Eye examinations in community optometric practice are aimed at optimising visual performance through correction of refractive error. Another important purpose of an eye examination is the assessment of visual function and ocular health with the aim of diagnosis and management. Ocular pathology is initially managed by treating the condition to restore or preserve sight. In some cases, however, sight cannot be restored and the patient may experience reduced task performance. Here the
priority in patient management shifts from intervention to treat the condition, to interventions to optimise task performance and participation in society leading to better quality of life. This article explores two models for patient care:
- The Medical Model
- The Social Model
The focus will be upon explaining how these two approaches come together in a low vision (LV) clinic.
Medical Model and Social Model
A health condition can lead to impairment, which results in activity limitation and eventually participation restriction.1
In eye care practice, a patient may initially notice that they can no longer read their paper or that they bump into things, and this impacts upon their participation in and quality of life (QoL). They then consult an eye specialist who diagnoses the condition which is the underlying cause of the impairment of visual function.
In order to address this patient’s concerns regarding reduced participation and QoL, it is important to both consider the impact of treatment options to restore eye sight and to find ways to maximise the patient’s remaining sight and solutions from within the person’s own environment. The first option falls within the Medical Model of patient care, and the latter falls within the Social Model of care. Table 1 provides an overview of interventions that are offered through the Medical Model, the Social Model and the LV clinic.
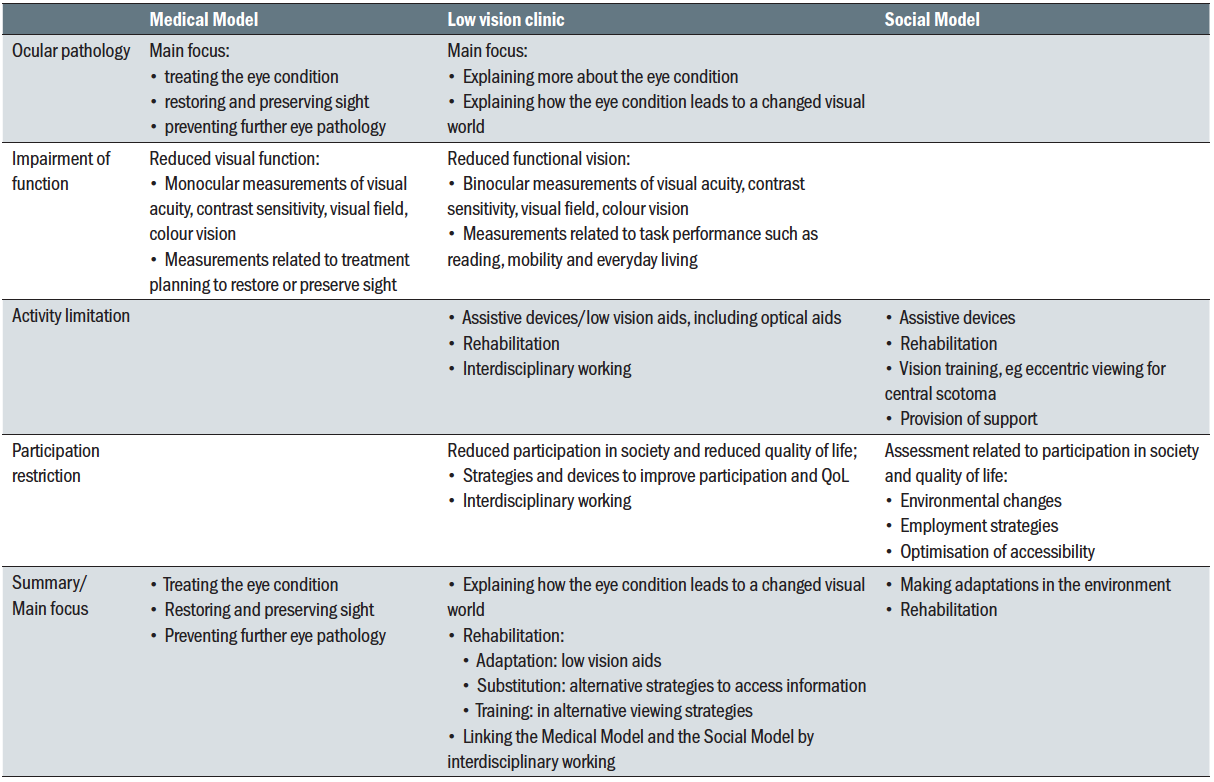 Table 1: Roles and interventions within the Medical Model, the Social Model and the low vision clinic
Table 1: Roles and interventions within the Medical Model, the Social Model and the low vision clinic
Medical Model
In the Medical Model, the focus is on treating eye conditions in order to improve or preserve sight. The emphasis is on restoring vision for those whose vision falls short of the patient’s needs. Solutions to improve vision are sought in order to meet these needs. Visual impairment can inappropriately be viewed as an obstacle to achieving the desired standard,2 which can result in a negative experience for the patient.
During a medical assessment, visual function tests serve to measure a loss of function with the purpose of planning medical interventions. Visual acuity, visual fields, contrast sensitivity, slit-lamp biomicroscopy, ophthalmoscopy, OCT scans and myriad other tests are designed to be carried out monocularly in order to diagnose and treat disorders of each eye separately (figure 1).
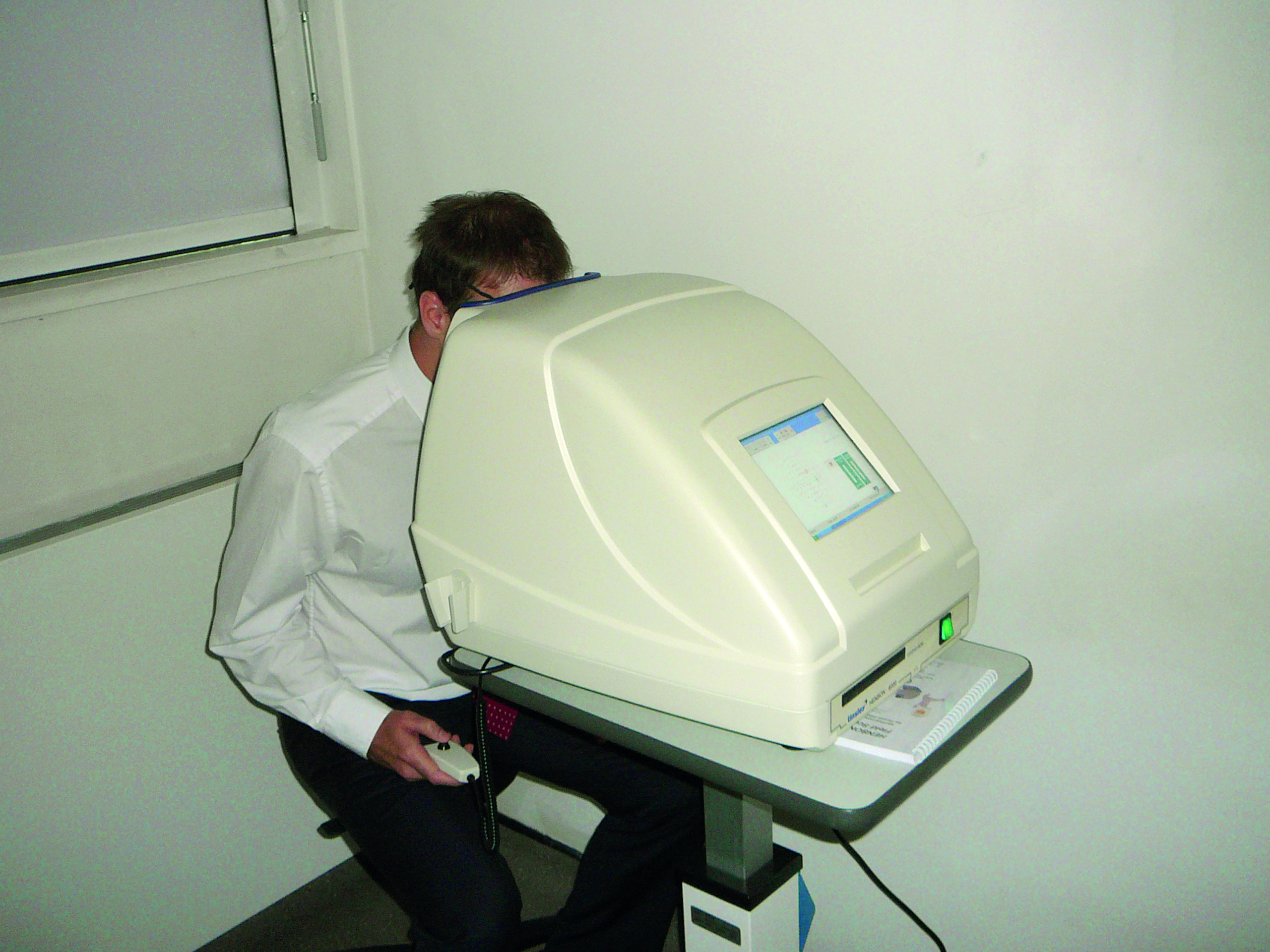 Figure 1: Medical assessment tends towards testing one eye’s visual functioning; the Medical Model
Figure 1: Medical assessment tends towards testing one eye’s visual functioning; the Medical Model
Communication with the patients is primarily focused on diagnosis, treatment options, medical interventions, risk factors and prognosis. When a patient first starts to notice reduced functioning due to sight loss, their main concern is often how their sight can be restored. Sub-normal vision has been found to be an important indicator for reduced health-related QoL.3 Therefore, prevention of sight loss and restoring vision are the first issues to address.
Social Model
However, in some cases, visual impairment is permanent and the focus shifts from aiming for optimal visual function to gaining optimal functional vision. In other words, if eyesight cannot be improved to reach a ‘normal standard’, one needs to focus on how this person with impaired vision can function optimally in their sub-optimal visual world (figure 2).
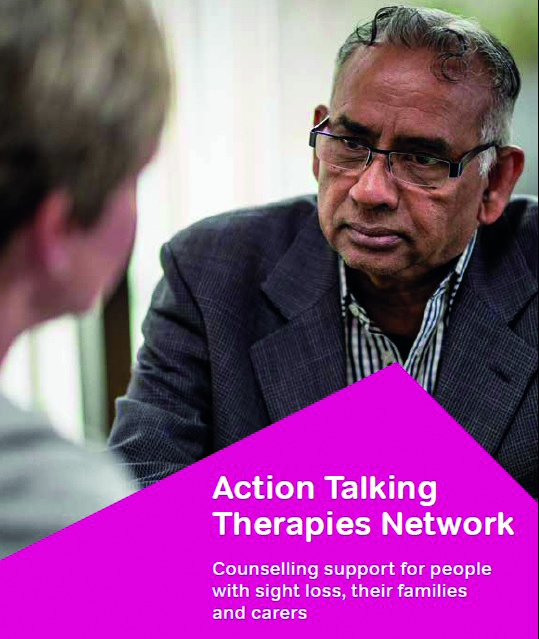 Figure 2: The Social Model is concerned with assessing the patient’s functional vision with a view to advising on its optimum use in everyday life, as for example included in this advice leaflet from the RNIB
Figure 2: The Social Model is concerned with assessing the patient’s functional vision with a view to advising on its optimum use in everyday life, as for example included in this advice leaflet from the RNIB
It is recommended that patients are offered rehabilitation at an early stage, as the need for this service is not dependent on the level of sight impairment,4 but rather on the level of functioning. Disability, which is a term denoting activity limitation, can have a negative connotation for medical students, due to the focus on negative personal attributes and a loss of abilities. This image can change when students receive appropriate training, learning to tune in to positive personal attributes and enablement.5 These are key ingredients for the Social Model.
The Social Model has its roots in the ‘Independent Living Movement’ which emerged in the late 1960s in the United States and the UK.6,7 The movement developed in response to the limitations that the Medical Model had on offer. Importantly, the Social Model is person-centred. Solutions are not sought in improvement of visual function, but in improvement of participation in society and quality of life. It is not the person’s ability that needs to change to adapt to the environment, but the environment that needs to change to best suit the needs of the person. This concept will be explored in a later section of this article.
Low Vision
The Medical Model and the Social Model are integrated in the low vision (LV) clinic. Interdisciplinary working is a key feature for the provision of holistic patient-centred care. Eye care professionals (ECPs) combine their knowledge of ocular conditions and visual processing with their knowledge of optics, low vision aids, assistive devices, rehabilitative strategies and the network of care providers and charities that seek to support patients with a visual impairment. ECPs in a LV service are uniquely placed to understand conditions that lead to sight impairment and to explain how these conditions affect daily functioning.
Ocular pathology
Ophthalmology clinics can be very busy and the primary focus tends to be diagnosing and treating eye conditions to restore or preserve sight. There is often limited time to explain the eye condition, to discuss the impact of the condition on visual function and functional vision and to answer any questions or concerns from the patient. The ECP in a LV service can address any concerns and explain more about a patient’s eye condition and how reduced visual functions lead to reduced functioning owing to impaired visual processing and even visual hallucinations. This information can also be shared with rehabilitation workers or any other professionals dealing with practical issues related to the patient’s sight loss and functioning.
Patients often appreciate it when the LV practitioner writes a summary (in accessible print size) for future reference. Accessible information about charities for the patient’s specific eye condition(s) can be provided in order to empower the patient with up-to-date advice and knowledge concerning recent salient research. It is also possible to provide access to a social network of peers affected by the same condition.
Impairment of function
In the LV clinic, visual function is primarily measured in order to assess requirements for task performance. It is usually first measured with both eyes open and with the habitual prescription. A refraction is indicated if the glasses are not up-to-date. Binocular visual acuity is assessed including an evaluation of how easily and fluently the letters can be read. Reading acuity and speed, contrast sensitivity, visual fields, ocular motility and colour vision assessments provide information about the patient’s visual world and their likely impact on QoL.8-11 This is helpful in terms of explaining to the patients, and to their family and carers, the impact of ocular pathology on functional vision. These measures are also helpful in terms of management. They inform the practitioner about the required magnification and light levels,12 as well as the need for adaptation, substitution and training.13
Activity limitation
Understanding the eye condition and measuring visual function are common ground for ophthalmologists and ECPs working in the low vision specialism. They each consider these aspects from different perspectives. Monocular visual functions are parameters required for diagnosis, management and treatment of conditions. Binocular visual function parameters inform the practitioner primarily about functioning and activity limitation. The Medical Model meets the Social Model when visual function measures are employed to understand how a medical condition impacts a person’s everyday functioning. The practitioner no longer looks at unmet visual standards, but rather focuses on the patient’s needs for successful task performance and participation. In this way, eye-centred care makes room for patient-centred care.
Participation restriction
Participation can be improved in two ways:
- By enabling patients to carry out tasks independently
- By making the environment more accessible
Task performance and optimising the personal environment lie within the realm of the LV practitioner and the rehabilitation worker. Interventions are designed to enable the patient. Social services and policy makers are concerned with providing an accessible environment in public spaces. Interventions are designed to promote equality.
The inability to perform a task only becomes a relevant problem if a patient has an interest in performing this task. It is therefore important to assess the visual requirements and functional requirements for patients and to formulate goals based on these requirements.
Historically, the LV practitioner’s main focus has been to provide optical aids to enable people to read, write and watch TV (figure 3). This is often an important requirement as it increases independence and allows people to access written information. In more recent years, adaptation, substitution and training have become an integral part of LV services. This includes advice about reading strategies and scanning strategies and about the effect of contrast and lighting on task performance as well as the use of other senses to enhance functioning (figure 4).
 Figure 3: Changing approach; historically, a major focus of management was offering magnification
Figure 3: Changing approach; historically, a major focus of management was offering magnification
 Figure 4: Changing approach; a more holistic approach to management is now adopted, and includes adaptations to environment such as advice on lighting
Figure 4: Changing approach; a more holistic approach to management is now adopted, and includes adaptations to environment such as advice on lighting
Interdisciplinary working is essential for the LV practitioner. During the LV assessment, the practitioner maps out what the requirements are for a patient to optimise participation and QoL. Some requirements are managed within the LV clinic. Other requirements are managed by other care providers and charities. Many hospitals have Eye Clinic Liaison Officers (ECLOs) who can act as a bridge between the LV clinic and the eye department at the one hand, and services outside the hospital service at the other hand. The LV practitioner can also refer patients directly to other care providers and charities and provide information and advice. Let us now consider some examples of how participation and functioning can be enhanced.
Adaptations, sight substitution and training
Adaptations, sight substitution and training are all employed to optimise functioning in an individual’s personal environment. Each individual patient has unique visual needs and challenges and the LV practitioner can identify appropriate solutions with the patient. It is essential to fully understand the patient’s visual world in order to enable the patient and their family or carers to make suitable adjustments. The home environment can be adapted to make the visual scene more accessible by introducing contrast and lighting and by reducing clutter (figure 5). The use of appropriate LV aids and electronic devices can improve task performance. One can also use sight substitution by introducing tactile stickers on appliances and adaptive kitchen utensils to support independent living (figure 6). Large and bold note books, games and toys can improve participation. Audio and e-books and newspapers can replace conventional format versions (figure 7). Training in scanning strategies and reading strategies can enable the patient to function optimally.
 Figure 5: Contrast here is good, but too much clutter may reduce its impact
Figure 5: Contrast here is good, but too much clutter may reduce its impact  Figure 6: Tactile stickers
Figure 6: Tactile stickers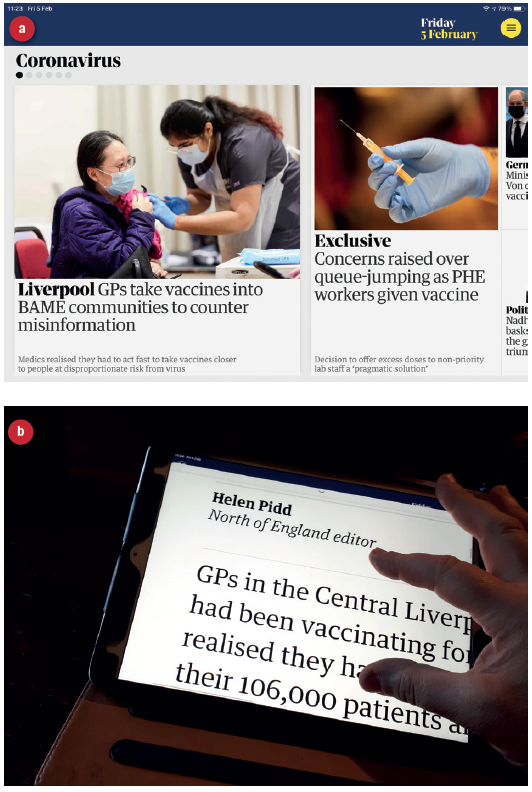 Figure 7: Online newspapers, such as the Guardian Daily Edition (a), allow simple magnification on-screen (b)
Figure 7: Online newspapers, such as the Guardian Daily Edition (a), allow simple magnification on-screen (b)
Mobility and way finding
Visual impairment often leads to decreased confidence in way finding and mobility with an increased risk of falling.14-17 LV practitioners can refer patients for mobility training and it can be helpful if the referral includes an explanation about the impact of visual function on mobility. For example, it is useful to have information about visual field and visual attention as well as contrast sensitivity and acuity as the mobility training can be much more focused on the specific requirements.
In some cases, the use of a monocular can be helpful in terms of reading street names and looking at traffic signs for example. The use of a symbol cane is well established as it alerts other road users of the visual impairment. For those who require tactile guidance, a variety of white canes can be considered.18 With the increase of technology, the options for navigating to new places have increased. Auditory navigation systems have been available for some time and tactile navigation systems are being introduced as well. These include hip-worn belts with turn-signals via vibrations19 and three-dimensional tactile maps to improve memorisation of routes and way finding.20
Road designs
Roads can be made more accessible for VI users when the needs of these users are understood. A study in Mexico indicated that people with severe sight impairment (SSI) use differences in ground level and surface, noise and smells for wayfinding.21 The majority of patients reported feeling unsafe in busy environments and road crossing. There is potential for improving the environment by using tactile guidance, olfactory and auditory signposting and street designs. Adaptations such as tactile paving (figure 8), spinning cones and audible signals at traffic lights are implemented in some areas and it is important to make patients aware of these features.
 Figure 8: Tactile paving
Figure 8: Tactile paving
Public buildings and indoor spaces
Buildings and public spaces are made accessible by introducing railings, floor markings and tactile paving to move through the space. Lifts can be made accessible with Braille buttons, large and bold buttons and speech announcements. Notice boards and signposting can be provided in large and bold print and Braille. Some museums, cinemas and theatres offer a variety of services to enhance the experience for VI users, such as audio tours, audio description, touch tours and pre-show notes.22
Conclusion
In summary, eye conditions that lead to visual impairment need to be managed in different ways. Initially, an eye examination is essential to diagnose and treat conditions with a view to restore or preserve sight. This essential follows a Medical Model of management.
If there is irreversible visual loss, a functional assessment is indicated, with a view to support patients at different levels. Firstly, support is offered in terms of understanding the ocular or medical condition. Secondly, optical aids are provided to improve task performance. Thirdly, adaptation, substitution and training are explored during the consultation and in the form of interdisciplinary working. And finally, the LV practitioner can identify patients who are eligible for visual impairment registration. This approach is more akin to a Social Model of care, and is essential for the immediate benefit for the patient as well as for the benefit for the society as a whole as changes in the environment are driven by sight loss statistics.
In recent months, with an increased focus on remote teleconsultation (figure 9), triaging and dispersing information about general health and well-being matters, all ECPs have had increased experience in developing a Social Model approach to patient management outside the low vision clinic environment.
 Figure 9: Teleconsultation commonly leans towards a Social Model approach to management
Figure 9: Teleconsultation commonly leans towards a Social Model approach to management
Cirta Tooth is a low vision specialist practising in Scotland with a special interest in people with sensory and learning impairment.
References
- WHO (2002). World Health Organisation. Towards a common language for functioning, disability and health ICF. Available at: www.who.int/classifications/icf/icfbeginnersguide.pdf [Accessed 17 December 2020]
- Porkertova H. (2020). ‘Almost equal’: Confronting norms and normality in experiencing vis-ual disability. Critical Sociology. http//doi:10.1177/0896920520945364
- Taipale J, Mikhailova A, Ojamo M et al. (2019). Low vision status and declining vision de-crease Health-related Quality of Life: results from a nationwide 11-year follow-up study. Quality of Life Research 28(12), pp.3225-3236
- MacNaughton J, Latham K en Vianya-Estopa M. (2019). Rehabilitation needs and activity limitations of adults with visual impairment entering a low vision rehabilitation service in England. Ophthalmic and Physiological Optics 39(2), pp.113-126
- Byron M, Cockshott Z, Brownett H et al. (2005). What does ‘disability’ mean for medical students? An exploration of the words medical students associate with the term ‘disability’. Medical Education 39(2), pp.176-183
- Gomez Bernal V. (2016). The organized disability: precedents and trajectories of move-ment of persons with disability. Historia Actual Online 39, pp.39-52
- Illich I. 1976. Limits to medicine—medical nemesis: the expropriation of health. 1st Edition. London. Marion Boyars
- Havstam Johansson L, Škiljić D, Falk Erhag H, Ahlner F, Pernheim C, Rydberg Sterner T, Wetterberg H, Skoog I, Zetterberg M. Vision-related quality of life and visual function in a 70-year-old Swedish population. Acta Ophthalmol. 2020 Jan 7. doi: 10.1111/aos.14341.
- Pondorfer SG, Terheyden JH, Heinemann M et al. (2019). Association of vision-related qual-ity of life with visual function in age-related macular degeneration. Scientific Reports 9. Article Number 15326
- Szlyk JP, Seiple W, Fishman GA et al. (2001). Perceived and actual performance of daily tasks: relationship to visual function tests in individuals with retinitis pigmentosa. Ophthalmology 108(1), pp.65-75
- Taipale J, Mikhailova A, Ojamo M et al. (2019). Low vision status and declining vision de-crease Health-related Quality of Life: results from a nationwide 11-year follow-up study. Quality of Life Research 28(12), pp.3225-3236
- Harvey W. Low Vision Refresher. Optician, 16 February 2018.
- Macle S. Low Vision Refresher – support services. Optician, 10 August 2018
- Duggan E, Donoghue O, Kenny RA et al. (2017). Time to refocus assessment of vision in older adults? Contrast sensitivity but not visual acuity is associated with gait in older adults. Journals of Gerontology Series A-Biological Sciences and Medical Sciences 72(12),pp.1663-1668
- Jian-Yu E, Mihailovic A, Kuo P et al. (2020). Characterizing the impact of fear of falling on activity and falls in older adults with glaucoma. Journal of the American Geriatrics Society 68(8), pp.1847-1851
- Mihailovic A, Swenor BK, Friedman DS et al. (2017). Gait implications of visual field dam-age from glaucoma. Translational Vision Science and Technology 6(3). Article Number 23
- Subhi H, Latham K, Myint J et al. (2017). Functional visual fields: relationship of visual field areas to self-reported function. Ophthalmic and Physiological Optics 37(4), pp.399-408
- RNIB (2020). Royal National Institute of Blind People. The cane explained. Available at: https://www.rnib.org.uk/cane-explained [Accessed 17 December 2020]
- Bharadwaj A, Shaw SB and Goldreich D. (2019). Comparing tactile to auditory guidance for blind individuals. Frontiers in Human Neuroscience 13. Article Number 443
- Toyoda W, Tani E, Oouchi S et al. (2020). Effects of environmental explanation using three-dimensional tactile maps for orientation and mobility training. Applied Ergonomics 88. Ar-ticle Number 103177
- Rey-Galindo JA, Rizo-Corona L, Luz Gonzalez-Munoz E et al. (2020). Environmental infor-mation for people with visual impairment in Mexico or what they need and how they use it. Applied Ergonomics 85. Article Number 103079
- Ferziger N, Dror YF, Gruber L et al. (2020). Audio description in the theater: assessment of satisfaction and quality of the experience among individuals with visual impairment. British Journal of Visual Impairment 38(3), pp.299-311
