Some simple facts help set the scene for this global review. It has been established that modern soft toric contact lenses are as quick and simple to fit as spherical lenses,1 with good visual outcomes and rotational stability across many visual tasks.2-7 However, when 400 eye care professionals (ECPs) in the US were asked, only around half agreed soft torics are as easy to fit as the equivalent spherical lens (49%), and that they have excellent rotational recovery (55%).8 How does this disparity between reported product performance and practitioner attitude influence fitting practices? Ultimately, what is the impact on patients, and how close does current practice come to meeting their
expectations?
How many patients have astigmatism?
To evaluate how proactive ECPs are with fitting soft toric lenses both the prevalence of astigmatism and the proportion of soft torics fit need to be known. A number of factors influence the estimated prevalence of astigmatism. Defining it by the presence of any astigmatism (0.25DC) naturally results in a higher number than using a minimum level of astigmatism of at least 0.75DC. For the purposes of soft toric fitting a more useful threshold to use is 0.75DC, the amount of astigmatism ECPs typically consider as the lowest amount that would need correcting with a soft toric design.9 The use of data from only one eye compared to both eyes changes prevalence estimates, and given that astigmatism becomes more common with age,10,11 the range of ages included in the dataset has an influence too. Prevalence also varies depending on the study population, with regional differences reported in a recent meta-analysis ranging from 11.4% (95% CI: 2.1 to 20.7) in Africa to 45.6% (95% CI: 44.1 to 47.1) in the Americas,12 and 44.8% (95% CI: 36.6 to 53.1) in South-East Asia.13
Keeping all these considerations in mind, the global prevalence of astigmatism of at least 0.75DC (described as >0.50DC) is 40% (95% CI: 34 to 47) among those aged over 30 years.13 Assuming the contact lens wearing population are representative of the larger visually corrected population, if ECPs were routinely recommending toric lenses to all astigmats of at least 0.75DC, it would be expected that use of soft torics would represent a similar proportion of soft lens fits. So how do fitting practices compare?
Current soft toric fitting practice
While the prevalence of astigmatism has not changed significantly during the last three decades,13 soft toric lens design and availability certainly has. Given the wide choice of materials, replacement schedules, prescription options and toric lens designs, the ECP has many options from which to choose. So how close are toric fitting practices to representing 40% of fits?
Data from the most recent international contact lens prescribing report show soft toric lenses represented 27% of all soft lens fits reported (average of 24 countries reporting more than 100 fits).14 Within the category of “soft fits”, the largest proportion came from spherical (51%) and toric lenses respectively (27%), with smaller contributions from the categories of multifocal, monovision, cosmetic and myopia control fits.14 It is helpful to remove the additional soft lens types and fitting categories and compare the proportion of soft toric to spherical fits only. Using data collected by the international contact lens prescribing report over the last five years it can be seen that, on average across twenty-five countries, soft torics have been fit 37% of the time (figure 1).14-18 Wide variation exists between countries, varying from just 9% in Russia and 17% in Japan to 54% in Switzerland.
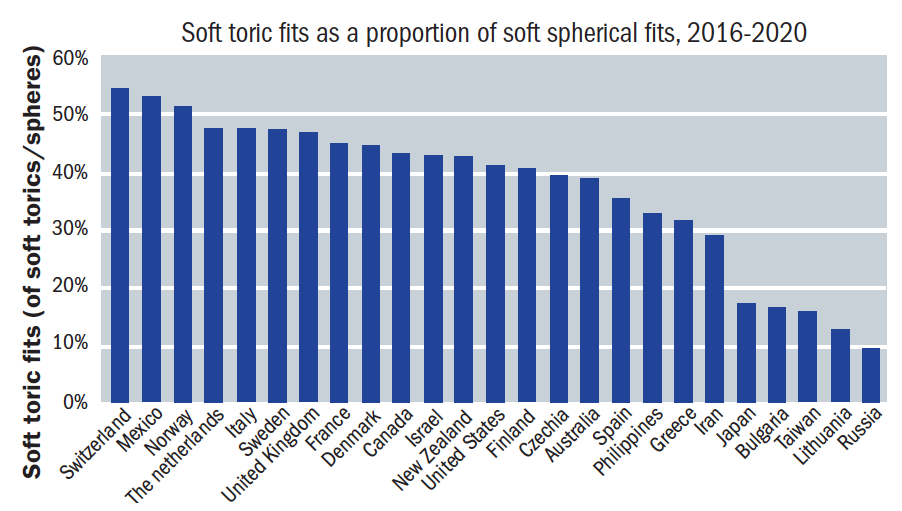 Figure 1: Average soft toric fits as a proportion of soft spherical fits from the past five years of the international contact lens prescribing report, 2016 to 202014-18
Figure 1: Average soft toric fits as a proportion of soft spherical fits from the past five years of the international contact lens prescribing report, 2016 to 202014-18
While the average figure from these data is 37%, placing just over half the countries comfortably at or over the 40% activity expected from the incidence of astigmatism in general, that is not quite the whole story. It should be noted that the international contact lens prescribing report provides a snapshot of fitting activity for each year the survey is conducted. The number of ECPs returning completed surveys varies by country, and of course represents a very small proportion of the total number of ECPs in that region. Given the time required to complete the survey it could be argued that those ECPs who choose to be involved in the survey are a self-selecting group of interested contact lens practitioners. Viewed in this light, it may be sensible to consider the results of the international contact lens prescribing report as a good reflection of proactive fitting; a potential predictor in a sense, of where the rest of that particular market may be heading over time.
In short, while the 700 ECPs in the UK who responded to the survey in 2020 are routinely fitting astigmats with soft toric lenses, this does not necessarily mean that the remaining majority of several thousand practitioners in this country are also doing the same. What is reassuring however, is that these data certainly show what is possible with proactive fitting, and should help encourage those ECPs within a country, and in those regions where lower fitting still exists, to feel more confident in increasing their use of soft toric contact lenses.
Daily disposable soft torics
It can be challenging to change fitting habits when lens availability is limited, and for some modality and material choices for soft torics this may once have been true. It is helpful to see that more soft toric options and expanded power ranges have become available for ECPs and patients as daily disposables. As choice increases, so clinical practice can change to embrace this. Use of daily disposables as a modality is increasing worldwide, and while countries such as the UK and Denmark have reported significant fits with this modality for years,15 the US has only more recently moved towards proactive fitting and refitting into daily disposables. Between 2018 and 2019, the growth in terms of value of soft toric daily disposables globally was nearly three times that of spherical lenses (14% vs 5%), with double digit growth in Japan (14%), the UK (13%) and the US (19%).19 This indicates increased fitting of soft toric daily disposables, and can be contrasted with global growth of frequently replaced soft torics at just 2% during the same period.19 These data show encouraging and growing use of soft toric daily disposables, suggesting for these countries at least, given time, the gap between astigmatism prevalence in the population and soft toric prescribing rate will close.
Eye care professional beliefs
Highlighted in the opening of this article, recent surveys serve as a reminder that not all ECPs trust the performance of soft toric lenses and there remains potential for growth even in the three countries mentioned above. Four hundred ECPs in the US were questioned to establish their beliefs and attitudes towards soft toric contact lenses.8 They were asked about several aspects of their fitting and performance. Are they beneficial for low astigmats compared to spherical contact lenses? Is vision with soft torics as good as spectacle acuity? Are they easy to fit? Fundamental beliefs that would clearly influence ECP confidence with using the lenses proactively with a wide range of patients.
The interesting results of the survey are shown in figure 2. Sixty percent of ECPs agree that toric lenses provide better visual acuity for low astigmats (0.75 and 1.00DC) than best vision sphere contact lenses.8 A result that leaves four out of 10 ECPs possibly believing that a spherical correction in these patients is ‘good enough’. Further, only half agreed that they believed toric lenses provide the same visual acuity as a patient’s up to date spectacles.8 Together, these two results suggest 40 to 50% of ECPs believe spherical correction for low astigmats is fine, and/or that toric contact lenses do not deliver visual acuity as good as spectacles. This appears to paint a picture of ECPs holding onto some historical concerns about the visual performance of soft toric lenses.
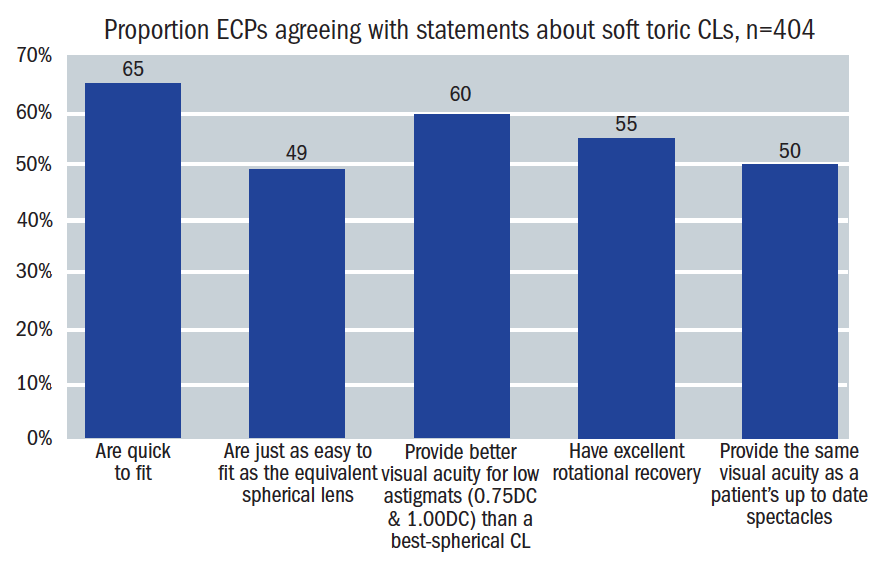 Figure 2: ECP agreement to statements about soft toric contact lenses (n=404) 8
Figure 2: ECP agreement to statements about soft toric contact lenses (n=404) 8
Ideally, to be widely adopted, a contact lens should be quick and easy to fit, with predictable performance in general. While nearly two-thirds (65%) of ECPs agreed toric lenses are quick to fit, only half agreed they are as easy to fit as the equivalent spherical lens (49%), and that they have excellent rotational recovery (55%).8 This leaves between one-third to one-half of ECPs potentially harbouring concerns that soft torics are not easy to fit, take longer than spherical lenses and may not have good rotational recovery.
Confident and proactive topic lens recommendation
The wide variation in soft toric fitting practices around the world, coupled with a sense that some ECPs are not fully confident in the ease of fitting and overall performance of soft torics provides a number of areas to address. Discussed below and summarised in table 1, these relate to broad areas such as patient needs, professional communication, product performance, and practice set up. Addressing these concerns should help support ECPs who do not already embrace soft toric options to feel more confident in recommending them more frequently.
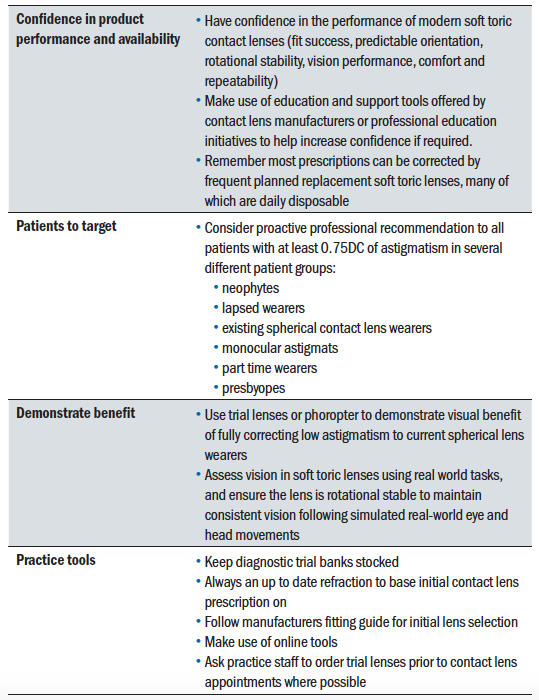 Table 1: Focusing on soft toric lens opportunities
Table 1: Focusing on soft toric lens opportunities
Importance of correcting low levels of astigmatism
Low to moderate levels of astigmatism are rarely omitted from spectacle corrections. Leaving 1.00DC of astigmatism uncorrected can result in a significant decrease in distance and near visual acuity,20 reading speed,20 decrease reading fluency,21 and stereoacuity.22 Symptoms of ocular discomfort, dry eye and headaches can also result from uncorrected astigmatism.20,21 A once popularly held view that thick or high modulus spherical designs can ‘mask’ astigmatism has proved not to be true.23-26 Likewise, aspheric lenses do not demonstrate improved visual outcomes for low astigmats compared to toric corrections.27,28
Poor satisfaction with vision in contact lenses is clearly undesirable and can ultimately lead to drop out. Sub-optimal vision performance is a significant cause of contact lens drop out by itself.29,30 Astigmats have been shown to over-index in contact lens drop outs,29,31,32 a fact which serves as a pertinent reminder to ensure the vision and comfort needs of this patient group are fully met in contact lenses.
The evidence summarised above shows that, when compared with spherical lenses, correction of astigmats with toric lens designs results in significantly improved subjective and objective visual performance.36,37 This can be demonstrated to a patient in practice by having them view the smallest line of letters they can see both with and without the cylinder correction in place. These differences can be subtle and are often better demonstrated using a real-world target. The benefit could be demonstrated via viewing small detail on digital devices, or with night driving for instance. If an extended trial is not practical or desired, ensuring examples of real-world visual tasks are available to view in practice is a good alternative.
Patient expectations
Sub-optimal vision or comfort can result in drop out from lens wear. For new wearers, a prospective study established the drop out at 12 months to be 22.4%, with poor vision being cited as the main cause of discontinuation (41%) followed by comfort (36%).32 This highlights once again the importance of ensuring a patient is happy with the vision in their contact lenses.
Recent insights have generated a better picture of the expectations that patients place on their ECP too. Health and vision are both in the minds of patients when considering what they want to hear from their ECP. In terms of health performance, a survey of more than 1,500 contact lens wearers found nearly seven out of 10 agree they expect their ECP to recommend the lenses that provide 100% of the oxygen that their eyes need, regardless of cost.38 A separate survey of more than 5,000 lens wearers in five countries established that 86% agree they expect their ECP to make a recommendation for the soft contact lenses that provide the best possible vision correction for their eyes, regardless of cost.39 The fact that patients expect to hear about their best options regardless of cost is noteworthy. This information should help overcome any barrier in the ECP’s mind about price. This is relevant both for silicone hydrogel materials for oxygen performance and for toric lens designs to optimise vision performance. The message from the patient is clear: ‘Tell me about the best options to help me make an informed choice.’
Product performance and practice set up
The performance of early hydrogel soft toric designs include reports of intolerance, inadequate fit, handling difficulties and problems with vision.40 Unpredictable fitting characteristics,41 and variable lens position with blinking,42 and head position,2,3 all contribute to fluctuating vision and poor outcomes. Given this history, it is understandable, as seen in the survey of US practitioners, that some ECPs may still hold concerns about the performance of soft toric lenses.8 However, the design of modern toric lenses has evolved over time, with currently available options designed to achieve both quick and consistent fitting for the ECP, along with delivering comfort and stable vision for the wearer. A number of different approaches to achieving reliable and predictable orientation position and rotational stability exist such as dual thin zones (Precision Curve lens design, Alcon) prism-ballast, modified or optimised prism-ballast (Optimised Toric Lens Geometry, CooperVision; Peri-ballast design, Bausch + Lomb), and dynamic stabilised designs (Eyelid Stabilised Design, Johnson & Johnson Vision).
Several studies have examined the performance of these designs for static high contrast acuity, real-world visual tasks, rotational stability with eye and head movements, and rotational recovery, generally reporting, with some small differences between designs, that modern methods of stabilisation perform well.2-7 In fact, a recent analysis of over 400 subjects from 10 clinical trials using one proprietary design established across a number of factors, that a successful lens experience was achieved in all categories 83% of the time.43 Those factors included orientation success, fit acceptance, visual acuity, visual quality and comfort, and each individually returned success over 90% of the time.43
Successful fitting of astigmats in three different groups has been demonstrated: existing soft spherical lens wearers, contact lens drop outs and neophytes.44 In order, the fit success rate for those three groups was 80%, 75% and 70%, with previous spherical lens wearers also recording an improvement in visual acuity, and the neophyte group a level of vision in their contacts lenses comparable to their spectacles. Results such as this should help build confidence in the visual performance of soft torics compared to spectacles.
Limited prescription availability is a barrier sometime cited by ECPs. It is of interest to note ECPs tend to underestimate the proportion of patients that can be corrected with available soft toric contact lenses. When asked in a recent survey, ECPs felt one single reusable soft toric on average could be prescribed to between 55-74% of their patients depending on the product.8 When modern soft toric lens availability was compared to a large database of spectacle prescriptions it was actually shown that typical coverage is higher than ECPs believe. An example of this is a toric lens with cylinder correction available up to -1.75DC, spherical powers from +4.00DS to -8.00DS and 10 degree axes available around the clock actually provides cover for at least 90% of spectacle prescriptions,45 and this would be even higher for some soft toric lenses that have additional parameters available.
The length of time required to achieve a successful soft toric fit has been voiced as a concern in the past. Modern soft toric lenses are actually as quick to fit as spherical lenses,1 the fitting of which can be further supported by manufacturer supplied fitting sets and online fitting calculators. Both of these enable time-efficient fitting for ECPs and patients.
Initial lens selection, either from the trial set or via pre-ordering, can be supported in a number of ways. This may be via printed manufacturer fit guides and tools that confirm available prescription range, through to online toric lens calculators available, for example, from CooperVision, Johnson & Johnson Vision and Mark’Ennovy. Accuracy of the online tool available from CooperVision, OptiExpert, has been shown to agree with investigator prescribed final prescriptions in nine out of 10 eyes for different toric lenses.46,47 Use of these systems support accurate initial trial lens selection for the brand of toric lenses in question, and also enables trained support staff to order trial lenses in ahead of scheduled-appointments if required. Both the accuracy of initial prescription choice and the ability to use staff to order ahead are helpful to ensure efficient use of time in practice. These approaches can be applied to other lens fittings, including spherical and multifocal.
Additional opportunities
In those countries that already have a proportion of toric fits which approaches the prevalence of astigmatism in the general population, what are the further opportunities to focus on? Those patients with astigmatism in one eye only, monocular astigmats, should not be forgotten and may gain visual benefits from having their astigmatism fully corrected. Their need to wear a single toric lens if the level of astigmatism in that eye is low (say 0.75 or 1.00DC) may depend on a few factors. For example, whether the cylinder is in the dominant eye, the axis of their astigmatism, and the visual needs of the individual. The availability of several ‘families’ of contact lenses enables patients to wear the same material in both eyes, one sphere and one toric design. Wide prescription availability across contact lens families results in the majority of patients being able to be fitted.45
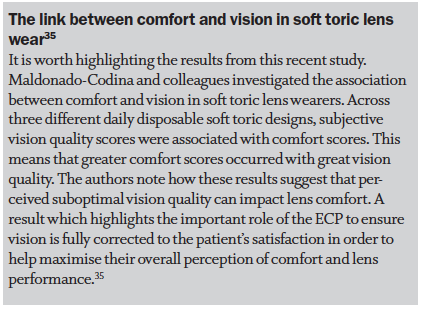
It is important not to overlook part-time contact lens wearers. The attitude of ‘spherical is good enough’ for part-time wear should be challenged, especially when the reasons for lens wear are factored in. Their part-time wear may be for sports, for hobbies requiring fine detailed vision or for social engagements where night driving may be necessary. Remember too that the association of visual quality with lens comfort.35 Optimising vision to be as good as spectacles could have significant benefits for these patients, and for those looking for part-time wear, availability of prescription range in daily disposable soft torics, in particular cylinder coverage and available axes, has increased over the last few years.
Always offer low astigmats wearing spherical contact lenses the option of toric lenses. Although adapted to their current level of acuity, they may benefit from improved quality of real-world vision if fully corrected. It was this group that did best when refitted into toric lenses, with eight out of 10 resulting in successful fits.44 Lapsed wearers also did well in this study, and with soft toric lens designs, and the materials they are available in, being distinctly different from just a few years ago, it is always worth offering the option of a contact lens trial to the lapsed astigmat too. It is even possible to improve quality of life scores by fitting soft torics compared to a spherical lenses for low to moderate astigmats.1 Finally, consider the aging population in the practice. An estimated one-third of current soft toric wearers are of presbyopic age.48 These patients need their near and intermediate vision corrected in addition to their distance vision and astigmatism. A toric multifocal design is required to achieve this in contact lenses, and no doubt in response to the growing need, the choice of lenses available in this category is increasing.
Conclusion
While a few countries report relatively high levels of soft toric prescribing, remember this is from a select group of ECPs in the international contact lens prescribing report and may not be reflective of wider prescribing practices in the region. Wide variation still exists in how proactively or otherwise soft torics are fit around the world. It remains important to ensure soft toric prescribing is not overlooked: patients’ visual demands and expectations of their ECP are high, and sub-optimal vision performance leads to drop out. ECPs who do not already feel comfortable with proactive recommendation of soft toric lenses can feel confident in the performance of modern soft toric contact lenses. They can deliver high first fit success rates, which can be made even more time-efficient in practice with the use of online fitting tools such as OptiExpert. Neophytes, lapsed wearers, low astigmats, monocular astigmats and astigmatic presbyopes all present significant opportunities to recommend toric lenses and ensure the patient’s visual needs in their contact lenses are being met.
Krupa Patel BScOptom(hons), MCOptom, FBCLA is Head of Professional Services at CooperVision UK & Ireland. Karen Walsh BSc, PGDip, MCOptom, FAAO is Professional Education Team Leader and Clinical Scientist at Centre for Ocular Research & Education (CORE), University of Waterloo, Canada.
References
- Cox SM, Berntsen DA, Bickle KM, et al. Efficacy of Toric Contact Lenses in Fitting and Patient-Reported Outcomes in Contact Lens Wearers. Eye & contact lens 2018;44 Suppl 1:S296-S9.
- Young G, McIlraith R, Hunt C. Clinical evaluation of factors affecting soft toric lens orientation. Optometry and vision science 2009;86:E1259-66.
- McIlraith R, Young G, Hunt C. Toric lens orientation and visual acuity in non-standard conditions. Contact lens & anterior eye 2010;33:23-6; quiz 43-4.
- Momeni-Moghaddam H, Naroo SA, Askarizadeh F, et al. Comparison of fitting stability of the different soft toric contact lenses. Contact Lens and Anterior Eye 2014;37:346-50.
- Edrington TB. A literature review: the impact of rotational stabilization methods on toric soft contact lens performance. Contact lens & anterior eye 2011;34:104-10.
- Zikos GA, Kang SS, Ciuffreda KJ, et al. Rotational stability of toric soft contact lenses during natural viewing conditions. Optometry and vision science 2007;84:1039-45.
- Chamberlain P, Morgan PB, Moody KJ, et al. Fluctuation in visual acuity during soft toric contact lens wear. Optometry and vision science 2011;88:E534-8.
- CVI data on file 2020. Kubic online survey; n=404 US ECPs who prescribe toric soft CLs.
- Young G, Sulley A, Hunt C. Prevalence of astigmatism in relation to soft contact lens fitting. Eye & contact lens 2011;37:20-5.
- Sawada A, Tomidokoro A, Araie M, et al. Refractive errors in an elderly Japanese population: the Tajimi study. Ophthalmology 2008;115:363-70 e3.
- Gudmundsdottir E, Jonasson F, Jonsson V, et al. “With the rule” astigmatism is not the rule in the elderly. Reykjavik Eye Study: a population based study of refraction and visual acuity in citizens of Reykjavik 50 years and older. Iceland-Japan Co-Working Study Groups. Acta ophthalmologica Scandinavica 2000;78:642-6.
- Varma R, Torres M, McKean-Cowdin R, et al. Prevalence and Risk Factors for Refractive Error in Adult Chinese Americans: The Chinese American Eye Study. American journal of ophthalmology 2017;175:201-12.
- Hashemi H, Fotouhi A, Yekta A, et al. Global and regional estimates of prevalence of refractive errors: Systematic review and meta-analysis. J Curr Ophthalmol 2018;30:3-22.
- Morgan P, Woods C, Tranoudis IG, et al. International Contact Lens Prescribing in 2020. Contact Lens Spectrum 2021:32-8.
- Morgan P, Woods C, Tranoudis IG, et al. International Contact Lens Prescribing in 2019. Contact Lens Spectrum 2020;35:26-32.
- Morgan P, Woods C, Tranoudis IG, et al. International Contact Lens Prescribing in 2018. Contact Lens Spectrum 2019;34:26-32.
- Morgan PB, Woods C, Tranoudis I, et al. International Contact Lens Prescribing in 2017. Contact Lens Spectrum 2018;33:28-33.
- Morgan PB, Woods C, Tranoudis I, et al. International contact lens prescribing in 2016. Contact Lens Spectrum 2017;32:30-5.
- CVI data on file, 2020. Industry reports and CooperVision data 2019.
- Wolffsohn JS, Bhogal G, Shah S. Effect of uncorrected astigmatism on vision. Journal of cataract and refractive surgery 2011;37:454-60.
- Wills J, Gillett R, Eastwell E, et al. Effect of simulated astigmatic refractive error on reading performance in the young. Optometry and vision science 2012;89:271-6.
- Al-Qahtani H, Al-Debasi H. The effects of experimentally induced graded monocular and binocular astigmatism on near stereoacuity. Saudi Journal of Ophthalmology 2018;32:275-9.
- Bernstein P, Gundel R, Rosen J. Masking corneal toricity with hydrogels: does it work? Int Contact Lens Clin 1991;18:67-70.
- Snyder C, Talley DK. Masking of astigmatism with selected spherical soft contact lenses. Journal of the American Optometric Association 1989;60:728-31.
- Edmonson LL, Edmondson W, Price R. Masking astigmatism Ciba Focus Night & Day vs Focus Monthly. Optometry and vision science 2003;80 (supp) 184.
- Cho P, Woo GC. Vision of low astigmats through thick and thin lathe-cut soft contact lenses. Contact lens & anterior eye 2001;24:153-60.
- Kollbaum PS, Bradley A. Aspheric contact lenses: Fact and fiction. Contact Lens Spectrum 2005;20:34 - 8.
- Morgan PB, Efron SE, Efron N, et al. Inefficacy of aspheric soft contact lenses for the correction of low levels of astigmatism. Optometry and vision science 2005;82:823-8.
- Young G. Why one million contact lens wearers dropped out. Contact lens & anterior eye 2004;27:83-5.
- Sulley A, Young G, Hunt C. Factors in the success of new contact lens wearers. Contact lens & anterior eye 2017;40:15-24.
- Young G, Veys J, Pritchard N, et al. A multi-centre study of lapsed contact lens wearers. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians 2002;22:516-27.
- Sulley A, Young G, Hunt C, et al. Retention Rates in New Contact Lens Wearers. Eye & contact lens 2018;44 Suppl 1:S273-S82.
- Rao SB, Simpson TL. Influence of Vision on Ocular Comfort Ratings. Optometry and vision science 2016;93:793-800.
- Orsborn G, Vega J, Orsborn G. Correlation Between Ocular Comfort and Vision Quality of Three Daily Disposable Soft Toric Contact Lenses with Different Moduli of Elasticity. Contact Lens and Anterior Eye 2019;42:e12.
- Maldonado-Codina C, Navascues Cornago M, Read ML, et al. The association of comfort and vision in soft toric contact lens wear. Contact Lens and Anterior Eye 2020.
- Cho P, Cheung SW, Charm J. Visual outcome of Soflens Daily Disposable and Soflens Daily Disposable for Astigmatism in subjects with low astigmatism. Clinical & experimental optometry 2012;95:43-7.
- Kruse A, Lofstrom T. How much visual benefit does an astigmat achieve being corrected with a toric correction? Int Contact Lens Clin 1996;23:59-65.
- CVI data on file 2018. YouGov online survey on silicone hydrogel lenses. N=1520 adult CL wearers (US 519, UK 501, Japan 500).
- CVI data on file 2020. Contact lens consumer confidence online survey, conducted Nov-Dec 2019 by YouGov Plc. Total of 5,347 contact lens wearers in 5 countries (Germany, Great Britain, Japan, Spain and the US).
- Evans J, Hau S. The therapeutic and optical application of a rigid gas permeable semi-limbal diameter contact lens. Contact lens & anterior eye 2009;32:165-9.
- Tan J, Papas E, Carnt N, et al. Performance standards for toric soft contact lenses. Optometry and vision science 2007;84:422-8.
- Tomlinson A, Ridder W, Watanabe R. Blink-induced variations in visual performance with toric soft contact lenses. Optometry and vision science 1994;71:545-9.
- Sulley A & Greenaway N. Success rates with a toric soft contact lens design. Optom Vis Sci 2020;97(E-abstract):205296.
- Sulley A, Young G, Lorenz KO, et al. Clinical evaluation of fitting toric soft contact lenses to current non-users. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians 2013;33:94-103.
- Luensmann D, Schaeffer JL, Rumney NJ, et al. Spectacle prescriptions review to determine prevalence of ametropia and coverage of frequent replacement soft toric contact lenses. Contact Lens and Anterior Eye 2018;41.
- Luensmann D, Woods J, Patel S. Validation of an online lens fitting app for two daily disposable toric lenses. Contact Lens and Anterior Eye 2019;42:e38-e9.
- Luensmann D, Woods J, McParland M. Toric lens fitting success supported by an online fitting App. In: NCC. Eindhoven; 2020.
- Industry fit data. January 2017-December 2017 Italy, UK and Germany. 41% of toric CL wearers age 41 years or over.
