The aftercare examination is a fundamental aspect of contact lens practice, providing an opportunity to review a patient’s needs, to assess for any changes to ocular physiology and to, where necessary, change the lens type in order to sustain, or even improve, patient satisfaction. As is the case with other areas of health, the saying that ‘prevention is better than cure’ applies here too, that is to say the best way to ensure successful long term wear of contact lenses is to avoid complications from occurring in the first place. For ongoing contact lens success, the importance of effective aftercare cannot be over-emphasised, particularly given the high drop-out rate. Among established wearers, the most common reason for discontinuation is discomfort, reported by around half of those who lapse.1
A patient’s requirement from their contact lenses will be dynamic and may change for a variety of reasons such as a change in job, environment or lifestyle. Thus, another key goal of the aftercare is to re-assess whether the patient’s current contact lenses still meet their requirements, to avoid the risk of the patient becoming unhappy and dropping out of lens wear. Due to the speed of development within the contact lens industry, practices and recommendations should constantly be reviewed, keeping up to date with the latest lens materials, designs and care systems. The aftercare appointment provides the ideal opportunity to discuss any new products that may have been introduced to the market.
The aftercare routine for a soft contact lens wearer comprises six distinct elements, each of which will be discussed in this article (figure 1, below). 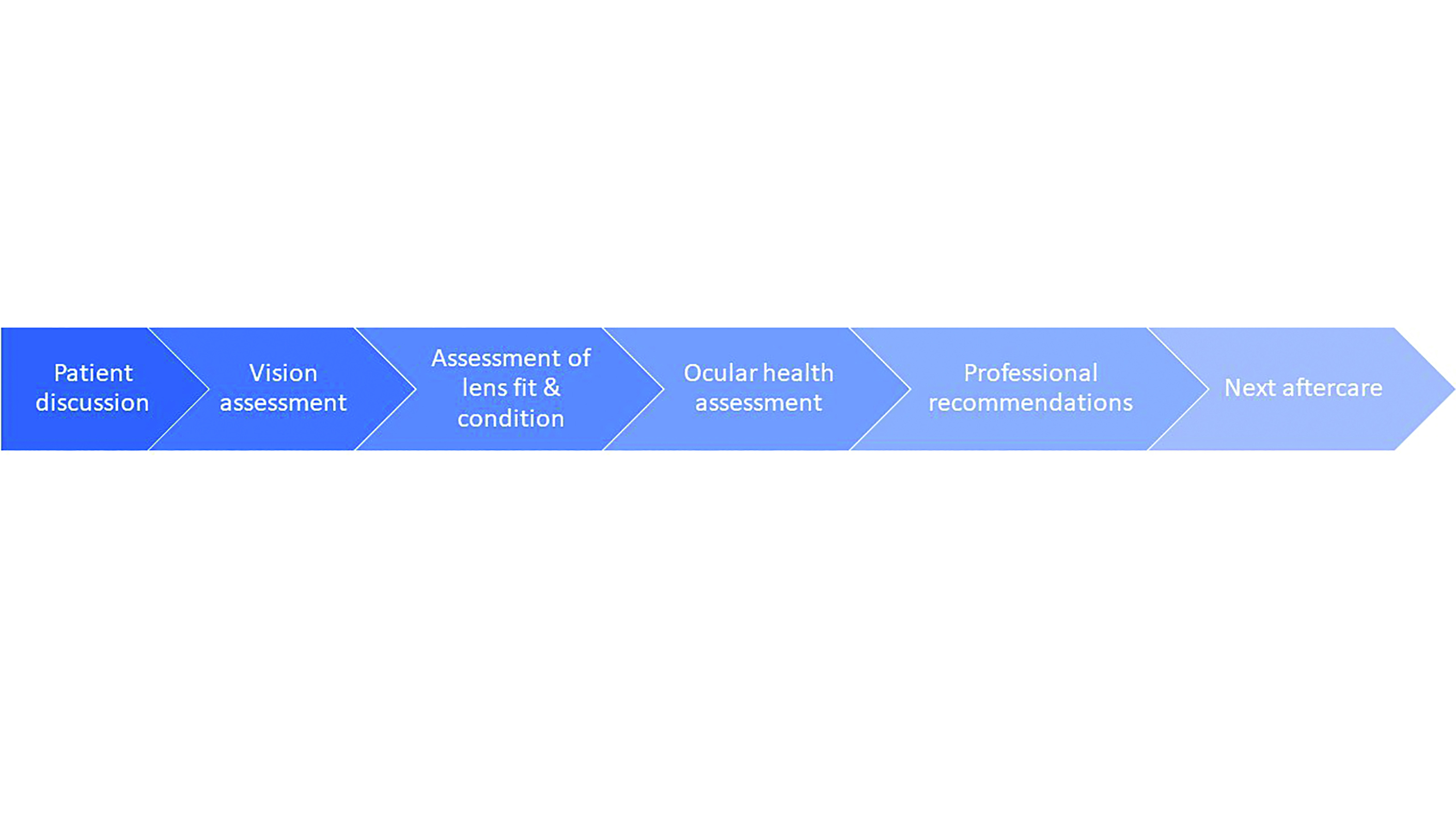
Aftercare routine
Patient discussion
Patient discussion is a vital aspect of the aftercare examination and clear communication is important to ensure that the correct information is gathered. During history and symptoms taking, it is best to adopt a conversational questioning technique with the use of both open and closed questions; this will encourage the patient to talk more freely and may allow additional important information to be elicited. A friendly and approachable manner will put patients at ease and is likely to result in them being more honest about their true practices.
While no two patient discussions will be the same, it is important to ensure that each discussion follows a similar structure, to avoid missing important information. The most comprehensive and logical way to structure the history and symptoms taking during a lens aftercare is indicated in table 1. If a problem or issue is reported then more probing questions should be asked in order to investigate this further. These might include questions such as asking whether the issue affects one eye or both, occurred suddenly or gradually, is constant or intermittent or worse at any particular time (such as after application), and so on. It is important to consider how best to word questions in order to ensure you gather the right information from the patient; some examples of questions that can be asked are given in table 1.
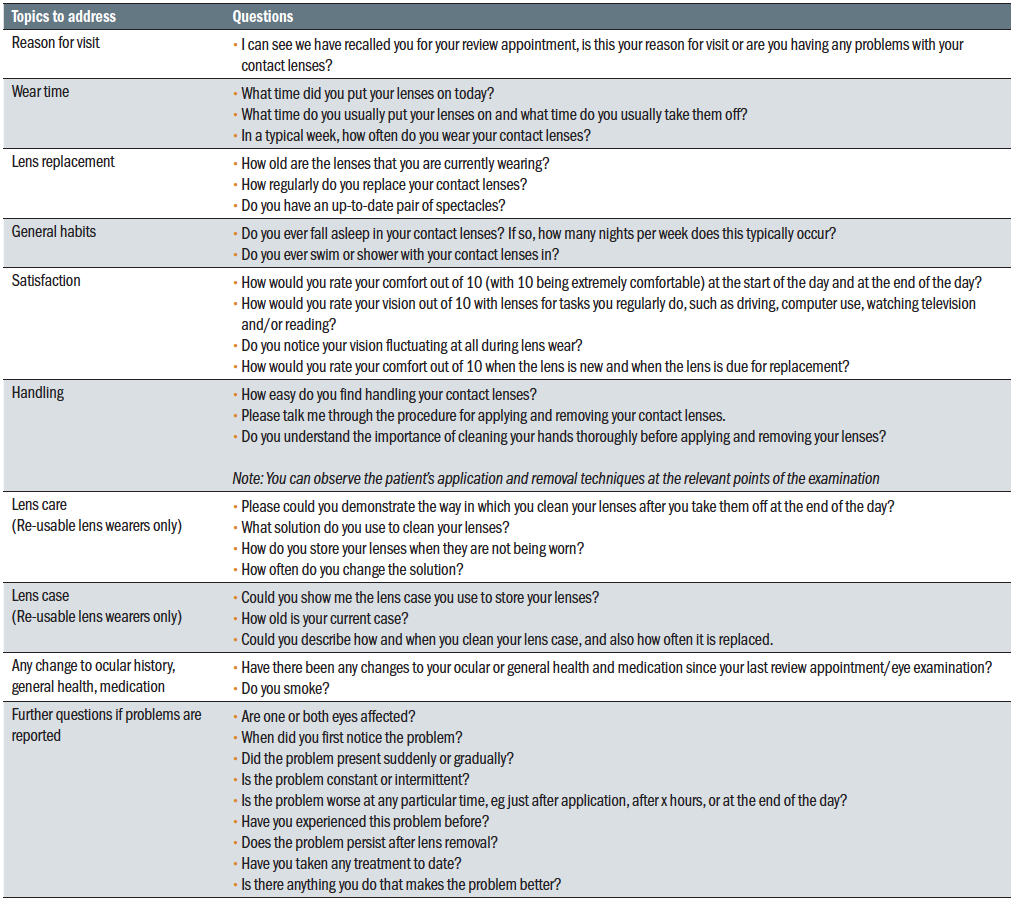 Table 1: Recommended structure for patient discussion in an aftercare appointment
Table 1: Recommended structure for patient discussion in an aftercare appointment
During the contact lens aftercare, it is especially important to review the patient’s compliance with hygiene practices. Poor hygiene can lead to a whole host of complications ranging from mild lens discomfort to severe sight-threatening infections,2
so good hygiene practices should be reinforced at every
appointment.
Research has shown that full compliance with the recommended lens and case regime is rare3 and most contact lens wearers do not follow the guidance that is given in at least some aspects. Daily disposable lens wearers are more likely to be compliant, and this is thought to be due to the relative simplicity of this modality of wear compared to reusable lenses, where there are several additional steps to follow in order to properly clean the lenses and case. Efron and Morgan,4,8 assessed the number of compliance steps that are needed for a lens wearer to be fully compliant and found there were 53 steps for those wearing reusable lenses compared with just 26 for daily lens wearers (table 2).
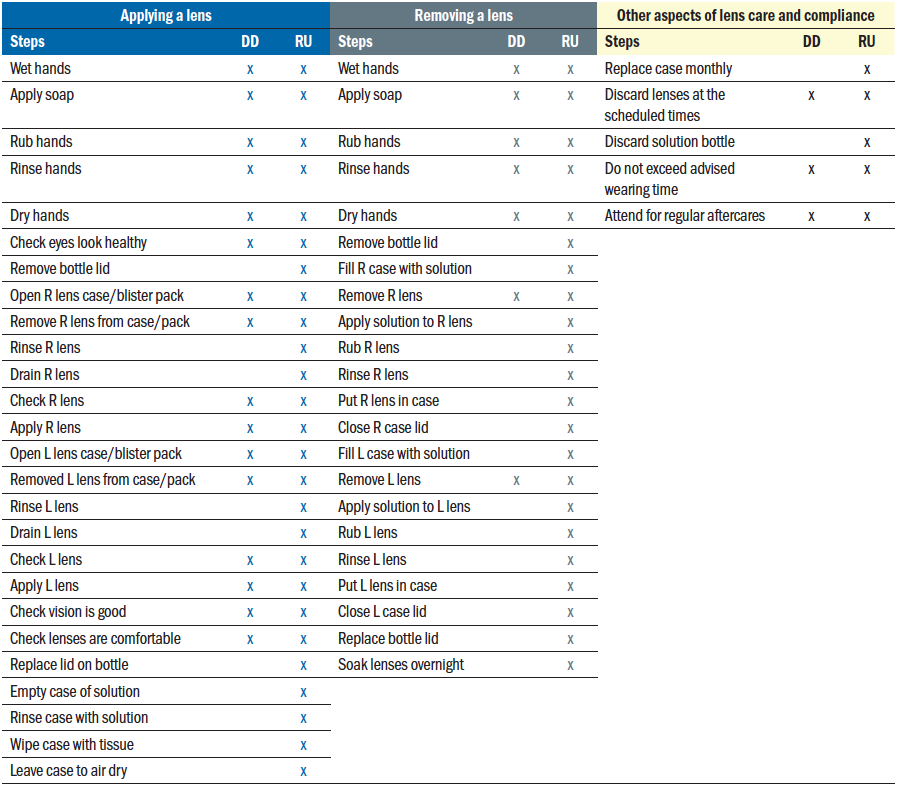 Table 2: A comparison of the number of steps required for compliant lens wear with daily disposable (DD) versus reusable lenses (RU). Adapted from Efron and Morgan4
Table 2: A comparison of the number of steps required for compliant lens wear with daily disposable (DD) versus reusable lenses (RU). Adapted from Efron and Morgan4
A thorough review of the patient’s application, removal and cleaning routine will help identify any bad habits. Practitioners should also make use of their observation skills to assess patient compliance; this can be done by checking things like the general cleanliness of the patient’s hands, length of fingernails, state of their lens case and observation of the process for contact lens removal.
Vision assessment
Contact lenses are primarily worn to improve vision, although they may also be worn for cosmetic reasons, in myopia control or for therapeutic applications. In all cases, measurement of visual acuity (VA) is a legal requirement that must be recorded at every aftercare appointment. There can be some disparity between VA and subjective experience of visual quality, and good VA does not necessarily equate to good visual quality, with one study showing a poor correlation between the two.5 Consequently, quality of vision should also be ascertained, and can quite easily be done using interval scales (as described in table 1) or a visual analogue scale.
Visual acuities should be measured and recorded both monocularly and binocularly. Where appropriate, monocular or binocular over-refraction should then be conducted to determine the most up to date lens power to achieve maximum VA. The use of retinoscopy can be particularly helpful in assessing both the quality of the reflex and the degree of over-refraction required. It should be noted that a reduction in acuity may not only arise as a result of a refractive change; there may be other causes such as the presence of pathology, which would require further investigation and appropriate management. Additional tests such as keratometry may be indicated at this point if any significant changes from baseline are observed.
Assessment of lens fit and condition
The fit and condition of a soft lens should be checked using a slit lamp while it is in situ. A study that looked at how initial fit reflected end of day fit found that soft lenses take up to 20 minutes to settle, and so should be evaluated after this point as the fit after 20 minutes is largely predictive of the fit after eight hours of wear.6
First, an assessment of the lens surface condition should be made, checking for the presence of deposits and on-eye wettability. Measurement of the tear film by non-invasive methods will help to determine lens wettability (figures 2 and 3). Where
deposits or poor wettability is observed, the practitioner should consider if changes need to be made to the lens material or replacement frequency.
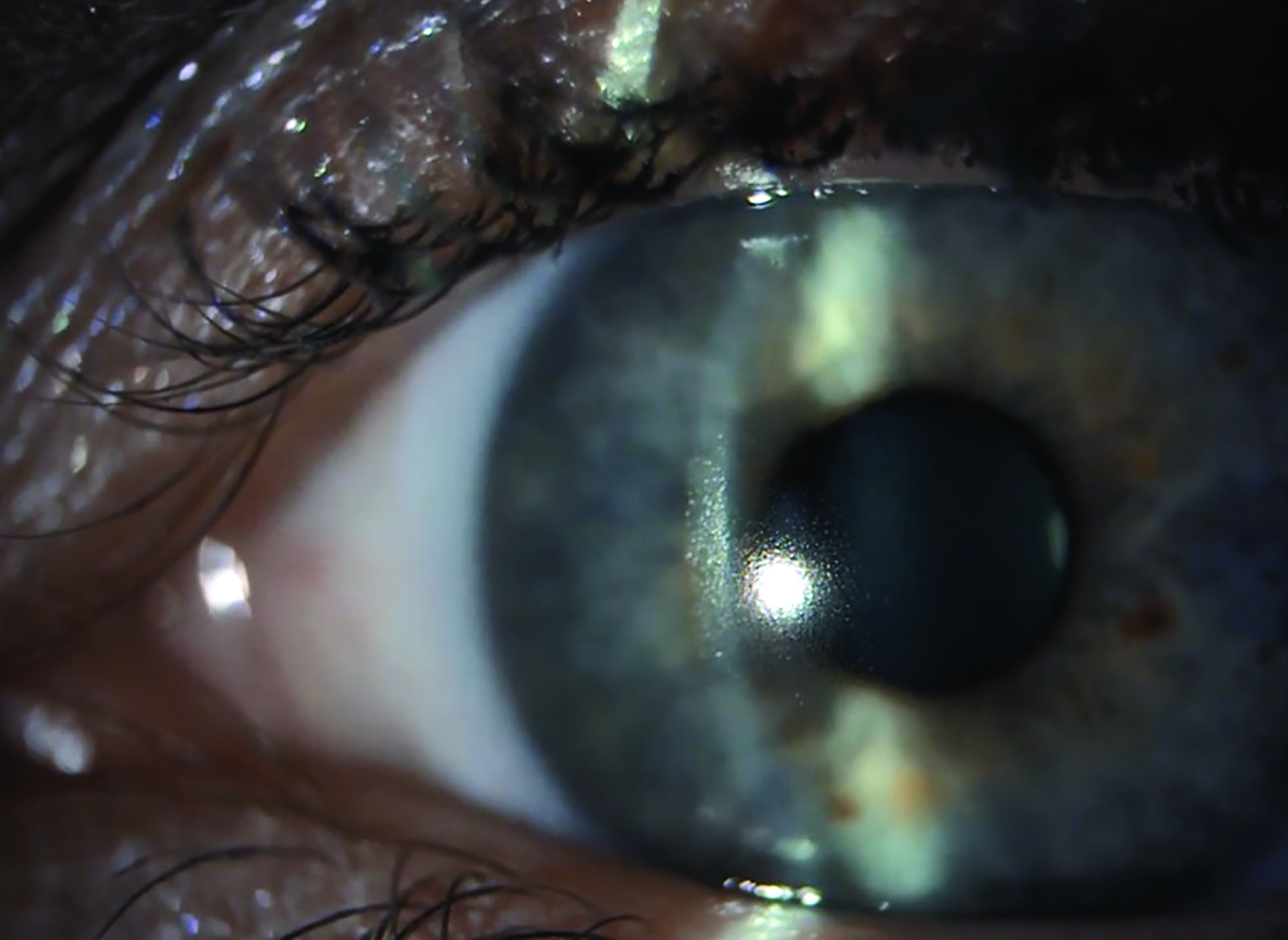 Figure 2: Assessment of contact lens wettability through observation of the 1st Purkinje image, with time to scatter following blink noted as the pre-lens thinning time
Figure 2: Assessment of contact lens wettability through observation of the 1st Purkinje image, with time to scatter following blink noted as the pre-lens thinning time
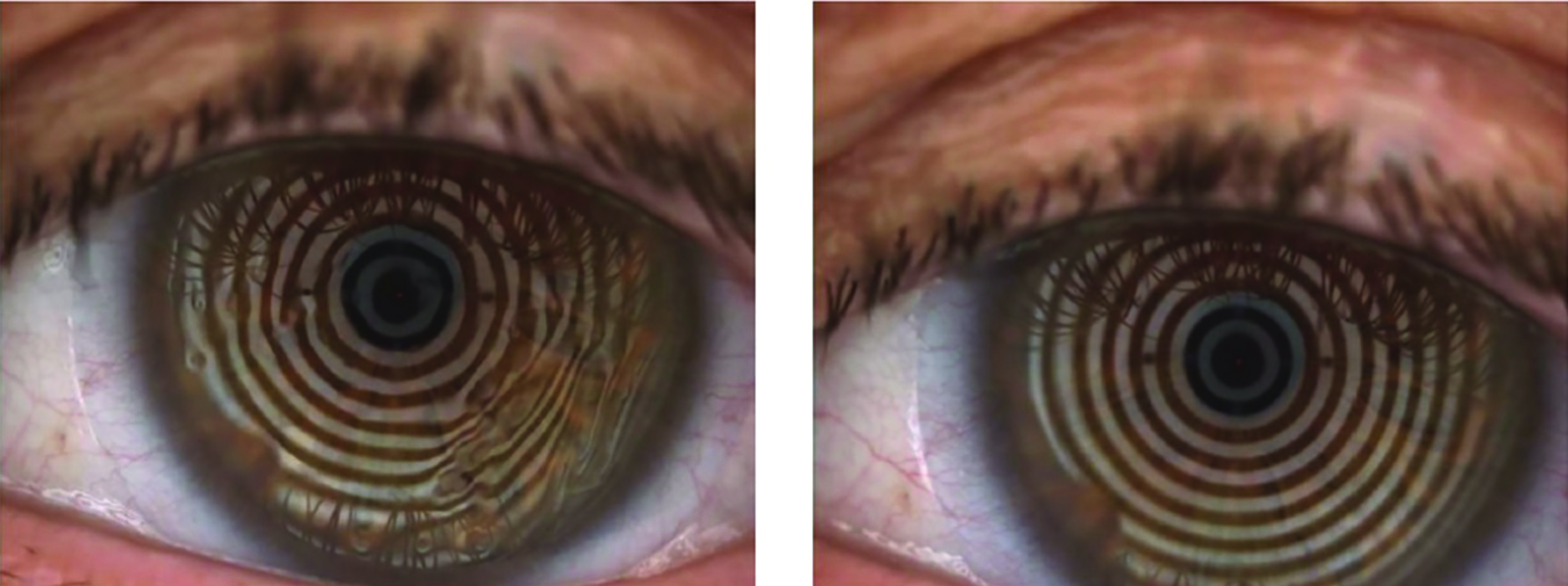 Figure 3: Assessment of pre-lens tear film break up time to provide information on contact lens wettability. Poor contact lens wetting is observed as distortion of Placido rings (left), versus good wetting (right)
Figure 3: Assessment of pre-lens tear film break up time to provide information on contact lens wettability. Poor contact lens wetting is observed as distortion of Placido rings (left), versus good wetting (right)
For soft lenses, corneal coverage, centration, edge alignment, movement on lateral gaze (lag), upgaze (sag), blink and push-up should all be assessed and recorded. An example record card is given in figure 4, as per Wolffsohn et al 2009.7 It is worth noting that fit can also be recorded in terms of millimetres of movement on blink and ease of recovery from push-up. For toric lens wearers, rotational alignment and stability should be checked using the markings on the lens. Any rotation can be assessed using the slit lamp graticule by overlaying a thin beam over the toric engraving.
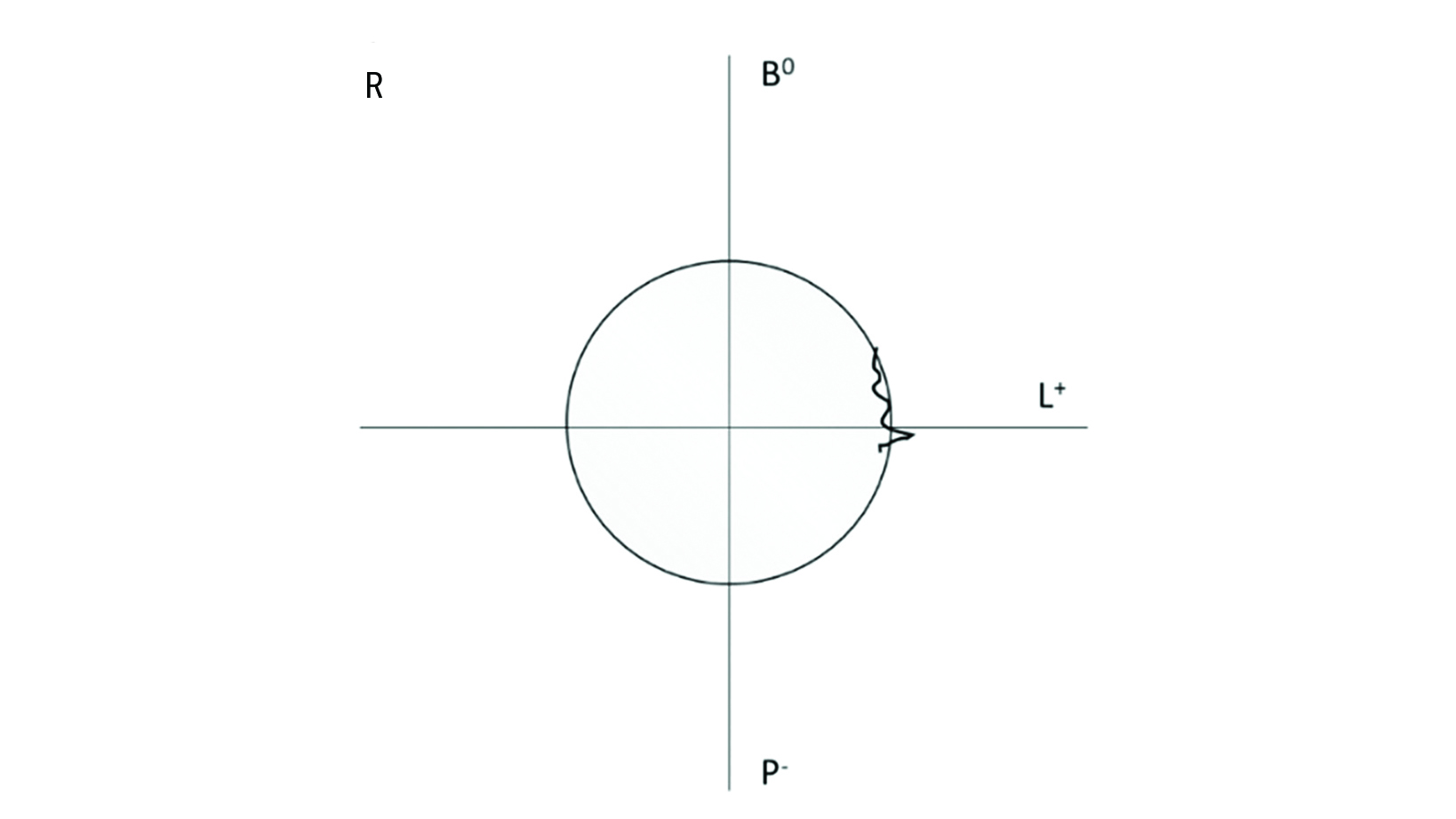
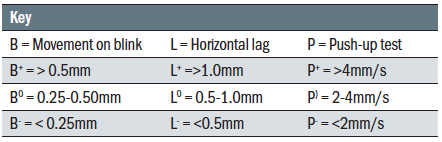
Figure 4: Example of a simplified method of recording soft lens fit according to Wolffsohn et al.7 showing central lens fit, with B0 indicating medium (0.25-0.5mm) movement on blink, L+ indicating large (>1.0mm) movement on excursions and P- indicating slow (<2 mm/s) recovery on push up. The scribbly line denotes limbal incursions occurring nasally
Ocular health examination
It is well known that contact lens wear can induce physiological changes to the eyelids, tear film, conjunctiva as well as all layers of the cornea,8 so it is important to conduct a thorough examination of anterior ocular health at every aftercare.
Advances in lens materials and the frequency with which most wearers now replace their lenses mean serious contact lens complications are not as commonly encountered at follow up appointments as they once were, and the majority of complications tend to only mildly affect vision or are self-limiting.11 Nevertheless, lens induced complications can still occur, and in general can be divided into those that are acute, chronic or both (figure 5). These complications should be kept in mind while examining the anterior ocular adnexa.
 Figure 5: List of acute and chronic ocular complications that can occur from contact lens wear. Adapted from Efron and Morgan4
Figure 5: List of acute and chronic ocular complications that can occur from contact lens wear. Adapted from Efron and Morgan4
As with history and symptom taking, the best way to proceed with this is to use a systematic approach going from low to high magnification, and from least invasive to most invasive techniques. As contact lens wearers should always have an in-date eye examination, it is not obligatory to carry out a fundus examination during a contact lens aftercare. The exception to this is if an abnormality is suspected that requires further examination.
Clear and comprehensive record keeping is essential to good practice, as well as being a requirement by law. Grading scales like the one shown in figure 6 should always be used to document any findings as they help to ensure a standardised approach to record keeping, particularly when a patient’s ocular complication is monitored by different practitioners within the same practice. There are different grading charts available and any can be used as long as the same one is used consistently each time and by all practitioners working together. It is recommended to make a note of which grading scale is used and record findings to one decimal place at every visit.9 All measurements should be compared to the previous or baseline measures in order to recognise and appropriately manage any changes early on.
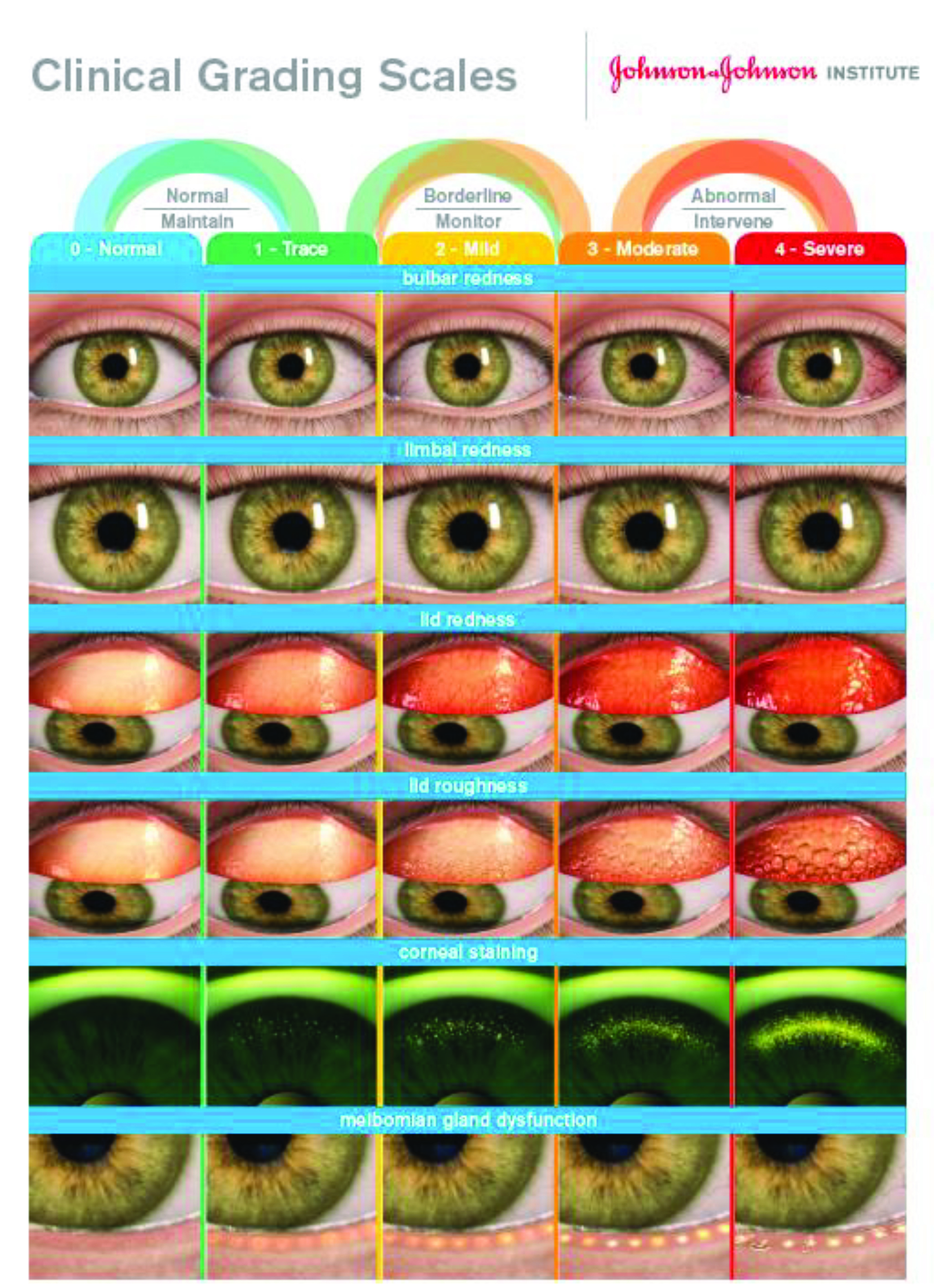 Figure 6: Grading scales should be used to document ocular health findings. The Johnson & Johnson Institute grading scale is based on the Efron scale
Figure 6: Grading scales should be used to document ocular health findings. The Johnson & Johnson Institute grading scale is based on the Efron scale
During a routine aftercare, practitioners should begin their examination of anterior eye health by checking that the lashes on both lids are clean and free of any crusting or flakes using diffuse illumination, medium brightness and low to medium magnification. Lid margins should be checked for any signs of oedema resulting from lens wear, which may show as thickened lids with poorly contoured edges, and meibomian glands should be examined for any signs of dysfunction.
At this early stage and before manipulation of the lids or instillation of fluorescein, the tear film should be assessed using the techniques described earlier in this series. This should include assessment of tear quantity by measurement of tear prism height, as well as assessment of tear quality from measurement of non-invasive tear break-up time should suitable tools exist in practice.
Corneal and limbal health should be checked using a series of different slit lamp techniques and higher magnifications, in order to thoroughly check for signs of corneal oedema, neovascularisation or the presence of infiltrates. While most modern contact lenses will meet the critical oxygen level of Dk/t over 24 x 10-9 for daily wear as defined by Holden & Mertz,10 it remains important to check for signs of oedema as shown by the appearance of microcysts and stromal striae. Signs can fade quite quickly once the lens has been removed and so it is recommended to check for signs of corneal oedema at the beginning of the ocular health check.
Microcysts are best viewed using retro-illumination, and will appear as small inclusions that do not move and show reversed illumination (figure 7). They can be mistaken for tear film debris and thus are often overlooked, however their presence in large numbers (>30) is indicative of epithelial metabolic distress. Vertical striae appear as a series of parallel white lines in the stroma (figure 7) and usually suggest that there is corneal oedema present that requires action. A further sign of hypoxia, neovascularisation, should also be assessed using retro-illumination or the red-free (green) filter on the slit lamp, and should be noted in terms of the millimetres of vessel growth into the cornea together with location.
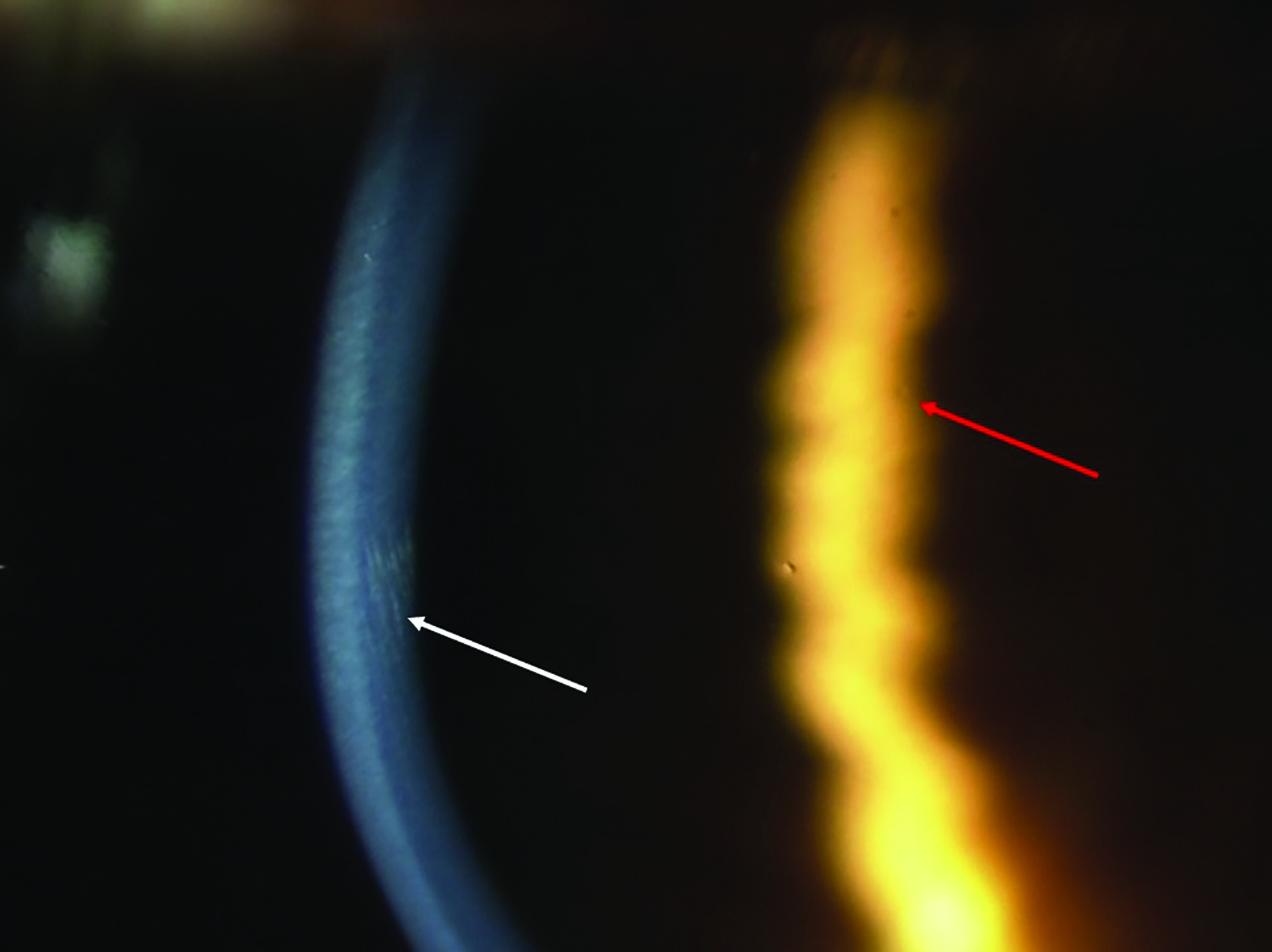 Figure 7: High magnification of the cornea showing simultaneous observation of striae (white arrow) in the optical section under direct illumination and a microcyst (red arrow) by indirect, retro-illumination
Figure 7: High magnification of the cornea showing simultaneous observation of striae (white arrow) in the optical section under direct illumination and a microcyst (red arrow) by indirect, retro-illumination
Following examining for signs of corneal oedema, a full slit-lamp routine should be carried out to assess the anterior ocular adnexa in detail. Adverse effects, such as conjunctival hyperaemia and corneal infiltrates should be noted and graded, then managed where necessary.
Fluorescein use is imperative at every aftercare visit for both soft and rigid lens wearers unless there are contraindications to its use such as in those with known hypersensitivity. When instilling fluorescein, it is important not to flood the eye and instead use the minimal amount in order to optimise viewing of any staining.11 The extent and depth of staining should be graded, with a particular focus on the pattern of staining as this can give an indication as to the cause (figure 8). With fluorescein instilled, invasive tear break up time can now be assessed.
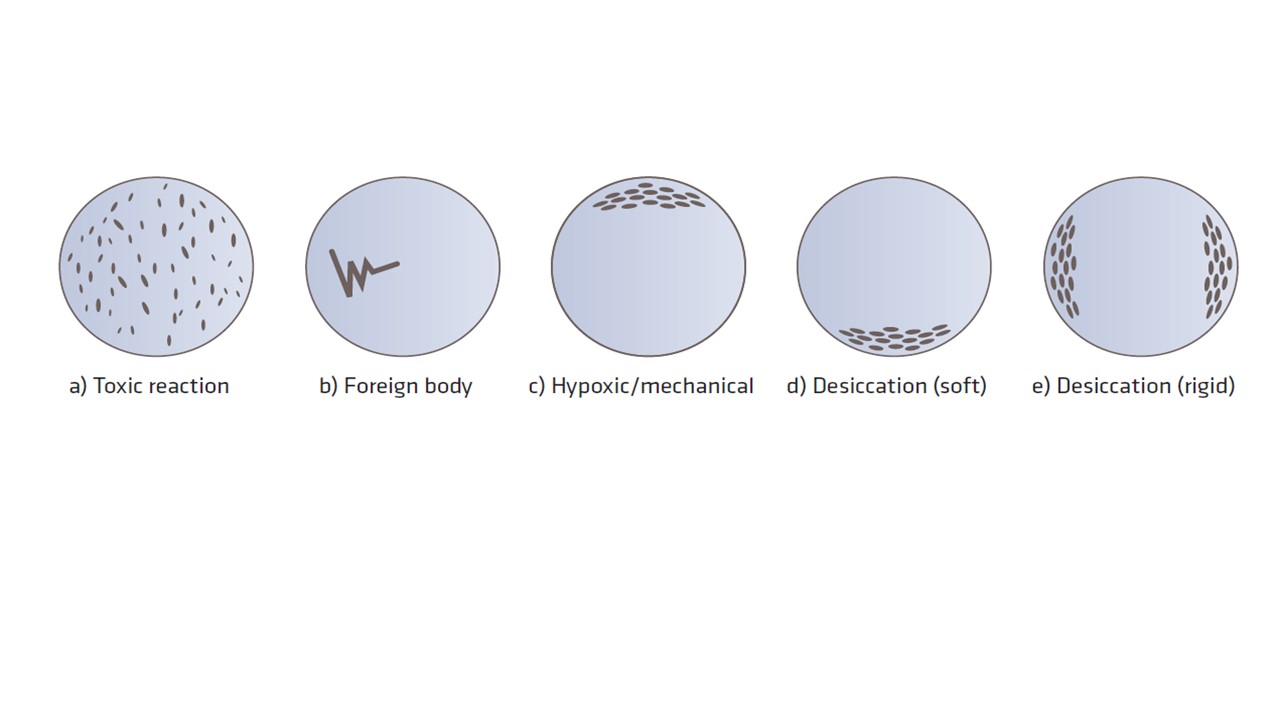 Figure 8: Epithelial staining patterns (schematic and for illustrative purposes only)
Figure 8: Epithelial staining patterns (schematic and for illustrative purposes only)
Lid eversion should be performed at all aftercare visits so that the palpebral conjunctiva can be assessed, and any allergic or mechanical effects of lens wear identified. The presence of follicles and/or papillae (figure 9) should be noted, along with their position, size and number.
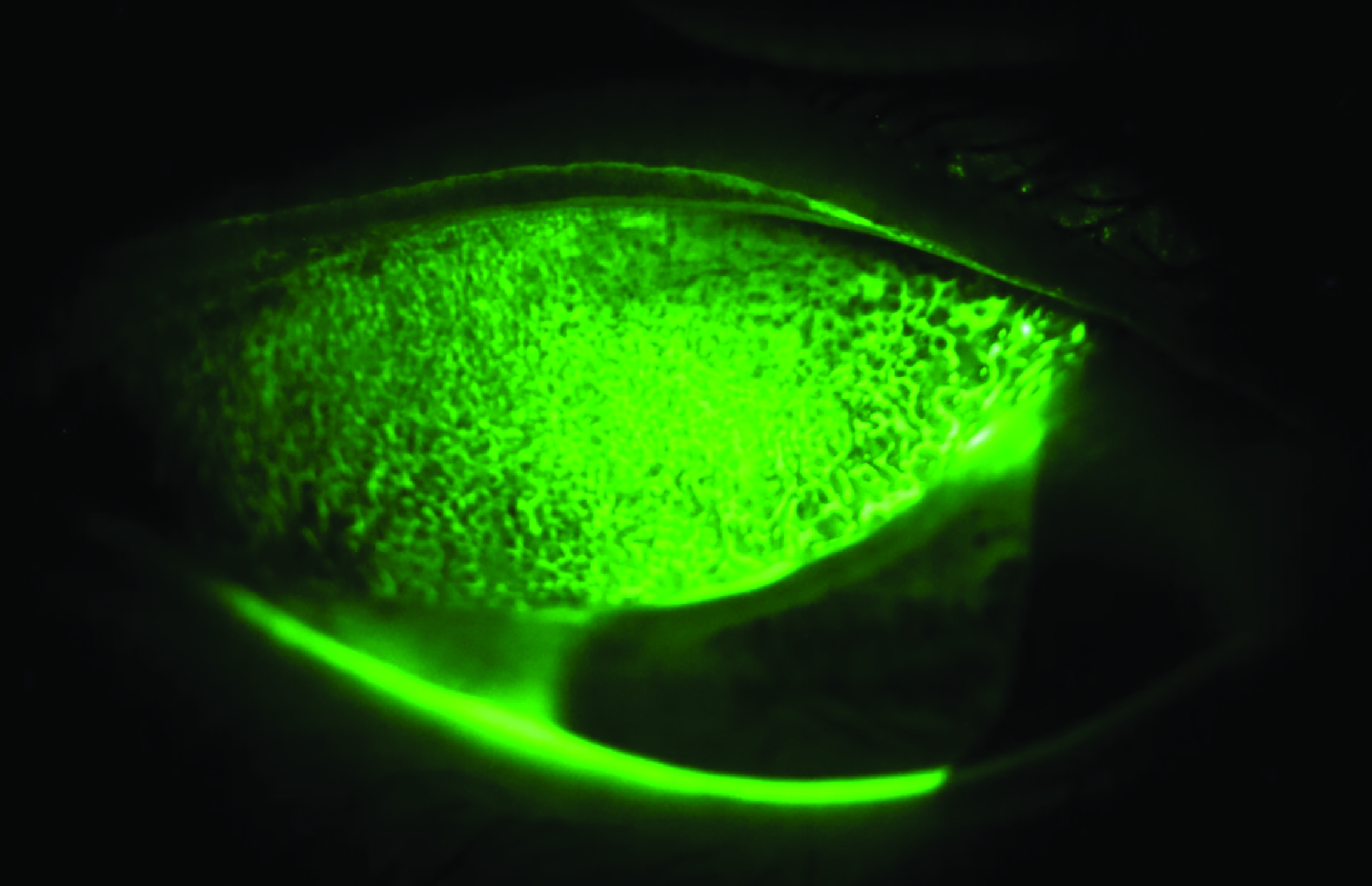 Figure 9: Examination of the superior palpebral conjunctiva using fluorescein to enhance visualisation of papillae
Figure 9: Examination of the superior palpebral conjunctiva using fluorescein to enhance visualisation of papillae
Professional recommendations
Once all the relevant tests and observations have been performed, results need to be considered in order to decide on the best course of action, ensuring the patient is involved in decisions and that their best interests are at the centre of all management plans. If any abnormalities or complications have been noted they should be addressed at this point. Additionally, any signs and symptoms that have been reported by the patient should also be dealt with. Common contact lens related signs and symptoms are given in table 3, along with suggestions for how to resolve them.
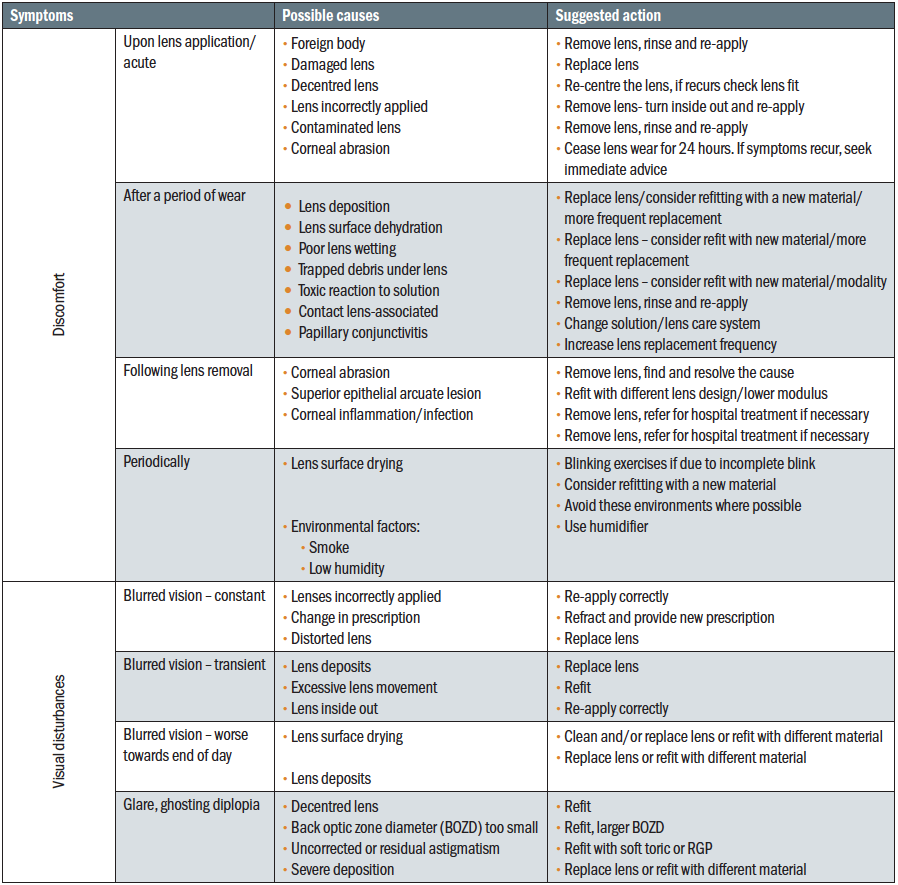 Table 3: List of common signs and symptoms associated with contact lens wear, along with suggested actions to resolve them
Table 3: List of common signs and symptoms associated with contact lens wear, along with suggested actions to resolve them
The recommendations you make at the end of the aftercare might include advising the patient to continue with their existing lenses, while addressing any compliance issues. Or, you might recommend trialling a different lens to resolve any observed ocular health complications, address any patient reported symptoms or to meet any changing needs. Alternative options might include trialling a different modality of wear, such as switching from reusable to daily disposable lenses for patients with discomfort issues or trialling a different lens material in view of any mechanical complications or patient reported symptoms. Any new contact lenses should be applied to check vision, fit and comfort before they are given to the patient to be trialled. This should then be followed up with a subsequent aftercare appointment after an appropriate interval.
Recommendations should be clearly communicated to the patient at the end of the aftercare, along with an explanation outlining the reasons for them as well as their potential benefits. It is good practice to give written instructions to supplement any
verbal advice given. A summary of the advice given should be noted on the patient record card for both future reference and legal purposes. It would be pertinent to remind all contact lens wearers of the importance of avoiding contact with water due to the increased risk of Acanthamoeba keratitis. Finally, the patient should always be given advice on what to do if they encounter any problems with their lenses before their next scheduled visit, as well as what to do in the event of an emergency including what signs or symptoms they should look out for.
Aftercare frequency
The importance of regular aftercare appointments should always be stressed to every contact lens wearer, both new and existing, and the review date for the next aftercare clearly communicated to the patient at the end of each appointment.
There is balance to be had between seeing a contact lens patient regularly enough to be able to detect any adverse complications at an early stage, but not so frequent that it becomes an inconvenience for the patient and they simply do not attend. In the early days of soft contact lenses, a more frequent approach was taken in the regularity of aftercare appointments since little was known about the long-term effects of lens wear. Current practice has evolved such that an initial aftercare is usually conducted one to two weeks after initially dispensing a soft contact lens to the patient for a trial. This will differ for extended wear patients who would normally be seen for an appointment the morning after their first night of sleeping in lenses, along with after one week and one month of continuous wear. Check-ups at these points allow the practitioner to ascertain whether the lenses are being handled and cared for correctly, and in accordance with the given instructions. It also allows lens performance with respect to vision, fit, comfort and ocular health to be verified to ensure this is in line with both the patient and practitioner’s expectations.
Following on from this initial aftercare, assuming both patient and practitioner are happy with the lens performance and patient compliance, the current guidance by the College of Optometrists is for all subsequent contact lens check-ups to be scheduled according to the patient’s clinical needs.12 This is in agreement with guidance issued by the Association of British Dispensing Opticians, which states that the frequency of contact lens aftercares should be based on the eye care practitioner’s professional judgement of the patient’s clinical needs, the type of contact lens worn, the modality of wear and judgement of the risk of an adverse event occurring.13
A review by Efron and Morgan in 201714 proposed frequency of review should be based on lens replacement frequency, lens type, wearing modality and predicated rate of refractive change. Recommendations were for soft daily disposable wearers to be reviewed every 24 months, based on a lower risk of keratitis, for soft reusable and rigid daily wearers to be reviewed every 12 months, enabling greater monitoring of compliance and for those in soft and rigid extended wear contact lenses to be seen every six months due to higher risk of keratitis. Based upon refractive change, it was advised young myopes (five to 15 years) should be monitored every six months, and presbyopes every 12 months. Of course, patients should always be reminded that they can return for a review sooner if they have any concerns.
Summary
The aim of successful contact lens aftercare is to check a patient’s ocular response to contact lens wear, ensure vision and comfort are optimal and to review compliance. Clear communication throughout the appointment is vital, as well as a systematic routine to ensure nothing is missed. Personalised recommendations should always be given at the end of the examination, ensuring that the patient is aware of the reasons for any changes in care needed. The importance of aftercare for the maintenance of eye health and comfort should be reinforced at every visit so that the patient appreciates the value of regular review.
Dr Sandeep Dhallu is an Optometrist and Senior Lecturer at the University of Hertfordshire and a paid consultant for the Johnson & Johnson Institute, UK. Dr Rachel Hiscox is a Professional Education & Development Manager, UK & Ireland for Johnson & Johnson Vision Care.
- This article is part of a revised and updated ‘Essential Contact Lens Practice’ series, originally authored by Jane Veys, John Meyler and Ian Davies. This article was produced without further input or review from the original authors.
References
- Dumbleton K, Caffery B, Dogru M, Hickson-Curran S, Kern J, Kojima T, Morgan PB, Purslow C, Robertson DM, Nelson JD. The TFOS International Workshop on Contact Lens Discomfort: report of the subcommittee on epidemiology. Investigative ophthalmology & visual science. 2013 Oct 1;54(11):TFOS20-36.
- Wolffsohn JS, Drew T, Dhallu S, Sheppard A, Hofmann GJ, Prince M. Impact of soft contact lens edge design and midperipheral lens shape on the epithelium and its indentation with lens mobility. Investigative Ophthalmology & Visual Science. 2013 Sep 1;54(9):6190-6.
- Morgan PB, Efron N, Toshida H, Nichols JJ. An international analysis of contact lens compliance. Contact Lens and Anterior Eye. 2011 Oct 1;34(5):223-8.
- Efron N, Morgan PB. Rethinking contact lens aftercare. Clinical and Experimental Optometry. 2017 Sep;100(5):411-31.
- Davies IP, Inglis A, Davies G. Correlation between visual acuity and visual quality in contact lens practice. The Journal of the British Contact Lens Association. 1992 Jan 1;15(4):155-7.
- Young G. Soft lens design and fitting. Contact Lens Practice, 2nd ed. Oxford, UK: Butterworth-Heinemann. 2010 Mar 10:109-8.
- Wolffsohn JS, Hunt OA, Basra AK. Simplified recording of soft contact lens fit. Cont Lens Anterior Eye. 2009 Feb;32(1):37-42.
- Efron N. Contact lens complications. Elsevier; 2019.
- Stapleton F, Keay L, Edwards K, Naduvilath T, Dart JK, Brian G, Holden BA. The incidence of contact lens–related microbial keratitis in Australia. Ophthalmology. 2008 Oct 1;115(10):1655-62.
- Holden BA, Mertz GW. Critical oxygen levels to avoid corneal edema for daily and extended wear contact lenses. Invest Ophthalmol Vis Sci. 1984;25:1161-1167
- Wolffsohn JS, Naroo SA, Christie C, Morris J, Conway R, Maldonado-Codina C. Anterior eye health recording. Contact Lens and Anterior Eye. 2015 Aug 1;38(4):266-71.
- The College of Optometrists. Guidance for Professional Practice. Available from: https://guidance.college-optometrists.org/guidance-contents/knowledge-skills-and-performance-domain/contact-lens-check-ups. Accessed 23rd February 2021
- ABDO. Press release: ABDO updates guidance on contact lens aftercare frequency. Available from https://www.abdo.org.uk/about-us/media-centre/press-release-abdo-updates-guidance-on-contact-lens-aftercare-frequency/ Accessed 23rd February 2021
- Efron N, Morgan PB. Rethinking contact lens aftercare. Clin Exp Optom, 2017;100(5):411-431.
