The authors both qualified in the 1980s when glass lenses remained commonplace and the fashion was moving towards frames that would be considered enormous by modern standards – Coronation Street character Dierdre Barlow wore a 61-eye Silhouette model 1198 and eye-sizes over 56mm were the norm rather than the exception, even for patients with narrow PDs. The increase in lens sizes brought problems with thickness, weight and comfort but perhaps the biggest challenge was accurate centration and avoiding prismatic effects that were outside of tolerance. Manufacturers rose to the challenge, introducing larger and decentred blanks, low powered aspheric and atoric lens designs and an ever-increasing range of lighter weight mid and high refractive index materials in both glass and plastic. For patients who considered plastic inferior to glass lenses (usually for reasons of scratch resistance) the challenge was even greater due to the smaller size of available lenses. Nevertheless, as is the way with fashion, customers got what they wanted.
At the time the British Standard tolerance (BS2738:1985) was 0.25Δ of differential prismatic effect in the vertical meridian and 1.00Δ horizontally. However, the received wisdom or rule of thumb was that patients could in fact tolerate 1.00Δ vertically and 3.00Δ horizontally, and then, as now, registrants could override the standards in the best interest of the patient by working to these tolerances rather than the British Standard.
Since the eyes are designed to converge, patients can still achieve fusion and binocular single vision with a good deal more base-out prism than 3.00Δ and because of this the requests of hyperopes with narrow interpupillary distances and a desire to look like a TV star were often agreed to against the better judgement of the practitioner. The situation was exacerbated because at the time dispensing was newly derestricted and increasingly patients would see non-registered dispensers who lacked comprehension of the issues that were being caused.
The standards did not differentiate between patient’s ability to overcome greater levels of base out prism compared to base in, and still do not. However, the ‘rule of thumb’ was sensible in many respects, since a pair of -20.00D lenses would need to be centred to a clearly unrealistic level of accuracy of an eighth of a millimetre, (c=P/F=0.25/20=0.0125cm).
Later the tolerances enshrined in BS 2738-1:1998 came into force to correct this anomaly with the new tolerances: 0.25Δ plus 1mm vertically and 0.25Δ plus 2mm horizontally for low powers (≥2.00DS) and 1mm vertically and 2mm horizontally for higher powers. There were additional tolerances on prescribed prisms of ≥2.00Δ and ≥10.00Δ of 0.37Δ and 0.50Δ respectively.
BS 2738-1 is much missed (and still used in some practices) as it was easy to remember the specifications for centration as well as those for the prescription itself, however having a relatively small set of tolerances applicable to a wide range of lens powers again produced levels of accuracy that were unrealistic in some prescriptions. BS 2738-1 was superseded by BS EN ISO 21987:2009, which was subsequently replaced by BS EN ISO 21987:2017, which was confirmed as remaining in force in 2020 by the publication of the tracked changes version to allow practitioners and manufacturers to easily view the amendments brought about by the technical revision in 2017. The details of the current standards relating to induced and prescribed prism are shown in table 1 and are also plotted in graphical form in figures 1 and 2.
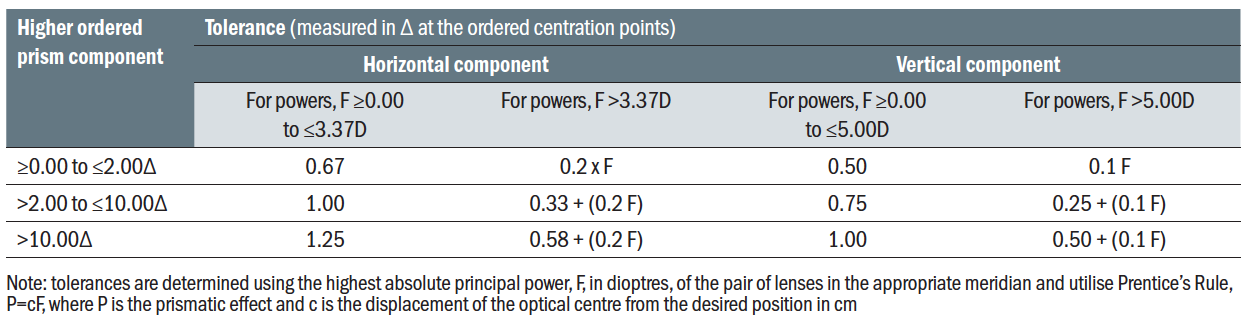
Table 1: Prism imbalance (relative prism error) tolerances for single vision lenses (excluding position-specific single-vision lenses) and multifocal lenses (values in prism dioptres Δ)
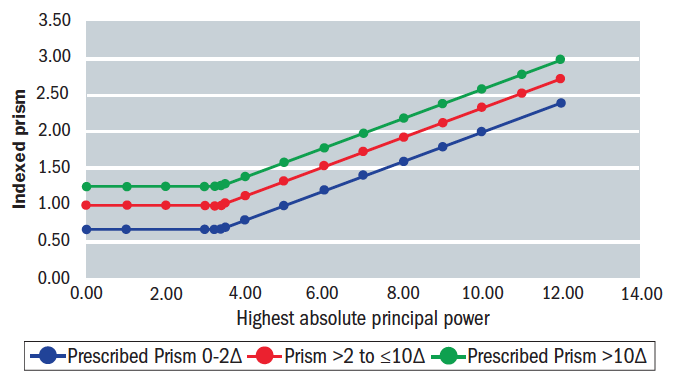 Figure 1: Horizontal relative prism error tolerances (BS EN ISO 21987:2017)
Figure 1: Horizontal relative prism error tolerances (BS EN ISO 21987:2017)
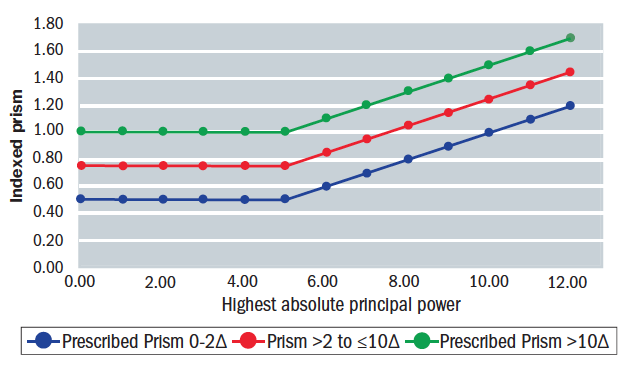 Figure 2: Vertical relative prism error tolerances (BS EN ISO 21987:2017)
Figure 2: Vertical relative prism error tolerances (BS EN ISO 21987:2017)
The issue of inadequately supervised non-registered dispensing staff, with little ability to recognise differential prismatic effect, let alone know what to do about it, remains an issue to this day. Induced prism is a common cause of eye strain, headaches and dissatisfaction with new spectacles. Clinical time is often wasted with unnecessary re-checks, and patients may be given a refund unnecessarily when practice staff do not have the knowledge or inclination to solve the problem. As the following cases show induced prismatic effects are not obvious to the untrained eye, and the solutions often require a level of underpinning knowledge that only comes with qualifications that lead to registration as an optician.
A lack of knowledge on the part of dispensing staff also extends to their ability to verify that finished spectacles actually comply to the applicable manufacturing standards. World weary lab managers often report spectacles returned as incorrect that are in fact within tolerance, and the authors have witnessed on several occasions, practices using out of date standards from 1998 and 2009 as recently as 2020.
BS EN ISO 21987 is still not perfect. In particular it does not allow for accurate provision of small prisms along with high levels of ametropia. For example, if a -12.00D was prescribed 1.00Δ Base UP, it could legitimately be supplied as 0.2Δ Base DOWN and still be within standard. Although such small prisms in combination with large prescriptions are very rare this situation is clearly
non-sensical.
The experience of a previous fashion for very large frames and induced prismatic effects beyond those determined by British Standards has led to a greater understanding that compromising centration for the purposes of fashion is a bad idea and did not in the end turn out to be in patients’ best interests. Patients with no alternative means of clear vision were easily persuaded to go away and get used to their incorrect centration.
However, when these patients returned a few years down the line, by which time fashions had changed to small round eyes, or shallow rectangular frames, the problem was clear to see. Having adapted to inaccurate centration they could no longer tolerate their centres being accurate and would not be prepared to go away and ‘get used to’ their new glasses a second time unless they were given a detailed explanation or dispensed several consecutive pairs with the centres gradually made more accurate.
The situation had been exacerbated by the practice of allowing dispensers to order spectacles without measuring the blank-size of the required lens, despite the large differences in cost price between standard and extra-large sizes, and leaving this to be determined by the lab who would often use maximum decentration from a standard blank that was held in stock. It should not be necessary these days to cut corners to this extent – even if a lens will not cut from an available blank size it is possible, at least in single vision non-aspheric lenses, to incorporate surfaced prism to counteract any prism that might be induced and move the optical centre to the correct position.
What little research there is into accuracy of ophthalmic dispensing demonstrates clearly that errors in centration are common,1 especially with spectacles ordered online to average measurements, and although patients can often tolerate large amounts of horizontal prism and maintain binocular single vision for distance it should be born in mind that this may have a detrimental effect on binocular near vision and disrupt the relationship between accommodation and convergence.
Accommodation is the eye’s ability to increase its positive refractive power measured in dioptres and enables the emmetropic eye to focus on near objects at a distance (in metres) equal to the reciprocal of the amount of accommodation exerted. The amplitude of accommodation is the maximum amount of dioptric change and can be measured clinically using an RAF rule. During accommodation the ciliary muscle contracts reducing the tension on the zonular fibres allowing change in the radii of the crystalline lens, most change is at the anterior surface producing a more steeply curved thicker lens of greater power. As both the ciliary muscle and the iris sphincter muscle receive innervation from the same nerve supply (parasympathetic root of the third cranial nerve, the oculomotor nerve) accommodation is accompanied by miosis.
The stimulus for accommodation is blur, as the eyes fixate a near object a disjunctive vergence movement occurs.
Case 1
A 45-year-old myope, -6.00DS R&L, vertex distance 12mm, has an amplitude of accommodation of 3.50D. They alternate between contact lenses and correctly centred spectacles (PD 62mm) and complain that they feel near vision is not as comfortable in their contact lenses.
Assuming that the patient views a near object at 40cm from the eye it can be determined that the patient will experience differing levels of both accommodation and convergence with contact lenses compared to spectacles.
With contact lenses the amount of ocular accommodation required to see an object at 40cm is the same as for the emmetropic eye and can be simply determined as the reciprocal of the working distance:
However, the ocular accommodation required with spectacles is different. If we assume the spectacle lens to be thin then the object distance, l1
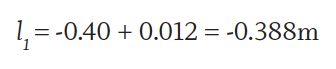
The near object is -38.80cm in front of the spectacle lens
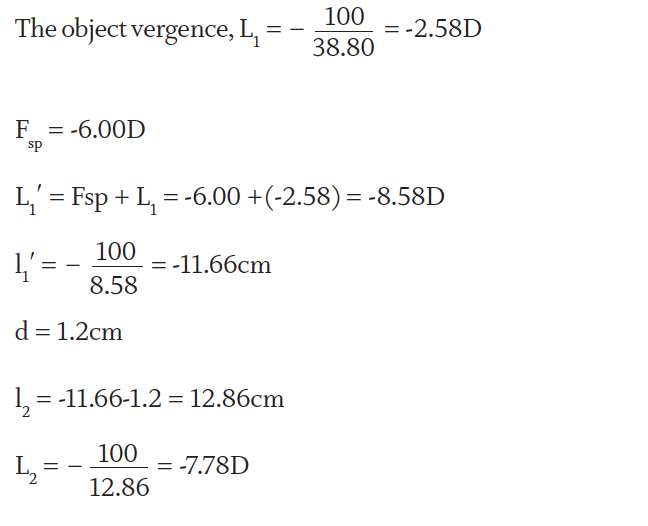
L2 will be the vergence meeting the eye
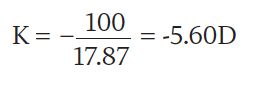
To determine the ocular ametropia, K=1/k;
Where k = fsp - d = -16.67 - 1.2 = -17.87cm
Ocular accommodation, A = K- L2 = -5.60 – (-7.78) = +2.18D
+2.18D of ocular accommodation would be required when wearing spectacles to place the image on the retina.
If the patient was wearing contact lenses (assuming the contact lens to be thin):
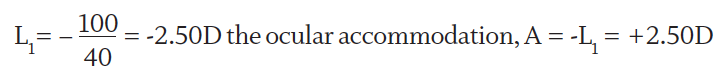
Wearing spectacles +2.18DS of accommodation is required compared to +2.50DS when contact lenses are worn, which equates to 62% and 71% of the patient’s amplitude of accommodation respectively. It is generally accepted that for protracted close work patients can only use half to two-thirds of their amplitude of accommodation comfortably and in this case wearing contact lenses requires more than 2/3 of the available accommodation to view an object at a working distance of 40cm and hence the patient had symptoms.
The opposite would be true for a hypermetrope and more ocular accommodation would be required when wearing spectacles than contact lenses.
Another aspect to consider is convergence. For the myope base in prism occurs when spectacles centred for distance are used to view a near object meaning the eyes are required to converge less and need less ocular accommodation compared to wearing contact lenses. Convergence needs to be considered alongside accommodation as they are linked with the drive to provide clear bifoveal images but, as long as there is equality of these actions, binocular single vision (BSV) is maintained.
While the myope will need to converge more and accommodate more when wearing contact lenses compared to spectacles the relationship of accommodation to convergence will remain consistent. Nevertheless, issues can arise when a myope wishes to be fitted with contact lenses and is approaching presbyopia or there is a an already large exophoria and it is wise to set expectations in advance including the potential need for multifocal contact lenses before any need for multifocal spectacles.
Much is made of the accommodative convergence/accommodation (AC/A) ratio remaining constant in both spectacles and contact lenses and therefore not being an issue. However, it is not uncommon to find myopes who are very comfortable reading without any optical correction where accommodation is zero, and because of the short working distance, convergence is much greater than would be the case if they were reading in specs or contact lenses. In myopic patients that are emerging into presbyopia it is therefore accommodation that is likely the problem rather than convergence.
Case 2
Patients often struggle to articulate problems associated with induced prismatic effects, and this is hardly surprising given the ability of the brain to move the eyes to maintain binocular single vision. Most patients have phorias to some degree and easily compensate for them, however induced prismatic effect can cause binocular vision to break down, and vertical prism even if compensated for can reduce the ability to compensate for horizontal imbalance. It is counterintuitive to realise that a patient who knocks their frame out of alignment such that one optical centre is now higher than the other could experience intermittent horizontal diplopia because the exertion of creating vertical fusion diminishes horizontal fusional reserves.
Patients who are at the limit of their fusional reserves may experience intermittent diplopia that might be obvious to them, however the diplopia might be so slight that the overlapping images are perceived as blur rather than diplopia. Figure 3 shows the relative position of the images seen by the left and right eyes (coloured white and red respectively for clarity though obviously the images would be the same in each eye). Esotropia (or decompensated esophoria) shows homonymous diplopia (the left eye’s image is on the left) whereas exotropia shows heteronymous diplopia (the left eye sees the image in the right). However, if we consider tiny phorias, including cyclophorias, or double vision caused by differing amounts of spectacle magnification in aniseikonia or aberrational oblique astigmatism we can easily imagine that without the benefit of each eye seeing a different colour as illustrated the diplopia could easily be perceived as blur. For this reason, optometrists should take more care to assess binocular vision, including at near, and especially if the patient is presenting for a recheck or second opinion.
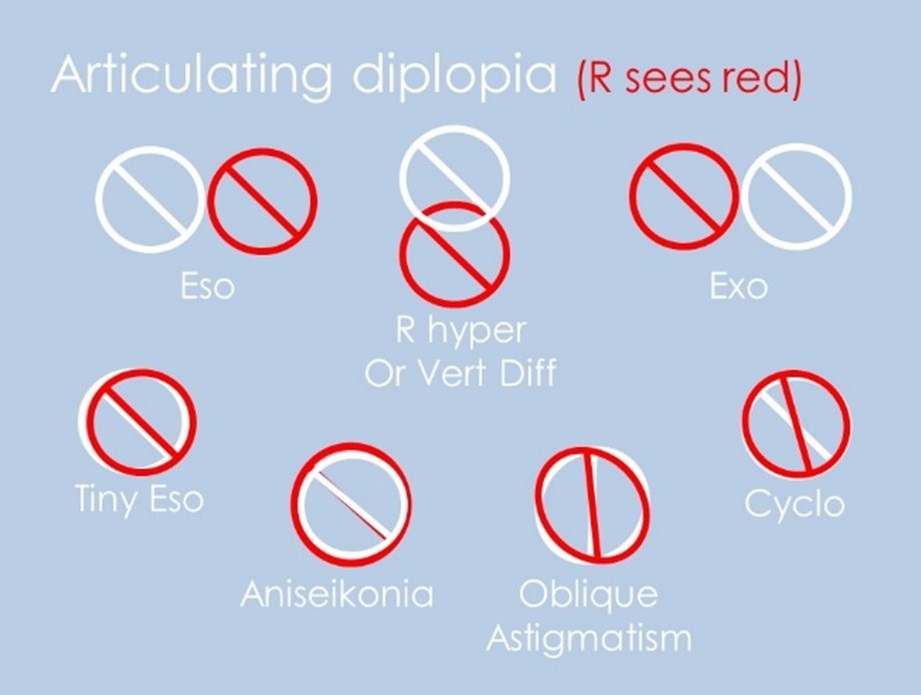 Figure 3: Patients may struggle to articulate that they are experiencing diplopia as slight diplopia, or superimposed images of slightly different shapes or sizes, may be perceived as blur
Figure 3: Patients may struggle to articulate that they are experiencing diplopia as slight diplopia, or superimposed images of slightly different shapes or sizes, may be perceived as blur
Tiny errors are commonplace in optics, some down to human error and misunderstanding, others built into the system of measurement. For example, a dispensing optician with a PD of 70mm taking the PD, using a ruler, of a child whose actual PD is 44mm would record a PD of 45.5 or 46mm even if the correct
procedures were followed thanks to parallax error.
Clinical audits of record cards often reveal a near centration distance that is only 2mm smaller than the distance interpupillary distance. Simple geometry reveals this to be untrue, yet it prevails in an erroneous ‘just knock 2mm off the PD’ instruction to optical assistants that somewhere along the line lost the clarifying ‘per eye’ that used to be in the middle of the sentence.
In each of these cases the measurements are within 1mm monocularly and therefore may be within tolerance, however if we then accept a further error due to manufacturing tolerance, we can see that a 4mm error of horizontal centration binocularly has become acceptable even with very high prescriptions.
Vertical centration is an even bigger issue, especially for single vision dispensing, and especially where it is measured. Clinical audits and experience of practitioners who deal with ‘visual concerns’ on an appointment basis each day show that most patients would be better off with their vertical optical centres glazed at the default position on horizontal centre line rather than having their heights measured and specified on the order.
Old habits die hard and many practitioners stick with what they are used to rather than looking at the scientific evidence that suggests a change in approach. Accurate vertical centration requires the centre of rotation condition to be satisfied (that the optical axis of the lens passes through the centre of rotation of the eye) and therefore requires pantoscopic tilt to be taken into account. Many dispensers have no means of measuring pantoscopic tilt, confuse pantoscopic angle with angle of side (see earlier articles in this series for more detailed explanation), or simply do not understand why it is necessary and therefore do not bother.
The following case shows an example of how measuring optical centre heights vertically and placing on pupil centre is likely to cause more problems than it will solve.
Spectacle prescription:
Tokai 1.76 bi-aspheric.
R -4.25/-1.50 x 180
L -5.75/-2.00 x 180
The patient complains of eye strain and the tell-tale ‘I feel like my eyes are being pulled out of their sockets, especially when using the computer.’
Checking the spectacles on the focimeter revealed optical centres perfectly aligned with pupil centre, both horizontally and vertically as had been ordered. The pantoscopic tilt was measured at 10°. There had been only minimal change in prescription from the previous 1.74 back surface aspherics, however they had been glazed on HCL which corresponded with a point 6mm below pupil centre and matched the previous pantoscopic angle of 12°.
A failure to match the vertical centration to the pantoscopic tilt induces aberrational astigmatism at the optical centre of the lens because the centre of rotation condition is not satisfied and although this was noticed by the patient it was of secondary importance to the anisometropia here.
In the primary position although there was some minor blur, there was no differential prismatic effect. However, relative to the old spectacles to which the patient was accustomed, the prism situation was very different.
It is worth considering how we use our eyes on a daily basis to understand why fitting vertical optical centres on pupil centre is a bad idea for anisometropic patients, aside from the obvious creation of unwanted small cylinders that change the effective power of the lens.
For most people, most of the time, their direction of gaze ranges between, perhaps, 25° either side of, 10° above, or 45° below the primary position. Outside of this area, any eye movement is likely to be accompanied by a head/body movement to lessen the deviation of the eyes and the effort exerted by the oculorotatory muscles. Even tasks thought to involve protracted concentrated distance vision at approximately eye level, such as driving for example, are actually quite varied in terms of the direction of gaze since drivers must also regularly look at their mirrors, speedometer etc. On average we spend our time looking down rather than straight ahead and the centration of single vision lenses (and therefore the pantoscopic tilt) should reflect this.
Considering our case, imagine the patient is using their computer screen at a distance of 50cm from the spectacle plane (figure 4). For ease we will assume the screen has been set up according to the recommended ergonomics with the top of the screen, A, at eye level and angled, not unreasonably, at an angle equal to the pantoscopic tilt, p, of the spectacle lens which we will assume to be 10°. The vertical screen dimension, AF, is 25cm.
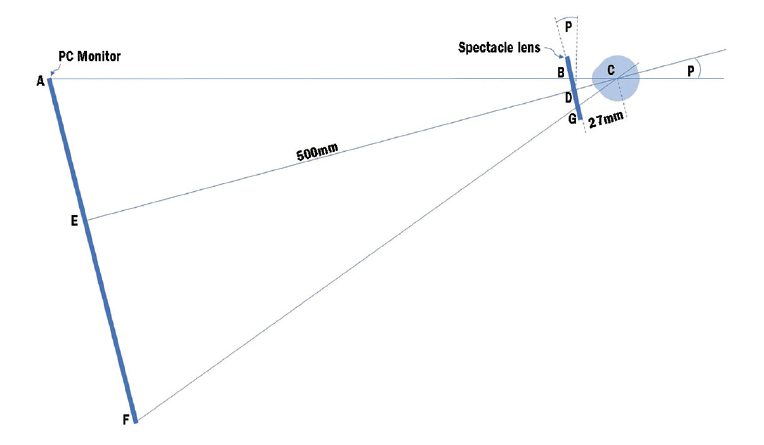 Figure 4: Computer screen position for case 2
Figure 4: Computer screen position for case 2
With the lenses fitted as originally dispensed, so with the optical centres lying on the primary direction of gaze at point B, there is no vertical differential prismatic effect. At the point D, the notional ideal position (5mm down from pupil centre for a 10° tilt) then prismatic effects can be calculated as follows:
R -4.25/-1.25 x 180 so the power in the vertical meridian is -5.50D.
P = cF = 0.5x5.50 = 2.75Δ Base Down
L -5.50/-2.00 x 180 so the power in the vertical is -7.50D.
P = cF = 0.5x7.50 = 3.75Δ Base Down
The differential prismatic effect when viewing the point E on the screen is 1.00Δ base down in the left eye which, as we have seen, is only just tolerable for most people.
Obviously, if the patient wishes to view a point lower on the screen say the point F at the bottom, which is 25cm lower than the top of the screen the differential prismatic effect will be increased dramatically unless the patient lowers their head in order to utilise more paraxial parts of the lens.
We can use simple geometry to determine the distance of point E on the screen and point G on the lens.
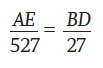
And since BD = 5mm for a pantoscopic angle of 10°
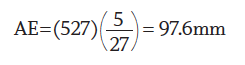
Since the screen is 250mm deep then EF is 152.4mm, so by similar triangles:
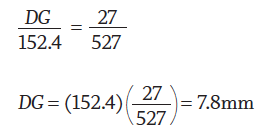
In other words, the patient will be looking through a point 13.8mm below the distance optical centre if the OCs are placed on pupil centre and will therefore experience 2.76Δ base down left eye of differential prism which is beyond the tolerance of the vast majority of patients. Keeping the distance optical centres on pupil centre should mean either finding frame with zero pantoscopic tilt, or, dispensing personalised single vision lenses where small cylindrical components are worked into the lens to counteract the cylinders induced by failure to meet the centre of rotation condition. Then the left eye could be slabbed off, removing 2.75Δ base down left eye from the bottom half of the lens positioning the dividing line of the bi-prism at the lower limbus.
Figure 5 shows the process used to slab off a minus lens, removing base down prism from the most minus eye. In examinations students often state that a slab off single vision lens looks similar to an executive E-Line bifocal, however it does not. The dividing line is a faint crease (see figure 6) rather than a ridge and with modern freeform techniques tends to be blended and therefore virtually invisible. Slab-off is however not available in all materials including the 1.76 material originally selected and the 1.74 previously worn so the patient would require to move to 1.67 material.
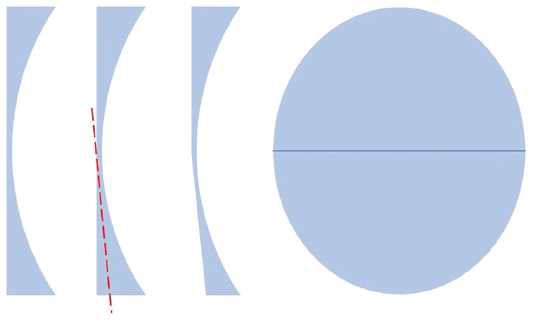 Figure 5: Slabbing off a minus single vision lens
Figure 5: Slabbing off a minus single vision lens Figure 6: A single vision slab off lens
Figure 6: A single vision slab off lens
However, with careful centration and adequate instruction, it may have been best in the first instance to dispense the lenses with the vertical optical centres positioned to satisfy the centre of rotation condition, 5mm below pupil centre for a tilt of 10º. Returning the patient to their previous satisfactory centration specification (at point D in figure 4) subjects them to 1.00Δ base up left eye of differential prismatic effect for distance when the eyes are in the primary position, and 1.00Δ base down left eye at a near vision point 10mm below this, both of which are just within tolerance and provide the patient with a much larger area of comfortable vision and a minimum of head movement to view the bottom of the screen comfortably.
Case record 3
Cataract surgery has always been a potent source of problems relating to induced prismatic effect, from the monocular aphakic with 10+ dioptres of anisometropia to the, no less problematic but slightly more manageable, modern obsession among ophthalmologists to leave the eye as close to plano as possible even though the other eye may be hyperopic or myopic to some considerable degree. However, even quite low post cataract prescriptions can cause significant problems.
The patient had cataract surgery on both eyes within six weeks of each other and the final Rx was as follows:
Silhouette Photo Sensation Panorama PPL (personalised progressive)
R. +1.50 / -1.50 x 120 Add +3.00
L.+1.00 / -1.00 x 30 Add +3.00
As post-cataract prescriptions go, this low powered prescription appears at first glance unlikely to cause problems especially as it is not too dissimilar to the patient’s previous Rx:
Previous Rx: Zeiss Progressive Individual 2
R. +1.00 / -1.00 x 180 Add +2.50
L. +0.75 / -0.75 x 180 Add +2.50
However, the patient complained of a sensation of her eyes being ‘pulled’ and suffered occasional vertical diplopia when tired, both tell-tale indicators of vertical differential prismatic effect. To determine the prismatic effect, it is perhaps easier to transpose into plus cylinder forms in each case.
The previous Rx once transposed is revealed as plano cylinders with their axes vertical and therefore no power in the vertical meridian and hence no vertical differential prismatic effect.
While it would be easy to ignore the cylinders, and only use the spheres to determine the differential prism, that does not tell the whole story. This is most easily demonstrated here by transposing to the plus cylinder form:
R.E. Plano / +1.50 x 30
L.E. Plano / +1.50 x 120
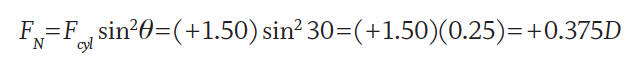
Using the formula for notional power of a cylinder:
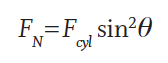
where θ is the angle between the power meridian (at right angles to the axis) and the meridian we want to calculate the notional power for (in this case the vertical meridian as we are seeking to determine the vertical differential prismatic effect when the patient looks down).
For the right eye, 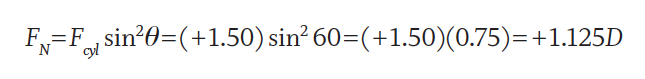
For the left eye,
At a point 10mm below the distance optical centre (prism reference point), using Prentice’s Rule (P=cF), we can see there is 0.75Δ base up right eye differential prism. This we might reasonably expect the patient to tolerate. However, with progressive lenses, the patient is likely to habitually be using a point lower down the lens in order to obtain the full reading addition so could easily be experiencing more prismatic effect. More to the point, this patient has previously had a lifetime with no vertical differential prismatic effect and as was discussed in the previous article there is considerable evidence that even small amounts of vertical prism cannot be tolerated.
In such cases problems might be expected and can be mitigated to some degree by opting for the shortest possible corridor length even in a deep frame. Where the differential is above 1.00Δ, it is still perfectly possible to keep the patient in progressive lenses. Modern freeform surfacing techniques mean that many progressive power lenses (PPLs) are available with slab off, removing base down prism from the bottom portion of the most negative/least positive lens (in this case, the left lens). Alternatively, a ‘reverse slab on’ adds base up to the distance portion only of the most plus/least minus lens. In this case, a Norville personalised progressive was selected and the prism split equally between the eyes. Unlike a traditional slab-off lens which has a noticeable ‘crease’ across the lens, freeform bi-prism lenses are barely noticeable (see figure 6 for a single vision example).
Clearly this patient had opted for premium quality lenses and this case was not, as is often the case with private patients, constrained by budget. NHS patients who require prism controlled multifocals, such as slab-off, are entitled to voucher H which goes at least part way to covering the cost.
Had this patient had concerns relating to cost then opting for bifocal lenses would be a less expensive option. A slab-off bifocal (shown on a fused glass D-seg in figure 7) is an option, although may not be much cheaper since slabbing-off can increase the cost price several-fold.  Figure 7: A glass fused slab off D-seg bifocal
Figure 7: A glass fused slab off D-seg bifocal
A cost-effective option would be to dispense odd sized bifocal segments. Round segments give the opportunity to correct significant differential prism, and in this case would be an option.
To alleviate 0.75Δ base up right eye, we need additional base down in the right near portion to counteract it, hence the larger round seg needs to go in the least minus or most plus eye measured in the vertical meridian. We know we require 0.75Δ base down more prism in the right segment than in the left so we can select an appropriate size segment in the left and then calculate the segment size for the right using Prentice’s Rule (P=cF). Normally the formulae are combined, recognising that segment diameter is twice the radius and there are 10mm to a cm, to give a formula for segment diameter difference as follows:
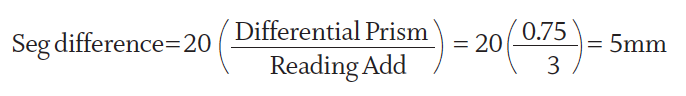
which in this case from the round segment bifocal lens options available can be exactly satisfied using R45 in the right and R40 in the left, or can be very nearly satisfied by R28 and R24 segments respectively.
A little known and little used alternative in cases of low amounts of differential prism is to use odd sized D-segments with differing amounts of base down at the dividing line. A favourite option used to be the S40 no-jump bifocal, however that has recently been discontinued by most labs. Nevertheless, some options remain. Figure 8 shows a solution to this prescription. The right lens is an S35 segment which is 22mm deep. Since the segment centre must be 17.5mm from the bottom of the seg (half of 35mm) then the seg OC must be 4.5mm from the segment top. The S45 segment is 22.5mm deep so the seg OC is 1.5mm below the seg top. 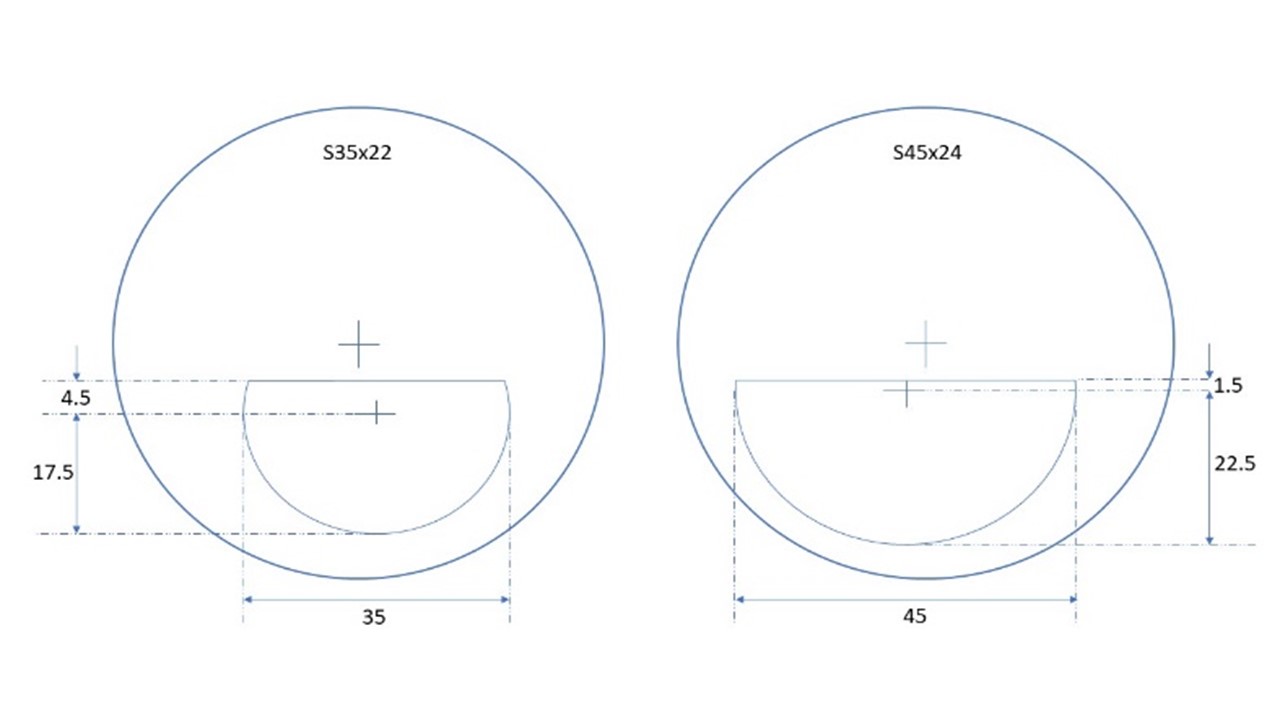 Figure 8: Correcting small amounts of differential prism with odd sized flat top bifocals
Figure 8: Correcting small amounts of differential prism with odd sized flat top bifocals
Using P=cF the prismatic effect due to the segment is 0.45 x 3 = 1.35Δ base down in the right eye, and 0.15 x 3 = 0.45Δ base down in the left, a differential of 0.9Δ base down right eye which very nearly counteracts our troublesome differential of 0.75Δ base up right eye and is another way of solving our problem.
Differential prismatic effect caused by oblique cylinders is often missed in practice with practitioners re-calling horrible formulae and time-consuming graphical constructions, however it is not complicated to estimate the vertical power of an oblique cylinder and determine a good approximation of any differential prism. By working through the notional power formula for common angles a simple table could be developed that could be memorised or referred to in practice.
It should be appreciated that a cylinder with its axis along 180 will deliver all of its power in the vertical meridian and that a cylinder with a vertical axis at 90 will have no power vertically. Working through the notional power formula for a variety of axes shows that cylinders with an axis of 45º or 135º will have a notional power in the vertical meridian 50% of that of the cylinder. When the axis lies closer to the horizontal then the power will be greater than half in the vertical meridian: 75% if the axis is 30º or 150º, ~88% if the axis is 20º or 160º. Similarly, if the axis is 60º or 120º then the notional power in the vertical will be 25% of the cylinder power, and at 70º or 110º about 12%.
Figure 9 shows the notional cylinder power in the vertical meridian expressed as a percentage for a variety of axes in 15º steps from 0º to 180º. Practitioners (and students in oral/OSCE examinations) should be in the habit of taking this into account when analysing prescriptions that incorporate oblique or uneven cylinders. In most cases, except if very large, cylinders within 20º of horizontal or vertical can be treated as though they have axes at 180º or 90º and remembering the values for 30º, 45º and 60º are sufficient for estimating whether a problem of differential prism is likely to occur.
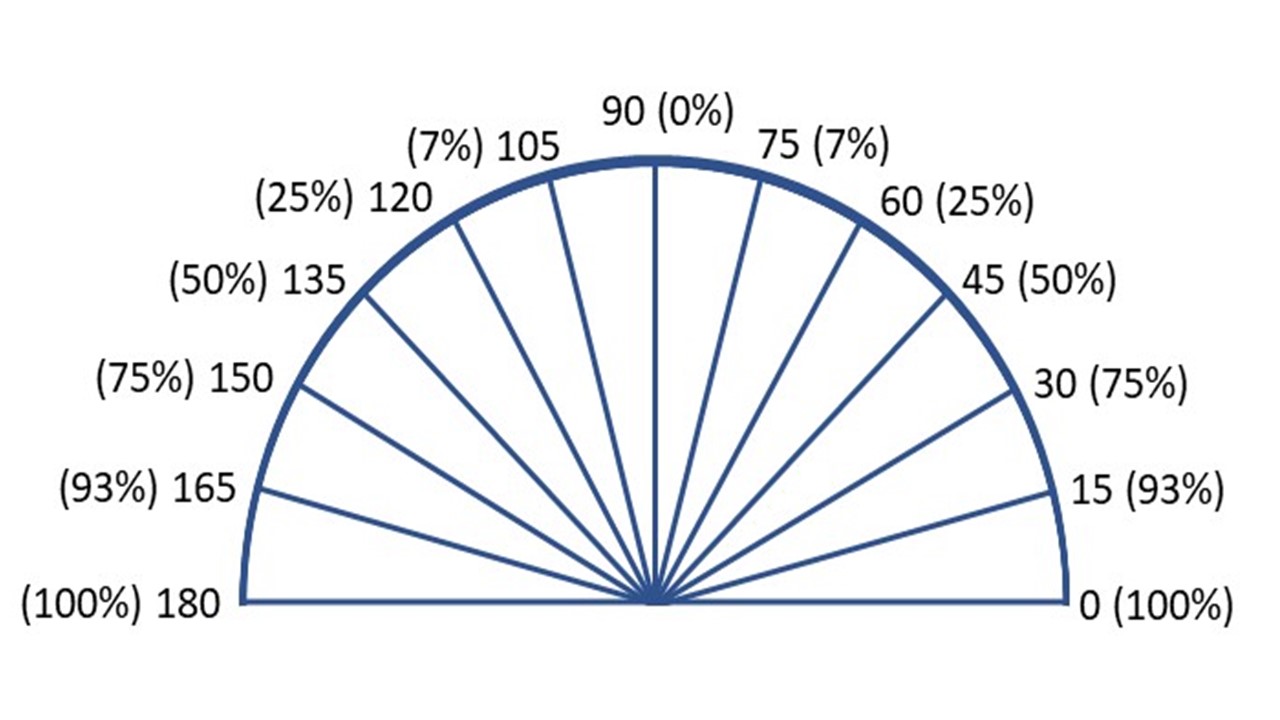 Figure 9: The notional cylinder in the vertical meridian expressed as a percentage for cylinders with axes lying between 0 and 180 degrees
Figure 9: The notional cylinder in the vertical meridian expressed as a percentage for cylinders with axes lying between 0 and 180 degrees
Case study 4
Contact lenses are often heralded, quite rightly, as a great solution to issues relating to anisometropia including aniseikonia and vertical differential prismatic effect. Previously we have seen that the anisometropia does not always cause aniseikonia since it depends on whether the eyes are axially or refractively ametropic. Differential prismatic effects always accompany anisometropia and are a problem unless the patient suppresses or is amblyopic or has some other cause of impaired visual acuity in one eye. Here we will discover that rarely contact lens can even cause differential prismatic effect.
Spectacle prescription
R.E. -3.00 / -0.75 x 5
L.E. -2.50 / -1.25 x 175
Corrected by contact lenses:
R: PureVision 2; 8.60/14.00/-3.25DS
L: PureVision 2 for Astigmatism; 8.60/14.00/-2.50 / -1.25 x 180
Px has no complaints with regard to spectacles but wears contact lenses a few times a week and complains of eye strain, discomfort, and occasional vertical diplopia.
Here the problem is caused by the failure to fit a toric lens in the right eye. Most practitioners would now correct an 0.75DC cylinder rather than utilise a best sphere approach as it is demonstrated to provide better visual acuity and contrast sensitivity. The issue here, however, is that the toric left lens is stabilised by means of prism ballast of approximately 1.00Δ base down which is not present in the right eye’s spherical lens as corrected.
By refitting the right eye with a toric lens with prism ballast matched to the left eye, the differential prism can be alleviated. An alternative approach would be to keep the right lens as a spherical lens and fit a toric lens (such as Acuvue Oasys for Astigmatism) that does not use prism ballast as its method of stabilisation. The use of a toric lens stabilised by ‘thick and thin zones’ should also be front of mind when one eye has a spherical prescription and the other is astigmatic.
Overall disposable toric lenses tend to have prism ballast of the order of 1.00Δ or less and so in theory should not present a problem if fitted monocularly. However as outlined in the previous article some patients are sensitive to levels of differential prism less than 1.00Δ, while for others they may already be compensating for a small vertical imbalance and the presence of prism ballast in one eye only could be the straw that breaks the camel’s back and causes decompensation of a barely compensated phoria.
Conclusion
Binocular vision, prescribed prism and minimising induced prismatic effects are at the heart of optometry and ophthalmic dispensing practice. In three short articles it is impossible to fully do justice to the subject, however practitioners should now be more mindful that many, if not most, complaints of a visual nature are likely to have at least some component that relates to the occasional break down of binocular vision caused by induced prismatic effects or a failure to prescribe required prism.
Often a good deal of detective work must go into solving problems of this nature and it is incumbent upon dispensing opticians and optometrists to be mindful of the likely problems and indicated solutions if they are to avoid inconveniencing patients and incurring unnecessary rechecks and refunds for problems that could easily be solved.
Lens availability is changing constantly. On the one hand, some traditional solutions, especially in glass, are being discontinued. However, on the other hand, free form digital surfacing technology is bringing new innovations and practitioners need to remain up to date.
Finally, perhaps the most important aspect missing from community optometric practice is an assessment of muscle balance, binocular vision and amplitude of accommodation during the eye examination.
Peter Black MBA FBDO FEAOO is senior lecturer in ophthalmic dispensing at the University of Central Lancashire, Preston, and is a practical examiner, practice assessor, exam script marker, and past president of the Association of British Dispensing Opticians.
Tina Arbon Black BSc (Hons) FBDO CL is director of accredited CET provider Orbita Black Limited, an ABDO practical examiner, practice assessor and exam script marker, and a distance learning tutor for ABDO College.
Recommended reading
- Norville prescription companion: https://www.norville.co.uk/acatalog/catalogues/Companion%2025518.pdf
- BS 2738:1985
- BS 2738-1:1998
- BS EN ISO 21987:2007
- BS EN ISO 21987:2017
