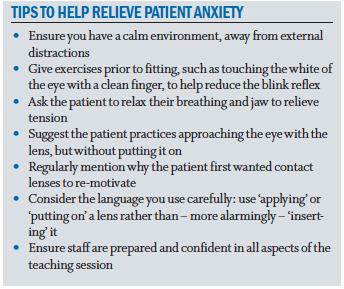
For all new contact lens wearers, the teach is an exciting part of their journey; the final step before independent lens wear at home. The fact that many eye care professionals delegate this part of the fitting is not due to lack of importance but more as a testament to the time required to ensure patients leave the practice feeling confident and motivated to wear their lenses. Done well, the teach appointment builds an important relationship between the practice and their contact lens wearers, instilling trust by offering professional advice and support.
Overcoming challenges faced by new wearers often requires motivation and persistence. Handling difficulties are the principal reason given by one in four new spherical lens wearers for dropping out of lens wear in the first year.1 Therefore, appropriate and personalised support, both during and after the teach appointment is important. Understanding a patient’s motivation for contact lens wear and recognising concerns and anxieties is essential to allow you to personalise the teach experience. Simple methods for continued support once patients leave the practice can then be employed to help reduce drop out in new wearers.
Are you sitting comfortably?
Practices need a designated private, clean area with a comfortable chair, wash basin and mirror for patients to learn how to apply and remove lenses (figure 1). First ensure you have everything you need; contact lenses, case and solutions (if needed), lint-free tissues, support materials and alcohol wipes to clean between patients. A magnifying mirror can also be a great help to high hyperopes and presbyopes. While setting up you can discuss the home environment and possible options for a suitable clean space where they can apply and remove lenses. Pointing out that sitting at a desk or table, rather than standing looking into a mirror over a crowded sink next to the toilet in the bathroom can be helpful advice for a novice wearer.
 Figure 1: A clean private space is essential to teach successfully
Figure 1: A clean private space is essential to teach successfully
Applying lenses
Before application or removal of lenses the first step will always be to ask the patient to wash their hands with soap (preferably anti-bacterial liquid soap) and dry them on a lint-free towel (figure 2). While many patients understand hand washing helps to reduce the risk of infection in contact lens wear, they may cut
corners and not always comply with hand washing advice. A study by Morgan et al in 2011 across 14 countries, found only around 40% of patients were correctly washing their hands before handling their lenses.2 With studies showing an increased risk of contact lens associated infections in patients following inadequate hand washing,3,4 it is important to take time to discuss a proper hand washing routine at this stage before reinforcing it later in the appointment.
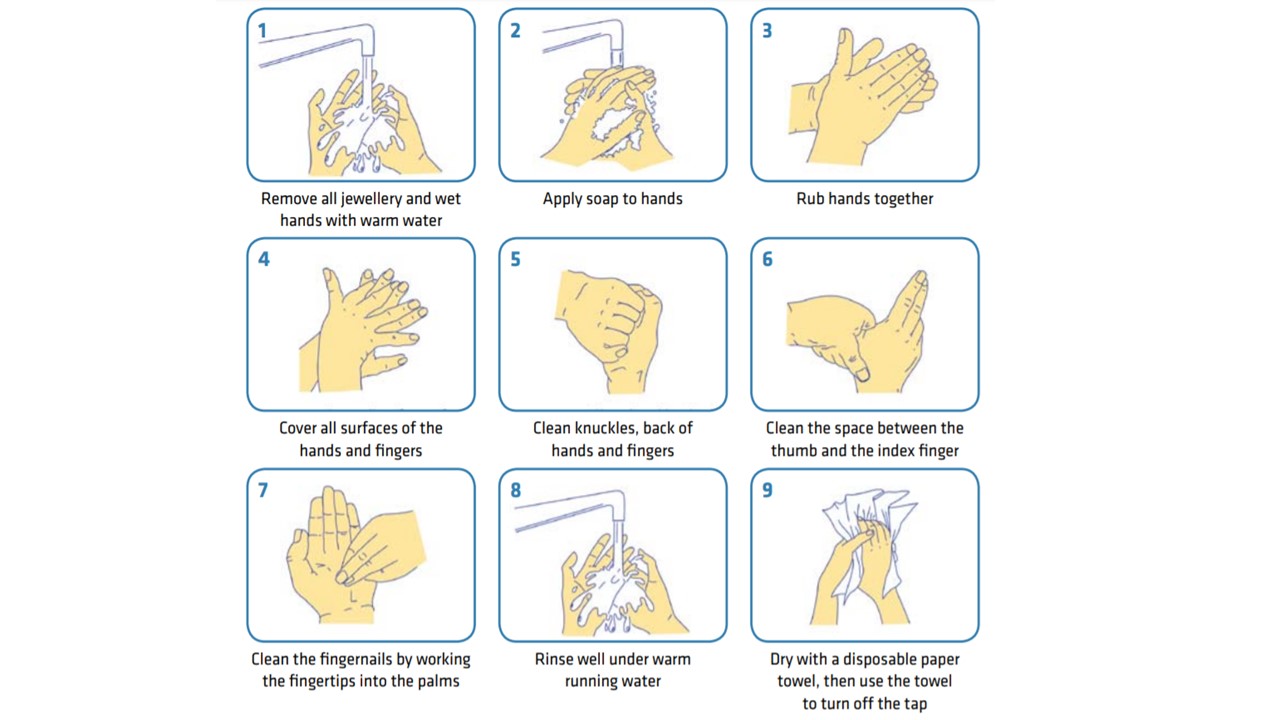 Figure 2: The first step for both application and removal is effective hand washing (Image courtesy of Johnson & Johnson Institute)
Figure 2: The first step for both application and removal is effective hand washing (Image courtesy of Johnson & Johnson Institute)
Preparing the lens
The patient can now learn to handle the lens (figure 3). They may be concerned about damaging the lenses and this is a good time to discuss the importance of short fingernails for novice wearers. Reassurance can be given, if needed, that as they become more proficient many wearers manage to safely apply and remove lenses with longer nails. Comparing the size of the lens to their eye aperture can help the patient understand that they need to hold their eyelids wide apart to get the lens in. At this point the patient should be advised to check that the lens is also clean, tear-free and safe to use (figure 4).
 Figure 3: Check for short clean fingernails as you allow the patient to handle the lens
Figure 3: Check for short clean fingernails as you allow the patient to handle the lens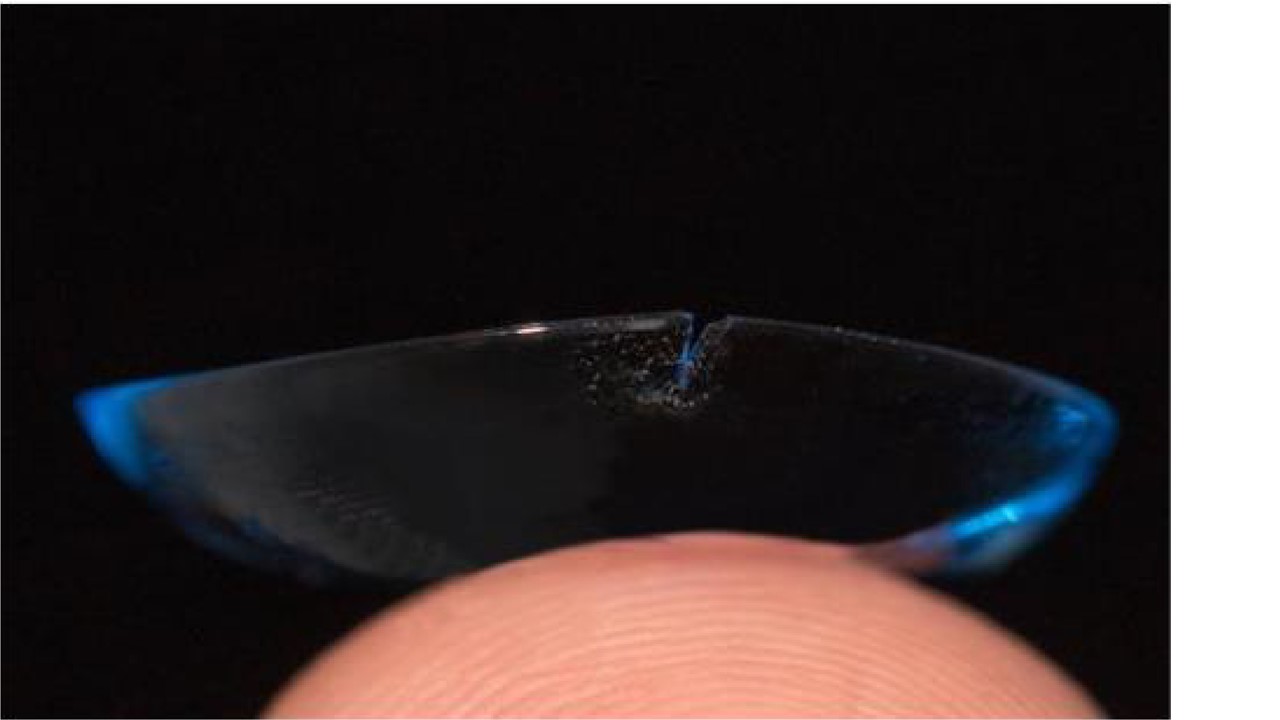 Figure 4: Before application, the lens should be inspected to ensure there is no dirt or debris on the lens and to check for tears, as shown here
Figure 4: Before application, the lens should be inspected to ensure there is no dirt or debris on the lens and to check for tears, as shown here
Which way round?
Preparing and positioning the lens for application is a key concern for patients and clear instructions should be given. Ask the patient whether they would like to apply the right or left lens first and encourage them to stick to this as it helps to prevent lenses getting mixed up.
Remove the lens from the blister pack or storage case. After checking the finger is still dry, carefully position the lens on the pad of the finger. Hold the lens up to the light and check it is the correct way round; if the edges flare out, it is inside out (figure 5). If it looks like a smooth-edged cup then it is the correct way round. Some lenses have indicators to help identify the correct way round and knowledge of these for the lens fitted is helpful.
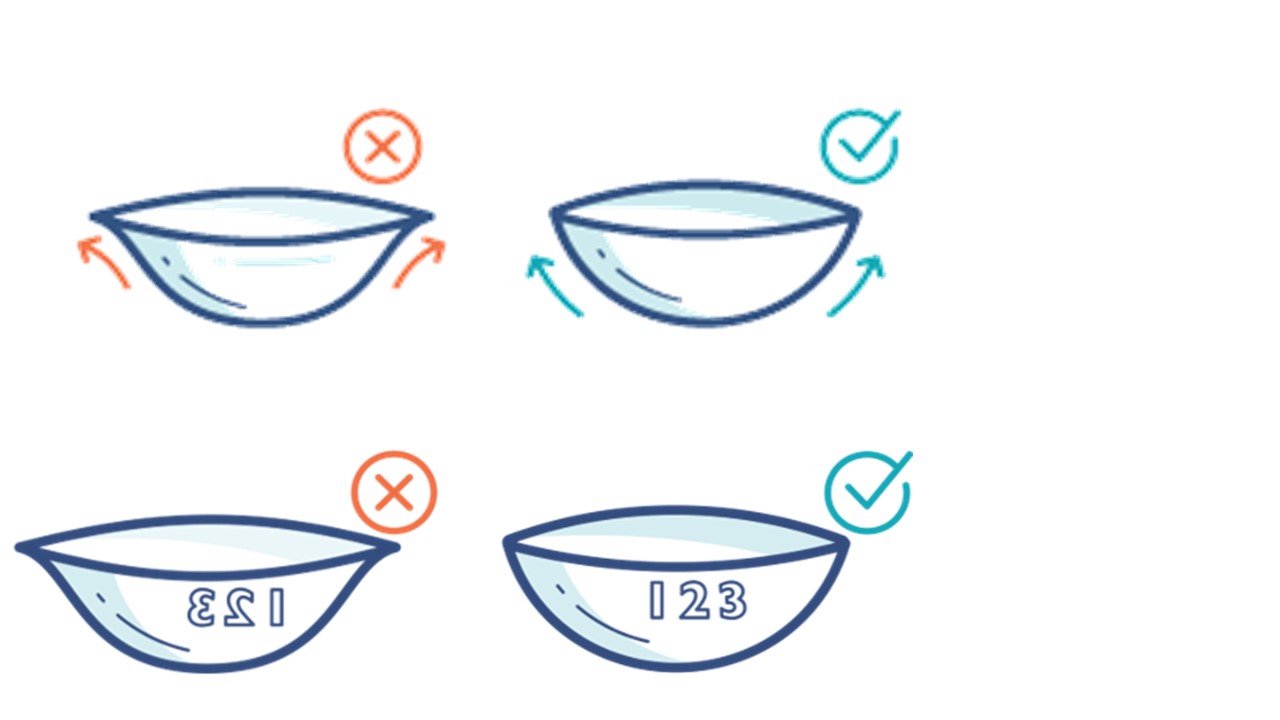 Figure 5: Check the lens is the correct way round before application. Inside-out markers, if available, may help this process
Figure 5: Check the lens is the correct way round before application. Inside-out markers, if available, may help this process
Apply gently and slowly
Both upper and lower lid should then be secured. This is an important step but often proves challenging for the patient. A flexible approach is needed to establish the best option for each patient. For their right eye, start by suggesting that the left hand is placed over their head using the fingertips to lift the upper lid. This may not work for left-handed patients so any approach that allows the patient to firmly hold the lids can be used. It is important the lid is grasped at the lid margin (figure 6). Reminding them that they need to hold lids firmly to overcome the natural blink reflex helps. Consider asking them to try to blink while looking in the mirror can help them understand whether they are grasping the lid firmly enough as the upper lid should
not move.
 Figure 6: Holding the lids correctly – An essential step for successful lens application and removal in a new wearer
Figure 6: Holding the lids correctly – An essential step for successful lens application and removal in a new wearer
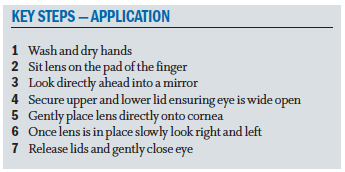
The lower lid should then be pulled down to open the eye wide. As a guide the lids need to be held wide enough for them to observe the entire cornea (figure 6). Lowering the chin slightly so they are looking up a little to the mirror can help widen the aperture. The patient can then be encouraged to slowly place the lens directly onto the cornea. The patient should be instructed to keep both eyes wide open throughout the application process, allowing the eye that is not having the lens applied to fixate and suppress the image of a finger coming towards the other eye. This can take a little time to master and a slow methodical approach is generally more successful. Patients often release the upper lid too soon and so are unable to successfully place the lens of the eye. This leads to frustration and may raise anxiety. Encouraging the patient to stop before application when the lids are not held correctly or if the lens is not in the correct place can help. Repeated attempts lead to anxiety and frustration, focus on a few slow quality attempts. Continue to talk to the patient and ask how they are feeling; remember patients may not recall what you have advised if they are feeling stressed.5 Positive feedback and encouragement, reminding them of their motivating factors, is important at this stage.
Removing Lenses
As with application of lenses the first step for removal will be to wash and dry hands. Then, with the patient looking into a mirror, explain that the lids now need to be secured in the same way they were for application. Reinforce that there are different ways to achieve this and suggest starting with the method that worked best for application. Once both upper and lower lids are secured the patient should be instructed to look up slightly.
Remove the lens gently and slowly
While looking up place the pad of the finger on the lens and slide the lens downwards until it is on the white of the eye. Gently squeeze the lens between the thumb and index finger to remove (figure 7). If unsuccessful at the first attempt, it is often best to encourage the patient to release their lids, blink and slowly start the removal process again. Once safely off the eye the patient should check the lens to ensure the whole lens has been removed. For both application and removal instruction, it can be useful to direct the patient to watch videos of other patients going through the process, some examples are available at www.acuvue.co.uk. If a patient continues to struggle with applying or removing their lenses, then you may want to reconsider their lens type. Some lenses can be a little easier to handle than others. Lenses with lower modulus can be more challenging to apply and remove.
 Figure 7: While looking up, the patient should gently squeeze the lens between the thumb and index finger to remove
Figure 7: While looking up, the patient should gently squeeze the lens between the thumb and index finger to remove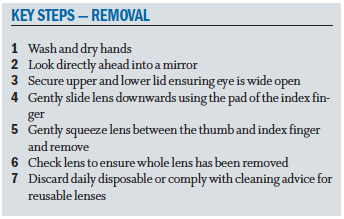
Reuseable lenses
Patients with reusable lenses can then be shown how to comply with their cleaning regimen and case cleaning. The patient instruction guide should always be followed when advising patients how to clean their lenses. Multipurpose cleaning regimens should all require a rub and rinse step; show the patient how to place the lens in the clean, dry palm of their hand, and apply a few drops of the multipurpose solution. Then get them to gently rub the lens back and forth using one finger to clean the lens surfaces on the palm of the hand. The lens should then be rinsed in a little more multipurpose solution before it is placed in a clean case with fresh solution. Case cleaning is also an essential part of the daily cleaning regimen; after applying lenses patients should empty the case discarding all old solution. The case can then be cleaned by rubbing and rinsing with fresh solution before allowing it to air dry, with both the case and cap face down on a clean tissue. Careful consideration needs to be given to a suitable clean place to dry the case, with warm, humid bathrooms being avoided. Remind the patient that the case should be replaced
regularly, typically every month. In a study by Dantum et al in 2016, more than 80% of storage cases were contaminated with microorganisms after only two weeks of use,5 with inadequate cleaning seen to increase the risk of microbial keratitis in another study.6
Lens disposal
Daily disposable lenses should be discarded responsibly after every wear. Setting phone reminders to dispose of reusable lenses at the required replacement interval can be helpful. Discussing local options for recycling of contact lenses and their packaging helps raise awareness of more ethical ways to dispose of lenses (figure 8). Patients should be warned against disposing of their lenses in the toilet or sink as this can add to plastic water pollution.
 Figure 8: Acuvue recycling boxes are available in some practices for all brands of soft contact lenses and their packaging
Figure 8: Acuvue recycling boxes are available in some practices for all brands of soft contact lenses and their packaging
Struggling to apply or remove lenses?
Some patients find application and removal easier than others; some who struggle may require a second appointment to reassure both patient and practitioner while others just need empathetic, honest and open discussion. For this to take place those teaching application and removal should have an understanding of common patient anxieties and barriers to successful lens wear. Practitioners carrying out a teach appointment may assume the barriers to successful lens wear have already been addressed. However, many of these fears and concerns may still remain. Exploring patient motivation to wear, anxieties and potential concerns further at this stage is necessary if we want to minimise drop out in the first few months of wear.
Understanding common barriers to lens wear
Being aware of common concerns raised by patients will help address them. For example, around five in 10 non-lens wearers report that touching their eyes is a key barrier to contact lens wear.7 Research has identified that patients experience a mix of rational and emotional barriers to lens wear. A rational barrier may be a patient who worries that they will poke themselves in the eye causing damage, how a contact lens may feel or whether it will roll behind their eye. An emotional one may be that they are concerned that their work colleagues will consider them as vain. To succeed in lens wear these barriers need to be outweighed by benefits of lens wear. If recognised at this stage concerns can be simple to address, perhaps offering a lens for the patient to feel how ‘soft’ they are or explaining basic anatomy to a patient concerned about lenses rolling behind the eye.
Patient motivation is important
So how do we help patients overcome barriers and progress to successful contact lens wearers? Research shows that highly motivated patients achieve higher levels of satisfaction with their contact lens wear.8 In the same way that a patient experiences a mix of rational and emotional barriers, they will also have a mix of rational and emotional driving forces motivating them to wear lenses. The intrinsic need of a patient to be self-confident at work or the extrinsic fact that they want others to think they are attractive are motivations that may not be discussed with the practitioner, but are perfectly valid reasons to improve the patient’s overall wellbeing. Research shows that emotional motivation and barriers have greater impact on retention of lens wearers than rational ones (figure 9).7 It is these emotional factors that patients are less likely to discuss with you so finding ways to address these issues can help reduce drop out.
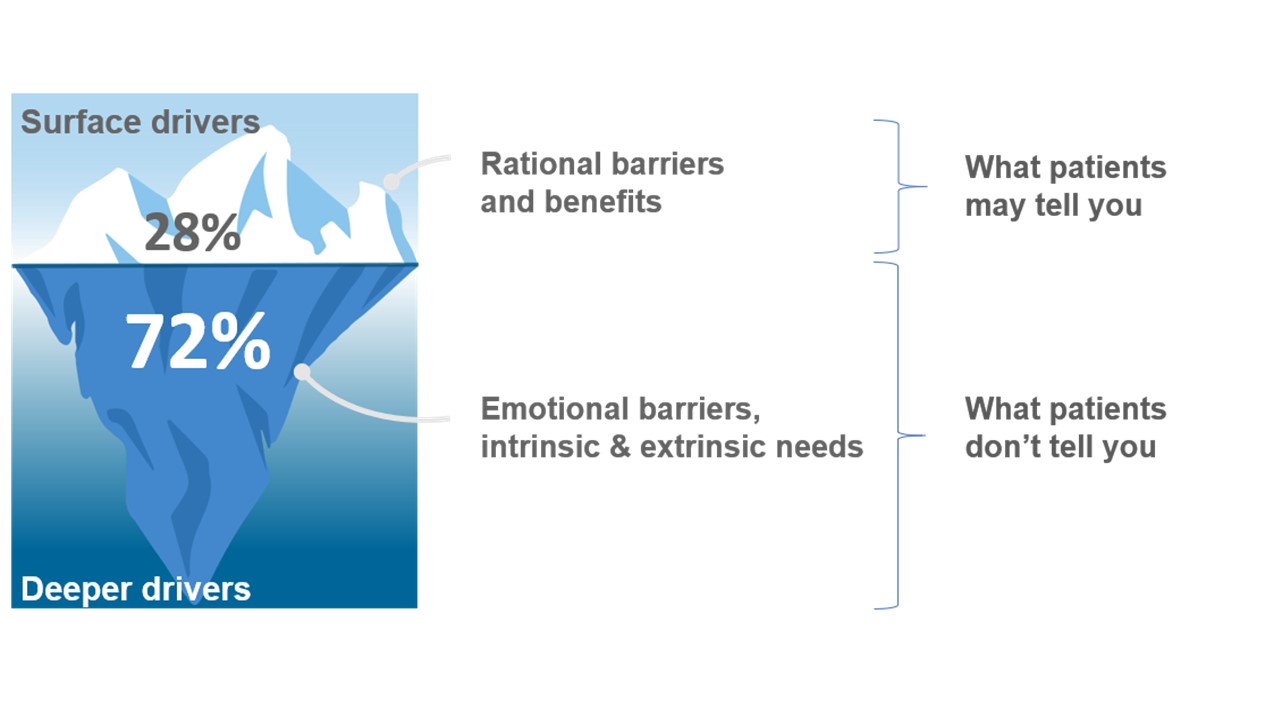 Figure 9: Understanding barriers and motivation to wear is important as patients may not always share their emotions with you7
Figure 9: Understanding barriers and motivation to wear is important as patients may not always share their emotions with you7
Reflecting on our own experiences and emotions when learning a new skill may enable a more empathetic approach. All of us have experience of learning new skills that we can relate to; perhaps learning to ride a bike, play tennis or drive a car. When reflecting on your own experiences some recollections will be more emotional than others. For many, learning new skills as a child or teen may have come more easily, while a relatively simple task learned as an adult takes time and commitment sometimes stirring up emotions of frustration, anger and blame as you struggle to achieve your goal. Success always feels good and for any task glimpses of success and achievement will motivate and encourage, but this often takes time and commitment. The stronger the motivation driving you towards your goal the more likely you are to persist. It is therefore important to identify which driving factor is most important to your patient, then consider using it to motivate them during the contact lens teach.
Don’t overlook patient anxiety
A study looking at anxiety levels for new wearers during the teach appointment found that anxiety peaks just before application and then again before removal.8 Understanding this can alert you to look for changes in tone of voice or body language at appropriate times. Is your patient getting flustered or flushed, do they have a dry mouth or are they starting to sweat? Evaluating patient anxiety levels during fitting, Court et al9 found increased anxiety led to disrupted recall of information, poor attention and reduced satisfaction. Practitioners should therefore anticipate anxiety and actively look for signs so that they can consider ways of managing it. Interestingly, anxious patients do not necessarily struggle more with application and removal; if they are highly motivated this helps them to persist and overcome their anxiety and handling difficulties.
Discussing the 'do's and don'ts' of contact lens wear
Ensuring that patients are aware of any risks involved when selling and supplying contact lenses is essential and practitioners should be open and honest with their patients when explaining the risks. The British Contact Lens Association (BCLA) lists common ‘do’s and don’ts’ for contact lens wear on their website10 and key points need to be discussed with all patients. For example, all wearers should know the importance of never using tap water on their lenses. Adding context to this statement by explaining that, although rare, Acanthamoeba keratitis (AK) is a serious corneal infection that can affect contact lens wearers11 is important. Expanding further to explain that Acanthamoeba can be found in UK domestic tap water as well as lakes, oceans, swimming pools and hot tubs will help to fully inform your patient of the risks associated with rinsing lenses with tap water, swimming or showering in lenses.
An understanding of what to do if the lens feels uncomfortable is important. A tiny filament, air bubble or other foreign body can occasionally become trapped under the lens. Carefully sliding the lens onto the white of the eye with a clean finger may sometimes dislodge it, but if discomfort persists explain that the lens will need to be removed, rinsed with saline or a multipurpose cleaning solution and re-applied, checking carefully that it is the correct way round. When summarising advice, the BCLA suggest you get patients to ask themselves three questions every time lenses are worn: Do my eyes feel good with my lenses? Do my eyes look good? Do I see well? If the answer to any of these questions is no, lenses should be removed and the contact lens practitioner contacted for further advice.
Informed consent
Practitioners should be aware of the legislation dictating contact lens fitting in the UK. The General Optical Council (GOC) Contact Lens Rules 198812 states who can fit lenses and states that the teach is considered as part of the initial fitting process. The GOC standards of practice regarding informed consent13 state that you should obtain explicit consent where the procedure, treatment or care being proposed is more invasive and/or has greater risks involved. It is therefore important when teaching a patient to apply and remove contact lenses that you obtain consent and provide your patient with clear and accurate information presented in a way they can understand. You can use your professional judgement to determine the most appropriate way of providing information to a patient; this could be in writing, for example in a leaflet, or by talking to the patient. Many practitioners ask patients to sign a document stating that key points have been covered. The patient can then be given a copy which can also include information on recommended wear schedules, emergency advice, with an out of hours number, and other hints and tips for lens wear.
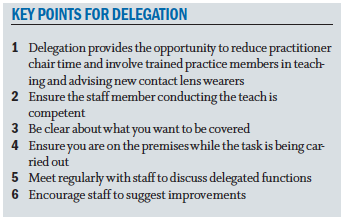
Delegated responsibility
Often optometrists and contact lens opticians choose to delegate the task of teaching a patient to apply and remove their lenses to another member of their practice team. The 2016 GOC Standards of Practice14 gives advice on delegated responsibilities; the person supervising must only delegate to those who have appropriate qualifications, knowledge or skills to perform the delegated activity. The registered professional must be on the premises, so they are able to intervene, if necessary. Details of those being supervised or performing delegated activities must be recorded on the patient record. Professional guidance from the College of Optometrists15 also provides advice on delegation making it clear that when you delegate care, you are still responsible for the overall management of the patient. It is therefore imperative that any person conducting a teach is well trained, ensuring they have the knowledge and skill to instruct a patient safely. To be done well, good communication between staff members is essential and anyone responsible for the teach should understand patient motivation for wear, type and modality of lenses worn, care regimen and recommended wearing times. A check list is useful when delegating responsibility as a way of ensuring everyone follows correct protocols (figure 10).
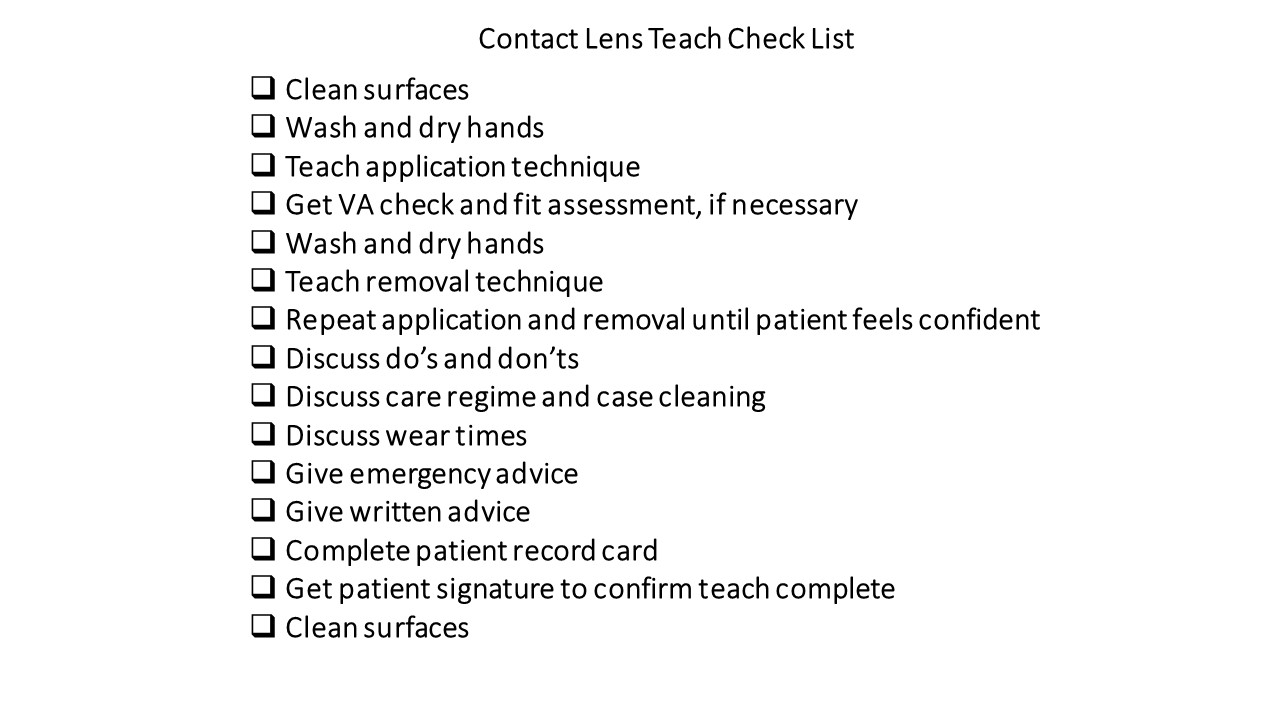 Figure 10: Sample check list for a contact lens teach to ensure protocol is followed
Figure 10: Sample check list for a contact lens teach to ensure protocol is followed
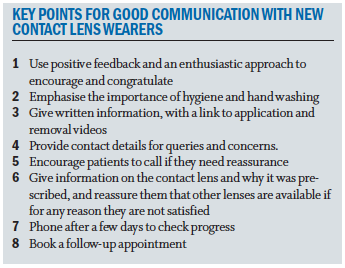
Follow-up
The early stages of contact lens wear are crucial to ongoing success. Many patients need additional support during their trial period to move them from an apprehensive novice wearer to a happy confident wearer as the first few days can be overwhelming. Repeated application and removal failures once the patient is at home may result in frustration and this can increase anxiety. It is clear that lens wearers have issues with handling lenses as these difficulties feature widely in social media chatter.8 This suggests our patients want more advice. If they turn to social media, practitioners have much less control over the advice that is given. Most manufacturers provide online support materials and giving them a link to manufacturer websites or a trusted YouTube video gives you more control over advice they receive at home. Most issues are simple to resolve; encourage the patient to call with any further questions or concerns and ensure they always have your number at hand, either in their phone contacts or using contact card for their wallet.
Consider a follow-up call
In addition to the usual follow-up appointment, a phone or video call from a member of the practice team after a couple of days can be invaluable. Remember, once at home anxiety will often continue and new wearers may find it difficult to recall advice given. Furthermore, patients may find that they need more time than expected to apply and remove lenses successfully. New wearers may consider time needed is too long and so cut corners to try and speed up the process.9 Practitioners should be aware that when a patient leaves the practice with new lenses it is simply the beginning of their journey as a lens wearer and further support at home may be needed to ensure the patient develops into a successful contact lens wearer. A call at this early stage can address difficulties that may have arisen early on and encourage patients to stay motivated. Enthusiastic communication is important remembering to relate back to their initial motivation, praise progress and give personalised advice relevant to their circumstances.
Summary
Learning to wear and care for contact lenses can be an emotional time for patients. The mix of excitement and anxiety can overwhelm at times and all staff delivering this part of the contact lens fitting need to be empathetic and well trained. Practices need a clean, private space to give patients the time needed to learn this new skill. Understanding motivation for contact lens wear and exploring possible concerns and anxieties is essential to personalise the experience ensuring patients leave the practice feeling confident and motivated. Once home it may be difficult for patients to recall advice given or find the time needed to master the new art of applying and removing their lenses. Offering continued support is important to build confidence and ensure the patient stays motivated. Good communication and simple methods for continued support once patients leave the practice can be employed to help reduce drop out in new wearers. •
Louise Munns is an Optometrist, College of Optometrists Examiner and Assessor, Clinical Supervisor at Aston University and a paid consultant faculty member for the Johnson & Johnson Institute, UK. Dr Rachel Hiscox is a Professional Education & Development Manager, UK & Ireland for Johnson & Johnson Vision Care.
- This article is part of a revised and updated ‘Essential Contact Lens Practice’ series, originally authored by Jane Veys, John Meyler and Ian Davies. This article was produced without further input or review from the original authors.
References
- Sulley A, Young G and Hunt C. Factors in the success of new contact lens wearers. CLAE, 2016;40:1 15-24
- Morgan PB, Efron N, Toshida H, Nichols JJ. An international analysis of contact lens compliance. Cont Lens Anterior Eye, 2011;34(5):223-8
- Dart JK, Radford CF, Minassian D, Verma S, Stapleton F. Risk factors for microbial keratitis with contemporary contact lenses: a case-control study. Ophthalmology, 2008;115(10):1647-54
- Stapleton F, Keay L, Jalbert I, Cole N. The epidemiology of contact lens related infiltrates. Optom Vis Sci, 2007;84(4):257-7
- Dantum J, McCanna DJ. Subbaraman LN et al. Performance of contact lens solutions study group. Microbial contamination of contact lens storage cases during daily wear use. OVS, 2016;93(8):925 932
- Houang E, Lam D, Fan D, Seal D. Microbial keratitis in Hong Kong: relationship to climate, environment and contact-lens disinfection. Trans R Soc Trop Med Hyg, 2001;95(4):361-7
- JJVC Data on file 2017. Quest Study. n=508 Quantitative interviews and diaries in Brazil, China, Japan, US
- JJV Data on file 2014. Training Wheels Research. n=1,200 Quantitative interviews in China, Japan, Russia and US with considerers, triallists and dropouts
- Court H, Greenland K and Margrain TH. Evaluating patient anxiety levels during CL fitting. OVS, 2008;85:7 573-80
- BCLA. Important Do’s and Don’ts of Contact Lens Wear. Available at: https://www.bcla.org.uk/Public/Consumer/Important_dos_and_dont_s_of_contact_lens_wear.aspx [Accessed 4th January 2021]
- Carnt N, Hoffman JJ, Verma S, et al. Acanthamoeba keratitis: confirmation of the UK outbreak and a prospective case-control study identifying contributing risk factors, British Journal of Ophthalmology, 2018;102:1621-1628.
- The GOC. The General Optical Council (Contact Lens (Qualifications etc.) Rules) Order of the Council 1988. Available at: http://www.legislation.gov.uk/uksi/1988/1305/made [Accessed 4th January 2021]
- The GOC. The General Optical Council Supplementary Guidance on Consent. Available at: https://www.optical.org/filemanager/root/site_assets/standards/new_standards_documents/supplementary_guidance_on_consent.pdf [Accessed 4th January 2021]
- The GOC. The General Optical Council Standard of Practice for Optometrists and Dispensing Opticians. April 2016. Available at: https://standards.optical.org/wp-content/uploads/2019/10/standards_of_practice_web.pdf [Accessed 4th January 2021]
- The College of Optometrists. Guidance for Professional Practice – Delegation. Available at: https://guidance.college-optometrists.org/guidance-contents/communication-partnership-and-teamwork-domain/working-with-colleagues/delegation/ [Accessed 4th January 2021]
