2020 marks the 25th anniversary of the introduction of daily disposable (1 day) contact lenses (CLs).1,2 According to recent worldwide prescribing data, an average of 45% of soft lenses prescribed in 2019 were 1 day lenses,3 varying significantly by country from 78% (Denmark) to 10% (Mexico). In the late 1990s, the first silicone hydrogel (SiH) reusable CLs were launched, although these were initially primarily for extended or continuous wear.4-7 Recognising the many benefits afforded by their high oxygen transmissibility, it was not long before eye care professionals (ECPs) started prescribing them for daily wear;8-11 however, it was not until 2008 that the first SiH 1 day lenses became widely
available.12
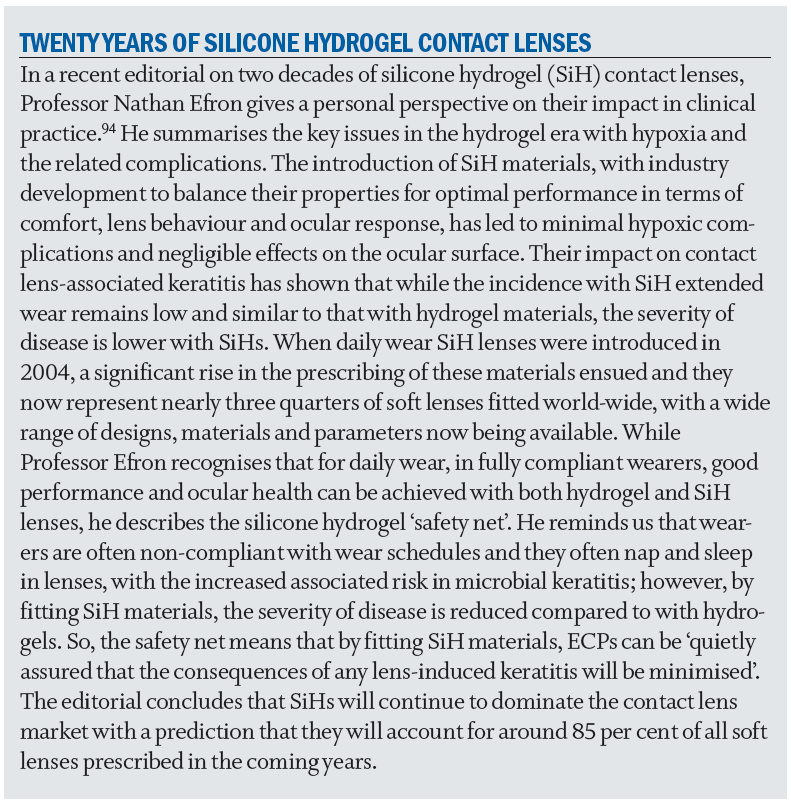
Figure 1 provides a summary of soft lens prescribing patterns from data collected each year by the International CL Prescribing Trends Consortium.13 There has been a steady decline in patients being fitted with reusable daily wear hydrogels and a corresponding increase in reusable SiH soft lenses, which then plateaued around 10 years ago. Prescribing of hydrogel 1 day lenses has remained relatively constant over the past two decades; however, there has been a steady increase in the prescribing rates of SiH 1 day lenses since their introduction, with SiH now the most prescribed lens material in the 1 day category. Interestingly around 90% of monthly replacement CLs have recently been reported to be SiH materials, as compared with only around 60% of 1 day CLs.3
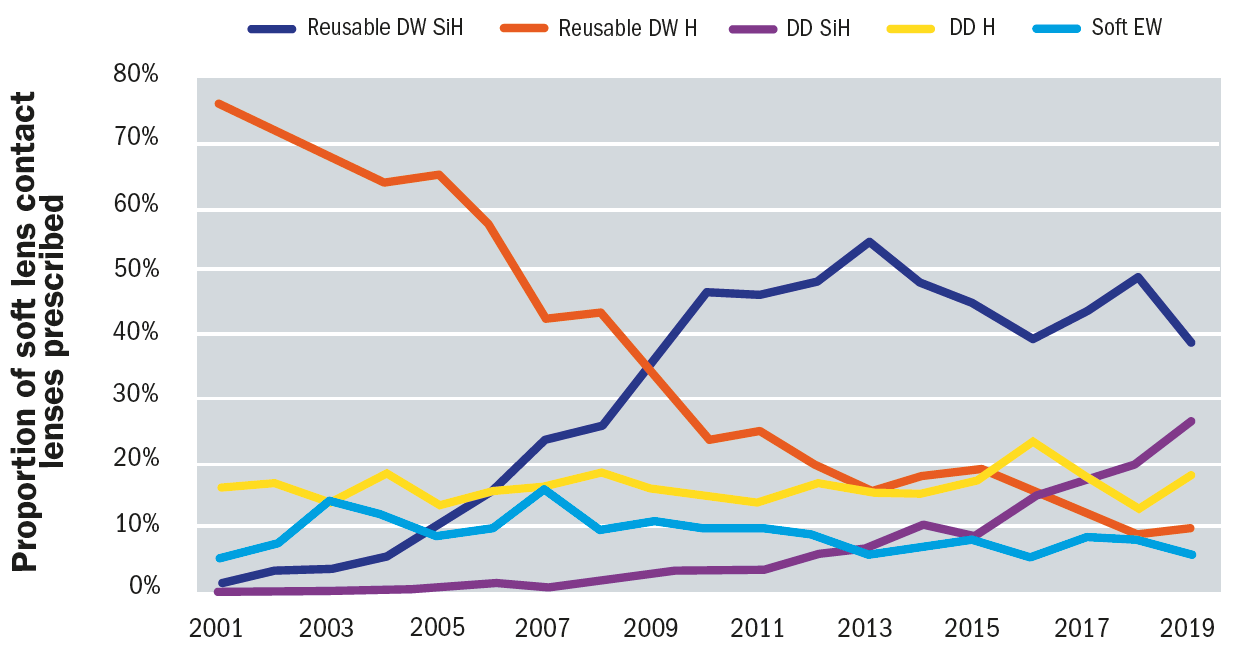
Figure 1: International Prescribing of Soft Contact Lenses 2001 to 2019. Data provided by the International Contact Lens Prescribing Trends Consortium13
What do ECPs Believe is Best for their Patients?
To find out what drives ECPs’ perceptions regarding prescribing 1 day SiH CLs, a survey was conducted among 300 ECPs in the US, UK and Japan.14 ECPs rated their level of agreement with statements relating to 1 day SiH CLs in the categories of patient’s eye health, comfort, satisfaction, standard of care and a series of other statements including oxygen requirements, lens design and cost. Clearly ECPs recognise the health benefits of 1 day SiH CLs with 90% agreeing that ‘Silicone hydrogel is the healthiest lens material for my 1 day patients’, 91% that ‘SiH 1 day lenses provide better long term eye health for my patients than hydrogel 1 day lenses’, and 90% that ‘SiH 1 day lenses provide a better wearing experience for my patients than hydrogel 1 day lenses’.
Even though the majority of ECPs agree that SiH CLs should be the standard of care for the 1 day modality, the barrier to prescribing them for more patients continues to be reported as presumed higher cost than 1 day hydrogel CLs; 95% reported that ‘If cost was equivalent, I would choose SiH over hydrogel for my 1 day patients’.14 Unfortunately many ECPs decide what their patients are prepared to pay for newer technology CL materials and designs, without even having this discussion with them,15 and despite some SiH 1 day lenses now being available at the same, or even lower, cost than their hydrogel equivalent. In an online survey of 1,520 adult CL wearers, 68% said they would expect their ECP to recommend the lens that provides 100% of the oxygen their eyes need regardless of cost, and 75% indicated they would follow their ECP’s recommendation, regardless of the lens cost.16
What Exactly are the Benefits of a Daily Disposable Modality?
Whether SiH or hydrogel, 1 day CLs, offer many benefits for both patients and ECPs, including:
- Convenience – no need to clean and disinfect after use
- No requirement for contact lens case maintenance
- Spare lenses always readily available
- Less spoliation from deposits17-19
- Absence of solution interactions with the ocular surface20-23
- Protection from environmental allergens24,25
- Ideal for part time or occasional wearers26
- Lower incidence of infiltrative and infective events compared to reusable CLs27,28
Arguably, the most important benefit though is fewer adverse events. 1 day lenses have been reported to be protective against the development of corneal infiltrative events (CIEs) and reduced their risk by 75% when compared with reusable modalities.28 A rate of only 0.2% symptomatic CIEs per year has been reported in a large post-market surveillance registry study, which is significantly lower than previously reported rates for reusable soft CLs of 3% to 4% per year.27 These findings are supported by a recent investigation of the subclinical inflammation of the ocular surface, in which a minimal subclinical inflammatory response was reported following one week of wear with a SiH 1 day CL when compared with no lens wear, in contrast to an up-regulated inflammatory response with reusable contact lenses.29 Furthermore, in comparisons between spectacle and 1 day wearers, very few or no differences have been reported in clinical performance and ocular response, with no reports of serious adverse events and an extremely low incidence of CIEs and/or CL associated papillary conjunctivitis in 1 day wearers.30, 31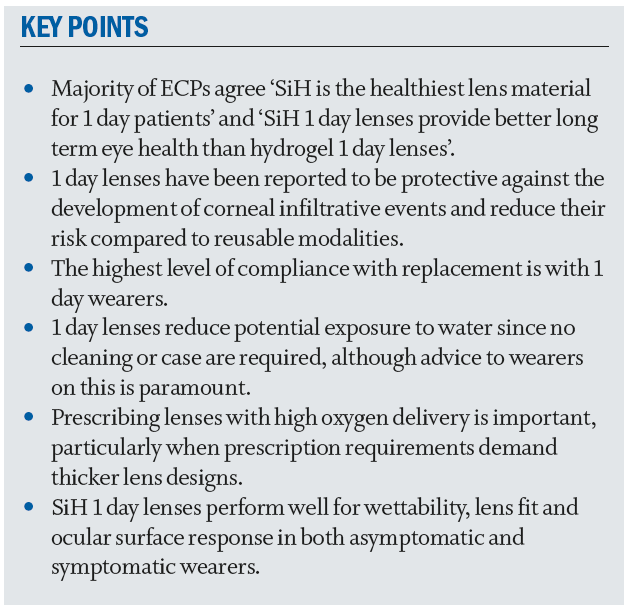
Daily Disposable Contact Lenses for Children
With all of these benefits, it is not surprising that 1 day lenses are frequently the first choice of CL for children, and a number of studies have reported success with this modality of wear in children.32-35 In a recent review, Bullimore reported no difference in the incidence of CIE events in children and adults and suggested that rates may even be lower for younger children.36 This finding was supported by the results from a retrospective review of 581 myopic children fitted with hydrogel 1 day lenses in six studies; no serious or significant adverse events were reported and there were only two cases of non-significant CIEs.37 Similarly, over a three-year study period with children wearing 1 day CLs, no serious ocular adverse events and only four asymptomatic, non-significant CIEs were observed.35 Contact lenses often improve a child’s view of themselves, including their view of their physical appearance, sporting ability and acceptance among friends.33
Are Contact Lens Wearers More Compliant with 1 Day Contact Lens Wear?
ECPs recognise that their patients are not always compliant with wear, care and replacement of their CLs. Several studies have reported that patients are most compliant with replacement of 1 day lenses.38-43 Often the reason given for not replacing lenses when scheduled is that the patients simply forget which day to replace them on, which is not an issue for a 1 day lens. While compliance with replacement of 1 day CLs is high, it is not 100%, with approximately one in 10 wearers reporting occasional re-use of 1 day lenses, and the primary reason for doing so is to save money. In a survey conducted in Italy, wearer attitudes towards CL use were assessed; psychological factors may play a role in compliance and recommended that ECPs warn 1 day CL wearers of the negative consequences when 1 day lenses are reused and how these can be prevented.44 Compliance with 1 day CL replacement has been reported to vary by country, but no differences have been found with respect to lens material (SiH versus hydrogel), age, sex, frequency of lens wear (part time versus full time) or number of years of CL wear.44,45
Another aspect of non-compliance in CL wear is napping or sleeping while wearing lenses that have not been prescribed for closed-eye wear. Unfortunately 1 day CL wearers can be non-compliant in this regard too; studies report 35% to 87% of adult wearers occasionally nap and 23% to 50% occasionally sleep in their 1 day lenses,45-48 with wearing CLs overnight being highest in those aged 18 to 24.45 While overnight wear with any 1 day CL is neither indicated nor recommended, it is arguably of greater concern with hydrogel 1 day lenses.
Despite warnings not to use CLs in water environments, exposure of CLs to water has been shown to be a significant risk factor for infection, and in particular for developing Acanthamoeba keratitis.49-51 Unfortunately, many CL wearers are non-compliant and do expose their lenses to water, while showering or swimming, and some wearers report they occasionally rinse or store their soft CLs in water overnight.47,48 Compliant patients wearing 1 day CLs have reduced exposure to water since no cleaning or case are required; nonetheless, it is still important to counsel these wearers and a ‘no-water’ campaign has been launched to try to address this issue.52 And if wearers do inadvertently expose their lenses to water during wear, they should be advised to remove them promptly and dispose of them if a 1 day modality.
How Much Oxygen is Required for Successful 1 Day Contact Lens Wear?
All CLs, regardless of oxygen transmissibility (Dk/t), limit the supply of oxygen to the cornea to some degree. If hypoxia results, this can lead to corneal swelling or oedema,53 and chronic hypoxia can result in a number of ocular complications.54 Early studies by Holden and Mertz reported that to prevent oedema, Dk/t values of 24 and 87 x 10-9 barrers/cm were required for open eye and closed eye wear respectively;55 however, Dk/t is a physical property of the CL and does not take into account the physiology of the tear film, CL and cornea. Furthermore, there is not a linear relationship between Dk/t and oxygen supply and very high Dk/t values may only result in relatively small differences in the actual amount of oxygen reaching the cornea for higher Dk/t materials.54,56,57 Quoted Dk/t values generally refer to the centre of a -3.00DS lens, whereas actual values vary by lens power and across the lens; for example, the Dk/t in the periphery of higher minus and toric lenses can be lower than the quoted figure. In clinical practice, ECPs may find it helpful to refer to oxygen profile maps which show the Dk/t across the whole lens and can demonstrate how different prescriptions and lens designs influence this.58
Since most soft CLs are worn during the day and removed at night, the amount of corneal swelling that occurs in open eye wear is most relevant clinically and measurements of the CL, or cornea, should be made both centrally and peripherally. In a study designed to investigate the central and peripheral Dk/t thresholds, a Dk/t of at least 33 x 10-9 barrers/cm across the entire soft CL was reported to be required ‘for a typical wearer’, to avoid corneal oedema during open eye wear.59 While Dk/t values for some 1 day hydrogel CLs may meet this threshold in spherical lenses with low minus powers, this is unlikely for higher minus, plus and toric soft lenses. Indeed, when the variation in thickness across hydrogel and SiH 1 day lenses ranging in power from -12.00 to +6.00DS was evaluated, the Dk/t values were found to range between 9.5 ± 0.5 and 178.1 ± 5.1 x 10-9 barrers/cm.60 This highlights the importance of prescribing 1 day CLs with high Dk/t values, particularly when patients’ prescription requirements demand thicker lens designs.
In addition to oedema, a reduced oxygen supply can result in other physiological changes to the cornea and its associated tissues, and Papas has published an extensive literature review of this topic, in which he estimates the minimum oxygen
transmissibility values to avoid contact lens induced changes during both open and closed eye CL wear.54 In a further publication, the peripheral and central Dk/t needed in soft CLs to prevent corneal neovascularisation in daily wear was reported to be between 30 and 40 x 10-9 barrers/cm;61 similar to the value reported by Morgan et al to prevent corneal oedema in open eye wear.59
Some hydrogel 1 day CLs provide sufficient oxygen to prevent corneal oedema, neovascularisation and limbal and bulbar hyperaemia for daily wear62-65 and while no difference in biomicroscopy findings has been reported between SiH and hydrogel 1 day CL wearers in some recent studies,62,63 in one, the average wearing time immediately prior to the subjects’ visit was less than five hours62 and in the other,63 the assessments were after just six hours of wear. While survey data show that 1 day patients typically wear their lenses for approximately 11 hours per day.66 ECPs should also consider thicker designs or non-compliance with 1 day hydrogels, which could potentially induce signs of hypoxia and therefore SiH 1 day CLs may be the most appropriate lens of choice for such patients. In a recent review article on the performance of a hydrogel 1 day,67 the authors concluded that: ‘It remains true that there are situations where consideration of oxygen access is necessary, for example, those patients with higher spherical prescriptions or those requiring certain thicker toric lens designs.’
And as mentioned earlier, many wearers wear their lenses for long hours and a high proportion are non-compliant with respect to napping or sleeping during lens wear, despite being given advice to the contrary by their ECP. It has been reported that after a period of only one hour of closed eye wear during the day, there is significantly greater corneal swelling with hydrogel contact lenses after a one hour nap with around 50% of the overnight swelling response.68
So while signs of hypoxia have essentially been eliminated with SiH contact lenses, and are not widely seen in daily wear with modern lenses, when all things are equal it is preferable for ECPs to have 1 day options that can provide their patients’ eyes with sufficient oxygen to avoid potential hypoxia-related complications if these can easily be avoided with products that otherwise have equivalent performance.
How are Silicone Hydrogel and Hydrogel Contact Lens Materials Different?
SiH CLs provide significantly more oxygen to the cornea as a result of the siloxy groups in their polymers. Unfortunately these siloxy groups are extremely hydrophobic.69,70 Unless the silicone is masked from the surface of the lens, deposits can quickly build up on the lenses and their wettability is dramatically reduced, which can have implications for the wearer’s vision and comfort.71,72 This is because a wettable contact lens surface is required to maintain tear film stability wettability.73 In order to minimise the impact of SiH materials on the tear film, significant developments have been made to render SiH CL surfaces more wettable, including surface treatments, internal and external wetting agents and the incorporation of hydrophilic monomers,72 resulting in similar wettability to hydrogel materials.72,74-77
SiH CLs initially had higher modulus (stiffness) values than hydrogels.71,78-80 While this resulted in a higher incidence of mechanical complications, particularly with overnight wear,81 the modulus of today’s SiH materials is now more consistent with conventional hydrogels, and in some cases may actually be lower.
Busting the Myths
There are some common misunderstandings relating to SiH CLs, including:
- SiH lenses may be less comfortable than hydrogels because of their higher modulus
- SiH lenses provide more oxygen and are therefore more comfortable than hydrogels
- Some patients may be allergic to the silicone in SiH CLs
Let us address comfort first. In a recent survey, 88% of ECPs agreed with the statement ‘Silicone hydrogel 1 day lenses provide better long term wearing comfort for my patients than hydrogel 1 day lenses’ and 80% with ‘SiH 1 day lenses are more comfortable than hydrogel 1 day lenses’.14 Scientific evidence does not strongly support this belief; results from studies comparing the comfort of reusable SiH and hydrogel lenses have been equivocal,82,83 principally because several different factors and properties of CL design relate to comfort.84 For 1 day CLs, while some studies have shown greater comfort with SiH materials,85,86 others have reported no difference.62,87
Silicone is commonly used in medical devices, however true allergies to silicone are not directly caused by the material alone. While there have been occasional anecdotal reports, to date there is no evidence in the literature to support allergic responses to SiH CLs.88 Cases where possible allergic responses have been reported are more likely attributable to inflammatory reactions88,89 and since SiH 1 days are discarded after a single use, there is significantly less opportunity for this type of response.
An Overview of Current Daily Disposable Silicone Hydrogel Contact Lens Materials and Designs
Table 1 summarises the properties of today’s most commonly prescribed SiH 1 day CLs. This is not an exclusive listing and recently additional products have been introduced, but only in some countries. This table shows that spherical, toric and multifocal lens designs are all now available in a wide range of parameters.
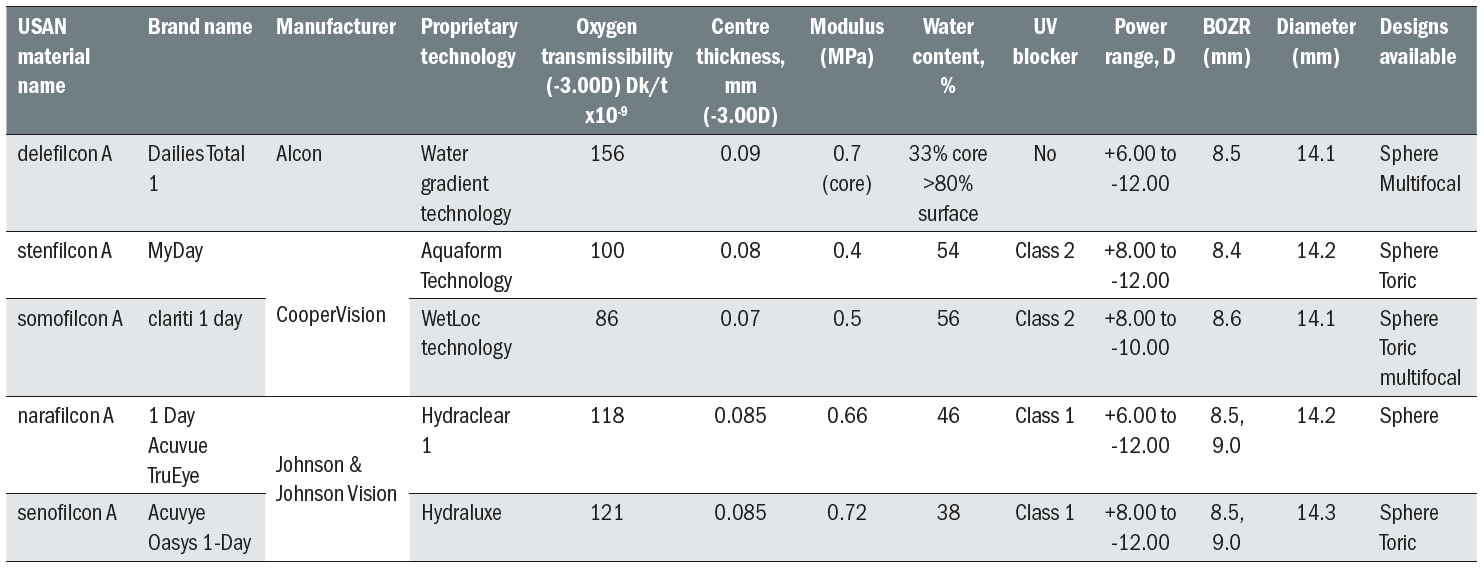
Table 1: Examples of widely prescribed Silicone Hydrogel Daily Disposable Contact Lenses in the UK
In studies conducted to evaluate lens wear in symptomatic and asymptomatic wearers, SiH 1 day lenses were shown to perform well with respect to wettability, lens fit and ocular surface response.85,90 Furthermore, in one of these studies longer comfortable wearing time and superior subjective comfort ratings were reported later in the day with a SiH 1 day when compared with a hydrogel 1 day CL.85 Results from a large, retrospective analysis in which wearers were evaluated over a three month wearing period with one of three SiH 1 day (delefilcon A, narafilcon A and somofilcon A) or two hydrogel (nelfilcon A and omafilcon A) CL types, neither lens type demonstrated superiority in comfort, and adverse event rates were low with both material types.62 Obviously factors other than lens material, such as lens design or surface characteristics, may also play a role in the performance of 1 day CLs; however, SiH 1 day CLs are able to offer many benefits and in some cases may actually perform better than their hydrogel counterparts. Ultimately the ECP must decide what CL is best for their individual patient; however, for patients who are at risk of hypoxia-related complications, those who have been unsuccessful with other soft lens materials and anyone who is new to CL wear, a 1 day SiH will frequently be the lens of choice. Since 1 day SiH lenses are becoming more widely available in multifocal designs, ECPs can now prescribe these lenses for their presbyopic patients.
Will Daily Disposable Silicone Hydrogel Lenses Reduce Contact Lens Dropout?
Last year, the global market value for soft contact lenses grew by 5% to 6% and was reported to approach $9 billion in 2019;91 however, it is not clear whether the actual number of CLs is increasing at the same rate. Despite the increased options available with respect to materials, designs, parameter availability and modalities for wear, dropout from wear is still prevalent. The primary reasons reported are discomfort, poor vision and difficulties with handling.92,93 Discontinuation has negative effects on patients, ECPs and the CL industry.
To date no studies have been conducted to specifically compare the drop out rates in wearers of SiH and hydrogel 1 day CLs. Therefore, we do not know whether patients who are either initially fitted, or who are refitted, with SiH 1 day CLs are more likely to be retained than those fitted with hydrogel 1 day lenses. Nevertheless, the convenience of 1 days combined with the health benefits of SiH materials should contribute to successful CL wear for the majority of patients, a belief already held by ECPs.14
The Bottom Line
ECPs strive to provide the best options for their patients by offering best contact lens technologies and replacement modalities that are available and they are embracing the transition to SiH for the 1 day modality as they have with reusable lenses over recent years. A 1 day modality will result in fewer complications, and SiH materials additionally provide long-term ocular health advantages, in particular for those with long-wearing days and thicker lens designs. There may be some occasions where 1 day SiH CLs are not available for a specific patient’s needs, or where hydrogel 1 day CLs are preferred by the patient; however, for the vast majority of patients SiH 1 day CLs are most likely to result in long term, successful wear.
Dr Kathy Dumbleton is a Clinical Associate Professor at the University of California, Berkeley and a Clinical Research Scientist and Consultant, and Anna Sulley is Global Medical Affairs Director at CooperVision.
References
- Efron N, Morgan S, Morgan PB. Clinical performance of a daily-wear, daily-disposable soft contact lens. Optician. 1995;210:18-22.
- Meyler J, Ruston D. The world’s first daily disposables. Optician. 2006;231:12.
- Morgan PB, Woods CA, Tranoudis IG, Efron N, Jones LW, Nelson L, et al. International Contact Lens Prescribing in 2019. Contact Lens Spectrum. 2020;35:26-31.
- Nicolson PC, Vogt J. Soft contact lens polymers: an evolution. Biomaterials. 2001;22:3273-83.
- Alvord L, Court J, Davis T, Morgan CF, Schindhelm K, Vogt J, et al. Oxygen permeability of a new type of high Dk soft contact lens material. Optom Vis Sci. 1998;75:30-6.
- Tighe B. Silicone hydrogel materials – how do they work? Silicone Hydrogels: The Rebirth of Continuous Wear Contact Lenses. Oxford: Butterworth-Heinemann; 2000. p. 1-21.
- Sweeney DF. The Max Schapero Memorial Award Lecture 2004: Contact lenses on and in the cornea, what the eye needs. Optom Vis Sci. 2006;83:133-42.
- Dumbleton K, Keir N, Moezzi A, Feng Y, Jones L, Fonn D. Objective and subjective responses in patients refitted to daily-wear silicone hydrogel contact lenses. Optom Vis Sci. 2006;83:758-68.
- Guillon M, Maissa C. Use of silicone hydrogel material for daily wear. Cont Lens Anterior Eye. 2007;30:5-10; quiz 71.
- Brennan NA, Coles ML, Ang JH. An evaluation of silicone-hydrogel lenses worn on a daily wear basis. Clin Exp Optom. 2006;89:18-25.
- Efron N, Morgan PB. Trends in the use of silicone hydrogel contact lenses for daily wear. Cont Lens Anterior Eye. 2008;31:242-3.
- Jones LW, Woods C. Compromises’ End? The introduction of a silicone hydrogel daily disposable lens. 2008; http://www.siliconehydrogels.org/editorials/jun_08.asp. Accessed September 27, 2019.
- Morgan PB. Personal Communication. 2019.
- Orsborn G, Dumbleton K. Eye care professionals’ perceptions of the benefits of daily disposable silicone hydrogel contact lenses. Cont Lens Anterior Eye. 2019;42:373-9.
- Hunter WG, Hesson A, Davis JK, Kirby C, Williamson LD, Barnett JA, et al. Patient-physician discussions about costs: definitions and impact on cost conversation incidence estimates. BMC Health Serv Res. 2016;16:108.
- Silicone hydrogel lenses. 2018. YouGov Plc. Total sample size was 1520 adults who wear contact lenses. Fieldwork undertaken March 26 - April 3, 2018. Survey carried out online.
- Nason RJ, Boshnick EL, Cannon WM, Dubow BW, Freeman MI, Kame RT, et al. Multisite comparison of contact lens modalities. Daily disposable wear vs. conventional daily wear in successful contact lens wearers. J Am Optom Assoc. 1994;65:774-80.
- Solomon OD, Freeman MI, Boshnick EL, Cannon WM, Dubow BW, Kame RT, et al. A 3-year prospective study of the clinical performance of daily disposable contact lenses compared with frequent replacement and conventional daily wear contact lenses. CLAO J. 1996;22:250-7.
- Cho P, Boost M. Daily disposable lenses: the better alternative. Contact Lens Anterior Eye. 2013;36:4-12.
- Papas EB, Carnt N, Willcox MD, Holden BA. Complications associated with care product use during silicone daily wear of hydrogel contact lens. Eye Contact Lens. 2007;33:392-3; discussion 9-400.
- Lofstrom T, Anderson JS, Kruse A. Tarsal abnormalities: a new grading system. CLAO J. 1998;24:210-5.
- Hamano H, Watanabe K, Hamano T, Mitsunaga S, Kotani S, Okada A. A study of the complications induced by conventional and disposable contact lenses. CLAO J. 1994;20:103-8.
- Porazinski AD, Donshik PC. Giant papillary conjunctivitis in frequent replacement contact lens wearers: a retrospective study. CLAO J. 1999;25:142-7.
- Hayes VY, Schnider CM, Veys J. An evaluation of 1-day disposable contact lens wear in a population of allergy sufferers. Contact Lens Anterior Eye. 2003;26:85-93.
- Wolffsohn JS, Emberlin JC. Role of contact lenses in relieving ocular allergy. Contact Lens Anterior Eye. 2011;34:169-72.
- Efron N, Morgan PB, Woods CA, International Contact Lens Prescribing Survey C. An international survey of daily disposable contact lens prescribing. Clin Exp Optom. 2013;96:58-64.
- Chalmers RL, Hickson-Curran SB, Keay L, Gleason WJ, Albright R. Rates of adverse events with hydrogel and silicone hydrogel daily disposable lenses in a large postmarket surveillance registry: the TEMPO Registry. Invest Ophthalmol Vis Sci. 2015;56:654-63.
- Chalmers RL, Keay L, McNally J, Kern J. Multicenter Case-Control Study of the Role of Lens Materials and Care Products on the Development of Corneal Infiltrates. Optom Vis Sci. 2012;89:316-25.
- Saliman NH, Morgan PB, MacDonald AS, Maldonado-Codina C. Subclinical Inflammation of the Ocular Surface in Soft Contact Lens Wear. Cornea. 2019.
- Morgan PB, Chamberlain P, Moody K, Maldonado-Codina C. Ocular physiology and comfort in neophyte subjects fitted with daily disposable silicone hydrogel contact lenses. Contact Lens Anterior Eye. 2013;36:118-25.
- Sankaridurg PR, Sweeney DF, Holden BA, Naduvilath T, Velala I, Gora R, et al. Comparison of Adverse Events with Daily Disposable Hydrogels and Spectacle Wear: Results from a 12-Month Prospective Clinical Trial. Ophthalmology. 2003;110:2327-34.
- Chalmers R, Hickson-Curran S, Keay L, Gleason W. Adverse events and retention of children and teens in a large daily disposable contact lens registry. Contact Lens Anterior Eye. 2018;41:S45.
- Walline JJ, Gaume A, Jones LA, Rah MJ, Manny RE, Berntsen DA, et al. Benefits of contact lens wear for children and teens. Eye Contact Lens. 2007;33:317-21.
- Walline JJ, Long S, Zadnik K. Daily disposable contact lens wear in myopic children. Optom Vis Sci. 2004;81:255-9.
- Chamberlain P, Peixoto-de-Matos SC, Logan NS, Ngo C, Jones D, Young G. A 3-year Randomized Clinical Trial of MiSight Lenses for Myopia Control. Optom Vis Sci. 2019;96:556-67.
- Bullimore MA. The Safety of Soft Contact Lenses in Children. Optom Vis Sci. 2017;94:638-46.
- Cheng X, Brennan NA, Toubouti Y, Greenaway NL. Safety of soft contact lenses in children: retrospective review of six randomized controlled trials of myopia control. Acta Ophthalmol. 2019;doi: 10.1111/aos.14283.
- Dumbleton K, Richter D, Bergenske P, Jones LW. Compliance with lens replacement and the interval between eye examinations. Optom Vis Sci. 2013;90:351-8.
- Dumbleton K, Richter D, Woods C, Jones L, Fonn D. Compliance with Contact Lens Replacement in Canada and the United States. Optom Vis Sci. 2010;87:131-9.
- Dumbleton K, Woods C, Jones L, Fonn D, Sarwer DB. Patient and practitioner compliance with silicone hydrogel and daily disposable lens replacement in the United States. Eye Contact Lens. 2009;35:164-71.
- Guthrie SE, Dumbleton K, Jones L. The association between eye examination frequency and contact lens purchase patterns. Contact Lens Spectrum. 2014;29.
- Rueff EM, Wolfe J, Bailey MD. A study of contact lens compliance in a non-clinical setting. Cont Lens Anterior Eye. 2019;42:557-61.
- Yeung KK, Forister JF, Forister EF, Chung MY, Han S, Weissman BA. Compliance with soft contact lens replacement schedules and associated contact lens-related ocular
complications: the UCLA Contact Lens Study. Optometry. 2010;81:598-607. - Livi S, Zeri F, Baroni R. Health beliefs affect the correct replacement of daily disposable contact lenses: Predicting compliance with the Health Belief Model and the Theory of Planned Behaviour. Cont Lens Anterior Eye. 2017;40:25-32.
- Dumbleton KA, Richter D, Woods CA, Aakre BM, Plowright A, Morgan PB, et al. A multi-country assessment of compliance with daily disposable contact lens wear. Contact Lens Anterior Eye. 2013;36:304-12.
- Bui TH, Cavanagh HD, Robertson DM. Patient compliance during contact lens wear: perceptions, awareness, and behavior. Eye Contact Lens. 2010;36:334-9.
- Cope J, Collier S, Rao M, Chalmers R, Mitchell G, Richdale K, et al. Contact Lens Wearer Demographics and Risk Behaviors for Contact Lens-Related Eye Infections — United States, 2014. Morbidity and Mortality Weekly Report. 2015;64.
- Wagner H, Richdale K, Mitchell GL, Lam DY, Jansen ME, Kinoshita BT, et al. Age, behavior, environment, and health factors in the soft contact lens risk survey. Optom Vis Sci. 2014;91:252-61.
- Anger C, Lally JM. Acanthamoeba: a review of its potential to cause keratitis, current lens care solution disinfection standards and methodologies, and strategies to reduce patient risk. Eye Contact Lens. 2008;34:247-53.
- Arshad M, Carnt N, Tan J, Ekkeshis I, Stapleton F. Water Exposure and the Risk of Contact Lens-Related Disease. Cornea. 2019;38:791-7.
- Carnt N, Samarawickrama C, White A, Stapleton F. The diagnosis and management of contact lens-related microbial keratitis. Clin Exp Optom. 2017;100:482-93.
- McCormick E, Derbyshire L. Campaigning recognition for ‘no water’ campaign 2016. 2017; https://www.aop.org.uk/ot/industry/charity/2016/06/13/%20campaigning-recognition. Accessed November 5, 2019.
- Leung BK, Bonanno JA, Radke CJ. Oxygen-deficient metabolism and corneal edema. Prog Retin Eye Res. 2011;30:471-92.
- Papas EB. The significance of oxygen during contact lens wear. Cont Lens Anterior Eye. 2014;37:394-404.
- Holden BA, Mertz GW. Critical oxygen levels to avoid corneal edema for daily and extended wear contact lenses. Invest Ophthalmol Vis Sci. 1984;25:1161 - 7.
- Brennan N, Morgan P. Clinical highs and lows of Dk/t. Part 1 - Has oxygen run out of puff? Optician. 2009;238:16-20.
- Brennan NA. Beyond flux: total corneal oxygen consumption as an index of corneal oxygenation during contact lens wear. Optom Vis Sci. 2005;82:467-72.
- OptiExpert TM. https://coopervision.com/practitioner/tools-and-calculators/optiexpert. Accessed September 6, 2019.
- Morgan PB, Brennan NA, Maldonado-Codina C, Quhill W, Rashid K, Efron N. Central and peripheral oxygen transmissibility thresholds to avoid corneal swelling during open eye soft contact lens wear. Journal of Biomedical Materials Research Part B: Applied Biomaterials. 2010;92:361-5.
- Lira M, Pereira C, Real Oliveira M, Castanheira E. Importance of contact lens power and thickness in oxygen transmissibility. Contact Lens Anterior Eye. 2015;38:120-6.
- Yeung KK, Yang HJ, Nguyen AL, Weissman BA. Critical Contact Lens Oxygen Transmissibility and Tear Lens Oxygen Tension to Preclude Corneal Neovascularization. Eye Contact Lens. 2018;44 Suppl 1:S291-s5.
- Diec J, Tilia D, Thomas V. Comparison of Silicone Hydrogel and Hydrogel Daily Disposable Contact Lenses. Eye Contact Lens. 2018;44 Suppl 1:S167-s72.
- Moezzi AM, Varikooty J, Luensmann D, Schulze MM, Ng A, Karkkainen T, et al. The short-term physiological impact of switching reusable silicone hydrogel wearers into a hydrogel daily disposable multifocal. Clin Ophthalmol. 2019;13:1193-202.
- Moezzi AM, Varikooty J, Schulze M, Ngo W, Lorenz KO, Boree D, et al. Corneal Swelling with Cosmetic etafilcon A Lenses versus No Lens Wear. Optom Vis Sci. 2016;93:619-28.
- Szczotka-Flynn L, Debanne S, Benetz B, Wilson T, Brennan N. Daily Wear Contact Lenses Manufactured in Etafilcon A Are Noninferior to Two Silicone Hydrogel Lens Types With Respect to Hypoxic Stress. Eye Contact Lens. 2018;44:190-9.
- Consumer insight survey UK. Adults who wear contact lenses: monthly replacement n=191, daily disposable n=279. CVI data on file 2018.
- Chalmers R, Brennan N, Ruston D. Contact Lenses: 2020 and beyond. Optician. 2020:23-7.
- Hamano H, Maeda N, Hamano T, Mitsunaga S, Kotani S. Corneal thickness change induced by dozing while wearing hydrogel and silicone hydrogel lenses. Eye Contact Lens. 2008;34:56-60.
- Kunzler JF. Silicone hydrogels for contact lens applications. TRIP. 1996;4:52 - 9.
- Kunzler J. Silicone-based hydrogels for contact lens applications. Contact Lens Spectrum. 1999;14:9 - 11.
- Tighe BJ. A decade of silicone hydrogel development: surface properties, mechanical properties, and ocular compatibility. Eye Contact Lens. 2013;39:4-12.
- Keir N, Jones L. Wettability and silicone hydrogel lenses: A review. Eye Contact Lens. 2013;39:100-8.
- Craig JP, Willcox MDP, Argüeso P, Maissa C, Stahl U, Tomlinson A, et al. The TFOS International Workshop on Contact Lens Discomfort: Report of the contact lens interactions with the tear film subcommittee. Invest Ophthalmol Vis Sci. 2013;54:TFOS123-TFOS56.
- Cheung S, Cho P, Chan B, Choy C, Ng V. A comparative study of biweekly disposable contact lenses: silicone hydrogel versus hydrogel. Clinical and Experimental Optometry. 2007;90:124-31.
- Thai LC, Tomlinson A, Doane MG. Effect of Contact Lens Materials on Tear Physiology. Optom Vis Sci. 2004;81:194-204.
- Varikooty J, Schulze MM, Dumbleton K, Keir N, Woods CA, Fonn D, et al. Clinical performance of three silicone hydrogel daily disposable lenses. Optom Vis Sci. 2015;92:301-11.
- Wolffsohn J, Hall L, Mroczkowska S, Hunt OA, Bilkhu P, Drew T, et al. The influence of end of day silicone hydrogel daily disposable contact lens fit on ocular comfort, physiology and lens wettability. Contact Lens Anterior Eye. 2015;38:339-44.
- Bhamra TS, Tighe BJ. Mechanical properties of contact lenses: The contribution of measurement techniques and clinical feedback to 50 years of materials development. Cont Lens Anterior Eye. 2017;40:70-81.
- Horst CR, Brodland B, Jones LW, Brodland GW. Measuring the modulus of silicone hydrogel contact lenses. Optom Vis Sci. 2012;89:1468-76.
- Kim E, Saha M, Ehrmann K. Mechanical Properties of Contact Lens Materials. Eye Contact Lens. 2018;44 Suppl 2:S148-s56.
- Lin MC, Yeh TN. Mechanical Complications Induced by Silicone Hydrogel Contact Lenses. Eye Contact Lens. 2013;39:115-24.
- Guillon M. Are silicone hydrogel contact lenses more comfortable than hydrogel contact lenses? Eye Contact Lens. 2013;39:86-92.
- Jones L, Brennan NA, González-Méijome J, Lally J, Maldonado-Codina C, Schmidt TA, et al. The TFOS International Workshop on Contact Lens Discomfort: Report of the contact lens materials, design, and care subcommittee. Invest Ophthalmol Vis Sci. 2013;54:TFOS37-TFOS70.
- Stapleton F, Tan J. Impact of contact lens material, design, and fitting on discomfort. Eye Contact Lens. 2017;43:32-9.
- Michaud L, Forcier P. Comparing two different daily disposable lenses for improving discomfort related to contact lens wear. Cont Lens Anterior Eye. 2016;39:203-9.
- Shah D, Richardson P, Vega J. Fitting MyDay into practice. Optician. 2013;246:12-6.
- Woods J, Ng A, Luensmann D, Jones L. Short-term comfort comparison of a low modulus hydrogel vs a higher modulus silicone hydrogel daily disposable lens. Contact Lens Anterior Eye. 2018;41:S42.
- Hall BJ, Jones LW, Dixon B. Silicone allergies and the eye: fact or fiction? Eye Contact Lens. 2014;40:51-7.
- Solomon A. Allergic manifestations of contact lens wearing. Curr Opin Allergy Clin Immunol. 2016;16:492-7.
- Varikooty JK, N.; Richter, D.; Jones, L. W.; Woods, C.; Fonn, D. Comfort response of three silicone hydrogel daily disposable contact lenses. Optom Vis Sci. 2013;90:945-53.
- Nichols JJ, Starcher L. Contact Lenses 2019. Contact Lens Spectrum. 2020;35:18-25.
- Dumbleton K, Woods CA, Jones LW, Fonn D. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens. 2013;39:93-9.
- Sulley A, Young G, Hunt C, McCready S, Targett MT, Craven R. Retention Rates in New Contact Lens Wearers. Eye Contact Lens. 2018;44 Suppl 1:S273-s82.
- Efron N. Twenty years of silicone hydrogel contact lenses: a personal perspective. Clinical and Experimental Optometry. 2020.
