An understanding of prismatic effects, whether induced or prescribed, is an essential skill for all optical practitioners. Yet many still struggle with some concepts of prism, and optometrists often report binocular vision as their least favourite area of competency, perhaps safe in the knowledge that tricky cases can always be referred to an orthoptist instead of being resolved in primary eye care
The aim of this first article on the subject is to revise some core aspects of eye movements and binocular vision, to understand the purpose and production of prescribed prism, to consider the calculation and effects of induced prism, and discuss the manufacturing tolerances and standards relating to both prescribed and induced prism when supplying spectacles.
Background
At a recent CET event on spectacle non-tolerance, the authors heard the presenter (an optometrist) describe prism as follows: ‘in a single word “prism” marks the difference between a dispensing optician and an optical dispensing assistant.’ While this may be an over-simplification, it also rings true, since an understanding of prismatic effects, both prescribed and induced, intended or accidental, is at the heart of solving problems of non-tolerance to spectacles, and ensuring patients are unlikely to have problems in the first place.
An important aspect of understanding prism is to understand the various anomalies of muscle balance that require it to be prescribed. A reliance on words derived from Latin, often with slight nuances where similar words have different meanings, signifying for example whether a movement is referring to one eye alone or both eyes together, can make the topic more than a little impenetrable. This is further compounded by the many textbooks on the subject written by and for orthoptists and which rarely give thought to the final corrective solution for the patient if it is to be spectacles rather than surgery or exercises.
When opticians consider a prismatic effect, they are interested in the ability of a prism or lens to deviate light, or displace an image, rather than any dispersive power the prism may have. Even this simple concept, that the purpose of a prism is to displace an image, is often misunderstood. The authors have often heard practitioners and students in examinations describe (incorrectly) how a prism moves the eye, or helps it to converge, or ‘makes a strabismusing eye straight’. And yet, the purpose of a prescribed prism is not to move the eye but to displace the image, to restore, as far as is possible, comfortable binocular single vision.
To further confuse the issue, of course, a prism can be used to induce eye movement under specific circumstances. The 20Δ base out prism test, favoured by those working in paediatric clinics and in child vision screening, is testament to this. Knowing that a prism refracts light towards its base, causing the image to be displaced towards the apex, we can envisage that a child with a 20Δ base out prism before one eye would need that eye to look along the refracted ray in order to see a single binocular image. In other words, if the eye could converge sufficiently then binocular single vision would be restored, and on this basis the child’s ability to converge and their fusional reserves be assessed as normal, or not.
Using a prism bar, or a trial lens prism of say 10Δ, we can easily satisfy ourselves that (as common sense would suggest) our eyes have considerable flexibility when it comes to converging, but much less ability to diverge or deviate vertically. Placing a prism with the base positioned up, down or in before one eye will usually induce double vision (diplopia), whereas most patients will quickly fuse the images created when the prism is placed base out, to restore binocular single vision.
By utilising differing amounts of prism, the limit of the patient’s ability to see singly rather than double can be determined and is described as their fusional reserve. This information can be used to prescribe an appropriate amount of prism to alleviate symptoms of permanent or intermittent diplopia, and additionally has provided the industry with manufacturing tolerances in terms of the amount of prism we can safely induce through inaccurate centration before causing the patients any discomfort or diplopia.
Prism basics
A prism is a three-dimensional shape, triangular in cross-section, that, when made from a transparent refracting material will deviate monochromatic light without focusing it. Polychromatic light, such as white light which represents a mix of visible light wavelengths, will also be split into its constituent wavelengths or colours (figure 1). The amount of this dispersion is dependent upon the Abbe number (often denoted by the lower case Greek letter Nu written as v) of the lens material. The lower the v-value, the greater the dispersion. Generally, the higher the refractive index of the lens material, the lower the Abbe number. In spectacle lenses, this dispersion is undesirable and is referred to as chromatic aberration and has been covered in a previous article (see Optician 19.06.20).
Figure 1: The dispersion of white light into the colours of the visible spectrum
A prism does not have any focusing power, but instead acts to deviate the light that is incident upon it. The deviation is dependent upon the following:
- The apical angle of the prism
- The refractive index of the prism material
- The angle at which incoming light is incident upon the first surface
The passage of a ray of light through a prism can easily be traced using Snell’s Law of Refraction in combination with some simple geometry or trigonometry. Snell’s Law of Refraction states:
n sin i = n’ sin i’
Figure 2 shows the minimum deviation through a prism with a large apical angle which occurs when i1’ = i2. Or put another way, if the prism is isosceles (such that the base angles at points B and C are equal), then the ray within the prism runs parallel to the base.

Figure 2: The refraction of light through a thick isosceles prism
It can also be seen that the total deviation, d is as follows:
d = d1 + d2
= the sum of the deviation at each surface
With prisms of low apical angle, as are generally prescribed in optometric practice, the minimum deviation closely observes the following relationship:
d = (n-1)a
The prism dioptre (Δ)
The deviating power of an ophthalmic prism can be categorised according to its apical angle in degrees, the deviation it produces in degrees (which takes the refractive index into account), or, as is the norm in optical practice the deviation it produces in prism dioptres (usually represented by the upper case Greek letter delta, or Δ).
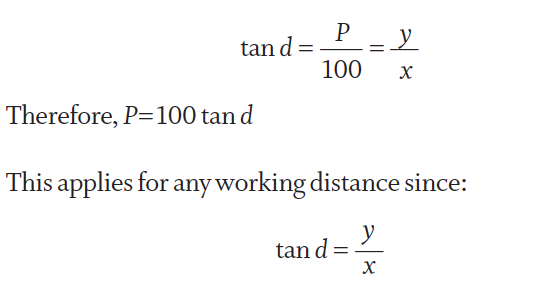
One prism dioptre is defined as a displacement of 1cm at a distance of 1m (100cm). The deviation measured in prism dioptres (the power of the prism) can easily be converted to degrees. Figure 3 shows the formation of an image of an object (the letter A) by a plano prism of power PΔ.
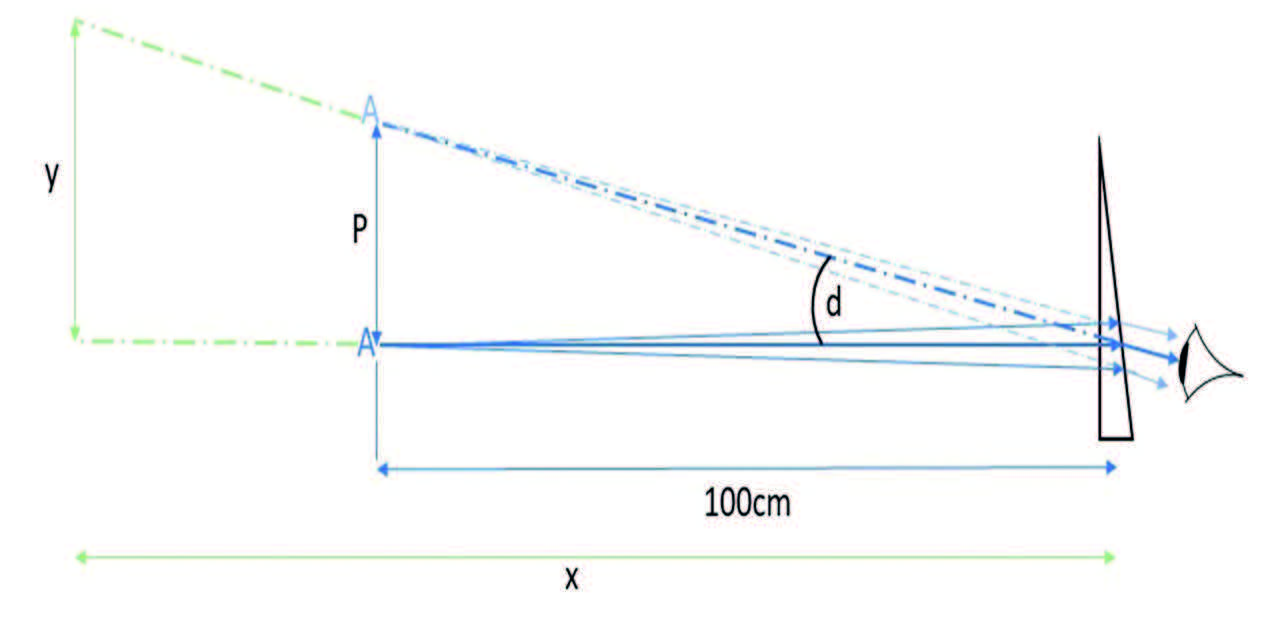
Figure 3: Formation of an image by a plano prism of power P prism dioptres (PΔ)
The deviation d, measured between the principle rays, can be determined simply using trigonometry:
In optical practice, although the amount of prism induced at different points on a lens can be quite large, in terms of prescribed prism we are usually only concerned with low prismatic power and small deviations.
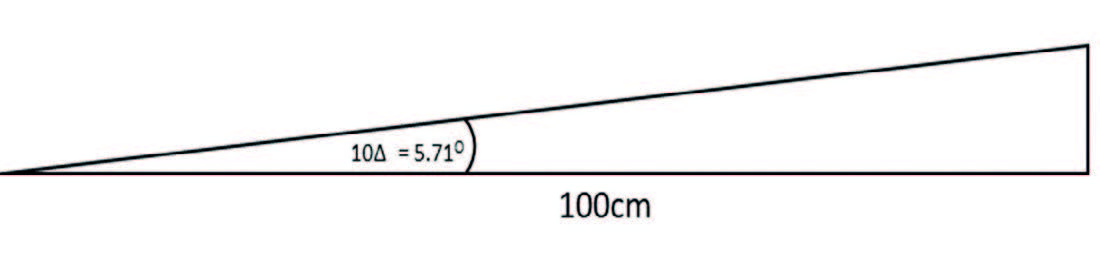
Figure 4: Scale drawing of a deviation of 10Δ
Figure 4 shows to scale an angle of 10Δ which is converted using tan-1 (P/100) to 5.71º and clearly shows that even high prisms cause relatively small deviations.
It is important to realise that the prism dioptre, although convenient, is not truly additive. For example; a deviation of 20Δ is tan-1
(20/100) = 11.31º and not the 2 x 5.71 = 11.42º that would perhaps have been expected based on twice the deviation shown in figure 4.
Prism thickness difference
Even in low amounts prismatic correction will cause the lens to be much thicker at one edge. How much thicker the base is compared to the apex can be determined by converting the deviation, P, in prism dioptres, to d, in degrees:
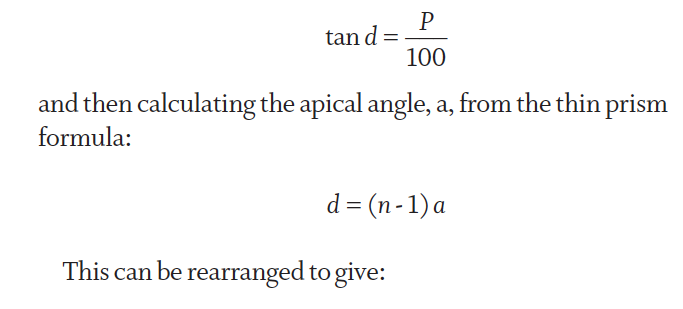
Where b is the diameter of the prism.
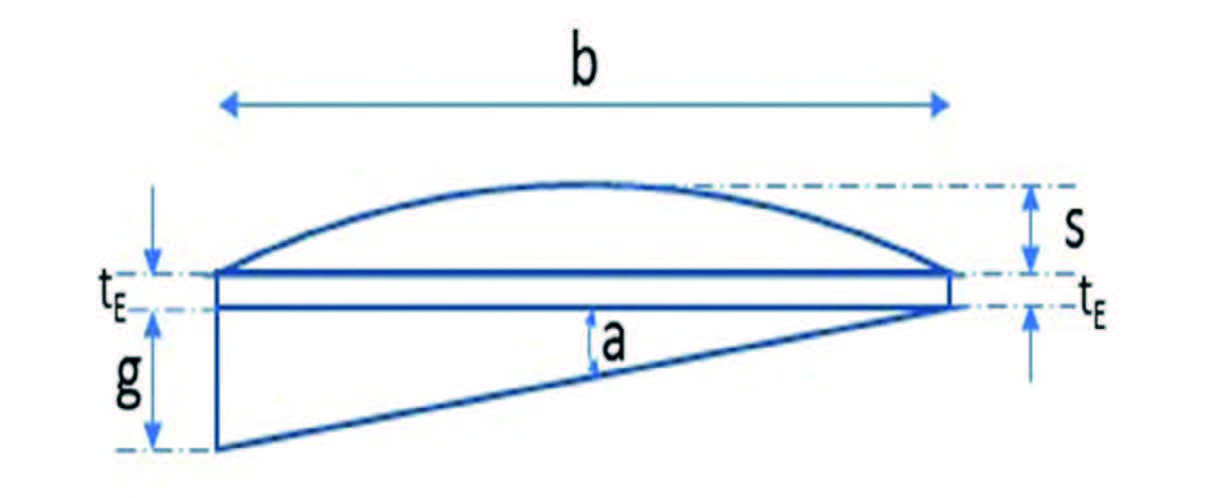
Figure 5: Thickness difference, g, of a plano prism or simple plano convex lens with prism
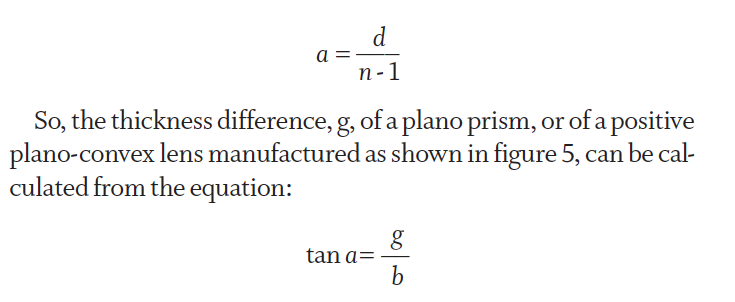
It is worthy of note that the thickness of a lens that incorporates a prism is rarely the sum of the thicknesses of the underlying lens and a plano prism with which it is to be combined during the surfacing process. This is most obvious in minus lenses, as shown in figure 6, and is also dependent upon the frame and the patient’s centration details. Nevertheless, the thickness difference remains the same even though the lens can be surfaced to a substance substantially thinner than the sum of its components as drawn.
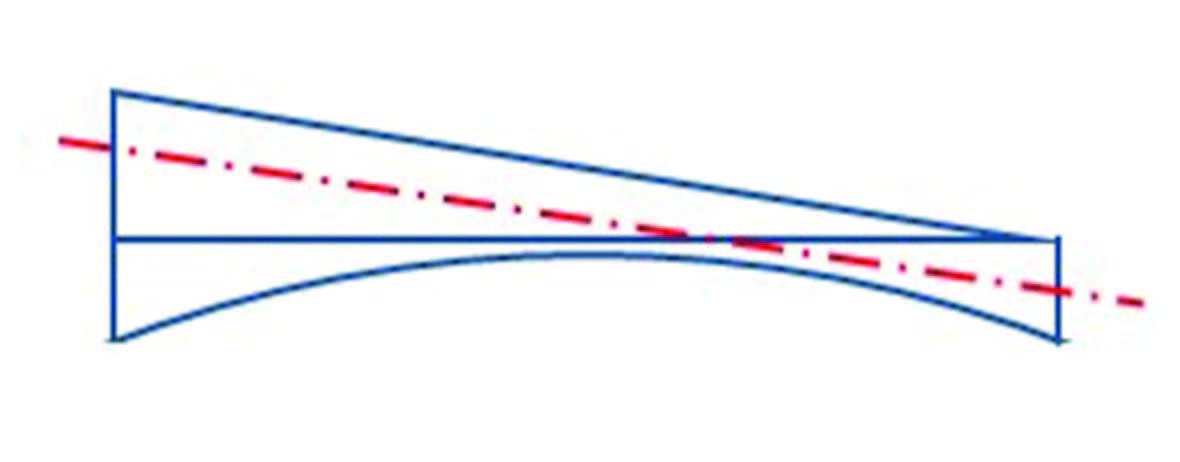
Figure 6: Thickness difference in a minus lens
Prism orientation
A prism is oriented before the eye according to the direction of the line that joins the apex and base of the prism perpendicularly (figure 7). If the lens has been edged round then the apex will correspond with the thinnest edge substance, and the base with the thickest part.
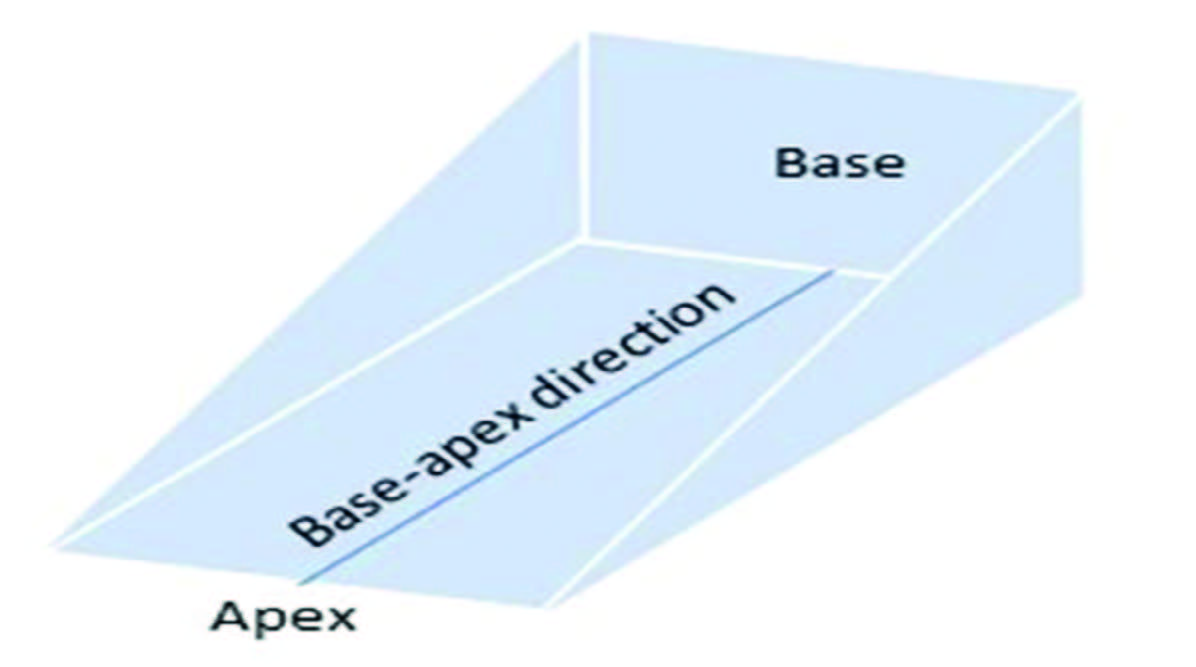
Figure 7: Base-apex direction
Unlike a cylinder axis, which can simply be expressed as running along a certain orientation within the range 1 to 180 degrees and acts in the same way if it is turned upside down by rotating through 180º, a prism acts differently at every point around the clock. Thus, a prism at 45º in the right eye could have a base direction that is UP and IN or a base direction that is DOWN and OUT along the same meridian. So, if standard axis is used for stating prism base direction, the additional qualifying description is essential.
Therefore, to avoid confusion and error, it is usual to use either 360º notation, where a single resultant is stated, or more commonly to state the prism required as a combination of vertical and horizontal prism, given that any single prism can be resolved into orthogonal components and any pair of prisms can be combined into a single resultant.
In 360º notation, the prism base that is DOWN and OUT along 45º in the right eye would be re-stated as having a base direction of 225º, whereas a prism along 225º in the left eye could be restated as DOWN and IN along 45º (see figure 8).
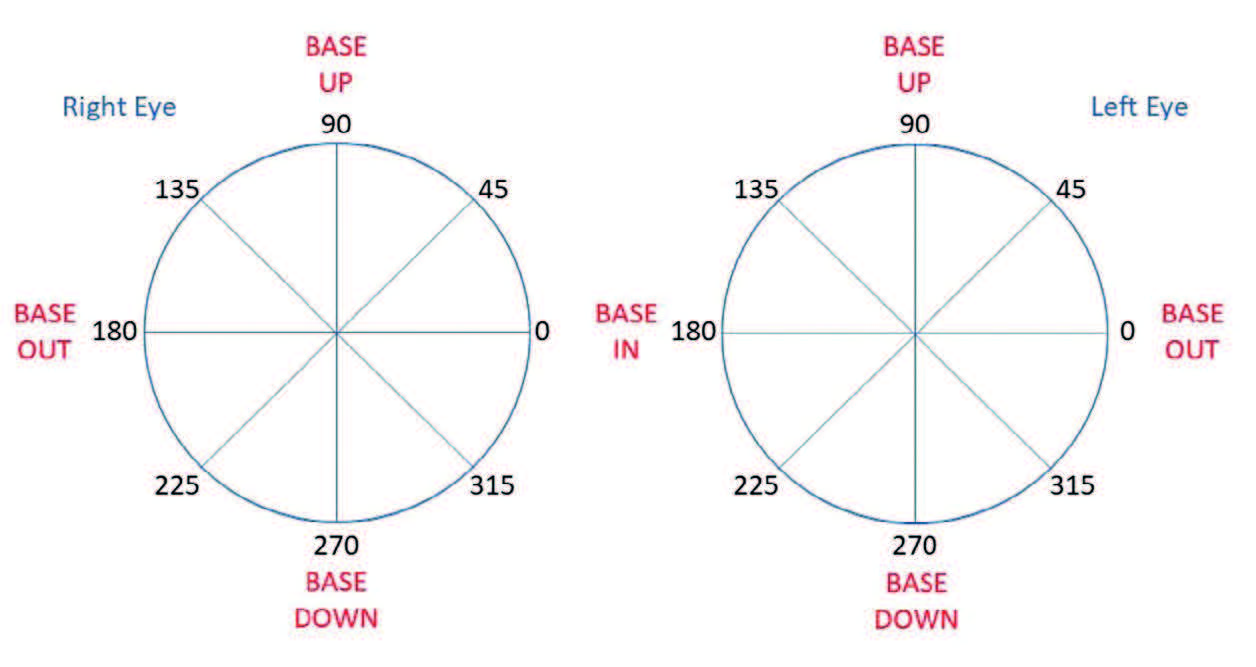
Figure 8: Standard and 360° base direction notation
The purpose of prism
Prism is prescribed when the visual axes are not parallel, either some or all of the time, and the purpose of the prism to alleviate symptoms of intermittent or constant double vision.
It is important to note that, where prism is prescribed in both eyes, they must work against each other so that the relative deviation between the visual axes is corrected and comfortable binocular single vision restored. The patient so corrected should no longer experience asthenopia (eye strain) or diplopia.
Hence, base UP in one eye will be accompanied by base DOWN in the other, and vice-versa, whereas in the horizontal meridian base OUT in the right eye would be found with base OUT in the left.
Similarly, base IN is appropriate in both eyes as the eyes are moving in opposite directions. Students often struggle with the concept of base IN prism, which for distance vision is prescribed to correct for eyes that are divergent relative to each other. Yet base IN prism is most often seen for near vision when the eyes are converging to see a near point. Practitioners must be mindful that the situation is relative, and base IN for near means that, relative to the normal position where the visual axes converge on the near point of interest, the eyes are relatively divergent. Put another way, it is used when the eyes have insufficient convergence. The prisms do not aid convergence, as is commonly stated. They simply displace the image in each eye so that binocular single vision can be achieved comfortably with the lesser amount of convergence that is available.
A note about yoked prisms
Based on data gleaned from a large practice management database, the authors estimate that prism is prescribed in fewer than 1% of sight tests that result in a prescription being issued. And very occasionally, prescriptions are encountered that break the rules with regard to prisms opposing each other. Consider this example.
Case 1. A patient who used an electric wheelchair had a spinal condition that meant his head was pointing to the right even when travelling forwards, such that he had to look leftwards through his spectacles to see obstacles ahead of him. He was prescribed large equal prisms, base OUT in the left eye and base IN before the right eye to enable him to see straight ahead more comfortably.
Where, using 360º notation, two equal prisms lie with their bases in the same direction, the emergent rays from a distant object, although deviated, remain parallel. In this instance, the prisms are said to be ‘yoked’. A yoke is something that joins together, such as the part of a shirt that fits the shoulder, or the wooden frame that in bygone times joined draught oxen at their necks when pulling a plough. Consider a second example of yoked prisms.
Case 2. An elderly woman with severe curvature of the upper spine, and whose natural head posture meant she could only look at the floor, was unable to lift her head to see straight ahead. Her problem was solved by fitting lenses with large equal base UP prisms right and left into a snooker spectacle with retroscopic (negative pantoscopic) angle (measured relative to her visual axis not the horizontal as is customary) to bring the area ahead of her into view.
Similar yoked corrections are sometimes offered to bed-bound, supine patients who are unable to lift their head to see objects other than those on the ceiling above, so called recumbent spectacles.
NICE cites the use of yoked prisms in stroke patients by orthoptists1 and they are also used by behavioural optometrists in treating patients whose visual problems accompany learning difficulties and neurological disorders. However, there is scant scientific evidence to support this latter use.2,3,4
Yoked prisms have been tried to help patients with macular conditions resulting in a central scotoma. The idea here is to ‘fool’ the brain into using a different part of the retina while leaving the head in its usual position, and so create an eccentric viewing point upon the retina. Though the use of yoked prisms in this case might not be expected to do anything other than move the scotoma and thus the patient’s direction of gaze, many who have habitually adopted a specific head position when reading over several decades and struggled to adapt this aspect of their visual impairment report yoked prisms, such as those found in E-scoop spectacles, to be beneficial.5
E-scoop spectacles (figure 9) incorporate base UP prism in each eye based upon the fact that the inferior macular suffers most damage in degenerative maculopathy and an assumption that it is best, on average, to displace the emergent light upwards towards the base of the prism and so utilise a superior portion of the retina. Interestingly online FAQs relating to E-scoop talk of the image being displaced upwards by base UP prism and, while the light is refracted upwards and the image on the retina is superior to the macula, the image the wearer sees is displaced downwards towards the apex of a base UP prism. As yet, the reported benefit of the yoked prism promoting eccentric viewing in these lenses, as distinct from the improved contrast gained by wearers from the yellow tint incorporated in E-scoop lenses, has yet to be proved satisfactorily.

Figure 9: E-scoop lenses – a form of yoked prism correction
The controversy over the benefit of yoked lenses highlights the need for both practitioners and students to be very clear in their communication during a consultation about what they are referring to regarding prism use. This is especially important if they are to avoid making errors of expectation as nothing will cause a loss of confidence more quickly than a patient seeing for themselves the exact opposite of what they are being told should be happening.
Prism splitting
Prism is sometimes prescribed in one eye only, but in most cases can be split between the eyes in order that right and left spectacle lenses can be made of approximately equal thickness and weight. Eye care practitioners who are prescribing prism, and do not want it to be split, need to annotate the prescription accordingly.
Prism is split equally, or unequally, depending upon the equality or otherwise of the ametropia between the two eyes. Where the right and left lens powers are equal, the prism, if it is to be split, should be split equally. However, where there is anisometropia (a difference in prescription between right and left), the lower powered lens should have a larger proportion of prism to balance the lenses in terms of weight. This has obvious advantages in terms of cosmetic appearance and also prevents the spectacles being lopsided when worn, something which in itself could induce further prismatic effect that is not wanted.
Figure 10 shows the effect of splitting base OUT prism when used to correct esotropia or decompensated esophoria, where one eye turns or tends to turn inwards relative to the other.
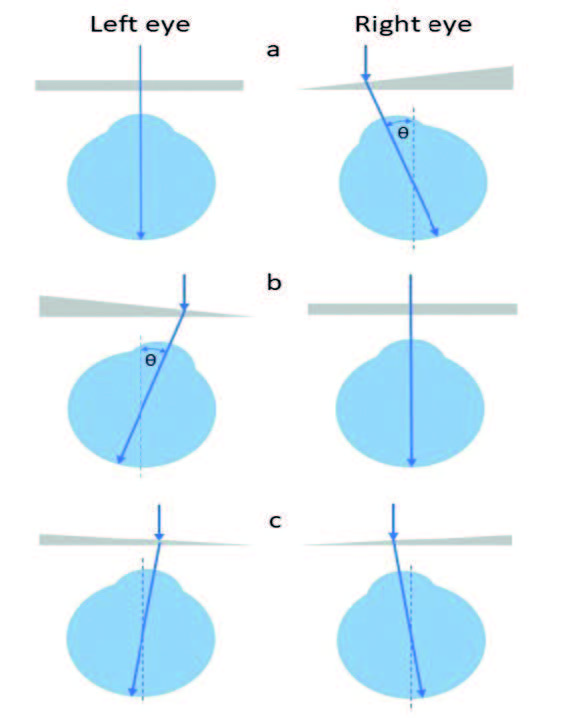
Figure 10: Splitting a base OUT prism; (a) prism before right eye, (b) before left eye, or (c) split between each eye
The patient may have been prescribed, for example, 4Δ Base OUT in the right eye (as in figure 10a). Here, the left eye is straight and fixates a distant object, while the right eye is turned inwards by the angle θ. This is identical to the deviation caused by the prism if binocular single vision is achieved and the right eye is similarly fixated on the same distant object. It can be appreciated that, if 4Δ Base OUT prism was placed before the left eye (figure 10b), then the right eye would now be straight and the left eye turned in by the same angle. Alternatively, the prism could be split equally, 2Δ Base OUT in each eye (as shown in figure 10c). This all assumes equality of acuity and without significant amblyopia having been established in the aberrant eye.
Figure 11 shows the effect of splitting base UP prism prescribed before the left eye (figure 11a) which is turned or tending to turn downwards (left hypotropia /decompensated left hypophoria).
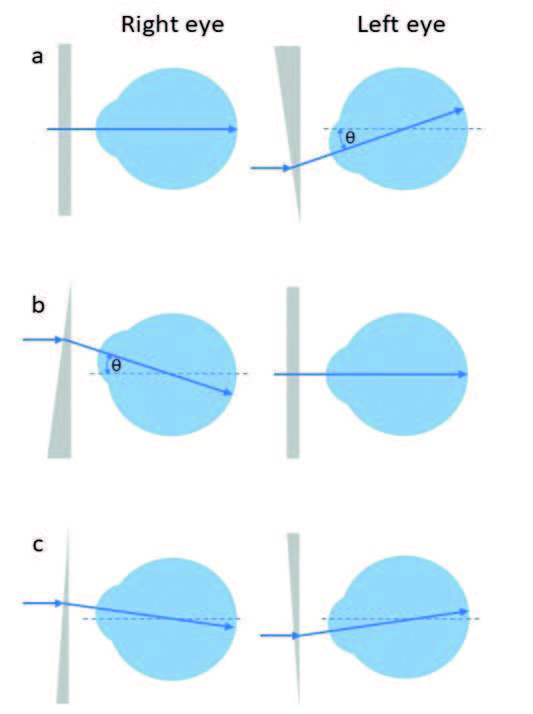
Figure 11: Splitting a vertical prism; (a) base UP before left eye, (b) base DOWN before right eye and (c) split between the two eyes
If the prism was 3Δ Base UP Left, then it can be seen the left visual axis is depressed relative to the right which is straight. The same relative position (angle θ) is achieved if 3Δ Base DOWN is placed before the right eye causing it to look upwards, and the left eye is straight (figure 11b). Hence left hypophoria is the same as right hyperphoria and, when describing vertical prismatic imbalance, it is important to be very clear. Remember, hypo can easily be misheard as hyper, and they are equivalent to each other in the opposite eye. Alternatively, the prism could be split equally, 1.5Δ base DOWN right and 1.5Δ base UP left (as shown in figure 11c), the angle between the visual axes remaining the same at 3Δ = tan-1 (3/100) = 1.72º.
When prisms may not be split
There are some occasions when it is not appropriate to split prisms. Principally this is when to split the prisms would cause the patient to adopt an unnatural compensatory head tilt (ocular torticollis).
Strabismus is said to be concomitant when the eyes have full movement in every direction and the visual axes remain inclined to each other at a constant angle regardless of direction of gaze and, typically, causing constant diplopia (double vision) if of recent onset and there has been no adaptation having taken place. Esotropia linked to accommodation in uncorrected hypermetropia is a good example of concomitant strabismus. Incomitancy, on the other hand, presents with an angle of deviation that changes depending upon the direction of gaze, as occurs with underaction of extraocular muscles or the nerves supplying them. In concomitant cases, it is normal, and perfectly acceptable, to split the prism between the eyes in the proportion that best matches the rest of the prescription to create a balanced pair of lenses in terms of thickness and weight.
However, in cases of recent incomitant deviation, prism might be better placed before the aberrant eye to avoid diplopia. The amount may vary from the straight-ahead position and also during the process of adaptation, requiring regular alteration of the prism correction, using for example Fresnel prism overlays. In other cases, the strabismus may be such that one eye is totally, or partially fixed in position away from the usual primary position. Examples in the authors’ experience include a blow-out fracture to the floor of the orbit (often caused by a squash ball impact) and where the right inferior rectus muscle becomes trapped within the fracture. The eye is then effectively tethered in a depressed (infraducted) position.
Technically, base UP prism before the tethered right eye is the same as base DOWN prism before the left eye. However, the latter would cause the patient to tilt their head back to allow the deviating eye to look straight ahead without any prism before it (assuming equality of acuity), which could be done without going to the trouble of spectacles and prisms. Where the angle between the visual axes varies depending on the direction of gaze of the ‘good’ eye the heterotropia is said to be incomitant – in such cases it may only be possible to alleviate symptoms of diplopia in one direction of gaze – typically the primary direction for distance spectacles and an appropriately depressed position for near vision tasks.
Conclusion
So far, we have looked at the essentials of prismatic effect, and barely touched upon the terminology used to describe eye movements and disorders of muscle imbalance and binocular vision. In the next article we will explore the terminology relating to eye movements and refresh the associated anatomy and visual optics. We will then move on to explore case studies and scenarios relating to the dispensing of prescribed prisms and the solutions to problems associated with induced prismatic effect that is sometimes avoidable, and sometimes, as in the case of anisometropia, not.
Peter Black MBA FBDO FEAOO is senior lecturer in ophthalmic dispensing at the University of Central Lancashire, Preston, and is a practical examiner, practice assessor, exam script marker, and past president of the Association of British Dispensing Opticians.
Tina Arbon Black BSc (Hons) FBDO CL is director of accredited CET provider Orbita Black Limited, an ABDO practical examiner, practice assessor and exam script marker, and a distance learning tutor for ABDO College.
References
- www.nice.org.uk/guidance/cg162/evidence/full-guideline-pdf-190076509
- Barrett, B.T. (2009). A Critical Evaluation of the Evidence Supporting the Practice of Behavioural Vision Therapy. Ophthal. Physiol Opt. 29: 4-25.
- https://uk.cochrane.org/news/cochrane-reviews-vision-screening-and-reading-aids-updated
- www.pencru.org/media/universityofexeter/medicalschool/ subsites/pencru/pdfs/WtE_Yoked_Prism_April_2014.pdf
- Meehan N, Beirne R. E-Scoop lens and non-exudative age-related macular degeneration. Optician, 31.08.2018, PP 22-26
