Our perception of myopia is changing. While it was long considered a mere inconvenience, there is now an increasing recognition that myopia can lead to sight-threatening conditions later in life. All over Europe, and in fact all over the world, children begin to develop myopia at an earlier age, and in many children and young people it progresses faster than it used to. Earlier onset and faster progression mean that increasing numbers of adults are short-sighted and have myopia of greater severity, leading to an increased risk of sight-threatening complications. This article reviews our current understanding of factors that have led to this rise in myopia prevalence and severity, and the burden it will place on individuals and healthcare systems across Europe.
Myopia on the rise
Eye care professionals (ECPs) are seeing increasing numbers of children and young people with myopia. While the predominant reason for prescribing spectacles in young children in a hospital setting is still hypermetropia (long- sightedness), there is an undeniable rise in myopic prescriptions.1 Across Europe, myopia now seems to start at a younger age and to progress faster. In the UK, the prevalence has doubled over the past 50 years. Now, 1.9% of six-year-olds, 10 to 16% of 12 to 13-year-olds and 28% of 15 to 16-year-olds have myopia.2 Figures are similar across Europe: In the Netherlands, 2.4% of six-year-olds are short-sighted.3 In France, a myopia prevalence of 19.6% has been reported in children up to the age of nine years, and of 42.7% in 10 to 19-year-olds.4 In Denmark, the prevalence in teenagers with a mean age of 15.4 years is 17.9%.5
Epidemiological studies across adult populations also reflect this trend (figure 1).6 Far from being a rare condition, myopia is now very common, particularly in younger adults. Across Europe, 30.6% of people between the age of 25 and 90 years have myopia, with a far higher prevalence of 47.2% in 25 to 29-year-olds.7
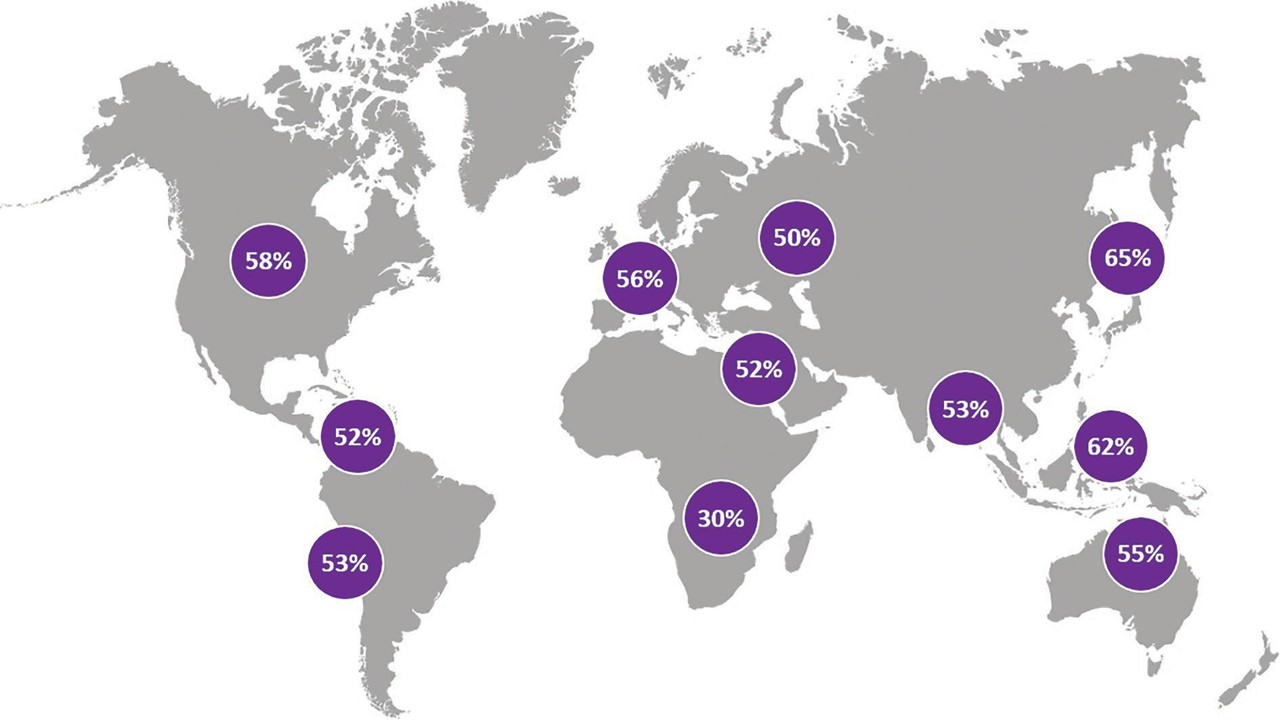 Figure 1: By 2050, 50% of the global population is predicted to be myopic6
Figure 1: By 2050, 50% of the global population is predicted to be myopic6
While these prevalence rates are not as high as those in East Asia, where over 80 to 90% of young adults are short-sighted, the rising trend is observed around the world. As a result, the WHO lists refractive error as a priority eye disease,8 recognising that by 2050 half the world population may have myopia.9 Figure 1 shows the global prevalence of myopia predicted for the year 2050.
Myopia and vision loss
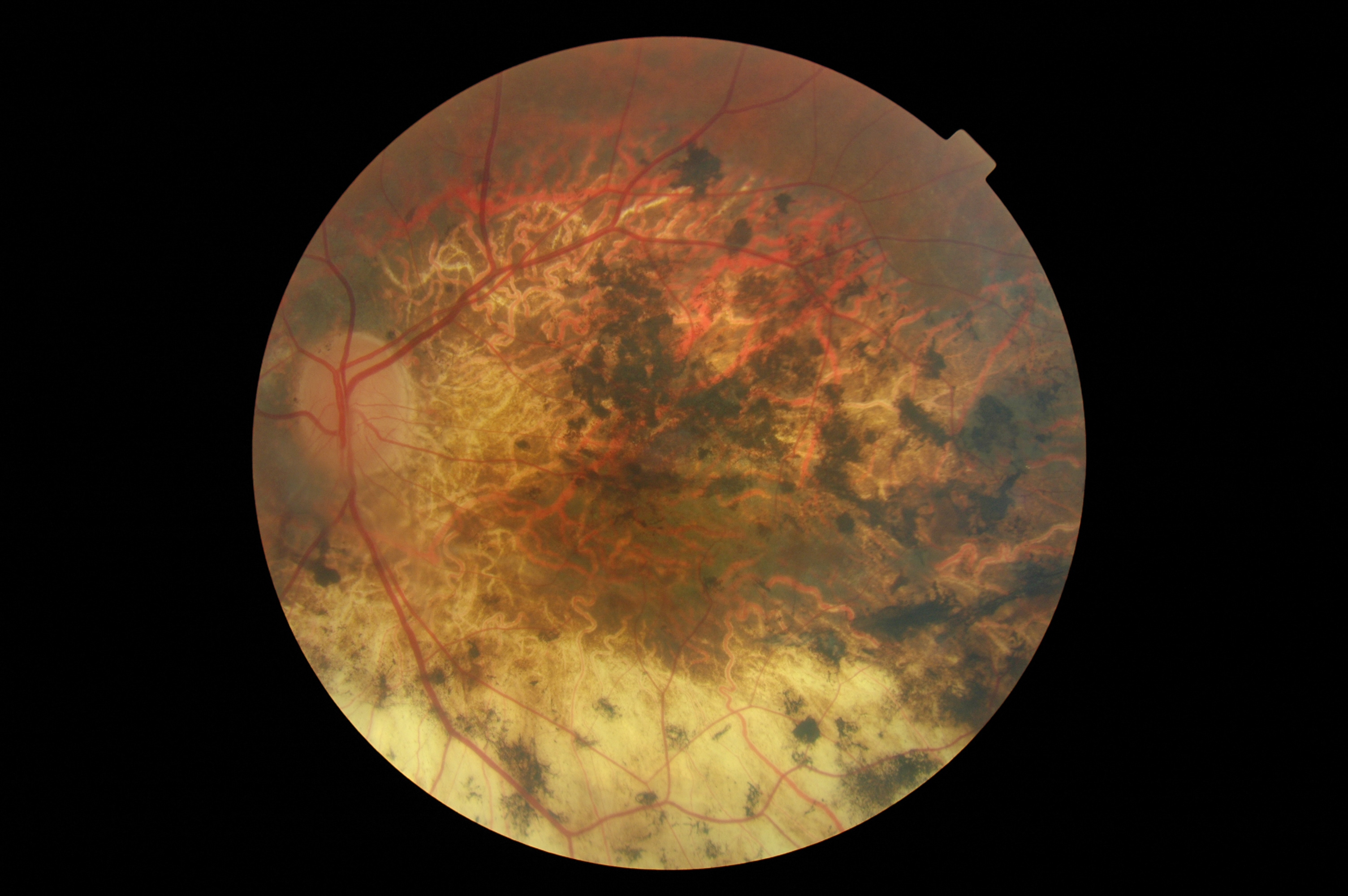
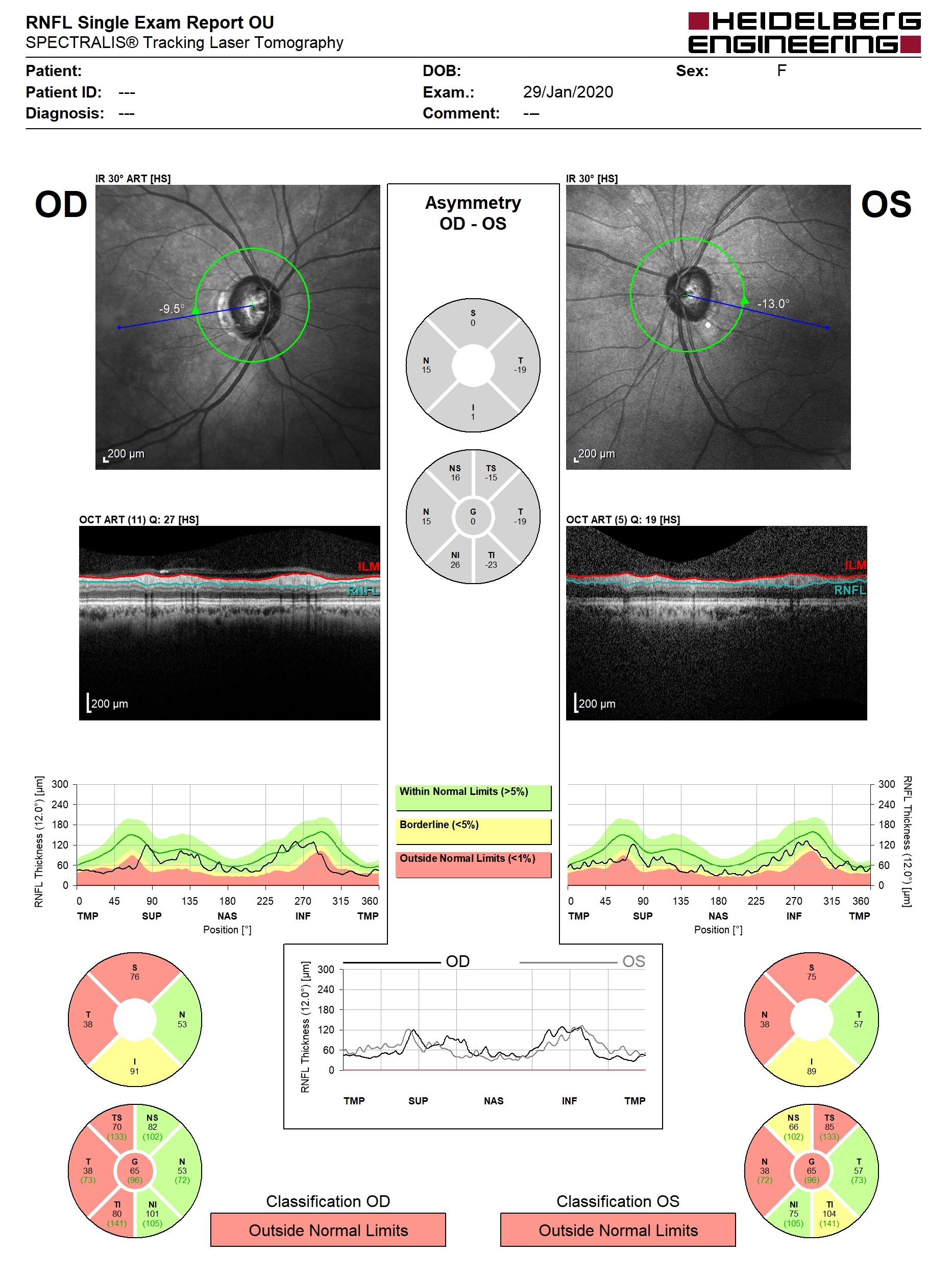
With increasing prevalence of myopia, including an increasing prevalence of high myopia, the number of people suffering permanent loss of vision from complications in middle and older age is also on the rise. Myopia increases the lifetime risk of permanent sight loss from retinal detachment, myopic macular degeneration, and optic neuropathy (figure 2).10 The risk increases with the degree of myopia; in the Netherlands, people with more than -6.00 DS have been reported to have a 39% risk of permanent sight loss by the age of 75 years.10
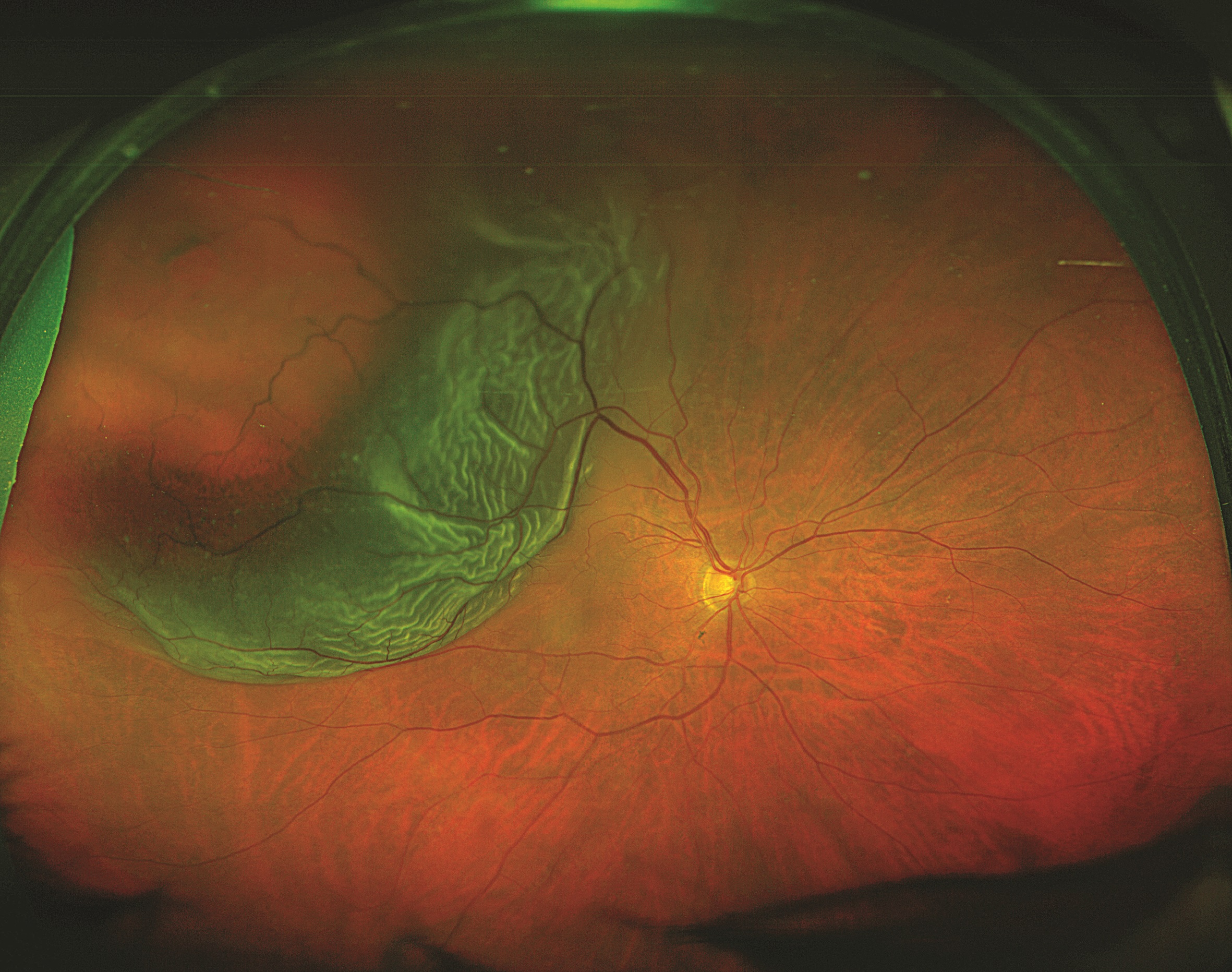
Figure 2: Myopia increases the lifetime risk of permanent sight loss from (above) retinal detachment, (below) myopic macular degeneration, and (bottom) optic neuropathy
Already by 2013, the UK National Ophthalmology Database study of vitreoretinal surgery found that half of the annual 12,000 vitreoretinal interventions were for retinal tears and rhegmatogenous retinal detachments (detachments caused by retinal breaks), which are usually myopia complications.11 More recently, in the Netherlands, an annual increase in retinal detachment repairs mirroring the rising prevalence of myopia has been observed.12
As early as 1998, the Rotterdam Study reported macular degeneration to be the predominant cause of sight impairment in people younger than 75 years.13 According to the UK National Institute for Clinical Excellence, 200,000 people in the UK have pathological myopia, around 0.3% of the population.14 While it is not known how many may develop choroidal neovascularisation, of those who do develop myopic maculopathy in one eye, 30% will develop it in the other eye within eight years.14 In Russia, the prevalence of myopic maculopathy is 1.3%, with associated moderate to severe vision impairment or blindness in 47%.15 In France, in a clinical setting, myopic maculopathy has been observed in 4.27% of patients with myopia greater than -10.00DS, and in 0.5% of those with myopia between -6.00DS and -10.00DDS, leading to a prevalence of certifiable sight impairment or blindness in 10.1% of those with myopia greater than -10.00DS.16 At 60 years old or over, the prevalence of blindness or vision impairment was 25.71% and 9.75%, respectively, in these two groups.16
Unfortunately, national sight loss registers mostly do not distinguish between age-related and myopia-related macular degeneration, and do not collect information on refractive errors at the time of sight impairment certification. Figures for myopia-related sight loss are therefore often an estimate. Global modelling indicated that in 2018, 32% of moderate to severe sight impairment and 47% of blindness were associated with myopia, with a projected increase to 35% and 61%, respectively, by 2050.17 In Western Europe, between 2000 and 2050, the age-standardised prevalence of visual impairment associated with myopic maculopathy across all ages is estimated to increase from 0.01 to 0.05%, and that of blindness from 0.002 to 0.012%.18
Impact of myopia
From its onset, myopia incurs costs that are borne either by children’s parents/carers or their healthcare systems. As adults, people continue to require spectacles and contact lenses, with some opting for corrective refractive surgery.
Major costs are linked to secondary complications and their treatments, as well as to irreversible sight loss with its impact on productivity and quality of life. The UK National Health Service currently spends £3 billion a year on eye care, and the cost of sight loss is £15.8 billion per year; specific figures for myopia-associated costs are not available.19
Globally, in 2015, the potential productivity loss from myopic macular degeneration was estimated at $6 billion.20 Worldwide, in 2018 direct, productivity and social security costs associated with myopia exceeded $670 billion and were estimated to rise to $1.7 trillion, putting its costs ahead of heart failure and lung or breast cancer.17
Development of myopia
The common form of myopia, with onset and progression in childhood and teenage years, is caused by a gradual elongation of the eye. It follows on from the normal eye growth from birth to around seven years, when the eye length increases from around 16-18mm to 22mm, with the fastest increase during the first two years of life.21,22 While the rate of elongation typically slows down during childhood and the teenage years, a significant minority of children now experience further rapid axial growth with resulting myopia.23,24
This axial elongation is driven by both genetic and environmental factors. Children whose parents are short-sighted have a higher risk of developing myopia, as do those who spend little time outdoors and much time on near vision activities. Some epidemiological studies also observed that children in families in lower socioeconomic circumstances have a higher risk.3 Children with myopia tend to spend less time outdoors than their normal-sighted peers, and lack of sunlight linked with an increasingly urban lifestyle is a key environmental risk factor for the earlier onset of myopia.3,25,26
Sunlight has higher intensity than any indoor lighting, and light falling onto the retina releases the neuro-chemical dopamine. In animal models, dopamine release triggers a signalling pathway from retina to sclera, which slows down eye elongation.27,28 In humans, genome-wide association studies have identified many genetic variants associated with myopia that are light-dependent and related to cell-cycle and growth pathways, underlining the critical importance of the light environment in the development of myopia.29
Causes of myopia
People who were children in the 1970s are likely to remember spending their afternoons outside with friends and no or little adult supervision. Since then, childhood has become far more structured, with adult-led after-school activities, many of which take place indoors. Many schools have sold their playing fields to housing developers. UK surveys indicate that children today spend 68 minutes a day outdoors or on sports, including indoor sports.30 Children from ethnic minority and socioeconomically disadvantaged communities spend less time outdoors than their more affluent peers, with 7% spending time in green and natural spaces less than once a month.31 Conversely, access to green spaces in urban areas is associated with a reduced prevalence of spectacle wear in children, as observed in Barcelona, Spain.32
In addition to a lack of time spent outdoors, increased near-vision activities and education are considered an additional environmental risk factor for myopia development, though the causal relationship is less clear.26,35,6 Educational pressure has increased and many parents invest in after-school tutoring offered in supermarkets, shopping centres and on the high street. Some children may also receive additional lessons to acquire extra-curricular skills and knowledge. Electronic devices, which are ever decreasing in size, have entered the mass market and the rise in myopia prevalence parallels the rise in the use of interactive electronic devices. In the UK, children and young people age five to 15 years spend on average two hours per day online and two hours watching TV.36 Children use electronic media to be in touch with their friends, for gaming and other leisure activities.37
Two-thirds of 12 to 15-year-olds use their phone in bed and a third can access a tablet computer in bed.36 Screen use by children in the UK is the second-highest in the world, at 44 hours per week.33 By the age of seven years, they will have spent twice a long looking at screens (four hours per day) than playing outside (two hours per day).38,39 At the same time as spending more time on screens, children and young people spend less time outdoors and on sports (figure 3).34 Smartphones are now available to many,40 and increased smartphone data usage is associated with myopia.41 The rise of electronic devices and lack of outdoor activities is not only linked with myopia, but also to sleep problems and increasing levels of anxiety and obesity, particularly in ethnic minority groups and poorer communities.39,42,43
Is myopia preventable?
If, at population level, myopia is largely caused by environmental factors, can it be prevented in the individual child? There are two parts to this problem:
- Identifying those at risk
- Taking preventative action
Identifying risk
Identifiable predictive factors include parental myopia and a greater axial length and lower refractive error than age-peers.44,45 However, these are not evaluated in current vision screening programmes. While vision screening is available in many European countries and regions, variations in funding, target age group and tests used persist.46 Many are linked to other public-health initiatives to assess child health. All aim to detect reduced visual acuity, typically in children approaching school entry who are old enough to cooperate with optotype-based assessment by lay screeners. However, as in Europe, myopia typically develops after the age of six years and neither parental myopia nor the child’s refraction are routinely evaluated, current screening programmes will not be able to identify children at risk of developing myopia. However, eye examinations for children by ECPs may be available free of charge, if covered by a national health programme.
Local ECPs are the first point of call when parents/carers or teachers are concerned about a child’s eyesight. Nevertheless, parents/carers from communities perceived as ‘hard to reach,’ for example ethnic minority and socio-economically disadvantaged groups, may not know about the availability of these services, or may be reluctant to engage with them, due to language and
cultural barriers. In general, parents also tend not be aware of complications of myopia in later life,47 and may therefore not seek advice until the child manifestly struggles with distance vision. Eye health education in schools, provided as part of mainstream education or by local campaigns, such as the ‘Eye Heroes’, can help spread the word within communities.48,49
Prevention
The second part of the problem is how to prevent or delay the onset of myopia in those at risk. Clinical trials in East Asia have shown that myopia onset can be delayed by children spending more time outdoors, though the effect on myopia progression is small.50,51,35 From these trials comes the recommendation of spending around 1.5 hours a day outdoors, as advocated by the Recess Outside Classroom Trial 711 (ROCT711) programme. Over seven days, this adds up to 11 hours.50 A meta-analysis calculated that every additional hour of outdoor time per week is associated with a 2% reduction in the risk of myopia onset.52
While strong evidence for a therapeutic effect of outdoor light is yet lacking for children in Europe, it is generally recommended that children should spend more time outdoors.53 Some ECPs recommend eye rests during prolonged near work, such as the 20-20-20 rule: rest your eyes for 20 seconds, looking at something 20 metres away, after every 20 minutes of near work. This advice was originally developed for addressing some of the problems arising from digital screen use, usually termed computer vision syndrome or digital eye strain.54
No intervention, other than ‘more time outdoors’, has been tested in pre-myopic children. It may be some time until the ethical question of whether an intervention that can potentially cause problems (blurred near vision, light sensitivity from pharmaceutical interventions and the rare, but serious complication of keratitis from contact lens wear) is justified in children who do not yet have the target condition.
Conclusion
Myopia can no longer be considered as a mere inconvenience. Increasing prevalence and severity will place an increasing burden on individual quality of life and cause a rise in healthcare expenditure to both individuals and healthcare systems across Europe. Early detection of predictive factors may enable families to delay the onset of myopia by engaging with outdoor activities. As the evidence of the burden of the condition on individuals and society increases and low-risk interventions emerge, the identification of children at risk of developing myopia and pre-emptive management options may become ethically acceptable.
- Dr Annegret Dahlmann-Noor is the director of the children’s eye service at Moorfields Eye Hospital in London where she also acts as Director of Children’s Eye Services Lead for Clinical Trials with Children, National Institute for Health Research based in the Moorfields Biomedical Research Centre.
This article was first published in March 2021 as part of a Special Hospital Report, ‘Advancing the Treatment of Myopia in Children’ by Global Business Media, supported by CooperVision. Inc.
References
- Wong K, Dahlmann-Noor A. Myopia and its progression in children in London, UK: a retrospective evaluation. Journal of Optometry 2020;13:146–54. doi:10.1016/j.optom.2019.06.002
- McCullough SJ, O’Donoghue L, Saunders KJ. Six Year Refractive Change among White Children and Young Adults: Evidence for Significant Increase in Myopia among White UK Children. PLoS ONE 2016;11. doi:10.1371/journal.pone.0146332
- Tideman JWL, Polling JR, Jaddoe VWV, et al. Environmental Risk Factors Can Reduce Axial Length Elongation and Myopia Incidence in 6- to 9-Year-Old Children. Ophthalmology 2019;126:127–36. doi:10.1016/j.ophtha.2018.06.029
- Matamoros E, Ingrand P, Pelen F, et al. Prevalence of Myopia in France. Medicine (United States) 2015;94:e1976. doi:10.1097/MD.0000000000001976
- Lundberg K, Suhr Thykjær A, Søgaard Hansen R, et al. Physical activity and myopia in Danish children—The CHAMPS Eye Study. Acta Ophthalmologica 2018;96:134–41. doi:10.1111/aos.13513
- Williams KM, Bertelsen G, Cumberland P, et al. Increasing Prevalence of Myopia in Europe and the Impact of Education. Ophthalmology 2015;122:1489–97. doi:10.1016/j.ophtha.2015.03.018
- Williams KM, Verhoeven VJM, Cumberland P, et al. Prevalence of refractive error in Europe: the European Eye Epidemiology (E3) Consortium. European Journal of Epidemiology 2015;30:305–15. doi:10.1007/s10654-015-0010-0
- WHO. The impact of myopia and high myopia. In: Joint World Health Organization - Brien Holden Vision Institute (WHO-BHVI) Global Scientific Meeting on Myopia Sydney, Australia. 2015.
- Holden BA, Fricke TR, Wilson DA, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016;123:1036–42. doi:10.1016/j.ophtha.2016.01.006
- Tideman JWL, Snabel MCC, Tedja MS, et al. Association of axial length with risk of uncorrectable visual impairment for europeans with myopia. JAMA Ophthalmology 2016;134:1355–63. doi:10.1001/jamaophthalmol.2016.4009
- Jackson TL, Donachie PHJ, Sparrow JM, et al. United Kingdom National Ophthalmology Database Study of Vitreoretinal Surgery: Report 1; Case mix, complications, and cataract. Eye (Basingstoke) 2013;27:644–51. doi:10.1038/eye.2013.12
- van Leeuwen R, Haarman AEG, van de Put MAJ, et al. Association of Rhegmatogenous Retinal Detachment Incidence With Myopia Prevalence in the Netherlands. JAMA Ophthalmology Published Online First: 25 November 2020. doi:10.1001/jamaophthalmol.2020.5114
- Klaver CCW, Wolfs RCW, Vingerling JR, et al. Age-specific prevalence and causes of blindness and visual impairment in an older population: The Rotterdam study. Archives of Ophthalmology 1998;116:653–8. doi:10.1001/archopht.116.5.653
- Appendix B National Institute for Health and Care Excellence Final scope for the appraisal of ranibizumab for the treatment of choroidal neovascularisation associated with pathological myopia. 2013.
- Bikbov MM, Gilmanshin TR, Kazakbaeva GM, et al. Prevalence of Myopic Maculopathy Among Adults in a Russian Population. JAMA network open 2020;3:e200567. doi:10.1001/jamanetworkopen.2020.0567
- Leveziel N, Marillet S, Dufour Q, et al. Prevalence of macular complications related to myopia – Results of a multicenter evaluation of myopic patients in eye clinics in France. Acta Ophthalmologica 2020;98:e245–51. doi:10.1111/aos.14246
- Predicting Costs and Disability from the Myopia Epidemic – A Worldwide Economic and Social Model. | IOVS | ARVO Journals. https://iovs.arvojournals.org/article.aspx?articleid=2744765 (accessed 28 Nov 2020).
- Fricke TR, Jong M, Naidoo KS, et al. Global prevalence of visual impairment associated with myopic macular degeneration and temporal trends from 2000 through 2050: Systematic review, meta-analysis and modelling. British Journal of Ophthalmology 2018;102:855–62. doi:10.1136/bjophthalmol-2017-311266
- Pezzullo L, Streatfeild J, Simkiss P, et al. The economic impact of sight loss and blindness in the UK adult population. BMC Health Services Research 2018;18. doi:10.1186/s12913-018-2836-0
- Naidoo KS, Fricke TR, Frick KD, et al. Potential Lost Productivity Resulting from the Global Burden of Myopia: Systematic Review, Meta-analysis, and Modeling. Ophthalmology 2019;126:338–46. doi:10.1016/j.ophtha.2018.10.029
- GOLDSCHMIDT E. REFRACTION in the NEWBORN. Acta Ophthalmologica 1969;47:570–8. doi:10.1111/j.1755-3768.1969.tb08143.x
- Mutti DO, Sinnott LT, Lynn Mitchell G, et al. Ocular Component Development during Infancy and Early Childhood. Optometry and Vision Science 2018;95:976– 85. doi:10.1097/OPX.0000000000001296
- Tideman JWL, Polling JR, Vingerling JR, et al. Axial length growth and the risk of developing myopia in European children. Acta Ophthalmologica 2018;96:301– 9. doi:10.1111/aos.13603
- McCullough S, Adamson G, Breslin KMM, et al. Axial growth and refractive change in white European children and young adults: predictive factors for myopia. Scientific Reports 2020;10. doi:10.1038/s41598-020-72240-y
- Guggenheim JA, Northstone K, McMahon G, et al. Time outdoors and physical activity as predictors of incident myopia in childhood: A prospective cohort study. Investigative Ophthalmology and Visual Science 2012;53:2856–65. doi:10.1167/iovs.11-9091
- Morgan IG, French AN, Ashby RS, et al. The epidemics of myopia: Aetiology and prevention. Progress in Retinal and Eye Research. 2018;62:134–49. doi:10.1016/j.preteyeres.2017.09.004
- Zhou X, Pardue MT, Iuvone PM, et al. Dopamine signaling and myopia development: What are the key challenges. Progress in Retinal and Eye Research. 2017;61:60–71. doi:10.1016/j.preteyeres.2017.06.003
- Troilo D, Smith EL, Nickla DL, et al. Imi – Report on experimental models of emmetropization and myopia. Investigative Ophthalmology and Visual Science 2019;60:M31–88. doi:10.1167/iovs.18-25967
- Tedja MS, Wojciechowski R, Hysi PG, et al. Genome-wide association meta-analysis highlights light-induced signaling as a driver for refractive error. Nature Genetics 2018;50:834–48. doi:10.1038/s41588-018-0127-7
- Office_for_National_Statistics. Children’s engagement with the outdoors and sports activities. https://wwwonsgovuk/peoplepopulationandcommunity/wellbeing/datasets/childrensengagementwiththeoutdoorsandsportsactivities. 2018.
- Monitor of Engagement with the Natural Environment The national survey on people and the natural environment Children and Young People report-of- engagement-with-the-natural-environment-survey-purpose-and-results. 2019. https://www.gov.uk/government/collections/monitor (accessed 30 Nov 2020).
- Dadvand P, Sunyer J, Alvarez-Pedrerol M, et al. Green spaces and spectacles use in schoolchildren in Barcelona. Environmental Research 2017;152:256–62. doi:10.1016/j.envres.2016.10.026
- Check Out the Best Countries for Child Online Safety | DQ Institute. https://www.dqinstitute.org/child-online-safety-index/ (accessed 30 Nov 2020).
- Media use increases while outdoor time decreases among older children|Nature of Americans. https://natureofamericans.org/findings/viz/media-use- increases-while-outdoor-time-decreases-among-older-children (accessed 30 Nov 2020).
- Wildsoet CF, Chia A, Cho P, et al. IMI – Interventions myopia institute: Interventions for controlling myopia onset and progression report. Investigative Ophthalmology and Visual Science 2019;60:M106–31. doi:10.1167/iovs.18-25958
- Making sense of media. 2019.
- Dr FB, Klemera E, Chester K, et al. HBSC England National Report 2018|3. www.hbscengland.org (accessed 22 May 2020).
- Children spend twice as long looking at screens than playing outside, study finds|The Independent. https://www.independent.co.uk/life-style/children-screens-play-outside-computer-
phone-time-healthy-games-a8603411.html (accessed 14 May 2020). - Perkins C, DeSousa E. Trends in childhood height and weight, and socioeconomic inequalities. The Lancet Public Health. 2018;3:e160–1. doi:10.1016/S2468- 2667(18)30050-1
- Poushter J. Smartphone Ownership and Internet Usage Continues to Climb in Emerging Economies | Pew Research Center. Pewglobal.orghttp://www.pewglobal.org/2016/02/22/smartphone-ownership-and-internet-usage-continues-to-climb-in-emerging-economies/ (accessed 15 May 2020).
- McCrann S, Loughman J, Butler JS, et al. Smartphone use as a possible risk factor for myopia. Clinical and Experimental Optometry Published Online First: 2020. doi:10.1111/cxo.13092
- Mental Health of Children and Young People in England, 2017 [PAS] - NHS Digital. https://digital.nhs.uk/data-and-information/publications/statistical/mental-health-of-children-
and-young-people-in-england/2017/2017 (accessed 22 May 2020). - Anujuo KO, Vrijkotte TGM, Stronks K, et al. Ethnic differences in sleep duration at 5 years, and its relationship with overweight and blood pressure. The European Journal of Public Health;26:1001–6. doi:10.1093/eurpub/ckw084
- Sheppard AL, Wolffsohn JS. Digital eye strain: Prevalence, measurement and amelioration. BMJ Open Ophthalmology. 2018;3. doi:10.1136/bmjophth-2018-000146
- Anshel JR. Visual ergonomics in the workplace. AAOHN journal:official journal of the American Association of Occupational Health Nurses. 2007;55:414–20. doi:10.1177/216507990705501004
- Sloot F, Hoeve HLJ, de Kroon MLA, et al. Inventory of current EU paediatric vision and hearing screening programmes. Journal of Medical Screening 2015;22:55–64. doi:10.1177/0969141315572403
- McCrann S, Flitcroft I, Lalor K, et al. Parental attitudes to myopia: a key agent of change for myopia control? Ophthalmic and Physiological Optics 2018;38:298–308. doi:10.1111/opo.12455
- Chang LC, Guo JL, Liao LL, et al. A coalition partnership of vision health through a health-promoting school program for primary school students in Taiwan. Global Health Promotion 2017;24:23–31. doi:10.1177/1757975915595347
- Y S, M R, AR B, et al. Eye Heroes: A Model of Raising Awareness about Eye Health by Training Children to Be Eye Health Champions. Journal of Community Medicine & Health Education 2018;08:1–5. doi:10.4172/2161-0711.1000639
- Wu PC, Chen CT, Lin KK, et al. Myopia Prevention and Outdoor Light Intensity in a School-Based Cluster Randomized Trial. Ophthalmology 2018;125:1239– 50. doi:10.1016/j.ophtha.2017.12.011
- He M, Xiang F, Zeng Y, et al. Effect of time spent outdoors at school on the development of myopia among children in China a randomized clinical trial. JAMA - Journal of the American Medical Association 2015;314:1142–8. doi:10.1001/jama.2015.10803
- Sherwin JC, Reacher MH, Keogh RH, et al. The association between time spent outdoors and myopia in children and adolescents: A systematic review and meta-analysis. Ophthalmology 2012;119:2141–51. doi:10.1016/j.ophtha.2012.04.020
- VisionUK. Myopia management consensus. 2018.
- Computer vision syndrome|AOA. https://www.aoa.org/healthy-eyes/eye-and-vision-conditions/computer-vision-syndrome?sso=y (accessed 18 Dec 2020).
