Accommodation is required to maintain clarity of an object at any distance closer than infinity. It is present in newborn infants from one month of age and becomes more precise and better controlled by six months.1 This control gradually decreases with age and shows a steady decline becoming noticeable at about the age of 40, a process we all know as presbyopia. While accommodation is essential for clear vision in everyday life, it can affect the accuracy of determining refractive error. In some cases, to obtain meaningful results requires cycloplegia – paralysing the muscles controlling accommodation and causing a loss in ability to focus.
Anatomy of accommodation
The crystalline lens is a clear convex structure behind the iris in the posterior chamber of the eye (figure 1). It is supported by the suspensory ligaments, the zonules of Zinn, that attach to the ciliary muscle in a 360-degree arrangement. In its relaxed state, an emmetropic eye should resolve objects at six metres and beyond to give clear distance vision. The light rays from a distant object entering the eye are nearly parallel upon reaching the eye. After travelling through the refractive structures, namely the cornea, aqueous, crystalline lens and vitreous, the rays come to a focus upon the retina. The ciliary muscles are relaxed and the ring they constitute is maximally dilated. This pulls on the zonules resulting in a flattening of the crystalline lens and reduced refractive power.
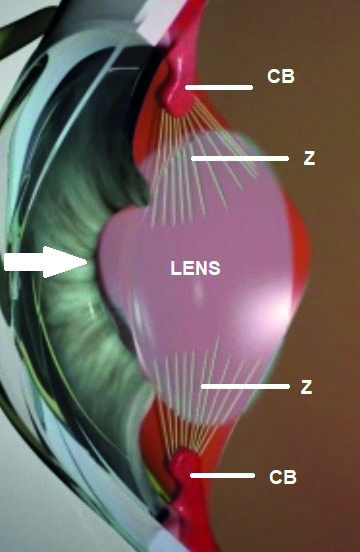 Figure 1: Schematic cutaway representation of the anterior eye with light entering from the left as shown by the arrow. CB represents a cross section of the top and bottom of the ring of ciliary muscle. Z represents the zonules by which the fluid crystalline lens is attached to the ciliary body and via which ciliary muscle tension is transferred to cause the lens to fatten or thin
Figure 1: Schematic cutaway representation of the anterior eye with light entering from the left as shown by the arrow. CB represents a cross section of the top and bottom of the ring of ciliary muscle. Z represents the zonules by which the fluid crystalline lens is attached to the ciliary body and via which ciliary muscle tension is transferred to cause the lens to fatten or thin
For viewing near objects, while the ciliary muscles remain relaxed and the lens of minimum thickness as described, light rays are focused behind the retinal plane and the images of the near objects are blurred. Accommodation, the mechanism whereby the eye changes to focus light from near objects, relies upon a contraction of the ciliary muscles in an inward and anterior direction, the resultant reduction in diameter of the ring of muscle causing a relaxing of the tension in the suspensory ligaments. The leads to a ‘fattening’ and hence more convex curvature of the lens surfaces, so increasing its positive refractive power and allowing closer focus. Figure 2 shows an ultrasound image of the crystalline pens in both the relaxed and the accommodating state.
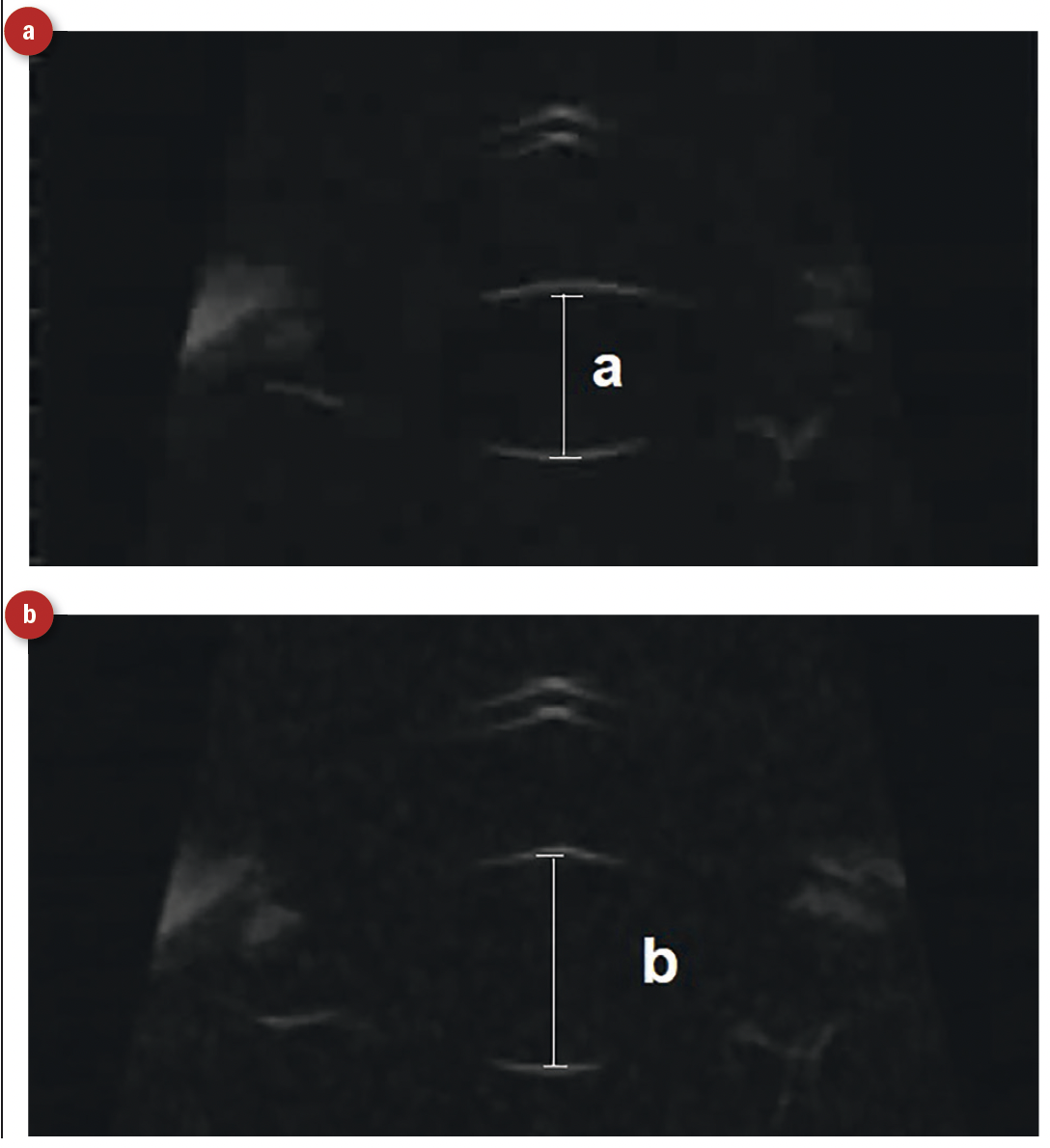 Figure 2: Ultrasound section views of the crystalline lens (anterior and posterior surface are seen clearly). (a) Relaxation of the ciliary muscle results in a flattening of the crystalline lens and a reduction of the distance from front to back surface of the lens as marked ‘a’. (b) Contraction of the ciliary muscles causes a fattening of the crystalline lens, an increased axial thickness (marked ‘b’) and an increase in positive refractive power
Figure 2: Ultrasound section views of the crystalline lens (anterior and posterior surface are seen clearly). (a) Relaxation of the ciliary muscle results in a flattening of the crystalline lens and a reduction of the distance from front to back surface of the lens as marked ‘a’. (b) Contraction of the ciliary muscles causes a fattening of the crystalline lens, an increased axial thickness (marked ‘b’) and an increase in positive refractive power
Innervation of ciliary muscle
The ciliary muscle is a ring of smooth muscle and, as such, depends on the autonomic nervous system for control. Anterior to the ciliary body, the iris contains two sets of muscles. The dilator fibres are radially distributed such that contraction decreases the size of the iris and opens out the pupil. The iris sphincter fibres are annular, similar to the ciliary muscle rings, and so contraction of these causes the pupil to narrow. The dilator fibres are supplied by sympathetic nerves (hence pupil dilation during moments of stimulation or excitement) while iris sphincter muscle activity, and therefore pupil miosis, is due to parasympathetic input.
Though there is some limited evidence of a sympathetic influence upon the ciliary muscle as a means of heightening muscle relaxation in certain environmental conditions, control of the ciliary muscle, and therefore accommodation, is a function of the parasympathetic system. Figure 3 summarises the autonomic control of mydriasis and accommodation.
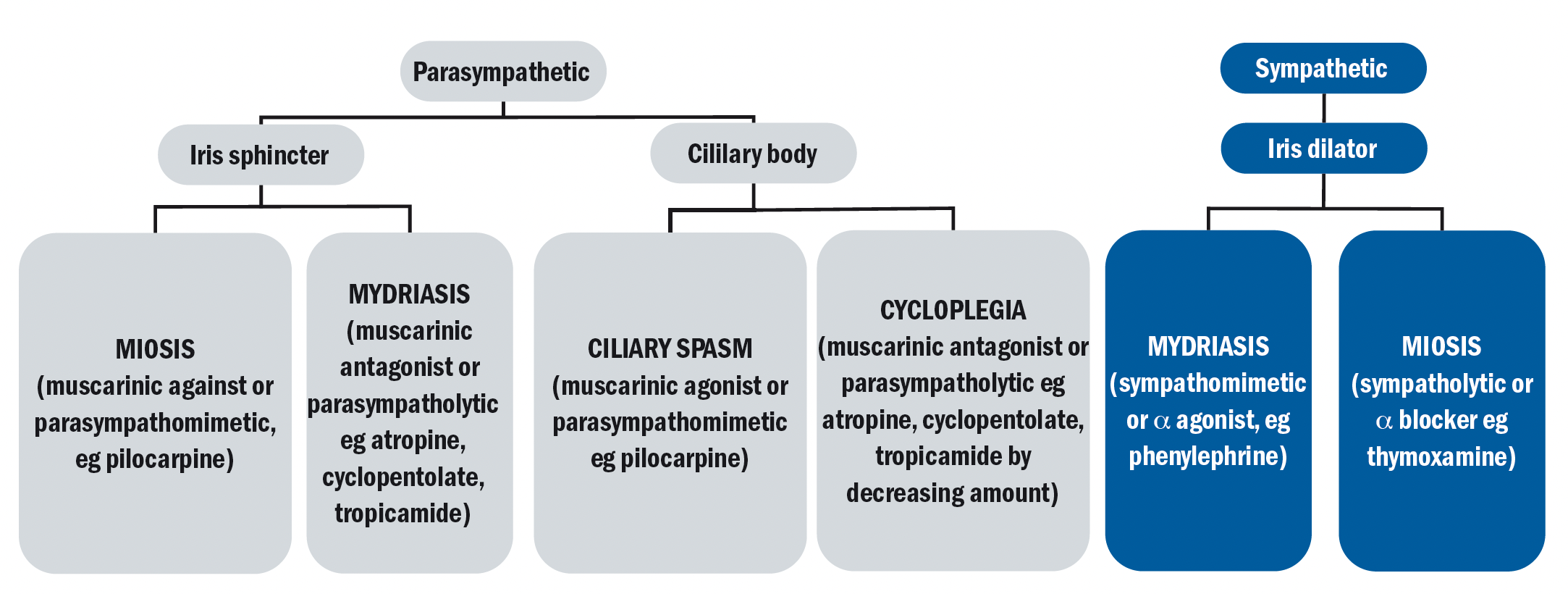 Figure 3: Flow chart showing the autonomic nervous supply of the eye and how it is influenced by different drugs
Figure 3: Flow chart showing the autonomic nervous supply of the eye and how it is influenced by different drugs
Parasympathetic input causes the ciliary muscle to contract, so increasing accommodation. Reduced parasympathetic input causes the ciliary muscle to relax, and accommodation to decrease. So, it is clear that the state of cycloplegia, where there is no accommodative activity, will result from the removal of any parasympathetic stimulation to the ciliary muscle.
Figure 4 shows a schematic representation of the main nerves and muscles of the eye. The ciliary muscle receives its parasympathetic input via fibres from the short ciliary nerves that arise from the ciliary ganglion.
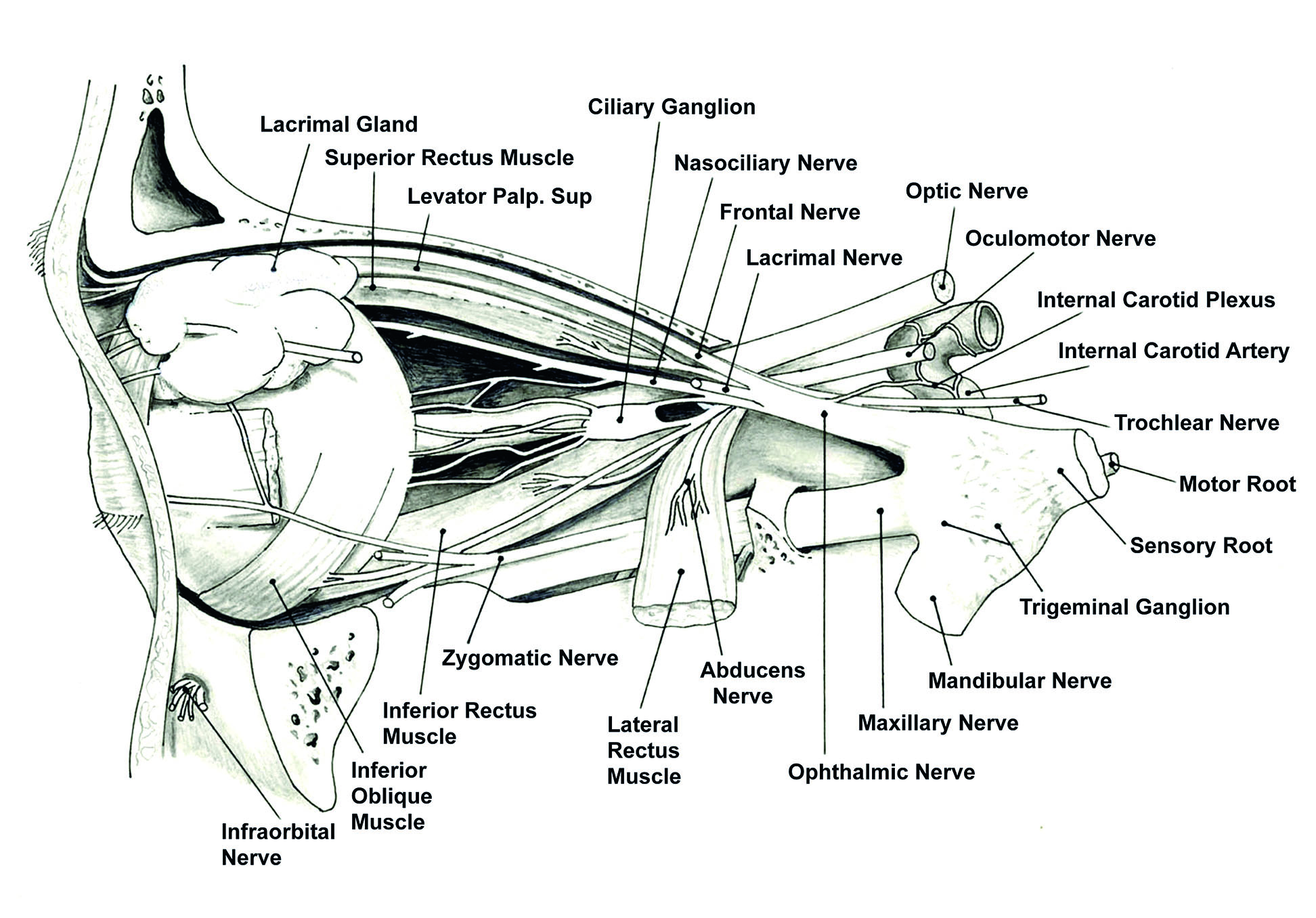 Figure 4: Nerves and muscles of the eye4
Figure 4: Nerves and muscles of the eye4
Presynaptic parasympathetic signals, originating in the Edinger-Westphal nucleus, are carried by the third cranial nerve, the oculomotor nerve, and travel through the ciliary ganglion from where the short ciliary nerves arise to supply the ciliary body and iris sphincter.
The sympathetic postganglionic fibres, primarily to the iris dilator muscle, reach their target via the nasociliary nerve, a branch of the ophthalmic nerve, the first branch (C1) of the trigeminal, or fifth, cranial nerve. The postganglionic sympathetic innervation arises from the superior cervical ganglia. Figure 5 shows the main autonomic innervation of the iris and ciliary muscle.
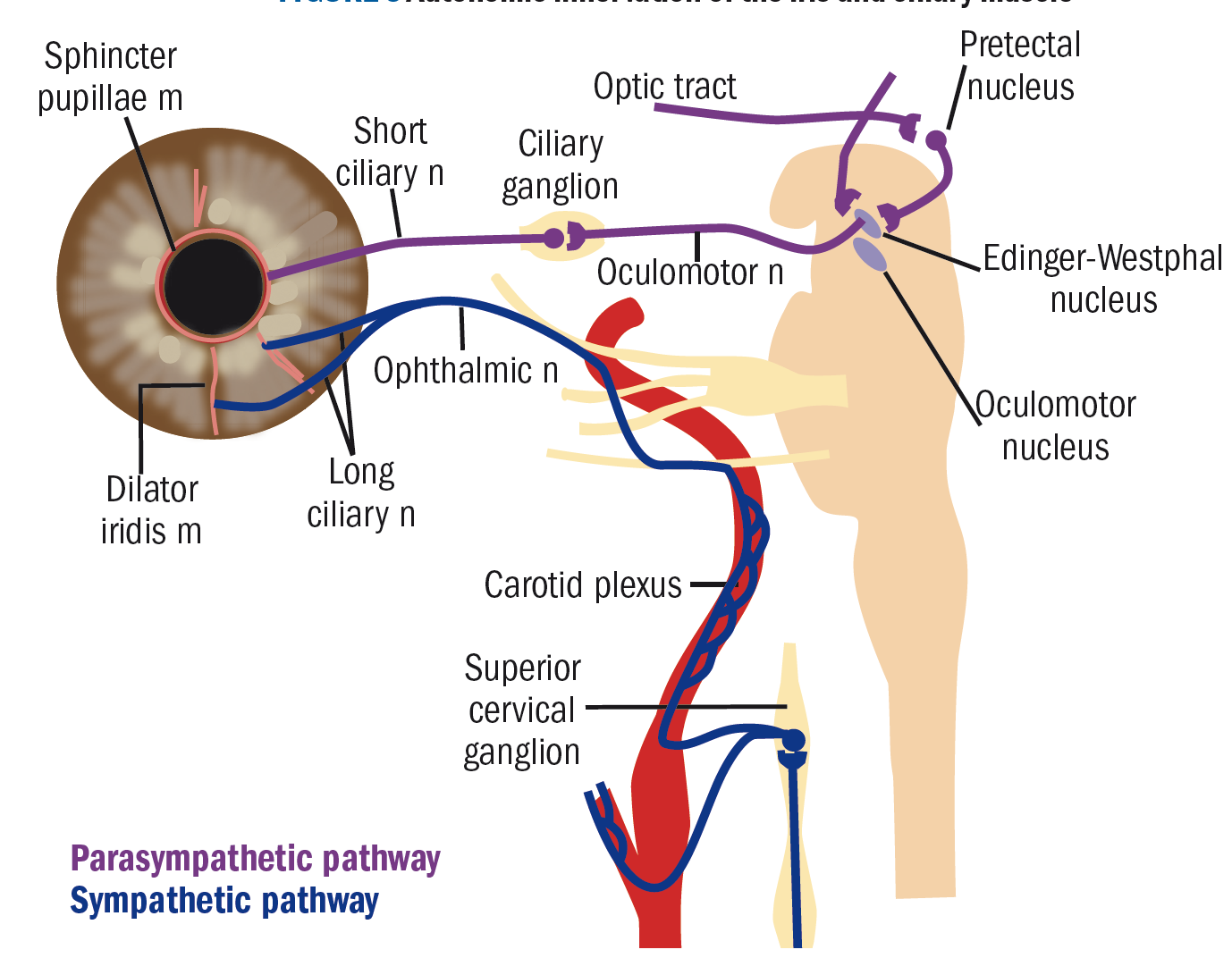 Figure 5: Autonomic innervation of the iris and ciliary muscle
Figure 5: Autonomic innervation of the iris and ciliary muscle
Parasympathetic activation of the M3 muscarinic receptors causes ciliary muscle contraction. The triad of the accommodative response is accommodation, miosis and convergence. Pupil constriction aids the reduction of peripheral light rays, which contribute to blurring and gives a greater depth of focus. The final component in the triad for clear near vision is convergence of the two eyes to allow bifoveal fixation.
Action of cycloplegic drugs
Drugs that arrest accommodation, cycloplegics, are used routinely in optometric practice to aid refraction. The ideal cycloplegic drug should:
- Produce adequate cycloplegia
- Work in a short space of time
- Be reversible in a short time
- Not have any serious systemic or ocular side effects
- Be easy to administer
- Not be cost prohibitive
Generally, full cycloplegia is not required and residual accommodation of 1 to 2 dioptres is acceptable in most primary care cases. This outweighs the dangers of the potential side effects of an increased dose or more potent drugs (such as atropine) required for full cycloplegia.
The most commonly used cycloplegic drugs are anti-muscarinic agents. These molecules compete with acetylcholine, the neurotransmitter released at the muscle by the parasympathetic stimulation to act on receptors to cause muscle contraction. Anti-muscarinic (or parasympatholytic) drugs, however, are able to bind to the same receptors as acetylcholine but do not stimulate the muscle response. In this way, they are able to block ciliary muscle activity. The molecular structures of acetylcholine and the key cycloplegic agents are shown in figure 6. Their structures are all similar enough to allow receptor site binding, but variation in structure influences the stability and duration of that binding. This helps to explain the great variation in onset and duration times for the different drugs.
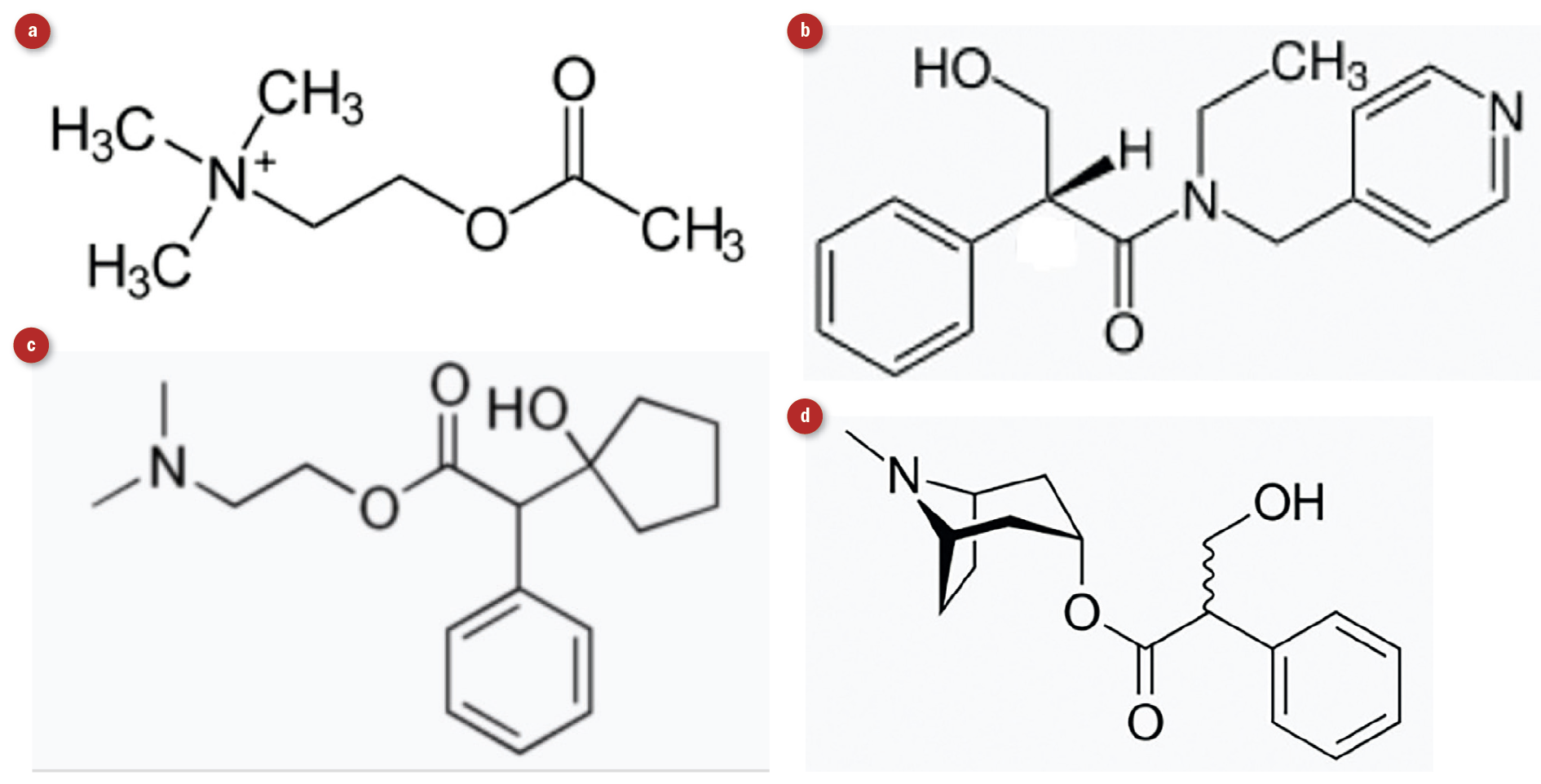 Figure 6: Molecular structure of (a) acetylcholine, (b) tropicamide, (c) cyclopentolate and (d) atropine
Figure 6: Molecular structure of (a) acetylcholine, (b) tropicamide, (c) cyclopentolate and (d) atropine
They also act on the iris sphincter muscle and produce pupil dilation. This side effect is sometimes useful for the fundal examination of children or uncooperative patients, although the associated photophobia is not pleasant. Patients should be advised to avoid driving or operating machinery. Advising the child’s school that their vision will be blurred for several hours would also be useful.
Cycloplegics in UK optometric practice
Commonly used cycloplegics drugs are listed in table 1. In the exemptions from Normal Supply Requirements of Human Medicine Regulations 2012, a list of medications that are prescription only (POM) can be sold or supplied to an GOC registered optometrist and may be used in the course of their professional practice. Atropine can only be used and supplied by those with additional supply and independent prescriber status.
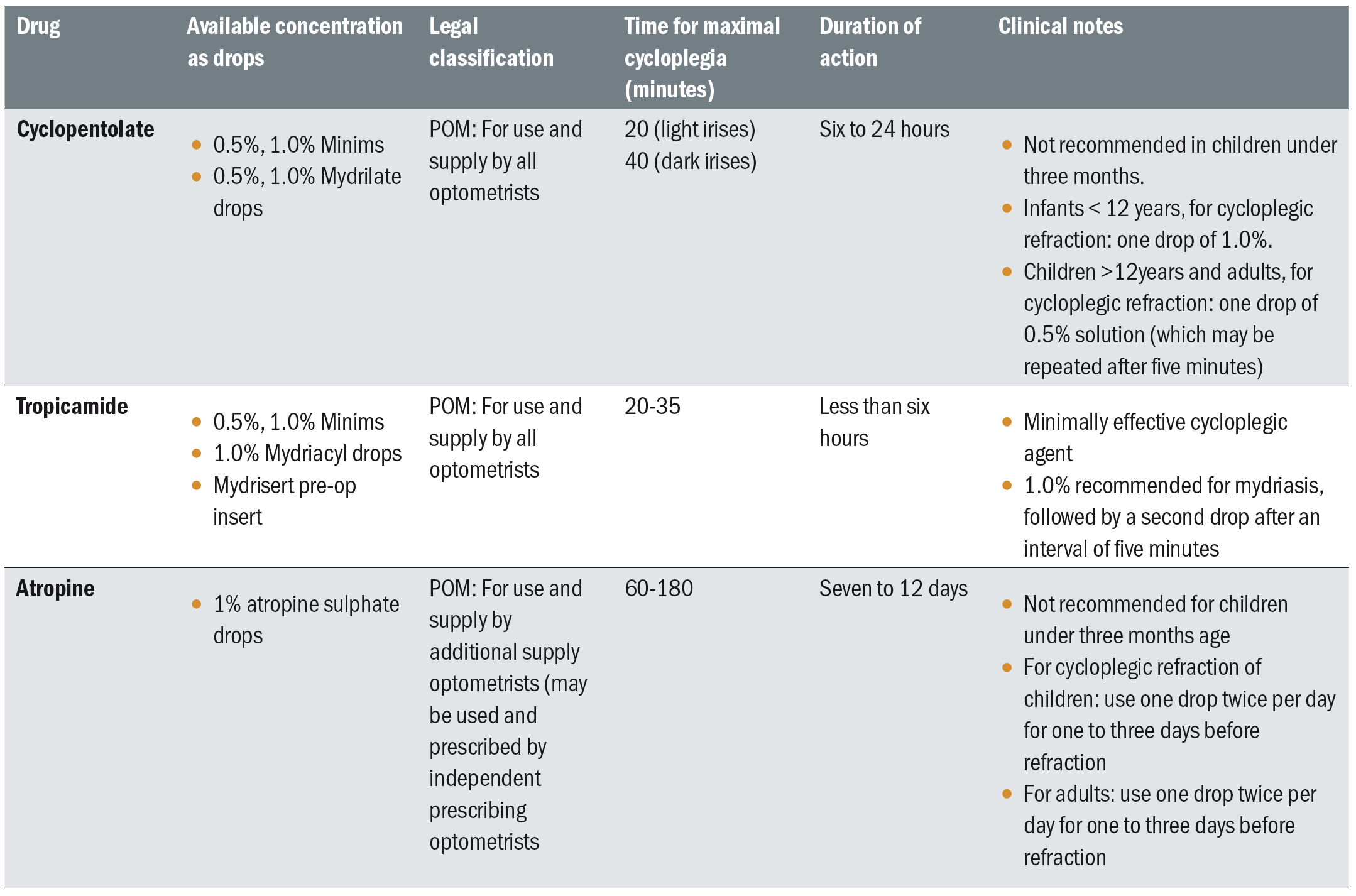 Table 1: Commonly used cycloplegic drugs and their properties
Table 1: Commonly used cycloplegic drugs and their properties
Cyclopentolate
This is the most commonly used cycloplegic drug readily available and appropriate for most cases requiring cycloplegia in primary practice. It is available in the UK, as either 0.5% or 1.0%
cyclopentolate hydrochloride in multidose bottles (as Mydrilate) and single dose Minims. Its effect begins fairly rapidly, and the maximal effect can be reached in 20 to 40 minutes. Recovery can allow reading by four hours, although it can take 12 to 24 hours. Which concentration to use varies according to different authors, though generally 0.5% is recommended for 12 to 16-year-olds and 1.0% for one to 11 years old.
The College of Ophthalmologists’ guidelines recommend refraction some 30 minutes after instillation of 1.0 % for infants aged over six months, and 0.5% for younger babies with suspected strabismus. Repeatability of refractive results when using 1.0% cyclopentolate after 30 minutes has been shown to be
excellent.
Tropicamide
For teenagers and adults, this may be enough to produce the full cycloplegic effect required for refraction and its effects wear off quicker than cyclopentolate. One percent with two drops at 15 minutes apart is recommended, either using Minim single dose application or the multidose preparation Mydriacyl (figure 7). Some argue that tropicamide produces too much residual accommodation as seen when using push-up measurements. However, objective measurements appear to show only 1D of residual accommodation and is therefore acceptable in most cases.
Atropine
Atropine is required when there is significant hypermetropia and esotropia, as the full cycloplegia result is needed before possible surgical intervention. Also, atropine will be considered for children with very dark irises, when cyclopentolate has been used and an inadequate dilation for fundal examination and cycloplegia has meant results are inconclusive.
It is available as atropine sulphate as eye drops, 1.0%. These can be used and supplied by optometrists holding the additional independent prescribing qualification.
Many studies show the repeated use of up to three drops of 1.0% cyclopentolate was as effective as using 1.0% atropine, although how practical this would be in primary practice needs to be considered. Atropine 1.0% as an eye drop produces full cycloplegia after a few hours. However, the risk of systemic effects can be higher and atropine ointment instilled twice a day for three days before the refraction appointment is often preferred. No ointment is used on the day of refraction as the oily residue may affect refraction results. It is not without risks and extreme caution should be exercised due to the risk of poisoning. This is a real risk as a small tube of atropine (3g) ingested accidently can cause death in a small child who can be seriously affected by as little as 10mg. Typical side effects seen include: rapid pulse, dry skin and mouth, excitement, respiratory paralysis.
Adverse effects of cycloplegic drugs
Systemic effects are possible in young children due to their low body weight and immature metabolism; therefore, precaution advice must be given to the parent in case this occurs after they leave the practice.
A decrease in anterior angle drainage and raised intraocular pressure can occur with the use of anti-muscarinics. The loss of contraction of the ciliary muscle during accommodation, which normally contributes to the aqueous flow, may also compound this effect. Fortunately, those disposed to this are at an age group that do not often need these drugs to aid refraction but should be avoided in those who have had closed angle glaucoma. Each cycloplegic has a different risk profile (as summarised in table 2) so will be considered separately.
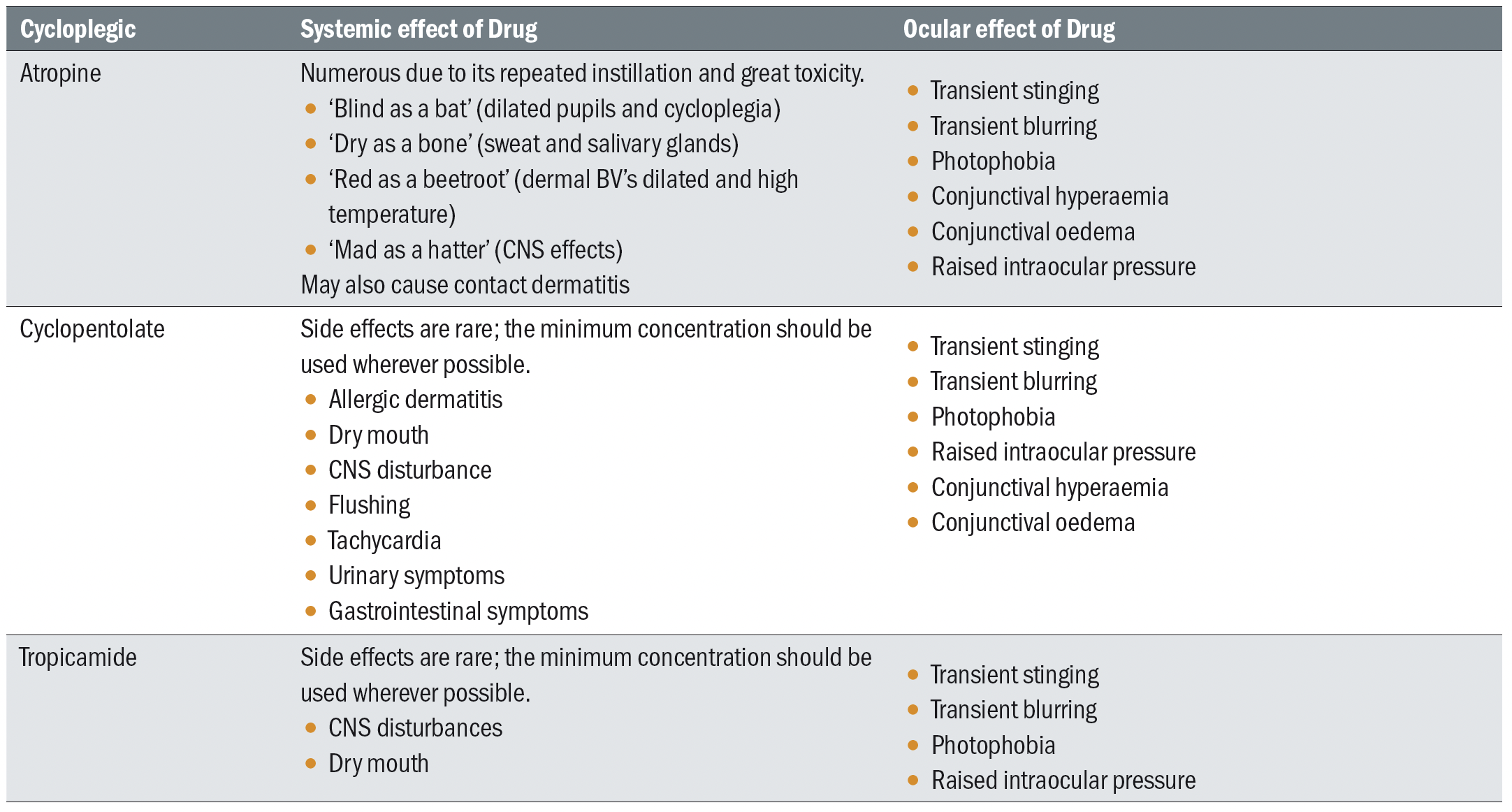 Table 2: Adverse effects of cycloplegic drugs
Table 2: Adverse effects of cycloplegic drugs
Atropine
The greatest risk of adverse response is from atropine. Beside blurred vision, atropine also have various systemic side effects ranging from drowsiness, dizziness and dry mouth, to myocardial infarction and anaphylaxis.
Other possible systemic side effects include urinary retention, inhibition of sweating (anhydrosis) and constipation. Atropine also affects the normal cardiac rhythm, and may induce cardiac arrest. It is, therefore, important to establish whether a patient has any cardiac disease before administering the drug.
The quote ‘red as a beet, dry as a bone, hot as a hare, blind as a bat, mad as a hatter and full as a flask’ is commonly used in relation to atropine poisoning. In this situation, the patient presents with:
- Red as a beet; face and trunk of body are bright red, also known as atropine flush
- Dry as a bone; dry mucous membranes and skin
- Hot as a hare; high fever
- Blind as a bat; dilated pupils
- Mad as a hatter; delirium, hallucinations, confusion, staccato speech, and picking at clothing and bedding
- Full as a flask; urinary retention
Other severe side effects, thankfully, are rare and only with the use of drops as opposed to ointment. Convulsions, coma and death have occurred after ocular instillation of atropine in infants and children. Accidental or intentional ingestion of atropine solution may also happen, and usually with disastrous consequences. Intentional poisoning with atropine solution has also been reported in a homicide case.
The lethal dose of atropine is between 100mg and 200mg. Therefore, parents and guardians should be encouraged to keep all medications in a safe place that is inaccessible to children. In addition, carers and patients should also be advised to wash hands before and after instillation, and to remove all excess ointment with cotton wool. The drug should be stopped immediately if any local reaction occurs. In addition, the tube should be returned to the prescribing centre after the three-day application so that it may be disposed of safely.
Cyclopentolate
Cyclopentolate is the main cycloplegic drug used in optometric practice due to its safety. However, systemic adverse effects have been reported to occur in up to 10% of patients after repeated instillation of 1% strength. These can include the following:
- Tachycardia; increased heart rate
- Restlessness
- Hallucinations
- Psychosis
- Hyperactivity
- Seizures
- Incoherent speech
- Ataxia
Such effects are especially likely in children. The central nervous system (CNS) toxicity of this drug is due to its anticholinergic action, causing stimulation of the medulla and cerebral centres. They occur within 20 to 30 minutes of administration and subside within four to six hours with no permanent sequelae and with the patients having no recollection of the hallucinations. Atropine-like systemic side effects can also occur. In addition, patients can present with rashes, headaches, nausea and wheeze or even severe anaphylactic reactions.
Although some of these effects occur after multiple instillations and are dose dependent, it is not unheard of for severe reactions to occur after the first use of this drug. Therefore, as with any other drug, close observation of the patient after
instillation of cyclopentolate is highly recommended and early recognition of systemic toxicity is important for a prompt
management.
Tropicamide
Tropicamide is mainly used as mydriatic and only occasionally used as a cycloplegic in optometric practice as its cycloplegic effect is weak and transitory. Tropicamide’s potential systemic side effects are due to its antimuscarinic properties and can include the following:
- Dry mouth
- Tachycardia
- Headache
- Nausea
- Vomiting
- Pallor (generalised)
- Allergic reactions
- Muscular rigidity
These adverse responses are, however, very rare.
How to use cycloplegic drugs
Before using cycloplegic eye drops, a full eye examination should be undertaken including a detailed history of any current medication (and possible interactions) or previous allergic reactions. A ‘dry’ retinoscopy result is also useful for prescribing purposes. In older patients, anterior chamber depth and tonometry should also be assessed. Warning about side effects should be given and consent from the patient or parent obtained to instil the drug.
It is recommended by some and used as standard protocol in clinical trials, using 0.5% proxymetacaine to anaesthetise the cornea before instillation of cyclopentolate. The advantages are that this may allow the patient to tolerate having the stinging drop in both eyes, especially in the second eye. Also, it improves the absorption rate of the cycloplegic drop. The disadvantages include trying to put more than one drop in each eye of less cooperative patients, the added cost and possible inconvenience of needing to store proxymetacaine in refrigeration.
Placing drops on the medial canthus of uncooperative patients and then allowing the drop to fall into the eye on opening has been found to be as effective as instilling directly into the open eye. This method is also found to be more comfortable for the patient. Using a spray has also been found to be effective but this option is less readily available in UK. It has also been shown that instilling a smaller drop produces less blinking and reflex tearing, increasing the efficacy of the drop. This was more effective than closing the eyes after instillation or performing nasolacrimal occlusion.
In primary care, the standard drug of choice in over one-year olds would be 1% cyclopentolate one drop and in light irises cycloplegia may be adequate in as little as 10 minutes. In dark irises at least 30 minutes is required before attempting refraction. For all iris colours, maximum cycloplegia is achieved after 40 minutes when residual accommodation is measured objectively. Greater amounts of residual are found in dark irises if measured subjectively.Mydriasis should not be used as an indicator for cycloplegia as although the onset is similar, full dilation can occur before full cycloplegia in light eyes. In dark eyes, cycloplegia can be reached before maximum dilation.
Determining when adequate cycloplegia is reached can be done in several ways. Measurement of residual accommodation in older patients eg using a RAF ruler can be performed with a +2.50DS in the trial frame and subtracting this amount after. Residual accommodation of 2D or less is considered acceptable.11 In younger patients, use of the retinoscopy reflex is required. Fluctuations of accommodation and hence a change in speed or direction of the retinoscopy reflex when asking patients to fix from distance to near would indicate inadequate cycloplegia. Usually waiting another 10 to 15 minutes is all that is required. Analysing the retinoscopy reflex should also just be concentrated on the central 4mm of the dilated pupil as the spherical aberration distorts the reflex. The patient’s fixation should be a distant target if possible (to counter any residual accommodation) but on the retinoscope light is workable for younger patients, which gives the added advantage of being on the visual axes. Loose trial lenses are preferable to phoropters for the younger children. Older patients can also have a subjective refraction bearing in mind that final VAs will be about two lines worse than best VA due to the mydriasis.
When to use cycloplegic drugs
Accurate refraction requires fixation to be at a distance target eg 6m or beyond, such that the accommodation is relaxed. When accommodation occurs either during objective (eg retinoscopy) or subjective refraction, this will result in an over myopic or under hypermetropic result. Where there are fluctuations of accommodative effort, the end point of the refraction would also be variable. Therefore, any cases where distance fixation or controlling accommodation cannot be done, a cycloplegic refraction should be considered. This would include those who are unable to cooperate due to their young age, language barriers, communication or learning difficulties and any other unusual circumstances. A cycloplegic refraction is useful to rule out any refractive error that would account for symptoms in those who are malingering. It is also useful for the diagnosis of many conditions listed, whose signs and symptoms are listed in table 3. Patients requiring cycloplegic refraction include:
- Bilateral or unilateral reduced visual acuity in child with unexplained cause
- Strabismus on first detection and possibly at annual review
- Non-verbal/communicative including very young children and babies
- Fluctuating retinoscopy reflex and reduced vision or VA
- Suspected latent hypermetropia/ pseudomyopia
- At first appointments at a hospital eye clinic
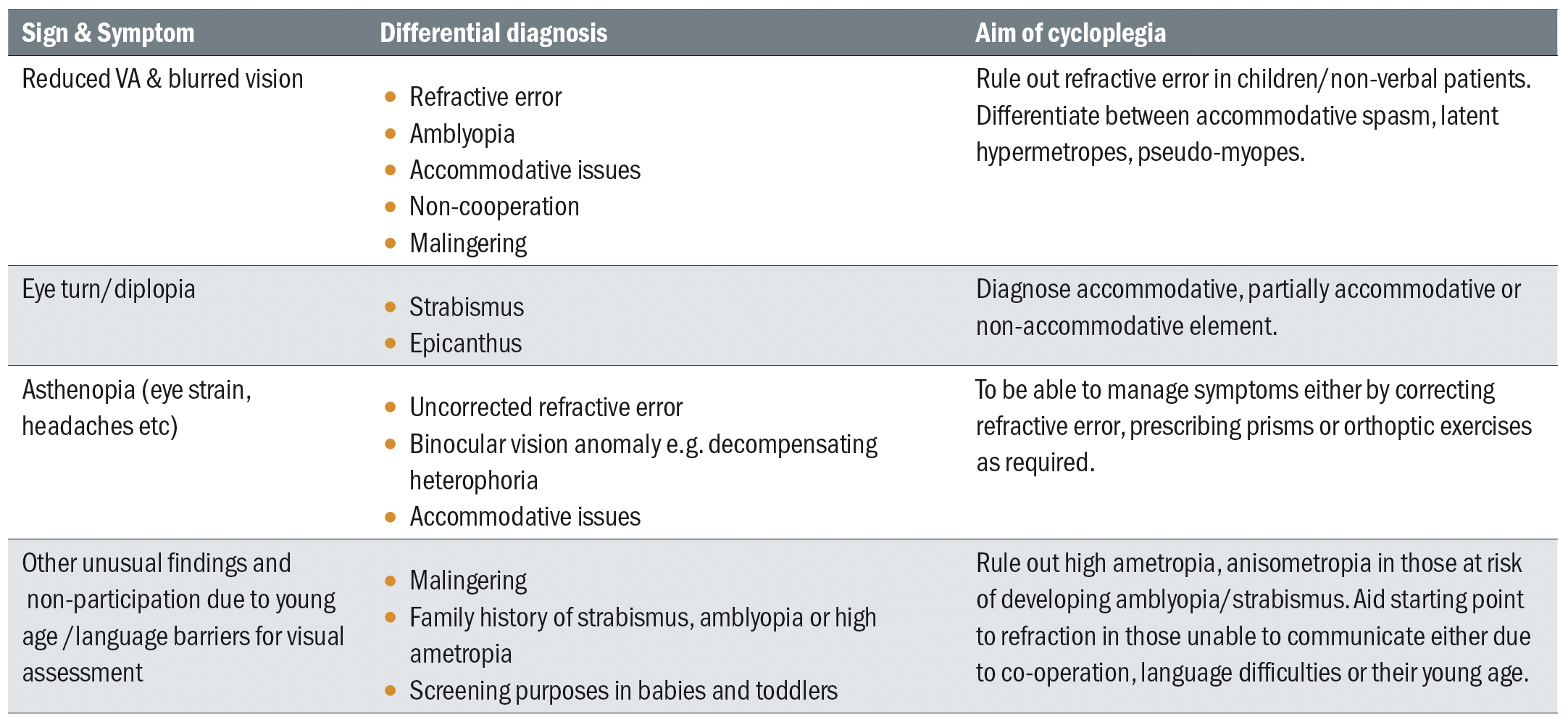 Table 3: Indications for a cycloplegic refraction
Table 3: Indications for a cycloplegic refraction
Prescribing tips
There are many opinions on prescribing and most practitioners will also rely on experience and judgement. Therefore, the following are based on recognised texts and the author’s own experience in community and hospital practice and will differ to other opinions.
Where there is a significant refractive error that is outside the norms for that age group, prescribing the refractive error found after cycloplegic refraction is a good line of first treatment. Visual acuities should be reviewed in six to eight weeks to check for improvement and monitoring at three to four monthly intervals until no further improvement is found before referring for amblyopia treatment.
In children with esotropia, full hypermetropia and astigmatism should be issued for full-time wear. A review should then take place in six to eight weeks to see the effect of the spectacles. If it is a fully accommodative esotropia ie it is eliminated by wearing the hypermetropic spectacles and the vision is improving, these can be monitored closely in the community every three to four months until there is any residual amblyopia that needs
treatment.
In non-strabismics, moderate hypermetropia could be reduced to help adaptation. A quarter or third off the cyclo result of the worst eye appears to be consistent with later subjective results. This will also depend on the presenting symptoms and uncorrected vision. If the VA is poor, consider prescribing more of the refractive error to try to improve the VA. Keeping the difference in anisometropia should be maintained. Eg cyclo result R +3.00DS L +1.00DS, take a 1/3 off the stronger eye (+3.00DS) prescribe R+2.00DS L Plano. This seems to avoid ‘over plussing’ and causing reduced distance VA and appear to be similar to the natural non-cycloplegic state of the eyes. A subjective refraction either on the same day or on another visit – a ‘post-cyclo’ would help the prescribing decision.
In the absence of any significant refractive error and reduced VA, in non-strabismic – consider the following. In a young child, is the type of test appropriate eg use pictures as well as letters or numbers. Late after-school appointments can result in tiredness and poor concentration for the tests. Sometimes simply rechecking on an early Saturday morning visit produces dramatically improved vision results. In children with strabismus and no significant refractive error, routine referral to a hospital for amblyopia and possible surgical treatment may be appropriate.
The relationship between accommodation and accommodative convergence should also be remembered. When correcting hypermetropia, this relaxes accommodative convergence meaning the eyes may diverge. Measurements of heterophoria and heterotropia are therefore important before refraction to see the effect of correcting refractive error has on ocular motor balance. For a child with exophoria, by correcting all their hypermetropia and relaxing their accommodative convergence may cause decompensation into an exotropia, which is undesirable. The AC/A ratio (accommodative convergence produced by each dioptre of accommodation) is usually 4 prism dioptres to 1D. Therefore, any spherical adjustment to a prescription can be used to manipulate this to the advantage of controlling a convergent or divergent muscle imbalance. Reducing plus or increasing minus can produce convergence to aid exo deviations and vice versa. The amount increased or decreased would also depend on the VA being maintained and the amount of excessive accommodation required for comfortable vision. This is usually no more than 1-1.5D of manipulation that can be tolerated. A cycloplegic refraction should be performed as a starting point before the change. Also measure the amplitude of accommodation to see if it will be adequate for this treatment.
One Hospital Paediatric Eye clinic’s view on cycloplegic refractions and prescribing
At the time of writing, waiting lists for NHS appointments due to the pandemic have increased. Therefore children referred for amblyopia/suspected strabismus/reduced vision face an extended wait. Optometrists in primary care can provide an invaluable service by conducting a cycloplegic refraction and prescribing spectacles to correct significant refractive error that is outside the norms for their age group. If refractive error is the only cause of reduced vision, this could be monitored in primary care. Benefits for the child include better cooperation as they become familiar with the optometrist, ease of access and flexibility of appointments for the patient. Visual acuities should be reviewed in three to four months until no further improvement is found.
Having had new spectacles, children with suspected strabismus or amblyopia should then be referred. Having their best corrected vision will benefit their visual development as the child may still be waiting several months above normal referral pathway targets.
In a hospital eye clinic, the first line of treatment in reduced VA or suspected strabismus is a cycloplegic refraction (1% cyclopentolate) and spectacles for any refractive error found. The child is then assessed 8-12 weeks with full time spectacle wear before any other treatment is considered. Therefore, a child already wearing prescribed spectacles from the community and whose refraction is confirmed by the hospital optometrist’s cycloplegic refraction, can commence further treatment e.g. occlusion without waiting another 12 weeks. Community optometrists who have prescribed spectacles before referral will reduce delay to the treatment process.
Case 1: Refraction results not expected with level of uncorrected vision
Symptoms: A 14-year-old teenager complains of intermittent blurred distance vision at school for the past month. This can occur any time of day. Near vision appears fine. He has been revising long hours for his exams and loves his computer games in his spare time.
Findings:
Vision R 6/7.6 L6/7.6 N5
Ret: R -2.50DS L-4.00DS (fluctuating reflex)
Subjective: R -1.75DS 6/6 L-2.00DS 6/6, N5.
Amplitude of accommodation R 5D L5D Bin 5.5D.
All other clinical findings including ocular motor balance normal. A cycloplegic refraction was performed in view of the uncorrelated findings of uncorrected vision and amount of myopia found, the large difference between the retinoscopy and subjective results, as well as the reduced accommodation.
Cycloplegic refraction findings (1% cyclopentolate): R +0.25DS 6/9.5 L Plano/-0.25 x 180. 6/9.5.
Action: Suspected accommodative spasm causing pseudo myopia. If the ‘dry’ subjective had been prescribed this would have caused more symptoms as the patient would have to accommodate to see clearly. These cases need careful counselling to find the cause of the spasm, such as stress, over-use of close vision due to revision and the importance of taking regular breaks. The cycloplegic refraction helps to diagnose pseudomyopia to enable the correct management.
Case 2: Unexplained reduced VA
Symptoms: Blurred vision for past 12 months, vague history in a 20-year-old man. Currently unemployed. One episode of presumed optic neuritis in RE one year ago and seen in the hospital eye service when VA first dropped and now both eyes. Many routine investigations including electrophysiology findings inconclusive. Now very depressed due to reduced vision. Observed to be reading on mobile phone in waiting area.
Signs:
Vision R 6/120 L 6/120 N4.8
Ret: R -2.00DS 6/120 L -2.25DS 6/60
Subjective R -2.00DS 6/60 L-2.25DS 6/60 N48.
Cycloplegic refraction was carried out as a baseline as no ocular pathology was found to account for the reduced VAs.
Ret R-1.50/-0.50 x180 6/7.6 L-2.00DS 6/6
Patient did not appear to surprised or pleased that his VA had improved with new refraction. New spectacles prescribed and patient further monitored. This patient presented with the same grossly disproportionately reduced VAs on his follow up. Only when he was under cycloplegia again, he would read smaller lines. In conjunction with his ophthalmologist he was prescribed 1% cyclopentolate for possible accommodative spasm but on review three months later, he did not continue this as he felt it did not help.
This case demonstrates an unusual presentation where the pattern of vision, refractive error and expected result do not add up. The cycloplegic refraction does reassure the clinician the ocular structures and visual pathway are normal as the VAs are normal. It seems highly likely that this is a psychosomatic case where the cause lies in non-ocular factors. Referral for counselling or psychiatric assessment may be required.
Case 3: Refraction dictates management
A five-year-old has attended an eye exam as his school feels he is not concentrating well and is behind with reading.
Vision:
R 6/7.6 L6/7.6 Bin N6, Cover test distance and near: moderate exophoria with moderate recovery breaking down to alternating exotropia. Refraction: fluctuating reflex. Cycloplegic refraction: R +2.00DS L+2.50DS. Ocular health: normal.
Action:
Not prescribed. Refer routinely or commence orthoptic exercises to improve control of exophoria/tropia.
Refraction is an important test but sometimes can be difficult to obtain in children. The cycloplegic refraction determined an accurate result to aid management options. The vision is within normal limits, there is no significant anisometropia and the child is not near the end of the critical period. Correcting the hypermetropia could result in possible increase of divergence, by relaxing the accommodative effort and hence the accommodative convergence. (This could be checked using cover test with the refraction in a trial frame on another day when the cycloplegia has worn off.) This illustrates a case where there is a refractive result, but it is not appropriate to prescribe.
- Sosena Tang is an optometrist based in Hertfordshire. She works in an independent practice and for the East and North Herts NHS trust and is also a College Assessor and Examiner.
