Eye drops, ointments and gels are the mainstay of treatment for various ocular conditions because they bring the advantage of administering medication directly to the eye (figure 1). This article will focus upon the most common categories and consider their systemic side effects as documented in the available literature.
 Figure 1: Eye drops; the mainstay of eye disease treatment
Figure 1: Eye drops; the mainstay of eye disease treatment
Antibiotics
Antibiotic eye drops, gels or ointments are used to treat a large variety of eye infections, from blepharitis and conjunctivitis, to hordeolum (figure 2), keratitis, and dacryocystitis (figure 3) to mention just a few.
 Figure 2: Internal hordeolum
Figure 2: Internal hordeolum
 Figure 3: Acute dacryocystitis
Figure 3: Acute dacryocystitis
The topical antibiotics most commonly used in eye care are listed in table 1.
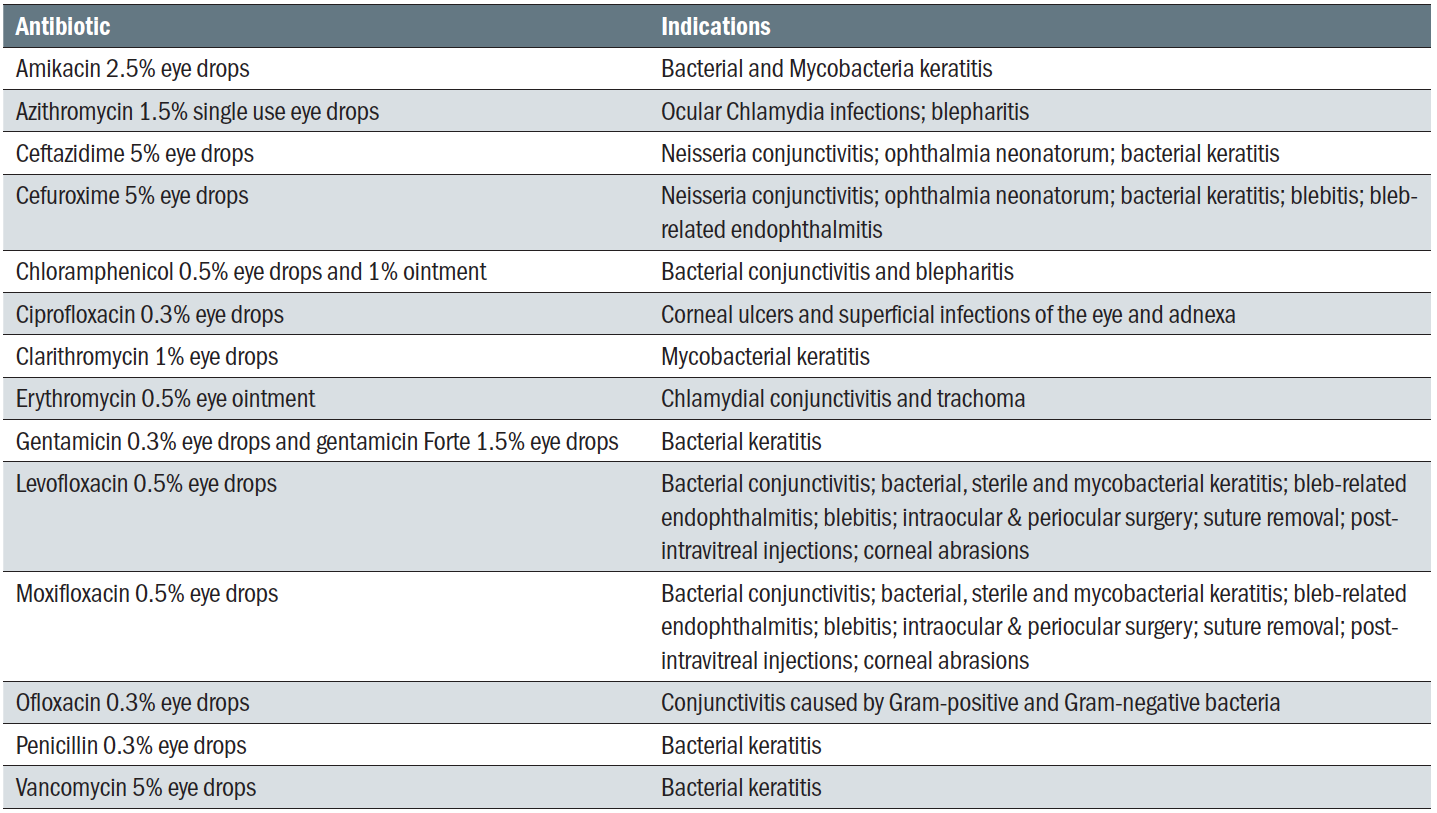 Table 1: Topical antibiotics in common use in eye care (adapted from 1)
Table 1: Topical antibiotics in common use in eye care (adapted from 1)
The effects of the few of the most commonly used will now be considered.
Chloramphenicol
Chloramphenicol (solution 0.5% and ointment 1%) is one of the most commonly used drugs for the treatment of bacterial eye infections. Chloramphenicol is usually well tolerated and is used as a first line antibiotic despite the fact that, historically, it has been associated with serious side effects such as anaphylaxis,2 blood dyscrasias, acute leukaemia, aplastic anaemia, and acute hepatitis.3 Contact dermatitis after topical administration of this drug has also been reported.4,5 In addition, there are recommendations to avoid this drug during the last weeks of pregnancy and when breastfeeding because it might cause cyanosis and hypothermia in the baby; a condition known as ‘grey baby syndrome.’6
Fluoroquinolones
Fluoroquinolones are broad spectrum antibiotics used to treat ocular infections or peri-operatively. The fluoroquinolone antibiotics available in the UK for ocular use are:
- Ciprofloxacin
- Ofloxacin
- Levofloxacin7
- Moxifloxacin
Ciprofloxacin (Ciloxan drops, 0.3%) is indicated for the treatment of corneal ulcers and superficial infections of the eye and adnexa (figure 4). Plasma levels of ciprofloxacin in human subjects, following two drops of 0.3% ciprofloxacin solution every two hours for two days and then every four hours for five days, ranged from non-quantifiable (<1.0ng/mL) to 4.7ng/mL, 450-fold less than that seen following a single oral dose of 250mg ciprofloxacin.7 Nevertheless, systemic side effects after treatment with Ciloxan can occur, and range from hypersensitivity and dermatitis, to headache, dizziness, nausea, diarrhoea, abdominal pain and ear pain.
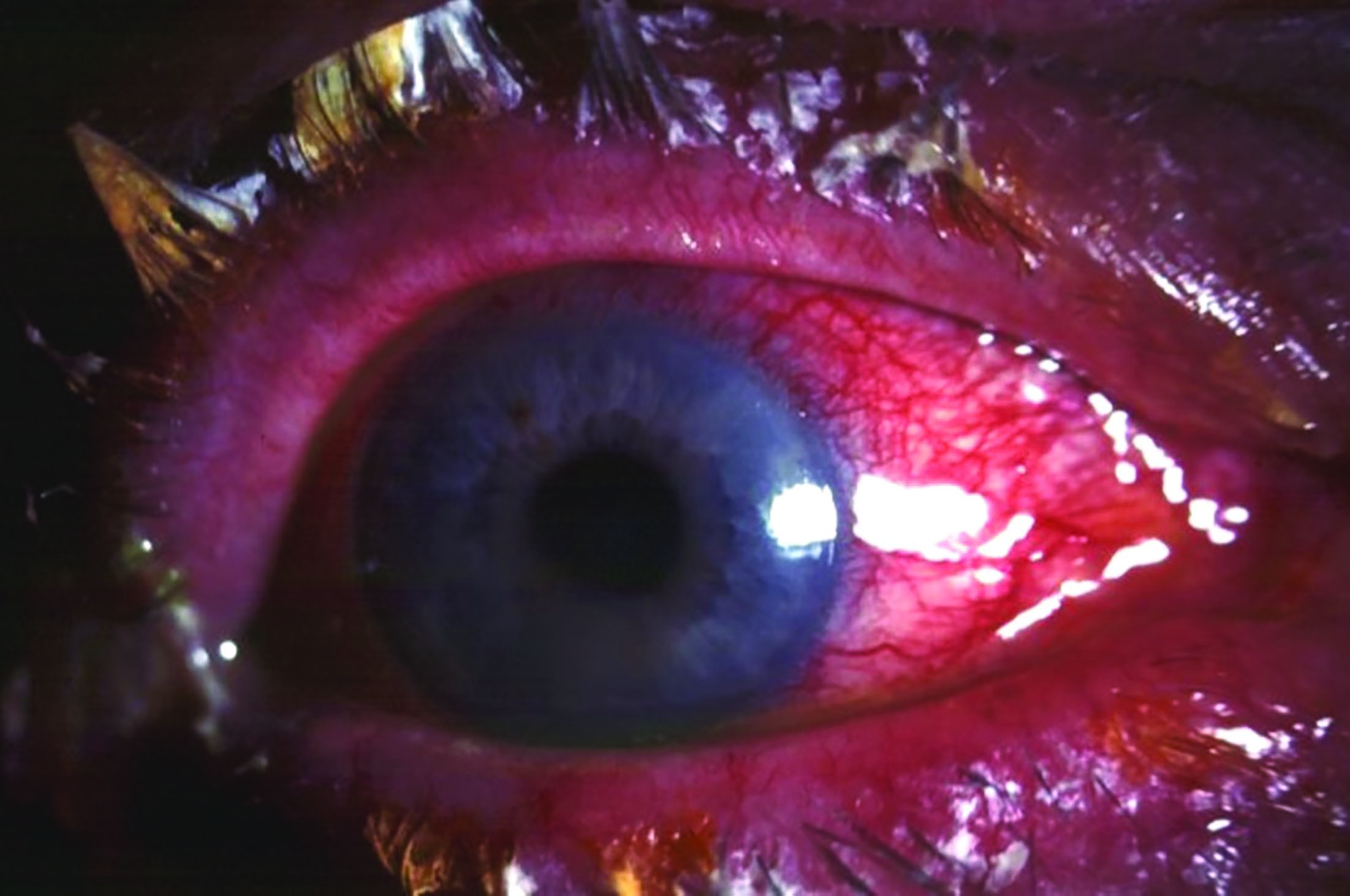 Figure 4: Acute bacterial conjunctivitis
Figure 4: Acute bacterial conjunctivitis
Ofloxacin (Exocin drops, 0.3%) is recommended in conjunctivitis caused by a large number of Gram-positive and Gram-negative bacteria. Systemic side effects after the use of this drug are rare. However, severe hypersensitivity reactions (angioedema, dyspnoea, anaphylactic reaction/shock, oropharyngeal swelling) and Stevens-Johnson syndrome (figure 5) have been reported after the use of this drug.8
 Figure 5: Stevens-Johnson syndrome
Figure 5: Stevens-Johnson syndrome
Levofloxacin (Oftaquix drops, 0.5%) has also a large spectrum, covering Gram-positive and Gram-negative bacteria. It is believed that, after the use of this drug, approximately 10% of patients can be expected to experience adverse reactions. However, most of those are restricted to the eye.7 Nevertheless, although rare, systemic side effects can also occur. These include hypersensitivity reactions, headache, laryngeal oedema and anaphylaxis.
Moxifloxacin (Moxivig drops, 0.5%, preservative-free) is a fourth-generation fluoroquinolone, licensed for treatment of conjunctivitis. It can also be used for the treatment of bacterial keratitis (figure 6) in patients with preservative allergies, with atopy and ocular surface disease as well as a prophylaxis agent in cataract and refractive surgeries.9 It has a better action than older fluoroquinolones against germs such as Streptococcus pneumoniae, Haemophilus influenzae, and methicillin-susceptible Staphylococci. It is usually safe to use but systemic side effects may occur and can range from hypersensitivity, to paraesthesia, dizziness and headache. Other side effects that have been identified include a decrease in haemoglobin, heart palpitation, dyspnoea, nausea, vomiting and skin rashes.
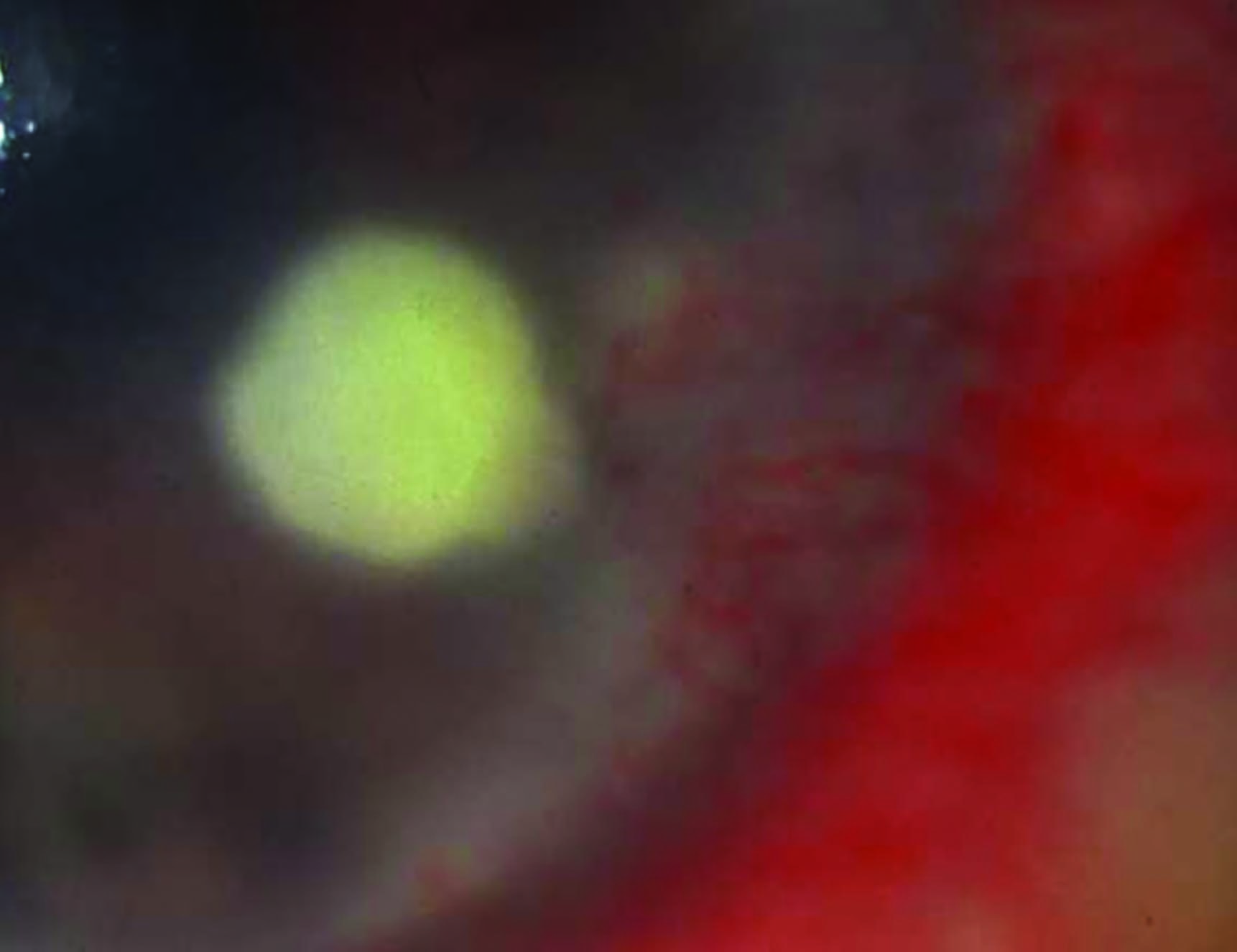 Figure 6: Corneal ulcer in bacterial keratitis
Figure 6: Corneal ulcer in bacterial keratitis
Antivirals
Antivirals, as the name indicates, are used to treat ocular viral infections. The most commonly used are:
- Acyclovir (Zovirax, 0.3% ointment); used to treat Herpes simplex keratitis (HSK, figure 7) and conjunctivitis
- Ganciclovir (0.15% eye gel); used mostly for the treatment of HSK.
- Trifluorothymidine (1% eye drops); also used in HSK and conjunctivitis.
Although known to cause various local adverse reactions, topical antivirals do not usually cause systemic side effects.
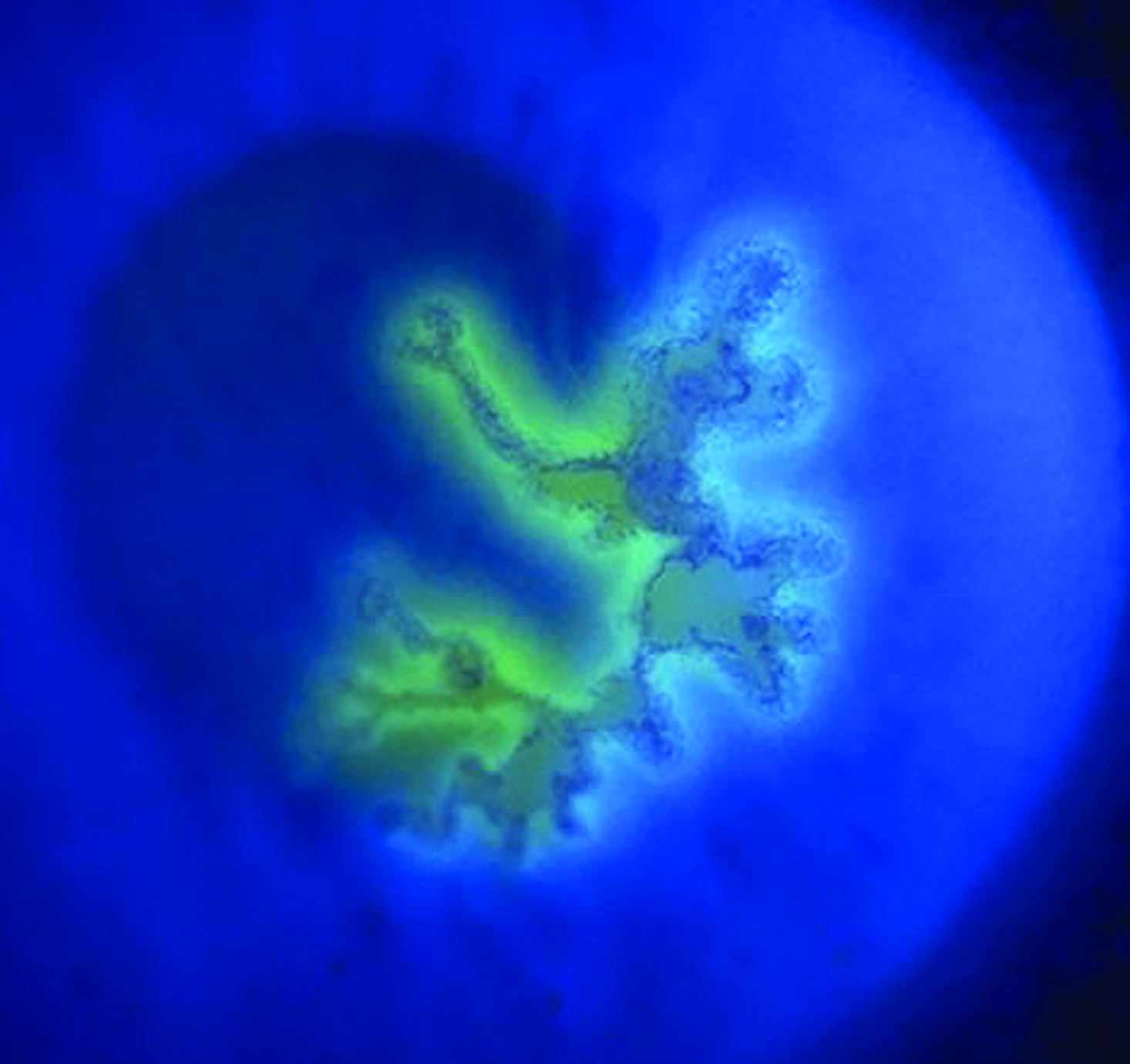 Figure 7: Dendritic ulcer in Herpes simplex keratitis
Figure 7: Dendritic ulcer in Herpes simplex keratitis
Corticosteroids
Topical corticosteroids are frequently used for the treatment of allergic or non-infectious conjunctivitis, following various ocular surgery and for the treatment of acute anterior and chronic uveitis (figure 8).10
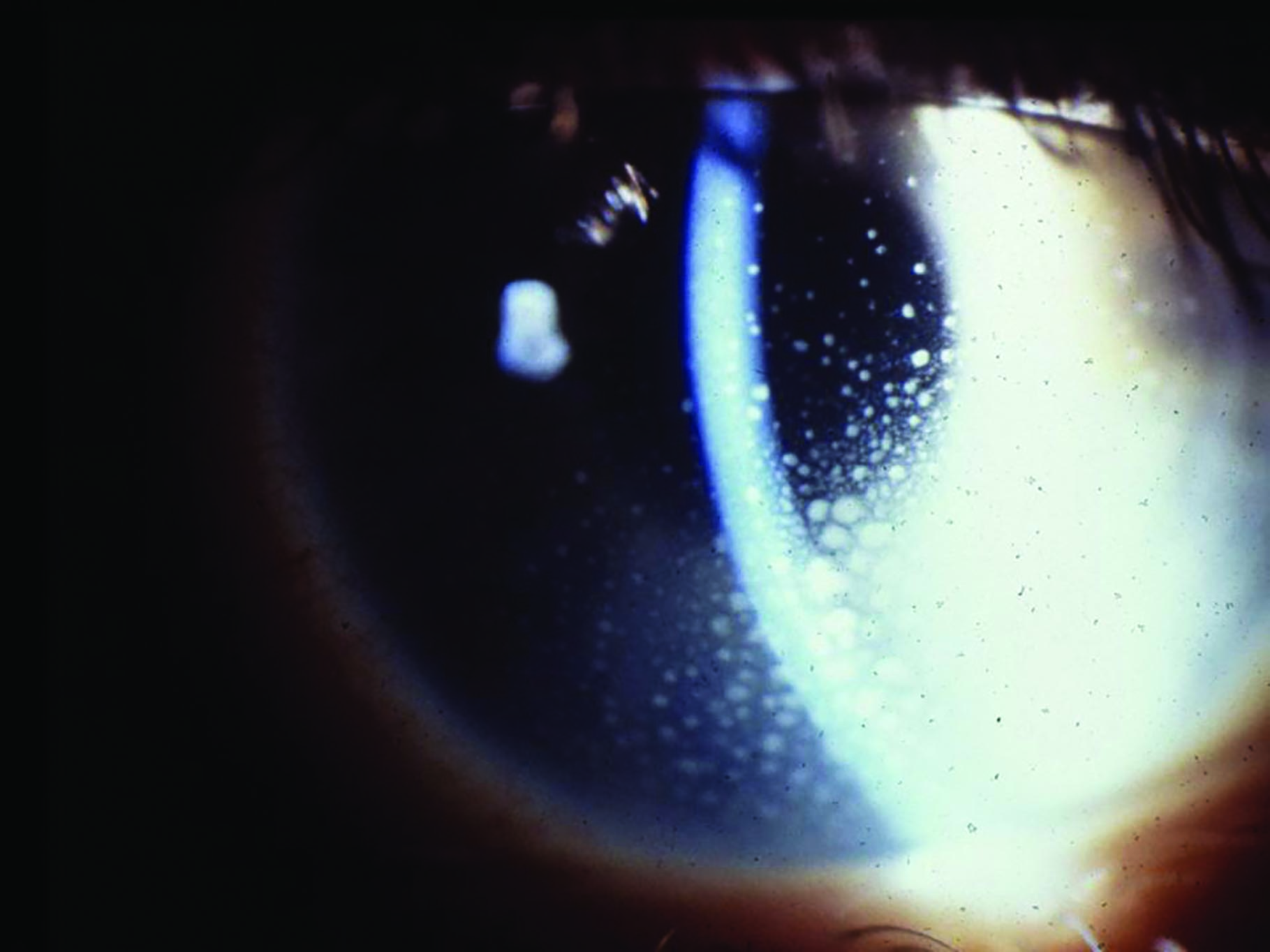 Figure 8: Chronic anterior uveitis
Figure 8: Chronic anterior uveitis
The most common topical corticosteroids used in ophthalmic practice are listed in table 2.
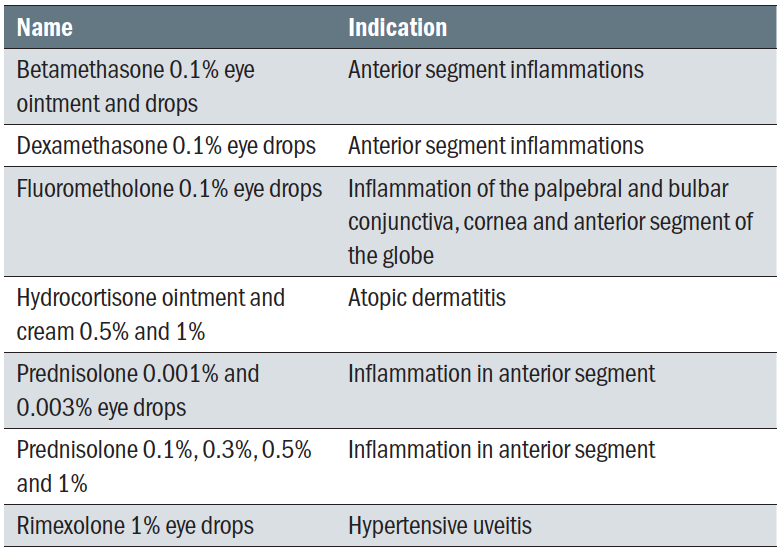 Table 2: Most common topical corticosteroids (adapted from 1)
Table 2: Most common topical corticosteroids (adapted from 1)
There are also combinations of corticosteroids and antibiotics, such as dexamethasone 0.1% with neomycin 0.35% and polymyxin B sulphate (6,000 units in 1ml eye drops) and hydrocortisone acetate or hydrocortisone acetate with neomycin (1.5% eye drops). These are used in uninfected inflammatory conditions of the anterior segment where the development of bacterial infection is possible.
Prolonged use of topical corticosteroids is known to be associated with a range of ocular complications including:
- Increased IOP (with or without secondary glaucoma)
- Cataract (typically posterior subcapsular, figure 9)
- Delayed wound healing
- Viral reactivation
- Increased susceptibility to infection
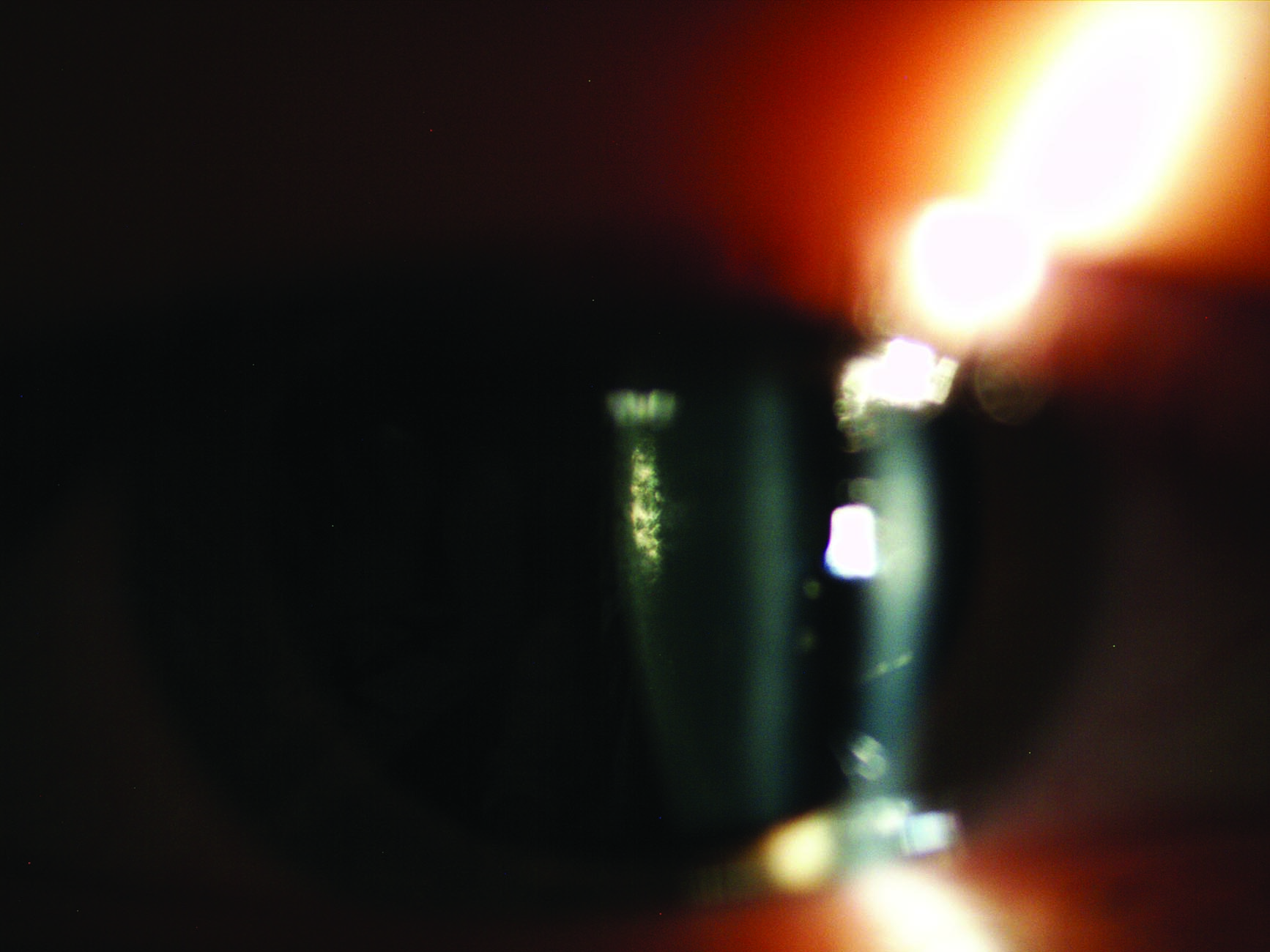 Figure 9: Posterior subcapsular cataract
Figure 9: Posterior subcapsular cataract
In addition, certain patients also need monitoring due to a potential risk of systemic side effects. Indeed, as with any other topical administrated drug, corticosteroids have the potential to create systemic adverse effects via their absorption through ocular tissues, the nasolacrimal tract and when swallowed.11 These effects are wide-ranging and may include:12
- Weight gain
- Osteoporosis
- Systemic hypertension
- Diabetes mellitus
- Gastric ulceration
- Aseptic necrosis
- Impaired immune function
- Sleep disturbance
- Depression
- Psychosis
In addition, it is known that corticosteroid administration is associated with impaired glucose tolerance in diabetic patients,13 therefore aggravating any pre-existing insulin resistance and hyperglycaemia. Consequently, it is very important to monitor very closely diabetic patients when giving corticosteroids to treat ocular conditions and work closely with the patient’s GP.
Nonsteroidal anti-inflammatory agents (NSAIDS)
In certain circumstances, the use of NSAIDs is preferred over the use of corticosteroids. The NSAIDs available in the UK for topical treatment of the eye are:
- Diclofenac sodium (0.1% single use eye drops)
- Ketorolac (0.5% eye drops)
Due to their additional analgesic effect, these drugs can be used for a range of reasons, from the inhibition of miosis during cataract surgery to the treatment of post-operative inflammation, pain and discomfort. Sometimes, they are used for the relief of the ocular signs and symptoms of seasonal allergic conjunctivitis. Their use can result in gastrointestinal symptoms, but they have been linked to triggering acute asthma attacks.14 There have also been cases of skin allergies after topical application.15
Antihistamines and antiallergics
The most commonly used antihistamines and antiallergics in eyecare practice are:
- Olopatadine (Opatanol); the first choice in ocular allergies
- Ketotifen (Ketofall); the second choice in patients with allergy or intolerance to benzalkonium chloride
- Lodoxamide (Alomide, 0.1% drops)
- Sodium cromoglicate (2% eye drops)
Their administration rarely results in systemic side effects. However, it is possible that, in some patients, there may be side effects such as dry mouth, nausea, headache or drowsiness.
Anti-glaucoma drugs
The most commonly prescribed anti-glaucoma drugs in the UK are listed in table 3.
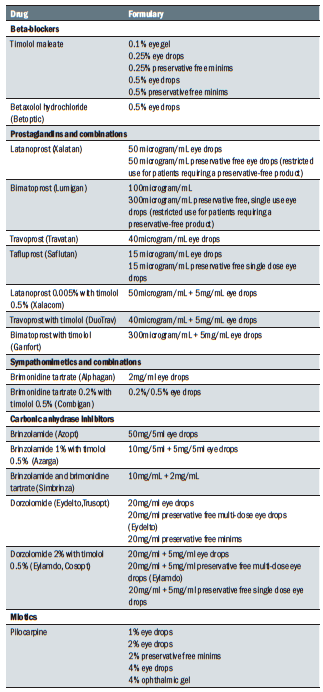 Table 3: Topical anti-glaucoma drugs (adapted from 16)
Table 3: Topical anti-glaucoma drugs (adapted from 16)
Beta-blockers
Topical beta-blockers have been an important class of agents in the management of glaucoma and ocular hypertension for nearly 40 years. It is well-known that their prolonged use can result in numerous systemic side effects. Therefore, they are absolutely contraindicated in patients with asthma, bradycardia or heart block, as well as in patients with a history of syncope.
They are also, albeit to a lesser extent, contraindicated in patients with symptomatic bradycardia, with heart rates less than 55 beats per minute without known aetiology, in those with pre-syncopal symptoms or dizziness without aetiology, or in patients with carotid sinus hypersensitivity.17
In addition, due to their blocking effect upon hypoglycaemia, beta-adrenergic blockers have been long considered a relative contraindication in diabetic patients. Nevertheless, studies in this area are contradictory and many conclude that ophthalmic beta-adrenergic blockers are safe for the majority of diabetic patients.17 However, they can affect HDL-C levels and, therefore, increase the risk for cardiovascular disease. Nevertheless, it is considered that the clinical impact of this effect is likely to be of relatively low importance as the concomitant lipid-lowering therapy that these patients receive would offset these effects.17
Other systemic side effects linked to the prolonged use of topical beta-blockers include depression and sexual dysfunction.
Prostaglandin analogues
Prostaglandin analogues are the most commonly prescribed topical antiglaucoma drugs and, despite their frequent ocular side effects, the fact that their plasma concentration is low following topical administration means that systemic adverse effects are unlikely to occur. Nevertheless, cardiac events, such as angina, have been reported18 along with symptoms of chest tightness.19 Prostaglandins also play a significant role in pain mechanisms,20 causing various types of visceral pain.
Sympathomimetic drugs
Brimonidine is another frequently used drug for the treatment of glaucoma. The use of this drug is associated with a large number of ocular side effects. In addition, there have been occasional reports of systemic adverse effects in infants, including apparent central nervous system depression21 as well as local allergy, tiredness, and fainting attacks in children.22 In adults, systemic side effects may occur in 20% to 52% of cases and typically include drowsiness, shortness of breath, dizziness, high blood pressure, skin rash, headache and low mood.23 These effects are more common in patients older than 60 years and when higher concentrations are used. Rare effects include a reduction in systolic blood pressure24 and acute psychosis.25
Carbonic anhydrase inhibitors
Carbonic anhydrase inhibitors (CAIs) are frequently prescribed for the treatment of glaucoma, usually as second-line therapies, either singly or as a combination of drugs with timolol or brimonidine. Systemic acidosis26 and taste disruption may occur in 3.0% to 7.8% of patients.
Dr Doina Gherghel is an academic ophthalmologist with a special interest in inter-professional learning for optometrists.
- The third and final part of this series will review the systemic side effects of intra-vitreal and peri-operative ophthalmic drugs.
References
- https://www.moorfields.nhs.uk/sites/default/files/uploads/documents/Ophthalmic%20Formulary%20v1.24%20Jul%202018.pdf- Accessed on the 17th of August 2020
- Liphshitz I, Loewenstein A. Anaphylactic reaction following application of chloramphenicol eye ointment. Br J Ophthalmol 1991; 75: 64
- Doshi B, Sarkar S. Topical administration of chloramphenicol can induce acute hepatitis. BMJ 2009; 338: b169
- Moyano JC, Alvarez M, Fonseca JLet al.Allergic contact dermatitis to chloramphenicol. Allergy 1996; 51: 67–69
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3964666/#CIT0001
- Bathia J, Sadiq MN, Chaudhary TA, Bathia A. Eye changes and risk of ocular medications during pregnancy and their management. Pak J Ophthalmol 2007; 23 . 1
- https://www.medicines.org.uk/emc/product/7357/smpc
- http://www.jcor.in/article.asp?issn=2320-3897;year=2016;volume=4;issue=1;spage=42;epage=46;aulast=Ramachandra
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2698721/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5153265/
- Gupta P, Bhatia V. Corticosteroid physiology and principles of therapy. Indian J Peds. 2008;75:1039-1044
- https://www.ophthalmologymanagement.com/issues/2014/december-2014/know-the-systemic-effects-of-ocular-steroid-therap#ref3- accessed on 18th August 2020
- Bahar I, Rosenblat I, Erenberg M, et al. Effect of dexamethasone eyedrops on blood glucose profile. Current Eye Research. 2007;32:739-742
- Sitenga GL, Ing EB, Van Dellen RG, Younge BR, Leavitt JA. Asthma caused by topical application of ketorolac. Ophthalmology. 1996;103(6):890–892
- Miyazato H, Yamaguchi S, Taira K, et al. Allergic contact dermatitis due to diclofenac sodium in eye drops. J Dermatol. 2011;38(3):276–279
- http://www.leedsformulary.nhs.uk/chaptersSubDetails.asp?FormularySectionID=11&SubSectionRef=11&SubSectionID=A100- accessed 0n the 18 August 2020
- https://pubmed.ncbi.nlm.nih.gov/12429254/
- Shigematsu S, Niwa H, Saikawa T. Vasospastic angina induced by prostaglandin F2 alpha. Br Heart J 1993; 69: 364–365
- https://www.nature.com/articles/6700351
- Besson JM . The neurobiology of pain. Lancet 1999; 353: 1610–1615
- Berlin RJ, Lee UT, Samples JR et al. Ophthalmic drops causing coma in an infant. J Pediatr 2001; 138(3): 441–443
- https://www.nature.com/articles/6700520
- Detry-Morel M, Dutrieux C . Treatment of glaucoma with brimonidine (Alphagan 0.2%). J Fr Ophtalmol 2000; 23(8): 763–768
- Waldock A, Snape J, Graham CM . Effects of glaucoma medications on the cardiorespiratory and intraocular pressure status of newly diagnosed glaucoma patients. Br J Ophthalmol 2000; 84(7): 710–713
- Kim DD . A case of suspected alphagan-induced psychosis. Arch Ophthalmol 2000; 118(8): 1132–1133
- Menon GJ, Vernon SA. Topical brinzolamide and metabolic acidosis. Br J Ophthalmol. 2006;90:247–8
