The health of the cornea is of the utmost importance in both the management of dry eye and in contact lens (CL) wear. The aim in both situations is always to maintain the homeostasis of the tear film. The following requirements need always to be met for healthy contact lens wear:
- Oxygen must be able to reach the anterior cornea through the tear film and the CL
- A stable tear film must be maintained
- A healthy glycocalyx layer must be present to prevent infections and dryness1
The tear film divides into two parts when a CL is applied to the eye; the pre-lens and the post-lens tear film. There is a decreased aqueous layer thickness in the pre-lens tear film.2 This difference is due partly to the wettability of the cornea being greater than that of most CL surfaces, so tears are less easily dispersed over the pre-lens area. Depending on the lens thickness, the pre-lens tear film may sometimes be too thin to spread effectively across the entire CL surface. This results in an unstable and fragile pre-lens tear film, leading to more friction between the CL and the adjacent ocular surface, the tarsal conjunctiva. This is a cause of CL discomfort (CLD).2
CL wearers discontinue wearing lenses for many different reasons, including several which fall under the heading of CLD.2 Though many studies reflect this wide variety of reasons for discontinuation of CL wear, most agree that poor comfort is most important. One of the causes for poor comfort is CL-associated dry eye. This may sound a simple conclusion to make but, in reality, it is not. CL-associated dry eye is multifactorial. It would be nice if there was just one sign or test to confirm this diagnosis, but sadly this is not so.3
In CL practice, each patient is unique and experiences dry eye differently. One large study, working with 200 symptomatic lens wearers, found a widely diverse set of clinical presentations, together with a range of factors for the CL-related dryness. This was even the case among wearers with the same underlying diagnosis.4 Identifying causes for any discomfort and then selecting the appropriate management strategy will need to be tailor-made for each patient. Therefore, it is very important to start with a good patient history and symptoms and evaluation. Asking the right questions and undertaking the relevant examinations will lead to the best management for each patient. And fewer
dropouts.
So, the big question has to be, is the dry eye due to the CL or are there one or more reasons for it? Knowing this should lead to the right management decision and strategy.
What is Contact Lens Discomfort (CLD)?
When discussing CL use and dry eye, one first needs to remember that, while there have already been many papers written and studies undertaken, there is still much to learn in order to fill the many gaps in our knowledge of this subject. The term CLD obviously indicates that it has something to do with wearing CLs. However, we should not assume that the CL itself is the cause of the discomfort during wear.
When looking at how CLs and dry eye are related, we first need some kind of definition to explain CL related dry eye. Let us consider the Tear Film and Ocular Surface Society (TFOS) workshop findings and what they say about CLD?5 While there was no agreement on a standard, single definition for CLD, there was some consensus on what the problem actually is. TFOS defined CLD as follows:
‘Contact lens discomfort is a condition characterised by episodic or persistent adverse ocular sensations related to lens wear, either with or without visual disturbance, resulting from reduced compatibility between the contact lens and the ocular environment, which can lead to decreased wearing time and discontinuation of contact lens wear.’
The most likely outcome associated with CLD is not necessarily clinical. It is, rather, that the CL wearer reduces their wearing time and wear frequency, and in some cases, ultimately drops out of CL wear altogether. In order to prevent this situation, we first need to know what the cause of their discomfort is. Possible influences include the following:5
- Contact lens material properties; these include surface friction, wettability and oxygen permeability
- Contact lens design factors; these include back surface geometry (not only the base curve or base curve equivalent), lens diameter, power distribution, power range and edge design
- Wearing environment; influences here include pollution levels and nature, air-conditioning, computer and digital display usage
- Medication
- Non-modifiable risk factors; including age, gender and ethnicity
- Ocular environment; this includes factors such as meibomian gland dysfunction (MGD) discussed
Considering the Ocular Environment
Examinations that we perform as part of the regular aftercare visit allow us to identify clinically detectable changes that might contribute to a less than optimal ocular environment. When appraising CLD presentations, key assessments include assessment of the
following:
- Conjunctival staining (figure 1)
- Conjunctival epithelial flap formation
- Lid parallel conjunctival folds (LIPCOF, figure 2)
- Lid wiper epitheliopathy (LWE, figure 3)
- Conjunctival indentation
- Meibomian gland dysfunction (MGD, figure 4)
- Demodex blepharitis (figure 5)
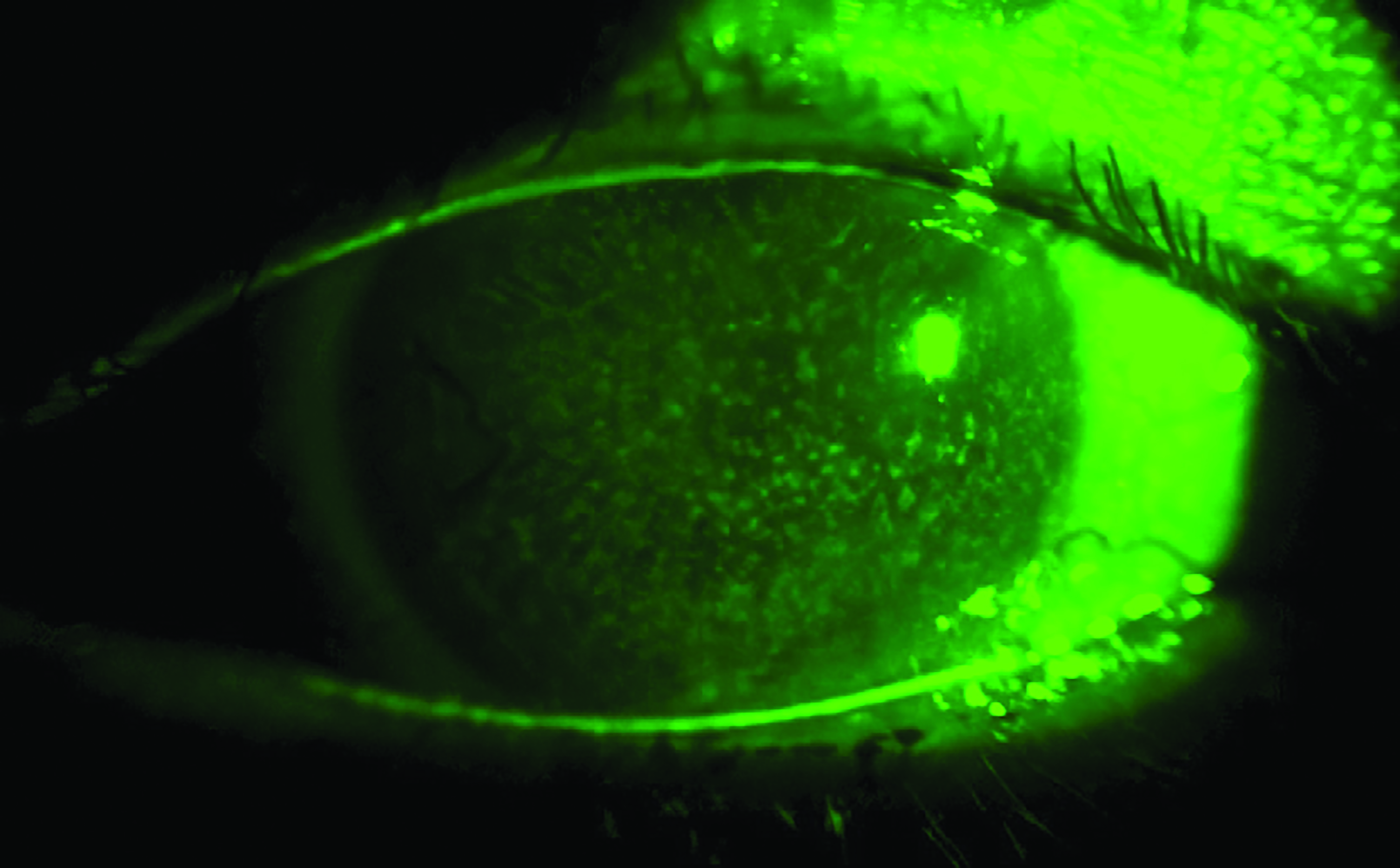 Figure 1: Conjunctival staining (figure enhanced using the AOS system)
Figure 1: Conjunctival staining (figure enhanced using the AOS system)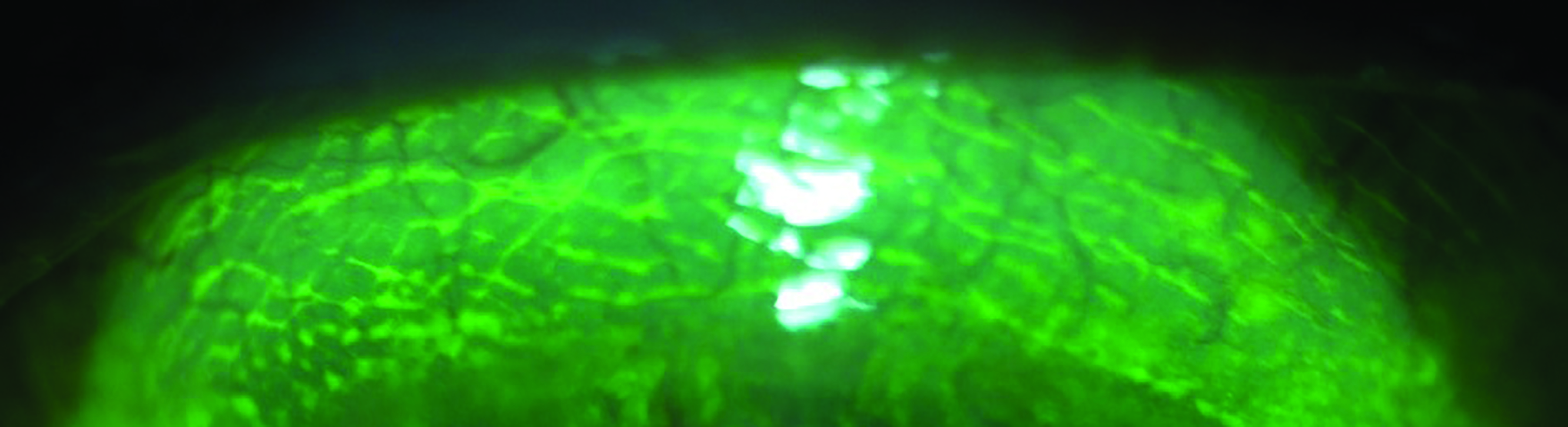 Figure 2: Lid parallel conjunctival folds
Figure 2: Lid parallel conjunctival folds 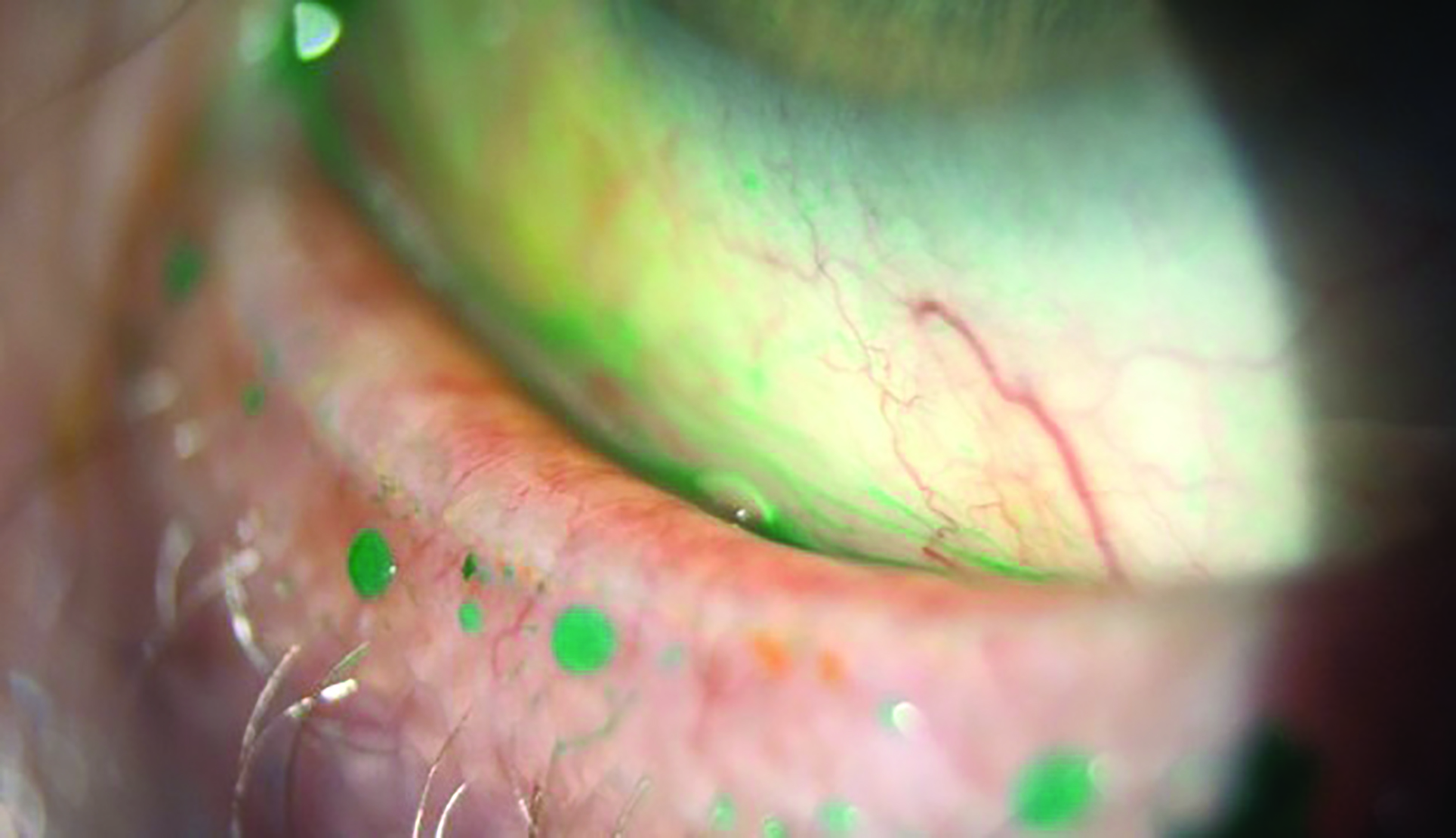 Figure 3: Lid wiper epitheliopathy (figure from Sarah Farrant)
Figure 3: Lid wiper epitheliopathy (figure from Sarah Farrant)  Figure 4: Meibomian gland dysfunction (figure from Sarah Farrant)
Figure 4: Meibomian gland dysfunction (figure from Sarah Farrant) 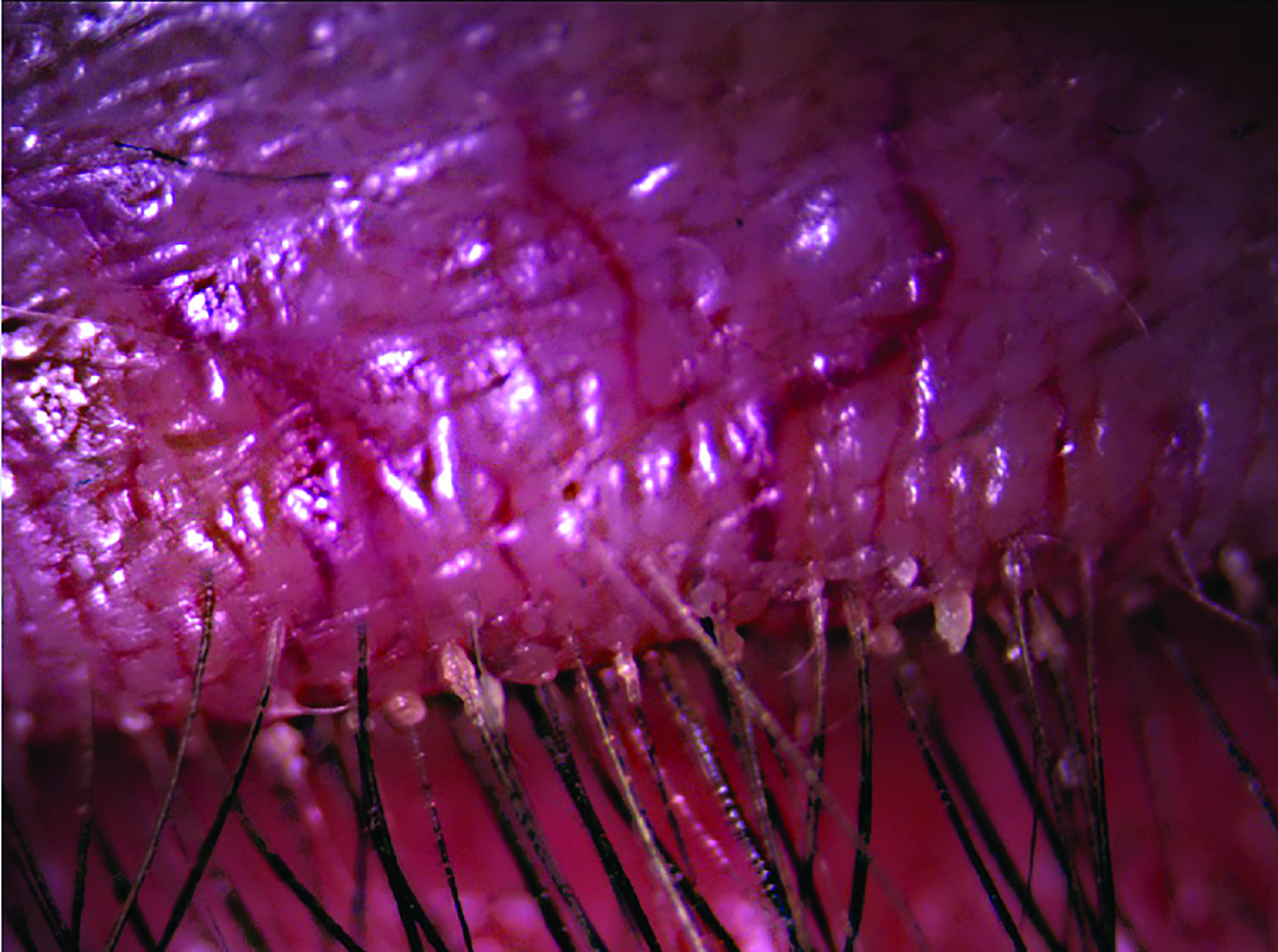 Figure 5: Demodex blepharitis (figure from Dr S Doshi using AOS software)
Figure 5: Demodex blepharitis (figure from Dr S Doshi using AOS software)
Because CLD is multifactorial, one needs a wide range of assessment techniques.4,6 The most important instrument for CL examinations is, obviously, the slit lamp with its capability for both macro and micro review of the anterior eye and adnexa. However, to be able to find the cause of dry eye and or CL-related dry eye, a variety of supplementary examinations, tests or measurements also need to be considered.1,7 These are, in no particular order:
- Symptomatology questionnaire; such as the OSDI (figure 6)
- Eyelid margin and lash assessment with white light; findings such as blepharitis need grading (figure 7)
- Blink patterns; frequency and integrity of blinking is important and many video capture software systems may accurately measure these (figure 8)
- Conjunctival and corneal white light assessment; helps identify, for example, LIPCOFs, tear debris and corneal scars
- Meibomian gland expression; expressability and quality of meibum to be noted
- Corneal and conjunctival staining (fluorescein / lissamine green); aids identification of desiccation or lid wiper epitheliopathy
- Interferometry; lipid layer thickness and integrity may be gauged (figure 9)
- Invasive (with fluorescein) or non-invasive tear film break up time (TBUT); again, modern software assists here (figure 10)
- Tear meniscus height (figure 11)
- Schirmer Test or Phenol red thread test
- Tearfilm osmolarity (figure 12)
- Meibography (figure 13)
This should identify an ocular cause, such as MGD, and remediation should address the problem.
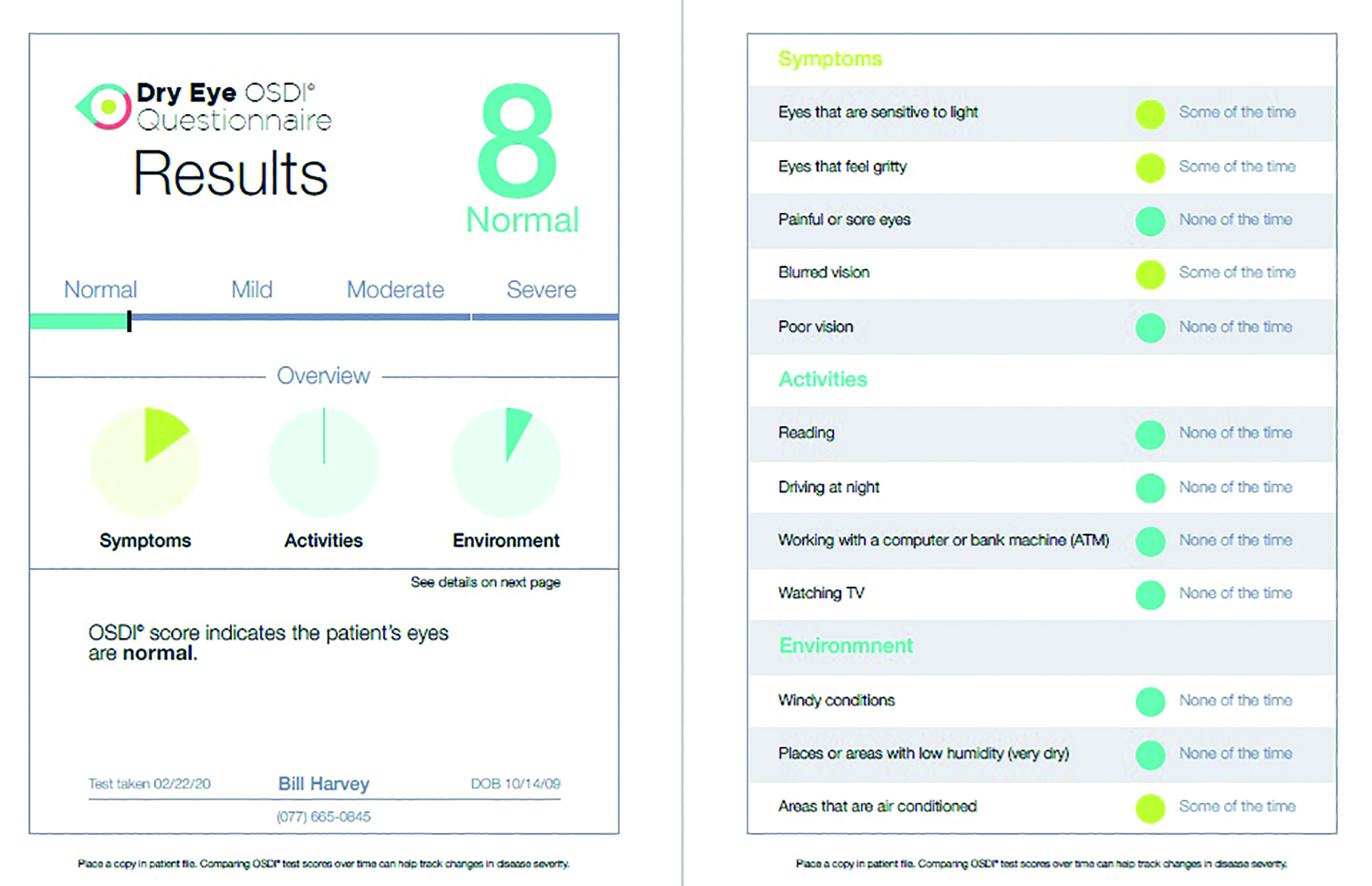 Figure 6: OSDI questionnaire
Figure 6: OSDI questionnaire
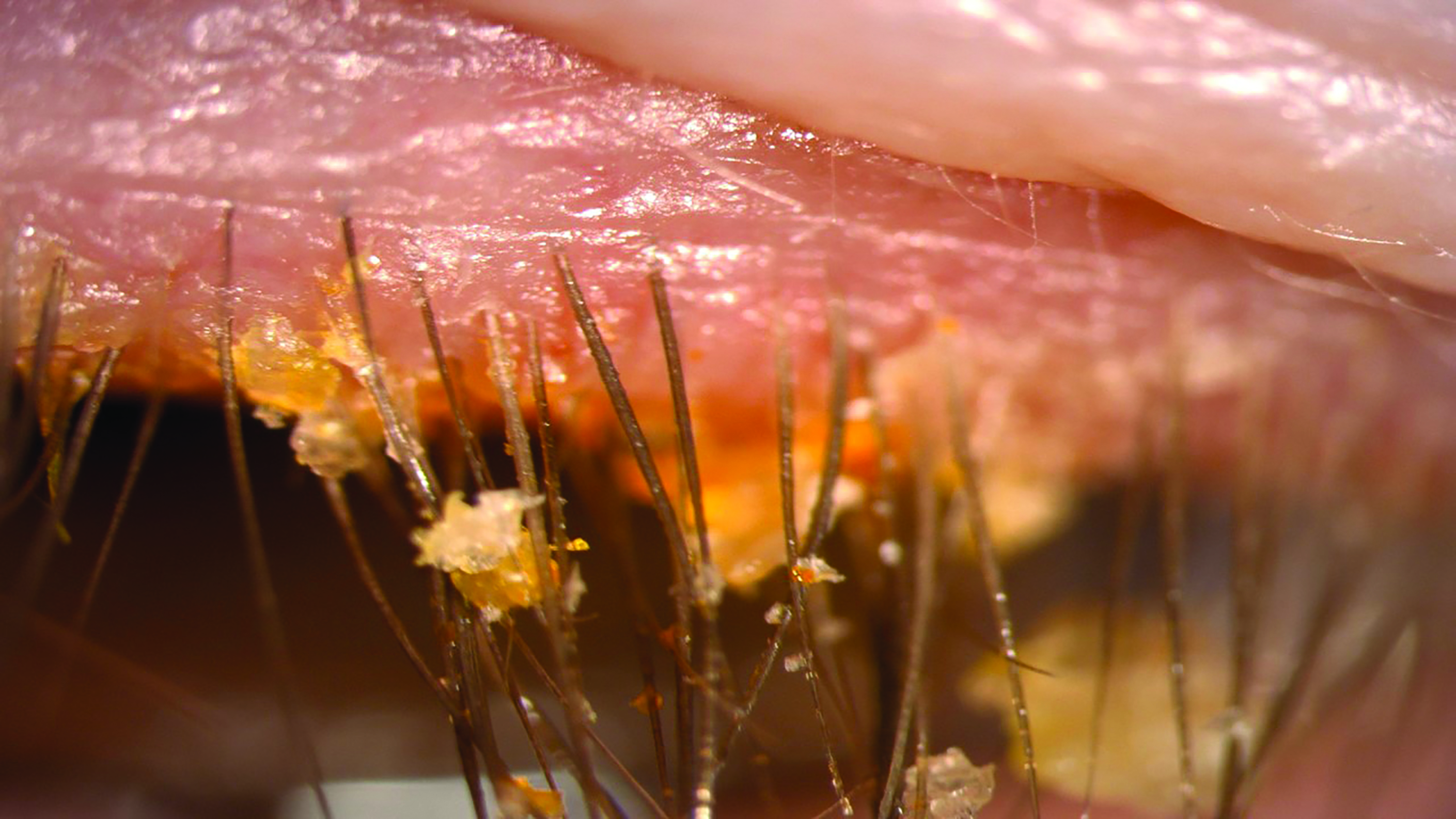 Figure 7: Blepharitis (figure from Sarah Farrant)
Figure 7: Blepharitis (figure from Sarah Farrant) 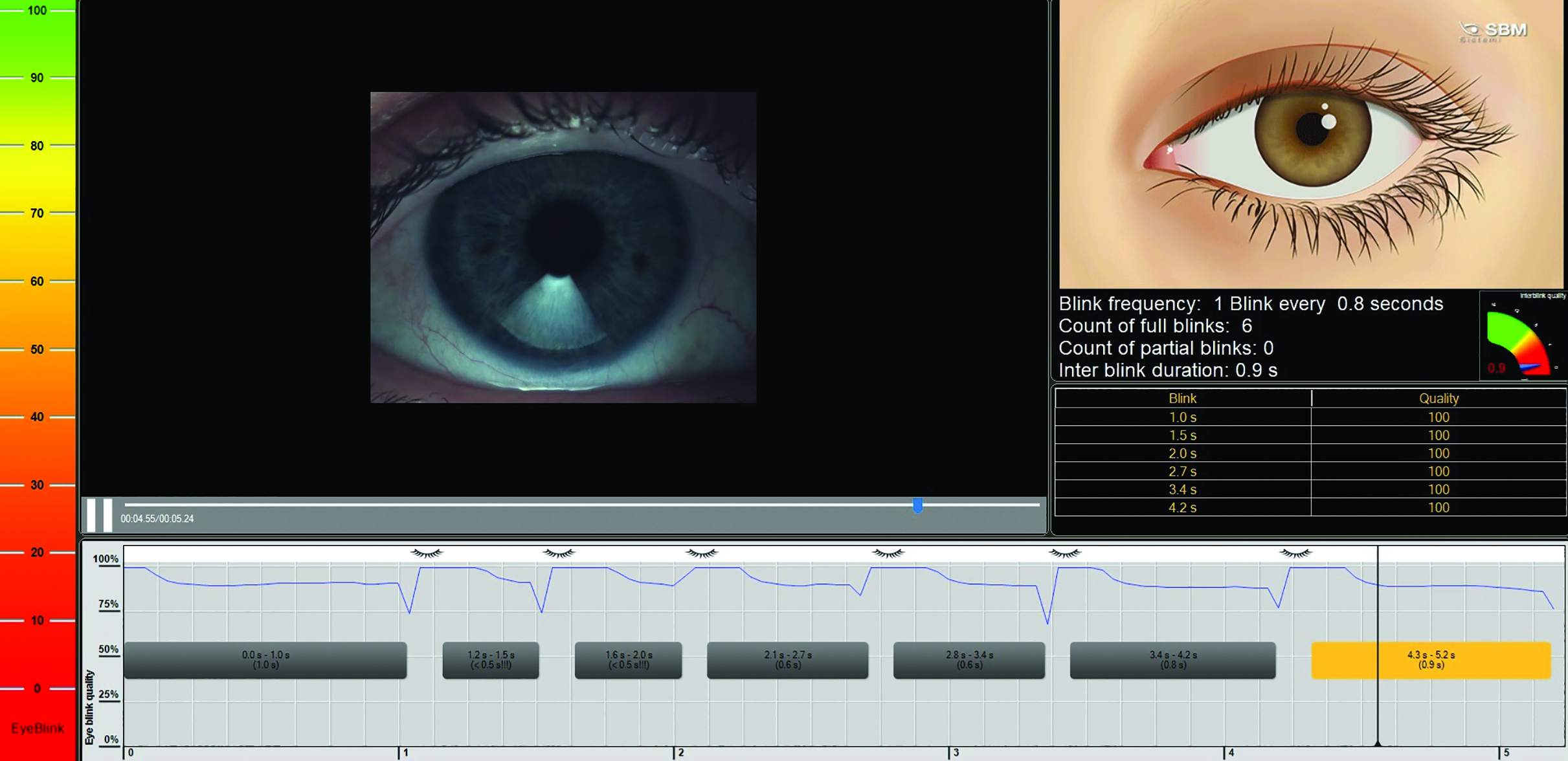 Figure 8: Blink analysis using the IDRA system
Figure 8: Blink analysis using the IDRA system
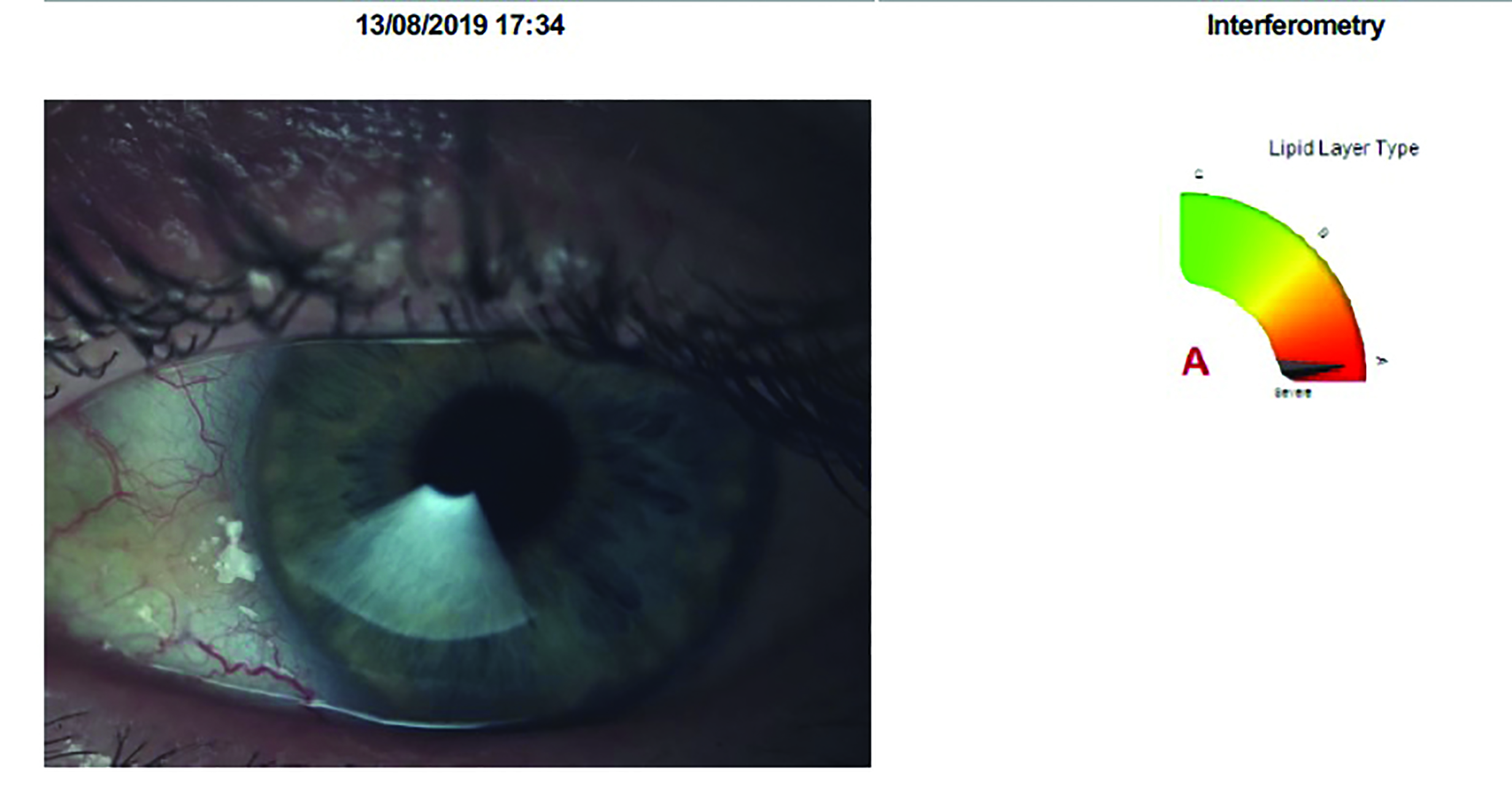 Figure 9: Interferometry using the IDRA system
Figure 9: Interferometry using the IDRA system
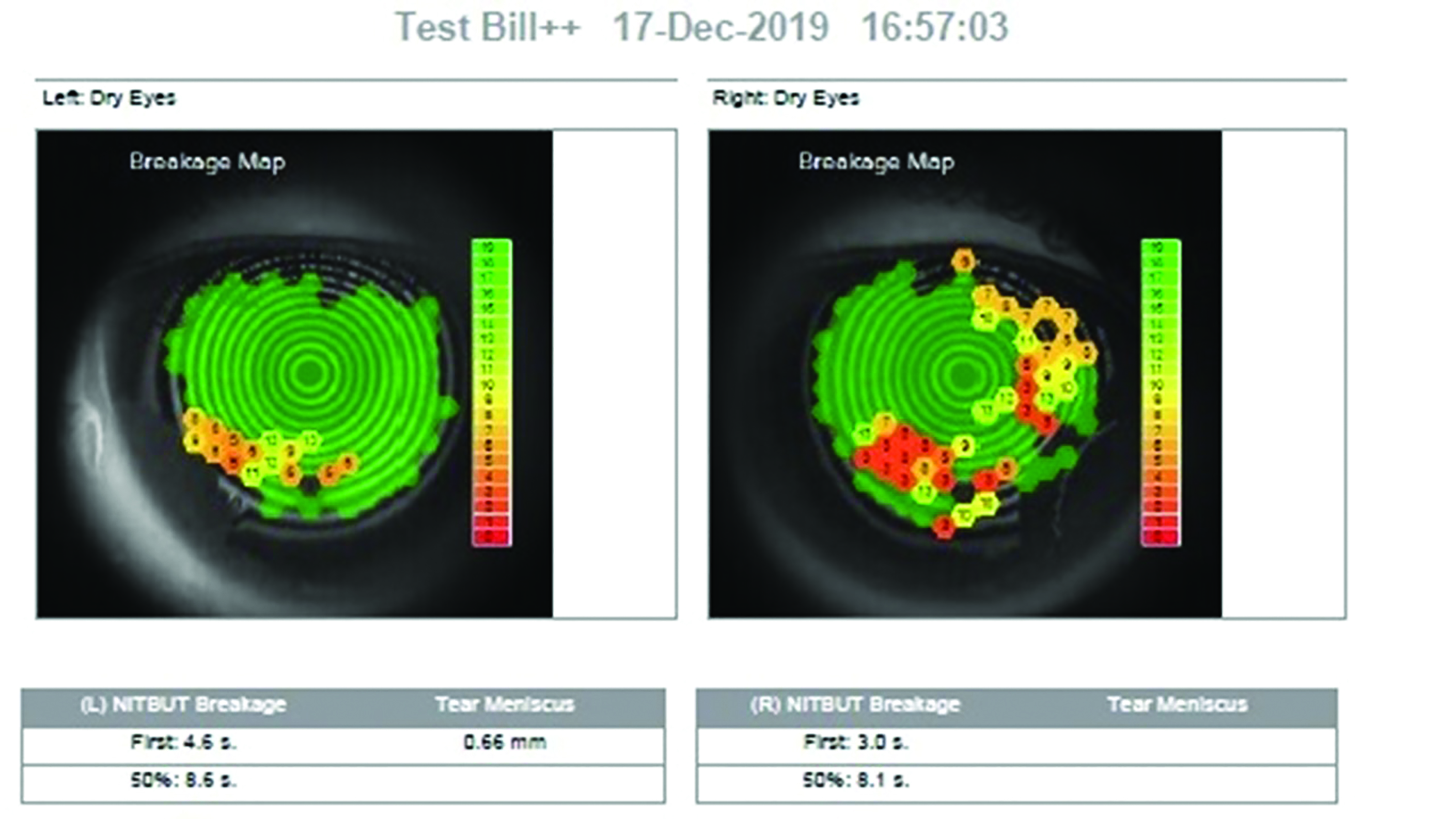
Figure 10: Tear film break up time (TBUT) measurement with the Visionix 120+ system
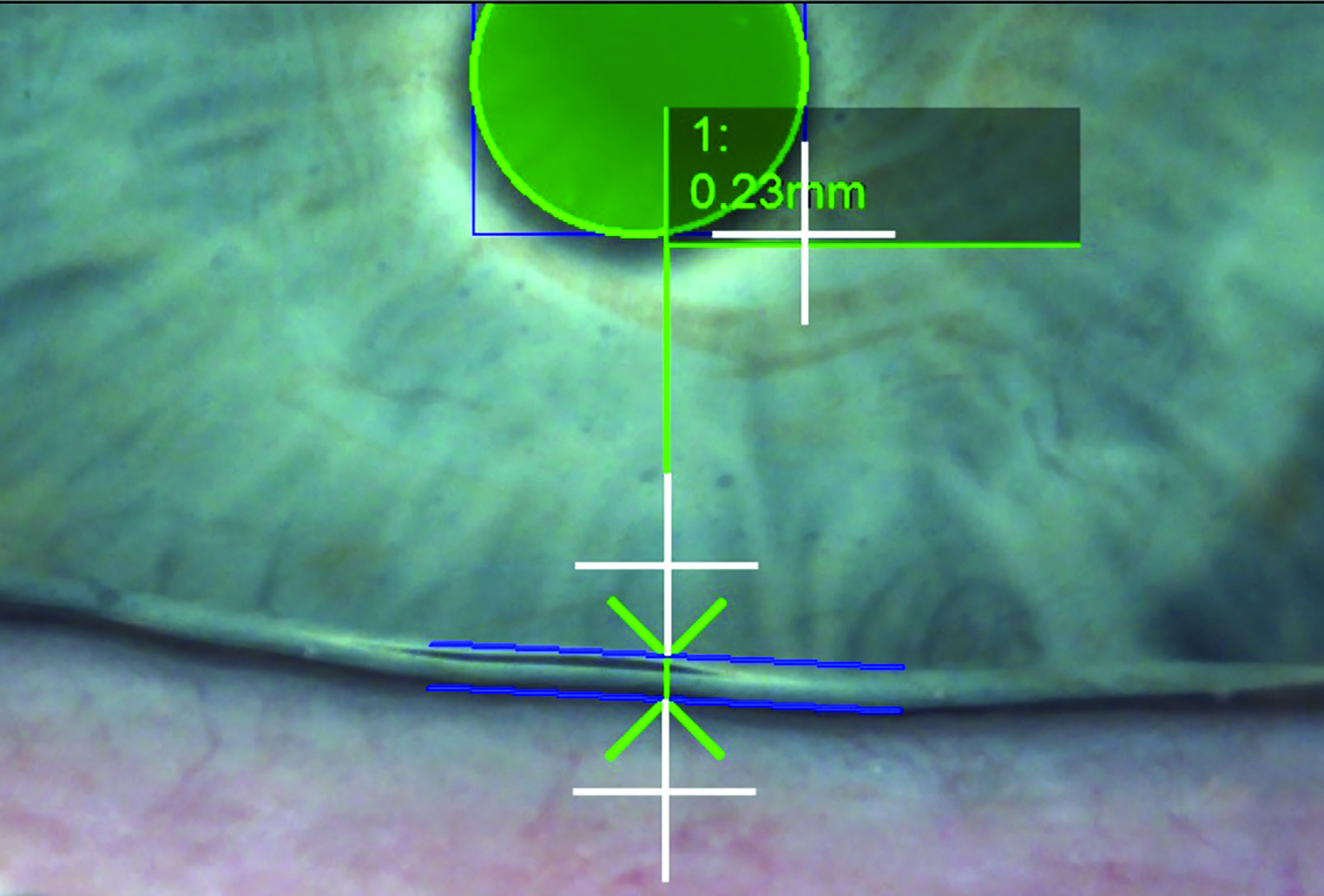
Figure 11: Tear meniscus height using the IDRA system
 Figure 12: Tearfilm osmolarity with the TearLab
Figure 12: Tearfilm osmolarity with the TearLab
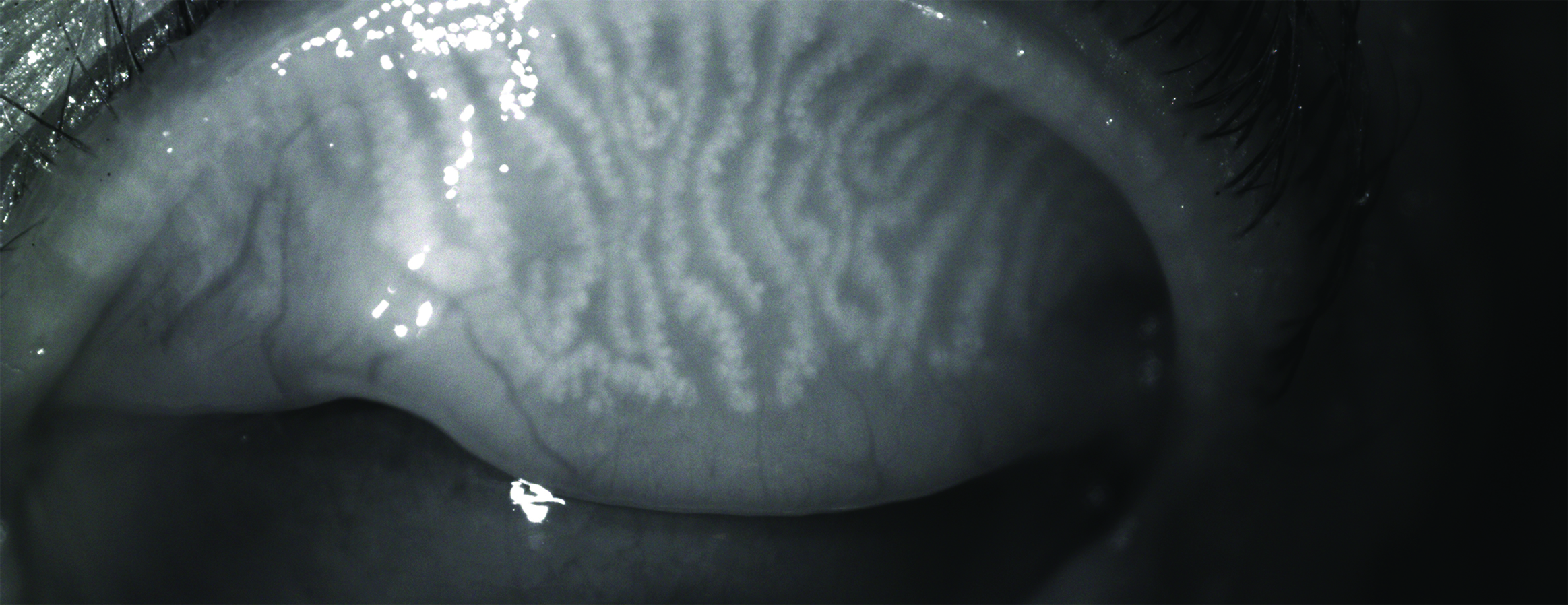 Figure 13: Meibography of the everted upper lid
Figure 13: Meibography of the everted upper lid
Considering Contact Lens Factors
We also need to look at CL-related influences, and in particular:
- Fit of the lenses; centration and movement
- Pre-lens tear film quality
- Corneal and conjunctival staining; after lens removal
- Solution sensitivity; where appropriate
- Compliance
Addressing any concerns found should help alleviate the problem.
If done well, it is possible one can find the cause or causes of the CLD. Still we see many clinical presentations in those patients with the same diagnoses of CLD. What are the most important features to look for? From my years in CL practice, I found that a comprehensive history and symptoms is powerful in uncovering what is happening. It is just as important to consider what your patient tells you as what they do not. Remember, some symptoms may be thought to be normal by a patient, for example some grittiness when viewing a computer screen, and so will not mention this unless specifically asked. Asking ‘are your eyes gritty?’ and ‘at what times do you notice grittiness?’ will usually elicit different responses from the same patient. This will be considered in greater detail in a forthcoming CET article on this subject.
You need to be a good detective in assessing CLD. You may find that what the patient experiences is not always what the examinations and clinical presentations tell you. Indeed, symptoms unrelated to signs or indeed signs without symptoms are both situations highlighted in the TFOS DEWS2 workshop. For example, you may find a lot of staining on the cornea while the patient has only minor symptoms. This may not be in line with the literature.3,5
Is the Contact Lens Always the Cause?
Which comes first; the chicken or the egg?
Likewise, is it always the CL that is the cause of CLD or was there a dry eye condition established before lens wear commenced? Did the CL trigger the dry eye or simply highlight an existing problem? Is there a completely different cause for the dry eye, such as new medications for example? Following this logic, if there is an underlying cause to the dry eye, it does not follow that changing the CL should be the first thing to do?
So how and when to treat CLD? Many dry eye interest groups around the world ‘have an eye’ on this question. In Japan, the Dry Eye Society advises firstly to do tear film-orientated treatment. They talk about contact lens associated dry eye disease (CLADE) more than CLD as they see CLD often being associated with an underlying dry eye disease.2
We have already discussed that regular CL checks with appropriate examinations, questioning and measurements can, in many cases, help prevent CL dropout. During my time in practice, I saw many people self-diagnosing that they have dry eyes and therefore assuming they cannot wear contact lenses.
Most people think that all CL materials are the same or similar and this extends to the CL care systems. Sometimes, patients return to a practice for new spectacles, telling that they cannot wear CLs anymore. In the mind of the ex-wearer, CL wear is no longer possible; but is this really the case? It is well within the capability of the clinician to make CL wear possible for them again. Where the concern has been primarily one with the lenses themselves, more modern materials may be the answer to their prayers. Many are willing to update their CL material if presented with the idea of resuming CL wear or extending their CL wear. And this may be facilitated by careful revision of their care system and regime.
As CLD is often multifactorial, it is important to see what factors may be addressed for each patient. Which are modifiable, or not? Some patient factors are non-modifiable, such as age, gender. Others may be addressed either directly, such as associated skin diseases like rosacea that may respond well to treatment or referral, or indirectly, perhaps by another medical professional, such as usage of some medication where there may be an effective alternative with a different adverse profile.
Many CLD risk factors are modifiable, at least to some degree, and include environmental factors like change of office and humidity, usage of screens or sick building syndrome. Ocular concerns, such as MGD, usually respond well to intervention. Always, patient compliance with instruction should be a consideration.
Some factors assumed to influence CLD are yet to have an established evidence base confirming such. These include smoking, alcohol consumption and pregnancy.2,9 This is most likely because of difficulties in isolating the one risk factor; for example, smokers may be less compliant with other health instructions, pregnancy may affect tear flow or sleeping patterns and so on. One notable study using a questionnaire-based methodology showed that these factors do not always affect the duration of daily lens wear, but still remain a challenge. More remarkable from this study was the finding that more patients between the age of 18 and 34 had dry eye symptoms when compared to 10 years previously.10 This is most likely to reflect how modern life impacts upon the ocular surface, with our increasing viewing of screens and longer hours in managed environments.
Particular attention should be paid to diabetes, currently one of the most serious general health problems in the world. Diabetes has a major influence upon both systemic and ocular health. In diabetics, MGD, a major cause of evaporative dry eye disease, is more prevalent.11 Diabetes is also associated with progressive degeneration of the corneal nerves. This can also increase the risk of dry eye disease as well as epithelial defects, both of which may lead to CL dropout.11
In summary, it is all to easy to assume that the cause of CLD (and a dissatisfied patient) is the fit or the physical properties of the worn contact lenses. The ocular surface and other external factors play just as important a role, possibly more important.12
What If CLD Is Due to The Contact Lens?
Let us assume that all modifiable influences upon CLD not related to the contact lenses have been addressed. All that is left is to address the CL, by either modifying it or ceasing its use. Many patients may not like the latter option, even if this is the only option left. So do not disregard the option of shorter wearing times and/or reduction in wearing frequency supported with spectacle wear.
Where the patient is wearing reusable lenses (whether weekly, bi-weekly, bi-monthly, quarterly or annual replacement), changing to daily disposables is often successful. This removes the challenges of cleaning and storing with assiduous compliance, as well as any potential toxic or allergic effects from the care products themselves. Changing the care system can be effective, and clinicians and patients alike often underestimate the significance of this. And always, do not forget to explore compliance. If this can be enhanced, it should be.
It has been hypothesised that changes in osmolarity has a role to play in CLD. Garaszczuk et al stated that one of the best diagnostic tests for DED is tear osmolarity (figure 12).8 Their 12-month prospective study demonstrated that refitting patients with daily disposable CLs reduced both the tear osmolarity and ocular symptoms. An osmolarity test, however, can be costly, so making it less commonly used in everyday practice.
Today, CL wearers want longer comfortable wearing times, while at the same time doing more near work and, in many cases, remaining in a dry air environment. All of which are challenges for comfortable CL wear and can easily lead to CLD. When selecting the most appropriate CLs for these circumstances, silicone hydrogels or water gradient hydrogel daily disposables immediately come to mind. In one study that compared the lens materials delefilcon A, stenfilcon A, narafilcon A and somofilcon A, most participants preferred delefilcon A when undertaking intensive visual tasks under challenging environmental conditions. The study concluded that this lens material may be preferable for CL wearers with intensive digital device use.13 From another study that looked at CLs employing water gradient material technology, such lenses appeared to reduce CL-related dryness and allowed longer, more comfortable, wearing times for previously symptomatic CL wearers.14
Conclusion
Though we know that CLs have the potential to affect the tear film, anterior ocular surface influences are also possible reasons for CLD. We need to be mindful that a challenged ocular surface may well have pre-existed CL wear and thus be the main cause of the CLD. It is therefore essential to do good history and symptoms and relevant examination before starting to fit CLs. In situations where you do identify an ocular surface anomaly and dry eye disease, or the potential thereof, this should first be addressed before, only then, proceeding with the CL fitting.
If the eyes are found to have no dry eye issues and yet CLD occurs, one should not only think about the CLs but, in the case of reusable lenses, also about the CL care system. When considering the CL itself, understand the material, design, and the replacement frequency. In these days of social isolation where computer use is more of a challenge because of longer hours, with many online digital meetings, be mindful that people who previously were satisfied CL wearers may now not be as happy. Many will welcome an update into a new CL material or change of solution if presented with the idea of resuming or extending comfortable contact lens wear.
As contact lens practitioners, we have to ‘be alert’ and think like a detective; what is the patient telling you (symptoms) and showing you (signs), but perhaps more importantly what are they not saying or showing? Some of the best ‘medicine’ we can dispense is that which prevents problems arising. Taking a proactive approach to the management of CLD discomfort can potentially prevent it happening in the first place, or address it before the patient reduces or stops contact lens wear altogether.
Simone Stad is International Senior Manager Professional Affairs OH, Vision Care at Alcon, holds a Master of Science in Optometry from City University, London and is a Fellow of the BCLA.
- Look out for a case study illustrating some of the points raised in this article in the next Contact Lens Monthly issue of Optician.
References
- Efron, N et al. Contact lens care and ocular surface homeostasis. Contact Lens & Anterior Eye, 2013,Vol. 36, pp. S9-S13.
- Kojima, T. Contact Lens-Associated Dry Eye Disease: Recent Advances. iovs.arvojournals.org., February 4, 2020.
- Walline, J et al. Clinical Controversies: The Ocular Surface and Lens Wear. www.clspectrum.com. [Online] January 1, 2016.
- Young, G. Contact lens comfort confusion. www.clspectrum.com. [Online] July 1, 2019.
- Nichols, J et al. TFOS International Workshop on Contact Lens Discomfort: Executive summary. Investigative Ophthalmology & Visual Science, 2013, Vol. 54, pp. 1-16.
- Markoulli, M, Kolanu, S. Contact lens wear and dry eyes: challenges and solutions. Clinical Optometry, 2017, pp. 41-48.
- Nichols, J, Sinnott, L. Tear Film, Contact Lens, and Patient-Related Factors Associated with Contact Lens–Related Dry Eye. IOVS, 4, 2006, Vol. 47, pp. 1319-1328.
- Garaszczuk I et al. A 12-month Prospective Study of Tear Osmolarity in Contact Lens Wearers Refitted with Daily Disposable Soft Contact Lenses. Optometry and Vision Science, 97, 2020, pp.178-185.
- Stapleton, F et al. TFOS DEWS II Epidemiology Report. Elsevier, 2017, pp. 334-368.
- Lubis RR, Gultom, M. The Correlation between Daily Lens Wear Duration and Dry Eye Syndrome. https://www.ncbi.nlm. April 29, 2018.
- Garzon SJ et al. Correlation between type 2 diabetes, dry eye and Meibomian glands dysfunction. Journal of Optometry, 2019, pp. 256-262.
- Barnett M et al. The role of the ocular surface in contact lens wear. www.clspectrum.com. [Online] January 2, 2020.
- Guillon M et al. Qualification of contact lens wettability after prolonged visual device use under low humidity conditions. CLAE, 2019, Vol. 42.
- Bauman E et al. Evidence for benefits of water gradient spherical and multifocal lens (delefilconA) for dryness symptomatic contact lens wearers. Contact Lens and Anterior Eye, 2019,Vol. 42.
