Since the introduction of the very first progressive lenses, the inevitable non-adaptation has followed. Why? Because we are asking our patients to cope with ‘bendy blended lenses’ that give different amounts of magnification and distortion and which we expect them to tolerate.
Lens design has moved on considerably since the introduction of the first rudimentary designs, but it is well worth looking at a brief overview of how progressives have developed in order to have a greater understanding of the key causes of non-adaptation.
Evolution of progressive lenses
Arguably, the first commercially available progressive lens was introduced in 1922, designed by Duke Elder and named Ultrifo. Later, Irving Rips (at Younger Optics) developed the first ‘blended’ lens in 1955. However, the accepted view is that the first successful, widely available progressive was developed by Bernard Maitenaz, patented in 1953, introduced by the Société des Lunetiers (later to become Essilor) in 1959 and marketed as Varilux.1
This first-generation progressive was symmetrical in profile and, to create inset, each lens was rotated nasally by an equal amount. The design resulted in strong surface astigmatism in the periphery and temporal and nasal to the umbilical. The design was improved in 1972 when the Varilux 2 was launched. This had a full aspherical front surface, so reducing surface astigmatism as well as having basic built in inset.
In 1983, Zeiss introduced the Zeiss Gradal HS progressive, a game changer in progressive lens design benefiting from horizontal symmetry. As the eyes tracked across the lens from left to right, gaze areas of similar surface astigmatism were viewed through. The key benefit to the patient was that the swim sway effect experienced with earlier designs was reduced as the wearer now perceived objects bending in the same direction with each eye rather than opposite directions.2
By the late 1980s and early 1990s, manufacturers had started describing their lenses as ‘harder’ or ‘softer’ designs, this classification being related to iso-cylinder lines and mean power plots (contour plots) which were used as a method of describing and comparing optical performance of progressive lenses. Essentially, harder designs had a focus on distance and near vision and placed the surface astigmatism into the nasal and temporal areas below the far zone, this resulting in a relatively quick ramp up of surface aberrational astigmatism. In contrast, softer designs allowed some surface astigmatism to encroach into the far and near vision areas to preserve the intermediate vision. These designs were considered better all-round designs.
Back in my younger days as a DO, I would always give the fierier types and engineers harder design progressives as, at the collection, they invariably checked the performance of their glasses monocularly, placing one hand alternatively over each lens. Consequently, they experienced good distance and near vision and it was job done. For softer design progressives, I selected my patients carefully as I knew they would have to be motivated to get the very best from the lenses, and always explained that, as they adapted to the lenses, the reading and intermediate areas would open up. Of course, what I was really saying was they would get used to the soft surface astigmatism of the lens design. At the time, one of the key learnings was that, once someone had got used to one particular lens design, future switching to other design concepts would be a challenge. This said, nowadays it is far easier to switch patients between progressive lens designs than ever before, but an understanding of designs characteristics is still necessary to avoid patient dissatisfaction. Generally, switching patients between softer designs or to harder designs is less problematic than switching from harder to softer designs.
The next evolutionary step for progressives was the multi-design concept (figure 1), with ‘mono’ designs, as the add increased, the width of the intermediate and reading areas decreased, so by making the design harder with increasing add the reading area was maintained. At least, that was the multi-design promise. In reality, with increased reading addition, while making the design harder, the actual physical width of the area around the progressive umbilical and reading zone decreased. This showed how, as the add increases, the accurate placement of monocular centre distances becomes more important. 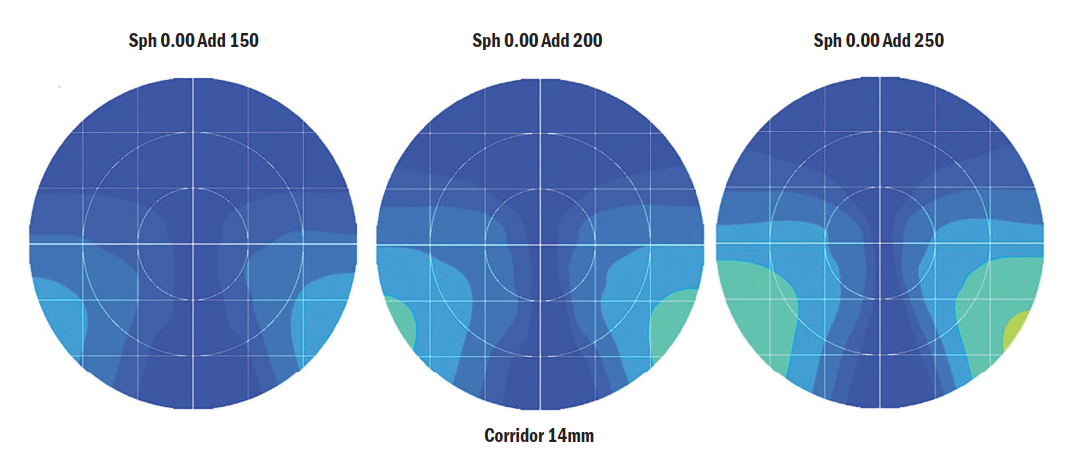 Figure 1: Multi-designs. As the add increased, the designs became harder
Figure 1: Multi-designs. As the add increased, the designs became harder
Around the same time as the introduction of multi-design lenses came the inset innovation. Older designs had one specific inset and slightly newer ones had two insets, one for plus prescriptions and another for minus. It may surprise some readers to know that, even now, some manufacturers have in their progressive lens portfolio simple designs based on the ‘two inset’ concept. With the multi-inset innovation, designers considered the distance Rx and add. We know that myopes with lower adds converge less than hypermetropes with high adds, so designs changed the inset related to this. Consequently, some designs at the time had over 100 insets resulting in enhanced binocular vision. This design feature, for sure, helped reduce some potential non-adaptation, but there was a problem. The insets are based on the average monocular centres of 32/32mm, so, for patients with larger, smaller or asymmetric monocular PDs, the designs will potentially not give the optimum comfort in vision one would expect.
By the late 1990s, fashion trends had changed with smaller frames becoming more and more popular, presenting a challenge for the eye care practitioner as progressives had minimum fitting heights of between 20 and 24mm. The first shorter corridor lens was the AO Compact, allowing a progressive to be fitted at a minimum height of 17mm. This was followed by the first true short corridor design, Hoya’s Summit CD, allowing heights as low as 14mm. The introduction of these short corridor designs created a new challenge for dispensing as, essentially, the designs were hard with higher levels of surface astigmatism which very quickly ramped up away from the umbilical, especially with higher additions. This is an effect predicted by the Minkwitz Theorem (figure 2).4 Interestingly, many practitioners found that patients tolerated these shorter corridors well as they had previously had to compromise their frame choice in order to accommodate the
fitting heights required by previous lens designs. So, psychologically, they were well motivated to persevere. Additionally, myopes generally prefer shorter corridor progressives as the base down prism experienced pulls the eyes upwards as they look down, resulting in uncomfortable vision with longer corridors during extended periods of downwards gaze. It also worth mentioning that, when a patient has been wearing a short corridor lens and been happy, it is not generally advisable to move them back to a longer corridor even if the new frame choice allows this. However, there is a caveat to this which will be discussed later in the article.
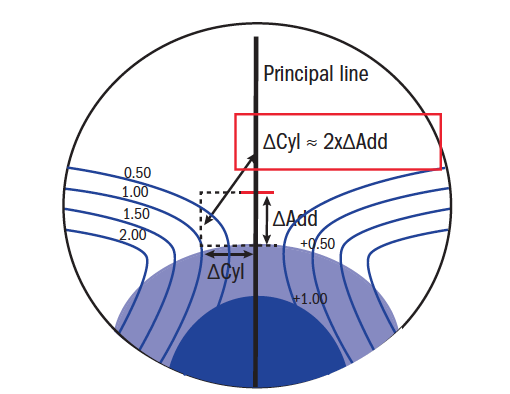
Figure 2: The Minkwitz Theorem which states that astigmatism perpendicular to the principal line changes twice as quickly at the rate of change of power along the line
The next major innovation in lens design came with the widespread, mainstream introduction of free form technology. This allowed the lens designers to control each single point on a lens surface and made it possible to create complex aspheric and atoric surfaces to help manage unwanted lens aberrations. With new, modern free form surfacing algorithms, very complex progressive lens designs can be produced that take into account binocular function in all directions of gaze, monocular centre distances, eye movements and how the prescription itself might impact on eye movement.
So, free form is a game changer. But, with such complex design innovations, why do we still get non-tolerance to progressives? The important thing to understand is that free form is actually just a surfacing technique and does not tell us how a lens will perform. For example, an unscrupulous supplier may take a single vision semi- finished lens and free form a progressive design from the distant past on the back surface to then market the lens as a free form progressive based on its manufacturing process. It is the technology in the design algorithm that makes the lens perform; a bad design is still a bad design.
Lens Matters
To avoid non-adaptation, we need always to consider the wants, needs, lifestyle and expectations of the patient, thus recommending a lens or lens type that meets these individual requirements.
First time wearers often need reassurance that presbyopia is part of the natural aging process. For some people, without such reassurance, they may feel their vision is deteriorating and the requirement to wear glasses for the first time may be traumatic. Given the boom in digital devices where fonts can be increased and print backlit, more patients are seeking their first spectacle solution with adds approaching +1.75DS or more. Indeed, in many cases, the ametropic presbyope may be better suited to occupational lenses than standard progressives so discussing different options is crucial.5
With existing wears, the current progressive solution gives the practitioner a vast amount of information which is often neglected or not recorded. The fit of the existing glasses, such as the pantoscopic tilt, frame face form angle and general frame positioning can all affect the patient’s adaptation to their new lenses. Indeed, if existing glasses are in poor adjustment, adjusting them to fit correctly can often aid the switch to the new glasses. Identifying the brand and lens design the patient is wearing, whether the design is front, back or double surfaced, can aid in the decision when switching to your preferred lens supplier. The author is aware that this is becoming harder with the abundance of manufacturer designs on the market including private and white label designs. However, using a spherometer can aid identification of lens structure and engravings which can be found in Ophthalmic Lens Availability by Phil Gilbert.
Other key information includes the progressive corridor length or minimum fitting height. To the most part, long corridor wearers will switch easily to short corridor designs, but the opposite can be more problematic. This said, if someone has a short corridor design in a frame which has an as-worn 8º to 10º pantoscopic tilt and the new frame has a very flat tilt, then in order to keep the near vision portion in a similar position a slightly longer corridor may be indicated.
It is equally important to check the fitting cross position of the previous design; are the lenses fitted slightly high or low? And was there a specific reason for this? Then there is the prism point; the point located directly between the engraved marking where prescribed prism and prism thinning must be checked. The latter should be equal in each lens. According to BS EN ISO 21987 2017 Ophthalmic Optics Mounted Spectacle Lenses, for a prescription of +/-5.00DS, the tolerance is 0.50Δ vertically. This suggests that there may be patients wearing progressive lenses that have this error and have got used to the error over time. Checking the spectacles at the prism point, and making the prescribing optometrist aware of any potential vertical prism, is well worth the short time it takes. Indeed, many optometrists are apprehensive about prescribing prism, but past professional experience suggests that prescribed horizontal and vertical prism is commonly missed in assessing the previously worn spectacles.
Historically, prism thinning (figure 3) was used to ensure an even distribution of lens thickness at the top and bottom of a positive spectacle lens. However, some manufacturers have elected to use two thirds of the add power in base down prism dioptres, regardless of the overall lens power. This has the desirable effect of shifting the object position upwards, but the negative effect of increasing the lens thickness in the lower part of the lens, particularly with shorter corridor designs. Other manufacturers have elected to use intelligent prism thinning. This takes into account the power distribution of the lens and, consequently, generates designs that may have equal amounts of base down, zero or base up prism. 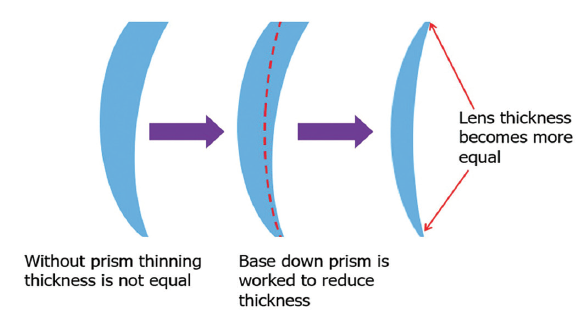 Figure 3: Prism thinning in a positive lens
Figure 3: Prism thinning in a positive lens
Most patients will appreciate the cosmesis of this thickness optimisation. However, a handful may not tolerate the apparent change in object position, resulting in them having to raise their head higher in search of clear vision. Another thing that should be borne in mind is that any prism, including prism thinning, has the adverse effect of distorting an image. For base down prism, when reading, print may seem to narrow towards the bottom of a page and indeed bend when looking from left to right.6 Prism of any type in a lens will also create dispersion, increased with higher index lens materials, and occasionally reported as a blue tinge when looking down and a yellow shift when looking up.
When dispensing any progressive lenses without the option to personalise to frame fit, it is important to understand that the lenses will have been designed to ‘default parameters’. Older progressive designs consider pantoscopic tilt of around 10º to 12º. However, more modern designs generally consider average pantoscopic angle to be around 8º. Flatter or more inclined angles can adversely affect the performance of these lenses resulting in the narrowing of the distance , intermediate and reading areas of the lens (figure 4).
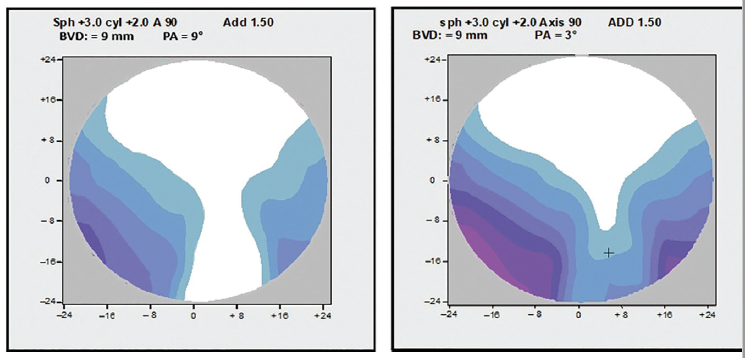 Figure 4: Reducing the pantoscopic tilt (PA) from 9° (left) to 3° (right) affects the power profile of the lens (image courtesy of Zeiss)
Figure 4: Reducing the pantoscopic tilt (PA) from 9° (left) to 3° (right) affects the power profile of the lens (image courtesy of Zeiss)
Many modern progressive designs also incorporate power compensation based on the assumed fitting position of the lenses, but again if the lenses are fitted outside what is considered the norm, the power compensation can contribute to poor tolerance of the lenses. So, whenever fitting progressives in flatter or more wrapped frames, lenses which can be optimised to those conditions are advisable. This said, longer vertex distances are never recommended for progressive designs. Even if the vertex can be built in to the power compensation, the surface astigmatism of the lens will feel to the wearer a bit like looking through a key hole; as the lens gets further away, the stable clear field will reduce.
Of course, for any spectacles to perform well, the prescription must be accurate and suitable for the patient’s needs. However, we must consider the possibility that the test room itself is flawed in that, in most circumstances, the examination is carried out at six metres which inherently produces a negative vergence of -0.16DS. Optometrists are routinely taught to ‘push the plus’ for distance and be careful of overminusing. This error, therefore, can enhance overplussing and underminusing and can compound vertex distance changes if not considered. While in practice, I would often query prescriptions that had any reduction in minus power, knowing that myopes in particular hated this. So often, the optometrist would take the patient to the practice door and check the prescription in true, everyday circumstances and not the sterility of the testing room before confirming the usefulness of such a change.
Something that also might seem obvious is the need to check whether the prescription history matches with the dispensing history. Occasionally, ‘small changes’ are reported in Rx which are actually significant as the patient may actually be wearing spectacles from two or three refractions ago, and a big change at one hit may prove problematic.
Dispensing Matters
As previously alluded to, the frame must be fully fitted before measurements can be taken, always ensuring that the patient is in their natural posture when undertaking this. Monocular centre distances will vary slightly from frame to frame, due to bridge variations and asymmetric noses, but will always equal the overall pupil distance.
When measuring, we should be directly in front of the patient. Being just 2cm offset will produce an error of 1.5mm per eye at 40cm, while being directly in front of the patient and having a PD 10mm larger will induce a 1mm total error.7 If a patient has a natural head tilt or turn, ensure this is considered if it is not intended to be resolved while wearing the new prescription.
It is a good idea to take measurements three times particularly where heights are concerned. Previous multifocal wearers, for example, may tend to lift their heads as you try to measure the heights. For taller and shorter patients, evaluate the fitting cross position carefully. Measuring heights and distance OCs through existing spectacle lenses, usually done if the same frame is to be utilised, is not ideal as the pupil position will be altered by the prescription. While many of us are experts with the ruler, a recent CET workshop with over 100 practitioners highlighted that over 50% could not accurately measure a PD, with a variance of 11mm.8
Digital measuring devices (figure 5) can, of course, aid in the dispense and have been shown to be accurate when used correctly.9 It must, however, be borne in mind that this is a ‘snapshot’ of one moment in time and the practitioner should use their professional judgment when interpreting these results.
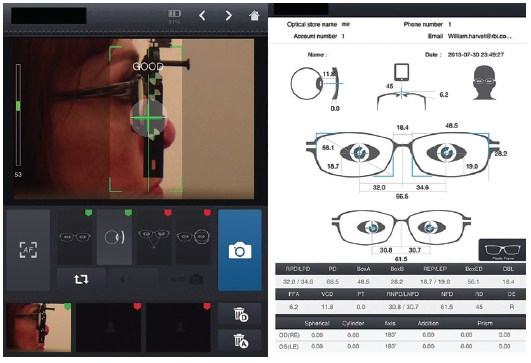 Figure 5: An example of a digital dispensing system
Figure 5: An example of a digital dispensing system
Incorrect monocular OCs can have a huge impact on the performance of any lens, but this is particularly so with progressives, affecting the binocular field of view dramatically with higher additions. Figure 6 gives an indication of the loss in binocular field related to centration error. Often, in the author’s experience, monocular OCs are simply copied across from the previous dispenses or are, in most cases of non-adaptation, exactly even.
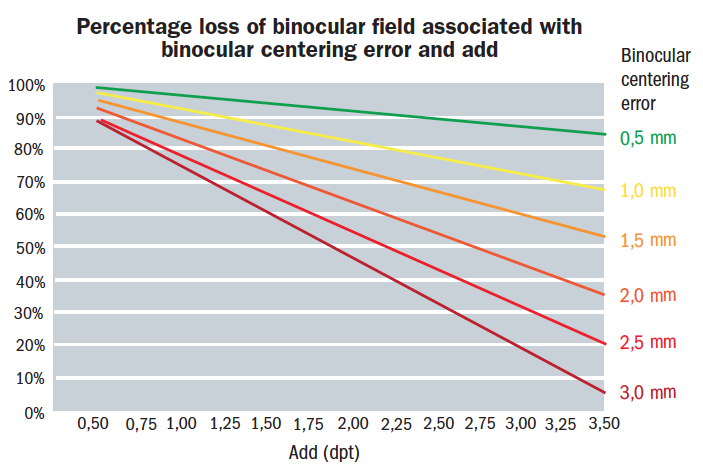 Figure 6: Percentage loss of binocular field associated with binocular centring error and addition
Figure 6: Percentage loss of binocular field associated with binocular centring error and addition
It might sound obvious, but when vertical heights are being measured and ordered, ensure that everyone in the practice is utilising the same method and that the lab knows the method being used. While there is good consistency when specifying heights above horizontal centre line, in the author’s experience there is some variation in measurements taken from the ‘lower rim’. Some practitioners use the lowest tangent, others use the lowest part of the inner rim without consideration of the bevel depth, and some measure to a point directly beneath the pupil. These errors within practice have been highlighted many times as causes of non-tolerance.
We also need to bear in mind the minimum vertical height requirement of a progressive lens design. This is usually specified to the middle of the near vision area, which is the minimum vertical height recommended and, in most cases, cuts the available reading area in half. Consequently, while fitting progressives at the minimum height allows a wider frame choice, patients with additions over around +1.75DS and who have lost a good deal of their accommodation, may struggle as they become more dependent on the add.
Additionally, it may well be the case that the required minimum at the lowest tangent is met. But, due to the upsweep of the frame rim directly beneath the pupil and inwards slightly where the reading area is placed, this is cut off. Likewise, if the frame has a deep bevel, again we lose some of the reading area.
The optimum fitting height for a progressive design is generally 4 to 5mm higher than the minimum, allowing the full reading zone to be placed within the frame. But we must not forget that equally important is the height above the fitting cross. This is fundamental in progressive lens adaptation. Most manufacturers suggest a minimum of 8mm above the fitting cross but recommend 10 to 12mm. Given that progressives are worn as general-purpose lenses, it stands to reason that the distance portion should be given reasonable bias.
From time to time, we see monocular patients who have never learned convergence and consequently look straight down to read. The basic test is to see how these patients hold and position their reading print. In the past, to satisfy these patients, a progressive lens may have to have been ordered off-axis and twisted temporally to line up the progressive intermediate umbilical and reading area, thus also correcting the cylinder orientation. Thankfully, there are now higher tier progressive designs that allow the practitioner to have full control over the reading inset. So, if required, a zero inset can be specified, or indeed a reduced inset. These designs offer, as an alternative, the ability to specify working distance. However, this is often incorrectly specified, such as where the patient has an indicated add of +3.00DS and a working distance of 45cm, which is clearly incorrect. Given that these premium designs have high grade technologies associated with them, arbitrarily playing with the insets and working distance associated with the designs is strongly discouraged as it often leads to intolerance and unhappy patients.
Anisometropia
Anisometropia presents its own unique challenges when considering dispensing progressive lenses, both due to prismatic effects and differential magnification. Some, more sensitive, patients find issues with even a modest 1.00DS difference. This said, many more patients cope well, even with prescription differences in excess of 3.00DS. But there are some caveats, such as if the anisometropia is recently acquired (possible due to cataract surgery). Do they have good binocular vision? Do they suppress one eye at near? The list goes on.10
Without resulting to slab-off or specialised progressive designs such as the Shaw Lens, a simple solution is to use the shortest possible corridor, thus reducing the prismatic difference at near. Indeed, some premium progressives consider the line of sight in the design calculation. This can also slightly reduce the prismatic difference at near. Also, historically, some practitioners have used two different progressive corridor lengths.
Disease
Pathology contributes to non-adaptation in approximately 9% of cases.11 Conditions such as AMD and cataract need careful explanation, as often the patients feel the new glasses should give a marked improvement over their existing pair. Nuclear cataracts often cause a myopic shift, resulting in reduced spectacle magnification at near and rejection from patients, while cortical cataracts induce cylinder swings which may not be well tolerated by the patient.12 Patients with superior oblique muscle palsy or paresis are not indicated for progressive lens wear due to restricted vertical movement on convergence, but there are always exceptions as optics is full of grey areas.
Conclusion
Of course, there are other multiple reasons for patient non-tolerance some psychological, some related to frame choice, expectations, general experience within the practice and price. What is key is good communication and discussion throughout the patient journey along with dispensing the most appropriate optical solutions be it progressive, occupational, single vision or multiple pairs plus accurate measuring and verification.
Andy Sanders is a dispensing optician, Hoya Professional Services Director UK and Ireland, Chair of the FMO lens Focus Group and standards Panel.
Further reading
- Schwendeman, F, Ogden, B, Horner, D, & Thibos, L. ‘Effect of Sphero-Cylinder Blur on Visual Acuity.’ Optometry and Vision Science, 1997; Vol. 74, No. 12; pp 180-181
- Jalie M. Ophthalmic Lenses and Dispensing.
- 2nd Ed. Butterworth- Heinemann, Edinburgh 2003.
- Harris WF. Sequential tilt and tilted power of thin lenses. Optom Vis Sci 2006 83 249-254
- Harris WF. Tilted power of thin lenses. Optom Vis Sci 2002 79 512-515
- Meister D. Free-form optical optimization. Zeiss, Technical Communication, 2006.
References
- The Cyril Kett Optometry Museum and Archive- museum.aco.org.au
- How a patent (EP0039497) filed by Zeiss set a new standard for progressive lenses 30 years ago Zeiss.co.uk
- Essential course in dispensing – part 9, Optician, March 2014, A Keirl
- Progressive Powered Lenses: the Minkwitz Theorem -James E Sheedy Optometry and Vision Science Vol 82 No. 10, October 2005
- Low Add Boost Occupational and Degressives: What are they all about? A Sanders Dispensing Optics April 2017
- Understanding Prism in Lenses- D Meister Feb 2014
- Walsh G, Pearce E. The difference between belief and reality for Viktorin’s method of inter- pupillary distance measurement. Ophthalmic Physiol.2009 Mar; 29(2):150-4
- Fundamentals of ophthalmic dispensing – part 1 – interpupillary distance, Peter Black, Optician, May 2019
- Comparison of PD measuring devices Part 1 Dr Wolfgang Wesemann, Optician, 12.3.2010
- ‘Anisometropia: does this mean we have to dispense single vision lenses?.’ The Free Library. 2019 Ten Alps Publishing 06 Nov. 2020
- Investigation of the causes of non-adaptation to optometric prescriptions for spectacles, Catharine E Freeman, Bruce JW Evans, Dec 2009
- Pesudovs K, Elliott DB Refractive error changes in cortical, nuclear, and posterior subcapsular cataracts British Journal of Ophthalmology 2003;87:964-967
