which would include most contact lens specific routines.3 A Type 1 mask (figure 1) could be issued to patients on entrance to the practice if they are not already wearing a fabric mask.
 Figure 2: Type 2R (or IIR), 4-ply waterproof surgical mask for clinical settings
Figure 2: Type 2R (or IIR), 4-ply waterproof surgical mask for clinical settings Figure 3: FFP3 mask for use when performing aerosol generating procedures
Figure 3: FFP3 mask for use when performing aerosol generating procedures Figure 4: Fabric mask for use by general public when using public transport or in a public space
Figure 4: Fabric mask for use by general public when using public transport or in a public space
The WHO offers the following information on the correct using of face masks:
- Perform hand hygiene before putting on the mask
- Place the mask carefully, ensuring it covers the mouth and nose, adjust to the nose bridge, and tie it securely to minimise any gaps between the face and the mask
- Avoid touching the mask while wearing it
- Remove the mask using the appropriate technique: do not touch the front of the mask but untie it from behind
- After removal or whenever a used mask is inadvertently touched, clean hands with an alcohol-based hand rub, or soap and water if hands are visibly dirty
- Replace masks as soon as they become damp with a new clean, dry mask
- Do not re-use single-use masks
- Discard single-use masks after each use and dispose of them immediately upon removal.
Proximity
Covid-19 is essentially a respiratory disease. Currently, transmission is understood to be via airborne droplets released by expiration and infecting others via the following entry points:
- Nose
- Mouth
- Eye
The UK Government has planned to reduce social distancing rules from 2m to ‘1m plus’ in England from July 4, 2020. In Northern Ireland, distancing was changed from 2m to 1m on June 29, 2020. At the time of publication, Scotland and Wales are maintaining a 2m separation recommendation. Whatever future guidance is given, it is vitally important to maintain maximum distancing and minimum time exposures.
Proximity, distancing and other Covid-19 related guidance varies from one country, possibly from one region of a country to another (localised second spikes may require localised implementation of stricter rules in the coming months). However, hand washing and disinfection routines should always warrant a consistent global approach.
Table 1 shows current different public social distancing regulations. Please note that countries adopting ‘closer’ social distancing rules may insist on the wearing of a face mask (see section on face coverings) in public.
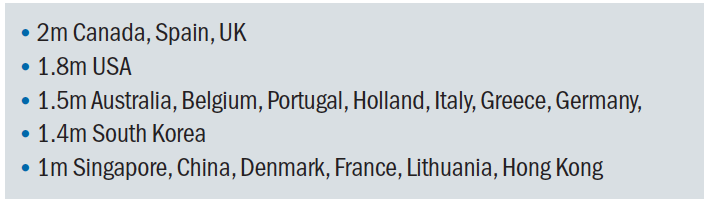 Table 1: Examples of recommended social distancing in a range of countries (July 2020)4
Table 1: Examples of recommended social distancing in a range of countries (July 2020)4
While social distancing guidance is calculated using mathematical modelling and dictated by science, the ability to measure a personal separation distance of, say, 1.4m is a tricky concept for the lay person to accurately implement, or indeed for the law to enforce.
Proximity values carry a risk of infection that is closely linked to the duration for which the proximity is maintained and accurate risk evaluation based upon proximity:time ratios are difficult to calculate. However, some broad, risk assessments have been documented as follows:5
- 1m proximity for six seconds carries the same exposure risk as 2m proximity for 60 seconds
- One cough at 2m proximity carries the same exposure risk as talking at 2m proximity for 30 minutes
- Exposure to infection risk is 19 times greater indoors than
outdoors - Exposure to infection risk at 1m proximity is 10 times greater than at 2m proximity.
There appear to be three clearly defined separation distances which have been subject of clinical research on Covid-19:
- Greater than 2m
- Greater than 1m
- Less than 1m (which is effectively zero distance)
For the purpose of clinical routines, and in particular contact lens fitting procedures, a zero-distance policy is the most appropriate to be considered, with appropriate PPE the primary objective. It can be clearly seen that close proximity and an increased time factor in limited or constrained spaces presents a palpable risk factor when completing contact lens work.
Changing behaviours and culture in your practice
As mentioned in our previous article (see Optician 05.06.20), the SARS-CoV-2 virus shows no preference, politeness or respect for cultural beliefs and behaviours in its cold, efficient spread of devastation across the planet. Man-made geographical or cultural boundaries present neither deterrent or obstacle to this invisible menace.
The stigmatisation linked to wearing face masks remains something of a hurdle to many6 and meets a peculiarly high level of resistance in the UK. This is despite the fact that face masks act as a valid method of reducing viral exposure and output. Residents of Hong Kong, Singapore and Taiwan, for example, have shown effective and admirable Covid-19 containment and wearing of face masks in these areas is second nature. Ready and prepared following previous virus epidemics in 2003 and 2007, immediate implementation of face coverings was a culturally acceptable behavioural pattern throughout the Far East. Perhaps such measures will be more readily adopted by the UK in the expected next pandemic. Lack of scientific certainty as to effectiveness is no longer an argument for failing to change behaviours. Consider the following viewpoints from the 2007 SARS Commission report:
‘...recognise, as an aspect of health worker safety, the precautionary principle that reasonable action to reduce risk, such as the use of a fitted facemask or respirator, need not await scientific certainty.’
‘...if we do not learn from SARS and we do not make the government fix the problems that remain, we will pay a terrible price in the next pandemic.’
Germany, with a population 30% greater than the UK, reports a Covid-19 fatality figure which equates to 80% fewer deaths than the UK total. Germany initially imposed a rule of one person per 20m2 in public retail spaces, but enforcement was difficult and the practical implementation of the measure was widely viewed as draconian, though albeit effective. The personal separation rule has since been reduced to one person per 10m2 of indoor public retail space.
Now consider a consulting room in a typical eye care practice, with dimensions 3m x 3m, or 9m2. By German standards, this clearly will not offer sufficient quality air for a practitioner, and certainly no available space for a patient.
Hand washing remains the primary method of avoiding cross infection and contamination. Soap and water are very simple to use, environmentally friendly and very effective in reducing virus. Hand hygiene and respiratory hygiene promoting behaviours are of primary importance moving forward.
Forearm washing warrants special attention. Short sleeved scrubs and single use gloves may leave the forearm exposed. Single use gloves may lead to some false sense of safety and recent research by the American Academy of Ophthalmology indicates that the forearm and shoulder are key areas of exposure to airborne droplets when operating a slit lamp.7 A simulated droplet transmission experiment, using video imaging of fluorescent droplet spread, clearly indicates that the forearm should be included in the rigorous hand washing routine (figure 5).  Figure 5: Forearms are exposed to virus and should be washed during handwashing
Figure 5: Forearms are exposed to virus and should be washed during handwashing
Communication
Practitioners in both healthcare, and non-healthcare settings have found distancing, face masks and eye protection acceptable and easily implemented. However, evidence of poor communication regarding new behaviours with patients and of a perceived lower empathy for patients from care providers when wearing PPE has been published.5 The observation that patients considered their health care professional to demonstrate a lower level of empathy when masked is easy to explain, though disappointing to accept and to mitigate against. Figure 6 and 7 show a change in facial expression underneath PPE. This is sometimes difficult to perceive even for seasoned professionals, certainly in the short term.  Figure 6: PPE may mask underlying facial expression and reduce the patient-practitioner rapport
Figure 6: PPE may mask underlying facial expression and reduce the patient-practitioner rapport Figure 7: But it is clear when someone is smiling
Figure 7: But it is clear when someone is smiling
Experienced practitioners will be acutely aware of the necessity to communicate effectively with a range of patients by the use of a range of styles and techniques. While a face covering may now be considered to be an essential part of personal protective equipment, it may also be a barrier against easy and effective communication. Verbal dialogue may be a solution to this barrier, but as this may also be considered a risk factor for spread of virus, it needs to be kept to a minimum. Imaginative and innovative patterns and styles of communication will need to be developed.
When dealing with hearing or visually impaired patients, an inability to accurately assess body language, in particular facial expression, puts both patient and practitioner at a disadvantage. In a typical clinical environment, often littered with complex instrumentation and imagery, a masked and unfamiliar facial expression is yet more difficult to interpret. Unlike the virus, humans are demonstrative, emotional and expressive creatures, and the development and widespread adoption of new communication styles will no doubt evolve from the current crisis.
Innovation and Technology in Clinical Procedures
Contact lens practice presents a significant challenge to maintaining separation and minimise contact time, so let us consider some aspects of this area of practice.
Contact lens fitting
Consideration for neophyte contact lens fitting was discussed in our previous article (see Optician 05.06.20) where we recommended postponement in the event that this was a non-urgent procedure. This advice may not have changed since.
A new fitting, particularly a new complex fitting, may prove to be a laborious and time-consuming exercise with the likelihood of a number of face-to-face, close proximity appointments being required. There is also a high chance that a number of diagnostic contact lenses, each requiring stringent cleaning and disinfection procedures, will be used.8
The use of accurate corneal topography may help to reduce the number of diagnostic products to almost nil (figure 8). Corneal, hybrid, mini-scleral and orthokeratology contact lenses can now be designed and fitted on an empirical basis from high quality corneal maps. Contact lens manufacturers are familiar with this concept and will be pleased to walk and talk inexperienced practitioners through this simple process. Drop them a line perhaps?
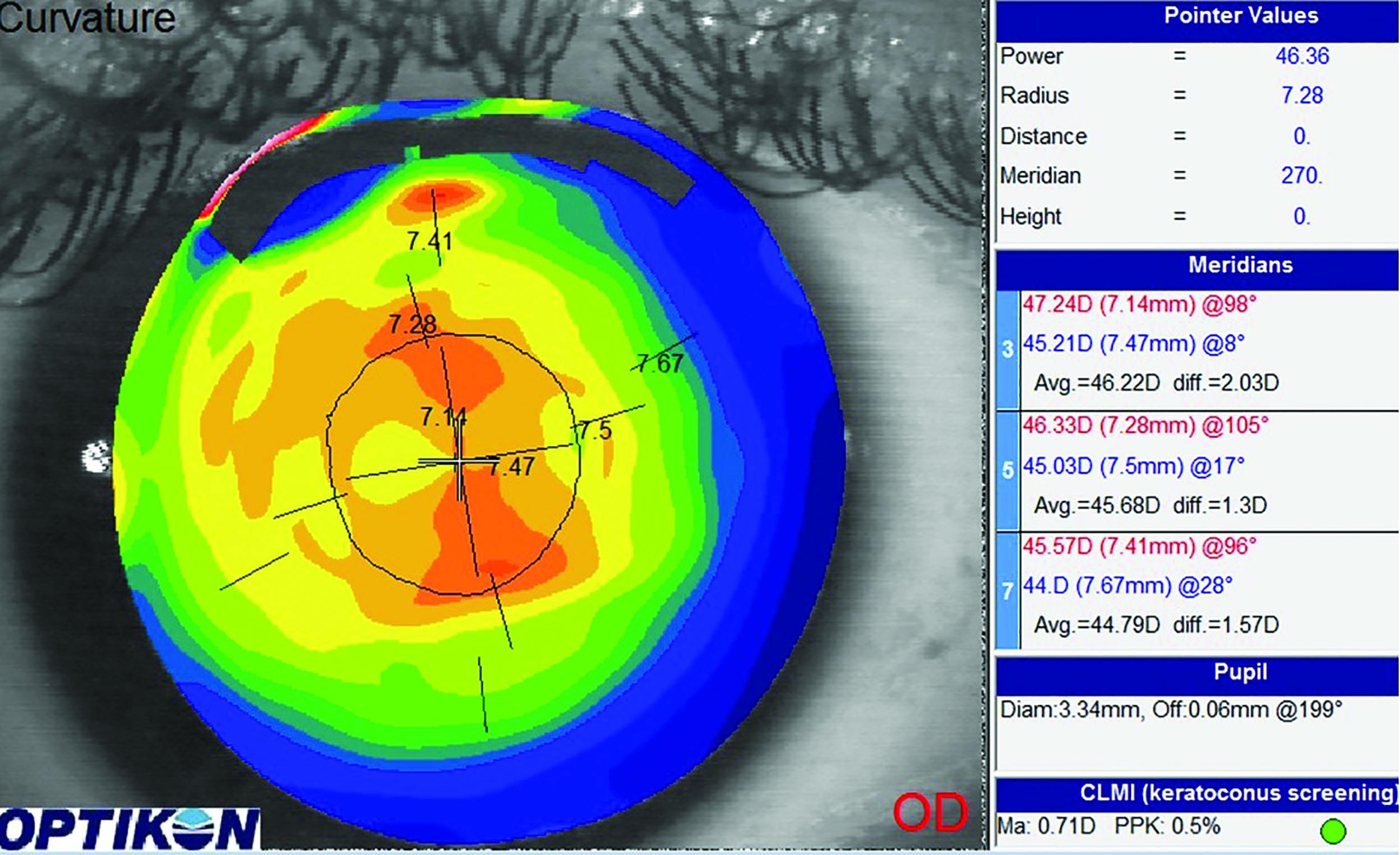 Figure 8: Topography helps to reduce contact and proximity risk in contact lens fitting
Figure 8: Topography helps to reduce contact and proximity risk in contact lens fitting
Simulated fluorescein patterns (figure 9) have been a subject of interest in recent years10 and may be a valuable tool in contact lens design, allowing adequate social distancing or even the possibility of remote assessment.
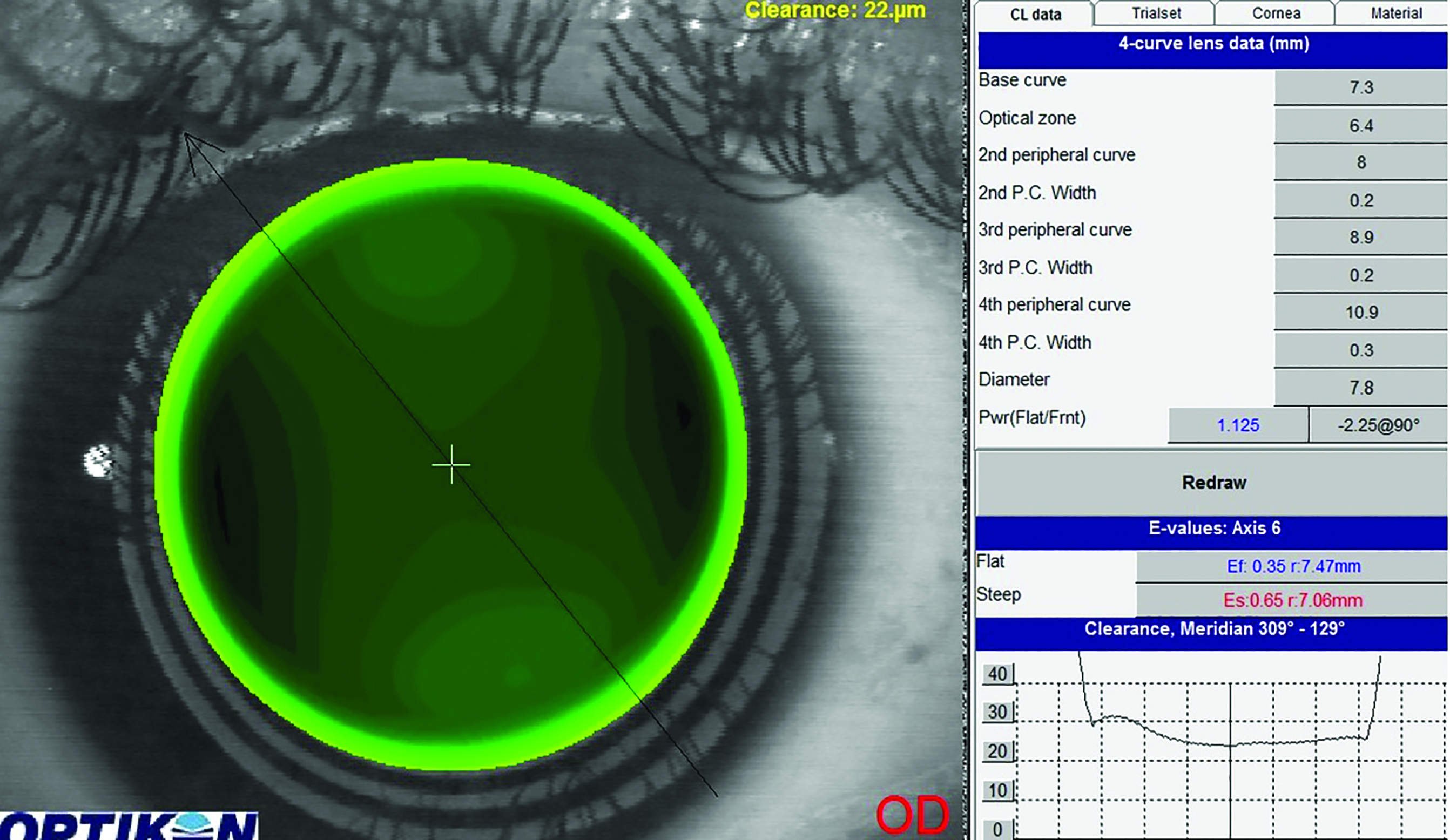 Figure 9: Simulated fluorescein patterns may be assessed and interpreted remotely
Figure 9: Simulated fluorescein patterns may be assessed and interpreted remotely
Contact lens teaching
Considerable debate, and some trepidation, exists concerning the subject of face-to-face contact lens tuition sessions. Guidance and advice, to date, is to maintain a 2m separation distance during the routine. This may prove difficult and the appropriate use of video tutorials, both before and during an appointment, is a useful innovation which may reduce both time and proximity with any given patient.
A short video, of a maximum duration of five minutes, may easily be sent via an email link to a patient for familiarisation pre-appointment. The same video may be displayed on a repeating loop for reference and allows the patient to still enjoy full guidance and supervision from a staff member at an acceptable distance.
Full instructions on cleaning, maintenance and wearing patterns may be delivered by exactly the same medium, with additional written instruction to be issued on satisfactory completion of the programme.
Video slit lamps
The use of innovative technology has a significant part to play in maintaining a 1m plus distance. A full range and variety of slit lamp modification was discussed in our first article (Optician 05.06.20) and this abstract modification has proven to be a popular method, not only of maintaining a 1m distance, but also by negating the need for mask or visor removal when operating the instrument.
That said, remember this important point – please ensure that any slit lamp modification does not invalidate any guarantees in place.
‘Bolt on’ slit lamp video cameras will have no effect on the base instrument and an imaginative adjustment of working style (at greater than 1m, with full PPE intact) is an easily implemented adaptation from well-established practice. Currently, 34% of German practitioners, in a country demonstrating one of the highest levels of Covid-19 containment in Europe, are using the technology provided by video imaging slit lamps.
Virus Testing
From June 1, Manchester University Hospitals NHS Trust introduced and developed a pilot programme which was undertaken at Manchester Royal Eye Hospital, whereby all healthcare workers are swab-tested on a weekly basis for the Covid-19 antigen (figure 10). This is an indicator of the presence of a current and contagious level of the virus. The tests are repeated on a weekly basis and all workers demonstrating positive Covid-19 test results are immediately quarantined for a period of seven days. 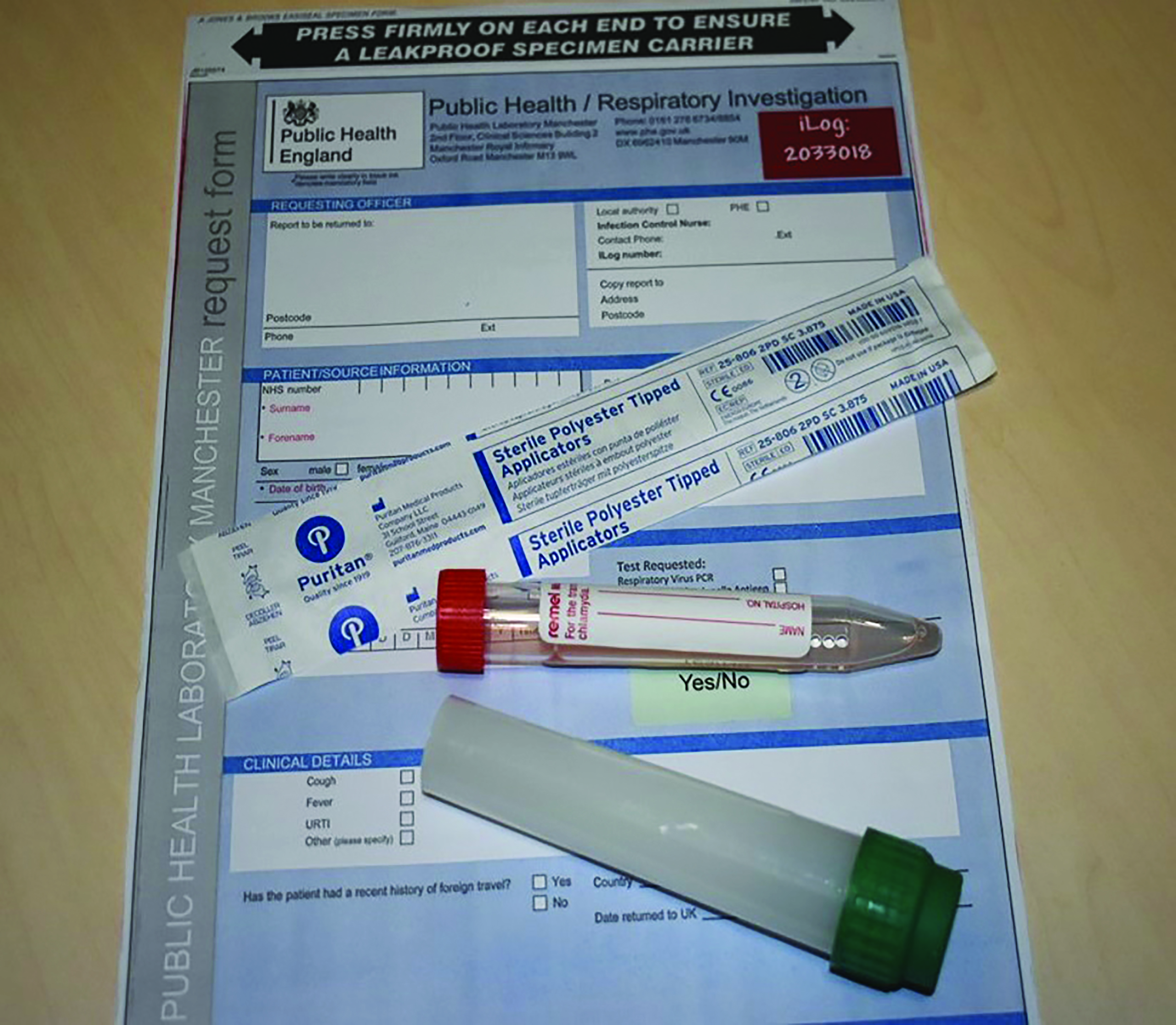 Figure 10: Antigen testing is carried out weekly at the Manchester Royal Eye Hospital
Figure 10: Antigen testing is carried out weekly at the Manchester Royal Eye Hospital
Any hospital workers or colleagues who have failed to complete the required distancing regulations are also quarantined for a period of 14 days. The size and impact of extensive quarantine measures on any working team may have a significant impact upon the ability of a department to function with any degree of efficiency or safety. In effect, it is possible to lose an entire team of professionals or support staff if strict compliance with social and professional distancing and proximity guidelines is not maintained.
Test, track and trace technology is being introduced to the general public in the UK in line with these measures and, one hopes, will result in parallel quarantine type control. This is a new way of life.
From 15th June, a testing programme was introduced at East Lancashire NHS Trust (Blackburn and Burnley Hospitals) for the Covid-19 antibody (figure 11). This blood test will quickly determine whether the individual has been exposed to the virus, and managed to recover. Community practices may want to consider a similar testing programme as an appropriate measure as part of their ‘back to work’ risk assessment.
 Figure 11: Blood testing for antibodies in Blackburn and Burnley
Figure 11: Blood testing for antibodies in Blackburn and Burnley
Germany introduced an extensive swab testing programme at the start of the pandemic. Social distancing rules were fixed at 1.5m and enforced by the police and Ordnungsamt (municipal police with fewer powers than the general police force), civil servants and local council employees. Their directive is to look after and care for the well-being and safety of German citizens.
All additional tests and measures should help to reassure patients that all possible precautions and actions are being taken to ensure the comfort and safety of a Covid-19 free environment.
Emotional impact on patients and staff
The emotional and psychological impact of Covid-19 is, as yet, an unknown entity but should not to be underestimated. Some patients are already indicating their high levels of anxiety and stress when visiting clinical settings, and practitioners too will inevitably suffer once the dust settles, to a greater or lesser extent. Public Health England has recognised the enormity of the impact of mental stress and has launched their Every Mind Matters platform. This offers advice focused upon looking after people’s mental wellbeing during the pandemic and can be found at www.nhs.uk/oneyou/every-mind-matters.
Actions to Consider
Think bigger – consider the following steps:
- Distancing. Think bigger. As far as possible, patients should be assessed and managed remotely. Remember, patients who cannot be managed remotely will require a face-to-face appointment. The CoO, FODO, ABDO and the AOP have issued a collaborative and typical validated form for completing remote contact lens consultations.11
- Social and professional distancing. Think bigger, at all times and with a keen eye on the duration of contact. Risk is a function of proximity + time + environment.
- Policing and diligence. Think bigger. A greater level of awareness, diligence and discipline. Think hard and stay on track. No deviations.
- Dimensions. Think bigger. Bigger consulting rooms, bigger retail areas, bigger displays, bigger waiting rooms (figure 12).
- Diary. Think bigger. Greater capacity. Increased number of hours, increased number of days, increased number of shifts per day, and greater time allowance for disinfection between appointments.
- Disinfection. Think bigger.
 Figure 12: Waiting rooms should allow maximum separation
Figure 12: Waiting rooms should allow maximum separation
Conclusion
Covid-19 has changed the world. The precise level of necessary adaptations and their impact have yet to be fully determined or documented. No single action or cultural or behavioural pattern change has yet proven to be 100% effective. Nonetheless, there are signs that a collective and collaborative approach is resulting in an encouraging level of containment success.
Final thought
Three men in a boat set sail in an attempt to identify and tame the shark. Their belief that nature ought to conform to man’s needs was ultimately naïve and they should have been more realistic in their expectations, more pragmatic and flexible in their preparations. A combination of law enforcement, science, and a brave, if at times reckless, captain eventually won the day. But not all returned to dry land. •
* The authors wish to note that the Covid-19 emergency is both fluid and dynamic. All protection measures and statistics are considered to be correct at time of writing.
Nick Howard is a specialty Contact Lens Optician working in two East Lancashire NHS hospitals. He is a BCLA Fellow and current BCLA Council member and has lectured widely on complex contact lenses and ocular surface disease in the UK, Europe, Middle East and Far East.
Dr Cindy Tromans is a Consultant Optometrist and Head of Optometry Services at Manchester Royal Eye Hospital, where she specialises in complex and therapeutic contact lenses and emergency eye care. She is also President of the European Council of Optometry and Optics and a Director of the World Council of Optometry.
References
- https://www.college-optometrists.org/uploads/assets/467d55b0-3c4c-41b4-9d708b627c122ffa/dab1e074-d76e-44f0-8a6c5bda30b0d2e5/Covid-19-traffic-light-guidance-table.pdf
- https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak 5 June 2020
- https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/893320/Covid-19_Infection_prevention_and_control_guidance_complete.pdf 18 June 2020
- https://www.bbc.co.uk/news/science-environment-52522460
- Derek K Chu, Elie A Akl, Stephanie Duda, Karla Solo, Sally Yaacoub, Holger J Schünemann, on behalf of the Covid-19 Systematic Urgent Review Group Effort (SURGE) study authors* Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and Covid-19: a systematic review and meta-analysis www.thelancet.com Published online June 1, 2020 https://doi.org/10.1016/S0140-6736(20)31142-9
- Bavel, JJV, Baicker, K, Boggio, PS et al. Using social and behavioural science to support Covid-19 pandemic response. Nat Hum Behav 4, 460–471 (2020). https://doi.org/10.1038/s41562-020-0884-z
- https://www.aao.org/clinical-video/infection-control-measures-during-simulated-slit-l 3 June 2020
- Barnett M, In office Contact Lens Disinfection. Contact Lens Spectrum, Volume: 35, Issue: January 2020, page(s): 17
- Kojima R and Caroline P (2009) Designing GPs from Corneal Topography. Contact Lens Spectrum October 2009
- Bhatoa, Hau S, Ehrlich D (2010) A comparison of a topography-based rigid gas permeable contact lens design with a conventionally fitted lens in patients with keratoconus. Cont Lens Anterior Eye 33(3):128-35
- https://www.abdo.org.uk/wp-content/uploads/2020/03/Contact-lens-telephone-review-form_FILL2.pdf
