Contact lenses provide visual, practical, and psychological benefits1 for an estimated 140 million wearers.2 Despite this, some individuals experience handling-related issues, such frustrations can lead to ceasing lens wear. Sulley et al reported that handling-related reasons were given by one in four new soft lens wearers who discontinued lens wear within their first year.3
A literature review of contact lens dropout research by Pucker and Tichenor found a pooled mean contact lens drop out frequency of 21.7%. For established wearers the most common reason provided was discomfort, and for new wearers it was dissatisfaction with vision. On a positive note, around three quarters (74%) of drops outs can successfully resume contact lens wear.4
Although there is awareness of handling-related dropout issues, there is surprisingly little published on what specific aspects of handling cause the most difficulties or have the greatest influence on contact lens retention. Wearer experiences are likely to differ between lens materials, lens types and modalities. That is even before personal motivation, expectation and mind set factors are taken into consideration.
As clinicians, some of the guidance provided is based on logic assumption rather than peer reviewed research findings. For example, the requirement for a new wearer to demonstrate application and removal techniques a specific number of times prior to allowing the patient to experience lens wear in their own environment, appears to stem from a general clinical consensus.
Fortunately, inappropriate lens handling, a modifiable behaviour, rarely causes long term consequences, although there have been reports of long-term lens retention in the eye5-7 and increased risk of ptosis.8 Most practitioners are likely to agree that short term lens retention and damaged or broken lenses, often a result of vigorous handling techniques, are more commonplace.
Nevertheless, the more unusual cases are the ones that tend to generate media interest. For example, the case of Good Morning Britain presenter Kate Garraway who had a contact lens stuck in her eye for six days9 and a surgeon reporting removing 27 contact lenses from a woman’s eye during a consultation for cataract surgery, She had been wearing disposable lenses for 35 years, with no complaints of any irritation10 (figure 1).
 Figure 1: 27 lenses that had accumulated in a patient’s eye without reported irritation
Figure 1: 27 lenses that had accumulated in a patient’s eye without reported irritation
This article focuses on patient reported outcomes from a survey exploring the handling experiences and wearing habits of 1,031 soft daily disposable contact lens wearers in the context of current literature and accepted clinical practice.11
Survey overview and wearing patterns
The questionnaire was conducted online in Japan. The respondents were aged between 12 to 49 years old, amongst whom a variety of different daily disposable soft contact lens materials were worn.
Reason for using daily disposables
The most common reasons for wearers preferring disposable lenses, over reusable soft lenses, related to safety, hygiene and convenience related (figure 2). From a handling perspective, factors such as shorter lens care times, and a potential for lower costs if lenses were torn, were also considered important (69% and 37% of wearers respectively).
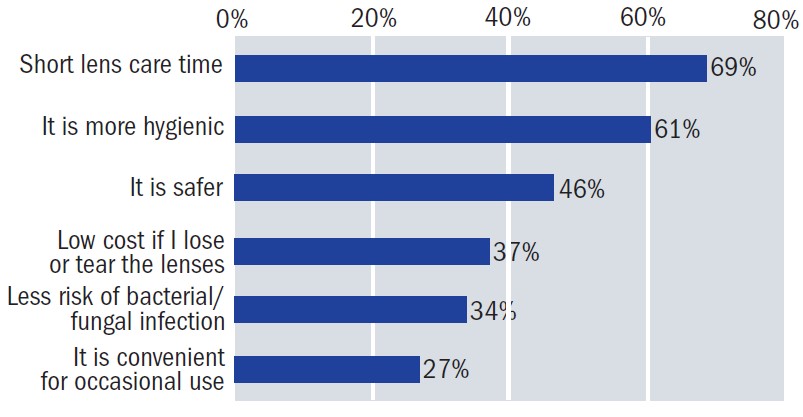 Figure 2: Top reasons for using daily disposables (wearers could select multiple answers)
Figure 2: Top reasons for using daily disposables (wearers could select multiple answers)
Wearing schedules
A quarter of respondents wore their lenses most days (using 50 or more lenses a month) and less than one in five (18%) wore lenses the equivalent to a day a week or less (figure 3).
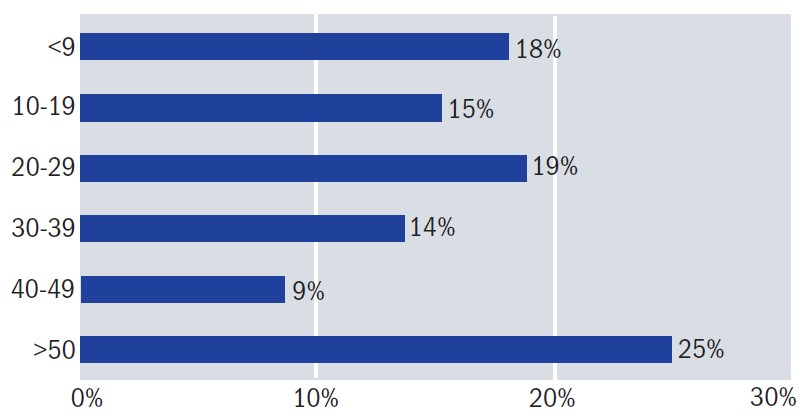 Figure 3: Number of lenses used per month by wearers
Figure 3: Number of lenses used per month by wearers
Just over a half the wearers (56%) wore lenses on average between seven and 13 hours around a third (31%) wore lenses longer and few (13%) wore their lenses less (figure 4).
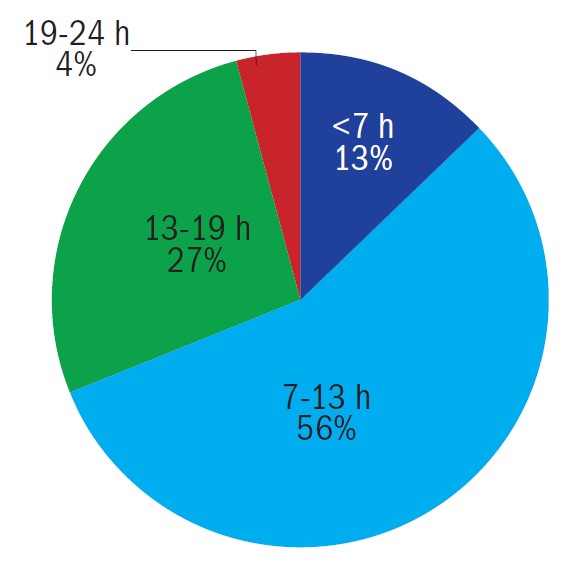 Figure 4: Wearing times per day (in hours, h)
Figure 4: Wearing times per day (in hours, h)
Speed of lens handling
The survey asked respondents about the time taken to apply both lenses following removal from the blister packs (figure 5). This varied from an impressive < 1 minute for just over half (51.3%) of the respondents through to a minority (0.2%) needing 10 minutes or longer. Most respondents (98.4%) spent up to 5 minutes on lens handling, about the same amount of time it takes to make a cup of tea.
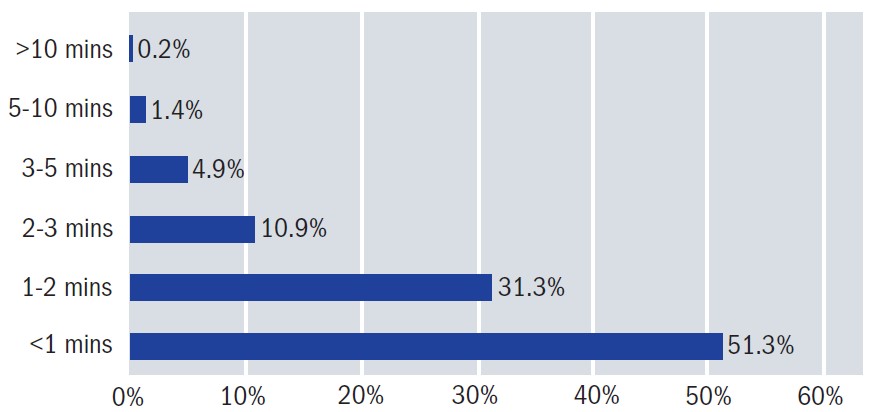 Figure 5: Speed of lens application (in minutes, mins)
Figure 5: Speed of lens application (in minutes, mins)
The findings show that even among established wearers, there is variation in the time spent on lens handling. The results highlight the importance of questioning and observing lens handling and compliance aspects during routine contact lens reviews, doing so may help identify any problem areas that could hinder performance.
Handling related challenges
The good news is that nearly a third (31%) of the wearers who responded to the survey reported no handling difficulties. The top five handling related issues (figure 6) were:
- Difficulty determining if their lenses were inside out
- Lenses easily sticking to the finger
- The blister seal being perceived as hard to open
- Lenses becoming contaminated
- Challenges applying the lens onto the eye
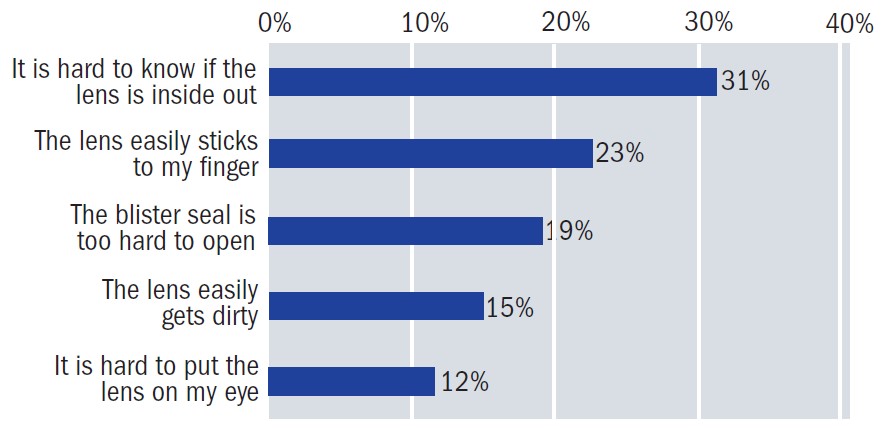 Figure 6: Lens handling related challenges (wearers could select multiple answers)
Figure 6: Lens handling related challenges (wearers could select multiple answers)
Overcoming handling frustrations
Correct orientation and avoiding mixing up lenses
To aid visibility soft lenses may have a handling tint incorporated. For soft reusable lenses, the habit of removing the same lens first (usually the right) followed by the contralateral lens, can a void confusion. For daily disposables, explicit labelling of boxes as ‘right’ and ‘left’ may also help patients avoid mixing up lenses.
Traditionally to help identify the correct orientation of a soft lens, the wearer is advised to view the shape profile in good lighting and check if it is bowl-shaped with the edges pointing straight up while on the finger. The alternative saucer-shape appearance, where the edges turn downwards, indicate the lens is inside out. Another technique is the ‘taco’ test: if the lens edges easily fold towards each other when flexed, the lens is the correct way around, but if there is resistance and curling outwards at the top of the lens edge then it is likely inside out (figure 7).
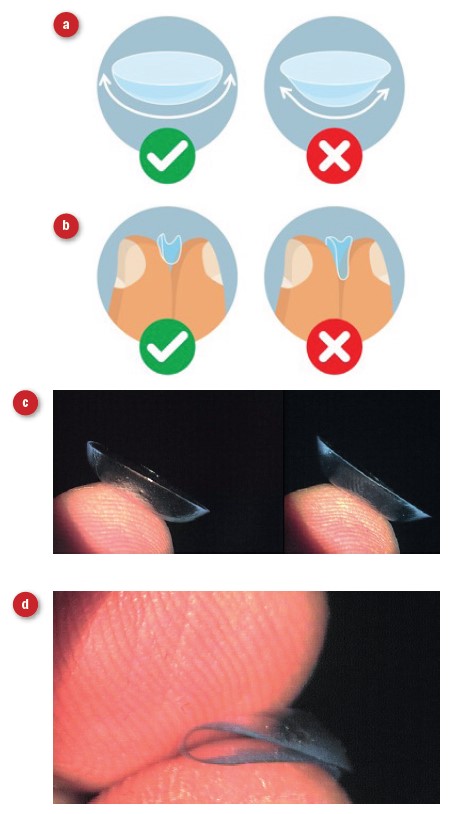 Figure 7: Orientation checks; schematics showing (a) naked eye appearance and (b) the ‘taco’ test. Real-life views of orientation are shown in (c), left correct and right inside out, and (d) the ‘taco’ test
Figure 7: Orientation checks; schematics showing (a) naked eye appearance and (b) the ‘taco’ test. Real-life views of orientation are shown in (c), left correct and right inside out, and (d) the ‘taco’ test
Manufacturers have taken various approaches to overcome the challenge of ensuring whether the contact lens is the correct way around. These includes lens marker engravings, for example 1, 2, 3 or OK indicators or innovative lens packaging focusing on the contact lens positioning within the blister packet. Smart Touch technology (from Menicon) achieves this by raising the lens within the blister packet, allowing it to be pinched from the packaging while maintaining the correct orientation on the finger prior to application. This differs from the traditional approach of scooping the lens out of the bowl-shaped blister packet which risk lens inversion (figure 8).
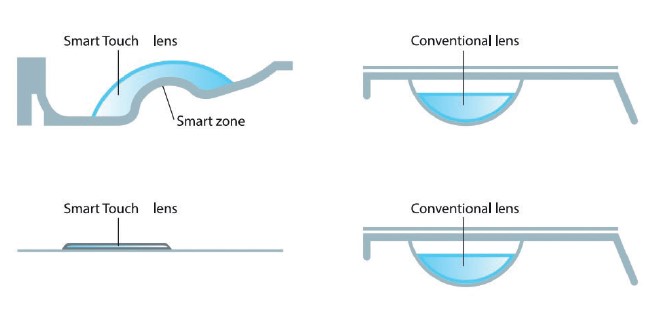 Figure 8: Two Smart Touch technology design concepts compared to conventional packaging. The Flat Pack in the lower image also has less solution (0.2mls versus 0.8mls¹²) to reduce the chance of reuse as a storage device
Figure 8: Two Smart Touch technology design concepts compared to conventional packaging. The Flat Pack in the lower image also has less solution (0.2mls versus 0.8mls¹²) to reduce the chance of reuse as a storage device
Lens interaction with wearer’s finger and hand hygiene
The issue of lenses that seem to stick to the finger (figure 9) was the second most frequently reported issue reported in the survey.
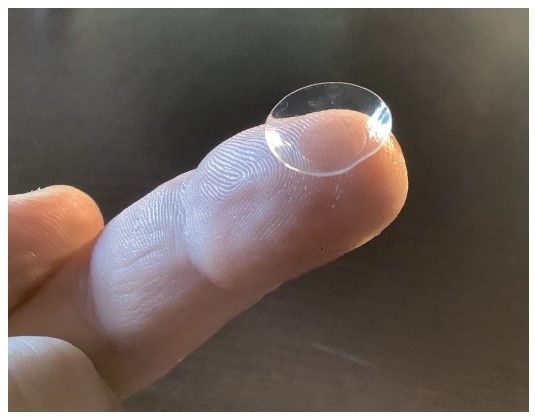 Figure 9: Lenses sticking to the finger is seen as a problem for many
Figure 9: Lenses sticking to the finger is seen as a problem for many
Prior to handling lenses, it is important to ensure hands are clean and thoroughly dried. Yet, in this survey, whilst just under two-thirds of respondents (62%) reported always washing their hands prior to lens handling, less than a third (27%) reported usually doing so and a small number (11%) admitted they rarely or never complied with this requirement.
The finding is consistent with the BCLA CLEAR reports, which indicate 50 to 60% of lens wearers admit to a lack of proper handwashing.13 This is despite handwashing being one of the most regularly discussed, promoted and emphasised compliance points by clinicians.14
Blister opening
The third most reported issue in the survey related to the effort required to open blister packaging. A quick search of the research literature reveals little information on the ideal force needed to open a blister packet. The tendency to produce harder to open contact lens blister packaging than may be optimal stems from a desire to guarantee sterility. During the manufacturing process, the blister package is sealed with heat and pressure before being subjected to sterilisation via autoclave. The autoclave process uses heated steam to sterilise the internal contents of the blister package and introduces a high level of heat and pressure whilst doing so. The seal needs to be capable of withstanding these forces and maintain hermetic integrity for a suitable shelf-life period (typically five years). Unique sealing systems and packaging materials are required to guarantee a low peel force characteristic.
Figure 10 highlights in-house data from a contact lens manufacturer showing the opening force requirements of traditional packaging compared to an innovative flat pack foil blister design. Overall, the force required for the flat pack version is much lower.15
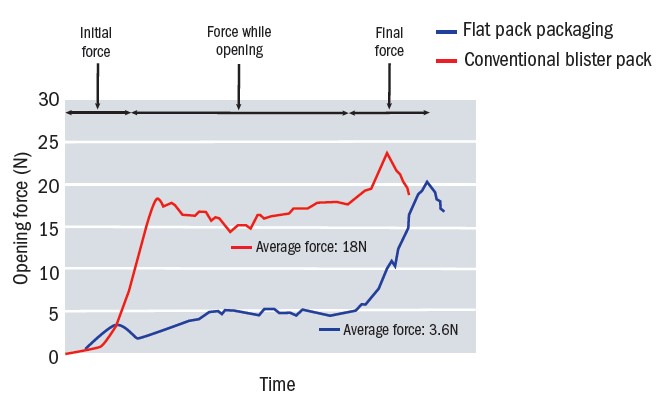 Figure 10: Force required to open contact lens blister packaging (N = Newtons)
Figure 10: Force required to open contact lens blister packaging (N = Newtons)
Lens contamination
Contamination of the contact lens with either pathogenic microorganisms; debris; make up or other particles the lens encounters, can occur during lens handling or wear. The eye’s own natural defence mechanisms may help remove deposition and support with preventing infection,16 but an obvious starting point is to encourage good hygiene principles and provide advice with respect to the patient’s environment and lifestyle.
Rather surprising was the finding that nearly a third (30%) of respondents to this survey reported being unaware of infection risks associated with contact lenses.
One approach to minimise the risk of daily disposable lens contamination during handling is to utilise innovative packaging aimed at avoiding the need to touch the inner contact lens surface, ie the part that comes into direct contact with the eye. A recently published randomised control trial by Tan et al (2021) evaluated the efficacy of such technology in minimising lens contamination. Compared to Smart Touch packaging, conventionally packaged lenses with EDTA and without EDTA had increased risks of contamination on the inner surface of the contact lens of 3.38 and 3.4 times respectively.17 Reinforcing the findings of an earlier study where 3x lower contamination of lenses was also reported when using the Smart Touch packaged lenses.18
Application and removal
The fifth most common reason indicated by respondents, related to time spent applying the contact lens to the eye (figure 11). When asked where they typically apply their lenses, most respondents indicated lens application is usually at their home (85%) with around half (52%) of the respondents revealing they stored their lenses near the washbasin. Bizarrely, some reported keeping their lenses in their fridge, some 2% of respondents.
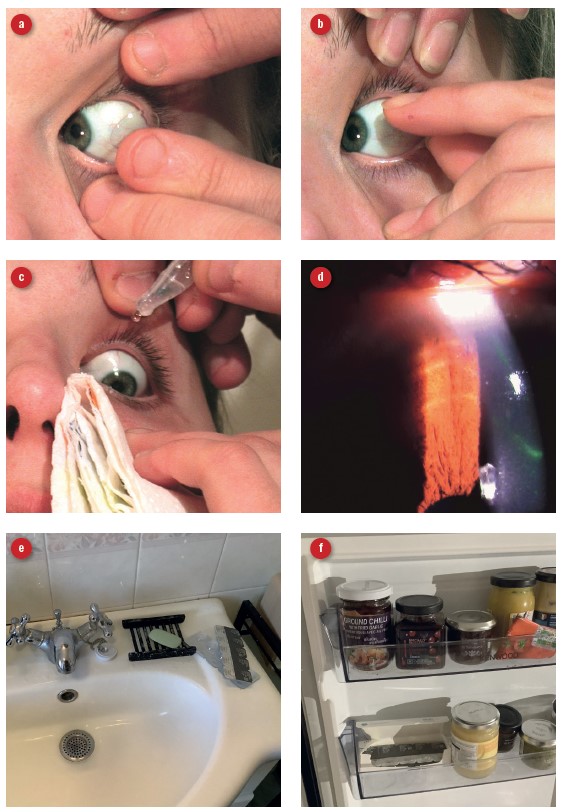 Figure 11: (a) Time spent applying lenses was the fifth most reported challenge. (b)Lens removal was more challenging for a tight, dry lens. (c) Instillation of topical lubricant may facilitate lens removal. (d) Lens removal damage to the epithelium is revealed by fluorescein assessment. (e) 52% of wearers store and handle their lenses near wash basins. (f) 2% of wearers store their lenses in the fridge
Figure 11: (a) Time spent applying lenses was the fifth most reported challenge. (b)Lens removal was more challenging for a tight, dry lens. (c) Instillation of topical lubricant may facilitate lens removal. (d) Lens removal damage to the epithelium is revealed by fluorescein assessment. (e) 52% of wearers store and handle their lenses near wash basins. (f) 2% of wearers store their lenses in the fridge
Observing the wearer’s behaviours and the use of fluorescein may reveal evidence of poor removal techniques. While many devices have been marketed to facilitate contact lens application and removal, there has been little research published to establish their efficacy.
Damaged and retained lenses
Inappropriate handling may result in contact lens shape retention changes, which could influence the contact lens fitting behaviour and performance. Aggressive handling techniques can lead to lenses becoming damaged, with the potential for lens fragments to be retained in the eye. The eye’s anatomical features make it unlikely for lenses to move ‘behind’ the eye, although there have been reports of lenses becoming trapped in the fornix.6 This may be difficult to visualise with the naked eye without manipulation of the lids during slit lamp examination. The use of vital stains such as fluorescein can aid locating dislocated lenses.
Practitioner approach and digital influences
The BCLA CLEAR report on evidence-based contact lens practice concluded that while practitioners may provide relevant advice, this can be poorly recalled by patients.19 Factors such as patient anxiety, which is linked to poor attention, may hinder recall of instructions.20 Additionally, recent work by Hind et al found that while practitioners often provided verbal advice, this was not always supported by written information.21 In the absence of such information recall, patients may seek advice elsewhere: in our ever-evolving digital world the influence of social media and use of the internet for health advice is increasing. Yildez et al reported that while useful online contact lens video resources exist, a large proportion have insufficient information or are poor quality.23 Directing patients to reliable more sources, or an investment in digital offerings either via the practice website or practice app, may help safeguard again erroneous advice.
Conclusion
While handling related issues are more frequently associated with new wearers, this survey highlights that even some established daily disposable wearers may harbour frustrations, including problems such as difficulties with opening lens packaging.
Consideration of all aspects of lens handling at each contact lens review may facilitate earlier detection of non-compliance and inappropriate handling technique. The availability of remote care offers an opportunity to review contact lens handling and compliance in the wearer’s own ‘real world’ environment.
Maintaining a proactive approach, keeping up to date with new technology and product innovation, may also help maximise contact lens performance and reduce the likelihood of dropout.
- Neil Retallic is an optometrist working as the Global Professional Services Manager for Menicon and is the current President of the British Contact Lens Association.
- Dr Manbir Nagra is an optometrist, educator, and researcher. She works as an independent consultant within the optical sector.
The authors would like to thank Kimiko Kadohara for her support with the data analysis.
References
- Sheena Tanna-Shah S, Retallic N. Health and well-being in eye care practice: Riding the emotional rollercoaster of the contact lens journey. Optician, 22 October 2021
- Jones L, et al. The COVID-19 pandemic: Important considerations for contact lens practitioners. Contact Lens & Anterior Eye, 2020. 43(3): p. 196-203
- Sulley A et al. Retention rates in new contact lens wearers. Eye & Contact Lens, 2018. 44 Suppl 1: p.S273-s282.
- Pucker A, Tichenor A. A review of contact lens dropout. Clinical Optometry (Auckl), 2020 Jun 25, 12:p.85-94.
- Agarwal P et al. Retained soft contact lens masquerading as a chalazion: a case report. Indian Journal of Ophthalmology, 2013. 61(2): p. 80-1.
- Holicki C et al. Two soft contact lenses retained in the superior fornix for 15 years in a patient with unique orbital anatomy. Eye & Contact Lens, 2020.
- Arshad I et al. Chronic conjunctivitis from a retained contact lens. Eye & Contact Lens, 2020. 46(1): p. e1-e4.
- Hwang K, Kim J. The risk of blepharoptosis in contact lens wearers. Journal of Craniofacial Surgery,2015;26(5):e373–4
- https://www.entertainmentdaily.co.uk/tv/gmb-kate-garraway-horrified-as-doctors-discover-contact-lens-was-stuck-in-her-eye-for-six-days
- https://www.bbc.co.uk/news/health-40630852
- Menicon data on file. Online survey 2011.
- Menicon data on file. Internal in-house measurements.
- Wolffsohn J et al. CLEAR - Evidence-based contact lens practice. Contact Lens & Anterior Eye, 2021. 44(2): p. 368-397
- Wolffsohn J et al. British Universities Committee of Contact Lens Educators (BUCCLE). History and symptom taking in contact lens fitting and aftercare. Contact Lens & Anterior Eye. 2015 Aug;38(4):p.258-65
- Menicon data on file: Internal in-house data
- Stapleton F et al. CLEAR - Contact lens complications. Contact Lens & Anterior Eye, 2021 Apr;44(2):p.330-367
- Tan J et al. Factors affecting microbial contamination on the back surface of worn soft contact lenses. Optometry & Vision Science, 2021. 98(5): p. 512-517.
- Nomachi M et al. Evaluation of diminished microbial contamination in handling of a novel daily disposable flat pack contact lens. Eye & Contact Lens, 2013. 39(3): p. 234-8
- Wolffsohn J et al. CLEAR - Evidence-based contact lens practice. Contact Lens & Anterior Eye, 2021. 44(2): p. 368-397
- Court H et al. Evaluating patient anxiety levels during contact lens fitting. Optometry & Vision Science. 2008 Jul;85(7):p.574-80
- Hind J et al. The differences between patient and optometrist experiences of contact lens hygiene education from the perspective of a Scottish university teaching hospital. Contact Lens & Anterior Eye. 2020 Apr;43(2):p185-188
- Business Insider Intelligence. Social media platforms used by US adults during the COVID-19 outbreak. March 2020
- Yildiz M et al. Evaluation of the quality, reliability, and educational content of YouTube videos as an information source for soft contact lenses. Eye & Contact Lens, 2021. 47(11): p. 617-621
