Eye care practitioners are now being increasingly exposed to situations where they can take part in myopia management; this ranges from a conversation about limiting myopia progression through to an active and multimodal approach to myopia management. Research evidence of both the safety and efficacy of myopia management is building rapidly, and it is encouraging to see data from well-controlled studies demonstrating useful levels of myopia management in a range of patients, using a range of interventions (see table 1).
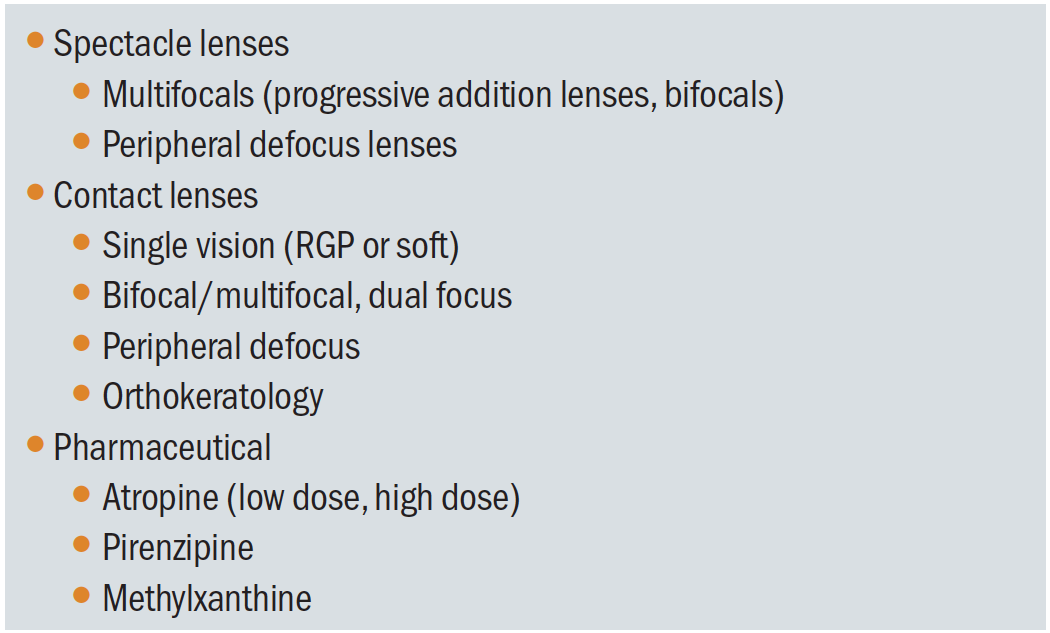 Table 1: Interventions aimed at modifying myopic progression
Table 1: Interventions aimed at modifying myopic progression
What is axial length?
Axial length of the human eye can be defined as the physical distance between the anterior corneal pole and some point within the retinal structure at the posterior pole. It is well understood that the axial length of the eye is a key parameter in determining the refractive status, and growth of the axial length is the most significant structural aspect of myopia progression. Technological advances in axial length measurement over the past two decades have increased accuracy and improved clinical utility.
Why is it important?
The question remains, however, whether the measurement of axial length is an essential tool that practitioners wishing to engage in myopia management must have access to. Clearly, a measurement of the success or otherwise of a myopia management strategy is key to the clinical decision-making process. It is likely that myopia management methods will evolve and be refined over time and the degree to which a tailored management plan, specific to individual patients, may be modified will increase. This might manifest as a patient starting on one given myopia management plan, for example the wearing of a multifocal soft contact lens and being monitored for a given period of time. The patient may subsequently be fitted with an orthokeratology-based intervention while monitoring of any myopia progression is continued. Similarly, a multifocal intervention (spectacle or contact lens-based) could be subtly modified in terms of the power of the near addition, with a view to minimise myopia progression.
In these scenarios, using the spectacle refraction as a primary outcome measure for myopia progression, particularly over the short term, has limitations in terms of repeatability. The variability of refraction measurements (generally assumed to be in the order of 0.50 DS) makes the evaluation of a myopia management intervention over the short run (say, one to two years) problematic. While the repeatability of measurements of very small refractive changes over shorter time periods is questionable, this is not the case for the accurate and repeatable measurement of axial length changes. Consequently, if we wish to enhance and adapt a myopia management intervention, the use of refraction alone makes the decision-making process difficult. Indeed, a growing number of researchers are now stating the axial length is the most important metric to monitor in pre-myopic and myopic children.1-5
How might we measure axial length?
Early studies of the relationship between refraction and ocular biometry used a radiographic technique to obtain a measurement of axial length of the eye.6 Measurement of axial length of the eye is a key parameter in cataract surgery, essential for the determination of the power of the intraocular lens (IOL) implant that will replace the natural crystalline lens. In fact, the main motivation for the development of many of the modern devices currently used for axial length measurement was to improve the accuracy of IOL implant selection and post-operative target refraction accuracy. Such devices very rapidly attracted the attention of the research community, particularly in the field of myopia study. I remember clearly the excitement during my postgraduate research studies when one of the first generation of modern ocular biometry instruments arrived at Aston University.
Ocular biometry systems are now being marketed with their application in myopia management overtly acknowledged. A detailed review of these systems is beyond the scope of this article, but table 2 lists some instruments likely to have a role in myopia management clinics.
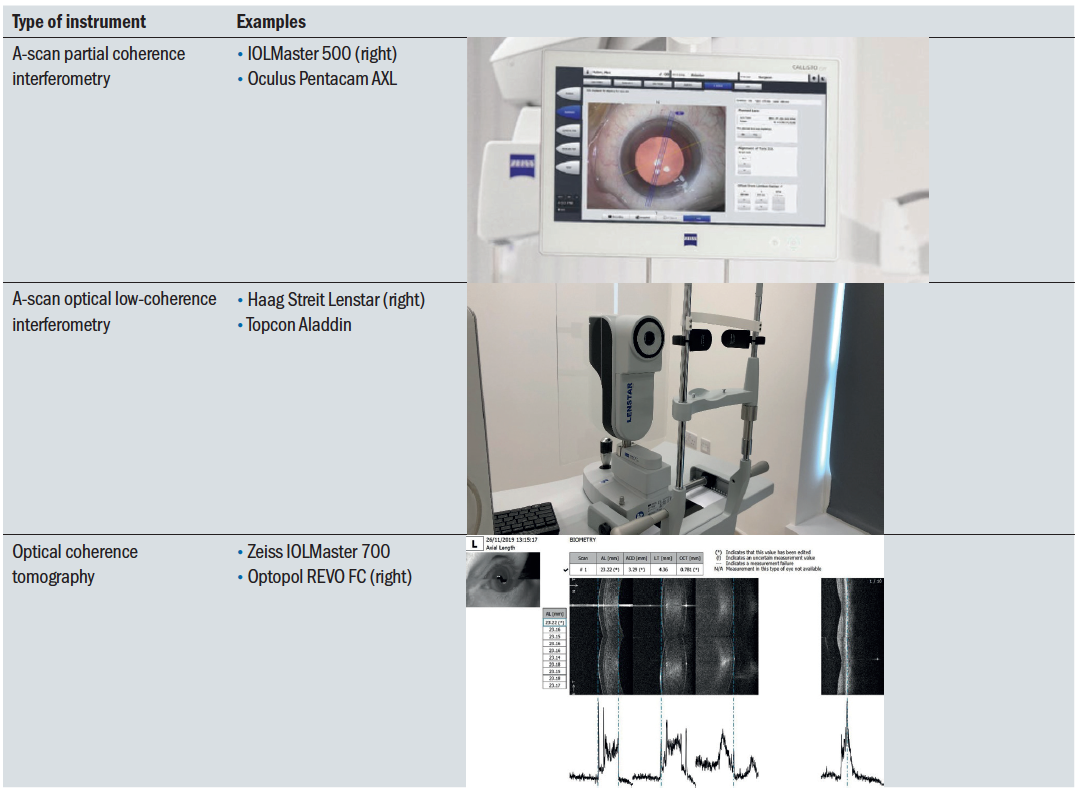 Table 2: Different instruments used for axial length measurement
Table 2: Different instruments used for axial length measurement
The axial length of the eye can be subdivided into major components, as shown in figure 1. Moving from the front of the eye to the back of the eye we can divide the total axial length into distinct sections:
- Central corneal thickness
- Anterior chamber depth
- Crystalline lens thickness
- Vitreous chamber depth
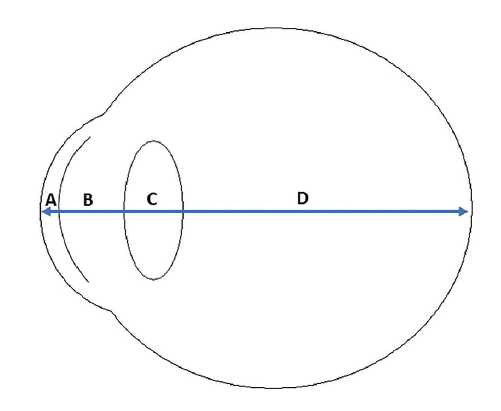 Figure 1: Components of the axial length of the human eye. A: central corneal thickness; B: anterior chamber depth; C: crystalline lens thickness; D: vitreous chamber depth
Figure 1: Components of the axial length of the human eye. A: central corneal thickness; B: anterior chamber depth; C: crystalline lens thickness; D: vitreous chamber depth
The use of axial length measurement using modern instrumentation greatly improves the level of repeatability of myopia progression data. Axial length measurement may be undertaken using either ultrasound (figure 2) or light. The IMI Clinical Trials and Instrumentation Report states that ultrasonography is limited in resolution to about 0.30DS, poorer repeatability than cycloplegic refraction in fact.7
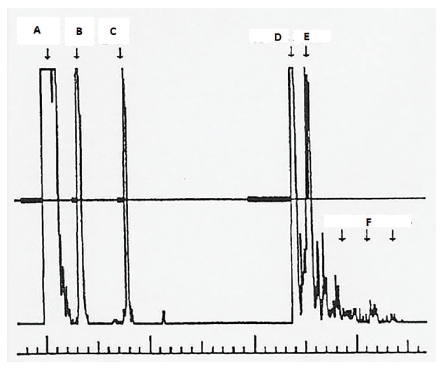 Figure 2: Ultrasound A-scan biometry data showing echo from A: Probe/corneal junction; B: Anterior surface of crystalline lens; C: Posterior surface of crystalline lens; D: retinal surface; E: sclera; F: orbital tissues
Figure 2: Ultrasound A-scan biometry data showing echo from A: Probe/corneal junction; B: Anterior surface of crystalline lens; C: Posterior surface of crystalline lens; D: retinal surface; E: sclera; F: orbital tissues
Modern instrumentation used for accurate biometry is, therefore, based upon the use of incident light, employing one of several optical techniques. These are:
- Partial coherence tomography
- Low-coherence reflectometry
- Optical coherence tomography
Ultimately, these terms refer to the same basic set-up; an interferometer under low coherence illumination. Most are based on the principle of the Michelson interferometer (figure 3). Essentially, a beam of light is directed via a beam splitter to form two paths. One path is directed into the eye and reflects off the various perpendicular surfaces, such as the anterior corneal surface and the retina. The other path is directed into a reference arm of known dimensions (represented by the scanning mirror in figure 3). Both paths are then recombined by the beam splitter, and the interference pattern of these paths is analysed (at the point marked as the detector in figure 3). The parameters obtained from this analysis are proportional to the physical separation of the surfaces in the eye under investigation.
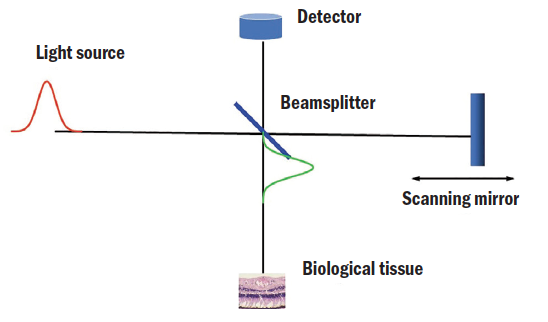 Figure 3: A schematic representation of the Michelson interferometer
Figure 3: A schematic representation of the Michelson interferometer
Commercial instruments can display resolution for axial length measurement in the order of just 0.01mm, and studies have shown that these instruments can provide a repeatability of around just 0.02 to 0.04mm (20 to 40µm), which provides eye care practitioners with axial length measurements with a high degree of certainty.8
When this level of repeatability is modelled in a schematic eye, for example the Bennett-Rabbetts schematic eye,9 we find that an axial length change equivalent to around 0.1 DS can be reliably detected. Thus, modern instrumentation for axial length measurement provides a refined and sensitive method for monitoring eye growth and myopic shifts.
Prior to the development of modern optical techniques for the measurement of axial length, A-scan ultrasonography was the technique of choice. Ultrasound is still in use of course, but modern optical methods offer a number of advantages:
- They are non-contact and therefore do not require topical anaesthesia
- They are less dependent on the skill of the operator
- The level of precision of the instrument is generally better
- Applanation of the eye during an A-scan ultrasound measurement can induce an error that will give an underestimation of the axial length
Clearly, ophthalmic ultrasonography still plays an important role in many areas of eye care and disease detection, but is unlikely to make an impression in myopia management clinics.
How accurate is axial length measurement?
A clear demonstration of the high-resolution axial length measurements achievable with modern optical instruments can clearly be seen in the various studies into the effects of physiological processes upon ocular biometry.
Work at Queensland University of Technology has examined the effect of water consumption on axial length. Read and Collins were able to detect reductions of 10 to 20 micrometres in the axial length of the eye following ingestion of one litre of water.10 From the same laboratory, Chakraborty and colleagues observed a repeatable pattern of axial length variation according to time of day. An average variation of around 30 micrometres was found, with axial length being longest around noon and shortest in the evening. Work has also shown that it is possible to detect changes in axial length that result from exposure to blur.11,12
What is the expected axial length?
This is a big question and the answer depends upon a number of factors.
Firstly, we know that the axial length will relate to the refractive error of the eye, with a negative correlation found between axial length and spherical refraction. The slope (or gradient) of this relationship can be determined using data either from cross-sectional studies of refractive error and ocular biometry or from longitudinal studies, such as myopia management trials. From the research literature, we generally see gradients that suggest that a 1mm increase in axial length will correlate with a negative shift in spherical refraction of between two and three dioptres.
The average axial length for a human emmetropic eye appears to be around 23.5mm.13 Figure 4 shows data from a small sample study of undergraduate optometry students. Within this study, 65% of the variation in spherical refraction was accounted for by the axial length of the eye.14
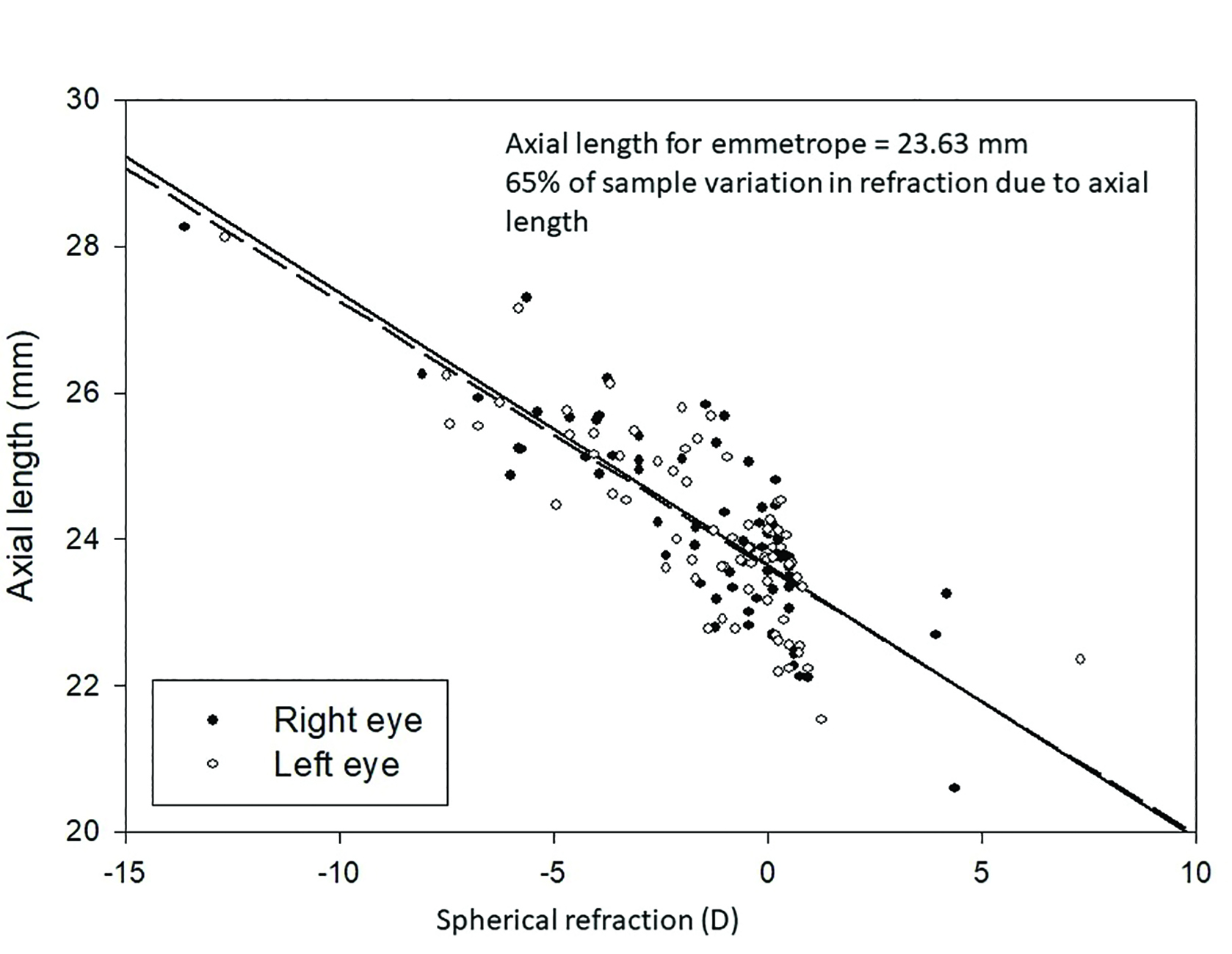 Figure 4: Distribution of axial length measurements against spherical refraction in a university student population
Figure 4: Distribution of axial length measurements against spherical refraction in a university student population
Further study of this topic can be conducted by reading the numerous research papers that have measured the axial length of the eye and drawn correlations with refractive error. These data have helped to understand the variation in axial length and myopia that might be expected according to patient age 15 and ethnicity (figure 5),1 and also the expected increases in axial length per year against the age of the patient.
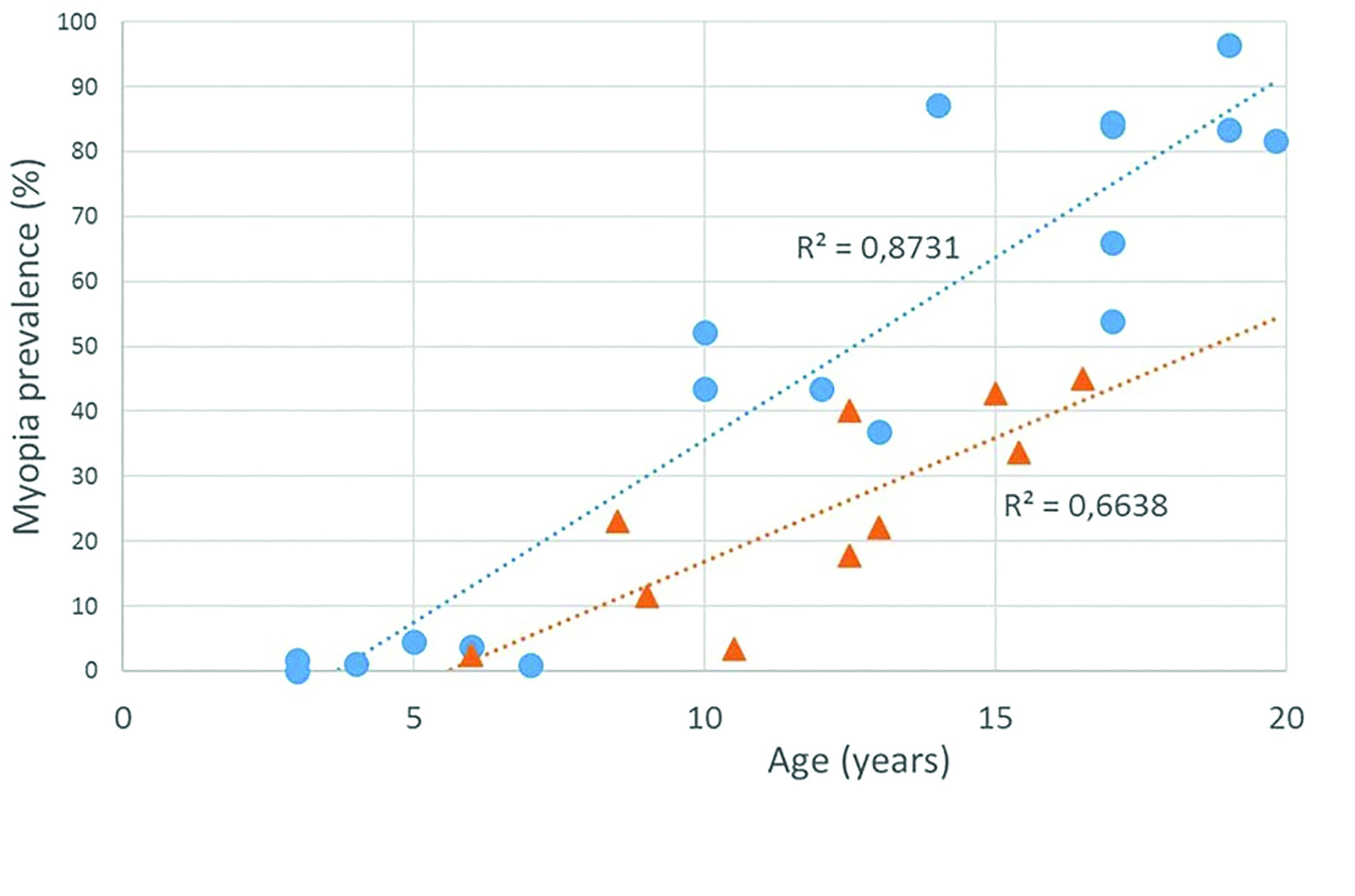 Figure 5: Myopia prevalence in East Asia (dots) and in Europe (triangles) in different age groups of children1
Figure 5: Myopia prevalence in East Asia (dots) and in Europe (triangles) in different age groups of children1
For practitioners interested in myopia management, there are some excellent resources now becoming available that help to collate the many different studies into a single, easy to access, location. One such resource is the Myopia Profile website (www.myopiaprofile.com), a very helpful source of up-to-date information on all things to do with myopia that was developed by husband-and-wife optometrist team Drs Paul and Kate Gifford.
Secondly, we must consider the other parameters of the eye. In particular, the refractive power of the cornea. If we sample a number of emmetropic eyes that cover a range of corneal radii, we will observe a relationship: emmetropic eyes with a steep cornea (small corneal radius measurement) will have a shorter axial length when compared to an emmetropic eye with a flat cornea (large corneal radius measurement).
Table 3 demonstrates this variability and presumed compensatory facility in three young adult research participants, all of whom were emmetropic.14 This relationship is one of the pieces of evidence that backs up the theory the eye undergoes coordinated growth to arrive at a state of emmetropia. Other parameters, such as the power and position of the crystalline lens, will have influence on the overall refractive power of the eye. A number of the modern axial length measurement platforms will provide access to crystalline lens measurements for the clinician. It therefore becomes possible for the practitioner to establish biometric models for the eye that can be used to predict the refractive status, and to use changes in ocular component values such as the vitreous chamber depth to predict their impact on myopia progression.
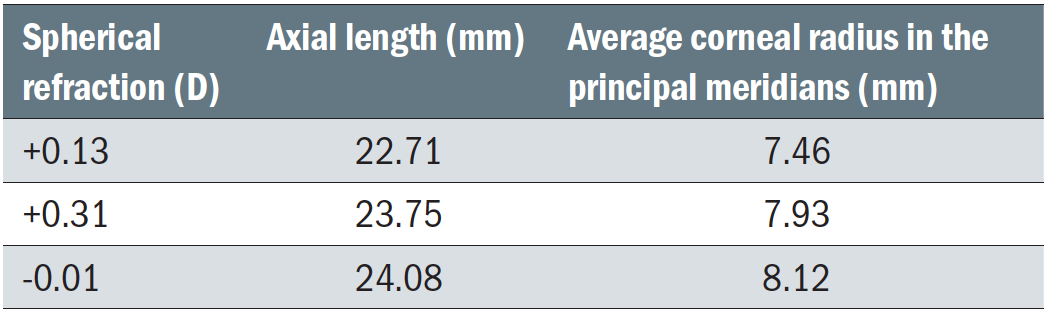 Table 3: Variation of refraction, axial length and corneal radius in three emmetropes
Table 3: Variation of refraction, axial length and corneal radius in three emmetropes
What are the research applications of axial length measurement?
There are many applications for axial length measurement devices in the research setting. Their use in myopia studies is well established, both as offering a baseline measurement and for the ongoing monitoring of patients in clinical trials.
Further study applications of ocular biometry and dynamics include furthering our understanding of:
- The relationship between refraction and axial length
- The influence of accommodation and eye rotation on axial length
- The effect of gravitational forces upon the eye
Instrumentation for the measurement of axial length may also include some facility for the measurement of anterior chamber depth and crystalline lens thickness (figure 6). This has provided researchers with further methods for the study of the performance of intraocular lens implants for example.
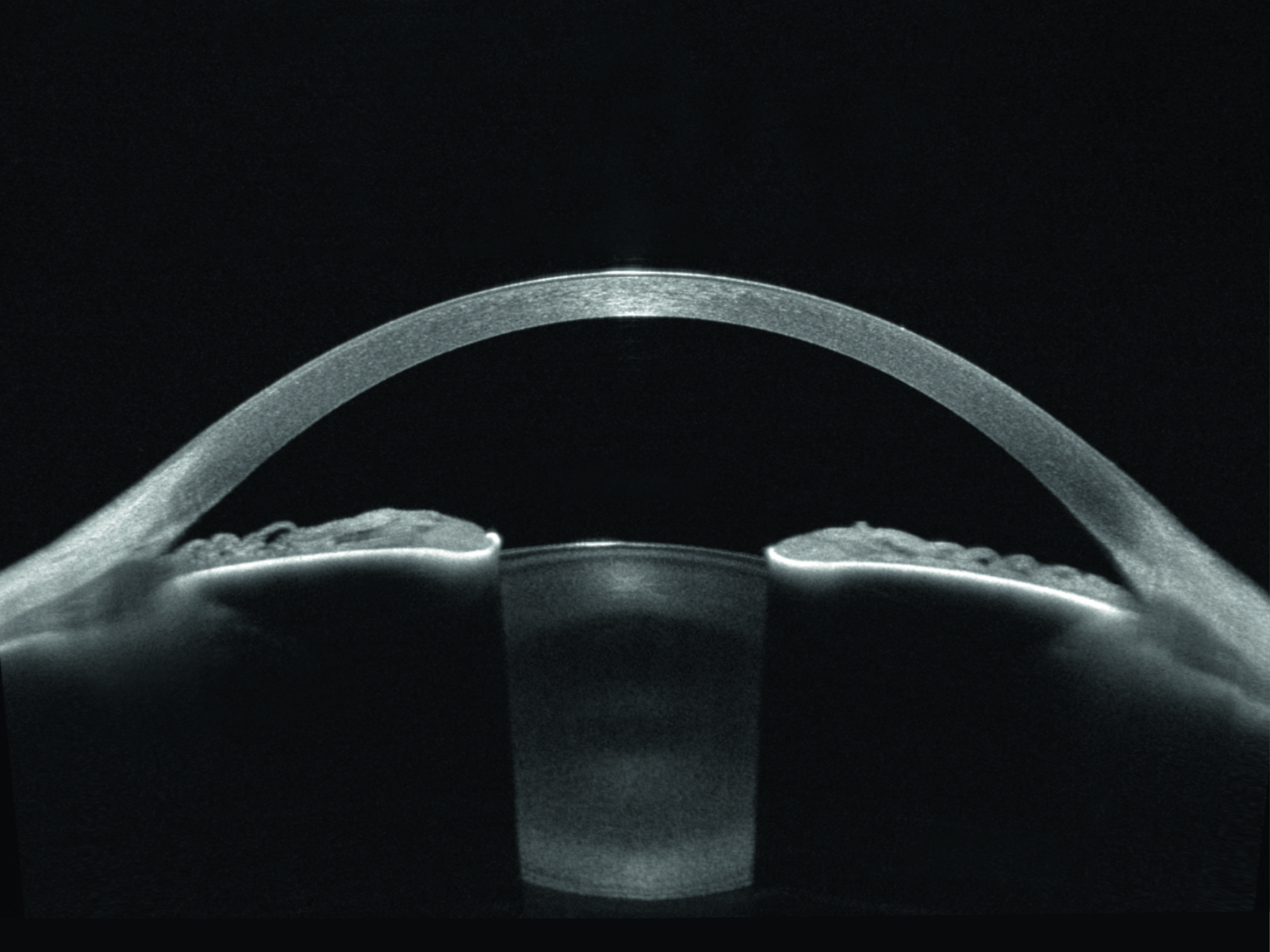 Figure 6: Cross-sectional view of the anterior chamber and crystalline lens using the Heidelberg Anterion OCT instrument
Figure 6: Cross-sectional view of the anterior chamber and crystalline lens using the Heidelberg Anterion OCT instrument
In the field of myopia research, a number of research studies have described techniques that enable an axial length measurement device to map out, following relatively simple modification, the profile of the retina over the central 40 or so degrees of the visual field either side of fixation. This provides researchers with other useful parameters regarding the curvature of the retina, which may prove useful in the refinement of myopia management interventions.
What is the value of axial length measurement for eye care practitioners?
So, we have available high precision instruments that can measure axial length, and these measurements will provide reliable data for the monitoring of eye growth; this will be of great utility for practitioners involved in myopia management.
As these instruments become more widely available in primary care optometry, we will be able to build up a large dataset of the distribution of eye lengths in the population, gather more data on the correlation between refractive error and axial length, and know more about the rate of normal eye growth in childhood. We will also be able to accrue data about the growth of the eye across a large number of patients as their myopia progresses. This will provide a firm basis for determining, with increasing accuracy, the success of various myopia management interventions for individual patients.
For practitioners without access to axial length measurement instrumentation, recent work has enabled the team at Ulster University to develop a model for the estimation of axial length from the spectacle refraction and keratometry (see table 4).
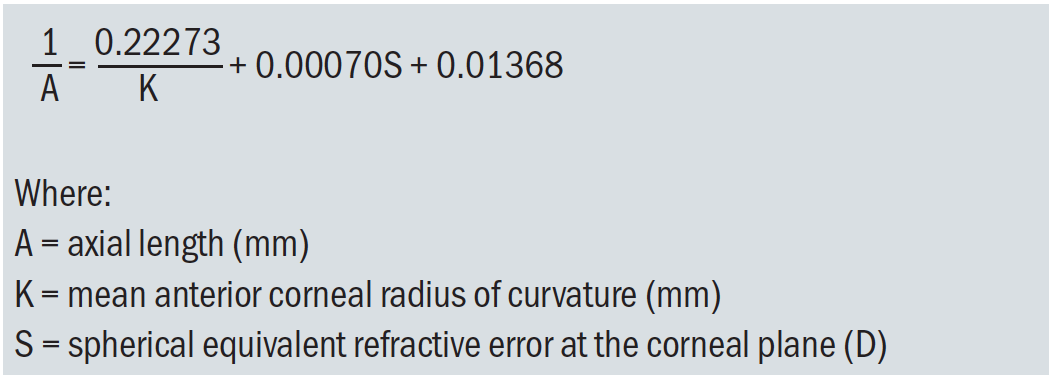 Table 4: A relationship derived from a large database showing the calculation of axial length from the keratometry and cycloplegic refraction results
Table 4: A relationship derived from a large database showing the calculation of axial length from the keratometry and cycloplegic refraction results
This provides useful additional information for the clinician involved in myopia management who may not yet have the means to measure axial length as part of their patient care pathway.16 The NICER study is a large-scale long-term cohort study of refractive error and ocular biometry in Northern Ireland and has already highlighted some ways of helping to predict future myopic profile.17 For example:
- Axial lengths greater than 23.07mm at six to seven years are associated with a strong risk of future myopia
- The presence of +0.75 D or less of hyperopia at the age of six years indicates that myopia is likely to develop in the near future
- Children presenting with a refractive error of <+0.63 D at six to seven years and with at least one myopic parent were likely to develop myopia by age 13 years and those with no myopic parents were likely to develop myopia by 16 years
What are my conclusions?
My hope for the future concerning this topic is that every practitioner involved in myopia management will have access to a reliable method of measuring the axial length of their patient’s eyes. They will use this information, alongside their measurements of spectacle refraction, to monitor myopia progression. They will use the data to refine their myopia management strategies, and will tailor their interventions to minimise myopia progression.
Finally, they will feed their clinical data (after obtaining patient consent and appropriate consideration of confidentiality) into a national database, so that large scale information on eye growth rate can be used by other clinicians to help them make decisions in their myopia management. Such decisions might include:
- When to start a patient on a myopia management intervention
- When to decide that a given intervention is working to control a patient’s myopia progression
- When to modify a current myopia management strategy, such as giving a different near addition power in a multifocal lens strategy
- When to consider changing to a different myopia management strategy
- When to stop a given myopia management plan
- When to restart myopia management in cases where myopia progression recommences
Myopia is a major ocular health problem18 and measurement of the axial length of the eye is a key parameter in the diagnosis, monitoring and treatment of this condition. We are becoming more equipped with research evidence, useful interventions, and excellent instrumentation to help us all fight myopia. The application of ocular component measurement will become increasing relevant to the work of the eye care practitioner.
- Edward Mallen is Professor of Physiological Optics at the University of Bradford. His research interests are the study of the myopic eye, ocular accommodation, and development of instrumentation for visual and physiological optics applications. He is Immediate Past President of the College of Optometrists. The author has no proprietary interests in any of the commercially available instruments for the measurement of axial length of the eye.
References
- Németh J, Tapasztó B, Aclimandos WA, et al. Update and guidance on management of myopia. European Society of Ophthalmology in cooperation with International Myopia Institute. European Journal of Ophthalmology. March 2021. doi:10.1177/1120672121998960
- Tideman JWL, Polling JR, Vingerling JR, et al. Axial in length growth and the risk of developing myopia European children. Acta Ophthalmologica, 2018; 96: 301–303.
- Brennan N, Toubouti Y, Cheng X, et al. Efficacy in myopia control. Progress in Retina and Eye Research. Epub ahead of print 27, November 2020. DOI: 10.1016/j.preteyeres.2020.100923
- Klaver C, Polling JR and Erasmus Myopia Research Group. Myopia management in the Netherlands. Ophthalmic and Physiological Optics, 2020; 40: 230–240.
- McCullough S, Adamson G, Breslin KMM, et al. Axial growth and refractive change in white European children and young adults: predictive factors for myopia. Science Reports, 2020; 10: 15189.
- Deller JF, O’Connor AD, Sorsby A. X-ray measurement of the diameters of the living eye. Proceedings of the Royal Society of Medicine, 1947, Sep 30;134(877):456-67
- Moore KE, Berntsen DA. Central and peripheral autorefraction repeatability in normal eyes. Optometry and Vision Science, 2014;91(9):1106-12
- Santodomingo-Rubido J, Mallen EA, Gilmartin B, Wolffsohn JS. A new non-contact optical device for ocular biometry. British Journal of Ophthalmology, 2002 Apr;86(4):458-62
- Bennett AG and Rabbetts RB. Clinical Visual Optics. (2007). Butterworth-Heinemann.
- Read SA, Collins MJ. Water drinking influences eye length and IOP in young healthy subjects. Experimental Eye Research, 2010 Aug;91(2):180-5
- Chakraborty R, Read SA, Collins MJ. Diurnal variations in axial length, choroidal thickness, intraocular pressure, and ocular biometrics. Investigative and Ophthalmological Visual Science, 2011 Jul 11;52(8):5121-9
- Chakraborty R, Read SA, Collins MJ. Hyperopic defocus and diurnal changes in human choroid and axial length. Optometry and Vision Science, 2013 Nov;90(11):1187-98
- Gordon RA, Donzis PB. Refractive development of the human eye. Archives of Ophthalmology, 1985;103:785–789
- Mallen,E. PhD thesis, 2002, Aston University
- Matamoros E, Ingrand P, Pelen F, et al. Prevalence of myopia in France: a cross-sectional analysis. Medicine, 2015; 94: e1976
- Morgan PB, McCullough SJ, Saunders KJ. Estimation of ocular axial length from conventional optometric measures. Contact Lens and Anterior Eye, 2020 Feb;43(1):18-20
- McCullough S, Adamson G, Breslin KMM, McClelland JF, Doyle L, Saunders KJ. Axial growth and refractive change in white European children and young adults: predictive factors for myopia. Science Report, 2020 Sep 16;10(1):15189
- Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 2016; 123:1036–1042
