The prevention of sight loss and the optimisation of vision through optical correction are core concepts for optometrists. However, just as sight loss is not always preventable, not every visual problem can be solved with optical correction alone. A comprehensive assessment of functional vision may be required to deal with the consequences of sight impairment. This skill becomes more important as the patient population gets older. Ageing is very much associated with an increased prevalence of sight impairment (table 1). However, it also goes hand in hand with hearing impairment.2 Combined visual and hearing impairment can lead to unique challenges. This article describes ways to assess and manage patients with dual sensory loss.
 Table 1: The association of age with sight loss in the UK1
Table 1: The association of age with sight loss in the UK1
Definitions and demographics
The legal definition of deaf-blindness was established by the Department of Health in 1995 as follows:
‘A person is regarded as deaf-blind if their combined sight and
hearing impairment cause difficulties with communication, access to information and mobility. This includes people with a progressive sight and hearing loss.’
According to Sense,3 there are around 390,000 deaf-blind people in the UK and this number is expected to increase to 600,000 by 2035. The majority (around 75%) of people with coexisting hearing and sight impairment have acquired deaf-blindness, having developed the condition in old age. Hearing loss is common with age, as are eye conditions such as diabetic retinopathy, AMD, glaucoma, cataract and myopic degenerative diseases. Optometrists in community practice are most likely to encounter people with dual sensory loss due to old age.
Deaf-blindness can also be congenital or develop before language acquisition. Examples of causes include:
- Premature birth; full sensory development is interrupted
- Foetal infections; including rubella, toxoplasmosis (figure 1) and cytomegalovirus
- Foetal alcohol syndrome
- Cerebral palsy
- Genetic abnormalities; including Usher syndrome, CHARGE syndrome and Down’s syndrome
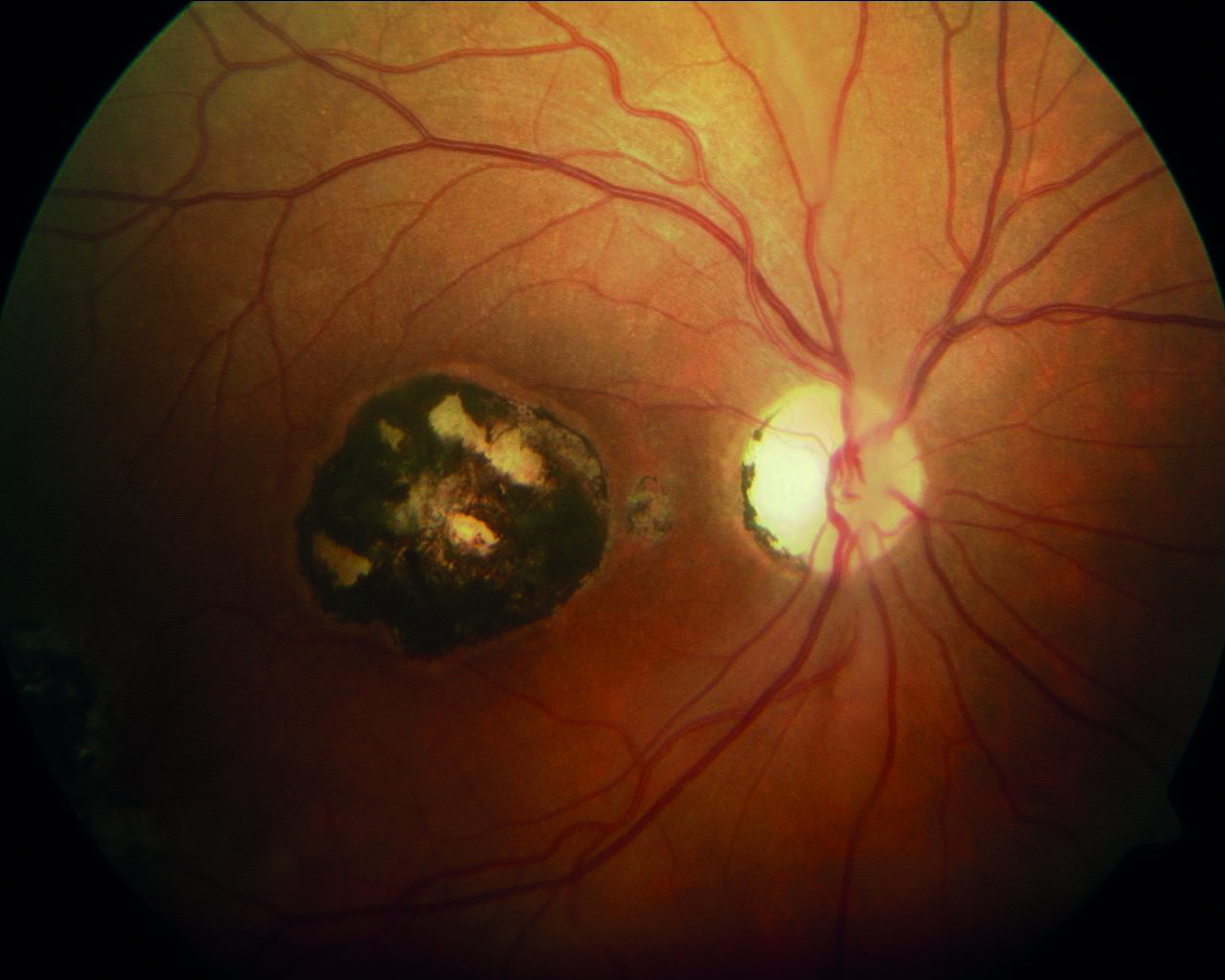 Figure 1: Infections during pregnancy may lead to deaf-blindness, such as toxoplasmosis shown here
Figure 1: Infections during pregnancy may lead to deaf-blindness, such as toxoplasmosis shown here
There are two genetic causes of deaf-blindness worthy of further mention:
- Usher syndrome; is a rare genetic disorder caused by a mutation in any one of at least 11 genes resulting in a combination of hearing loss and visual impairment. It is a major cause of deaf-blindness and is, at present, incurable. Usher syndrome is characterised by hearing loss and a gradual visual impairment. Depending on the type of inheritance, hearing loss may be profound from birth, progress from birth, or be maintained as a less profound level of hardness of hearing. The hearing loss is caused by a defective inner ear, whereas the vision loss results from retinitis pigmentosa or RP (figure 2). Usually in RP, the rod cells of the retina are affected first, leading to early night blindness (nyctalopia) and the gradual loss of peripheral vision. In other cases, early degeneration of the cone cells in the macula occurs, leading to a loss of central acuity.
- CHARGE syndrome4; a rare genetic condition affecting many part of the body and known to be related to a specific gene mutation in around 50% of cases. The name of this syndrome is an acronym from the following:
- •Coloboma (figure 3)
- •Heart defects
- •Atresia choanae (blockage of the back of the nasal passage)
- •Growth retardation
- •Genital abnormalities
- •Ear abnormalities
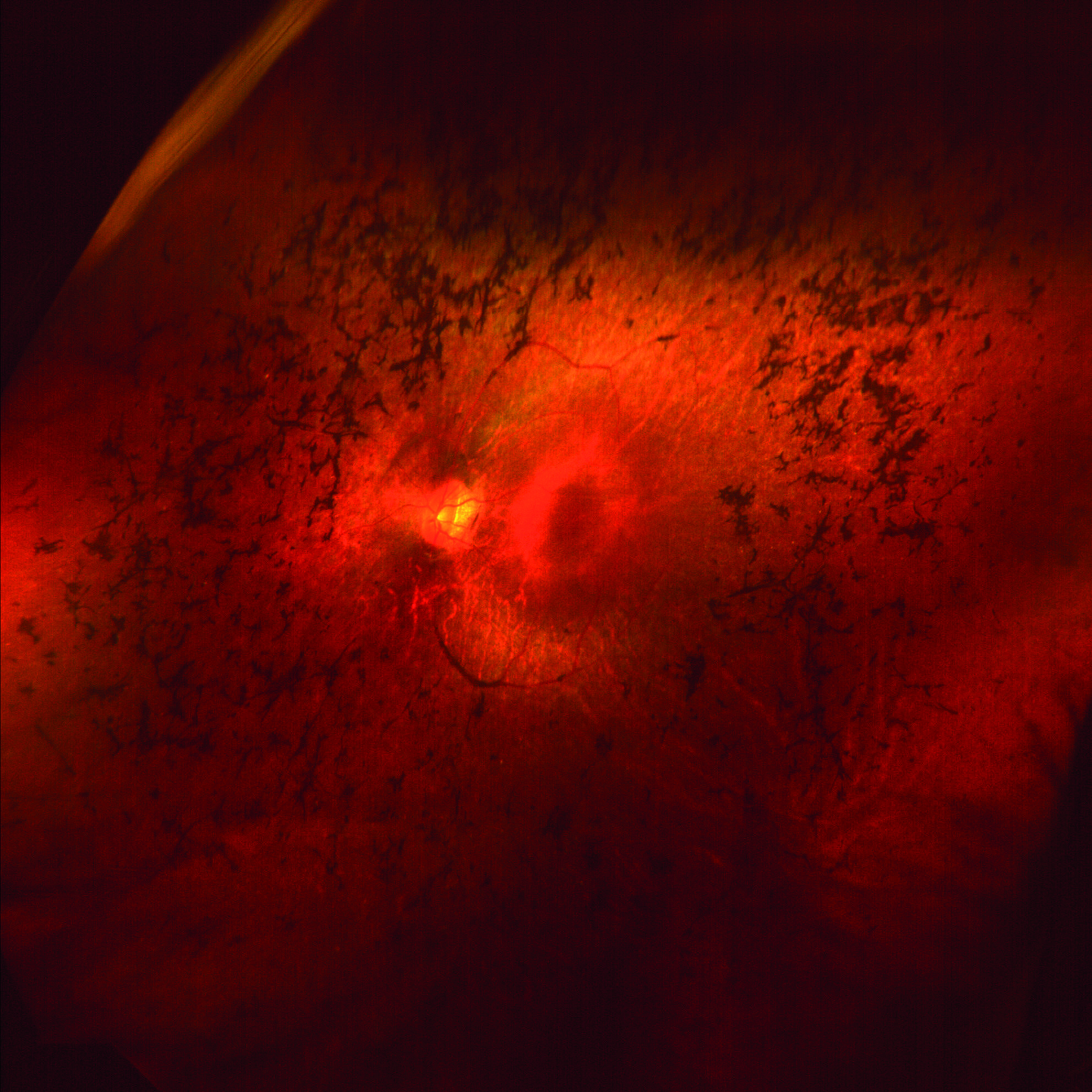 Figure 2: Retinitis pigmentosa in a patient with Usher syndrome
Figure 2: Retinitis pigmentosa in a patient with Usher syndrome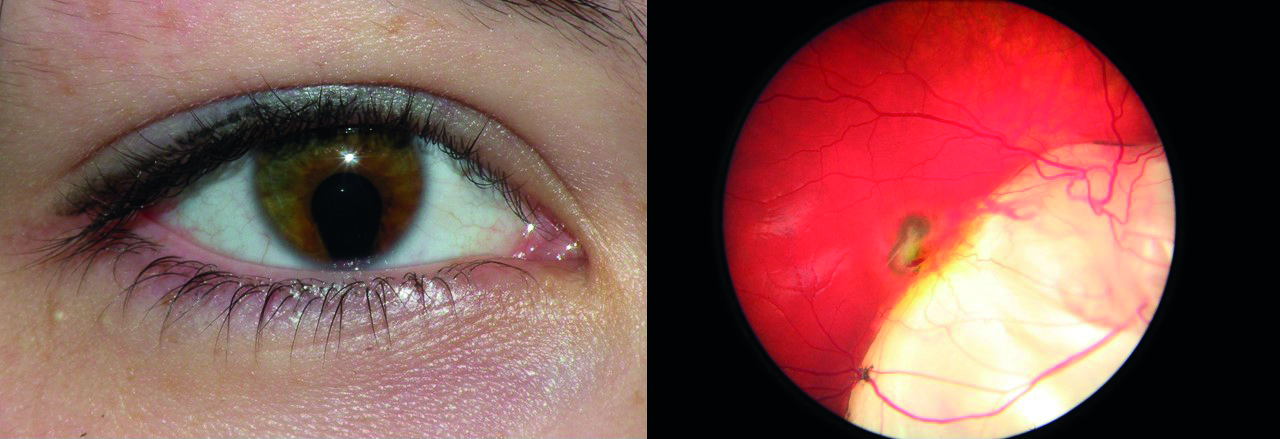 Figure 3: Iris (left) and chorioretinal (right) coloboma as part of CHARGE syndrome
Figure 3: Iris (left) and chorioretinal (right) coloboma as part of CHARGE syndrome
Communication in the optometric practice
When a patient with dual sensory impairment (deaf-blind) attends optometric practice, it is important to establish their preferred mode of communication right at the beginning. Stevens et al carried out a survey among people with a hearing impairment in a healthcare setting.5 In this survey, the majority of respondents indicated that they ‘sometimes’ or ‘often’ let care providers know about their hearing impairment (93%). However, almost a third of respondents indicated that no arrangements were made to improve communication.
So, the question arises as to how eye care professionals (ECPs) and practice staff can ensure effective communication in their practice or clinic. The minority group of British sign language (BSL) users, who tend to have congenital and developmental deaf-blindness, needs to be approached in a very different way to the more commonly presenting person with age-related dual sensory impairment.
BSL users may be accompanied by a BSL interpreter or a note taker,6 or may have to rely on a combination of BSL, gestures, writing and lip-reading. People with acquired deaf-blindness are more likely to rely on a combination of lip-reading, writing and adapting the tone and volume of speech. In any case, the practitioner can aid communication by making sure their face is clearly visible at all times and the voice is projected in the direction of the patient.
During the Covid-19 pandemic, face masks can be a hindrance to communication and the use of transparent face shields and face masks (figure 4) could be considered. Communication strategies were discussed in greater detail in an earlier article (see Optician 18.09.20).
 Figure 4: Transparent face masks are useful for communicating with deaf-blind patients while minimising airborne virus transmission
Figure 4: Transparent face masks are useful for communicating with deaf-blind patients while minimising airborne virus transmission
Common needs of people with dual sensory loss
People with sight impairment tend to rely more upon their hearing and people with hearing loss attempt to compensate by using their sight. These strategies are obviously less effective when both senses are impaired. Dual sensory loss, therefore, presents unique challenges.
McDonnall et al carried out a survey among people with combined visual and hearing impairment.7 They found that the four most common needs in this patient group were as follows:
- Transportation help
- Technology training
- Assistance with errands
- Need for improved communication
The aforementioned definition of deaf-blindness ties in with this. ECPs may be able to help people to meet these needs and so overcome many of the barriers restricting normal daily functioning. A multidisciplinary approach is often most beneficial to patients8 as most ECPs do not have the necessary specialist training to deal with all the different needs of this patient group. However, ECPs working within low vision services need to be particularly aware of concurrent hearing loss and the specific challenges related to this. For this reason, let us now consider some strategies in a little more detail.
Communication and social interaction with the deaf-blind
Facial expression
A frequent complaint of patients with a visual impairment is the inability to recognise people’s faces and interpret facial expressions. Many older patients rely on facial expressions, lip reading and body language to compensate for hearing loss. When their sight deteriorates, this compensation strategy is no longer available. The ECP can address this problem in several ways.
First of all, any residual sight the patient has may be optimised by ensuring that appropriate and up-to-date optical correction is worn. The ECP can further optimise functional vision by giving advice on lighting and positioning of objects relative to light sources. Avoiding back light scatter is a useful way of significantly enhancing the contrast of people’s faces when viewed. This is easily demonstrated by asking the patient to look at the practitioner’s face with the window behind the practitioner and again with the window behind the person with dual sensory impairment (figure 5). In the author’s experience, this simple demonstration can be an eye-opener for patients and result in improved functioning in social environments.
 Figure 5: The position of a face under view relative to a light source has a major impact upon the ease of interpretation of facial appearance and expression. Light source behind the viewer (left) improves facial interpretation compared with light source behind the person under view (right) makes interpretation difficult
Figure 5: The position of a face under view relative to a light source has a major impact upon the ease of interpretation of facial appearance and expression. Light source behind the viewer (left) improves facial interpretation compared with light source behind the person under view (right) makes interpretation difficult
Contrast and clutter
A study by Schneck suggested that hearing loss in old age is associated with poor contrast sensitivity in particular.9 This highlights the importance of assessing contrast sensitivity in the elderly population as these patients may be deaf-blind despite reasonable visual acuity. Reducing clutter can also help to minimise the complexity of the visual scene and focus the attention on the primary activity. The more clutter, the greater the contrast variation and the less able a deaf-blind person may be able to differentiate between objects. In practice environments, this may impact upon the effectiveness of communication and also have safety implications. In the home environment, this may increase the likelihood of falls or injury.
Hearing aids
The ECP should ask the patient about their hearing aids and history of hearing assessment. It could be that the patient has not had their hearing assessed for a long time and could benefit from more suitable hearing aids. Hearing aids are constantly evolving and many of the latest include a wide range of adaptations, such as Bluetooth linkage, that might be a great help. It is also possible that the current hearing aids have become difficult to operate due to progression of the visual impairment since first being fitted. This is particularly problematic with many of the modern small and complex hearing aids.
There is also a significant group of people with hearing impairment who do not wear hearing aids at all for a range of reasons.10,11 Integration of hearing and vision services can make a positive difference for this patient group.12 In the author’s experience, organisations such as Deaf-blind Scotland and Deaf Action are keen to liaise and accept referrals from ECPs. It is worth visiting these organisations in person or via their websites in order to get an appreciation of the services they offer to deaf patients (see useful web links at the end of the article). Resources include patient support groups, Braille and Moon tuition, lip reading and sign language courses, and useful gadgets and aids.
People with dual sensory loss who struggle with holding conversations often benefit from a device that enhances the sound of a voice while cancelling background noises. Support organisations may supply these, as well as offer advice on the use of hearing aid linked amplification systems; loop systems are still widespread, while newer Wi-Fi and remote electronic communication and enhancement systems have been introduced. These can help, for example, the user to hear someone over the phone better or be able to help someone to better orientate themselves in a social environment. A letter from an ECP to the general practitioner to highlight a hearing impairment can be an important step in accessing specialist help and assisting patients with dual sensory loss.
Telephone conversations
Telephone conversations are a common problem for people with dual sensory loss. The visual impairment makes it difficult to look up phone numbers and to then dial the number. The hearing impairment prevents patients from understanding the person on the other end of the phone. Many patients do not hear the ringtone of the phone.
A phone with an extra loud ring-tone or with a flash-signal can make a significant difference to a person with a hearing impairment. In order to overcome the visual impairment, it can help to have a list of commonly used phone numbers in large bold print that the patient can see, or the phone can be pre-programmed. Large-dial phones for the visually impaired can be another helpful tool. Some phones have a built-in option to increase the volume and enhance the voice (see figure 6). Charities such as the RNIB and Deaf Action can advise patients, depending on their specific needs.
 Figure 6: Enhancements to telephones of use to the deaf-blind include large buttons, flashing light indicator of ring tone, volume increase and voice enhancement capability, pre-programmable dialling and speed-dialling face image buttons
Figure 6: Enhancements to telephones of use to the deaf-blind include large buttons, flashing light indicator of ring tone, volume increase and voice enhancement capability, pre-programmable dialling and speed-dialling face image buttons
Facial recognition
For helping patients in recognising people from across the street, certain strategies can be considered which can be of help. These include the ECP encouraging the patient to consider the
following:
- Look at the distinctive ways other people walk to help
identification - Remember the colour of people’s coats
- Encourage the patient to ask others to introduce themselves when they meet in the street
Such simple strategies can ensure that no time and energy is wasted by a patient in trying to decide who is speaking to them. The author has come across patients who find it very helpful for their partner (parent or carers) always to wear a specific bright-coloured scarf, or to meet them always in the same location. This avoids confusion and frustration.
Emotional well-being
Emotional well-being is another important consideration. Patients with dual sensory impairment are more likely to suffer with depression, anxiety,13,14 loneliness15 and, in general, a poorer quality of life.16 Reduced social function is also common among people with dual sensory impairment.17 On the other hand, a healthy social network in people with a visual impairment is associated with lower levels of depression (figure 7).18 Therefore, improving effective communication can have practical benefits as well as emotional benefits. Patients who feel isolated and lonely often benefit from support groups. The RNIB, Deafblind UK, Deaf Action and sight loss charities such as the Macular Society run support groups in many areas.
 Figure 7: Charities such as Deafblind UK offer support and social network opportunities that have a significant positive impact upon the emotional and mental well-being of the deaf-blind population
Figure 7: Charities such as Deafblind UK offer support and social network opportunities that have a significant positive impact upon the emotional and mental well-being of the deaf-blind population
Access to information
People with a visual impairment often find it difficult to read their mail. The usual strategies for sight impairment can be usefully applied here. This includes the introduction and demonstration of the use of appropriate magnifiers, telescopic aids and electronic devices (figure 8).
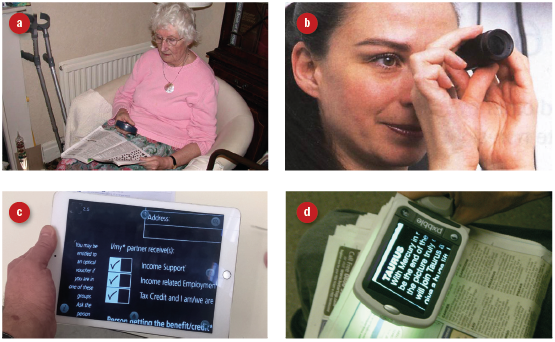 Figure 8: Assistance with visual tasks, such as reading mail, may be offered to the deaf-blind. Aids might include (a) simple optical magnifiers, (b) telescopic devices, (c) adapted digital devices and (d) specialist electronic devices
Figure 8: Assistance with visual tasks, such as reading mail, may be offered to the deaf-blind. Aids might include (a) simple optical magnifiers, (b) telescopic devices, (c) adapted digital devices and (d) specialist electronic devices
Unfortunately, speech technology is of less value to a person with a hearing impairment. The patient might instead be sign-posted to classes and one-on-one tuition for technology to optimise the use of these devices. However, one has to bear in mind that older adults, even with normal hearing for their age, tend to experience some difficulty with speech output of assistive technology devices.19
Some patients are not aware that bank statements and bills can be provided in large print or Braille. Large and bold print stationary, such as address books and writing paper, and wide-nibbed felt tip pens are often very useful for people with a visual impairment and so may also help the deaf-blind (figure 9).
 Figure 9: Non-optical aids for reading and writing may benefit the deaf-blind
Figure 9: Non-optical aids for reading and writing may benefit the deaf-blind
Mobility and independence
Sight and hearing impairment may have a significant impact upon a person’s mobility and, therefore, independence. In the home environment, independence can often be maintained by making some simple changes. Examples include the following:
- Light switches, dials and control knobs may be marked with tactile stickers, called ‘bump-ons’ (figure 10)
- High contrast chopping boards and other utensils and surfaces (figure 11)
- Localised light enhancement (figure 12)
- Liquid level indicators for filling cups (figure 13)
- Anti-slip surfaces or add-ons to cups and receptacles
- Doors, steps and stairs can be marked with high contrast strips or localised lighting to prevent falls and bump
 Figure 10: A selection of ‘bump-ons’
Figure 10: A selection of ‘bump-ons’
 Figure 11: Use of contrast in the kitchen – here a dark chopping board stands out from the underlying surface
Figure 11: Use of contrast in the kitchen – here a dark chopping board stands out from the underlying surface Figure 12: Stick-on LED lights under overhanging cupboards help enhance, for example, kitchen surfaces
Figure 12: Stick-on LED lights under overhanging cupboards help enhance, for example, kitchen surfaces Figure 13: Liquid-level indicators prevent spillage of hot drinks
Figure 13: Liquid-level indicators prevent spillage of hot drinks
Many patients report that navigating is relatively easy around their own home as familiar obstacles can be remembered and avoided. However, going out is often much more challenging and the risk of falling becomes a major concern. If this is the case, mobility training may be beneficial and, if this need is identified by an ECP, the involvement of a rehabilitation officer might be suggested. The RNIB and Guide Dogs have excellent mobility and rehabilitation officers who can help patients increasing their confidence for navigating in their area and beyond. They offer mobility training and cane training. Longer canes for obstacle detection may be of value, but many find significant help from using a symbol cane as a means of signalling to others that the user has an impairment. Most readers will be aware that a cane with red stripes signifies deaf-blindness. But how many of the general public know this?
The availability of high-tech canes has increased in recent years. These devices usually combine a cane with a camera device to allow object recognition and may offer a range of orientation and navigation.
The use of public transport poses unique challenges for a patient with dual sensory loss.20,21 Smartphone applications designed to help when using public transport and navigation have made a significant contribution to independent travel. The use of a simple monocular or binoculars can be helpful for seeing the traffic lights, road signs, street names and numbers, notices on platforms or at bus stops. They can also be useful in shops for seeing the notices above the isles. Traffic lights at pedestrian crossings have a cone at the bottom of the light box, which spins when the green light for pedestrians is on. Stations and town centres are equipped with tactile paving to facilitate navigation. The author has come across patients who gained independence by learning Braille numbers specifically to allow them to access lifts in public buildings unaccompanied.
Support for care-givers
Dual sensory impairment is related to higher rates of cognitive impairment and increased dependence on others.22 Caring for a person with dual sensory impairment can be both challenging and demanding, requiring adaptations to communication and changes to social skills, and leading to feelings of worry about the deaf-blind person and emotional reactions to the necessary adaptations.23 It is, therefore, good practice to consider the support needs of the carer. Sometimes people are keen to assume the role of carer and cope well. In other situations, the carer might benefit from support or some occasional respite. Introducing a befriend-er or other support to alleviate the burden can be invaluable.
Conclusion
Eye care professionals are in a privileged position in being able to improve the quality of life for patients with dual sensory loss. Depending upon their level of experience, support can be offered either directly or via liaison with allied professionals. For ECPs with little experience in this area, the aim could be to make an appropriate referral to a local low vision service or charity dedicated to support people with sight and hearing loss. For more experienced practitioners, interventions can be undertaken directly and more specific referrals made to appropriate professionals and charities. Doing more than managing refractive error alone creates opportunities for patients to function optimally and reach their maximum potential – and also enhances the role of the ECP.
Cirta Tooth is a low vision specialist practising in Scotland with a special interest in people with sensory and learning impairment.
Useful resources
The following weblinks are well worth visiting and offer a wide range of helpful information and resources for ECPs:
- www.rnib.org.uk
- www.sense.org.uk
- www.deaf-blind.org.uk
- https://dbscotland.org.uk
- http://www.deafaction.org
- www.usher-syndrome.org
- www.british-sign.co.uk
References
- RNIB: Key information and statistics on sight loss in the UK. Available at: https://www.rnib.org.uk/professionals/knowledge-and-research-hub/key-information-and-statistics [Accessed on 08/10/20].
- Akeroyd, M. A. et al. 2014. Estimates of the number of adults in England, Wales, and Scotland with a hearing loss. International Journal of Audiology 53(1), pp.60-61
- Sense. What is deafblindness? Available at: www.sense.org.uk/get-support/information-and-advice/conditions/deafblindness [Accessed on 08/10/2020]
- Sense. CHARGE syndrome. Available at; www.sense.org.uk/get-support/information-and-advice/conditions/charge-syndrome [Accessed on 08/10/2020]
- Stevens MN, Dubno JR, Wallhagen MI et al. 2019. Communication and healthcare: self-reports of people with hearing loss in primary care settings. Clinical Gerontologist 42(5), pp.485-494
- Iezzoni, L.I. et al. 2004. Communicating about health care: observations from persons who are deaf or hard of hearing. Annals of Internal Medicine I140(5), pp. 456-362
- McDonnall, M.C. et al. 2016. Needs and challenges of seniors with combined hearing and vision loss. Journal of Visual Impairment & Blindness 110(6), pp. 399-411
- Fraser SA, Southall KE, Wittich W. 2019. Exploring professionals’ experiences in the rehabilitation of older clients with dual sensory impairment. Canadian Journal of Aging 38(4), pp.481-492
- Schneck ME, Lott LA, Haegerstrom-Portnoy G et al. 2012. Association between hearing and vision impairments in older adults. Ophthalmic and Physiological Optics 32(1), pp.45-52
- Gregory S, Billings J, Wilson D et al. 2020. Experiences of hearing aid use among patients with mild cognitive impairment and Alzheimer’s disease dementia: a qualitative study. Sage Open Medicine 8(205031212090472)
- Sawyer CS, Armitage CJ, Munro KJ et al. 2019. Correlates of hearing aid use in UK adults: self-reported hearing difficulties, social participation, living situation, health, and demographics. Ear and Hearing 40(5), pp.1061-1068
- Vreeken HL, van Rens GHMB, Kramer SE et al. 2015. Effects of a dual sensory loss protocol on hearing aid outcomes: a randomized controlled trial. Ear and Hearing 36(4), pp. e166-e175
- Han JH, Lee HJ, Jung J et al. 2019. Effects of self-reported hearing or vision impairment on depres-sive symptoms: a population-based longitudinal study. Epidemiology and Psychiatric Sciences 28(3), pp.343-355
- Simning A, Fox ML, Barnett SL et al. 2019. Depressive and anxiety symptoms in older adults with auditory, vision, and dual sensory impairment. Journal of Aging and Health 31(8), pp.1353-1375
- Shukla A, Harper M, Pedersen E et al. 2020. Hearing loss, loneliness, and social isolation: a systemat-ic review. Otolaryngology Head and Neck Surgery;162(5):622-633
- Tseng Y, Liu SH, Lou M et al. 2018. Quality of life in older adults with sensory impairments: a system-ic review. Quality of Life Research 27(8), pp.1957-1971
- Mick P, Parfyonov M, Wittich W et al. 2018. Associations between sensory loss and social networks, participation, support, and loneliness analysis of the Canadian longitudinal study on aging. Canadi-an Family Physician 64(1), pp.E33-E41
- Van Nispen RMA, Vreeken HL, Comijs HC et al. 2016. Role of vision loss, functional limitations and the supporting network in depression in a general population. Acta Ophthalmologica 94(1), pp.76-82
- St-Amour L, Jarry J, Wittich W. 2019. The audibility of low vision devices with speech output used by older adults with dual sensory impairment. Optometry and Vision Science 96(5), pp.345-353
- Azenkot, Shiri et al. (2011). Enhancing independence and safety for blind and deaf-blind public transit riders. Conference report. Proceedings of the International Conference on Human Factors in Computing Systems, CHI 2011, Vancouver, BC, Canada, May 7-12, 2011, 3247-3256
- Fürst, E.W.M. and Vogelauer, C. (2012) Mobility of the sight and hearing impaired: barriers and so-lutions identified. Qualitative Market Research, Vol. 15 No. 4, pp. 369-384
- Davidson JGS, Guthrie DM. 2019. Older adults with a combination of vision and hearing impair-ment experience higher rates of cognitive impairment, functional dependence, and worse out-comes across a set of quality indicators. Journal of Aging Health. Jan;31(1):85-108
- Nandurkar A and Shende S. 2020. Third party disability in spouses of elderly persons with different degrees of hearing loss. Ageing International 45, pp.136-148
