Presbyopia is a global problem affecting over 1.8 billion people worldwide1 and in the UK, around 42% of the population is presbyopic (>45 years of age).2 Traditionally perceived as challenging, contact lens fitting of presbyopic patients has steadily risen over the past 15 years from 20% to 35% of all fits, with multifocal contact lenses prescribed around 40% of the time.3 This may be due, in part, to the visual demands of emerging presbyopes including increasingly active lifestyles, desire for continuation of successful contact lens wear, or cosmesis.4 Advances in optical designs, daily disposability and enhanced materials has improved the visual and physiological outcomes making contact lenses an integral choice of vision correction for these patients.
Currently, there are three general approaches for correcting the presbyopic patient with contact lenses; single-vision with over-spectacles, monovision, and multifocals (figure 1). Each option has advantages and disadvantages with the success dependent upon the lens type and design, the fitting approach used and the amount of presbyopia present. While all options will be presented here, this article will focus on the most common correction options used; monovision and simultaneous vision.
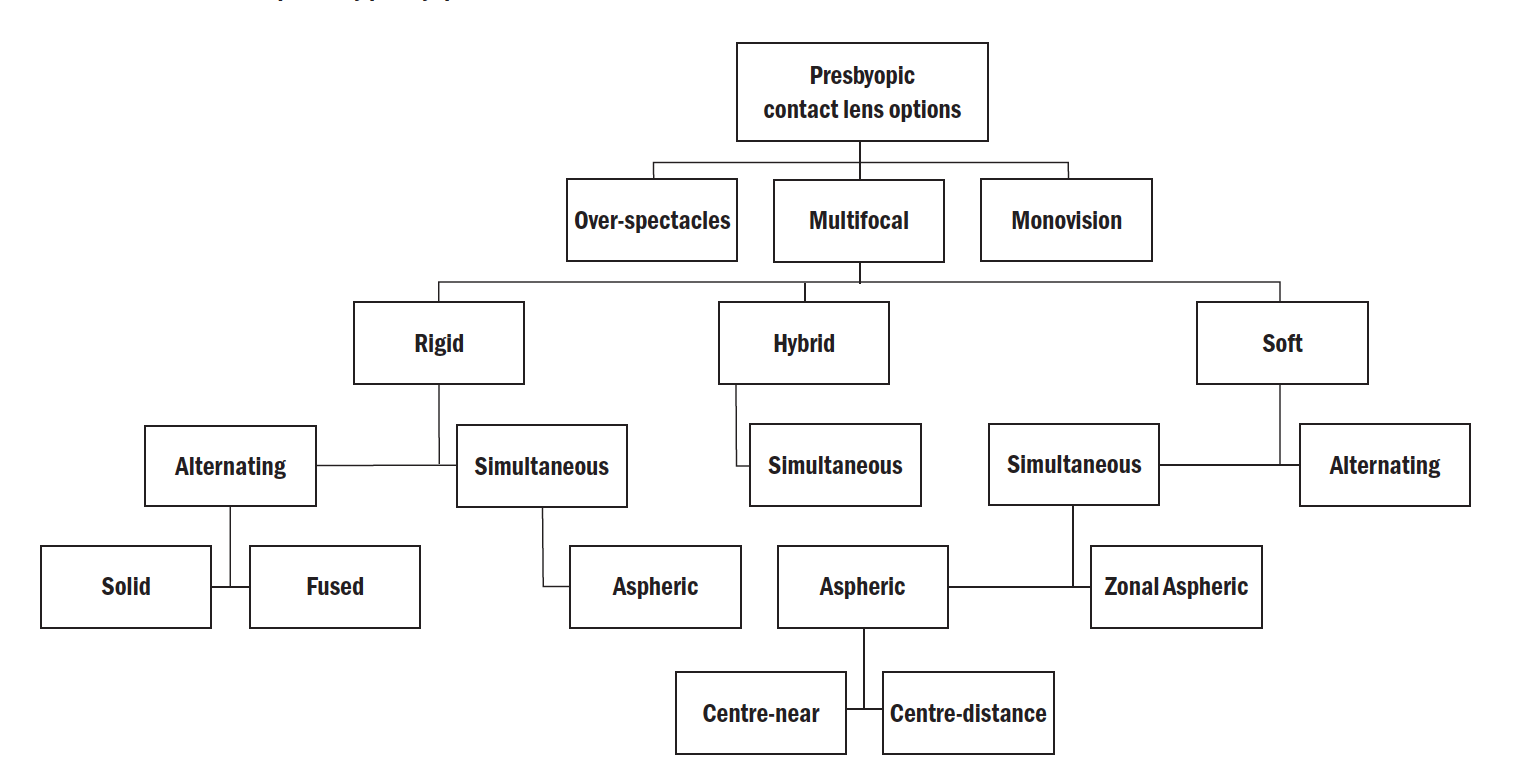 Figure 1: Contact lens options by presbyopia correction
Figure 1: Contact lens options by presbyopia correction
Patient Selection and Expectations
Consideration should be given to patient selection prior to fitting with contact lenses for presbyopia (table 1). Motivation plays a major factor in contact lens fitting and the practitioner should ensure their patient is aware of the advantages and disadvantages of all options prior to fitting. Expectations should be set using positive language, reinforcing the benefits of contact lens correction, ie spectacle free vision, vision in all directions of gaze, no peripheral distortion, while acknowledging the limitations compared to spectacle correction. Thought should also be given to the binocular status of the patient, as compromised binocular vision will impact outcome. High and low contrast VA charts (figure 2) give more information about acuity, and the difference in low-contrast acuity between spectacles and contact lenses gives some indication of possible success. As well as the VA charts, the practitioner should have access to other near tasks, such as mobile phone, laptop etc, to mimic ‘real-life’. It is generally accepted that patients’ expectations should be realistically managed during visual assessment, in our experience the aim is to meet around 80% of a patient’s visual needs.
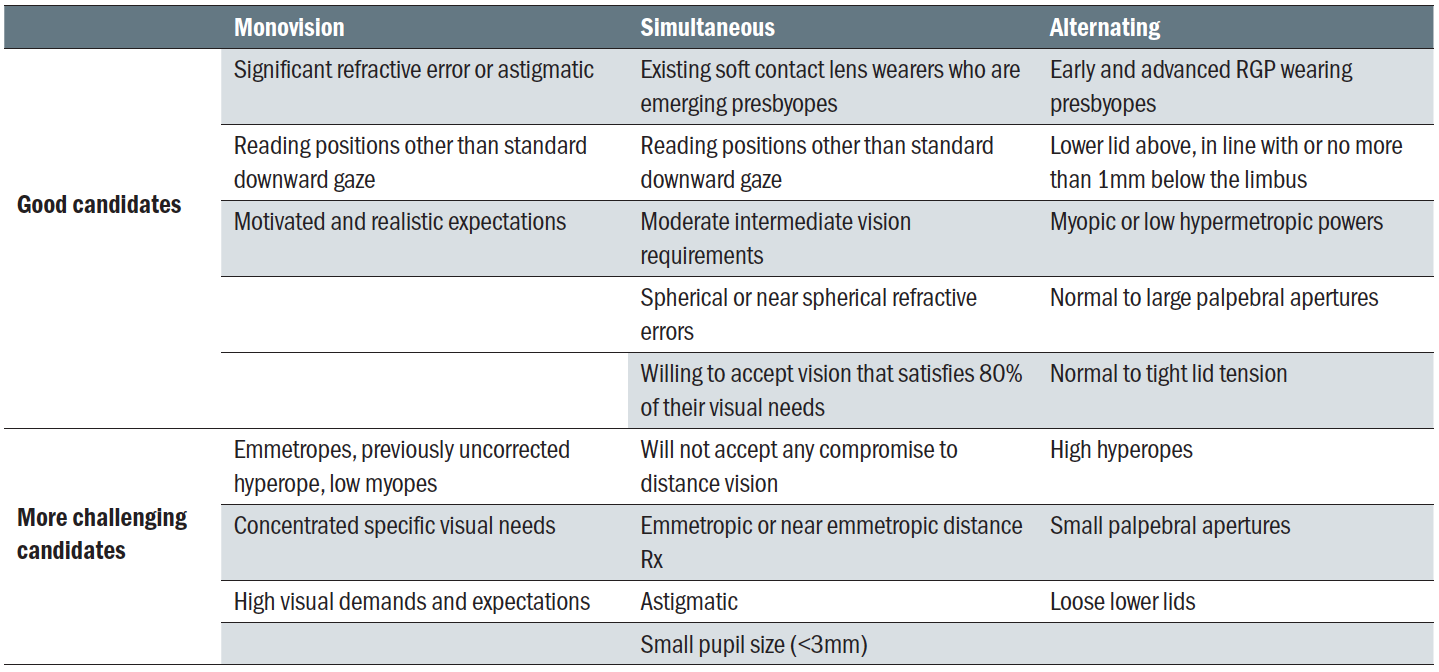 Table 1: Patient selection for presbyopic contact lens correction. (Modified from Bennet 2018)4
Table 1: Patient selection for presbyopic contact lens correction. (Modified from Bennet 2018)4
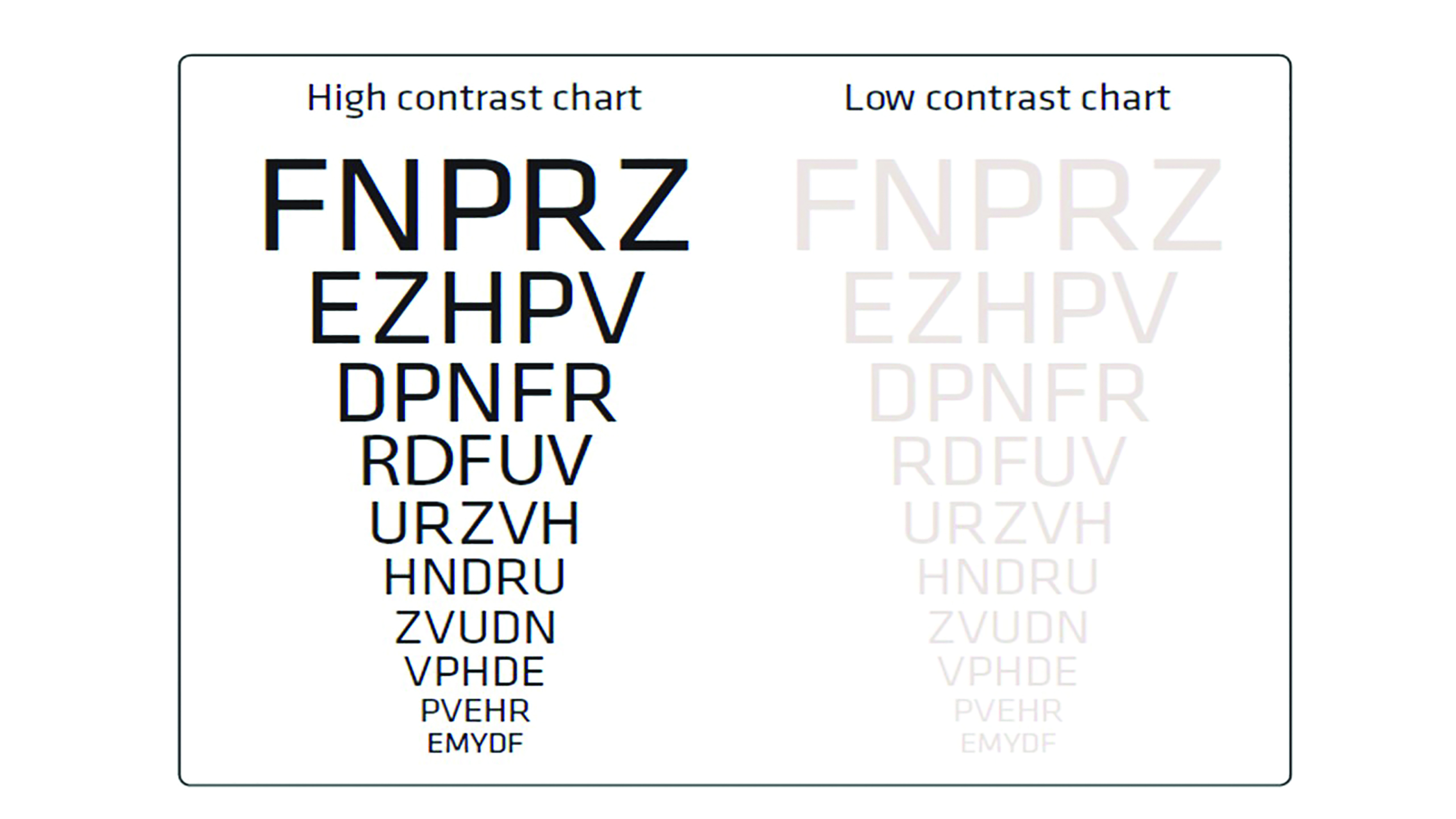 Figure 2: High and low contrast visual acuity chart
Figure 2: High and low contrast visual acuity chart
Initial measurements
Ocular dominance
It is important to establish ocular dominance in order to determine which eye to correct for distance vision when fitting monovision and for adjustments when fitting a simultaneous lens design. Dominance can be assessed using either sensory or sighting (motor) dominance, with the former being the recommended method by most manufacturers. Sensory dominance is assessed by placing the best binocular distance refraction in the trial frame and, while the patient observes the lowest line they can read on a distance chart, a +1.00DS is placed alternatively in front of each eye, with the patient indicating when the vision is clearest. If the +1.00DS lens is in front of the left eye when the image is reported as clearest then the right eye is considered as distance dominant and vice versa. Should a patient be unable to spot a difference between the two, the test should be repeated using a +0.75DS lens.
Lighting
Lighting plays an important role in assessing vision for the presbyope. Ideally, the consulting room should have a wide range of lighting possibilities. These should range from bright, direct illumination on targets to maximise the chances of a patient first seeing the in-focus image, through to the ability to decrease the level of illumination so visual performance at, or near, darkness can be assessed.
Ocular health
As with any contact lens fitting, careful examination of the anterior eye should be conducted prior to fitting. The prevalence of clinically diagnosed dry eye and meibomian gland dysfunction increases with age.5 This should be noted and taken into account when deciding on the most appropriate lens material for each patient in order to maximise comfort. (For further information on soft contact lens material properties see Optician 06.03.2020).
Pupil size
Thought should also be given to factors that affect pupil size, due to the impact pupil size could have, particularly when fitting some multifocal lens designs. While it is well acknowledged that pupil size decreases with age, reduced working distance and increased light intensity, it is perhaps less well acknowledged that pupil size also varies with refractive error. Research shows that myopes tend to have larger pupils than hypermetropes, particularly in mesopic conditions.6,7 Though most multifocal contact lens designs account for the change in pupil size with age by varying the optical design with increasing add, to date only one also takes into account pupil changes with refractive error, optimising optics across 183 different designs (figure 3). 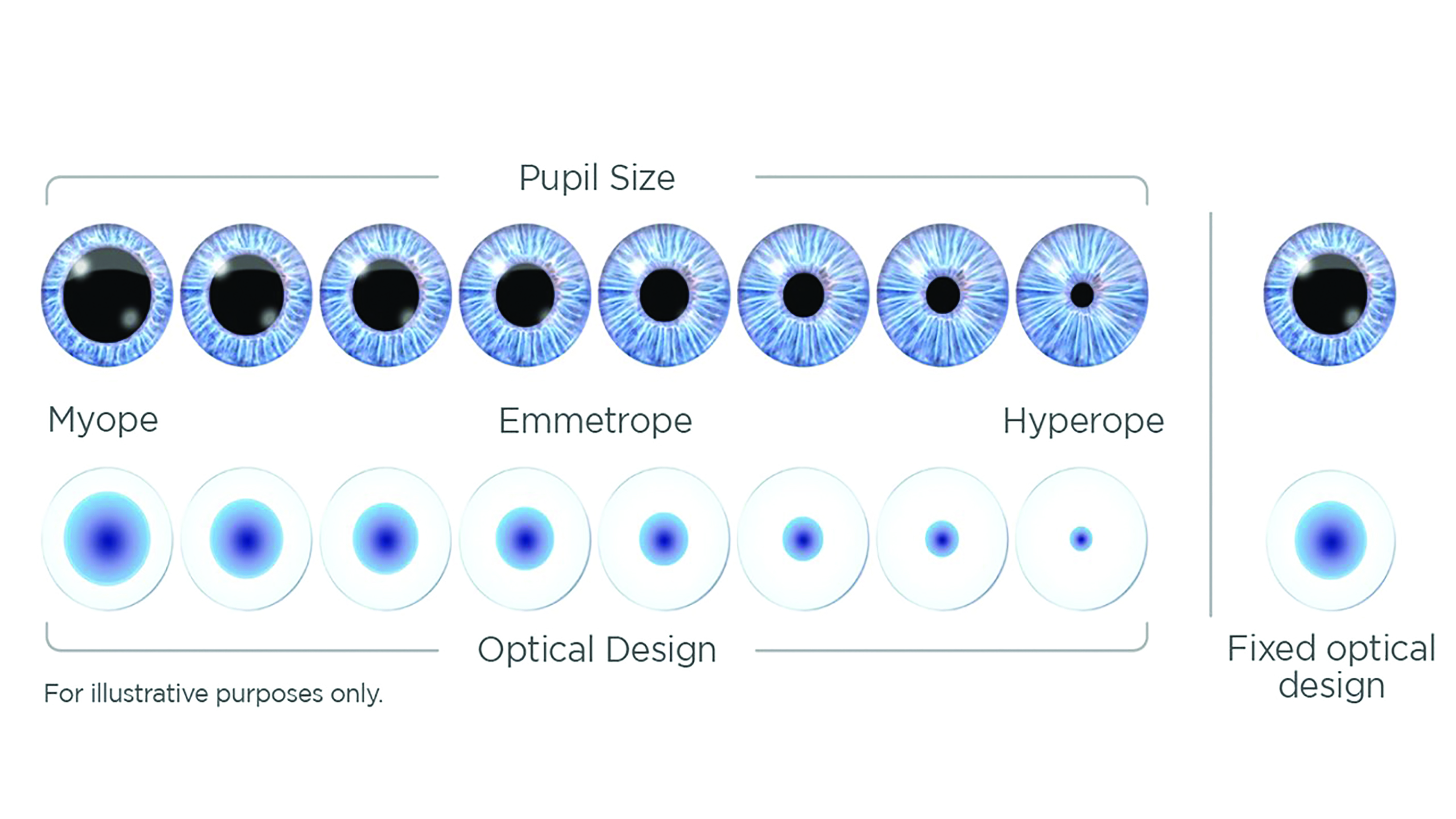 Figure 3: Illustration showing how pupil size varies with refractive error and how the optical design of one simultaneous vision multifocal has been optimised to take this variation into account
Figure 3: Illustration showing how pupil size varies with refractive error and how the optical design of one simultaneous vision multifocal has been optimised to take this variation into account
Overview of correction options
Over-spectacles
One of the most common methods of correcting the contact lens-wearing presbyope is with a pair of reading spectacles worn over the distance contact lens correction. These may either be single vision, bi/trifocal, or progressive lenses depending on the needs of the individual.8
There are obvious advantages to this method in that the contact lens correction requires no modifications and improvements in progressive lens technologies make this option more visually acceptable for patients.9 However, there are still fundamental limitations, such as inadequate intermediate vision correction, appearance and general inconvenience. For a longstanding contact lens wearer, or a previous emmetrope, this option is likely to be poorly accepted due to the inconvenience of glasses wear.
Despite these disadvantages, the use of over-spectacles is still one of the most popular methods of presbyopic correction with research reporting approximately 50% of all presbyopes fitted with soft contact lenses receive a distance-only correction.3
Monovision
Another common method of correcting the contact lens-wearing presbyope is monovision, which accounts for 10 to 15% of the total lenses prescribed for presbyopia.3 Here, an unbalanced correction between the two eyes is utilised, with one eye corrected for ‘distance’ (usually the dominant eye) and one for ‘near’.10 This approach works on the principle that the visual system can alternate central suppression between the two eyes, thus enabling the object of interest to be seen clearly.
Monovision tends to work more successfully in younger presbyopes with residual accommodation and where a lower add value is used.9 The optimum near addition for monovision has been reported to be around +1.50DS, with lower or higher levels having a negative impact on vision.11 The main benefits of monovision include ease of fitting, relative low cost and flexibility, allowing the practitioner to choose the most suitable lens material and design for the patient.
One of the main disadvantages of monovision is the disturbance to stereopsis. For patients who have either little tolerance for visual disruption or who are engaged in detailed visual tasks, this may prove too great. A recent study published by Fernandes et al12 reviewed the objective and subjective results for vision corrected by both multifocals and monovision and concluded that stereoacuity was significantly better in multifocal contact lens patients compared to those wearing monovision. Reduction in contrast sensitivity13 and glare when driving at night14 are also noted disadvantages of monovision.
For patients with high near vision demands across all illuminations, monovision may be a good option. Whereas when critical or sustained tasks requiring good binocularity predominate, it is advisable to avoid monovision or to consider supplementary correction.
Principles of Monovision fitting
Physical fit
This should be the same as the fit required for any other spherical or toric soft or RGP contact lens fit, as described in previous chapters in this series.
Trial lens power selection
For most patients, a good starting point in selecting appropriate lens power is to fit the dominant eye with the distance correction and the non-dominant eye with the near correction. It is important to correct any astigmatism equal to or greater than 0.75DS in either or both eyes which, if left uncorrected, can result in reduced visual performance, asthenopia and poor tolerance.
Visual assessment
The first task for the practitioner is to encourage the patient to suppress each eye to see clearly.
Under binocular viewing, looking at a high-contrast, well-illuminated distance chart, the patient should be asked to read as far down the chart as possible without comment on visual quality. This should then be repeated for near type. If the patient is unable to read the distance or near type, the practitioner should not occlude either eye. Instead, the ‘non-viewing eye’ should be progressively blurred with spherical lenses until the image comes into view. When the distance or near type is seen clearly, the amount of blur should be progressively reduced while asking the patient to continue to read. Once the full extent of the blur has been removed, the patient should be asked to view a distant object (if it was the near test that was causing problems before) and then return to reading. This technique will demonstrate the ability of the patient to suppress the ‘non-viewing’ eye. Once the ability to suppress has been demonstrated, the practitioner should optimise the refraction, again binocularly, to check that the optimum correction for distance and near has been achieved.
After static visual acuity has been assessed, the patient should be encouraged to walk around the practice wearing the full monovision correction and dynamic vision assessed. Dynamic visual assessment should start with an appreciation of the effect of suppression on peripheral acuity before allowing the patient to carry out other tasks, such as judging distance. These assessments are important, both clinically and ethically, in showing the patient the advantages and limitations of the correction. Ideally, an extended trial period is preferred in monovision correction so that the patient can fully assess the benefits of the correction. Before this occurs, the onus is on the practitioner to explain fully the type of correction fitted and to make sure the patient understands that the adaptation period may involve problems in close work and a ‘learning curve’ in driving, especially at night.
When fitting monovision, and indeed all presbyopic contact lens corrections, the practitioner has an obligation to inform patients of the adaptation that may be required. If a patient is unable to adapt to any visual disturbance caused by monovision in specific situations, a practitioner may consider prescribing a spectacle over-refraction.
Partial monovision
The acceptance and therefore the success of monovision reduces as the reading add increases.15,16 As the spectacle add exceeds +2.00DS, tolerance can often be improved if a reduced reading addition is given in the contact lens prescription. This method is called partial monovision. This is advantageous for social users whose near vision demands will be lower than full-time wearers and for those with greater intermediate vision needs. However, patients may need supplementary glasses for certain near tasks or indeed additional glasses for driving.
Enhanced monovision
Enhanced monovision involves fitting one eye with a multifocal lens and the other with a single-vision lens. Most commonly, the dominant eye is fitted with a single-vision distance lens and the non-dominant eye with a multifocal lens, though other options are available. This improves binocular summation and offers some level of stereo-acuity to the wearer that is experiencing increasing blur with a higher reading add. Alternatively, the same approach can be used when fitting patients that require sharper distance vision than bilateral simultaneous vision multifocals can offer. In this scenario, the multifocal lens in the non-dominant eye may require more bias for near vision. This modification can be achieved by increasing the distance power of the multifocal lens by +0.50DS to +0.75DS.
Modified monovision
One way to alleviate visual problems associated with monovision is to employ a modified approach. This involves adjusting the lens power or utilising different lens designs in each eye to improve the distance vision in one eye at the expense of the near vision and vice versa. This can be done in several ways such as minimising plus on the dominant eye to enhance distance vision, while ‘pushing’ plus in the non-dominant eye, or to utilise different add powers in each eye with the lower add power being fitted to the dominant eye to maximise distance vision. Another option would be to fit a centre-distance simultaneous design lens in one eye and a centre-near design in the other. Some recent lens designs use this modified monovision approach automatically when fitting presbyopic patients. The advantage of this method is that binocular summation will still occur, providing acceptable vision at all distances under binocular conditions. Despite being utilised clinically, little evidence exists as to the success of modified monovision, although in 2016, Sivardeen et al17 reported a centre-distance, centre-near model outperformed a model using the same design in both eyes.
Multifocal
Multifocal contact lenses are another presbyopic vision correction option and they are growing in popularity due to advancements in materials and lens design. In their most recent international survey, Morgan et al3 reported the continued increase in multifocal prescribing from approximately 25% of lenses fitted to presbyopes in 2005 to around 40% in 2019, indicating a preference for multifocal lenses over monovision which are fitted only 10 to 15% of the time.
There are a vast array of multifocal lens designs available in both rigid and soft materials, offering spherical and toric optics with designs typically using either the simultaneous vision- or alternating-image principle. In contact lenses which utilise the simultaneous-image principle, distance and near images are simultaneously presented to the retina through a stable lens, with the visual system ‘selecting’ the clearer image. Conversely, alternating-image lenses rely upon lens displacement on the eye to correctly position the appropriation portion of the lens over the pupil.
Simultaneous vision designs
In simultaneous vision contact lens systems, the basic principle of the system remains the same irrespective of whether the power varies in a discrete or progressive manner across the surface. A wide variety of simultaneous lens designs are now available, with the introduction of daily disposable aspheric soft contact lenses resulting in increased prescribing of this form of lens correction in recent years.18
Bi-concentric
Early simultaneous vision designs had discrete zones of distance and near power (figure 4). A centre-distance design has a central portion for distance vision surrounded by a near vision periphery. Conversely, a centre-near design has a central portion for near surrounded by a distance vision periphery. The main disadvantage of these lenses is their dependency on pupil size. These bi-concentric designs are still available from some RGP manufacturers, although are rarely used due to the availability of more advanced, easier to fit designs and single use disposable lenses.
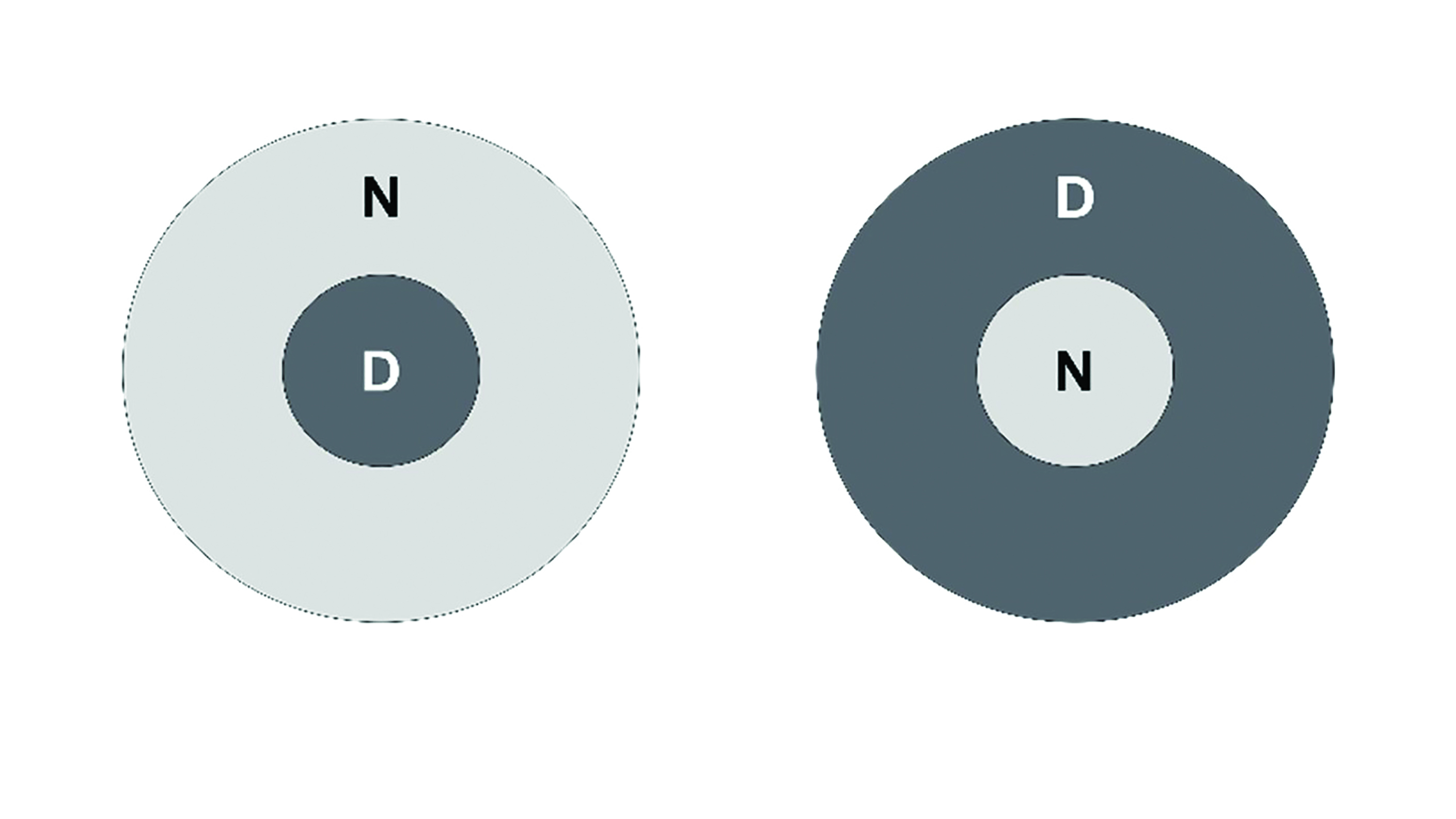 Figure 4: Bi-concentric simultaneous vision contact lenses. Centre-distance, left; centre-near, right.
Figure 4: Bi-concentric simultaneous vision contact lenses. Centre-distance, left; centre-near, right.
Diffractive bifocals
Diffractive bifocal lenses utilised refraction and diffraction and worked on the principle of placing a ‘phase plate’ on the rear surface of the lens, which split the light passing through into two discrete focal points, one for distance and the other for near vision (figure 5). Unlike bi-concentric designs, diffractive bifocal lenses were largely independent of pupil size, although were sensitive to lens centration. The main limitation with diffractive bifocals is the loss of around 20% of incident light to higher orders of diffraction,19 resulting in a reduction in low contrast visual acuity.20 This design was available in both soft and rigid materials but neither products are currently available.
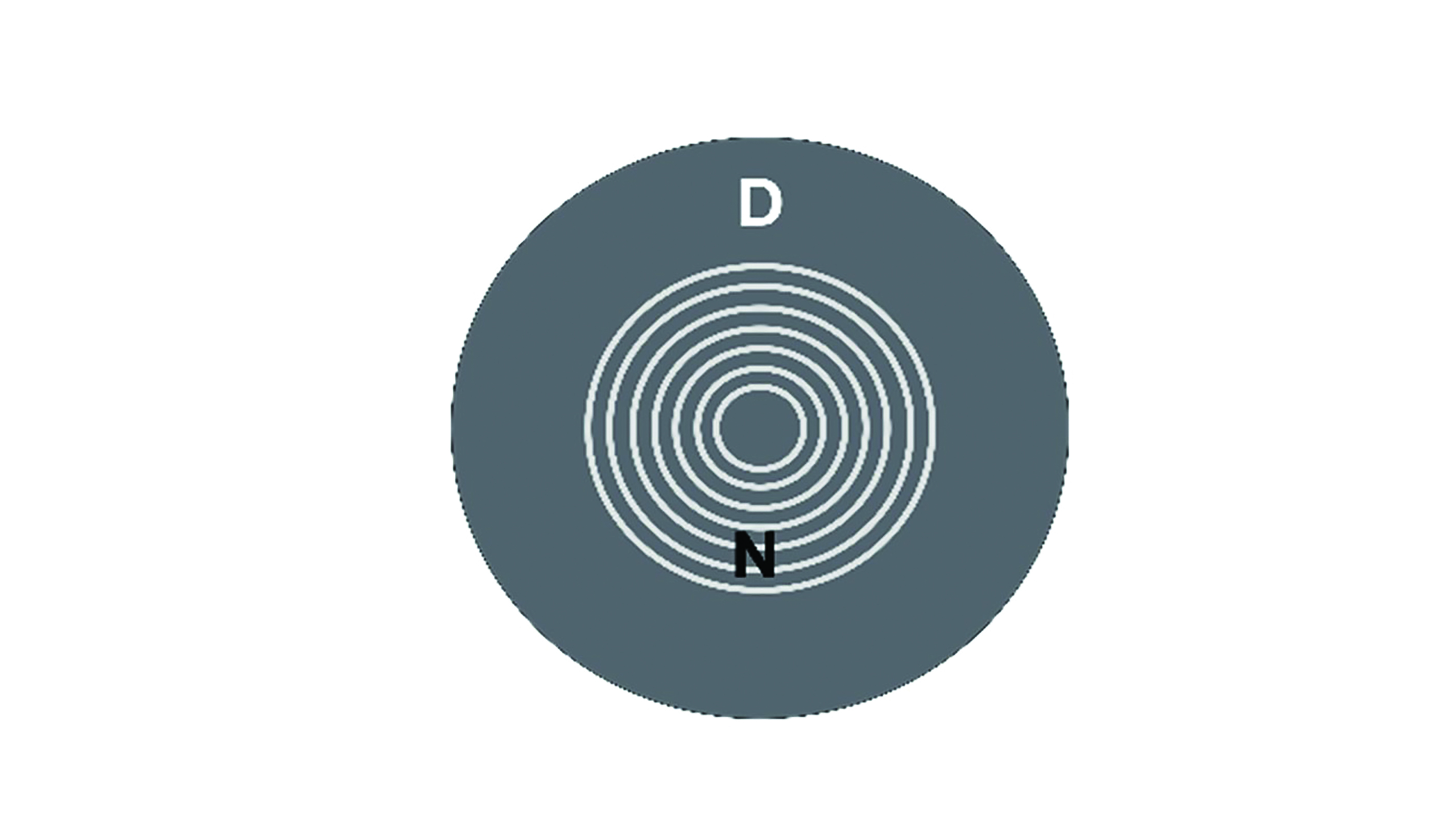
Figure 5: Diffractive bifocal lens design
Multi-zone
An approach to minimise the impact of pupil size on vision, especially in relation to different lighting conditions, was to increase the number of concentric zones alternatively powered for distance and near vision. This concept resulted in a centre-distance multi-zone design consisting of five alternating distance and near powered zones (figure 6).21 The width and spacing of the zones are based on the variation of pupil size in different illuminations within the presbyopic population. Theoretically, the lens design favours distance vision in extreme high and low lighting conditions and provides a more equal ratio of light division in ambient illumination conditions.8
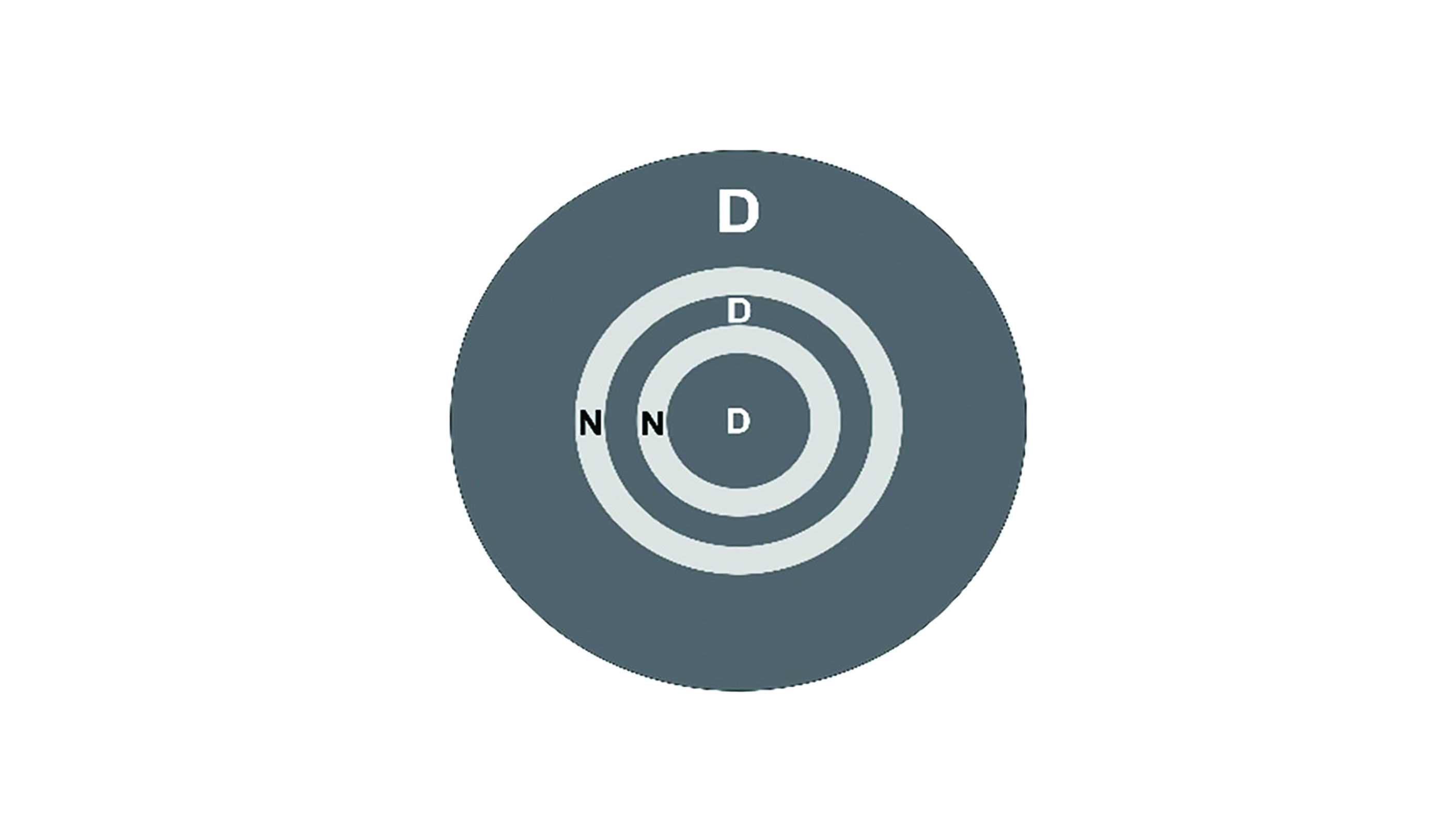
Figure 6: Multi-zone concentric centre-distance design
Aspheric
More modern simultaneous vision designs utilise aspheric optics to achieve a gradual change in the power distribution across the lens and have hence been described as multifocal or progressive lenses. Aspheric lenses can be subdivided according to whether the power changes from distance to near (most minus, least plus centrally) resulting in a centre-distance design or from near to distance (most plus, least minus centrally) resulting in a centre-near design (figure 7). Both options are available in a range of materials, although the most prevalent design in current soft multifocal contact lenses is centre-near front surface aspheric.
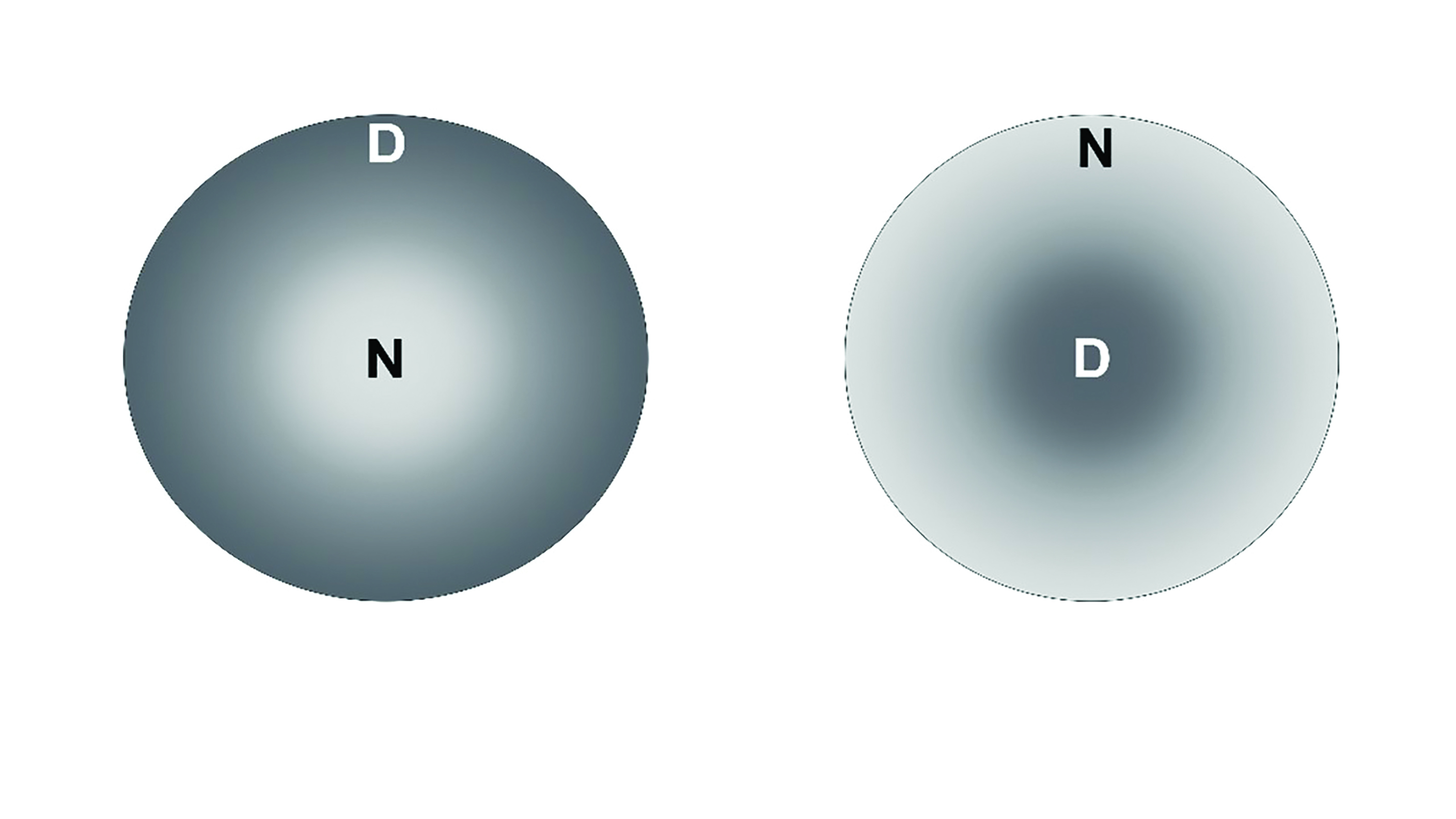 Figure 7 Left: Front surface centre-near design. Right: back surface centre-distance design
Figure 7 Left: Front surface centre-near design. Right: back surface centre-distance design
Centre-distance
A centre-distance lens usually has a back surface aspheric curve resulting in the central portion of its optical zone correcting distance vision, surrounded by an area containing the power of the lens required for near work. This is achieved by the aspheric curve inducing positive spherical aberration. Rays of light from a distant object are focused by the central zone on the retina and compete with the out-of-focus rays being formed by the surround (figure 8). When viewing a near object, the reverse occurs, where the light rays from the peripheral zone come into focus. At each moment the visual system picks out the clearer of the two images.
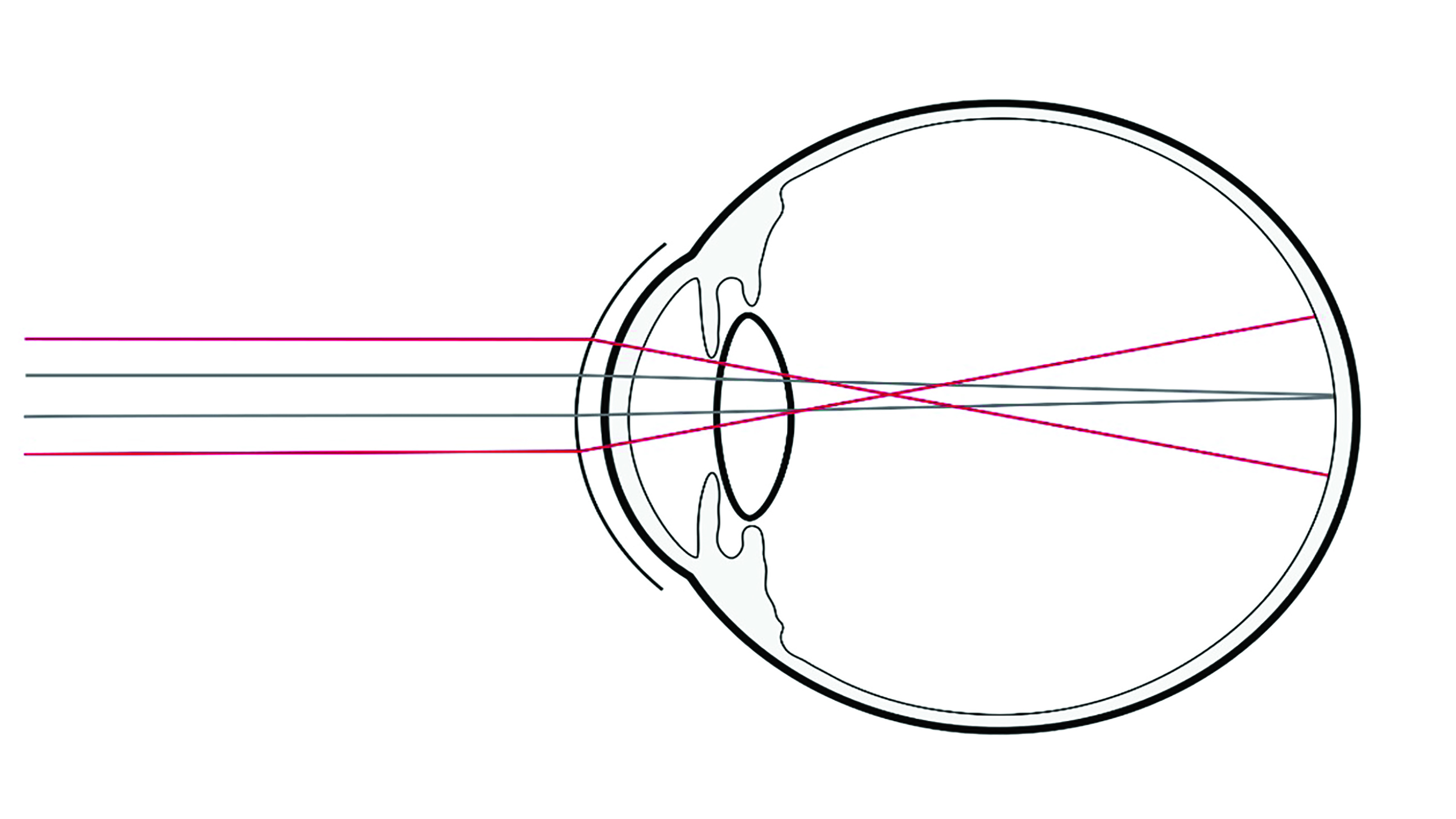
Figure 8: Principle of a simultaneous vision centre-distance design, where the grey rays illustrate light passing through the distance portion of the lens and the red rays illustrate rays passing through the near portion of the lens
The greater the eccentricity (or rate of flattening) of the back surface aspheric curve, the higher the reading power in relation to distance power. However, the higher the reading addition, the more likely that distance vision will be affected adversely, especially in low contrast and/or low light conditions where the pupil is larger.
One disadvantage of a centre-distance system is the limited positive spherical aberration generated and as such, they are only suitable for early presbyopes up to ~+1.25DS. Another fundamental concern of this design is its dependency on the pupil size. The near pupil reactions mean that as a near object is brought into view proportionally, less of the pupil allows light in from the near zone of the lens.
Centre-near
Centre-near designs were introduced to address the problem of pupil constriction for close work. The optical principle is the same as for the centre-distance lens, although reversed, so this time it is the central portion of the lens that provides the near correction, with the surround providing the required distance power (figure 9). This is achieved by utilising a front surface aspheric design which generates negative spherical aberration from the centre of the lens. 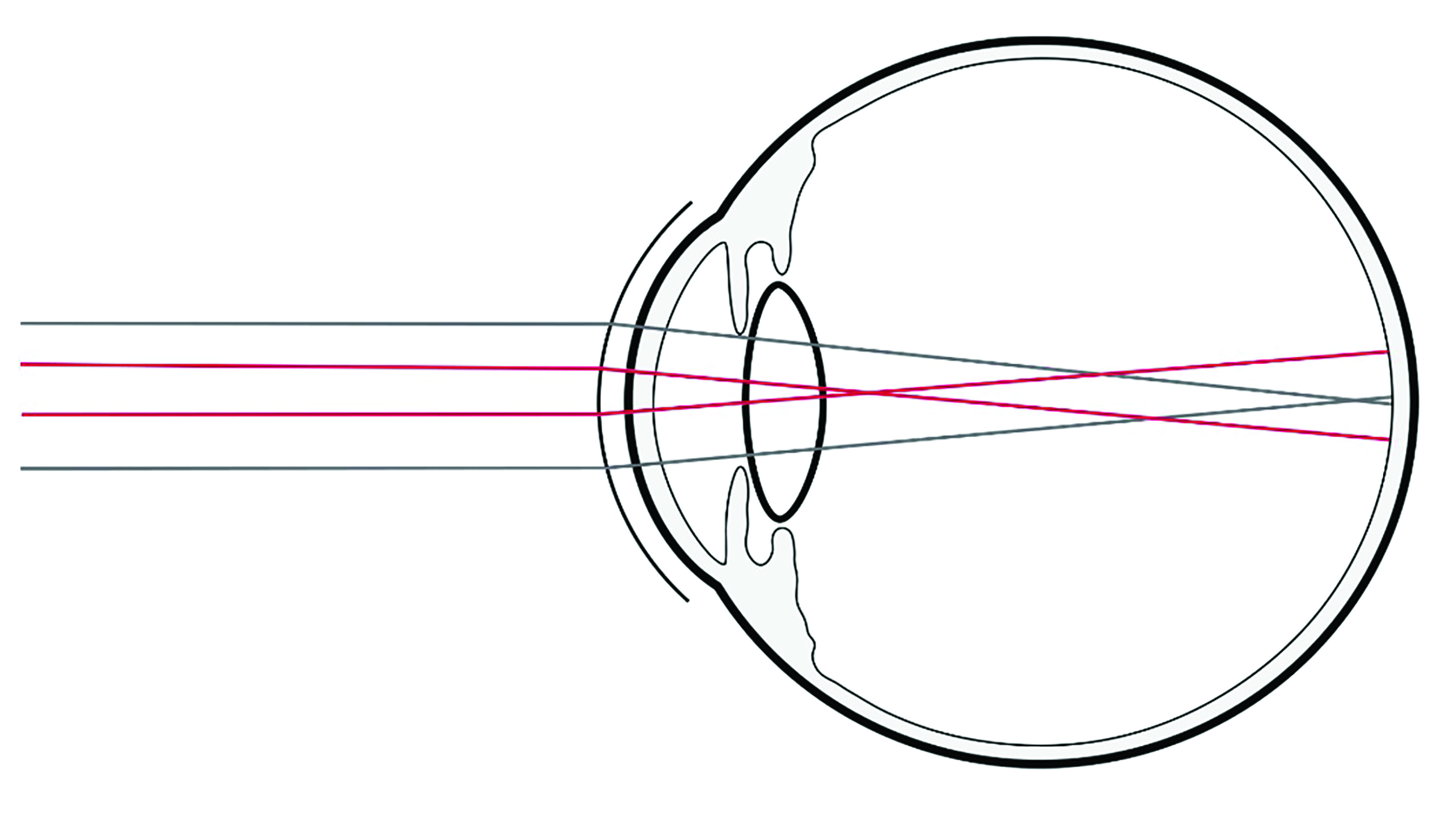 Figure 9: Principle of a simultaneous vision centre-near design where the red rays illustrate light passing through the near portion of the lens and the grey rays illustrate rays passing through the distance portion of the lens
Figure 9: Principle of a simultaneous vision centre-near design where the red rays illustrate light passing through the near portion of the lens and the grey rays illustrate rays passing through the distance portion of the lens
It would be expected that the visual performance achieved would depend upon the interaction of the optical characteristics of the lens design with the natural aberrations of the eyes of the wearer. Consequently, variations in ocular aberration between individuals may explain in part why lenses of this type meet the needs of some wearers but not others.22 The power distributions of centre-near lenses are seen to vary from one lens to another, therefore, it is often worth attempting a different lens to see if performance can be improved if vision is unsatisfactory with the first design.
With improving levels of optical performance and patient satisfaction, centre-near lens designs now dominate much of the soft multifocal contact lens market and have contributed to the recent growth in presbyopic contact lens correction.3
Principles of simultaneous vision lens fitting
Physical fit
Simultaneous image lenses, particularly aspheric design, should be fitted with good centration and minimal movement. It is critical that the lens is well centred over the visual axis to enable the correct portion of light to pass through each part of the lens. As the lens decentres away from the optical axis, aberrations increase, to the detriment of vision. Slit lamp assessment of centration is not sufficient to determine centration with regards to the pupil. A simple method to assess whether higher order aberrations are impacting vision involves directing the patient to observe a spot of light under dim illumination and to describe the shape of the light. Should they describe the light as having a ‘streak’ or ‘tail’ this is indicative of induced coma. Alternatively, if a topographer is available, corneal elevation maps can be used to help determine centration.
Trial lens power selection and visual assessment
Initial lens power will vary, with manufacturers recommending different strategies for varying designs, as such the corresponding fitting guide should be followed. A good starting point for any fitting is an up to date refraction, measured best vision sphere and an add that delivers adequate functional vision. Most designs are sensitive to 0.25DS adjustments to the distance lens power which can have a profound effect on distance or near visual performance, pushing the highest plus acceptable for distance, and the least plus for near, to avoid excess accommodation (in patients that have residual accommodation) with an over-minused refraction. Lens power adjustments are best investigated by using +/-0.25DS twirls/flippers or trial lenses during binocular vision in ambient illumination or the illumination where problems are being experienced by the wearer. The use of phoropters should be avoided during over-refraction as the resulting light reduction will increase pupil size and alter optical performance.
Both static and dynamic visual assessment should be carried out as previously described. If a satisfactory distance and near correction cannot be achieved, many manufacturers recommend moving towards a ‘modified monovision’ technique, by over-correcting one eye and under-correcting the other. This typically required the assessment of ocular dominance as previously described, with binocular variation to the prescription as in monovision.
Extended depth of focus
Recently, contact lenses providing an extended depth of focus (EDOF) have been introduced to correct presbyopia. EDOF optics utilise higher-order aberrations on the front surface of the lens to broaden the depth of focus to include a larger range of foci, extending vision from distance to near. The optical design of EDOF lenses is expected to mitigate the impact of pupil size, contact lens decentration and individual ocular aberrations on the final visual outcome.23
Alternating
The alternating bifocal was one of the first types of bifocal contact lenses to be produced, designed in a similar way to bifocal spectacle lenses. With alternating contact lenses, the patient looks through the distance portion of the optic zone in primary gaze, then on down gaze, the lens is held up against the lower eyelid, allowing the visual axis to be directed through the near portion (figure 10). The advantage of this design is that visual quality will remain high if the visual axis is directed through the appropriate part of the lens. The disadvantage is that for this to occur, significant eyelid/lens interaction needs to occur, which can lead to decreased patient comfort through increased lens bulk and mobility as well as suffering with issues from lens rotation and stability. The majority of alternating designs are available as RGP lenses due to the requirement of the lens to move effectively on eye; however, soft options are available though not widely prescribed.
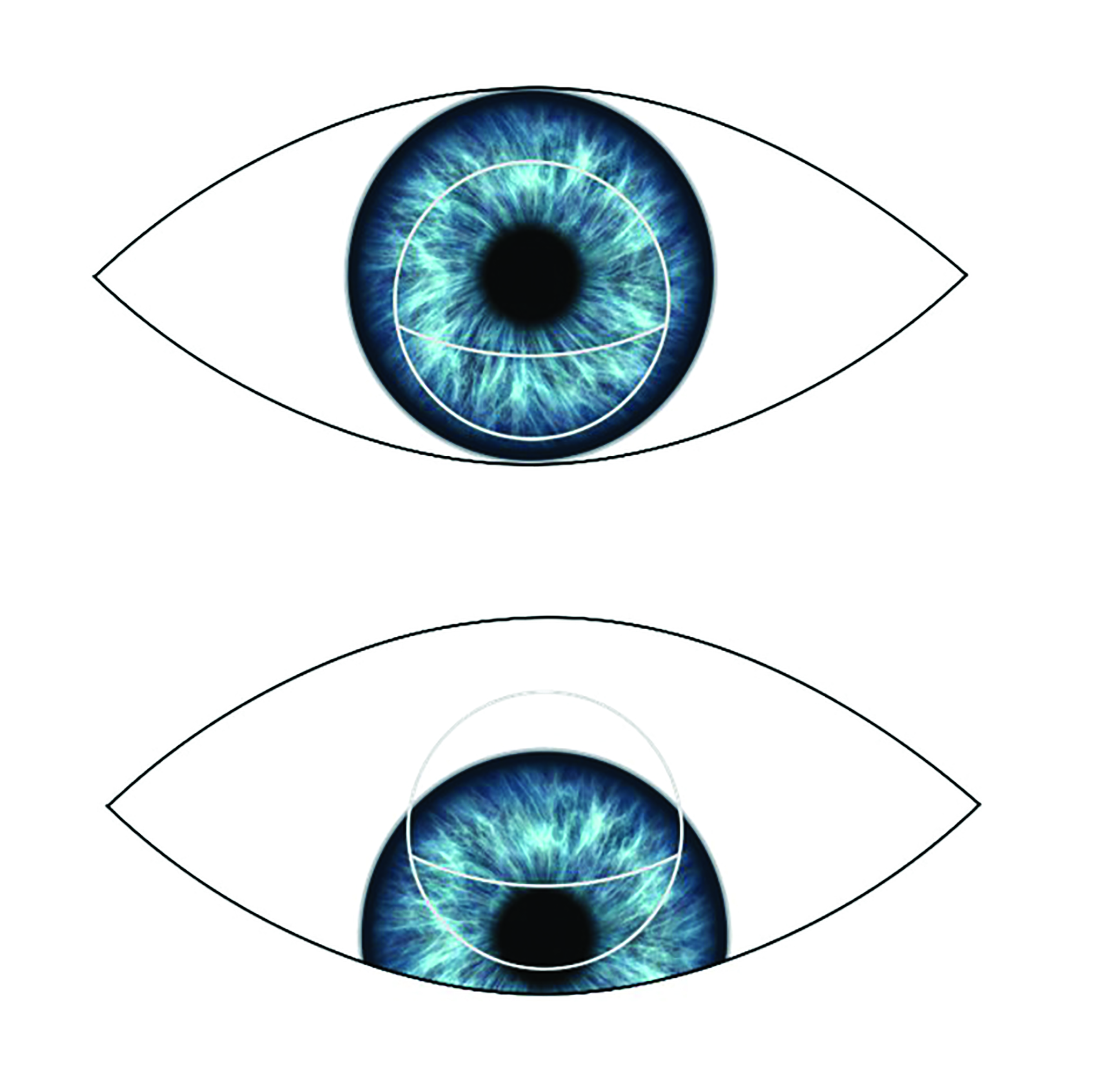 Figure 10: The principle of the alternating bifocal contact lens
Figure 10: The principle of the alternating bifocal contact lens
Principles of Alternating lens fitting
Physical fit
An alternating vision rigid bifocal must be fitted to allow translation between the distance and near zone to occur. The lens should, therefore, be mobile and supported by the lower eyelid. This is normally achieved by fitting on alignment or with minimal apical clearance. In primary gaze, the lower pupil margin should be in line with the top of the near segment (figure 11). On near vision, the pupil should look through the near segment (figure 12).
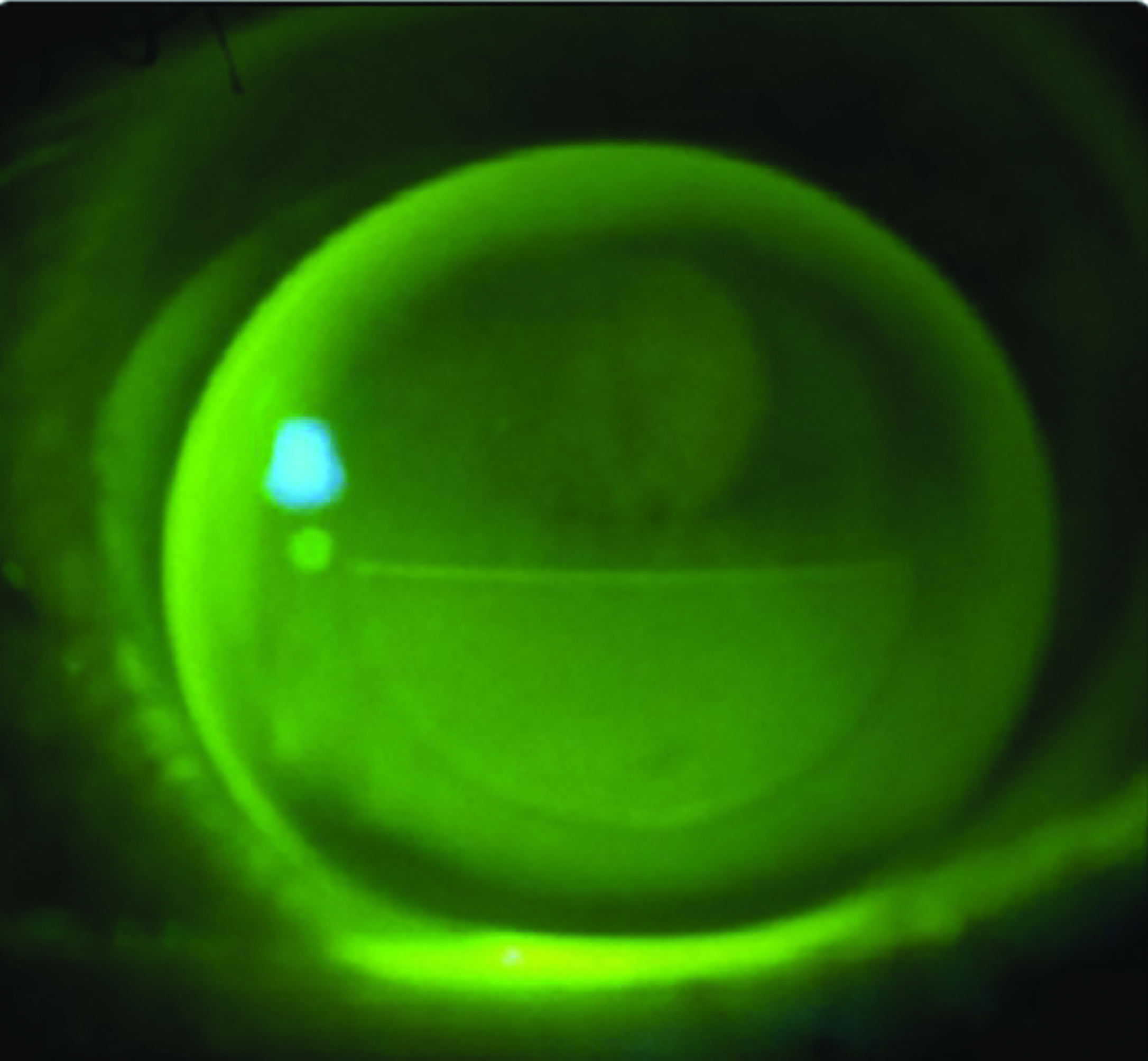 Figure 11: Alternating RGP lens fit showing segment position in primary position of gaze
Figure 11: Alternating RGP lens fit showing segment position in primary position of gaze
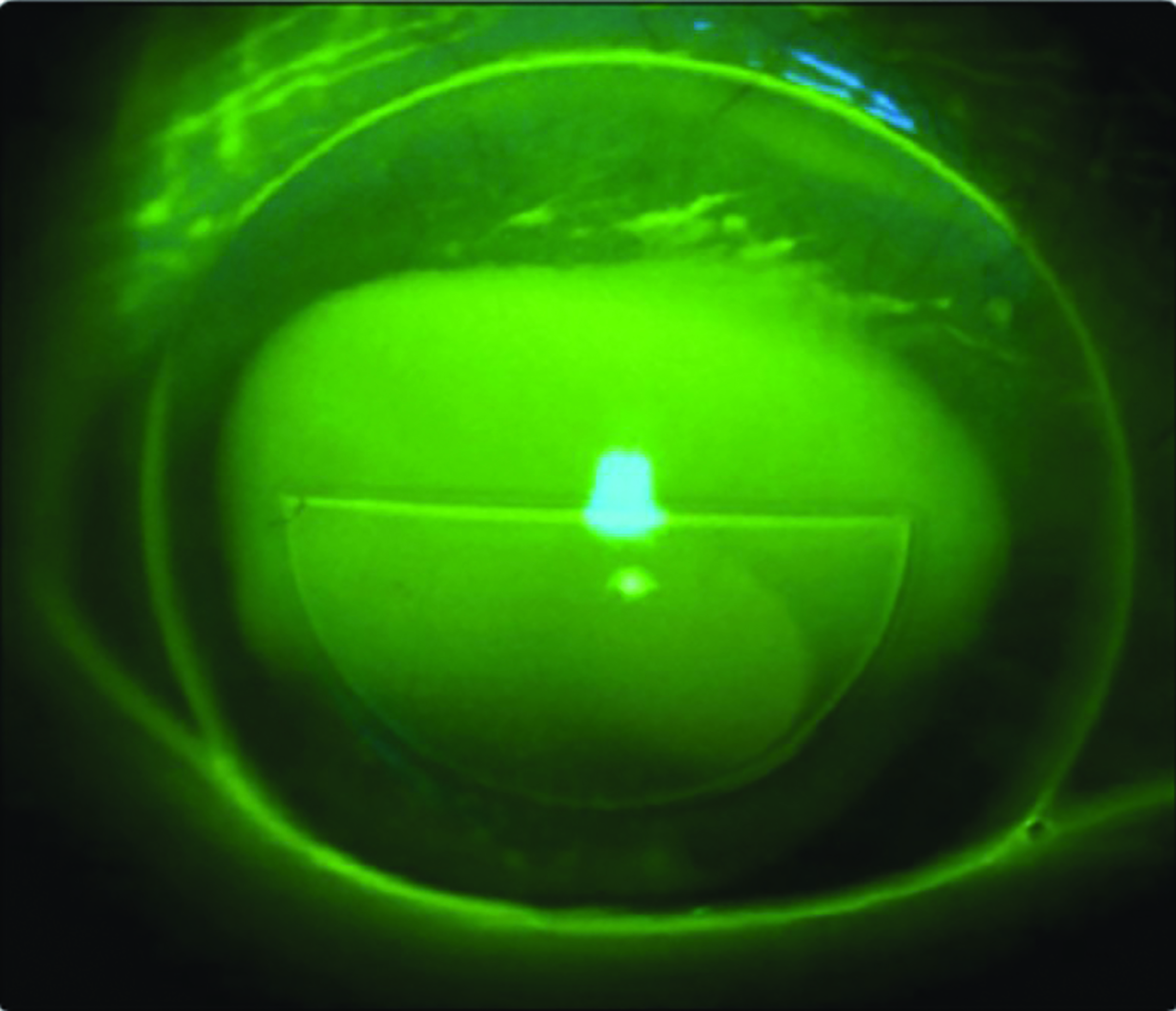
Figure 12: Alternating RGP lens fit showing near segment positioned over the pupil in downgaze due to successful translation
Trial lens power selection
Once the lens fit has been optimised, a normal binocular over-refraction should be carried out at both distance and near. The use of a trial frame and lenses is preferred to a phoropter as it allows a more natural head posture, which is critical in fitting this type of lens.
Conclusions
As the number of presbyopes rises, so too does the demand for contact lens correction for these individuals. Being aware of the different lens designs, fitting approaches and the associated advantages and disadvantages (table 2),24 along with the patient’s personality, occupation and previous lens wearing history, helps in understanding which is the more appropriate starting point in meeting the patient’s visual needs. With 70% of presbyopic patients stating poor vision as a reason for drop out,25 every effort should be made to maximise the visual outcome. 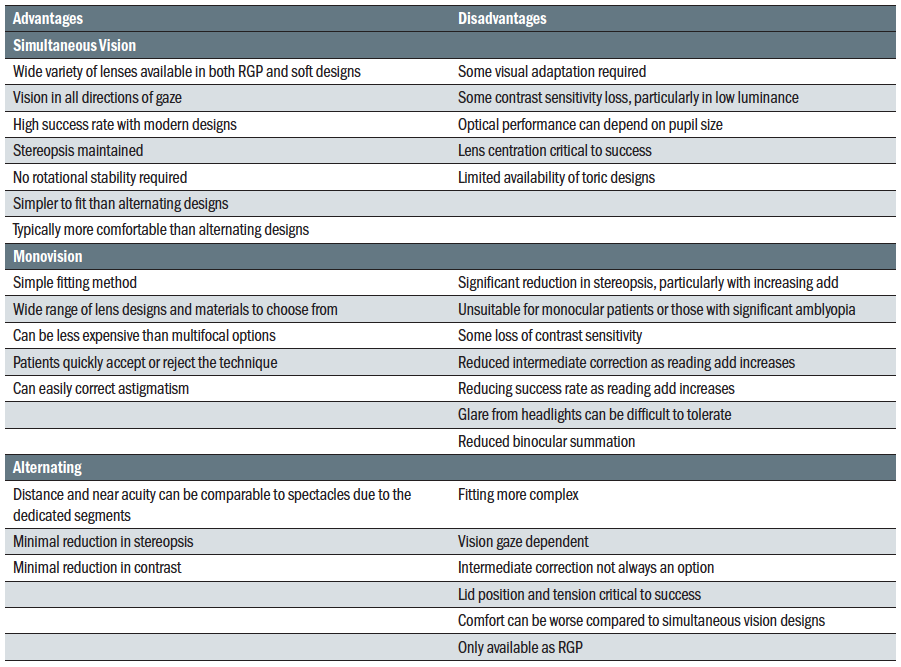 Table 2: Advantages and disadvantages of lens fitting options for presbyopia correction (adapted from Efron24)
Table 2: Advantages and disadvantages of lens fitting options for presbyopia correction (adapted from Efron24)
There are now more lens options than ever to offer our presbyopic patients and the lack of the ‘perfect’ solution (spectacles included) for the presbyope should not discourage practitioners from fitting this ever-increasing patient base. New simultaneous designs with improved optical performance are now quick and easy to fit, with a high fit success rate and good acceptance as the add increases. Daily disposable multifocal lenses offer patients greater levels of convenience and more flexibility for the part-time wearer. As no one lens design fits all, practitioners should be proficient in fitting two or three alternative lens designs so that a sound clinical approach can be developed and used with confidence, with the result that this form of fitting becomes an integral part of contact lens practice. •
Dr Louise Madden is an Optometrist, Senior Specialist Educator for NHS Scotland, Visiting Lecturer at Glasgow Caledonian University and is a paid consultant for Johnson & Johnson Vision. Dr Rachel Hiscox is a Professional Education & Development Manager, UK & Ireland for Johnson & Johnson Vision Care.
- This article is part of a revised and updated ‘Essential Contact Lens Practice’ series, originally authored by Jane Veys, John Meyler and Ian Davies. This article was produced without further input or review from the original authors.
References
- Fricke TR, Tahhan N, Resnikoff S, Papas E, Burnett A, Ho SM, et al. Global Prevalence of Presbyopia and Vision Impairment from Uncorrected Presbyopia: Systematic Review, Meta-analysis, and Modelling. Ophthalmology 2018 Oct;125(10):1492-1499.
- 2011 Census: Population Estimates for the United Kingdom. Office for National Statistics: London, Statistical Bulletin 2011.
- Morgan PB. International Contact Lens Prescribing in 2019. Contact Lens Spectrum, 2020;35:26-32
- Bennett ES. Bifocal and Multifocal Contact Lenses. Phillips A & Speedwell L (eds). In: Contact Lenses, 6th Edition, Elsevier. 2018:265.
- Stapleton F, Alves M, Bunya VY, Jalbert I, Lekhanont K, Malet F, Na KS, Schaumberg D, Uchino M, Vehof J, Viso E, Vitale S, Jones L. TFOS DEWS II Epidemiology Report. Ocul Surf. 2017 Jul;15(3):334-365
- Cakmak HB, Capil N, Simavli H, et al. Refractive error may influence mesopic pupil size. Curr Eye Res, 2010:35;130-136
- Dumbleton K, Guillon M, Theodoratos P, et al. The effects of age and refraction on pupil size and visual acuity: implications for multifocal contact lens design and fitting. BCLA Conference Presentation, 2015
- Wolffsohn JS, Davies LN. Presbyopia: Effectiveness of correction strategies. Prog Retin Eye Res 2019 Jan;68:124-143.
- Charman WN. Developments in the correction of presbyopia I: spectacle and contact lenses. Ophthalmic Physiol Opt 2014 Jan;34(1):8-29.
- Evans BJ. Monovision: a review. Ophthalmic Physiol Opt 2007 Sep;27(5):417-439.
- Hayashi K, Yoshida M, Manabe S, Hayashi H. Optimal amount of anisometropia for pseudophakic monovision. J Refract Surg 2011 May;27(5):332-338.
- Fernandes PR, Neves HI, Lopes-Ferreira DP, Jorge JM, Gonzalez-Meijome JM. Adaptation to multifocal and monovision contact lens correction. Optom Vis Sci 2013 Mar;90(3):228-235.
- Rajagopalan AS, Bennet ES, Lakshiminarayanan V. Visual performance of subjects wearing presbyopic contact lenses. Optom Vis Sci, 2006;83:611-615
- Schor C, Landsman L, Erickson P. Ocular dominance and the interocular suppression of blue in monovision. Am J Optom, 1987;64:723-730
- Schor C, Landsman L, Erickson P. Ocular dominance and the interocular suppression of blur in monovision. Am J Optom Physiol Opt 1987 Oct;64(10):723-730
- Erickson P. Potential range of clear vision in monovision. J Am Optom Assoc 1988 Mar;59(3):203-205.
- Sivardeen A, Laughton D, Wolffsohn JS. Randomized crossover trial of silicone hydrogel presbyopic contact lenses. Optometry Vision Sci 2016;93(2):141-149.
- Morgan PB, Woods CA, Tranoudis I, Helland M, Efron N, Jones L, et al. International contact lens prescribing in 2015. Contact Lens Spectrum 2016;31(1):24-29.
- Benjamin WJ, Borish IM. Presbyopia and the influence of aging on the prescription of contact lenses. In Ruben M & Guillon M (Eds), Contact Lens Practice. London: Chapman & Hall. 1994:763-828
- Harris M, Sheedy J, Gan C. Vision and trask performance with monovision and bifocal contact lenses. Optom Vis Sci, 1992;19:609-614
- Meyler J, Veys J. A new ‘pupil-intellifent’ lens for presbyopic correction. Optician, 1999;217(5687):18-23
- Pérez-Prados R, Piñero DP, Pérez-Cambrodí RJ, Madrid-Costa D. Soft multifocal simultaneous image contact lenses: a review. Clinical and Experimental Optometry 2017;100(2):107-127.
- Bakaraju RC, Ehrmann K, Ho A. Extended depth of focus contact lenses vs two commercial multifocals: Part 1. Optical performance evaluation via computed through-focus retinal image quality metrics. J Optom. 2018 Jan-Mar;11:10-20
- Efron N. Contact lens Practice, 3rd Edition. Elsevier Health Science, 2018.
- Sulley et al. Prospective evaluation of new contact lens wearer retention rates. Scientific paper presentation at BCLA/NCC Conference, May 2016
