Normal colour perception requires clear media, healthy retinal photoreceptors and a normal functioning of the optic nerves and brain. Systemic conditions and diseases of the eye and central nervous system have the potential to negatively affect colour perception. This article describes some of these conditions along with practical examples of how colour vision impairment can impact life choices and functioning.
Congenital colour vision deficiency classification
Congenital hereditary colour vision deficiency is the most common type of colour vision deficiency and affects around 8% of men and 0.5% of women.1 It is usually classified by severity, and further subdivided into various types dependent upon the nature of the cone receptors affected. Three different classes of photopsins in the cones react to different ranges of light wavelength and frequency; one set sensitive to red, one to green and one to blue.2 The three types of cone photoreceptor allow trichromatic vision based around variable ratios of the three for different object perception. Colour deficiency results when one or more of the three receptor types does not function fully or is absent altogether. Patients with colour defects of the various types may be described as follows:
- Anomalous trichromat; one of three pigments functions at a reduced level to normal resulting in reduced sensitivity to the wavelength for which the receptor is normally attuned. The three types of anomalous trichromats are;
- Protanomaly; reduced red sensitivity
- Deuteranomaly; reduced green sensitivity
- Tritanomaly; reduced blue sensitivity
- Dichromat; one cone type is absent altogether and which one dictates the type of dichromacy;
- Protanope; red receptor absent
- Deuteranope; green receptor absent
- Tritanope; blue receptor absent
- Monochromat; colour discrimination is usually absent1
Table 1 provides an overview of the different types of hereditary colour vision deficiencies. A discussion of the various tests for colour deficiencies falls outside the scope of this article, but are well covered in the literature.2
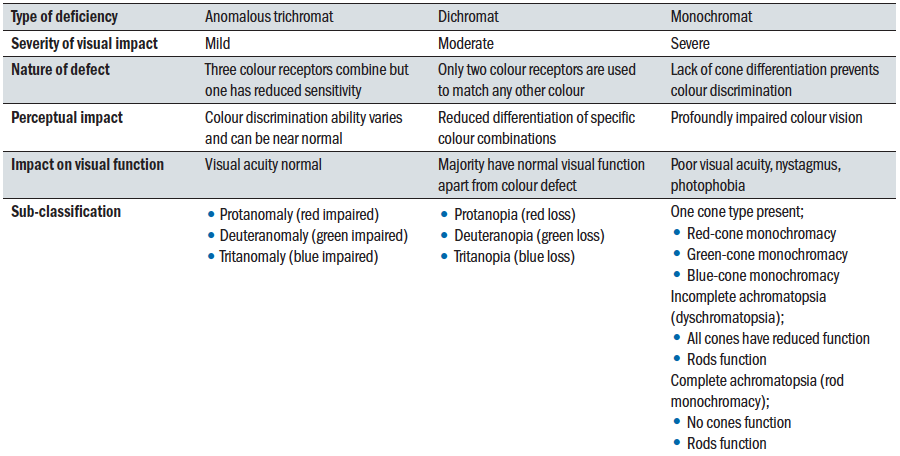 Table 1: Comparison of congenital colour deficiencies
Table 1: Comparison of congenital colour deficiencies
Impact of congenital colour vision deficiency
All too often, explanations of the nature of colour deficiency reflect very poorly what the sufferer actually experiences in everyday life. To avoid this, it is useful for eye care professionals to use some of the many available resources, such as the simulations offered online by Colour Blind Awareness (figure 1) or the RNIB (figure 2).
 Figure 1: A multicolour image as seen by (a) a trichromat, (b) a deuteranope, (c) a protanope and (d) a tritanope. Note the great similarity of (b) and (c). Simulations available at www.colourblindawareness.org
Figure 1: A multicolour image as seen by (a) a trichromat, (b) a deuteranope, (c) a protanope and (d) a tritanope. Note the great similarity of (b) and (c). Simulations available at www.colourblindawareness.org
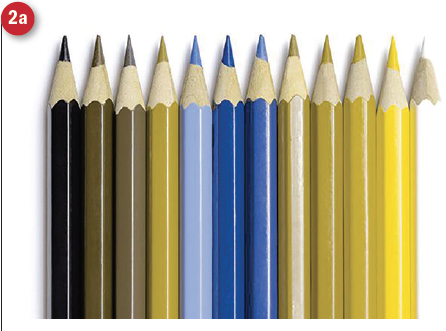
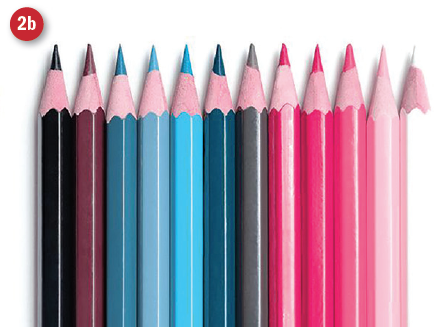
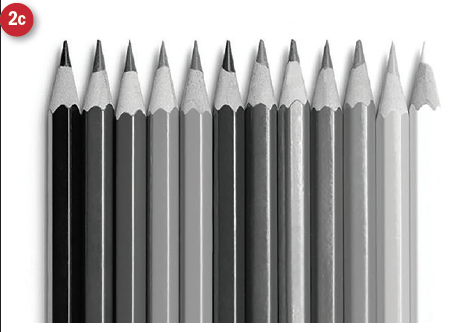 Figure 2: Coloured pencils as seen by (a) deuteranope, (b) tritanope and (c) monochromat. Images from www.rnib.org.uk
Figure 2: Coloured pencils as seen by (a) deuteranope, (b) tritanope and (c) monochromat. Images from www.rnib.org.uk
Another excellent resource is the free Chromatic Vision Simulator app. Once downloaded to a smartphone or tablet, this app allows you to take any image with the camera and see what it would look like for a dichromat of each type (figure 3).
 Figure 3: Images taken using the Chromatic Vision Simulator app showing the view of (a) a cat and (b) Optician as seen with normal colour vision (C), protanopia (P), deuteranopia (D) and tritanopia (T)
Figure 3: Images taken using the Chromatic Vision Simulator app showing the view of (a) a cat and (b) Optician as seen with normal colour vision (C), protanopia (P), deuteranopia (D) and tritanopia (T)
Colour vision deficiency and ocular disease
Ocular media
Conditions affecting the ocular media, such as cataract, affect colour perception,3,4 with colours typically appearing ‘washed out’. Crystalline lens brunescence, or yellowing, with age prevents shorter blue wavelengths from reaching the retina.
AMD
Colour vision impairment occurs in dry age-related macular degeneration (AMD), the severity of which is related to that of the disease.5 However, although dyschromatopsia has been identified as a feature of neovascular (wet) AMD,6 it is unclear if achromatopsia increases the risk of neovascular AMD.7
Receptor dystrophies
Cone and rod-cone dystrophies form a group of conditions that can be stationary or progressive and typically present in childhood or early adulthood. Symptoms vary in severity and include reduced vision, reduced colour perception and photophobia.8 Examples of such conditions include:
- Stargardt disease
- X-linked retinoschisis
- Best disease
- Pattern dystrophies
- Central areolar choroidal dystrophy9
- Macular dystrophy
- Retinitis pigmentosa10
Glaucoma
Damage to the retinal nerve fibre layer (RNFL) can result in colour vision impairment in glaucoma patients. Glaucoma can lead to all types of colour vision deficiency, with tritanomalous defects being far the most common.11 Combined blue-yellow and red-green confusion is most commonly associated with temporal RNFL defects in glaucoma.12 Glaucoma patients with reduced visual acuity are more likely to have difficulties with identifying green and orange bottle cap colours.13
Diabetic retinopathy
Neuroretinal dysfunction in (pre)diabetes with an associated colour vision dysfunction often occurs in diabetes before the onset of retinopathy.14,15 Diabetic patients typically have a blue-yellow defect16,17 and develop more severe dyschromatopsia with red-green colour vision defects later on as the disease progresses.17,18
Optic neuropathies
Optic nerve diseases usually present with the following signs:19,20
- Visual loss
- Dyschromatopsia
- Visual field defects
- Relative afferent pupillary defect
- Disc swelling or optic atrophy
- Loss of retinal volume
Dyschromatopsia usually persists, even when visual acuity has recovered.21 Examples of acute optic neuropathies include:22
- Optic neuritis
- Ischaemic optic neuropathy (figure 4)
- Inflammatory (non-demyelinating) disorders
- Trauma
Examples of causes of chronic or subacute optic nerve disease include:22
- Compression
- Toxicity
- Nutritional deficit
- Hereditary-genetic anomalies
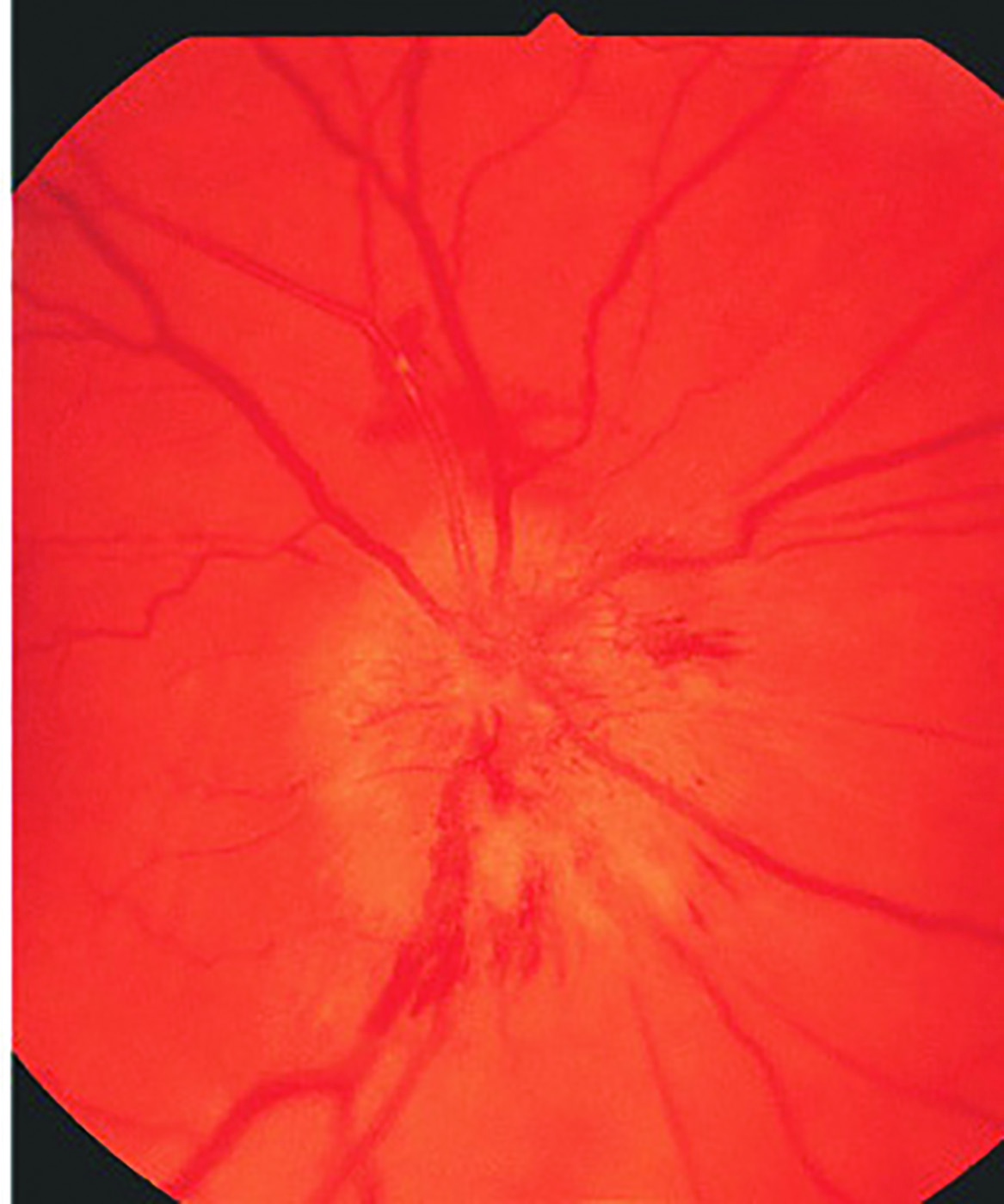 Figure 4: Anterior ischaemic optic neuropathy may result in dyschromatopsia
Figure 4: Anterior ischaemic optic neuropathy may result in dyschromatopsia
Nerve damage as a result of compression can occur in Graves’ orbitopathy.23 An example of a hereditary condition is Leber’s hereditary optic neuropathy, which usually presents with sudden visual loss, red-green dyschromatopsia and a central or centrocoecal scotoma.24 Optic neuritis is common in multiple sclerosis (MS), and is often the first detected sign. However, colour vision impairment can also occur in MS in the absence of optic neuritis25 and in the absence of visual complaints.26 Red-green colour vision deficiency (parvocellular) and blue-yellow colour vision deficiency (koniocellular) are both found in MS.27,28 Colour confusion is correlated with clinical and paraclinical features of MS.29 There are indications that the type of colour vision deficiency to manifest depends upon the stage of MS progression. Colour deficiency in MS is associated with reduced peripapillary RNFL thickness and reduced cognitive performance.30
Toxicity
Finally, colour vision dysfunction may result as a side effect of certain drugs, such as hydroxychloroquine31 and tamoxifen.32 Alcohol consumption can also lead to colour vision deficiency.33
Colour vision deficiency and central nervous system disease
Colour vision impairment due to brain damage does not follow the specific patterns that are typical of colour vision dysfunction due to congenital photoreceptor disorders. Colour vision impairment is associated with damage to the occipital cortex.34,35
Colour processing is a complex task that involves colour perception, colour naming and knowledge about typical colours for specific objects. Table 2 summarises some of the terminology used to describe colour vision impairments associated with brain injury. Although the Ishihara colour vision test is a helpful tool for detecting congenital colour vision impairment (figure 5), and is widely used in optometric practice, it is less useful for acquired defect detection and it may be more appropriate to measure
colour saturation thresholds for acquired colour vision impairments.36 Colour vision impairments can occur due to pre- peri- or post-natal complications or may be acquired later in life.
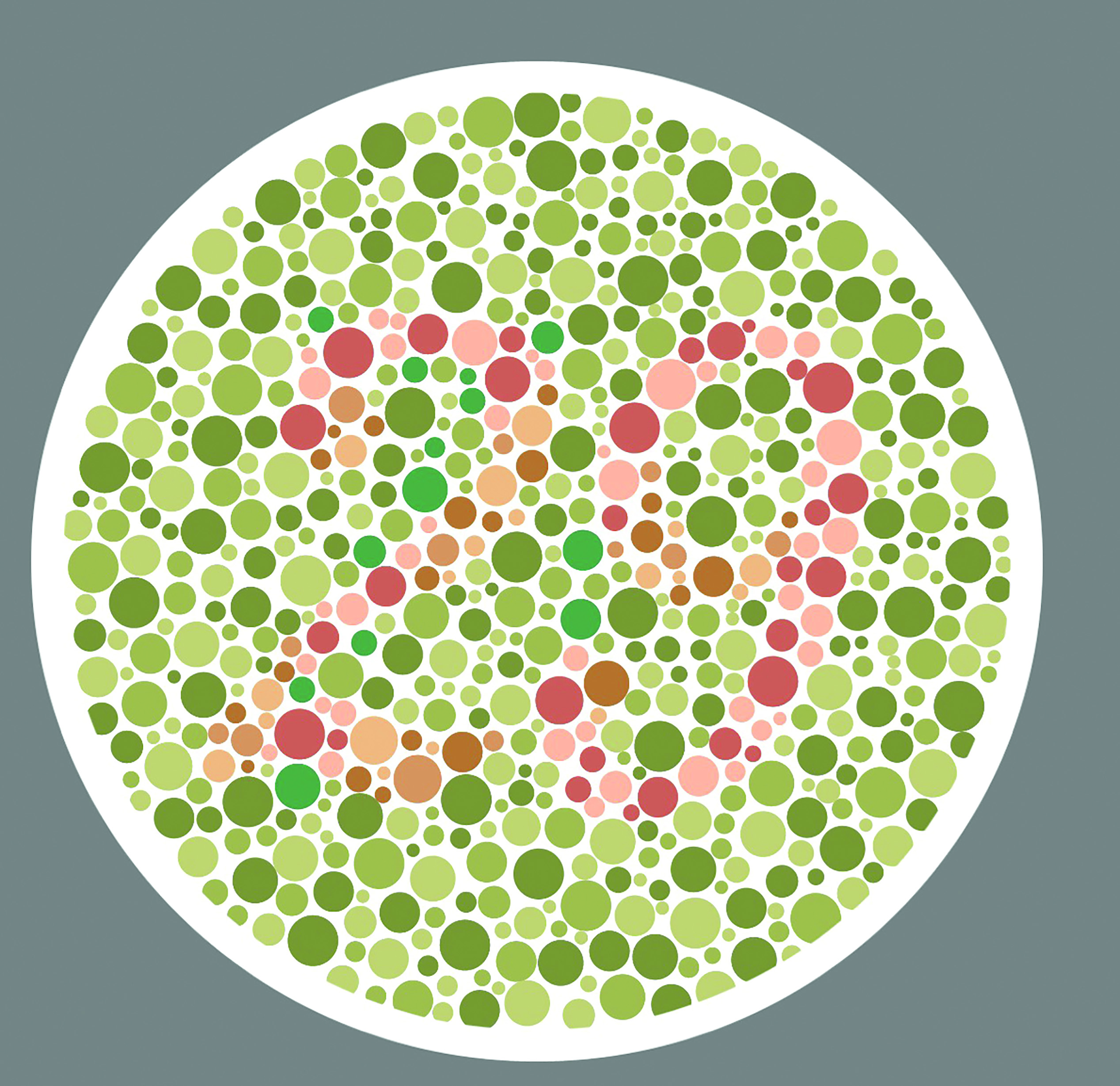 Figure 5: Ishihara is sensitive for screening for congenital
Figure 5: Ishihara is sensitive for screening for congenital
colour defects but less useful for acquired defects.
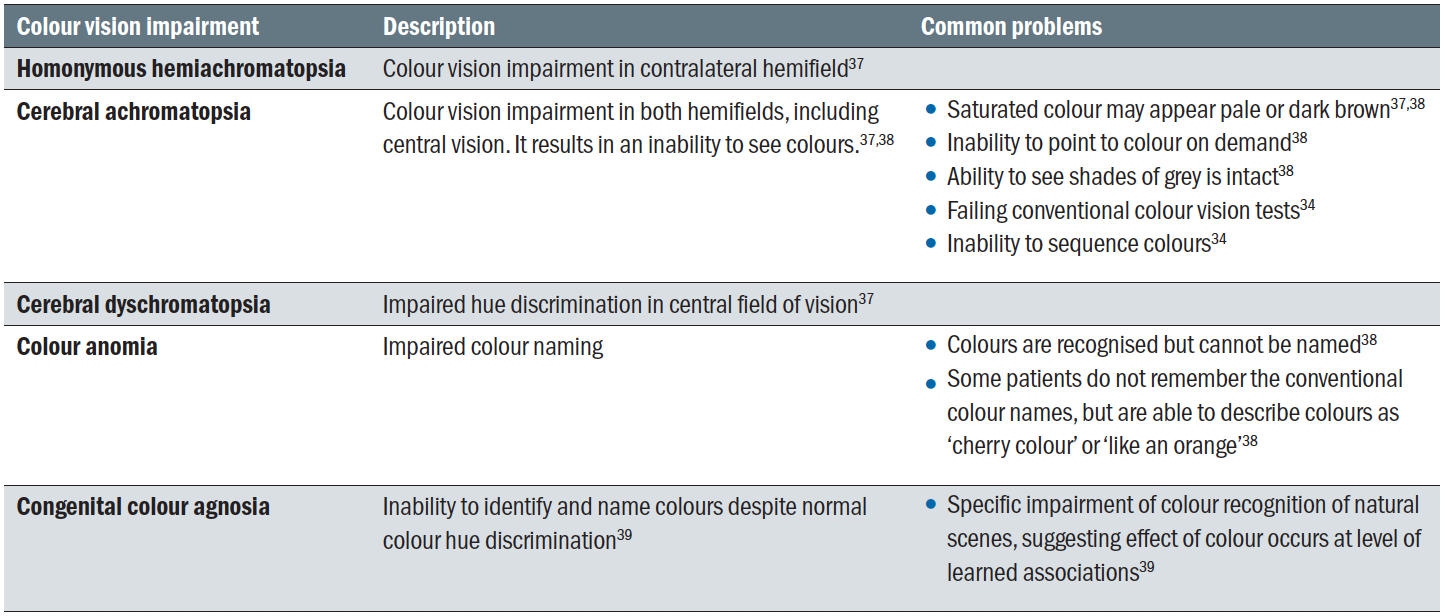 Table 2: Colour vision impairment due to brain injury
Table 2: Colour vision impairment due to brain injury
Cerebral visual impairment
Colour vision impairment is one of many possible features of cerebral visual impairment.37 In normally sighted children, the concept of colours is usually learned from a young age as the child explores their visual scene and receives feedback from their parents and other people.
Children with visual impairment often find it more difficult to understand the abstract concept of colours. This can result in an inability to name colours and sometimes gives the impression the child cannot discriminate certain colours. For a child who does not understand the concept of colours, it can be helpful to teach them by associating colours with specific objects, whereby the object is named before the colour. For example, ‘grass-green pencil’, ‘sky-blue T-shirt’ and so on. This technique of attaching the colour pronoun to the colour of the object is very well explained on the CVI Scotland website (www.cviscotland.org).
Low birth weight is associated with colour vision deficiency, particularly blue-yellow deficits that are found in 2.5% of pre-term infants.40 Interestingly, attention-deficit hyperactivity disorder (ADHD) is more common in children who were born prematurely, and blue-yellow deficits are more common in children with ADHD compared to healthy children. Both colour naming and colour discrimination are affected in ADHD.41
Complications before, during or after birth can cause cerebral palsy. Spastic cerebral palsy is associated with impaired colour perception, which tends to be worse in children with tetraplegia as compared to hemiplegia.42 Hydrocephalus is another perinatal condition associated with visual impairment and affecting the higher processing pathway. Patients can experience difficulties with colour naming and matching.43
Stroke and acquired brain injury
Brain injury can cause colour vision impairment. A case study of a patient who suffered a bilateral stroke of the posterior cerebral arteries described initial achromatopsia, which partially recovered after three years.44 Zhou et al45 described a patient with complete achromatopsia after an ischaemic stroke involving the occipital-temporal cortex. Jakobson et al47 described a case whereby a patient had hue-specific colour memory impairment with intact colour vision and colour naming. This case confirms that colour naming, colour memory and colour discrimination can be clinically dissociated.
Dementia
Dementia is an umbrella term for a number of conditions that lead to brain damage, causing cognitive decline, communication difficulties and memory loss. The most common subtypes are Alzheimer’s disease, vascular dementia, disease with Lewy bodies (DLB), frontotemporal dementia and mixed dementia48 It is thought that colour vision is affected in different ways, depending on the type of dementia. Some studies suggest that colour vision impairment is more commonly found in DLB compared to Alzheimer’s disease.48,49 Furthermore, impaired colour vision in DLB is associated with visual hallucinations and impaired visuospatial function.50 Colour vision tests, preferably the 15-hue tests, may be a useful and simple tool for early diagnosis and differentiation between the two conditions (figure 6).
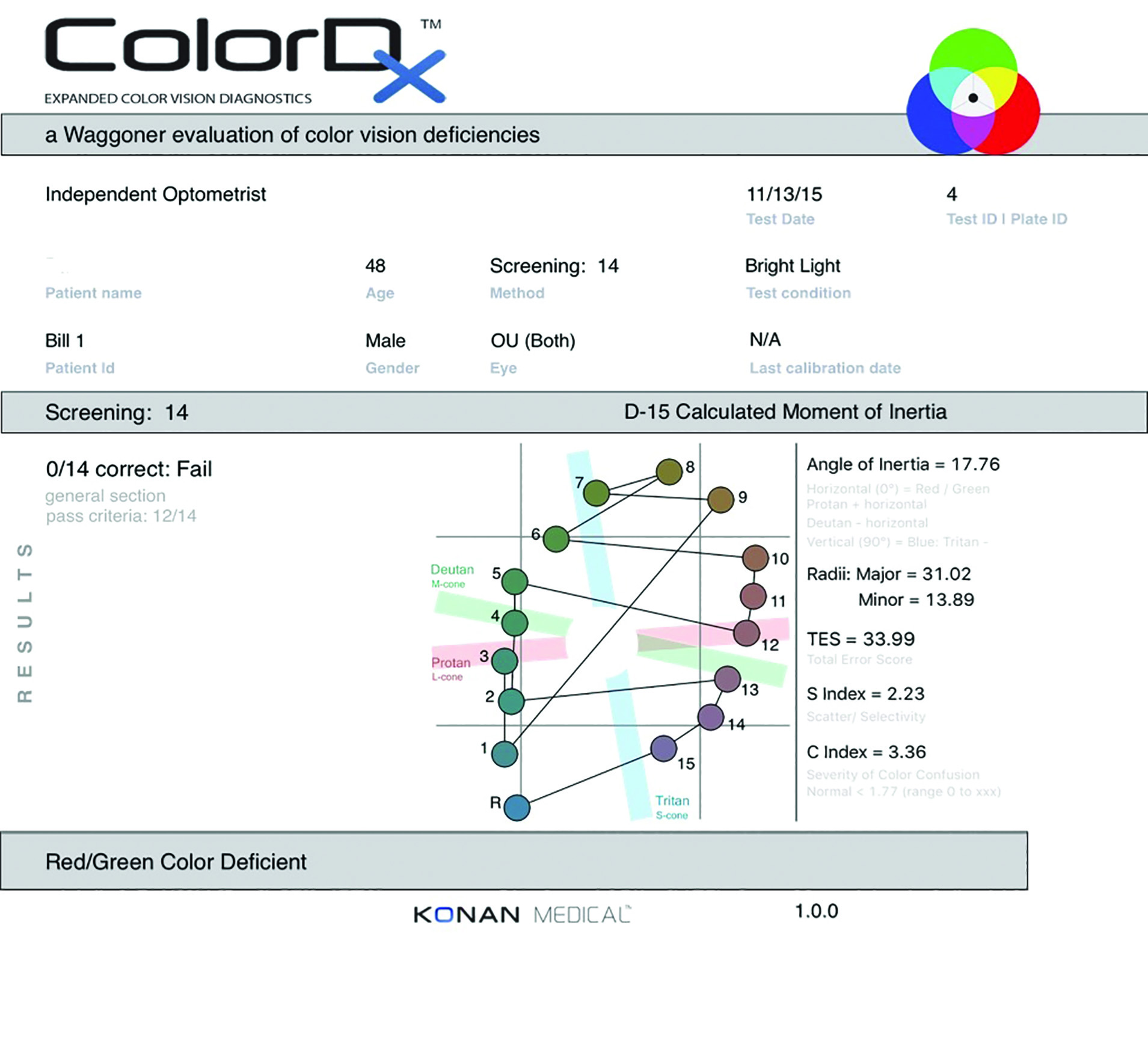 Figure 6: 15-hue tests are preferred when assessing colour loss in dementia
Figure 6: 15-hue tests are preferred when assessing colour loss in dementia
Living with colour vision impairment
In terms of everyday functioning, colour vision deficiencies can lead to varying degrees of difficulty. In protan and deutan colour vision deficiency (protanomaly, deuteranomaly, protanopia and deuteranopia), one may have difficulties in distinguishing between red, orange, yellow brown and green or between red and black or shades of purple and these colours may appear duller. Blues, greens and yellows are more commonly confused in tritan colour vision deficiency (tritanomaly and tritanopia).
Colour vision deficiency may lead to functional impairment. Stoianov et al51 identified seven areas in which colour vision can affect a person’s life and these are summarised in table 3.
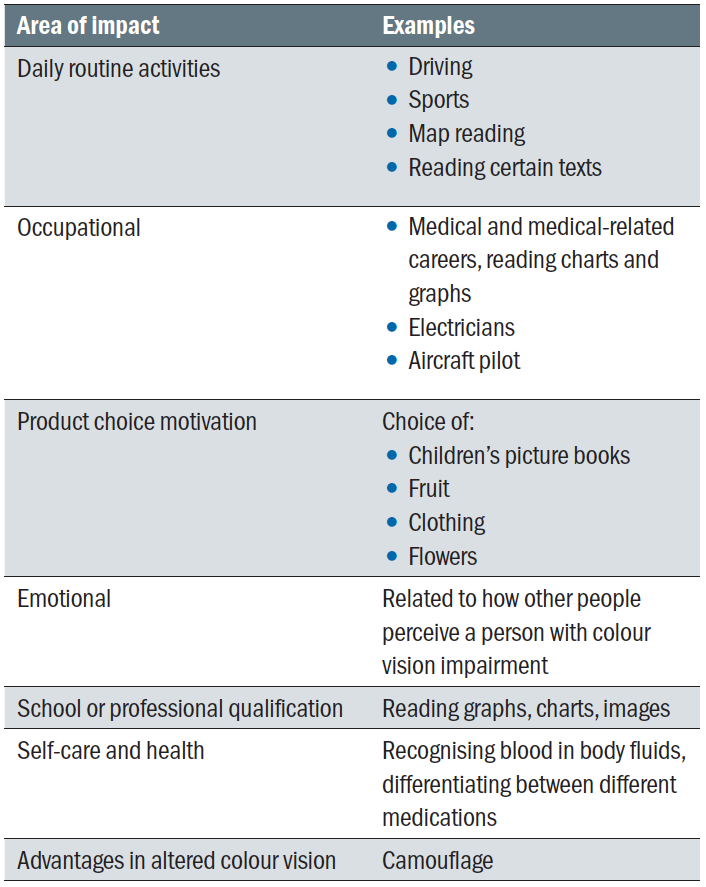 Table 3: Impact of colour vision impairment on different areas of life51
Table 3: Impact of colour vision impairment on different areas of life51
Patients are likely to experience some difficulties in daily routine activities, such as reading labels on food packages with coloured print and background. Driving is another area of difficulty as the colours of traffic lights and rear lights can be difficult to distinguish, though sequencing and variable intensity help overcome these challenges. Although one can hold a driving licence with colour vision deficiency, rear-end collisions are more common in people with protanomaly (Cole 2002).52
A number of professions state a minimum requirement for colour vision standards (see table 4). There are no formal standards for either working in a laboratory or as a medical doctor in the UK. Working in a laboratory and interpreting colour change or as a doctor looking at retinal images, skin colour nuances or test strips may result in misinterpretations. Whether specific specialities within medicine should meet a standard for colour discrimination or if workplace adaptations are sufficient to reduce the risk of clinical errors due to colour vision impairment is a topic of ongoing debate.53
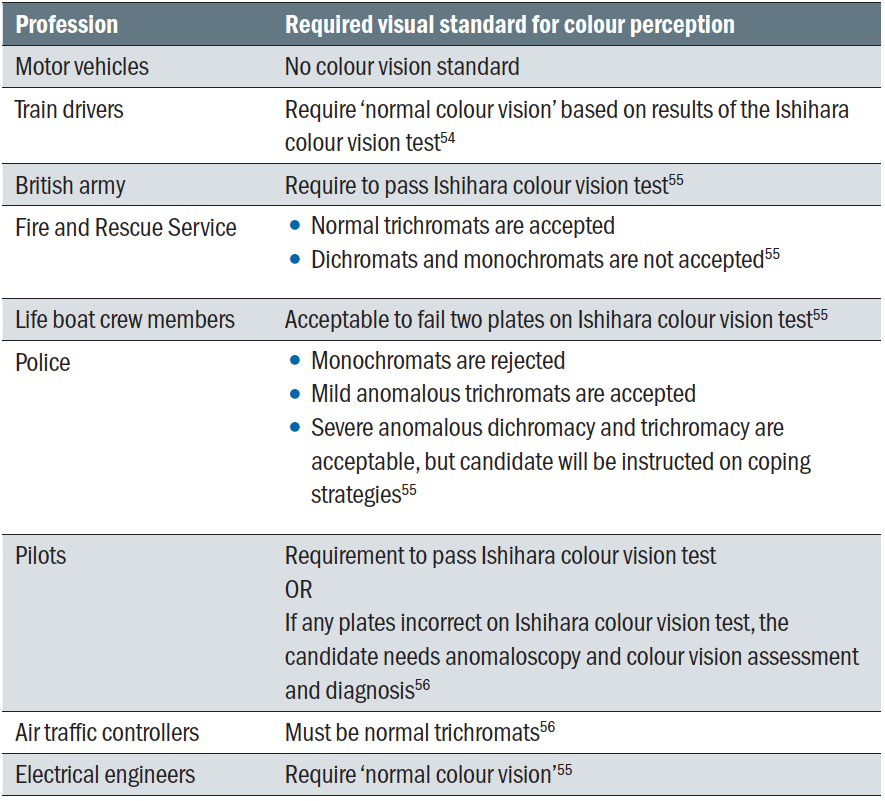 Table 4: Colour vision standards for professions
Table 4: Colour vision standards for professions
Colour vision impairment may also translate into difficulties at school and university where colour-coding is regularly used for learning activities. The interpretation of graphs and maps can be affected. Some people experience emotional impact from negative attitudes of peers about colour vision impairment. The choice of clothes, picture books and toys can be influenced by impaired colour perception.
In terms of health and well-being, a colour vision impairment can make it difficult to distinguish if fruit is ripe and if meat is cooked. For people using multiple medications, extra care needs to be taken to label different medications to avoid confusion if colour differences on packages or bottle caps are not perceived.
Educating patients about their colour vision deficiency means they can make informed (career) choices and adapt their environment in such a way that the visual scene is optimised. Despite obvious benefits colour vision is no longer routinely tested as part of pre-school screening.57
Consider the following two scenarios.
Case scenario 1. Achromatopsia
A girl aged 12 attended the low vision clinic with a history of achromatopsia caused by a mutation of the CNGA3 gene. In this condition, logMAR visual acuity is typically around 0.78±0.14.58 Achromatopsia can be complete or incomplete, depending on whether all cone receptors are affected. Colour vision tests show a rod-dominated function when the achromatopsia is complete. In incomplete achromatopsia, there can be residual colour discrimination due to the interaction between rods and cones1 and visual acuity tends to be better than in complete achromatopsia.59 Other typical features of this condition are nystagmus and
photophobia.1,58,60
This girl presented with a binocular logMAR acuity of 0.70 (6/30 Snellen) when wearing glasses for myopia and astigmatism. She had mild nystagmus and severe photophobia, for which she had been wearing prescription sunglasses.
She failed all plates on the Ishihara colour vision test. However, her dad was convinced that she used to be able to distinguish blue from pink as a toddler. The parents used to give the girl and her twin brother identical toys, a pink one for the girl and a blue one for her brother and she always knew exactly which toy belonged to her. It is possible that she has some residual colour vision that is not picked up with the Ishihara colour test. Alternatively, the pink and blue toys may have been perceived as different shades of grey.
The dad found it hard to imagine what the world looked like for his daughter and how he could improve the visual scene. It was explained to him that his daughter essentially saw the world in shades of grey, just like an old black-and-white television with poor definition. He was encouraged to take black-and-white photos in and around the house in order to appreciate what these scenes looked like for his daughter in terms of shades of grey. He could then start thinking about removing clutter or using different colour schemes to make items stand out more for his daughter.
At school, this girl was being supported by her qualified teacher for the visually impaired (QTVI), who had made adjustments in terms of classroom position, enlarged learning material and ensuring the girl was allowed extra time to complete tasks. In physical education lessons, appropriate bibs were used that were perceived as different shades of grey. Although she was using a tablet at school, she was keen to start using a bar magnifier as well. A monocular was issued to allow her to see items of interest from across the other side of the classroom and for navigation outside.
There is currently no treatment for achromatopsia. However, several studies are offering some initial hope for possible future gene therapies.61-63 One of these studies suggests that early intervention in childhood is essential for a good clinical outcome.62
Case scenario 2. Childhood multiple sclerosis
A girl aged 10 with a history of optic atrophy and reduced vision due to multiple sclerosis struggled with her schoolwork. Her logMAR acuity had dropped to 1.08 (Snellen equivalent <6/60) in her right eye and 1.28 (count fingers) in the other eye. Only a small area of vision remained in the upper left quadrant. She failed all plates on the Ishihara colour test and her contrast sensitivity was significantly reduced.
At school and at home, she had access to a tablet that allowed her to enlarge her learning material. However, she struggled to concentrate and complete tasks in the expected time frame. She felt that the teacher was asking her to complete impossible tasks. On one occasion, she was asked to create a colourful piece of art and the teacher did not understand why this had been so difficult. After explaining the colour vision impairment in clinic, this episode made a lot more sense.
At home, her parents had bought her an attractive and colourful desk mat for her home learning, which led to a lot of frustration as the girl was unable to locate her pens, pencils,
rubbers and other items. She simply thought her vision was getting worse and had not realised that her colour contrast was impaired, which caused the objects to blend in with the background. When this was explained to her, she was able to de-clutter her desk and use plain surfaces in order to make the objects stand out.
A report was written to inform the teacher and the family about the specific aspects of her sight impairment, so that adaptations could be made in the learning environment.
Management
In some cases, such as cataract, it is possible to improve colour vision by treating the underlying condition. However, treatment options for hereditary dyschromatopsia are limited. Gene therapy to improve cone function could potentially improve visual acuity, colour discrimination and reduce photophobia in patients with genetic achromatopsia in future.60 In the meantime, a number of companies have developed special tinted lenses with the intention of enhancing colour discrimination for people with protan and deutan colour vision deficiency. It appears that such filters change the appearance of colours without actually improving overall colour discrimination.64
In situations where colour vision cannot be improved with medical intervention, one can manage the patient in a different way. The first step is to explain the causative condition so that the patient understands the underlying problem. Information and advice are especially important for patients in education and patients considering career options. Practical tips, such as reducing clutter, the use of contrast and lighting and strategic positioning to avoid glare, can make a significant difference to some patients. Advice about colour identification apps to assist in everyday situations, such as preparing food and getting dressed, can also be helpful.
Conclusion
Optometrists are likely to encounter colour vision impairment on a regular basis. This article has shown that colour vision testing is relevant for diagnosis and management of ocular and neurological conditions as well as screening for congenital colour defects.
The impact of colour vision impairment can be significant. However, with the right advice and support, patients can reach their full potential. The eye care practitioner is well placed to initiate discussions about colour vision impairment as this can help the patient to make life and career choices. It can also help in terms of adapting the environment to optimise functional vision.
- Cirta Tooth is a hospital optometrist based in Edinburgh with a special interest is low vision and functional vision.
References
- Simunovic MP. (2010). Colour vision deficiency. Eye, 24, pp.747-755
- Harvey W, Doshi S. Eye Essentials; Investigative Techniques. Chapter 2, 2005, Butterworth Heinemann
- Delbarre M and Froussart-Maille F. (2020). Signs, symptoms, and clinical forms of cataract in adults. Journal Francais d’Ophthalmologie 43(7), pp.653-659
- Langina-Jansone Z, Truksa R and Ozolinsh M. (2020). Visual acuity and color discrimination in patients with cataract. Journal of the Optical Society of America A-Optics Image Science and Vision 37(4), pp.A212-A216
- Lott, LA, Schneck ME, Haegerstrom-Portnoy G et al. (2020). Simple visual function tests that distinguish eyes with early to intermediate age-related macular degeneration. Ophthalmic Epidemiology [Online]. https://doi.org/10.1080/09286586.2020.1793371
- Hessellund A, Larsen DA and Bek T. (2012). The predictive value of subjective symptoms and clinical signs for the presence of treatment-requiring exudative age-related macular degeneration. Acta Ophthalmologica 90(5), pp.471-475
- Calcagni A, Howells O, Eperjesi F et al. (2020). Colour contrast sensitivity in eyes at high risk of neovascular age-related macular degeneration. European Journal of Ophthalmology 30(6), pp.1487-1494
- Gill JS, Georgiou M, Kalitzeos A et al. (2019). Progressive cone and cone-rod dystrophies: clinical features, molecular genetics and prospects for therapy. British Journal of Ophthalmology 103(5), pp.711-720
- Kellner U, Jandeck C, Kraus H et al. Hereditary macular dystrophies. (1998). Ophthalmologe, 95(9), pp.597-601
- Huchzermeyer C, Fars J, Stoehr H et al. (2020). New techniques for quantification of color vision in disorders of cone function Cambridge color test and photoreceptor-specific temporal contrast sensitivity in patients with heterozygous RP1L1 and RPGR mutations. Ophthalmologe;118(2):144-153
- Bayer L, Funk J and Toeteberg-Harms M. Incidence of dyschromatopsy in glaucoma. International Ophthalmology 40(3), pp.597-605
- Yum HR, Hae-Young L and Park CK. (2020). Characteristics of normal-tension glaucoma patients with temporal retinal nerve fibre defects. Scientific Reports 10(1). Article Number 6362
- Paul J, Hammer JD, Akhtari R et al. (2019). Effect of glaucoma on identification of bottle cap color in ophthalmic medications. International Journal of Ophthalmology 12(1), pp.169-171
- Neriyanuri S, Pardhan S, Gella L et al. (2017). Retinal sensitivity changes associated with diabetic neuropathy in the absence of diabetic retinopathy. British Journal of Ophthalmology 101(9), pp.1174-1178
- Tan NC, Yip WF, Kallakuri S et al. (2017). Factors associated with impaired color vision without retinopathy amongst people with type 2 diabetes mellitus: a cross-sectional study. BMC Endocrine Disorders 17. Article Number 29
- Gella L, Raman R, Kulothungan V et al. (2017). Colour vision abnormalities in type II diabetes: Sankara Nethralaya Diabetic Retinopathy Epidemiology and Molecular Genetics Study II report no 2. Indian Journal of Ophthalmology 65(10), pp.989-994
- Piro A, Tagarelli A, Lagonia P et al. (2019) Color vision study to assess the impaired retina-brain cortex pathway in type 2 diabetes: a pilot study in Calabria (Southern Italy), Neurological Sciences 40(9), pp.1939-1942
- Karson N, Smith J, Jones M et al. Functional retinal outcomes in patients with prediabetes and type 2 diabetes. Ophthalmic and Physiological Optics 40(6), pp.770-777
- Buompadre CM. (2013). Acute optic neuropathy: differential diagnoses. Revista de Neurologia 57(1), pp.S139-S147
- Levin N, Devereux M, Bick A et al. (2019). Color perception impairment following optic neuritis and its association with retinal atrophy. Journal of Neurology 266(5), pp.1160-1166
- Slamovits TL, Rosen CE, Cheng KP et al. (1991). Visual recovery in patients with optic neuritis and visual loss to no light perception. American Journal of Ophthalmology 111(2), pp.209-214
- Mazzurco M, Pavone P, Di Luca M et al. (2019). Optic neuropathy, secondary to ethmoiditis, and onodi cell inflammation during childhood: a case report and review of the literature. Neuropediatrics 50(6), pp.341-345
- Tramunt B, Imbert P, Grunenwald S et al. (2019). Sight-threatening Graves’ orbitopathy: Twenty years’ experience of a multidisciplinary thyroid-eye outpatient clinic. Clinical Endocrinology 90(1), pp.208-213
- Priglinger C, Klopstock T, Rudolph G et al. (2019). Leber’s hereditary optic neuropathy. Klinische Monatsblatter fur Augenheilkunde 236(11), pp.1271-1282
- Lampert EJ, Andorra M, Torres-Torres R et al. (2015). Color vision impairment in multiple sclerosis points to retinal ganglion cell damage. Journal of Neurology 262(11), pp.2491-2497
- Sanchez-Dalmau B, Martinez-Lapscina EH, Pulido-Valdeolivas I et al. (2018). Predictors of vision impairment in multiple sclerosis. Plos One 13(4). Article Number e0195856
- Anssari N, Vosoughi R, Mullen K et al. (2020). Selective colour vision deficits in multiple sclerosis at different temporal stages. Neuro-Ophthalmology 44(1), pp.16-23
- Piro A, Tagarelli A, Nicoletti G et al. (2019). Impairment of acquired color vision in multiple sclerosis: an early diagnostic sign linked to the greatness of disease. International Ophthalmology 39(3), pp.671-676
- Barreiro-González A, Sanz MT, Carratalà-Boscà S, Pérez-Miralles F, Alcalá C, España-Gregori E, Casanova B. Dyschromatopsia in multiple sclerosis reflects diffuse chronic neurodegeneration beyond anatomical landmarks. Acta Neurologica Belgique. 2020, Oct 12
- Felgueiras H, Parra J, Cruz S et al. (2016). Dyschromatopsia in multiple sclerosis patients: a marker of subclinical involvement? Journal of Neuro-Ophthalmology 36(3), pp.275-279
- Pluta JP and Ruether K. (2009). Retinal damage by (hydroxy)chloroquine intake: published evidence for an efficient ophthalmological follow-up. Klinische Monatsblatter fur Augenheilkunde 226(11), pp.891-896
- Ritter C, Renner AB, Wachtlin J et al. (2008). Tamoxifen retinopathy: a case series of clinical and functional data. Ophthalmology 105(6), pp.544-549
- Brasil A, Castro AJO, Martins ICVS et al. (2015). Colour vision impairment in young alcohol consumers. Plos One 10(10). Article Number e0140169
- Cowey A and Heywood CA. (1995). There’s more to colour than meets the eye. Behavioural Brain Research 71(1-2), pp.89-100
- Houlsiton MJ, Taguri AH, Dutton GN et al. (1999). Evidence of cognitive visual problems in children with hydrocephalus: a structured clinical history-taking strategy. Developmental Medicine and Child Neurology 41(5), pp.298-306
- Heinrich SP and Hoffmann MB. (2018). Visual acuity, contrast sensitivity, colour vision: thoughts on psychophysical exams in neuro-ophthalmology. Klinische Monatsblatter fur Augenheilkunde 235(11), pp.1212-1217
- Zihl, Joseph; Dutton, Gordon N. 2015. Cerebral visual impairment in children. Wien: Springer-Verlag
- Pagani R, Bosco G, Dalla Valle E et al. (2012). The assessment of colour perception, naming and knowledge: a new test device with a case study. Neurological Sciences 33(4), pp.801-809
- Nijboer TCW, van Zandvoort MJE and de Haan EHF. (2007). A familial factor in the development of colour agnsia. Neuropsychologia 45(8), pp.1961-1965
- O’Connor AR and Fielder AR. (2007). Visual outcomes and perinatal adversity. Seminars in Fetal and Neonatal Medicine 12(5), pp.408-414
- Banaschewski T, Ruppert S, Tannock R et al. (2006). Colour perception in ADHD. Journal of Child Psychology and Psychiatry 47(6), pp.568-572
- Costa MF and Pereira JC. (2014). Correlations between color perception and motor function impairment in children with spastic cerebral palsy. Behavioral and Brain Functions. 10. Article Number 22
- Houliston MJ, Taguri AH, Dutton GN et al (1999) Evidence of cognitive visual problems in children with hydrocephalus: a structured clinical history-taking strategy. Developmental Medicine and Childhood Neurology, 41:298-306
- Spillmann L, Laskowski W, Lange KW et al. (2000). Stroke-blind for colors, faces and locations: partial recovery after three years. Restorative Neurology and Neuroscience 17(2-3), pp.89-103
- Zhou C, He Y and Li X. (2018). Cerebral achromatopsia secondary to ischemic stroke. Neurology India 66, pp.573-575
- Jakobson LS, Pearson PM and Robertson B. (2008). Hue-specific colour memory impairment in an individual with intact colour perception and colour naming. Neuropsychologia 46(1), pp.22-36
- Dementia UK. (2021). What is dementia? Available at: https://www.dementiauk.org/get-support/diagnosis-and-next-steps/what-is-dementia [Accessed on 14th January 2021]
- Flanigan PM, Khosravi, Leverenz et al. (2018). Color vision impairment differentiates Alzheimers dementia from dementia with Lewy Bodies. Journal of Geriatric Psychiatry and Neurology 31(2), pp.97-102
- Unger RH, Flanigan PM, Khosravi M et al. (2019). Clinical and imaging characteristics with color vision impairment in Lewy Body Disease. Journal of Alzheimers Disease 72(4), pp.1233-1240
- Matar E, Phillips JR, Martens KAE et al. (2019). Impaired color discrimination- a specific marker of hallucinations in Lewy body disorders. Journal of Geriatric Psychiatry and Neurology 32(5), pp.257-264
- Stoianov M, Silva de Oliveira S, Lobato dos Santos Ribeiro Silva et al. (2018). The impacts of abnormal color vision on people’s life: an integrative review. Quality of Life Research 28(4), pp.855-862
- Cole BL. (2002). Protan colour vision deficiency and road accidents. Clinical Experimental Optometry 85(4), pp.246-253
- Thomas PBM, Nesaratnam NMB, Chaudhuri-Vayalambrone PBA et al. (2019). Color vision deficiency among doctors: can we make useful adaptations to the color codes used in the clinical environment? Journal of Patient Safety, available at; https://doi.org/10.1097/PTS.0000000000000611
- UK Government. (2010). The train driving licences and certificates regulations 2010. Available at: https://www.legislation.gov.uk/uksi/2010/724/schedules/made [Accessed on 16th January 2021]
- Association of Optometrists. Vision standards. Available at: https://www.aop.org.uk/advice-and-support/clinical/vision-standards [Accessed on 16th January 2021]
- Civil Aviation Authority. (2015). Colour vision guidance material GM. Available at: https://www.caa.co.uk/Aeromedical-Examiners/Medical-standards/Pilots-(EASA)/Conditions/Visual/Colour-vision-guidance-material-GM [Accessed on 16th January 2021]
- Holroyd E and Hall DMB, (1997). A re-appraisal of screening for colour vision impairments. Child Care Health and Development 23(5), pp.391-398
- Zobor D, Werner A, Stanzial F et al. (2017). The clinical phenotype of CNGA3-related achromatopsia: pre-treatment characterization in preparation of a gene replacement therapy trial. Investigative Ophthalmology and Visual Science 58, pp.821-832
- Ueno S, Nakanishi A, Sayo A et al. (2017). Differences in ocular findings in two siblings: one with complete and other with incomplete achromatopsia. Documenta Ophthalmologica 134(2), pp.141-147
- Hirji N, Aboshiha J, Georgiou M et al. (2018). Achromatopsia: clinical features, molecular genetics, animal models and therapeutic options. Ophthalmic Genetics 39(2), pp.149-157
- Gootwine E, Ofri R, Banin E et al. (2017). Safety and efficacy evaluation of rAAV2tYF-PR1.7-hCNGA3 vector delivered by subretinal injection in CNGA3 mutant achromatopsia sheep. Human Gene Therapy Clinical Development 28(2), pp.96-107
- Hassall MM, Barnard AR and MacLaren RE. (2017). Gene therapy for color blindness. Yale Journal of Biology and Medicine 90(4), pp.543-551
- Pascual-Camps I, Barranco-Gonzalez H, Avino-Martinez J et al. (2018). Diagnosis and treatment options for achromatopsia: a review of the literature. Journal of Pediatric Ophthalmology and Strabismus 55(2), pp.85-92
- Gomez-Robledo L, Valero EM, Huertas R et al. (2018). Do EnChroma glasses improve color vision for colorblind subjects? Optics Express 26(22). Article Number 28682
- Flatla DR, Andrade AR, Teviotdale RD et al. (2015). Colour ID: Improving colour indentification for people with impaired colour vision. 33rd Annual CHI Conference on Human Factors in Computing Systems (CHI), pp. 3543-3552. Seoul, South Korea
