In the last part of this series, we considered those intravitreal drugs used to manage neovascularisation and inflammation (see Optician 18.09.20). The intravitreal route of drug administration is also important in the management of a range of severe ocular infections and proliferative diseases.
INTRAVITREAL ANTI-INFECTIVES
Antibiotics
Intravitreal antibiotics are the treatment of choice in endophthalmitis resulting from an infection, either endogenous (caused by an infective agent already present within the body) or exogeneous (from an external infection source). Such endophthalmitis cases are extremely devastating to the eye and vision and a challenge for all ophthalmologists (figure 1).
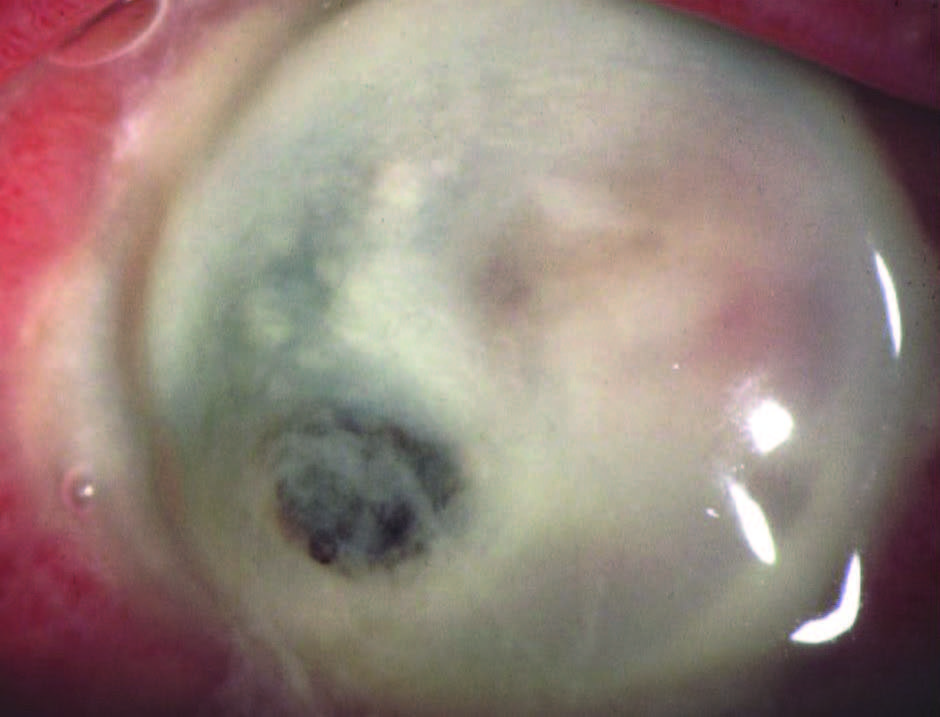
Figure 1: Endophthalmitis of infective origin is a devastating condition and difficult to manage
Topical antibiotics will not be able to reach the posterior segment at the desired therapeutic concentrations, while the distribution of systemically administrated drugs into the intraocular space via the retina is limited by the retinal pigment epithelium (RPE) and the retinal endothelium.1 Therefore, the only way to bypass the blood-retinal barrier and achieve high concentrations of drugs for prolonged periods of time is to administer these drugs intravitreally. Nevertheless, although intravitreal injections are effective in many cases, patients with severe infections or concurrent retinal detachments are often better managed with pars plana vitrectomy (PPVs) with silicone oil tamponades in order to decrease the bacterial load, remove inflammatory mediators, and reattach the retina.
The most commonly used intravitreal antibiotics (and their recommended doses) are as follows:
- Amikacin (0.4mg/0.1ml)
- Ceftazidime (2mg/0.1 ml)
- Vancomycin (2mg/0.1ml)
Vancomycin and ceftazidime are used as a first line treatment. Amikacin can be used on its own or in combination with steroids. However, amikacin carries a higher risk of retinal infarction and so is used only if well-defined penicillin or cephalosporin allergy has been established. The choice of antibiotic is guided by culture results and sensitivity patterns of the causative organism. Moreover, in order to make the best choice, we also need to be familiar with their pharmacokinetics.
It has been shown that the pharmacokinetics of intravitreal antibiotics is influenced by a number of properties.2 These include properties of the drugs and tissues into which they are introduced:
Ionicity; cationic antibiotics undergo clearance by passive diffusion into the aqueous and then leave the eye via the anterior chamber. They have a half-life of about 24 hours. Anionic antibiotics undergo a more rapid clearance, crossing the blood retinal barrier via the posterior route to exit the eye via uveal blood flow. This means their half-life is reduced in comparison, to about eight hours.
- Molecular weight; the ‘heavier’ the drug, the higher is their half-life. This means the injections do not have to be repeated as often.
- Solubility coefficient; antibiotic activity is influenced by whether they are lipophilic or soluble.
- Solution density; this may be higher or lower than that of water. Those antibiotics with a high solution density may precipitate under gravity and cause localised toxicity.
- Metabolism inside the vitreous; The vitreous, retina, ciliary body and the iris are known to contain enzymes involved in drug metabolism.
Other influences upon the drug activity and pharmacokinetics are related to the patient being treated and include:
- Patient age; the vitreous changes significantly with age (figure 2). The vitreous humour exists in two states, one liquid and the other a gel. Ageing modifies the ratio between these two forms, with the liquid increasing while the gel decreases. This liquefaction of the vitreous is responsible for an increase in drug diffusivity, particularly for high molecular weight drugs.3
- Presence or absence of ocular inflammation.
- Surgical status of the eye; clearance of those antibiotics which leave the eye through the anterior route is more rapid in aphakic eyes, while those which leave the eye primarily through the posterior route are cleared more rapidly in vitrectomised eyes. In silicone oil-filled eyes, it is also recommended to reduce the dose of antibiotics to prevent retinal toxicity.
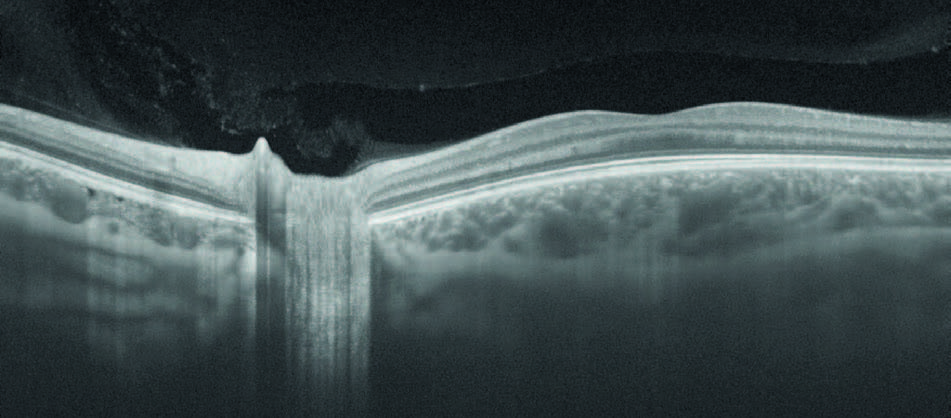
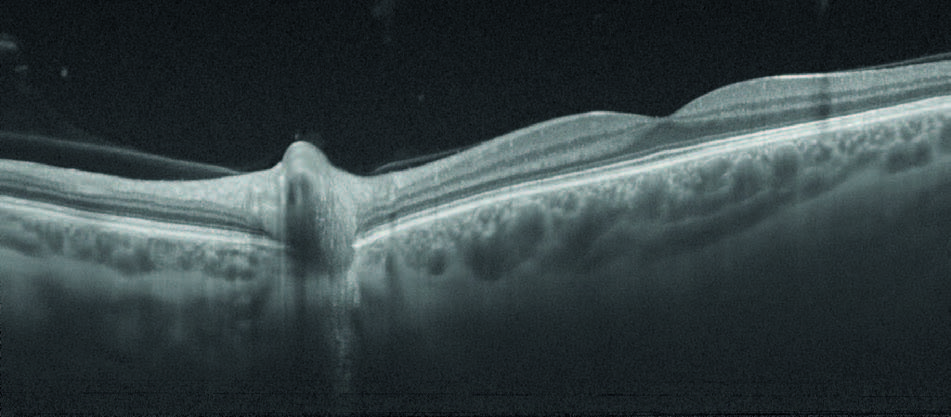
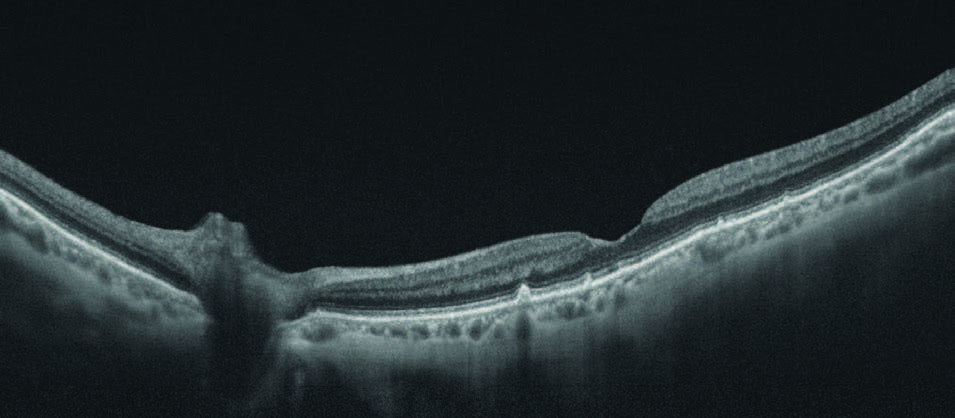
Figure 2: Vitreous changes with age shown by SS-OCT; (top) 18-year-old, (middle) 42-year-old and (lower) 84-year-old
Antifungals and antivirals
The most commonly used antifungal intravitreal drug is amphotericin B (5 micrograms/0.1ml). Other intravitreal antifungals are:
- Fluconazole (10 μg/0.1ml)
- Voriconazole (50-200 μg/0.1ml)
The drugs are administered as an acute treatment in cases of fungal endophthalmitis.
Foscarnet is an intravitreal antiviral drug used in the treatment of viral retinitis (figure 3) in immunocompromised patients (AIDS, cancer or transplant patients).
Intravitreal anti-infectives can pass into the systemic circulation via two routes. Hydrophilic drugs are cleared through the vitreous humour towards the anterior chamber, the Schlemm’s canal and, then, into the general circulation. Lipophilic drugs, however, pass through the retina and towards the capillaries, and from there into the systemic circulation. Therefore, it is possible that, in susceptible patients, they could induce systemic side effects similar to those encountered when these drugs are given systemically. Amikacin, for example, is a drug known for its renal toxicity, while amphotericin B can result in renal toxicity, electrolyte imbalances, cardiac arrhythmias, and hepatotoxicity. Nevertheless, a search of the current literature did not reveal any such effects after intravitreal administration of these drugs.
Intravitreal anti-metabolites
Intravitreal anti-metabolites are used for the treatment of a variety of intraocular conditions, ranging from malignant lesions (figure 3) to uveitis (figure 4), and in the prevention of proliferative vitreoretinopathy (PVR) in patients with retinal detachment. Drugs such as methotrexate and anti-tumour necrosis factor-α agents have been used intravitreally for the treatment of non-infectious uveitis. In addition, anti-vascular endothelial growth factor (VEGF) agents have been used in an effort to control uveitis-related complications, such as macular oedema as well as retinal and choroidal neovascularisation.4 A few of these drugs are described now.
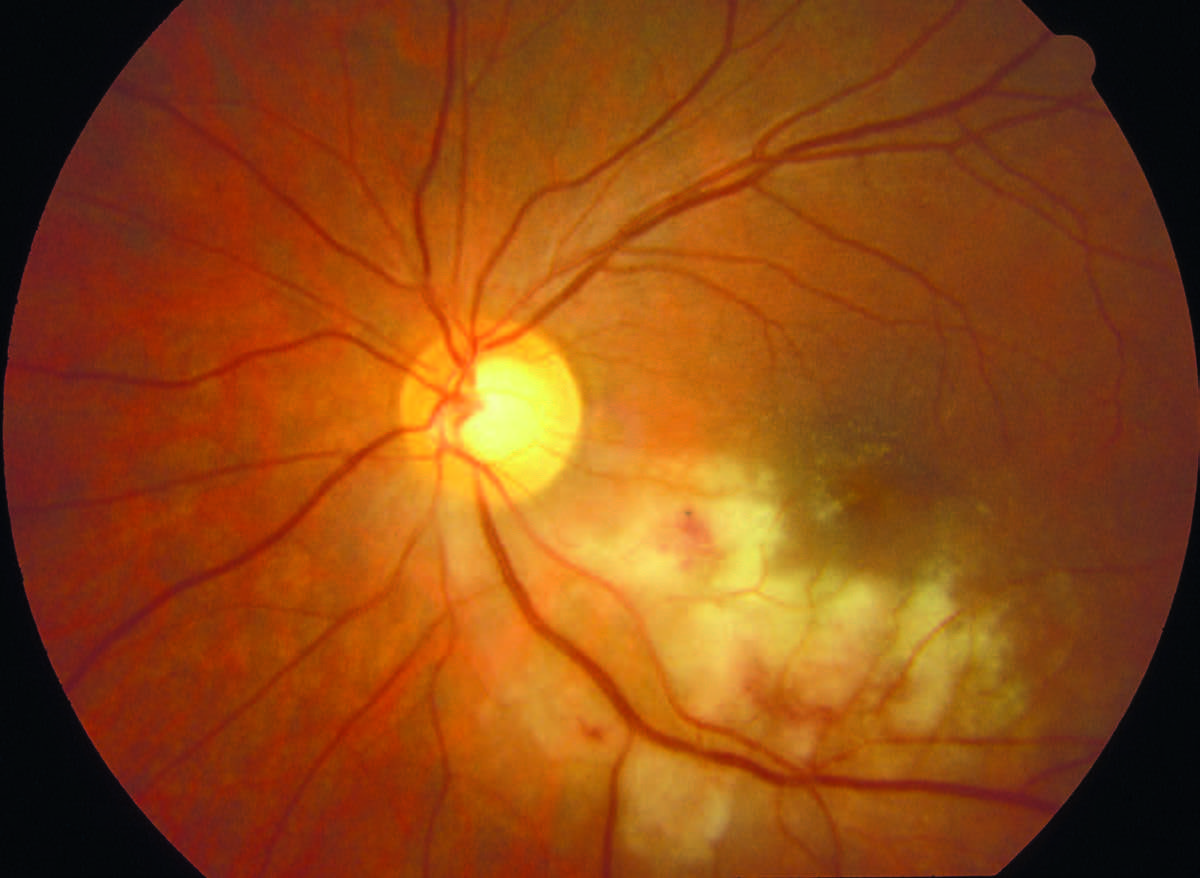
Figure 3: Viral retinitis caused by cytomegalovirus

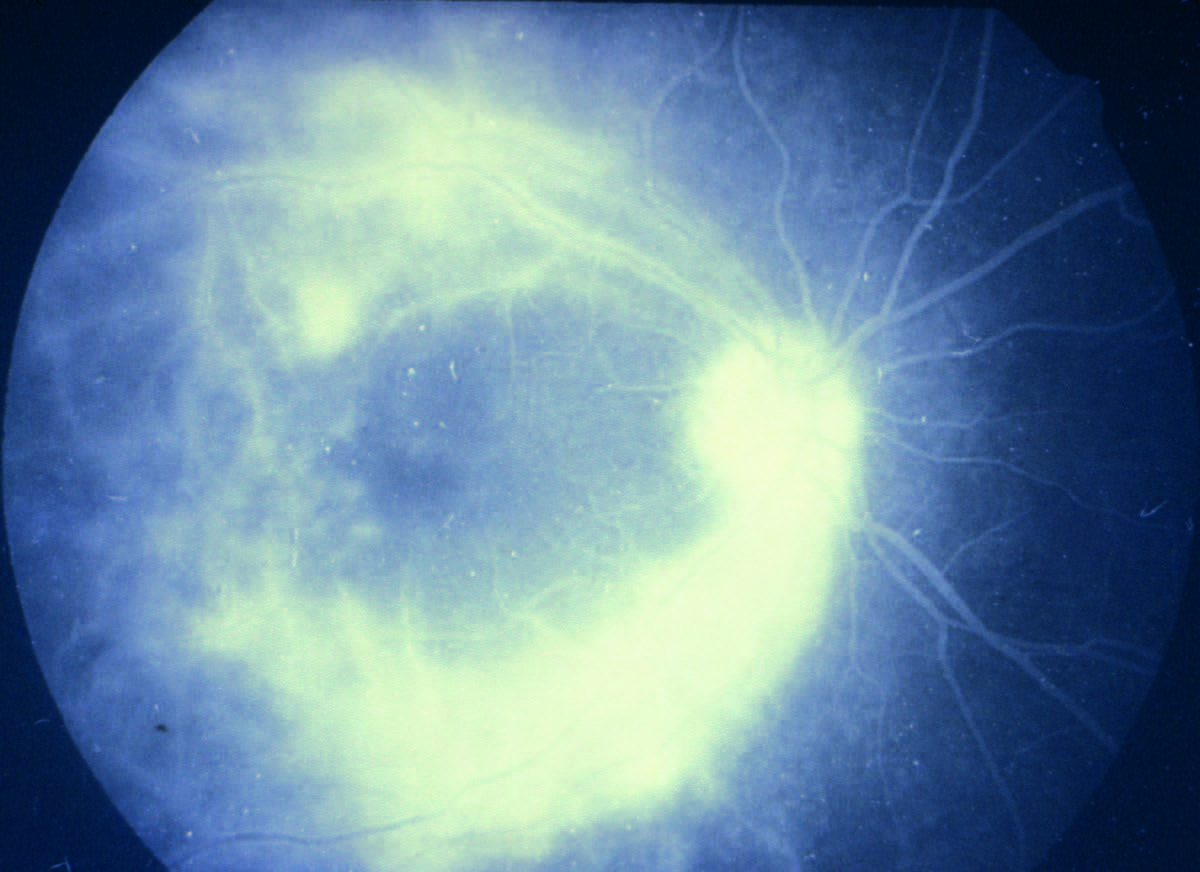
Figure 4: Lymphoma in full colour (top) and with retinal angiography (lower)
Methotrexate is an anti-metabolite immunosuppressive drug used in the treatment of lymphoma and also for non-infectious posterior uveitis. When used systemically, methotrexate is associated with many toxic side effects including cytopenia, hepatotoxicity, and interstitial pneumonia. No systemic side effects have yet been reported, however, after its intravitreal administration.
Anti-tumour necrosis factor-α (TNF-α) is a pro-inflammatory cytokine involved in the regulation of immune cells, tumour suppression and the inhibition of viral replication. It is also mentioned as having a role in the pathophysiology of those ocular inflammatory conditions related to autoimmune diseases and those with an inflammatory component, such as diabetic macular oedema and neovascular age-related macular degeneration.5 Examples of these drugs included:
- Infliximab
- Adalimumab
- Golimumab
Despite the fact that systemic administration of anti-TNF therapies are associated with a myriad of side-effects, no ocular or systemic side effects have yet been reported in association with the use of these drugs.
To prevent PVR after vitreoretinal surgery for primary rhegmatogenous retinal detachment (RD), 5-fluorouracil (5-FU) and low-molecular-weight heparin (LMWH) are used in the form of intraocular infusions.
5-FU is a pyrimidine analogue that interferes with DNA and RNA synthesis and may also be used in glaucoma surgery for its anti-scarring properties.6 On rare occasions, the drug is also used as an anterior chamber injection to prevent post-operative epithelial downgrowth.7 No systemic side effects have been reported after the intraocular administration of any of these drugs.
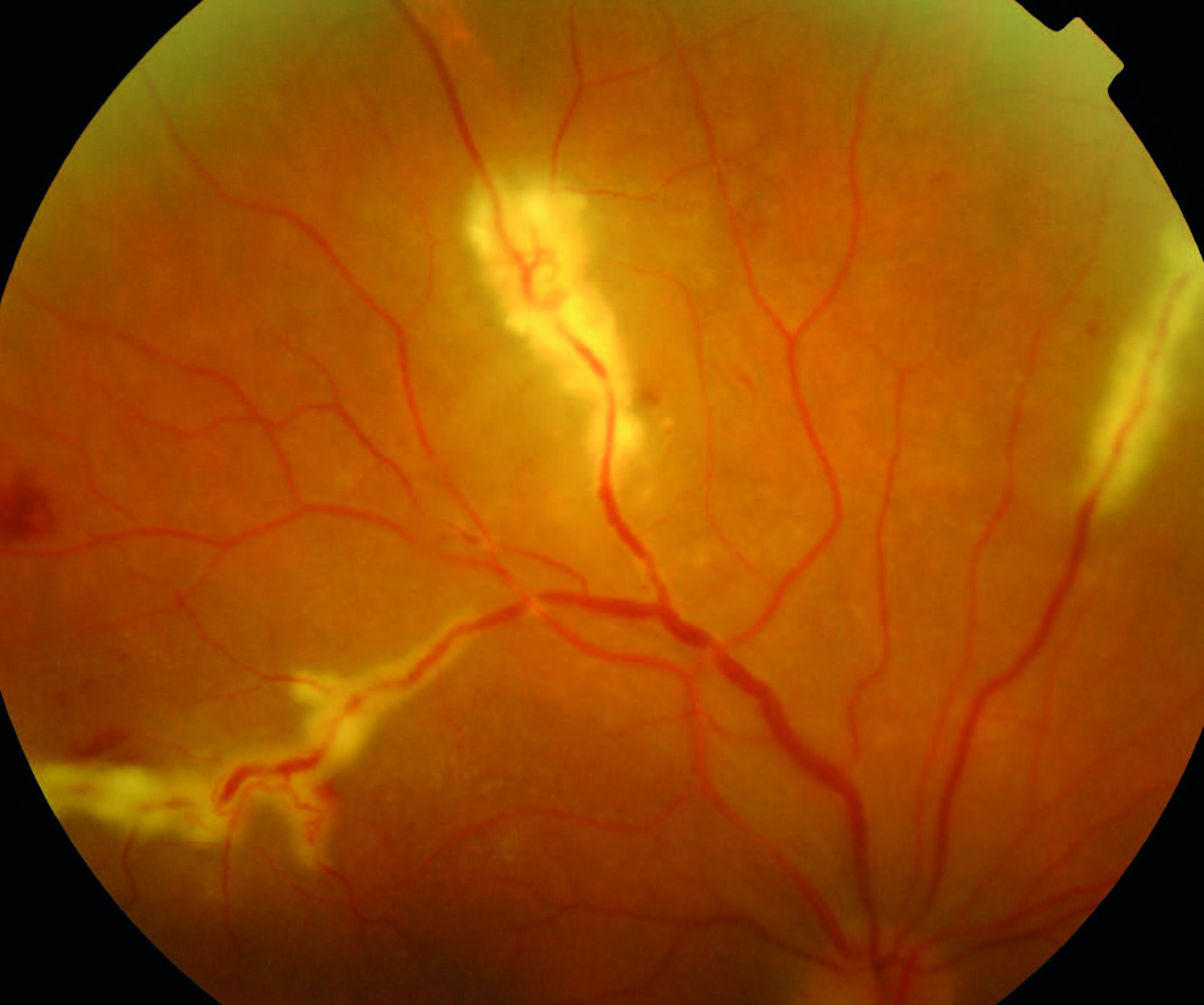
Figure 5: Chorioretinitis due to sarcoidosis
PERIOPERATIVE DRUGS
Perioperative preparation of the patient is essential for the success of any eye operation. In addition to the use of specific ocular drugs (such as mydriatics, for example), perioperative preparations also include adjustments to a patient’s systemic therapies for existing co-morbidities. This might be required where a patient has been prescribed antihypertensives and anticoagulants, for example, as these are medicines that could affect the bleeding during surgery.
Before surgery
Before eye surgery, it is important to think of the many factors that will allow the best surgical experience and to avoid any kind of complications during and after the procedure.
In glaucoma surgery, especially in the case of trabeculectomy, the state of the conjunctiva is very important for the success of the operation. Therefore, the perioperative preparation sometimes starts up to a month before the procedure. Indeed, some studies claim that topical ketorolac or fluorometholone for one month before surgery was associated with improved trabeculectomy outcomes.8 Other anti-inflammatories used perioperatively include:
- Diclofenac
- Flurbiprofen
- Ketorolac
- Nepafenac
These drugs are used for the prophylaxis and treatment of post-surgical inflammation and pain. Diclofenac and flurbiprofen are also used to prevent miosis during surgery. Their systemic side effects were discussed in a previous article (Optician 28.08.2020).
In order to reduce intraocular pressure (IOP) before cataract and glaucoma surgery, mannitol 20% (1-2g/kg body weight) is given about half an hour before the procedure. This drug should be avoided in patients with certain cardiovascular and renal diseases, as well as in patients with pulmonary oedema. Systemic side effects associated with this drug could include pulmonary congestion, electrolyte imbalance, acidosis, dry mouth, urinary retention, headache, blurred vision, nausea and vomiting among others.
Diamox (acetazolamide, a carbonic anhydrase inhibitor) can also be given before and after cataract surgery in eyes with glaucoma in order to reduce any post-surgery IOP elevation.9 Side effects associated with this drug can include blurred vision, dry mouth, drowsiness, loss of appetite, nausea, vomiting, diarrhoea, or changes in taste.
Anaesthesia is also a very important step before surgery. This can be performed using topical drugs, injections or using general anaesthesia.
The possible systemic side effects of topical anaesthetics have been presented previously (Optician 28.08.2020). Some ocular procedures require that anaesthetics are injected locally. If, by accident, the local anaesthetic is injected into the optic nerve, the drug may reach the brain and cause brainstem anaesthesia. This may result in impaired consciousness or coma, apnoea, cardiovascular instability and even death.10 The onset of symptoms is usually within 10 minutes of the anaesthetic injection and may last for many hours, depending on the local anaesthetic used.
Brain stem anaesthesia has been reported with retrobulbar/ peribulbar and sub-Tenon’s anaesthesia.11,12 Ophthalmologists should be aware of this risk and be prepared to resuscitate and transfer the patients urgently to the intensive care unit.13
Local and general anaesthesia have also been associated with anaphylaxis. In addition, some patients need pre-operative sedation using various drugs that depress the central nervous system (CNS). The reported complications of such sedation include excessive restlessness, sudden movement, and airway obstruction.14
Dilating drops (tropicamide and cyclopentolate) are given immediately before some surgical procedures. The systemic side effects of these drugs have already been discussed previously (Optician 31.07.2020).
It is important to avoid any risk of postoperative infection (endophthalmitis). This prevention starts at this stage, by using preoperative povidone iodine (PI), a broad-spectrum antiseptic used mainly for the treatment of contaminated wounds but also for preoperative preparation of the skin, mucous membranes and the ocular surface (figure 6). The European Society of Cataract and Refractive Surgeons (ESCRS) recommends PI (5-10%) application to the conjunctival cul-de-sac for at least three minutes before surgery.15 However, high concentrations can have potentially damaging effects on the cornea. PI may also cause allergic dermatitis or, in rare cases, anaphylaxis. Chlorhexidine is the most popular alternative antiseptic to use in patients with ‘iodine-allergy’.
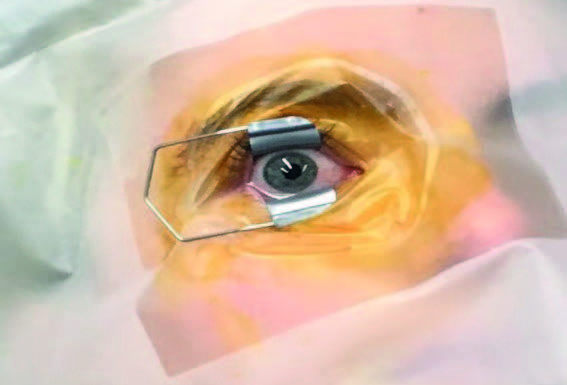
Figure 6: Pre-operative povidone iodine applied as antiseptic around entry site
During surgery
Acetylcholine 1%, a neurohormone that mediates nervous signal transmission in all cholinergic sites involving autonomic and somatic nerves, is instilled into the anterior chamber of the eye during surgery to induce a rapid miosis. As it is rapidly inactivated by acetylcholinesterase, there is little chance of inducing systemic side effects. However, there is a small risk that patients can develop slow heart rate, flushing, low blood pressure, breathing difficulty and sweating.
Intraocular sodium hyaluronate and balanced saline are used during ocular surgical procedures. This is generally well tolerated, but rare systemic side effects such as various allergic reactions can occur.
Mitomycin-C is an anti-tumour antibiotic, generally used in glaucoma surgery because of its ability to inhibit fibroblast proliferation and suppress vascular ingrowth. It is effective at prolonging the life of a filtration bleb. No systemic side effects are reported after this type of use.
5-Fluorouracine, as mentioned earlier, is a pyrimidine analogue that inhibits fibroblast proliferation and enhances bleb formation and function in glaucoma surgery. The treatment with this drug is not associated with known systemic side effects.
It is routine to use intracameral or subconjunctival antibiotic at the end of surgery. The National Institute for Health and Care Excellence (NICE) recommends using intracameral cefuroxime to prevent endophthalmitis.16 This drug, administered using this procedure, seems to be safe even for those with penicillin allergies.
After surgery
The mainstays of topical antibiotics in the perioperative period are the fluoroquinolones, which have a wide spectrum of coverage and good penetration into ocular tissues. They are given for about one to two weeks after surgery. The side effects of fluoroquinolones have been discussed elsewhere (Optician 28.08.2020).
In addition to antibiotics, steroid preparations are also given as routine to control the inflammatory response after surgery. Their dosing is for a few weeks, depending on each patient’s response after surgery. When so used, the IOP should be carefully monitored. The systemic side effects of various topical steroids have been previously discussed (Optician 28.08.2020). In patients who have previously developed a disproportionate increase in IOP when treated with traditional corticosteroids, loteprednol (Lotemax) is the preferred drug. Headache and vomiting are the most common systemic side affects, although they occur rarely.
One percent apraclonidine, an alpha-2 adrenoreceptor agonist, may be instilled one hour before and immediately after extracapsular cataract extraction with artificial lens implantation. This may help prevent an increase in IOP after the operation. This drug is contraindicated in patients with unstable cardiovascular diseases. It can result in systemic side effects such as constipation, depression, dizziness, dry mouth, fatigue, headache, nausea; postural hypotension, sedation, sexual dysfunction, sleep disorders and vomiting.17
Dr Doina Gherghel is an academic ophthalmologist with a special interest in inter-professional learning for optometrists.
REFERENCES
- Maurice DM, Mishima S. In: Handbook of experimental pharmacology. Sears ML, editor. Springer, Berlin-Heidelberg; 1984. Ocular pharmacokinetics
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4306439/
- https://www.mdpi.com/1999-4923/10/2/66/htm
- https://www.wjgnet.com/2218-6239/full/v5/i3/125.htm
- Croft M. The role of TNF superfamily members in T-cell function and diseases. Nature Reviews Immunology, 2009;9:271-285
- https://pubmed.ncbi.nlm.nih.gov/24554410/
- https://jamanetwork.com/journals/jamaophthalmology/fullarticle/272104
- https://pubmed.ncbi.nlm.nih.gov/20382428/
- https://www.healio.com/news/optometry/20170216/oral-acetazolamide-reduces-iop-elevation-during-after-cataract-surgery#:~:text=Oral%20acetazolamide%20given%201%20 hour,more%20postoperatively%2C%20according%20to%20 researchers
- Chin YC, Kumar CM. Brainstem anaesthesia revisited: Mechanism, presentation and management. Trends in Anaesthesia and Critical Care, 2013;3(5):252–256.
- Eke T, Thompson JR. Serious complications of local anaesthesia for cataract surgery: a 1 year national survey in the United Kingdom. Br J Ophthalmol 2007;91(4):470–475;
- Kumar CM, Eid H, Dodds C. Sub-Tenon’s anaesthesia: complications and their prevention. Eye (Lond) 2011;25(6):694–703
- Royal College of Ophthalmologists & Royal College of Anaesthetists. Local Anaesthesia for Ophthalmic Surgery. (Internet). London: 2012. Feb, p. 38
- https://www.rcophth.ac.uk/wp-content/ uploads/2014/12/2012-SCI-247-Local-Anaesthesia-in-Ophthalmic-Surgery-2012.pdf
- Barry P, Seal DV, Gettinby G, et al. ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery: Preliminary report of principal results from a European multicenter study. J Cataract Refract Surg 2006;32(3):407-10
- NICE Guideline [NG77] Cataracts in adults: management. 2017
- https://bnf.nice.org.uk/drug/clonidine-hydrochloride.html
