Over recent years, optometrists, especially therapeutic optometrists, have assumed a greatly extended role, both in hospital and community settings. Initially, this was mainly involvement with glaucoma shared care and age-related macular degeneration co-management schemes. More recently, optometrists have taken on further roles including the provision of front-line primary care emergency eye services, the management of embedded foreign bodies, treatment of bacterial and viral infections, management of inflammatory conditions such as uveitis, and the diagnosis and treatment of post-operative ocular complications such as cystoid macular oedema to name but a few.
Optometrists are now involved in administrating intravitreal injections1 and treating glaucoma, both medically and with laser surgery.2 At present, this usually takes place in the hospital setting, but moves to allow such procedures to be undertaken in community practice locations are under way. The main challenge to this development, at present, is the lack of affordable indemnity insurance rather than clinical skill set.
In this article, I will be discussing the use of the Nd:YAG treatment of capsular opacification by our profession.
Background
How often do we get a patient telling us that their vision was amazing immediately after their cataract operation a couple of years ago, but now they have noticed that the vision is less crisp, especially in low light conditions, and they now suffer glare from oncoming car headlights when driving at night? Almost as often, the patient may even ask if their cataracts ‘have started growing back’. Such reports usually indicate the presence of capsular opacification.
At least 10% of cataract patients develop capsular opacification, though there is variation with a number of different influences and cited prevalence figures range from 5% to as high as 50%.3 Opacification may begin within weeks of surgery or after several years and may affect the anterior capsule, but more typically the posterior capsule. Younger patients are at a higher risk of developing fibrosis.
Posterior capsular opacification (PCO) is usually treated with the neodymium-doped yttrium aluminium garnet (Nd:YAG) laser, more usually referred to simply as the YAG laser. Essentially, the laser blasts a hole through the opacified capsule to allow light to pass through again unhindered; a technique described as laser capsulotomy. Rarely, PCO is treated with surgical capsulotomy by a vitreoretinal surgeon on the few occasions that YAG treatment is not possible.
YAG laser
The YAG laser is usually a stand-alone instrument, similar in appearance to a slit lamp, capable of producing a treatment pulse at 1064nm in the infrared (IR) part of the spectrum. In this mode, it is used for PCO treatment as well as for peripheral iridotomy for the treatment of narrow angle glaucoma. Some YAG instruments can operate in a frequency doubled mode, where the wavelength produced is halved to 532nm, a wavelength now in the green part of the visible spectrum. This mode is used for selective laser trabeculoplasty (SLT) treatment of open angle glaucoma.2 In SLT, the laser power used is very low, causing a thermal photo-stimulation effect on the cells of the trabecular meshwork. The pulse of high energy laser light used is very short, just four nanoseconds. The power levels used are typically between 1.0 to 3.5mJ, the exact level dependant on the degree of capsular fibrosis and whether or not a capsulotomy lens is to be used (as discussed later).
When operated at 1064nm, the YAG laser causes photo-destruction, reducing the tissue to a plasma. No thermal effect occurs, and so its impact is not pigment-dependant as is the case in argon laser trabeculoplasty. Instead, the YAG produces a hydrodynamic shock wave, the direction of which is largely anteriorly, towards the operator of the laser. For this reason, the laser is focused just behind the opacified capsule, and the acoustic shock wave travelling anteriorly towards the capsule disrupts the opacified tissue. Because of this, tissue is impacted indirectly rather than as a result of a direct photo-disruptive effect. Indeed, if the laser is focused directly on the capsule, pitting of the intraocular lens implant may result. Luckily, where lens pitting does occur, it is clearly seen on slit-lamp examination and rarely impairs the patient’s vision.
Capsular opacification
It is important to eliminate other potential causes of the post-operative symptoms reported by the patient. These may include:
- Rebound cystoid macular oedema (CMO)
- Forward movement of vitreous opacities
- Uveitis
- Dry eye
Once this is done, we must now consider the possibility that the patient may be suffering from capsular opacification, usually of the posterior capsule (PCO). This can be missed if subtle, especially through a small pupil. So, it is important either to dilate and examine with retro-illumination, or to image with IR photography. This has the advantage that, because the retina is insensitive to IR light, the pupil will dilate naturally, so enabling a detailed view of both the implant and lens capsule (see Matheson imaging article for more information on this, 2019).4
Capsular haze may take many forms and as a result, different power settings are likely to be needed in each case. Three different presentations are shown in figure 1. Cloudiness of the anterior vitreous face can mimic capsular opacification and may occur in conjunction with PCO. In such cases, dense floaters located immediately behind the implant can often be dispersed with the YAG laser after the capsulotomy has been undertaken.
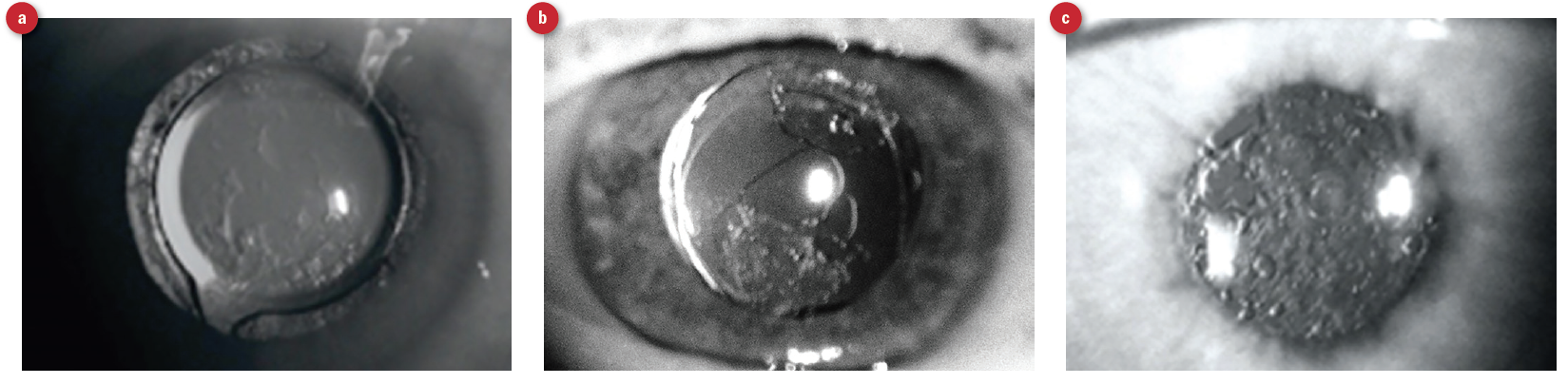 Figure 1: Three cases of posterior capsular opacification showing the variation in presentations. For this reason, different power settings for the laser are used for each different case
Figure 1: Three cases of posterior capsular opacification showing the variation in presentations. For this reason, different power settings for the laser are used for each different case
Sometimes, in cases of mild diffuse opacification, visual acuity may still be near to normal, though a significant loss of contrast sensitivity may be apparent when tested. Interferometry and aberrometry of the retinal image quality allow evaluation of the modular transfer function (MTF), which can be helpful in determining if borderline cases might benefit from a YAG capsulotomy (figure 2). Future surgical implant exchange is technically much more demanding if the patient has already had a YAG capsulotomy, and this needs to be borne in mind when considering laser treatment of mild PCO. Where the MTF is minimally affected, it may be advisable not to treat at that point.
 Figure 2: Aberrometer assessment of the retinal image quality indicates the integrity of the modulation transfer function
Figure 2: Aberrometer assessment of the retinal image quality indicates the integrity of the modulation transfer function
Contraindications
Contraindications for YAG capsulotomies include the following:
- Corneal opacities
- Corneal scarring
- Corneal oedema
- Corneal surface irregularity
- Intraocular inflammation
- Cystoid macular oedema
- Macular hole
- Vitreomacular traction
- Retinal tears
Where these have been excluded and the opacification impact on MTF deemed worthy of intervention, the procedure may go ahead.
Procedure
Capsulotomy lens use
YAG capsulotomy can be performed either directly or using a capsulotomy lens (figure 3). These lenses magnify the image, typically by about 1.5 to 1.8 times. The laser spot may be intensified by increasing the cone angle of the lens so giving a smaller spot size a greater energy density. This means lower laser power settings can be used. The lens is held against the patient’s anaesthetised cornea using a coupling fluid in the same way as a gonioscopy lens (figure 4).
 Figure 3: A Volk capsulotomy lens
Figure 3: A Volk capsulotomy lens
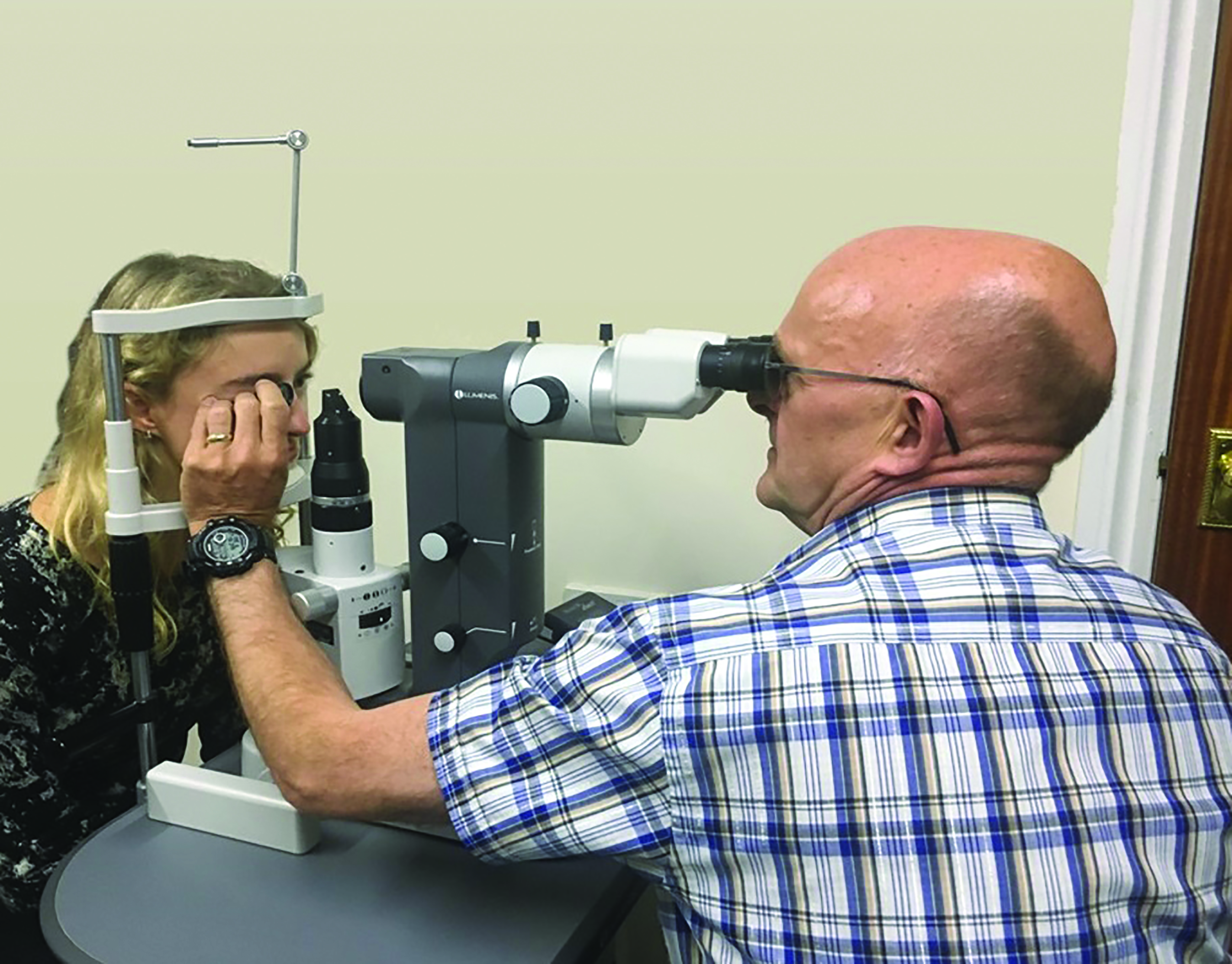 Figure 4: YAG laser used with a capsulotomy lens
Figure 4: YAG laser used with a capsulotomy lens
The capsulotomy lens is particularly useful when treating patients with extremely dry or irregular corneas, patients with a small palpebral aperture and those with blepharospasm. The lens may offer a slightly clearer, magnified view and also act as a lid retractor.
However, many patients find the treatment lens intimidating. So, it is sensible to use a lens solely for the treatment of those tricky cases already mentioned, along with patients in higher risk groups for whom minimum power levels should be used, such as high myopes, diabetics with retinopathy or with a history of cystoid macular oedema. This then enables the clinic to see adequate patient numbers, both safely and efficiently, and minimises negative patient response.
In the eye unit I work in, we do not routinely use a contact lens to perform the procedure. This has several advantages, patients prefer it as it is less invasive, no anaesthetic drops are needed, the whole treatment is much quicker and there is a lower risk of infection or corneal abrasions.
Disposable capsulotomy lenses are available, but are a significant additional cost to a busy clinic if used on every case.
Cutting patterns
The YAG laser system projects two He/Ne red laser dots to allow accurate aiming. The way they work is similar to the method used to calculate the appropriate aircraft height for the release of the bouncing bombs during the ‘dambusters’ raids of World War
Two.
The optometrist starts with the joystick definitely pulled back anterior to the capsule surface and two red dots are seen. The joystick is then advanced until these converge into a single red dot focused on the capsule. With our setup I would normally advance the joystick until the single dot once again just starts to split into two again indicating that I am focused just posterior to the capsule (figure 5). Alternatively, the laser can be set with a posterior offset of 125 to 250microns. This means that when a single red focusing dot is seen, the treatment laser is focused just behind the capsule.
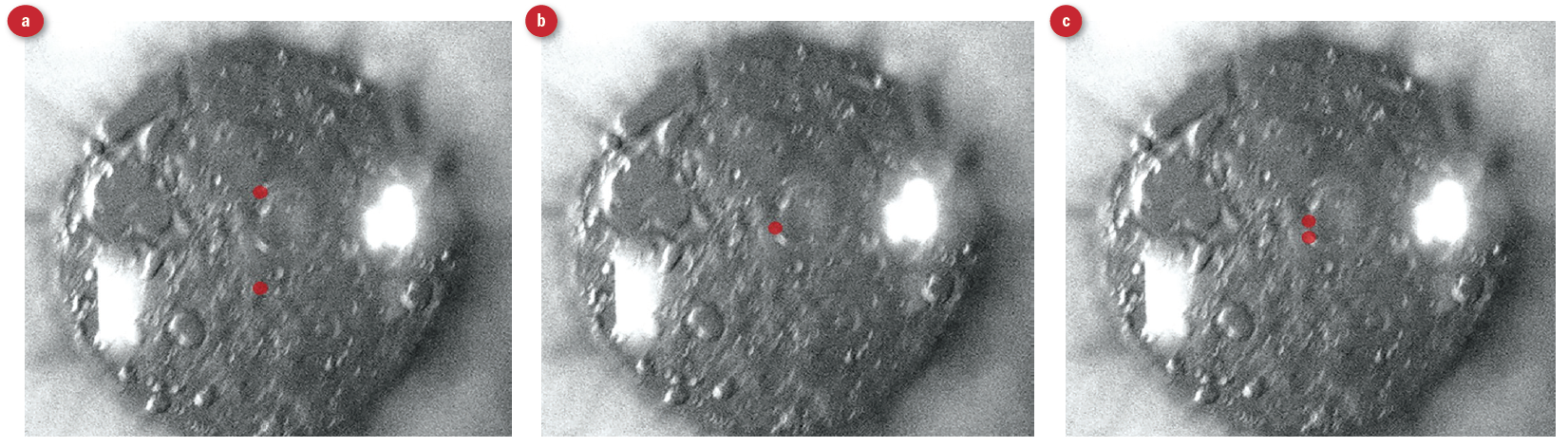 Figure 5: Use of positioning targets to focus the laser. (a) Two dots tell the operator to move the instrument toward the patient. (b) Dots now joined as one signifies the laser is focused on the posterior capsule. (c) Moving slightly further forward reseparates the dots and the laser is now focused just posterior to the capsule
Figure 5: Use of positioning targets to focus the laser. (a) Two dots tell the operator to move the instrument toward the patient. (b) Dots now joined as one signifies the laser is focused on the posterior capsule. (c) Moving slightly further forward reseparates the dots and the laser is now focused just posterior to the capsule
Generally, I use the lowest laser power setting that will adequately cut through the capsule. This may vary considerably, depending on how fibrosed and thick the opacified capsule has become. The capsular opening should not be greater than the diameter of the implant. Typically, dense fibrous capsular haze might require a power setting of about 3mJ and total power usage of around 65mJ. This will be slightly higher when no capsulotomy lens is used.
The most commonly used cutting pattern is cruciate. I would normally start at the 12 o’clock position, set the power level and then work vertically down to six o’clock. This would be followed by horizontal cutting from centre, firstly to three o’clock then nine o’clock (figure 6). This has the advantage of being able to adjust the laser power setting away from the visual axis, so minimising the risk of implant lens pitting.
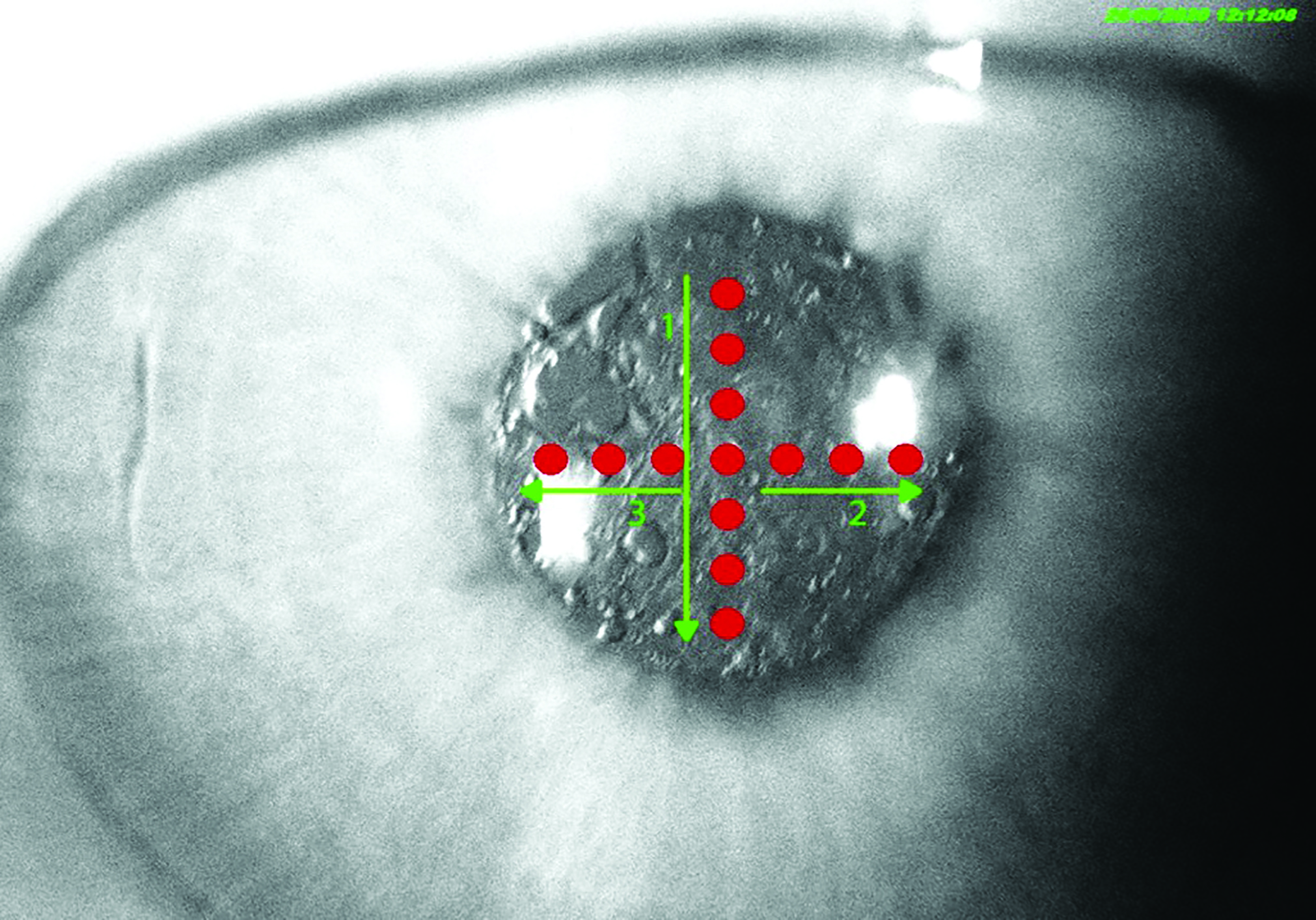 Figure 6: Cruciate pattern laser cutting
Figure 6: Cruciate pattern laser cutting
Once the cruciate cutting is complete, the result is a square/diamond shaped aperture (figure 7).
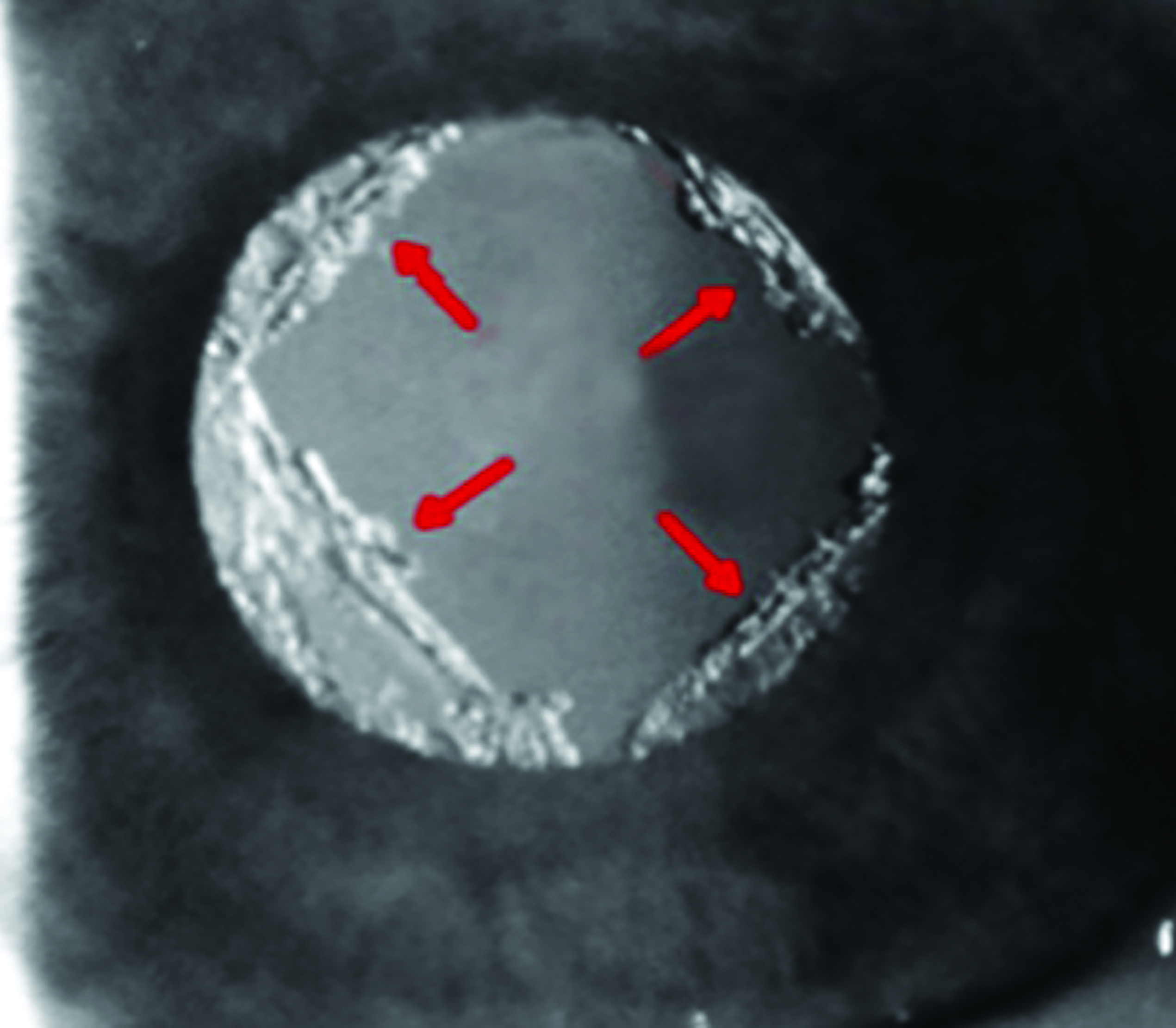 Figure 7: Aperture through opacified capsule on completion of cruciate pattern laser application
Figure 7: Aperture through opacified capsule on completion of cruciate pattern laser application
An alternative technique, preferred by some, is to use a circular pattern (figure 8). This has the advantage that the laser does not cut across the visual axis at all. Further minimising the risk of pitting of the implant. The main disadvantage of this method, however, is that a large free-floating vitreous opacity is produced and this can prove to be very troublesome for some patients.
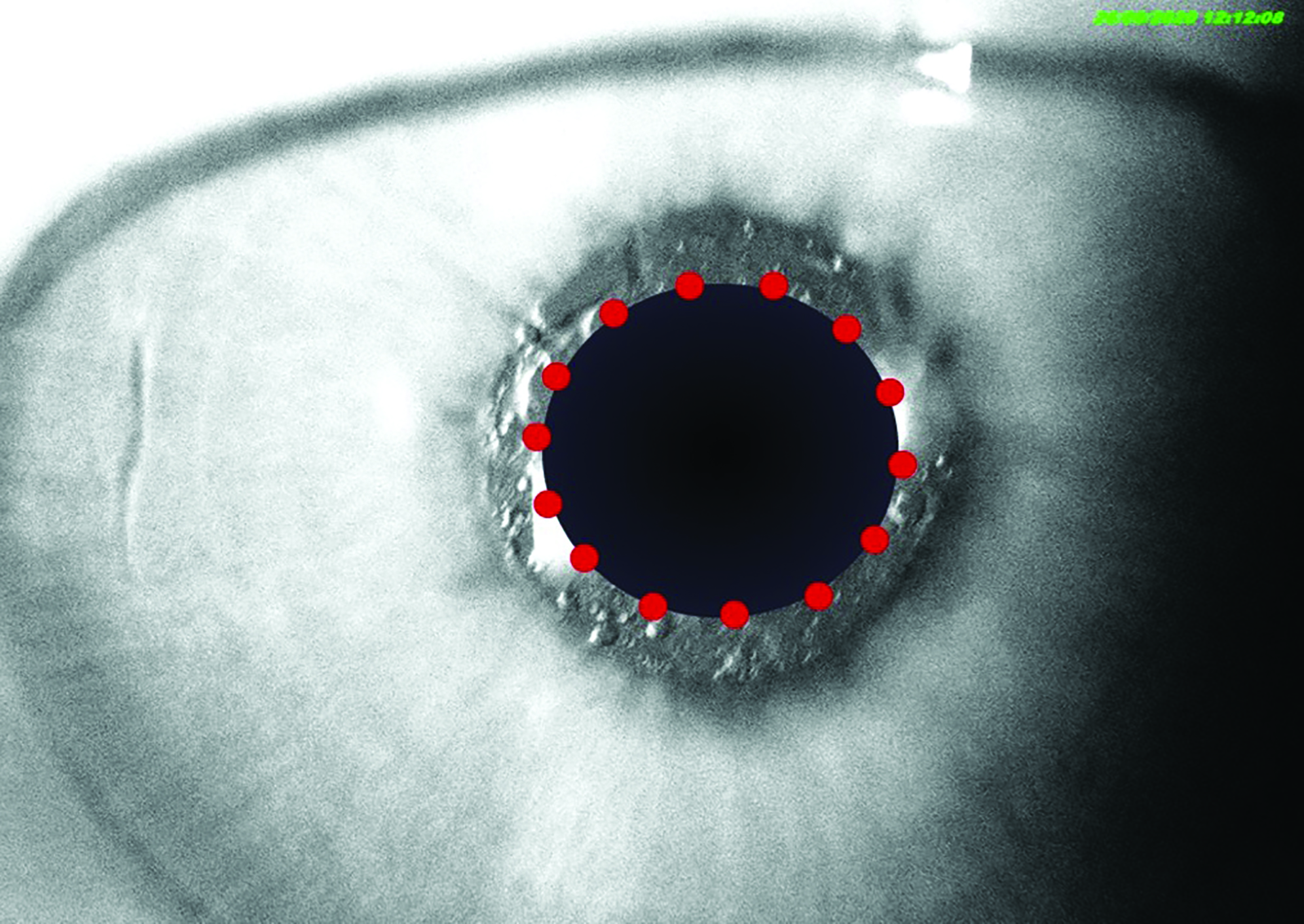 Figure 8: Result of a circular pattern application
Figure 8: Result of a circular pattern application
A variant on the circular pattern is the inverted horseshoe (figure 9). This aims to keep the capsular tissue captive at the six o’clock position, folding down below the visual axis. Unfortun-ately, while removing the problem of a floater, the flap position is not always constant and it can float back upwards and degrade vision.
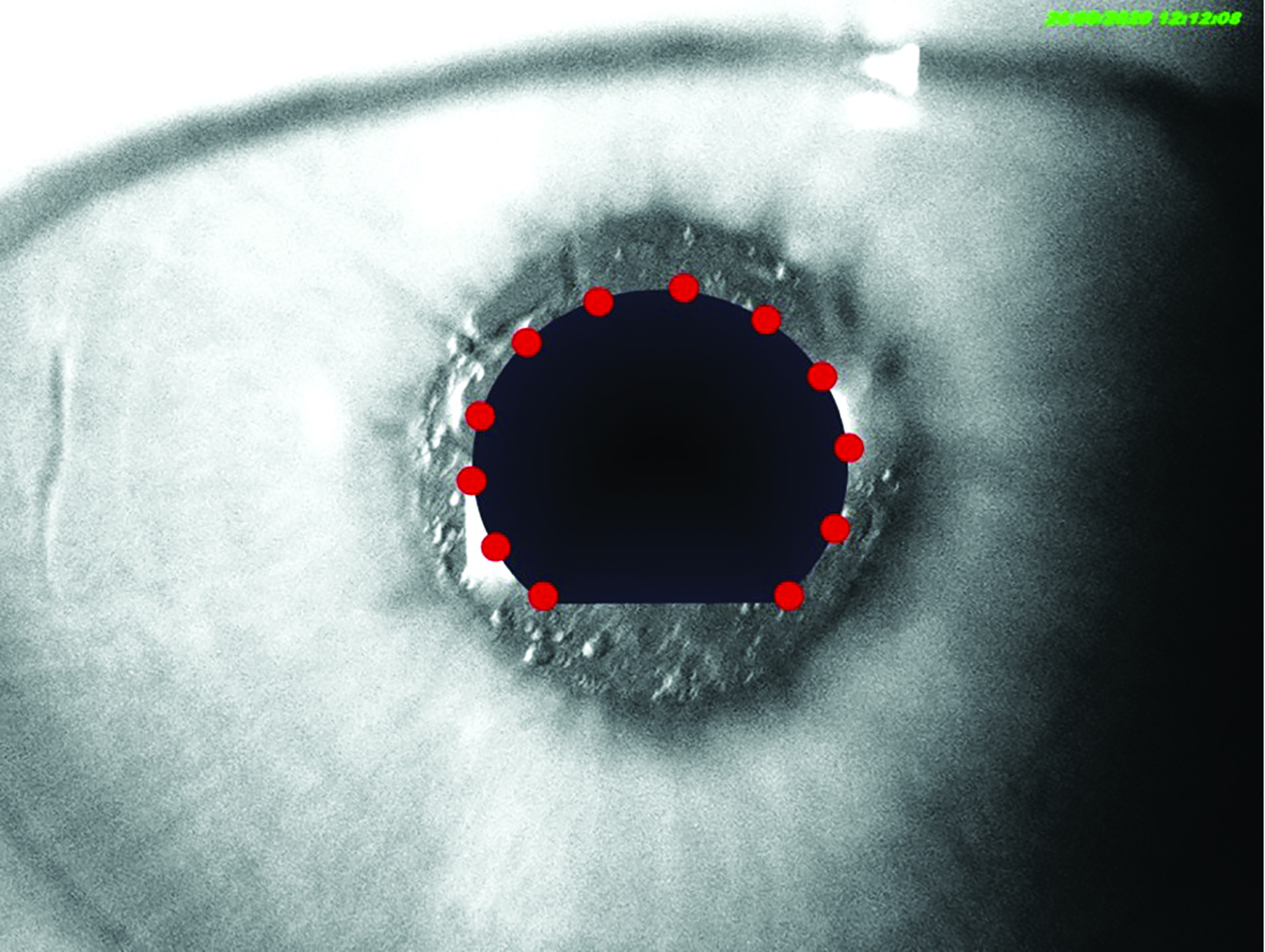 Figure 9: An inverted horseshoe pattern cut
Figure 9: An inverted horseshoe pattern cut
Post-procedure complications
These are uncommon, but may include any of the following:
- Retinal detachment
- Implant damage or dislocation
- Cystoid macular oedema
- Elevated intraocular pressure
- Anterior uveitis
- Iris haemorrhage
- Corneal oedema
- Macular hole
- Corneal endothelial cell loss
- Exacerbation of localised endophthalmitis
All patients are counselled about the risks of the procedure, have to sign an informed consent form and instructed to contact the clinic if they have symptoms especially pain or reduced vision, flashes or floaters. Let us consider some of these in a little more detail.
IOP spike
Some clinics advocate the instillation of a drop of brimonidine or Iopidine prior to surgery, while others recommend this only for high risk groups or where an IOP increase has been measured after treatment.
The IOP rise may be caused by angle blockage with debris liberated from the lasered capsule or by inflammatory cells, or may be a response to any steroids introduced during the procedure as an anti-inflammatory measure. If the IOP rise is significant, corneal oedema may result and lead to an increase in corneal centre thickness. Sometimes, the capsulotomy liberates previously
captive soft lens matter or viscoelastic gel from the original phacoemulsification. This has the potential to cause inflammation and a subsequent IOP rise.
Retinal detachment
The risk of retinal detachment (figure 10) is relatively low in the general population, though the lowest possible power settings should be always used in patients with high axial lengths (>24mm). A thorough assessment of the peripheral retina in such cases should pick up any retinal changes that might pre-dispose them to retinal detachment and needs to be undertaken even when there are no suspicious symptoms reported. All patients must be instructed to report any new flashes and/or floaters immediately as they require urgent examination.
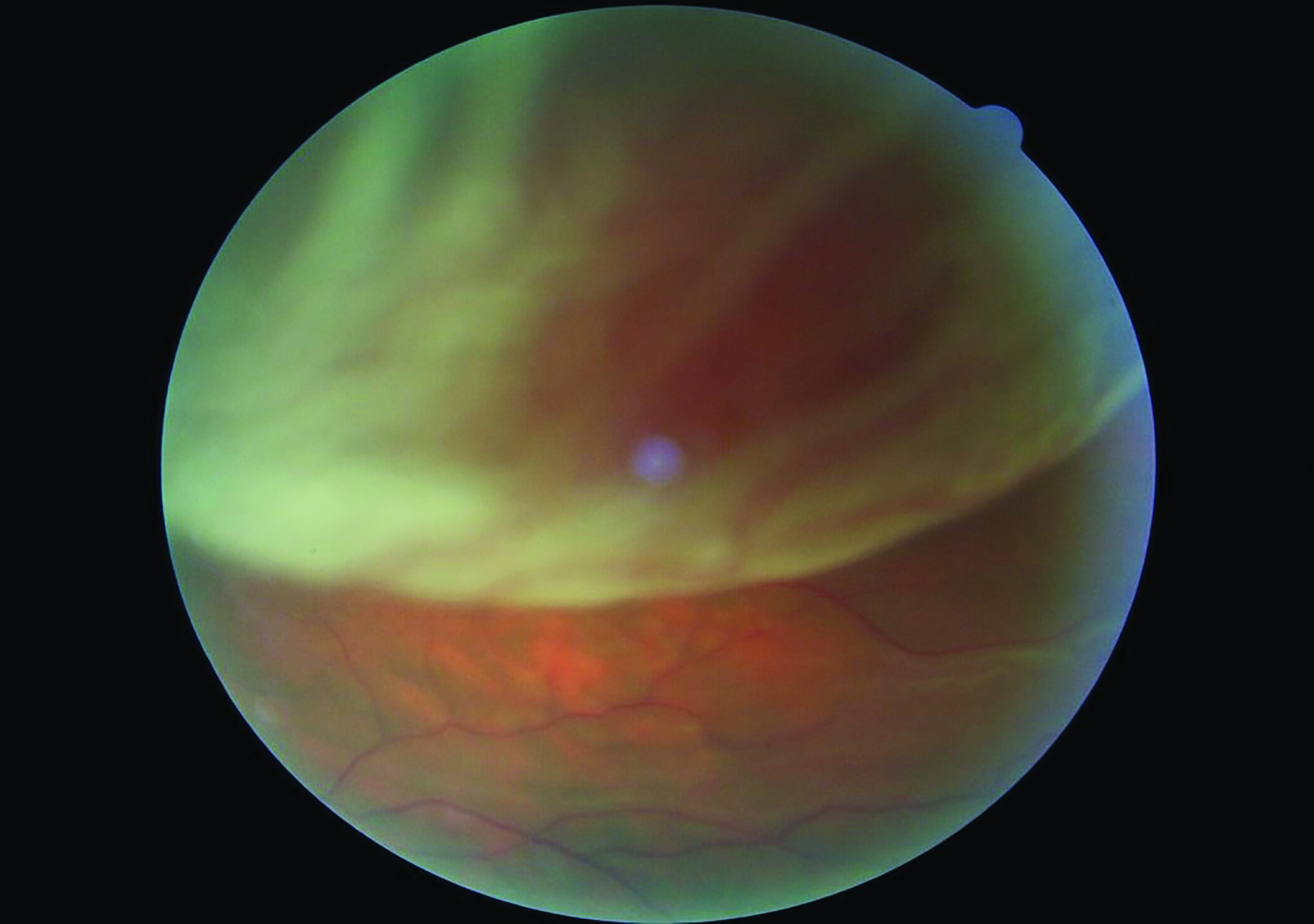 Figure 10: The risk of retinal detachment after laser capsulotomy is low in the general population
Figure 10: The risk of retinal detachment after laser capsulotomy is low in the general population
Inflammation: cystoid macular oedema
In high risk groups, those with a history of CMO (figure 11) or diabetic retinopathy, non-steroidal anti-inflammatory drops (NSAIDs) are often used to reduce this risk of the procedure aggravating an easily inflamed eye.
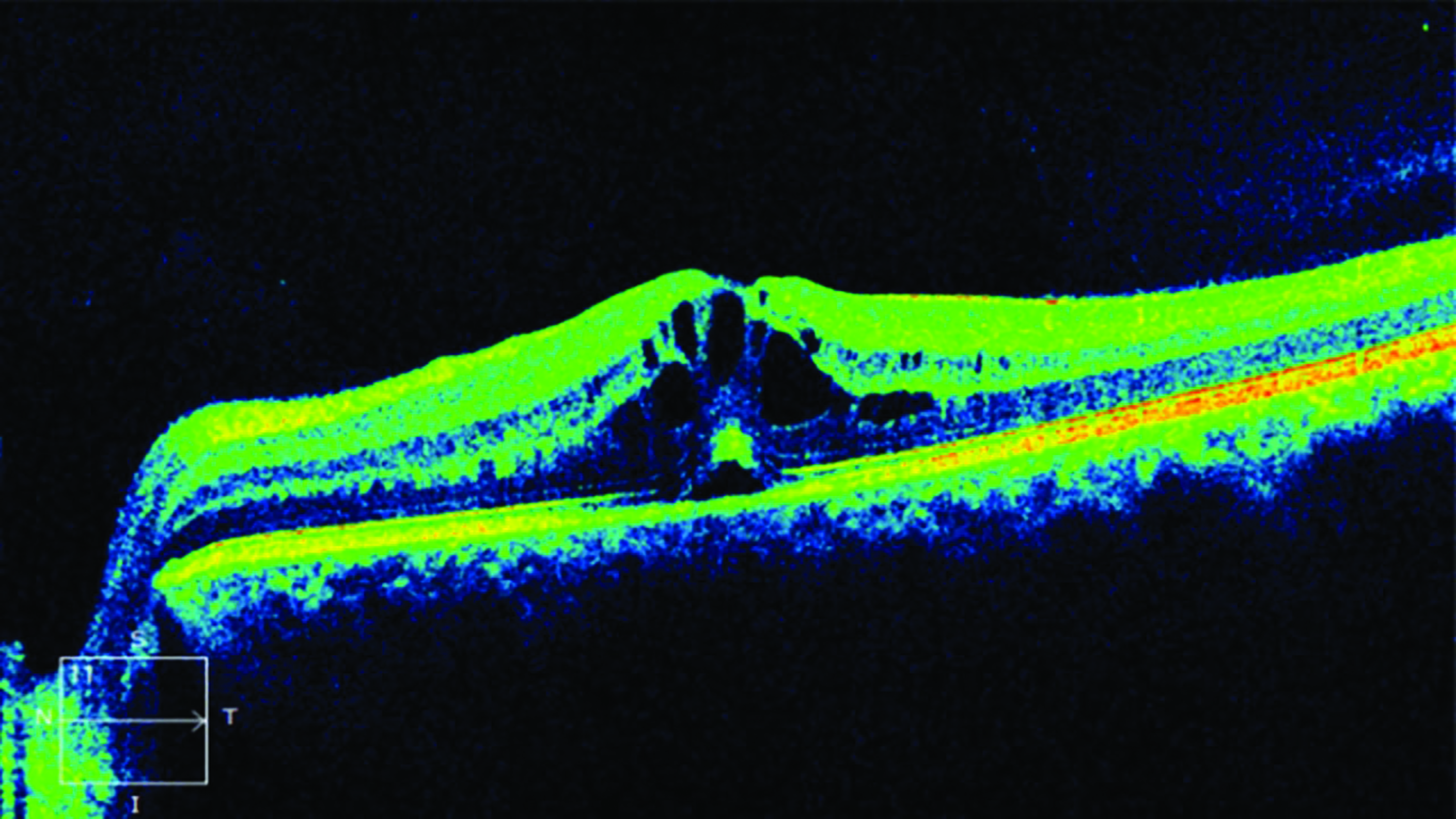 Figure 11: Where there is a history of CMO, non-steroidal anti-inflammatory drops may minimise the risk or further inflammatory response
Figure 11: Where there is a history of CMO, non-steroidal anti-inflammatory drops may minimise the risk or further inflammatory response
Inflammation: anterior uveitis
Prophylactic NSAID or steroid drops instilled both prior to and for a few weeks after the procedure are beneficial where it is suspected that anterior uveitis is a risk (figure 12). Soft lens matter liberated at the time of capsulotomy increases the risk of inflammatory conditions, such as iritis and CMO.
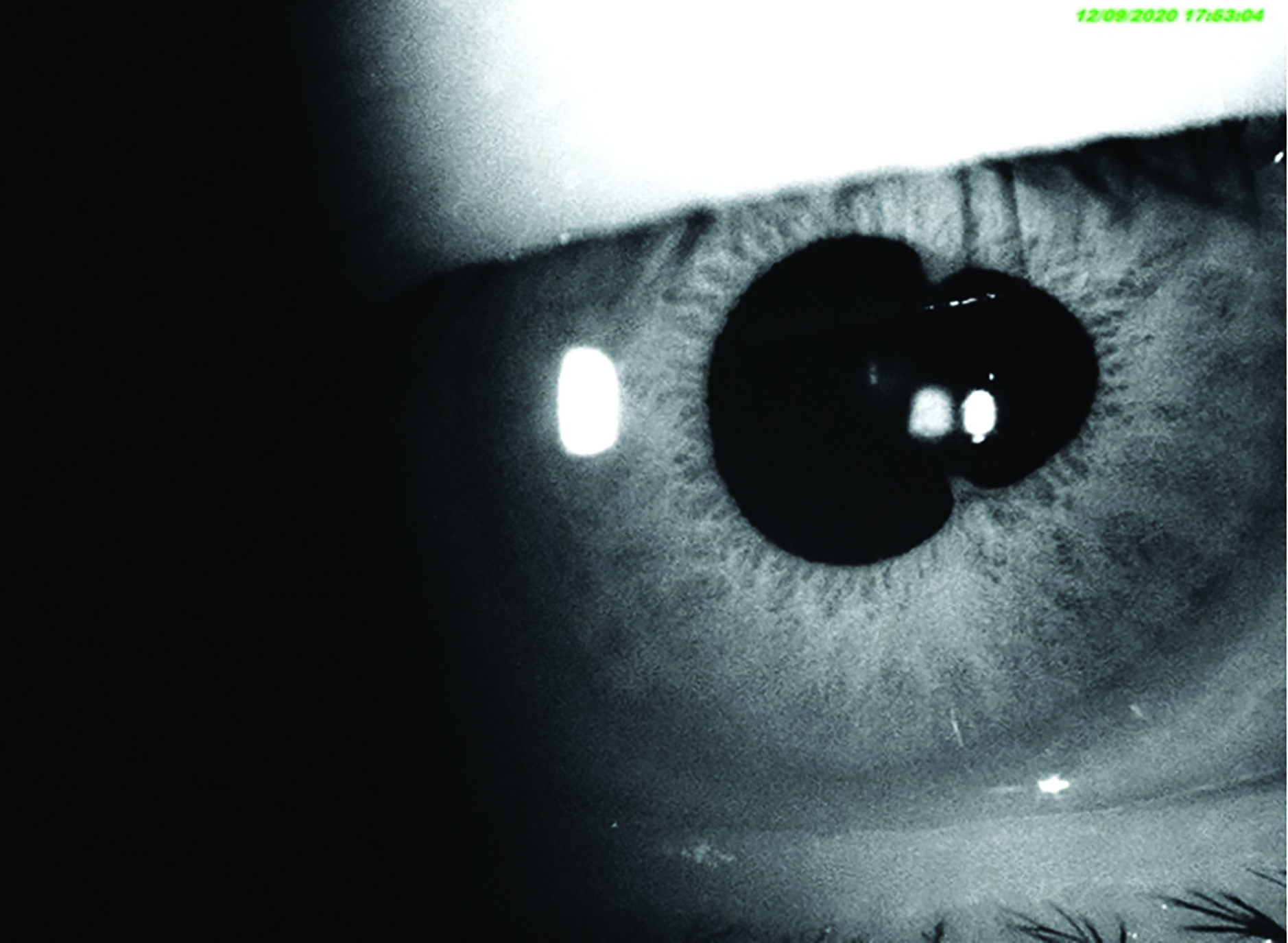 Figure 12: Posterior synechiae formation due to anterior uveitis
Figure 12: Posterior synechiae formation due to anterior uveitis
Macular hole
Patients with pre-existing vitreomacular traction (figure 13) are more likely to progress to a full thickness macular hole subsequent to laser capsulotomy due to shock waves through the vitreous. An OCT prior to the procedure can help identify patients at risk. As with high myopes, low power settings, perhaps with capsulotomy lens use, helps to minimise the risk of this
complication.
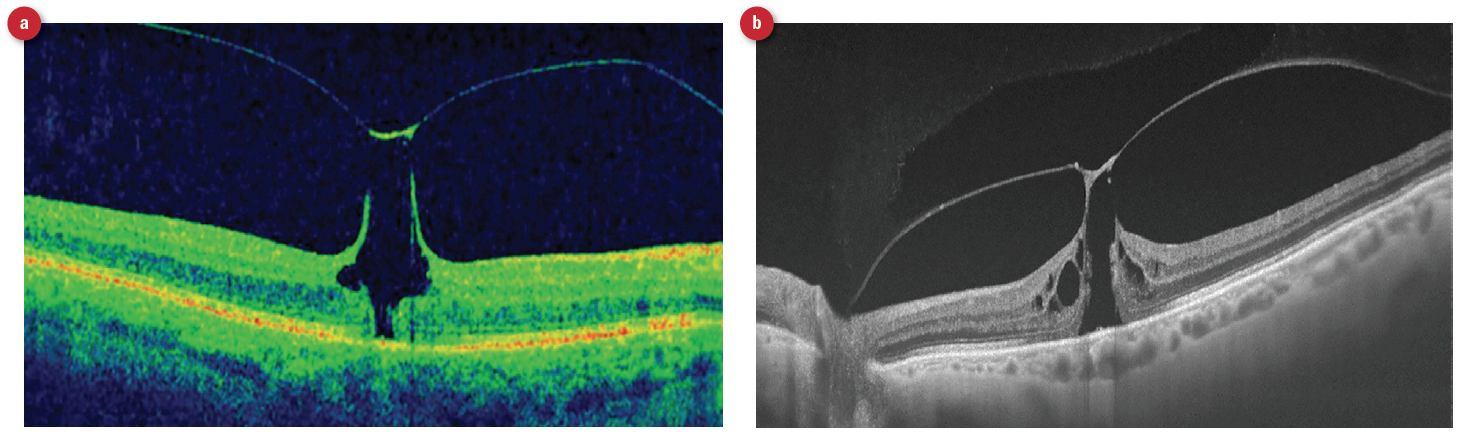 Figure 13: Vitreomacular traction seen with (a) colour OCT display and (b) black and white OCT display
Figure 13: Vitreomacular traction seen with (a) colour OCT display and (b) black and white OCT display
Pitting or displacement of the intraocular lens
Pitting of the implant can occur when the laser is focused anterior to the appropriate point of focus for a given laser power setting. Lens dislocation can occur if the capsulotomy results in too large an aperture. The clear opening should always be slightly smaller than the implant.
Lens dislocation is more common where a patient has accommodating lens implants. Ironically, these lenses also cause more opacification as they are continually moving against the posterior capsule. Generally, the trend is to make smaller capsulotomy openings, less than 4mm diameter, in these patients. This way, the accommodating implant movement can enlarge the small diameter aperture after the capsulotomy. Also, for these implants, I prefer to use a circular cutting pattern to avoid acute edges.
Patients with weakened lens zonules should be treated with extra care and with low power settings. The most common cause of zonular weakness is pseudoxanthoma elasticum (PXE), though there are several other rare causes. The very development of aggressive capsular fibrosis (capsular contraction syndrome) can lead to zonular dehiscence. It is theoretically possible that the shockwaves produced by the YAG laser during capsulotomy might be the precipitating factor that further weakens the already weak zonules.
Iris bleed
An iris bleed (figure 14) is rare but can occur with nervous or non-cooperative patients. Patients in wheelchairs, the severely obese and those with breathing difficulties, all pose challenges as far as keeping their head and eyes still while the laser is precisely focused and fired.
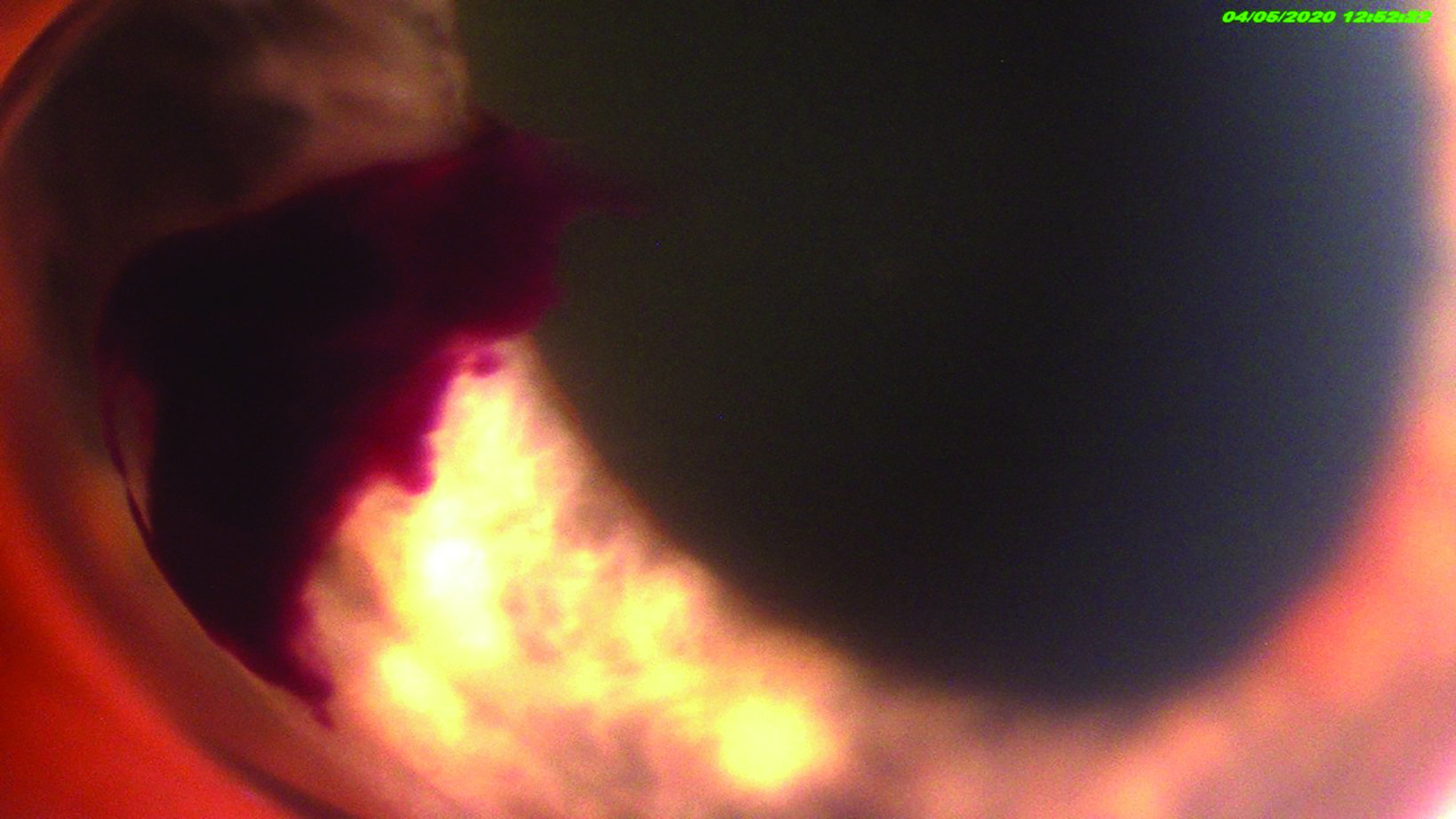 Figure 14: Iris bleed is a rare complication of capsulotomy and may result from patient movement or position change
Figure 14: Iris bleed is a rare complication of capsulotomy and may result from patient movement or position change
Corneal oedema
Damage to the corneal endothelial pump is a rare complication and results in corneal oedema. This may be visualised by anterior OCT assessment (figure 15).
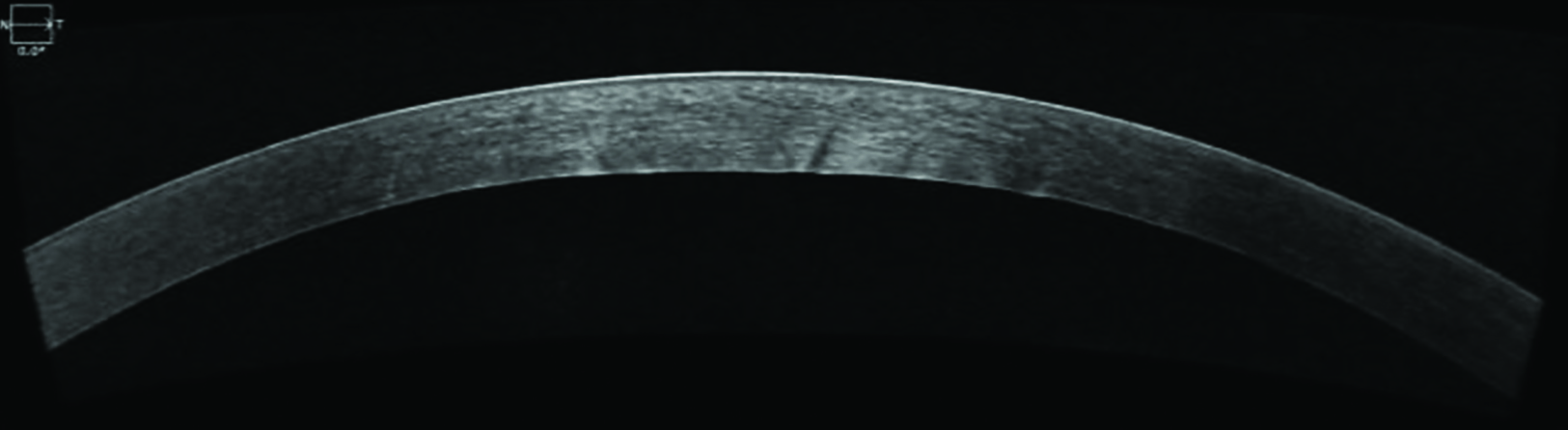 Figure 15: Anterior OCT scan showing thickening of the central cornea
Figure 15: Anterior OCT scan showing thickening of the central cornea
Although these examples of possible complications may be somewhat daunting, thankfully they are rare and are usually avoided with careful technique and sensible patient selection.
The future of optometry
This last year has made clear the benefit of farming out many diagnostic and treatment procedures to the community specialist therapeutic optometrist. Hopefully, YAG capsulotomy may soon become one of the several new services we might offer in our practices, along with SLT laser for open angle glaucoma, laser peripheral iridotomy for angle closure, laser trabeculoplasty for plateau iris and intravitreal injections for the treatment of wet AMD, diabetic macular oedema and retinal vein occlusions with CMO.
Our profession has already started using such techniques in hospital eye units. We need to continue to press for them to be made available in our community practices. This will enable patients to be treated on their doorstep, by their already respected specialist optometrist, in a timely fashion. Secondary care ophthalmology facilities currently lack the manpower, the clinic time and the space to be able to treat everyone. We need to work closely with our ophthalmologist colleagues to enable this evolution as soon as possible.
- Andrew Matheson is a Specialist Therapeutic Optometrist involved in medical retina treatments, glaucoma management and providing hospital laser surgery services.
- All digital photos taken with ARC Optical Imaging Suite
References
- Matheson A. Intravitreal injections in optometry. Optician, 15.11.2019, pp 24-29
- Matheson A. Laser trabecular modulation in optometry. Optician, 18.10.2019, pp 26-30
- Raj SM, Vasavada AR, Johar SRK, Vasavada VA, Vasavada VA. Post-operative capsular opacification: a review. International Journal of Biomedical Science, 2007;3:237–50
- Matheson A. Imaging – part 1. Are you on the right wavelength? Optician, 24.01.2020, pp 24-30
