The previous article discussed myopia prevalence predicting that myopia may affect approximately 50% of the world’s population by the year 2050 based on trending myopia prevalence figures.1 Critical to minimising the irreversible visual impairment of myopia-related ocular pathologies are interventions to actively manage myopia.2 These interventions may prevent or delay the onset of myopia, or halt or slow its progression.3 The physiological axial length changes associated with the progression of myopia is the precipitating factor in sight-threatening ocular conditions such as retinal detachment. Consequently, any intervention to slow myopia progression must also reduce the rate of axial elongation of the eye.
Management strategies are growing in number with a significant body of research committed to enhancing and developing new approaches. However, we are at an exciting time whereby we can translate the evidence from research evidence through to commercially available interventions that can be used in clinical practice. This article highlights the research behind such interventions under three categories, behavioural, optical, and pharmacological and discusses the evidence to integrate these into clinical practice.
Behavioural interventions
Epidemiological and animal studies have suggested that an individual’s environment and lifestyle play a key role in myopia development.4
Time outdoors
There is a large body of epidemiological evidence that points to the protective effect of time outdoors in delaying or preventing the onset of myopia. A systematic review and meta-analysis found that the odds of myopia can be reduced by 2% per additional hour of time spent outdoors.5 Additionally, it has been found that different amounts of light exposure correlate with the axial growth rate of the eye.6
The research prompted three intervention trials to take place, all of which were based in China where the prevalence of myopia in school-aged children is as high as 60%.7 He et al,8 and Jin et al,9 introduced an extra 40 minutes of outdoor activity during the school day and both found a significant reduction in myopia progression of 11% and 18%, respectively. Wu et al introduced an additional 80 minutes per day and found a 23% reduction in
myopia progression and reported a reduction of 50% in the incidence of new myopic cases over a one-year period.10 This research supports the theory that increased time outdoors is influential in myopia development. The research evidence is stronger in terms of delaying the onset of myopia compared with slowing progression and this in itself is beneficial, as we know that the younger a child is when they develop myopia the greater the final amount of myopia is likely to be.11
The protective effect of time outdoors on myopia onset has been widely investigated however, despite this large body of supportive evidence the exact mechanism behind this protective effect is still unclear. It has been suggested that circadian rhythms and their associated hormones triggered by sunlight may play a role in myopic growth. The retinal dopamine system has been found to be involved in the control of eye growth and the production of dopamine in the retina is stimulated by light.12 Additionally, research has found that myopes have significantly higher levels of serum melatonin concentration than non- myopes.13 It may also be related to the different dioptric environment, we observe much greater distances when outdoors compared to the many close objects we view indoors.2
Despite the lack of certainty surrounding the mechanism of the protective effect of time outdoors, it should be considered as an effective and straightforward strategy to reduce the risk of myopia development in children. Countries in East Asia such as Singapore and Malaysia have launched campaigns to educate parents and promote time outdoors. Advocating a little extra time outdoors is better than none and it is ideally aimed at children not yet myopic but with a high risk of developing myopia.14
Near work
The other aspect of behaviour that has long been associated with myopia is near work. With the increase in use of digital devices, many parents question the impact on their child’s eyes. Evidence is equivocal as to whether there is any impact on myopia development and progression.15 Given the high association with near work the recommendation is to take regular breaks and increase working distance whenever possible (figure 1).16
 Figure 1: Children should be encouraged to take regular breaks from near work and increase time spent outdoors
Figure 1: Children should be encouraged to take regular breaks from near work and increase time spent outdoors
Interventions to slow myopia progression
For decades, we have corrected the visual error resulting from myopia with standard single vision spectacle or contact lenses. Current evidence supports optometrists to actively manage myopia in children through use of a range of options. The evidence of treatment efficacy is variable both between intervention strategies and among individuals; however, research is directed at improving efficacy and refining individual response.
Optical Interventions
Various optical approaches to myopia control have been developed and evaluated over the past few decades. Optical interventions to slow myopia progression have stemmed from two key theories that in relation to a connection between amount of blur the eye receives and myopia progression. The first theory proposes that excessive accommodative demand caused by near work and a small focussing error at near could be influential in myopia development. The second hypothesis is that even in the presence of a clear image centrally the amount and type of blur falling elsewhere on the retina may influence myopia development.
Spectacles
As a minimum children should have full correction of their myopia as there is some evidence that under-correction accelerates rate of growth of the eye and faster myopia progression.17 Numerous studies have investigated the impact of different designs of spectacle lenses on myopia progression. Early studies focused on the use of bifocal and progressive addition lenses. A modest reduction in myopia progression was found when compared with single vision spectacles.18 However, although these studies have found a statistically significant result their outcomes are less impactful clinically. For instance, the largest clinical trial of 469 children aged six to 11 years found a difference of 0.20DS myopic progression when comparing progressive addition lenses to controls;19 this change was over a three-year period and is, therefore, of limited value clinically. Interestingly, a study examining the effect of an executive bifocal found that over a three-year period the degree of myopia progression was reduced by 0.75DS equating to 39% compared to single vision spectacles and this was increased to 1.00DS (51%) with prismatic bifocals.20 However, the cosmetic appearance of executive bifocals may deter children and their parents from considering this option.
More recently some novel spectacle lenses have gained attention. One such design has a central zone that corrects for distance vision surrounded by micro lenses of a relatively more plus power have shown reduction in myopia progression and rate of axial length growth in two year randomised controlled trials compared with single vision spectacles. The efficacy of these lenses is around 50 to 60%.20 (https://www. opticianonline.net/features/in-focus-spectacle- lenses-that-slow-myopia-progression). Another novel design of spectacle lens using light scattering technology has shown promising one year clinical study results in slowing myopia progression in children.21 Spectacle lens options for myopia management are becoming available commercially in some parts of the world and are expected to be launched in the UK and Europe in the coming months.
Contact lenses
Different designs of contact lenses have been successful in slowing the progression of myopia. In addition to the myopia control benefits contact lens wear provides other advantages to children and adolescents who do not enjoy wearing spectacles (figure 2). As well as providing the necessary vision correction, they have been shown to improve vision-specific quality of life in myopic children younger than 12 years of age.22
 Figure 2: Children from as young as eight are able to confidently handle contact lenses
Figure 2: Children from as young as eight are able to confidently handle contact lenses
Orthokeratology
Orthokeratology (also known as orthoK) is an effective way to correct myopia through corneal reshaping with overnight wear of rigid gas permeable contact lenses. It has also been found to be a successful strategy in myopia control by causing central corneal flattening and paracentral corneal steepening, which alters the image shell and thus the type of blur falling on the retina (figure 3).
Two recent meta-analyses both concluded that orthokeratology can slow eye growth on average by 48%.23,24 Further studies have found between 32 to 63% reduction in myopia progression compared to controls.25,26 Most importantly, orthokeratology appears to slow axial elongation, which is the precipitating factor in many of the pathological consequences of myopia, such as retinal detachment. Cho and Cheung concluded that orthokeratology could reduce the risk of rapid axial elongation (>0.36mm/year) by 88.8%.27 There is large amount of research supporting orthokeratology as an effective and successful strategy for myopia control. The other advantage of orthokeratology is that children are then both spectacle and contact lens free during the daytime.
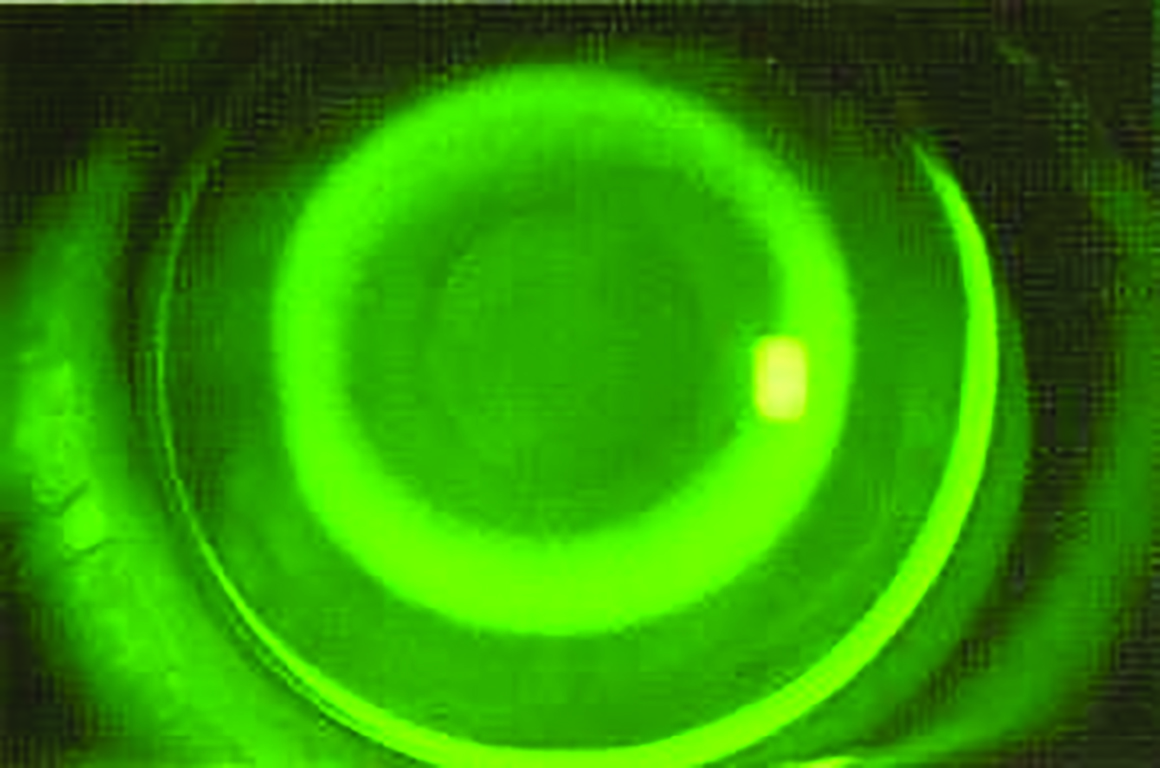 Figure 3: Orthokeratology lenses are fitted to promote the redistribution of epithelial cells when worn overnight, resulting in a central flattening and peripheral steepening of the cornea
Figure 3: Orthokeratology lenses are fitted to promote the redistribution of epithelial cells when worn overnight, resulting in a central flattening and peripheral steepening of the cornea
Multifocal and dual focus contact lenses
Both innovative myopia control specific soft contact lens designs and multifocal soft contact lenses (with a centre-distance design originally intended for presbyopia correction) have been trialled in children. A novel dual focus daily disposable contact lens, MiSight 1 day by CooperVision, has been licensed for myopia control use and is available commercially. It is CE marked in Europe and, in the US, it is the only FDA approved intervention for myopia control. The lens has a large central distance area and several concentric peripheral ‘treatment’ zones which create 2.00DS of relative peripheral myopic defocus.28 The simultaneous defocus from the distance and relative plus zones seems to slow the progression of myopia.
Recent data published from a three- year randomised double-masked multi-centre clinical trial involving 144 children aged eight to 12 years, found that the dual-focus contact lens was able to slow myopia progression by 59% and axial elongation by 52%.28 A recent study using multifocal soft contact lenses in children with myopia found treatment with high add power multifocal contact lenses significantly reduced the rate of myopia progression over 3 years compared with medium add power multifocal and single-vision contact lenses.29 Other designs of soft contact lenses have also shown promising results for myopia management.30,31 Multifocal and dual focus contact lenses are an effective interventional strategy for practitioners working in primary care to implement and actively manage myopia progression in children.
Pharmacological Interventions
Atropine
Atropine has been widely investigated in myopia control research for decades. It is a non-selective muscarinic receptor antagonist which causes mydriasis and cycloplegia. The typical indication is for 1% atropine eye drops to be used in children to treat inflammation, as a potent cycloplegic agent or for penalisation treatment in amblyopia (www.medicines.org.uk/). The majority of research with atropine in the field of myopia stems from East Asia and in particular Singapore.
The Atropine for Treatment of Myopia (ATOM) study investigated the efficacy of using 1.0% atropine for myopia control.32 It found that children who used 1.0% atropine had a significantly reduced myopic progression over a two-year period; however, a rebound effect was found after cessation of treatment. This study was followed up by ATOM2 which compared three lower doses of atropine 0.5%, 0.1% and 0.01%.33 Over a five-year period the 0.01% atropine dose was found to be the most effective in slowing myopia progression with an overall progression of -1.38DS compared to -1.83DS in the 0.1% dose group, and -1.98DS in the 0.5% dose group; the 0.01% dose also showed less of a rebound effect. Furthermore, atropine at the lowest dose demonstrated the least number of side effects compared to the higher doses, in particular there was minimal impact on pupil size and accommodation.34 There are some queries, however, over the impact of this low concentration of atropine on axial length progression suggesting that we do not currently know the optimum concentration of atropine for use in management of myopia. In Europe there are a number of ongoing trials using low concentrations of atropine to determine the efficacy in European populations.35 It should be noted that the mechanism behind this myopic control strategy is not well understood at this stage.
Other pharmaceutical interventions
Other pharmaceutical options that have been used in clinical trials are pirenzepine and 7-methylzanthine. Pirenzepine is also an anti-muscarinic drug that has been used in the treatment of gastric ulcers. It is more selective than atropine and as such produces fewer side effects, such as photophobia and blurred near vision.36 Studies in the US and Singapore have found a reduction in myopia progression of approximately 50%.18 However, it is not currently approved for commercial use in myopia control in any countries.
7-methylxanthine (7-mx) is a metabolite of caffeine and theobromine that is created when coffee or chocolate is consumed. Animal studies have found that 7-mx thickens the sclera by increasing the diameter of the scleral collagen fibrils. A study of children aged eight to 13 years in Denmark investigated the effect of a 400mg dose of 7-mx taken twice a day.37 After a year, the myopia progression was reduced by 44% compared to a placebo. It appears to have a low toxicity and minimal side effects and, therefore, further work in this area could identify a prospective myopia control intervention.
It should be remembered that with any pharmacological intervention, the child would still require an optical correction for their myopia to allow them to see clearly in the distance. Therefore, a natural question would be to consider if combination therapies could be additive in their effect. Work is underway with both optical and atropine interventions with some supportive evidence emerging.38
Conclusions
This review highlights that, although no single treatment is 100% effective in all patients, substantial benefit is obtained in terms of slowing the rate of myopia progression in children. Myopia management is time sensitive, with greater impact on younger children. By slowing myopia progression and rate of axial length growth in a child’s eye, we not only benefit the individual from reduced risk of future ocular pathology but make gains on a public heath scale.
The next article in this series on myopia will explore the risk and benefits of myopia management in more detail. Myopia management is a rapidly advancing field with new evidence and strategies emerging. In the meantime, we have access to a range of interventions with good evidence that should inform our clinical practice and ensure that myopia management becomes the standard of care for children with myopia.
- Professor Nicola Logan is Reader in Optometry at Aston University and a internationally renowned authority in myopia research.
- This article was first published in March 2021 as part of a Special Hospital Report, ‘Advancing the Treatment of Myopia in Children’ by Global Business Media, supported by CooperVision. Inc.
References
- Holden BA, Fricke TR, Wilson DA, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-1042.
- Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012;31(6):622-660.
- Wildsoet CF, Chia A, Cho P, et al. IMI – Interventions myopia institute: Interventions for controlling myopia onset and progression report. Investi Ophthalmol Vis Sci. 2019;60(3):M106-M131.
- Sherwin JC, Reacher MH, Keogh RH, Khawaja AP, Mackey DA, Foster PJ. The association between time spent outdoors and myopia in children and adolescents: a systematic review and meta-analysis. Ophthalmology. 2012;119(10):2141-2151.
- Read SA, Collins MJ, Vincent SJ. Light Exposure and Eye Growth in Childhood. Invest Ophthalmol Vis Sci. 2015;56(11):6779-6787.
- Zhou W-J, Zhang Y-Y, Li H, et al. Five-Year Progression of Refractive Errors and Incidence of Myopia in School-Aged Children in Western China. J Epidemiol. 2016;26(7):386—395.
- He M, Xiang F, Zeng Y, et al. Effect of time spent outdoors at school on the development of myopia among children in China a randomized clinical trial. JAMA Opthalmology. 2015;314(11):1142-1148.
- Jin JX, Hua WJ, Jiang X, et al. Effect of outdoor activity on myopia onset and progression in school-aged children in northeast china: The sujiatun eye care study. BMC Ophthalmol. 2015;15(73).
- Wu PC, Tsai CL, Wu HL, Yang YH, Kuo HK. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology. 2013;120(5):1080-1085.
- Chua SY, Sabanayagam C, Cheung YB, et al. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol Opt. 2016;36(4):388-394.
- Feldkaemper M, Schaeffel F. An updated view on the role of dopamine in myopia. Exp Eye Res. 2013;114:106-119.
- Kearney S, O’Donoghue L, Pourshahidi LK, Cobice D, Saunders KJ. Myopes have significantly higher serum melatonin concentrations than non-myopes. Ophthalmic Physiol Opt. 2017;37(5):557-567.
- Morgan IG, French AN, Ashby RS, et al. The epidemics of myopia: Aetiology and prevention. Prog Retin Eye Res. 2018;62:134-149.
- Lanca C, Saw SM. The association between digital screen time and myopia: A systematic review. Ophthalmic Physiol Opt. 2020;40(2):216-229.
- Huang H-M, Chang DS-T, Wu P-C. The Association between Near Work Activities and Myopia
- Logan NS, Wolffsohn JS. Role of un-correction, under-correction and over-correction of myopia as a strategy for slowing myopic progression. Clin Exp Optom. 2020;103(2):133-137.
- Walline JJ, Lindsley KB, Vedula SS, et al. Interventions to slow progression of myopia in children. Cochrane Database Syst Rev. 2020;(1).
- Gwiazda J, Hyman L, Hussein M, et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci. 2003;44(4):1492-1500.
- Cheng D, Woo GC, Drobe B, Schmid KL. Effect of Bifocal and Prismatic Bifocal Spectacles on Myopia Progression in Children: Three-Year Results of a Randomized Clinical Trial. JAMA Ophthalmol. 2014;132(3):258-264.
- Lam CSY, Tang WC, Tse DY, et al. Defocus Incorporated Multiple Segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial. Br J Ophthalmol. 2020;104(3):363-368.
- Rappon J, Neitz J, Neitz M, Young G CT. Safety and Efficacy from a Pivotal Study of Novel Spectacle Lenses Designed to Reduce Myopia Progression. Optom Vis Sci. 2020;97:E-abstract 200036.
- Rah MJ, Walline JJ, Jones-Jordan LA, et al. Vision specific quality of life of pediatric contact lens wearers. Optom Vis Sci. 2010;87(8):560-566.
- Si JK, Tang K, Bi HS, Guo DD, Guo JG, Wang XR. Orthokeratology for myopia control: a meta-analysis. Optom Vis Sci. 2015;92(3):252-257.
- Sun Y, Xu F, Zhang T, et al. Orthokeratology to control myopia progression: a meta-analysis. PLoS One. 2015;10(4):e0124535.
- Charm J, Cho P. High myopia-partial reduction ortho-k: a 2-year randomized study. Optom Vis Sci. 2013;90(6):530-539.
- Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutiérrez-Ortega R. Myopia control with orthokeratology contact lenses in Spain: refractive and biometric changes. Invest Ophthalmol Vis Sci. 2012;53(8):5060-5065.
- Cho P, Cheung SW. Protective Role of Orthokeratology in Reducing Risk of Rapid Axial Elongation: A Reanalysis of Data From the ROMIO and TO-SEE Studies. Invest Ophthalmol Vis Sci. 2017;58(3):1411-1416.
- Chamberlain P, Peixoto-De-Matos SC, Logan NS, Ngo C, Jones D, Young G. A 3-year Randomized Clinical Trial of MiSight Lenses for Myopia Control. Optom Vis Sci. 2019;96(8):556-567.
- Walline JJ, Walker MK, Mutti DO, et al. Effect of High Add Power, Medium Add Power, or Single-Vision Contact Lenses on Myopia Progression in Children: The BLINK Randomized Clinical Trial. Jama. 2020;324(6):571-580
- Cooper J, O’Connor B, Watanabe R, et al. Case Series Analysis of Myopic Progression Control With a Unique Extended Depth of Focus Multifocal Contact Lens. Eye Contact Lens. 2018;44(5):e16-e24.
- Lam CS, Tang WC, Tse DY, Tang YY, To CH. Defocus Incorporated Soft Contact (DISC) lens slows myopia progression in Hong Kong Chinese schoolchildren: a 2-year randomised clinical trial. Br J Ophthalmol. 2014;98(1):40-45.
- Chua WH, Balakrishnan V, Chan YH, et al. Atropine for the treatment of childhood myopia. Ophthalmology. 2006;113(12):2285-2291.
- Chia A, Chua WH, Cheung YB, et al. Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2). Ophthalmology. 2012;119(2):347-354.
- Loughman J, Flitcroft DI. The acceptability and visual impact of 0.01% atropine in a Caucasian population. Br J Ophthalmol. 2016;100(11):1525-1529.
- Azuara-Blanco A, Logan N, Strang N, et al. Low-dose (0.01%) atropine eye-drops to reduce progression of myopia in children: A multicentre placebo- controlled randomised trial in the UK (CHAMP-UK) - Study protocol. Br J Ophthalmol. 2020;104(7):950-955.
