In the first quarter of 2020, routine clinical eye care underwent a temporary cessation in most regions around the world due to the coronavirus pandemic. Optometric practice is now predominantly back up and running, albeit with the occasional return to a higher alert level as the infection rates in countries ebb and flow over time. The demands of working in a world with Covid-19 have necessitated changes to how routine practice is conducted. As a result, the attitudes and needs of eye care practitioners (ECPs) and patients related to eye care in general, and contact lenses (CLs) in particular, may have altered. Within this new shape of optometric practice, the question of where CL practice fits naturally arises. While aftercare for the routine assessment and resupply of existing wearers may seem acceptable, how does the profession approach the option of new fits and upgrades? Given the wider challenges faced by practitioners, is this really the time to focus on such areas? Is it even ‘safe’ to fit CL now, given the close contact required? However, looking at it from a different point of view, are there in fact opportunities arising from the changes dictated by Covid-19 that could be beneficial for CL practice? This article reviews the recommendations for safe CL practice, looks at their relevance for both practitioners and patients, and addresses how CL can be accommodated into the daily clinic routine as easily as possible.
Clinical practice in the face of Covid-19
It is likely the majority of ECPs have already made the transition back into routine clinical practice, embracing the necessary health and safety guidelines that have been shared widely by health authorities1,2 and professional bodies3-7 at international and national levels. These recommendations are designed to keep both patients and staff as safe as possible, aiming to reduce potential contact and spread of the virus that causes Covid-19; namely, severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). The virus spreads predominantly via person-to-person contact through respiratory droplets produced when an infected person coughs or sneezes.8,9 The outer lipid envelope of the virus is vulnerable to contact with the surfactants found in simple soap,10 which is known to destroy the virus completely.8,11 Where hand washing is unavailable, alcohol-based hand sanitisers, used in sufficient volume, as well as alcohol concentration, and covering the whole hand should also be effective.12 Given the understanding of how SARS-CoV-2 spreads, and how it can be destroyed, recommendations to limit transmission include physical distancing, wearing a face mask, adequate ventilation, avoiding crowded places, and regular and scrupulous hand hygiene with soap and water.11 This advice has permeated the everyday lives of people around the world and it is the advice on which safe practice guidelines are founded.
A further consideration specific to the eye care profession is the question of whether or not Covid-19 can be transmitted via an ocular route. This topic has been the subject of a number of published reviews,10,13-16 studies17-25 and case reports.26-32 These publications have reported on the detection of SARS-CoV-2 on the ocular surface, viral conjunctivitis connected to confirmed Covid-19 cases, and the likelihood of the eye being a pathway by which a person could either be infected or infect others. While outside of the scope of this piece, these questions were recently addressed in an Optician article on return to CL practice.33 That article concluded a review of the available evidence (at that time) indicated the average incidence for detection of the virus on the ocular surface of patients with Covid-19 is 3%, and, for studies with up to 1,100 subjects, the average incidence of conjunctivitis is 2.5%.33 One large UK based observational study was noted as reporting a much lower incidence of conjunctivitis, with just 0.34% of 13,680 Covid-19 patients exhibiting this complication.34 The general conclusion from the review paper by Willcox and colleagues was also stated in the article: ‘While precautions by eye care practitioners and patients remain necessary, the virus appears thus far unlikely to bind to the ocular surface to initiate infection, as SARS-CoV-2 has been found rarely in tears, and then predominantly only in confirmed, symptomatic patients.’10
Putting all of the information together with the safety recommendations, what has this meant for how routine eye care is conducted? The measures necessary to practice as safely as possible in optometry and ophthalmology settings have been highlighted in recent publications.33,35-38 Those measures fall into a number of areas and start with all patients and staff being screened for symptoms and risk factors prior to arriving in the practice (table 1). It has been suggested that history and symptoms can be conducted via telephone or video communication prior to the appointment to help reduce contact time on site.39 Changes in practice include limiting the number of people in the practice, physically distancing as much as possible, reducing waiting times, removing shared items such as waiting room magazines, thorough and regular disinfecting protocols, and the addition of physical barriers in the form of transparent plastic shields.35
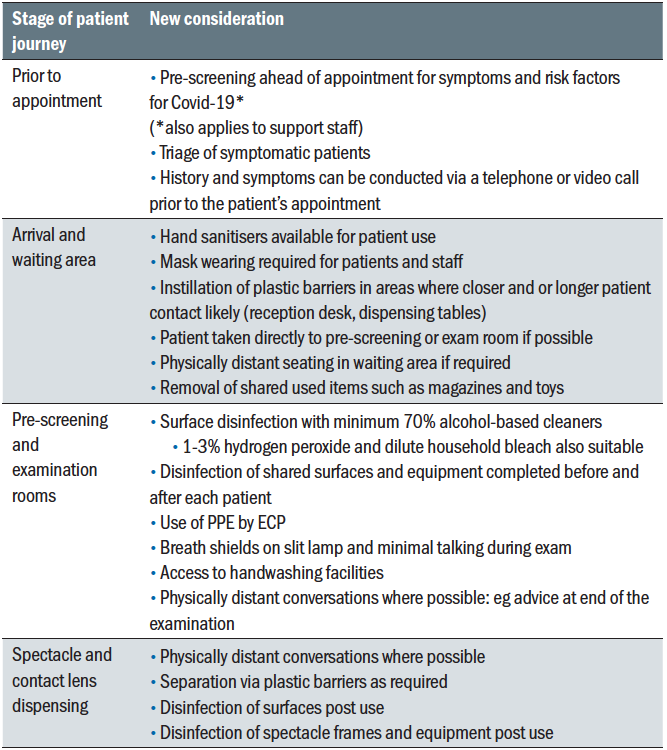 Table 1: Changes required to practice during the coronavirus pandemic
Table 1: Changes required to practice during the coronavirus pandemic
In the pre-screening and examination areas, thorough disinfection of all shared surfaces with alcohol-based cleaners should be carried out before and after each patient. Breath shields are recommended to be installed on the slit lamp. The use of personal protective equipment (PPE) is necessary. Patients should wear face masks throughout their time in the practice, as should all support staff. ECPs and any other staff who are required to be in close contact with patients are typically advised to take some extra measures, including the use of protective eye wear or face shields in addition to face masks.35 The advice on use of gloves is equivocal. There are occasions where the ECP may need to touch the patient’s eye, yet there is no evidence to suggest using gloves makes this a safer interaction. Thorough hand washing with soap and water is enough to destroy the virus and can be conducted before and after any patient contact. Gloves, if used, have to be donned and removed correctly.40 Care should be taken because they can provide a false sense of security, while inadvertently acting as a vector in the transfer of pathogens. That said, the advice of the British Contact Lens Association (BCLA) also points out that patients may expect to see their ECP wearing gloves, providing from the patient’s point of view, what they may feel is a visible reassurance of safety measures being applied.41
The sum total of the precautions necessary for routine practice may result in fewer patients being seen per day due to the extra time taken to clean and disinfect between patients. It is also true that the level of precautions recommended, and the balance between emergency, essential and routine eye care practice will naturally alter in response to local recommendations, based on the numbers of cases and deaths present in each location. An example of this is the UK’s tiered colour coded system that different advice on conducting eye examinations depending on whether practices are in an area of red, orange or green level of alert.42
The experience of existing contact lens wearers
Just as clinical practice has undergone significant changes, so have patient’s lives. Periods of lockdown, where leaving home is limited to essential grocery shopping and healthcare needs, understandably alter the habits of CL wearers. In surveys conducted in the UK, Spain, France, Germany, Italy, Australia and South Korea, reduced CL use during lockdown was reported by 43 to 72% of wearers.43-46 The primary reason given for the
change in wearing frequency was ‘decreased need’ while being at home.43-45 In Spain in particular, there was a correlation between the 46% who temporarily discontinued lens wear, with an increase in concern about CL-related infection.44 While an extensive literature review concluded lens wear does not pose an increased risk of contracting Covid-19,47 it is clearly important for ECPs to ensure their patients hear this. Simple information for patients that reassures them about lens wear, while also reminding them of the importance of practicing good hygiene and compliant behaviours is available in a number of languages at CovidEyeFacts.org.
Although overall use of lenses reduced during lockdown, an increase in occasional wear from 29% to 62% was reported by Spanish lens wearers,44 indicating an opportunity exists for ECPs to introduce the flexible benefits of daily disposable lenses to more patients. An intention to increase lens wear once lockdown ceased was consistently reported, with 93% and 78% of Spanish wearers who had ceased wear wishing to resume lens wear post the pandemic, or post lockdown respectively.44 Reduced use of lenses was predicted to return to normal wear times by 90% of wearers within two to three months post lockdown, and three- quarters of those surveyed were open to discussing upgrading their lenses.46
These data are reassuring. Patients still wish to wear CL, even being open to discussing options that may deliver additional benefits. It is also reassuring to see an increase in some aspects of patient compliance, with nearly 80% of CL wearers saying they are conducting more diligent behaviours such as replacing lenses more frequently, and frequent handwashing using soap and water.45,46
It appears then that the ECP has a number of opportunities with existing wearers, summarised in an infographic (figure 1). First, to reassure them about the safety of lens wear when compliant habits are used, and then to remind them of what those compliant steps are. Next, to check in with the patient on their frequency of use, possibly recommending the convenience of daily disposable lenses if they are seeking flexible wear and not already using that modality. Finally, it is important to ask about lens comfort. The additional time spent living and working from home has increased use of digital devices by around one hour extra a day, with a focus on communication and entertainment use.48 This higher level of use is expected to remain as people continue to work from home, along with relying on their devices for practicalities such as online grocery shopping.46,49 In parallel with increased device use, 41% of lens wearers have reported increased awareness of dry eyes since the start of the pandemic when completing these tasks.46 In addition to the ECP checking and managing any issues on the ocular surface, and advising on ways to minimise digital eye strain, this also presents an opportunity for lens wearers to try new material technology or replacement frequencies, like daily disposables that may help improve their CL comfort.
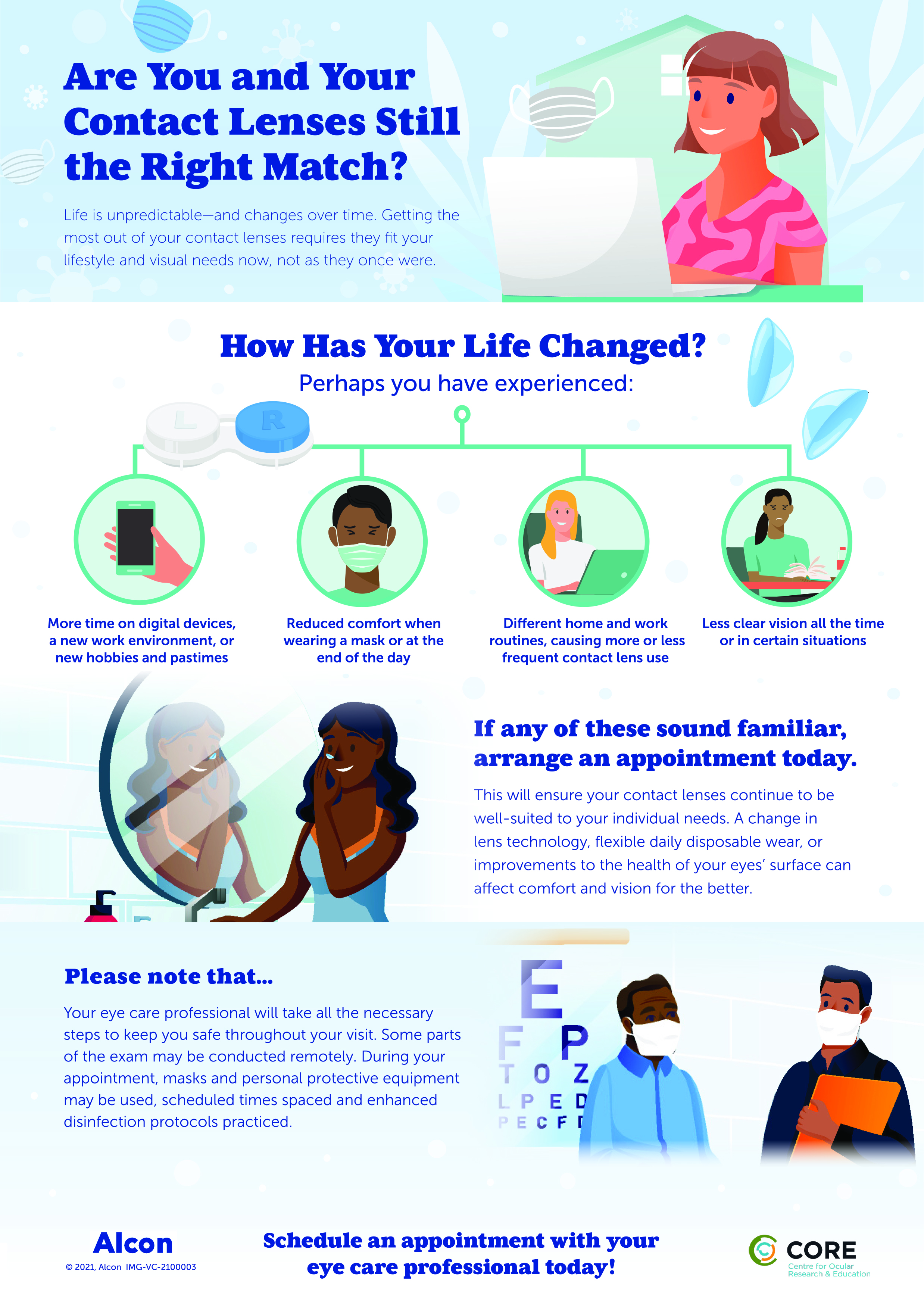 Figure 1: Considerations for existing contact lens wearers
Figure 1: Considerations for existing contact lens wearers
Relevance of contact lenses to spectacle only wearers
Almost every aspect of people’s lives have been touched and changed by the pandemic. The environment in which people live and work may be substantially different. Leisure time has altered; changes may exist with the choice of hobbies and physical activity people pursue. For spectacle only wearers, awareness of the patient’s current situation can present opportunities for which CL may be beneficial. Perhaps the patient in the chair has taken up running or attending a gym more frequently and would prefer to wear CL rather than spectacles; perhaps they would appreciate the flexibility of creating a different appearance on their likely numerous video calls. Maybe their own personal situation has returned to something close to normal and they would consider CL for the more typical reasons of improved confidence, unrestricted vision and social or sporting activities. It remains important to include the option of CL, given via a professional recommendation, to every suitable patient seen for a routine eye examination.
In addition, there is one pandemic-specific situation where CL have a true advantage: avoiding the fogging of spectacle lenses that occurs when they are worn with a mask. Exhaled air escapes out of the top of the mask, forms as condensation on the spectacle lenses and significantly interferes with vision. Front line workers wearing PPE are all too familiar with this issue, with some choosing to switch to CL to help avoid fogging altogether. As mask-wearing mandates have increased around the world, the general public has also encountered this frustrating problem. The ECP is well placed to give advice on correct mask fitting to help reduce the flow of air out of the top of the mask, along with the use of anti-fogging wipes and sprays for spectacles. Where measures taken to alleviate spectacle fogging are simply not enough, and where people have to wear masks for long periods in the day, then CL are an important option to suggest as an alternative. Patient benefits of CL in general, with some specific Covid-19 related reasons, are shown in figure 2.
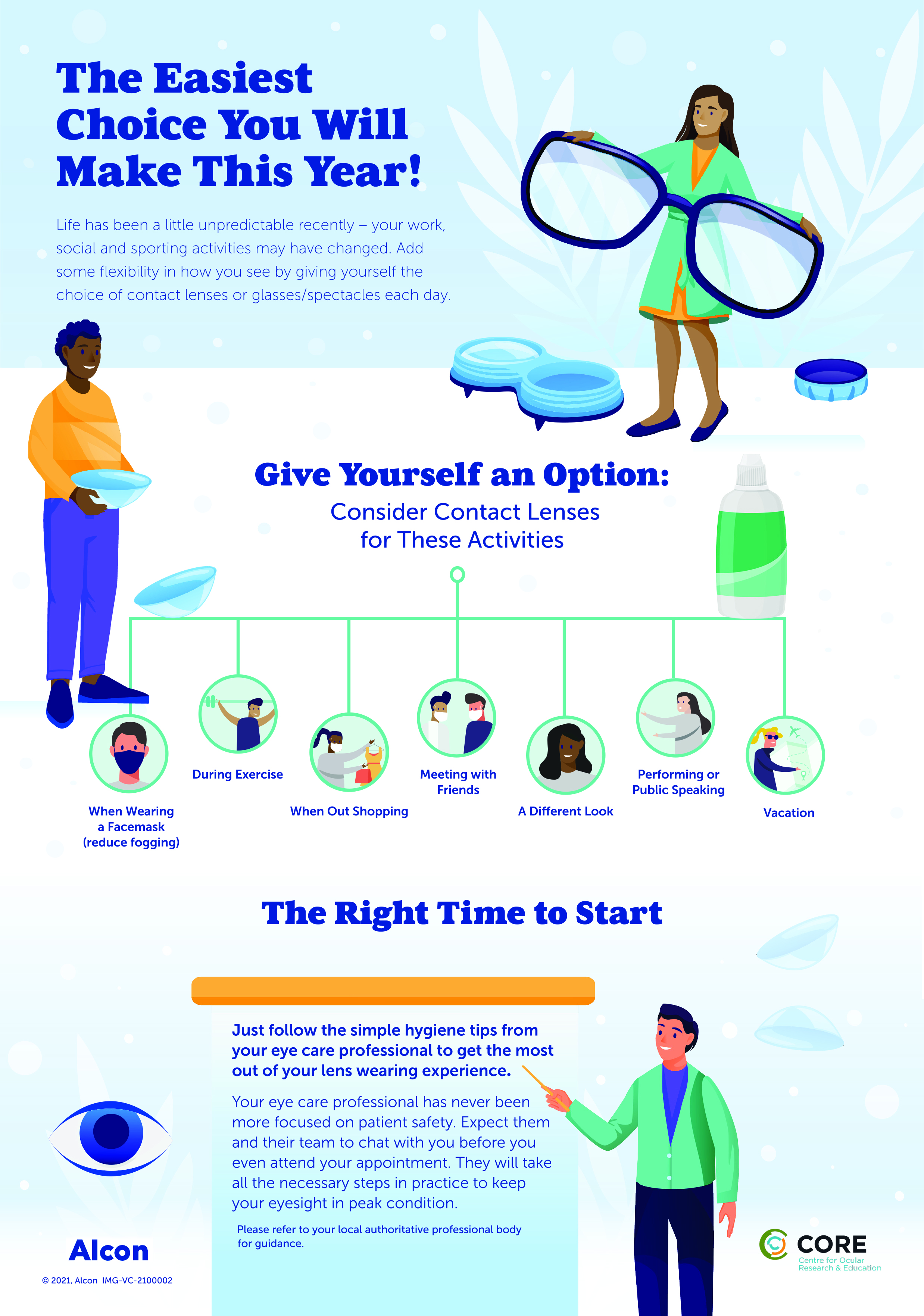 Figure 2: Information for spectacle wearers
Figure 2: Information for spectacle wearers
Reducing air flow over the ocular surface is also important to help minimise the risk of mask-associated dry eye (MADE) occurring too.50 Repeated flow of exhaled air over the surface of the eye causes increased evaporation of the tear film, resulting in increased symptoms of dry eye being reported. A well-fitting mask, breaks from drying tasks such as prolonged digital device use, and the use of lubricating drops can all help reduce this issue; advice that is summarised for patients in multiple languages at CovidEyeFacts.org.
Practice benefits
It is clear that these are challenging times for practice and business owners. A period of closure to all but emergency care, followed by reduced numbers of patients per day once reopened, and a need to catch up on overdue routine eye health checks for patients with chronic conditions all impact practice revenue. These priorities made it logical for ECPs initially to focus on the twin aims of providing essential community eye care and spectacle sales as a way of getting back to normal and on target financially. CL practice, particularly upgrading patients to new technologies and fitting neophytes, may have seemed superfluous to these immediate aims. However, the benefits of using CL when selecting new spectacles have been demonstrated in two studies.51,52 Introducing a CL experience to enable patients to more easily see themselves when choosing frames increases the value of the spectacle dispense, increases the number of CL trials and new wearers, and increases patient satisfaction.51,52 With the need for lower footfall in practice during the pandemic, perhaps now is the time to consider using that time with the patient to double-up on both spectacle and lens wearing recommendations. CL wearers help to increase practice revenue, provide cross-selling opportunities for add-ons such as sunglasses and can develop loyal patients who recommend the practice to others.53 These known business benefits are arguably more relevant than ever as business owners look to recoup lost revenue from periods of lockdown. It is also worth recognising that the need for the current safety measures adopted in clinical practice are unlikely to stop soon. This makes it all the more important to adapt fully to the new way of working, ensuring that all routine services, including new CL fits, continue to be offered to patients.
Keep it simple
Given the proven benefits of CL to patients and ECPs, the question remains how best to add upgrades and new fits into a clinical practice routine that now includes necessary distancing, cleaning and minimal contact protocols. How can the patient experience be maximised while keeping things as simple as possible in an already busy and complex day?`
A typical patient journey is outlined in figure 3 with key points highlighted to help achieve those aims. The first tip starts off-site, with a remote history and symptoms taking. Existing wearers can be asked about their lens comfort and wearing habits. This may reveal options to upgrade and/or to try daily disposables to enable more flexible wear schedules. Should this be highlighted, any trial lenses not available in practice could be ordered in ahead of the appointment. Spectacle only wearers can be asked about situations where they may find their spectacles inconvenient, especially in relation to the wearing of masks or other PPE. The option of CL could be mentioned at this point, with the caveat that the ECP will assess them for suitability and make a professional recommendation during the eye examination.
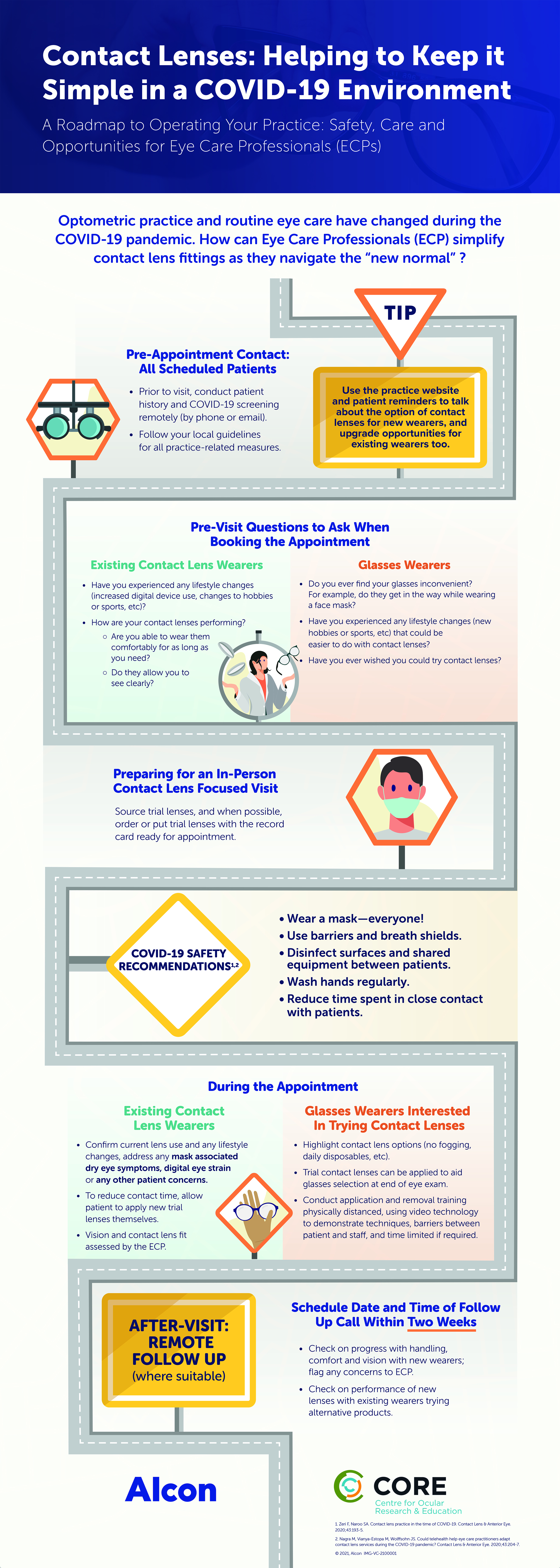 Figure 3: Simplified new or existing contact lens patient journey working with Covid-19 safety measures
Figure 3: Simplified new or existing contact lens patient journey working with Covid-19 safety measures
Much of CL practice is no different to conducting routine eye examinations. Use of appropriate disinfection between patients, breath shields, PPE for the ECP, masks for the patient and minimal talking at the slit lamp should limit potential risk. For existing wearers, following assessment of vision, lens fit and anterior eye health, options for changes to material and/or replacement frequency can be discussed. An existing wearer can apply any new trial lenses themselves and following one further acuity check and slit lamp assessment continue with the trial at home. Follow up can be prearranged, with a booked call from a member of the support staff, from which lenses could be ordered and sent to the patient.
Applying a trial lens to a new wearer realistically requires contact with the patient’s ocular adnexa for a short period of time. This can be conducted either with thorough hand washing before and immediately after lens application; or with clean, tight-fitting gloves that are removed and discarded after coming into contact with the patient. For the relatively few trial and diagnostic lenses that need to be reused, clear guidelines exist on the correct steps required for the safe disinfection of both rigid and soft materials. Initial disinfection of both material types involves a minimum three-hour soak in un-neutralised hydrogen peroxide. The hydrogen peroxide soak is typically conducted in a standard flat CL case. This is necessary to prevent the usual neutralisation process that would occur with the presence of a platinum disc catalyst, and is also often necessary to accommodate the larger diameter of scleral trial lenses. Rigid corneal and scleral lenses are then rinsed and stored dry according to guidelines; soft contact lenses go through the regular disinfection procedure with a hydrogen peroxide system in its usual case, followed by rinsing and storing in multipurpose solution. Based on international standards and endorsed by the American Optometric Association and the American Academy of Optometry the full guidelines, which are no different to before Covid-19, can be accessed in a free factsheet available from Contact Lens Update. Due to vCJD, the use of sodium hypochlorite to sterilise reusable rigid fitting lenses is recommended in the UK.
Following assessment of lens fit and vision, the neophyte patient needs to be taught how to apply and remove the lenses themselves. It is this step in the process of a new fit that likely results in spending the longest time with the patient. To reduce contact time, the patient can be instructed to review videos and information about the application and removal and wear and care of CL at home, ahead of their appointment. That said, a patient may wish to have experienced the lens on their eye first, helping to overcome the unknown of how the lens will feel when worn prior to watching the detail of lens handling. Access to instructional videos and self-guided learning can be provided in practice too, enabling support staff to observe from an acceptable physical distance, stepping in only when required. Examples of videos can be found via many professional organisations and CL manufacturer’s websites. The initial trial lenses can be left in, with removal being the first technique that is taught. To reduce risk in practice when in closer contact, barriers can be constructed between the patient and staff member (figure 4). If total time spent in practice or close to staff is a concern then consider booking the patient back in for a follow up teaching session, having them practice techniques and ‘lid holds’ at home before the next appointment.
 Figure 4: Example of barrier between staff and patient for application and removal training
Figure 4: Example of barrier between staff and patient for application and removal training
A final point relevant for new fits is the need to see the patient again in a relatively short space of time. New wearers benefit from early follow up, without which potential concerns with handling, vision or comfort can all result in significant numbers dropping out within the first three months of wear.54,55 The opportunity exists to move what may traditionally have been done as a follow up appointment to a phone call or video consultation. Trained staff members could carry this out initially, with the ECP following up if any specific concerns are highlighted.
In practices where specialist CL fitting is offered there are also options to help reduce the time spent with the patient in practice. Increasingly it is possible to make use of empirical fitting, with patient details, refraction and topography sent to the manufacturer. The resulting lens will need to be assessed on eye of course, but subsequent follow up can be conducted remotely.
Conclusion
The year 2020, the so-called ‘year of vision’, took an unprecedented turn and ended with clinical care looking quite different to the previous ‘normal’. Mask wearing is common, physical distancing is necessary, and stringent disinfection and hygiene protocols have to be followed. Focusing on CL practice in this new way of working may seem both daunting and not a top priority. However, the need for patients to have choice in their vision correction remains. Patient’s lives may have changed, with new living and working practices potentially creating the opportunity for CL to be recommended. They may just make the difference to a patient’s confidence at work, be helpful for a new sporting activity, or eliminate spectacle fogging issues with PPE. The needs of existing wearers are important to address too, to ensure their lenses are performing optimally, offering alternative materials and modalities if they are not. Integrating use of telehealth calls pre- and post- CL appointments, having trial lenses ready for use, and adding CL experiences to spectacle frame selection are all simple ways to ensure the needs of patients continue to be met as best as possible. •
Professor Lyndon Jones is Director of the Centre for Ocular Research & Education (CORE) at the University of Waterloo. Karen Walsh is Education Team Leader and Clinical Scientist at CORE.
References
- Center for Disease Prevention and Control (CDC) Information for Healthcare Professionals about Covid-19. 2020 [updated 2020. Available at: https://www.cdc.gov/coronavirus/2019-nCoV/hcp/index.html. Accessed: 05 Nov 2020]
- World Health Organisation (WHO) Coronavirus. 2020 [updated 2020. Available at: https://www.who.int/health-topics/coronavirus#tab=tab_1. Accessed: 05 Nov 2020];
- The College of Optometrists Covid-19: Updates, guidance, information and resources. 2020 [updated 2020. Available at: https://www.college-optometrists.org/guidance/covid-19-coronavirus-guidance- information.html. Accessed: 05 Nov 2020]
- BCLA Contact Lens Wear and Coronavirus (Covid-19) Guidance. 2020 [updated 2020. Available at: https://www.bcla.org.uk/Public/Consumer/Contact-Lens-Wear-and-Coronavirus- guidance.aspx?hkey=a6920621-8aa9-4488-8316-84421baee4c0&WebsiteKey=cfa0aa8b-7f48-4d52- 8deb-0eeaab6928d8. Accessed: 05 Nov 2020];
- Euromcontact CONTACT LENS PRACTICE DURING Covid-19 : Recommended Considerations. 2020 [updated 2020. Available at: https://euromcontact.org/2020/05/08/recommended-considerations/. Accessed: 05 Nov 2020];
- American Academy of Optometry Covid-19 Hub. 2020 [updated 2020. Available at: https://www.aaopt.org/my-covid-hub. Accessed: 05 Nov 2020];
- American Optometric Association Covid-19 latest updates. 2020 [updated 2020. Available at: https://www.aoa.org/covid-19/covid-19-latest-updates?sso=y. Accessed: 05 Nov 2020];
- Wu D, Wu T, Liu Q, et al. The SARS-CoV-2 outbreak: What we know. Int J Infect Dis 2020;94:44-8.
- Habibzadeh P, Stoneman EK. The Novel Coronavirus: A Bird’s Eye View. The international journal of occupational and environmental medicine 2020;11:65-71.
- Willcox MD, Walsh K, Nichols JJ, et al. The ocular surface, coronaviruses and Covid-19. Clinical & experimental optometry 2020.
- World Health Organization Coronavirus disease (Covid-19) advice for the public. [Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public. Accessed: 28 Oct 2020];
- Golin AP, Choi D, Ghahary A. Hand sanitizers: A review of ingredients, mechanisms of action, modes of delivery, and efficacy against coronaviruses. American journal of infection control 2020;48:1062-7.
- Cheong KX. Systematic Review of Ocular Involvement of SARS-CoV-2 in Coronavirus Disease 2019. Curr Ophthalmol Rep 2020:1-10.
- Güemes-Villahoz N, Burgos-Blasco B, Vidal-Villegas B, et al. Novel Insights into the Transmission of SARS-CoV-2 Through the Ocular Surface and its Detection in Tears and Conjunctival Secretions: A Review. Advances in therapy 2020;37:4086-95.
- Aiello F, Gallo Afflitto G, Mancino R, et al. Coronavirus disease 2019 (SARS-CoV-2) and colonization of ocular tissues and secretions: a systematic review. Eye (Lond) 2020;34:1206-11.
- Lawrenson JG, Buckley RJ. Covid-19 and the eye. Ophthalmic and Physiological Optics 2020;40:383- 8.
- Guemes-Villahoz N, Burgos-Blasco B, Arribi-Vilela A, et al. SARS-CoV-2 RNA detection in tears and conjunctival secretions of Covid-19 patients with conjunctivitis. J Infect 2020;81:452-82.
- Karimi S, Arabi A, Shahraki T, et al. Detection of severe acute respiratory syndrome Coronavirus-2 in the tears of patients with Coronavirus disease 2019. Eye (Lond) 2020;34:1220-3.
- Kumar K, Prakash AA, Gangasagara SB, et al. Presence of viral RNA of SARS-CoV-2 in conjunctival swab specimens of Covid-19 patients. Indian journal of ophthalmology 2020;68:1015-7.
- Seah IYJ, Anderson DE, Kang AEZ, et al. Assessing Viral Shedding and Infectivity of Tears in Coronavirus Disease 2019 (Covid-19) Patients. Ophthalmology 2020;127:977-9.
- Wu P, Duan F, Luo C, et al. Characteristics of Ocular Findings of Patients With Coronavirus Disease 2019 (Covid-19) in Hubei Province, China. JAMA Ophthalmol 2020;138:575-8.
- Xia J, Tong J, Liu M, et al. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol 2020;92:589-94.
- Zhang X, Chen X, Chen L, et al. The evidence of SARS-CoV-2 infection on ocular surface. The ocular surface 2020;18:360-2.
- Zhou Y, Duan C, Zeng Y, et al. Ocular Findings and Proportion with Conjunctival SARS-COV-2 in Covid- 19 Patients. Ophthalmology 2020;127:982-3.
- Zhou Y, Zeng Y, Tong Y, et al. Ophthalmologic evidence against the interpersonal transmission of 2019 novel coronavirus through conjunctiva. medRxiv 2020:2020.02.11.20021956.
- Cheema M, Aghazadeh H, Nazarali S, et al. Keratoconjunctivitis as the initial medical presentation of the novel coronavirus disease 2019 (Covid-19). Canadian Journal of Ophthalmology 2020;55:e125-e9.
- Chen L, Liu M, Zhang Z, et al. Ocular manifestations of a hospitalised patient with confirmed 2019 novel coronavirus disease. The British journal of ophthalmology 2020;104:748-51.
- Colavita F, Lapa D, Carletti F, et al. SARS-CoV-2 Isolation From Ocular Secretions of a Patient With Covid-19 in Italy With Prolonged Viral RNA Detection. Ann Intern Med 2020;173:242-3.
- Daruich A, Martin D, Bremond-Gignac D. Ocular manifestation as first sign of Coronavirus Disease 2019 (Covid-19): Interest of telemedicine during the pandemic context. Journal francais d’ophtalmologie 2020;43:389-91.
- Khavandi S, Tabibzadeh E, Naderan M, et al. Corona virus disease-19 (Covid-19) presenting as conjunctivitis: atypically high-risk during a pandemic. Contact lens & anterior eye : the journal of the British Contact Lens Association 2020;43:211-2.
- Ying NY, Idris NS, Muhamad R, et al. Coronavirus Disease 2019 Presenting as Conjunctivitis. Korean journal of family medicine 2020.
- Scalinci SZ, Trovato Battagliola E. Conjunctivitis can be the only presenting sign and symptom of Covid- 19. IDCases 2020;20:e00774.
- Jones L, Walsh K. Covid-19 and contact lenses: practice re-entry considerations. Optician 2020;07 Aug:22-8.
- Docherty AB, Harrison EM, Green CA, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. Bmj 2020;369:m1985.
- Zeri F, Naroo SA. Contact lens practice in the time of Covid-19. Contact lens & anterior eye 2020;43:193-5.
- Amesty MA, Alio Del Barrio JL, Alio JL. Covid-19 Disease and Ophthalmology: An Update. Ophthalmol Ther 2020;9:1-12.
- Safadi K, Kruger JM, Chowers I, et al. Ophthalmology practice during the Covid-19 pandemic. BMJ open ophthalmology 2020;5:e000487.
- Lai THT, Tang EWH, Chau SKY, et al. Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: an experience from Hong Kong. Graefe’s Archive for Clinical and Experimental Ophthalmology 2020;258:1049-55.
- Nagra M, Vianya-Estopa M, Wolffsohn JS. Could telehealth help eye care practitioners adapt contact lens services during the Covid-19 pandemic? Contact lens & anterior eye : the journal of the British Contact Lens Association 2020;43:204-7.
- Center for Disease Control and Prevention. How to remove gloves. 2020 [updated 2020. Available at: https://www.cdc.gov/vhf/ebola/pdf/poster-how-to-remove-gloves.pdf. Accessed: 10 Nov 2020];
- BCLA Re-/fitting contact lens wearers in practice. 2020 [updated 2020. Available at: file:///C:/Users/k7walsh/Downloads/BCLA%20Re%20Fitting%20Contact%20Lens%20guidance%20sheet %20FINAL%20(1).pdf. Accessed: 08 Nov 2020];
- The College of Optometrists Covid-19: College Guidance 2020 [updated 2020. Available at: https://www.college-optometrists.org/guidance/covid-19-coronavirus-guidance-information/covid-19- college-guidance.html. Accessed: 05 Nov 2020];
- Morgan PB. Contact lens wear during the Covid-19 pandemic. Contact Lens and Anterior Eye 2020;43:213.
- García-Ayuso D, Escámez-Torrecilla M, Galindo-Romero C, et al. Influence of the Covid-19 pandemic on contact lens wear in Spain. Contact Lens and Anterior Eye 2020.
- Vianya-Estopa M, Wolffsohn JS, Beukes E, et al. Soft contact lens wearers’ compliance during the Covid-19 pandemic. Contact Lens and Anterior Eye 2020;https://doi.org/10.1016/j.clae.2020.08.003.
- Polk M. Seizing the moment. Optician 2020;Aug:14-7.
- Jones L, Walsh K, Willcox M, et al. The Covid-19 pandemic: Important considerations for contact lens practitioners. Contact lens & anterior eye 2020;43:196-203.
- Coronavirus productiviwty data: How the pandemic is changing the way we use digital devices, apps, and tools. 2020. [Available at: https://blog.rescuetime.com/corona
