This is the second part of two articles in which the role that multifocal contact lenses (MFCLs) can play in the correction of presbyopia is examined. In part one, an overview was provided of current attitudes and beliefs relating to presbyopia and MFCLs, requirements for presbyopic CL correction, MFCL design options and performance comparisons with monovision CL correction. Part two covers prescribing trends for both MFCLs and 1 day CLs, recommendations for prescribing, supplemental fitting tools and patient satisfaction with MFCLs.
Prescribing trends for MFCLs
In 2011, Morgan et al published the results of international surveys conducted to determine world-wide patterns of fitting CLs for the correction of presbyopia over a preceding five-year period.1 The authors reported that at this time there appeared to be significant under-prescribing of CLs for the correction of presbyopia, but that for those fitted with CLs, three times more MFCL were prescribed compared with CLs for monovision correction. The International Contact Lens Prescribing Trends Consortium has continued to conduct the surveys each year since 2003 and a recent report evaluating seven key markets (169,440 fits across all ages: Australia, Canada, Japan, Netherlands, Norway, United Kingdom, United States) showed an increase in fits to presbyopes from about 20% of all fits to about 35% in 2019.2,3
Figure 1 illustrates these findings, along with MFCLs and monovision CLs that were fitted as a proportion of all soft lens fits. Although presbyopic wearers account for 35% of all fits, only about 20% of lenses are either MFCLs or monovision, since a significant number of presbyopes are still fitted with single vision CLs used in conjunction with spectacles for reading. In 2003, only 30% of presbyopes received a multifocal or monovision correction; however, this increased to 58% in 2019, mainly due to the increase in MFCL prescribing, and the increased availability of 1 day MFCLs. Furthermore, the prescribing of MFCLs was found to be relatively high in young presbyopes (45-54 years) and mid presbyopes (55-64 years) but less commonplace in older presbyopes (age 65+ years). While MFCL fitting has increased significantly over the past 17 years, prescribing of these lenses is still relatively low, highlighting that they are under-indexed in the vision correction category compared to their potential. There is undoubtedly a huge opportunity for eye care professionals (ECPs) to prescribe more MFCLs.
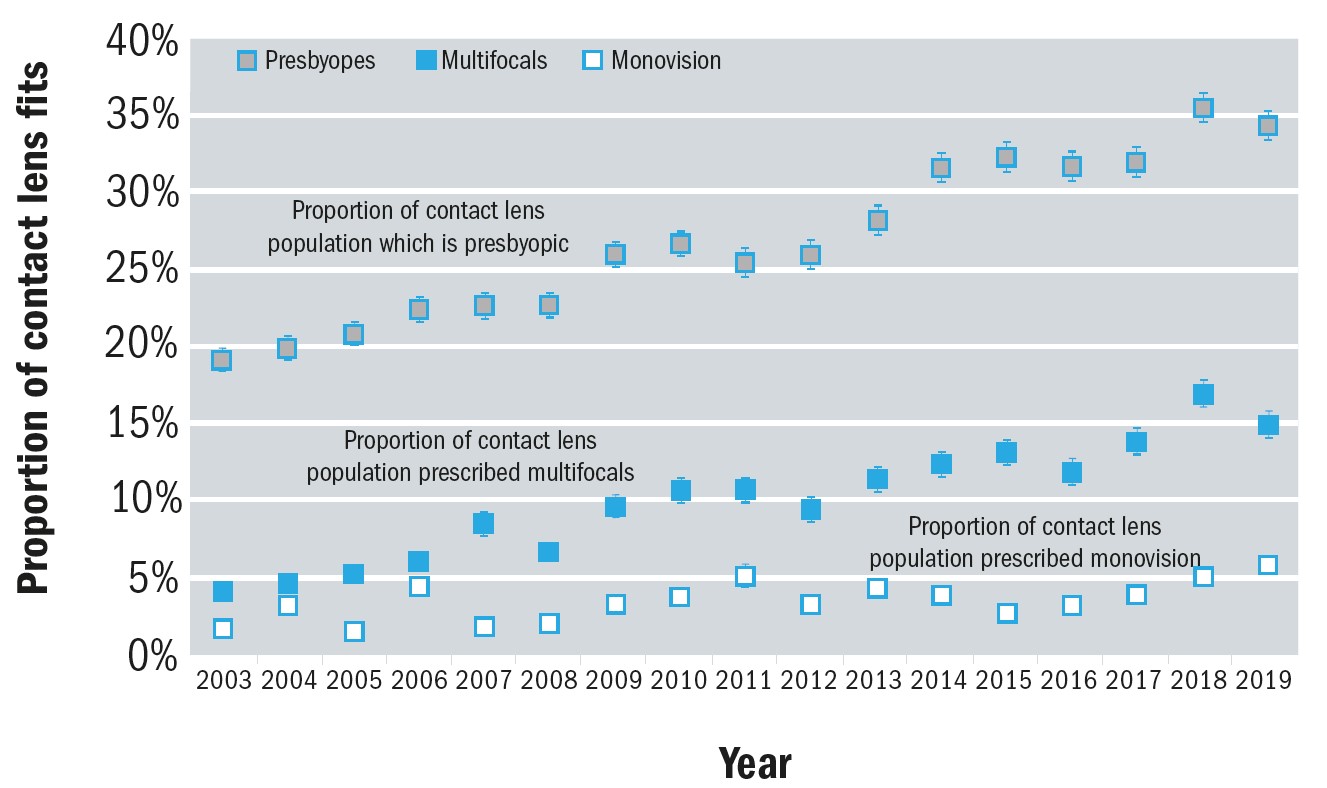 Figure 1: Various metrics about contact lens fitting to presbyopes. Upper symbols show that the fraction of contact lenses prescribed to presbyopes has increased 2003-19. The middle symbols reveal that, taken as a proportion of all contact lens fits, the number of multifocals has also risen significantly. The lower symbols suggest that the proportion of all contact lens fits described as ‘monovision’ has remained approximately static over this time period2
Figure 1: Various metrics about contact lens fitting to presbyopes. Upper symbols show that the fraction of contact lenses prescribed to presbyopes has increased 2003-19. The middle symbols reveal that, taken as a proportion of all contact lens fits, the number of multifocals has also risen significantly. The lower symbols suggest that the proportion of all contact lens fits described as ‘monovision’ has remained approximately static over this time period2
According to the International CL Prescribing Trends Consortium, MFCL prescribing has increased from approximately 25% of lenses fitted to presbyopes in 2005 to around 50% in 2020 (figure 2), with a further 10% of this group being prescribed CLs for monovision.4 This suggests that close to 40% of presbyopes were being fitted with single vision, distance-only correction, presumably to be used in conjunction with spectacles for reading. The Consortium also reported that overall, them proportion of presbyopes within the cohort of CL fittings has increased over the past 15 years.4
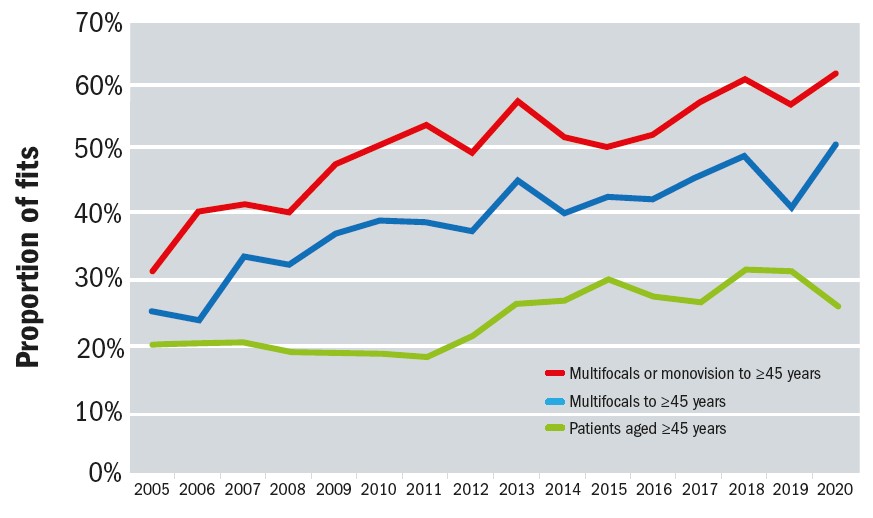 Figure 2: Prescribing of MFCLs (blue line) and combined MFCL/monovision CLs (red line) when presbyopes are fitted. Also shown is the proportion of CL fits to people aged 45 years and over (green line). Data from 18 markets: Australia, Belgium, Canada, Czech Republic, Denmark, Spain, Hungary, Israel, Japan, Lithuania, Netherlands, Norway, New Zealand, Portugal, Sweden, Taiwan, UK and USA (after Morgan et al 20214)
Figure 2: Prescribing of MFCLs (blue line) and combined MFCL/monovision CLs (red line) when presbyopes are fitted. Also shown is the proportion of CL fits to people aged 45 years and over (green line). Data from 18 markets: Australia, Belgium, Canada, Czech Republic, Denmark, Spain, Hungary, Israel, Japan, Lithuania, Netherlands, Norway, New Zealand, Portugal, Sweden, Taiwan, UK and USA (after Morgan et al 20214)
Prescribing trends for 1 day CLs
It is 25 years since the introduction of 1 day CLs,5,6 and in 2020 an average of 46% of soft lenses prescribed were 1 day lenses.7 Figure 3 provides a summary of soft CL prescribing patterns for daily wear (DW) and extended wear (EW) from surveys conducted each year by the International CL Prescribing Trends Consortium.8 While patient fits in reusable daily wear hydrogels (H) has steadily declined, the proportion of patients fitted with reusable silicone hydrogel (SiH) CLs has gradually increased over the years, plateauing around 10 years ago. Prescribing of hydrogel 1 day, or daily disposable (DD), lenses has remained relatively constant over the past two decades, but the prescribing rates of SiH 1 day CLs has been steadily increasing since their introduction to the market in 2008.9 Interestingly, despite ECPs clearly recognising the health benefits of 1 day SiH CLs10, in 2019 only around 60% of 1 day CLs prescribed were reported to be SiH materials as compared with around 90% of monthly replacement CLs.3 The attitude may be different for presbyopic CL wearers though, and in a survey conducted among 300 ECPs in the US, UK and Japan 75% of the ECPs agreed that SiH should be the material of choice and a 1 day modality, the optimal CL for their multifocal patients.10
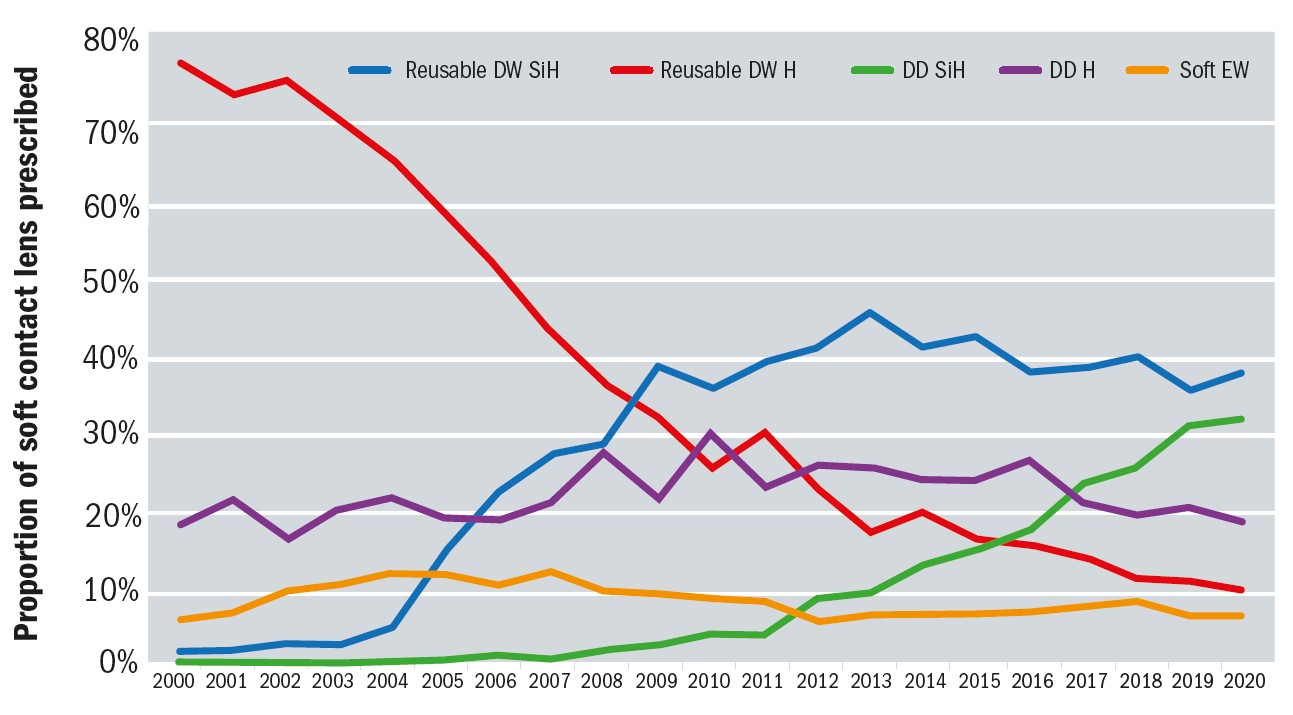 Figure 3: International Prescribing of Soft Contact Lenses 2001 to 2020. Data provided by the International Contact Lens Prescribing Trends Consortium8
Figure 3: International Prescribing of Soft Contact Lenses 2001 to 2020. Data provided by the International Contact Lens Prescribing Trends Consortium8
Despite these beliefs, and the many benefits of 1 day SiH CLs,11 the barrier to prescribing 1 day SiH CLs to more patients continues to be reported as a perceived higher cost than 1 day hydrogel CLs.10 This belief is contrary to patient expectations, with 68% of adult CL wearers reporting that they would expect their ECP to recommend the CL that provides 100% of the oxygen their eyes need regardless of cost, and 75% would follow their ECP’s recommendation, regardless of the lens cost.12 This is further supported by work of Hutchins and Huntjens investigating patients’ attitudes and beliefs to presbyopia and its correction; 46% of study participants indicated that comfort, convenience and standard of vision were more important than cost of correction.13 Furthermore, ‘Baby Boomer’ and ‘Gen X’ presbyopic patients very often have more senior positions in their workplaces and more disposable income to spend on CLs than their ‘Millennial’, ‘Gen Y’ and ‘Gen Z’ counterparts. Some ECPs continue to perceive barriers to fitting 1 day MFCLs, including comfort, vision and the fitting process,14-16 although the proportion believing this is low.
Individual recommendations and patient/lens selection
Lens selection for the individual presbyopic patient should be guided by consideration of all their visual needs and the degree to which distance, near or intermediate tasks dominate their lives. For successful MFCL fitting, the correct lens selection and ECP expertise should be considered. It is important for the lens to be fitted to the patient, and not the patient to the lens.
Since success is also influenced by age and hence near addition power, these factors should be taken into account when fitting patients with MFCLs. ECPs need to consider the working distance and illumination encountered by presbyopes while they are conducting habitual tasks at home or in their workplace.17 Patient selection considerations (eg degree of refractive error, astigmatism, age, prior contact lens wear, motivation etc) and their habitual tasks, visual demands and viewing distances (eg computer work, writing, driving, sports etc) should also be carefully considered when determining the optimal MFCL design and modality of wear.18,19
MFCLs that offer three near add powers may be able to offer greater flexibility with respect to an individual’s visual demands. If a MFCL is offered in both centre-distance and centre-near designs, ocular dominance should be assessed, following the manufacturers’ fitting guidelines;20,21 details on this are covered in part one of this article. In some cases, toric MFCLs may be prescribed to correct both presbyopia and astigmatism, providing optimal distance, intermediate, and near visual performance without compromising binocular vision.22 A full discussion of all the factors to be considered is beyond the scope of this article, however further details can be found in the review paper by Pérez-Prados et al.19
Chair time required for MFCL fitting and supplemental fitting tools
Historically, ECPs believed that MFCL fitting required more chair time, and this is why they may have been reluctant to offer these options to their presbyopic patients.23 More recent online survey data has shown that only 4% of US ECPs and only 7% of UK ECPs agreed that MFCL fitting was difficult and takes up too much time.24 Following the manufacturer’s fitting guide, and assessing ocular dominance when applicable, are extremely important in order to achieve the optimal lens parameters, often with the first trial lenses selected. Selecting the optimal sphere power is crucial for success with MFCLs, just as it is for spherical lens designs,25 and sometimes small changes of +/-0.25D for one or both eyes can significantly improve subjective performance.
The provision of additional online support and resources may also help to counter the perception of increased chair time; one such example is OptiExpert (CooperVision Inc), a multifunctional app and website tool designed for ECPs in their day-to-day CL practice.26 The app incorporates calculators to help the ECP select the most appropriate design and lens parameters,27 in addition to providing product information and fitting guides.
While in-practice measurements and assessments play an important role in fitting MFCLs, the importance of allowing time for adaptation, and for patients to experience their visual performance in ‘real world’ settings cannot be over-emphasised. Early assessments can be unrepresentative of longer term performance and objective visual acuity measures do not always give clear indicators of overall performance.28-30
Table 1 provides details of potential perceptions that might influence ECP decisions on fitting MFCLs and the reality with the wide range of soft MFCLs available today.
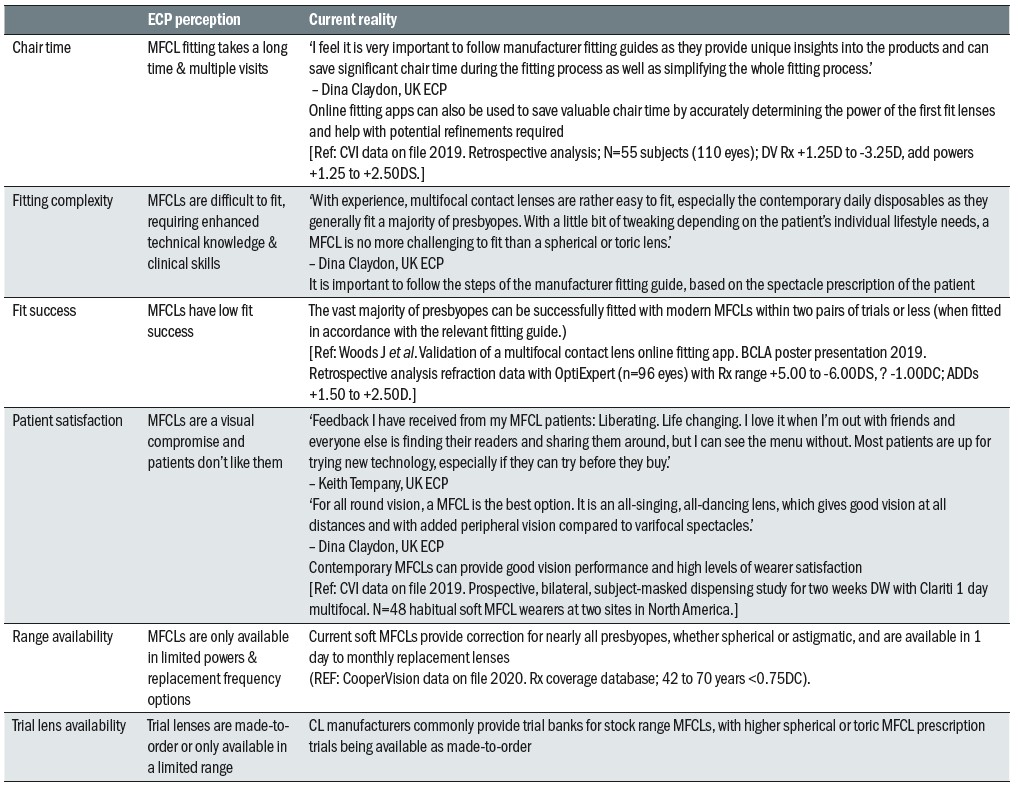 Table 3: ECP perceptions of multifocals versus reality
Table 3: ECP perceptions of multifocals versus reality
Satisfaction with MFCLs
Unfortunately, not all MFCL fittings are successful and ECPs would benefit greatly from being able to better predict which of their presbyopic patients can be successful MFCL wearers. Zeri et al have summarised the main factors that are considered to be important for the success of presbyopic CL wearers, according to textbook sources.31 These include the type and degree of refractive correction, the overall ocular health and tear film quality and a number of personal characteristics of the patient. The authors subsequently conducted a multicentre survey designed to clarify some of the factors predicting the success, or failure, of CL use among presbyopes. Both successful and unsuccessful wearers completed the survey and the most important reason for continuing to wear CLs was convenience (61%), while the most important reason for discontinuing wearing CLs was poor vision (80%). The absence of astigmatism, higher subjective satisfaction, better subjective perceived vision at distance, and a lower subjective loss of visual contrast were all found to be able to predict the success of CL use for presbyopia.31
Rueff et al conducted a survey of current or lapsed presbyopic CL wearers which was designed to determine the reasons for discontinuation and the opinions relating to comfort and visual quality with CLs.32 The authors reported that vision and discomfort were equally reported as primary reasons for CL drop out, followed by inconvenience, among presbyopes. These findings differ from previous studies investigating discontinuation from CL wear, in which dryness and discomfort have been reported to be the main reasons.33-35 However, the higher proportion of participants reporting poor visual quality as their reason for discontinuation is consistent with the findings of Sulley et al , whose study sample included a higher proportion of presbyopes.36 Rueff et al also noted: ‘CL wearers who start their use after the onset of presbyopia are no more or less likely to drop out of lens wear than habitual wearers.’32
Since there are several different MFCL designs available, it would be expected that design may play a role in the overall success of presbyopic patients that are prescribed these CLs. One such multicentre study was designed with this specific objective in mind.37 One-hundred-and-fifty successful single-vision soft CL wearers were randomly assigned to wear either a spherical near centred lens, a distance centred lens, or an aspherical near centred lens. After one month of wear a higher proportion of the individuals randomised to the spherical near centred lens had discontinued when compared with the other two designs. The principal reason for discontinuation was poor vision, 32% poor distance vision and 28% both poor distance and near vision.
The criteria for satisfaction and success with MFCLs is not well defined and will also vary significantly for the individual wearer. While some presbyopes may expect to be able to successfully wear their MFCLs every day of the week for all waking hours and all visual tasks, others may be extremely satisfied with a more part-time wearing schedule that allows them to realise the benefits of MFCLs for work, sporting activities and social occasions. It is therefore extremely important for the ECP to discuss each patient’s expectations and requirements for MFCL wear at the outset.
Opportunities to grow a practice with MFCLs
Given the rapidly increasing number of presbyopes worldwide, MFCL fitting is an often-overlooked practice building opportunity. ECPs are encouraged to bring up MFCLs with all presbyopes, regardless of the type of visit that they are attending the office for. Having routine conversations and educating presbyopic patients about MFCLs and their benefits goes a long way towards building a multifocal practice.38,39,40 Discussions with patients need not only be with the ECP; having a practice-wide commitment is important in encouraging MFCL wear. In addition to improving patients’ vision and quality of life, MFCLs also provide a way to build a practice and increase profitability from professional fitting fees and multiple eyewear purchases.41
To help elicit specific patient needs, ask presbyopic patients, ‘when would you prefer not to have to wear your glasses?’
Conversely, contact lens dropout in early presbyopia can have a significant long-term impact on a practice in terms of lost revenue over time. Factors such as multiple correction-type purchases, additional fitting fees and frequency of follow-up make contact lens patients more profitable on average than spectacle-only wearers.38 Figure 4 demonstrates the potential average loss in profitability over the lifetime of an individual who drops out of contact lens wear at or near 43 years of age.
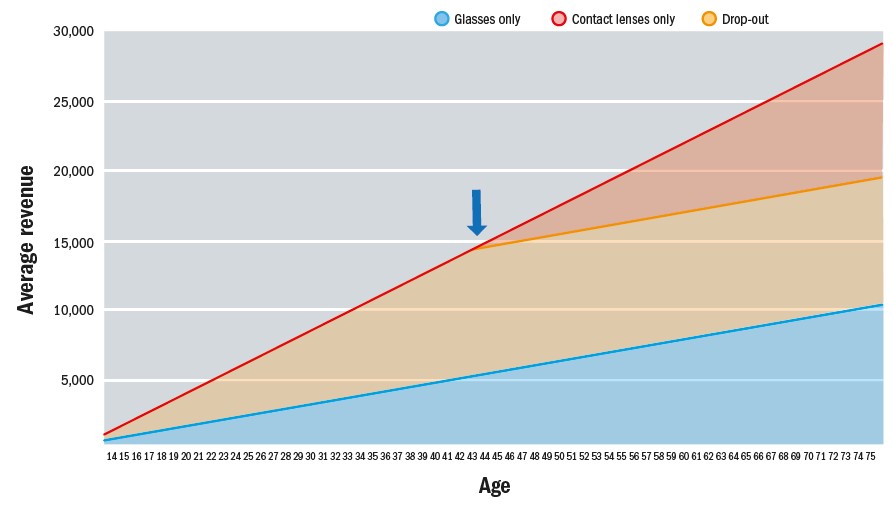 Figure 4: Lifetime profitability of contact lens wear (Industry data and CooperVision estimates, US 2018)
Figure 4: Lifetime profitability of contact lens wear (Industry data and CooperVision estimates, US 2018)
Summary and conclusions
The number of presbyopes worldwide is rapidly increasing and while a high proportion will continue to be prescribed spectacles, increasing numbers of patients are expressing interest in MFCL correction and ECPs attitudes towards recommending and prescribing these CLs is changing. MFCLs are a great option for new and established presbyopes, offering good vision performance with the added benefit of improved cosmesis and convenience compared to spectacles, and provide them the ‘flexibility to change-up their vision correction’.21 CL manufacturers are continually innovating in this area, with the increased availability of soft MFCLs with novel designs in a range of replacement frequencies from daily disposable to monthly replacement, and different materials including silicone hydrogels.
Successfully fitting MFCLs provides ECPs with enhanced professional satisfaction and business opportunities, without needing much longer appointment times thanks to product developments with simple fitting procedures. Helping to prevent presbyopes from lapsing and introducing new wearers into the CL category can improve patient loyalty and average spend.
Fortunately, there are now a wide range of options of MFCL design and material, and since selecting the most appropriate option for each individual patient is so important, it is no longer a case of ‘should I prescribe a MFCL?’ but rather ‘which MFCL?’ For the greatest opportunity for success, ECPs need to counsel patients on how MFCLs work and the possible benefits, and in some cases inconveniences, that can be associated with their wear. Individual patient visual demands must be carefully considered and the appropriate fitting guides and recommendations for adaptation should be closely followed.
- Professor Kathy Dumbleton is a Clinical Associate Professor at the University of California, Berkeley and a Clinical Research Scientist and Consultant. Dr Debbie Laughton is Professional Affairs Manager for CooperVision, EMEA and Dr Jennifer Palombi is Senior Manager, Professional Education & Development for CooperVision in North America.
Acknowledgements
This article was funded by CooperVision Inc who will be launching MyDay multifocal contact lenses in September 2021 across the UK & Ireland.
References
- Morgan PB, Efron N, Woods CA. An international survey of contact lens prescribing for presbyopia. Clinical and Experimental Optometry 2011;94(1):87-92.
- Morgan PB. Contact lens prescribing for presbyopia: an update for 2020; data from 2003-2019 for Australia, Canada, Japan, Netherlands, Norway, UK and USA. Analysis conducted for CooperVision Inc. 2020( April).
- Morgan PB, Woods CA, Tranoudis IG, Efron N, Jones LW, Nelson L, Merchan B, Grupcheva CN, Jones D, Beeler-Kaupke M, et al . International Contact Lens Prescribing in 2019. Contact Lens Spectrum 2020;35(1):26-31.
- Morgan P. Personal communication with CooperVision; February 2021. Contact lens prescribing for presbyopia: an update for 2021; data from 2005-2020 for Australia, Belgium, Canada, Czech Republic, Denmark, Spain, Hungary, Israel, Japan, Lithuania, Netherlands, Norway, New Zealand, Portugal, Sweden, Taiwan, UK and USA.
- Efron N, Morgan S, Morgan PB. Clinical performance of a daily-wear, daily-disposable soft contact lens. Optician 1995;210(5517):18-22.
- Meyler J, Ruston D. The world’s first daily disposables. Optician 2006;231(6053):12.
- Morgan PB, Woods CA, Tranoudis IG, Efron N, Jones LW, Grupcheva CN, Jones D, Beeler-Kaupke M, Qi P, Tan K, et al . International Contact Lens Prescribing in 2021. Contact Lens Spectrum 2021;36(1):32-8.
- Morgan PB. Personal Communication. 2021.
- Jones LW, Woods C. Compromises’ End? The introduction of a silicone hydrogel daily disposable lens. 2008 [cited 2019 September 27th ]; Available from: http://www.siliconehydrogels.org/editorials/jun_08.asp
- Orsborn G, Dumbleton K. Eye care professionals’ perceptions of the benefits of daily disposable silicone hydrogel contact lenses. Cont Lens Anterior Eye 2019;42(4):373-9.
- Sulley A, Dumbleton K. Silicone hydrogel daily disposable benefits: The evidence. Cont Lens Anterior Eye 2020;43(3):298-307.
- Silicone hydrogel lenses. 2018. YouGov Plc. Total sample size was 1520 adults who wear contact lenses. Fieldwork undertaken March 26 - April 3, 2018. Survey carried out online. 2018.
- Hutchins B, Huntjens B. Patients’ attitudes and beliefs to presbyopia and its correction. J Optom 2020:https://doi.org/10.1016/j.optom.2020.02.001.
- Nichols KKR, R. L.; Jacob, J. T.; Nelson, J. D.; Fonn, D.; Forstot, S. L.; Huang, J. F.; Holden, B. A.; Nichols, J. J. The TFOS International Workshop on Contact Lens Discomfort: Report of the definition and classification subcommittee. Invest Ophthalmol Vis Sci 2013;54(11):TFOS14-TFOS9.
- Morgan PBE, N. Contact lens correction of presbyopia. Cont Lens Anterior Eye 2009;32(4):191-2.
- Sulley A, Young G, Hunt C, McCready S, Targett MT, Craven R. Retention Rates in New Contact Lens Wearers. Eye Contact Lens 2018;44 Suppl 1:S273-s82.
- Cardona G, Lopez S. Pupil diameter, working distance and illumination during habitual tasks. Implications for simultaneous vision contact lenses for presbyopia. J Optom 2016;9(2):78-84.
- Gispets J, Arjona M, Pujol J, Vilaseca M, Cardona G. Task oriented visual satisfaction and wearing success with two different simultaneous vision multifocal soft contact lenses. Journal of Optometry 2011;4(3):76-84.
- Perez-Prados R, Pinero DP, Perez-Cambrodi RJ, Madrid-Costa D. Soft multifocal simultaneous image contact lenses: a review. Clin Exp Optom 2017;100(2):107-27.
- Pence NA. Contact Lens Design and Materials: Two New SiHy Lens Options. Contact Lens Spectrum 2011;26(11).
- Sanders E, Wagner H, Reich LN. Visual Acuity and ‘Balanced Progressive’ Simultaneous Vision Multifocal Contact Lenses. Eye & Contact Lens 2008;34(5):293-6.
- Madrid-Costa D, Tomas E, Ferrer-Blasco T, Garcia-Lazaro S, Montes-Mico R. Visual performance of a multifocal toric soft contact lens. Optom Vis Sci 2012;89(11):1627-35.
- Bennett ES. Contact lens correction of presbyopia. Clin Exp Optom 2008;91(3):265-78.
- CVI data on file. Kubic LLC: Global Multifocal Benefit Online Survey. 2020.
- Young G, Moody K, Sulley A. Anomalies in the prescribing of soft contact lens power. Eye Contact Lens 2009;35(1):11-4.
- Bogers A, Prest D. Review of a digital contact lens fitting support tool for eye care professionals. In: British Contact Lens Association Clinical Conference; Manchester, UK; 2019.
- Woods J, Varikooty J, Lumb E. Validation of a multifocal contact lens online fitting app. In: British Contact Lens Association Clinical Conference; Manchester, UK; 2019.
- Papas EB, Decenzo-Verbeten T, Fonn D, Holden BA, Kollbaum PS, Situ P, Tan J, Woods C. Utility of short-term evaluation of presbyopic contact lens performance. Eye and Contact Lens 2009;35(3):144-8.
- Woods J, Woods C, Fonn D. Visual Performance of a Multifocal Contact Lens versus Monovision in Established Presbyopes. Optom Vis Sci 2015;92(2):175-82.
- Woods J, Woods CA, Fonn D. Early symptomatic presbyopes-What correction modality works best? Eye and Contact Lens 2009;35(5):221-6.
- Zeri F, Di Censi M, Livi S, Ercoli A, Naroo SA. Factors That Influence the Success of Contact Lens Fitting in Presbyopes: A Multicentric Survey. Eye Contact Lens 2019;45(6):382-9.
- Rueff EM, Varghese RJ, Brack TM, Downard DE, Bailey MD. A survey of presbyopic contact lens wearers in a university setting. Optom Vis Sci 2016;93(8):848-54.
- Dumbleton K, Woods CA, Jones LW, Fonn D. The impact of contemporary contact lenses on contact lens discontinuation. Eye and Contact Lens 2013;39(1):93-9.
- Pritchard N, Fonn D, Brazeau D. Discontinuation of contact lens wear: a survey. Int Contact Lens Clin 1999;26(6):157 - 62.
- Richdale K, Sinnott LT, Skadahl E, Nichols JJ. Frequency of and factors associated with contact lens dissatisfaction and discontinuation. Cornea 2007;26(2):168-74.
- Sulley A, Young G, Hunt C. Factors in the success of new contact lens wearers. Cont Lens Anterior Eye 2017;40(1):15-24.
- Novillo-Díaz E, Villa-Collar C, Narváez-Peña M, Martín JLR. Fitting success for three multifocal designs: Multicentre randomised trial. Cont Lens Anterior Eye 2018;41(3):258-62.
- Cole J. Multifocal sales: opportunity is near: with new modalities, materials and designs, don’t bypass this practice-building correction for your presbyopes. Review of Optometry 2016;153(8):46-50.
- Ritson, M. (2006). Which Patients are More Profitable? Retrieved January 08, 2021, from https://www.clspectrum.com/issues/2006/march-2006/which-patients-are-more-profitable
- Bennett E, T.G. Q. Building a practice with multifocal contact lenses. Contact Lens Spectrum 2018;35:36-9.
- Anderson D. Growth Opportunity: Tips to Move Patients into Multifocal CLs. Review of Optometric Business 2017.
