One of the best ways of learning and developing skills is through practical experience. This week, we are introducing an opportunity for you to earn an interactive CPD point by submitting a case study of your own. This might relate to clinical practice, a management decision, an interesting dispense or a legal issue you have resolved.
Optician has assembled a panel of experts in a full range of subjects that cover the four main CPD domains. These are:
Core domains
- Professionalism; maintaining standards of practice
- Communication; issues of consent and good communication
- Clinical practice; see later examples
- Leadership and accountability; record-keeping, supervision, practice environment
Specialty domains
- Contact lens opticians; contact lens cases
- Therapeutic optometrists; therapeutic cases
Each day, each patient encounter can teach us something. By considering each case, what the challenge was and what we did, we continue to develop our professional skills to the benefit of the patient. In this article, we show some case examples we have previously published in the hope that they might spur you on to send in some of your own. Every submission will be reviewed by our assembled panel of experts, feedback will be given, and where appropriate, confirmation of an interactive CPD point will be given.
I hope you find this an exciting opportunity to supplement your CPD portfolio in the coming years.
Case - Crowded optic disc (Kirit Patel)
Presentation
An 11-year-old Chinese patient attended for a routine eye examination with no obvious complaints.
Clinical findings
Refraction was normal, with no need for spectacles, and no colour vision defect was found.
Fundus examination revealed a very hyperaemic right optic disc, the redness central to nasal with a temporal crescent seen. The left optic disc appeared normal. Autofluorescence revealed no fluorescence suggesting no obvious evidence of drusen at the nasal edge. OCT showed a raised right optic disc along the nasal aspect, with a maximum 469 µ lift on the superior nasal aspect (see figure 1). The diagnosis was probable buried disc drusen along the nasal aspect.
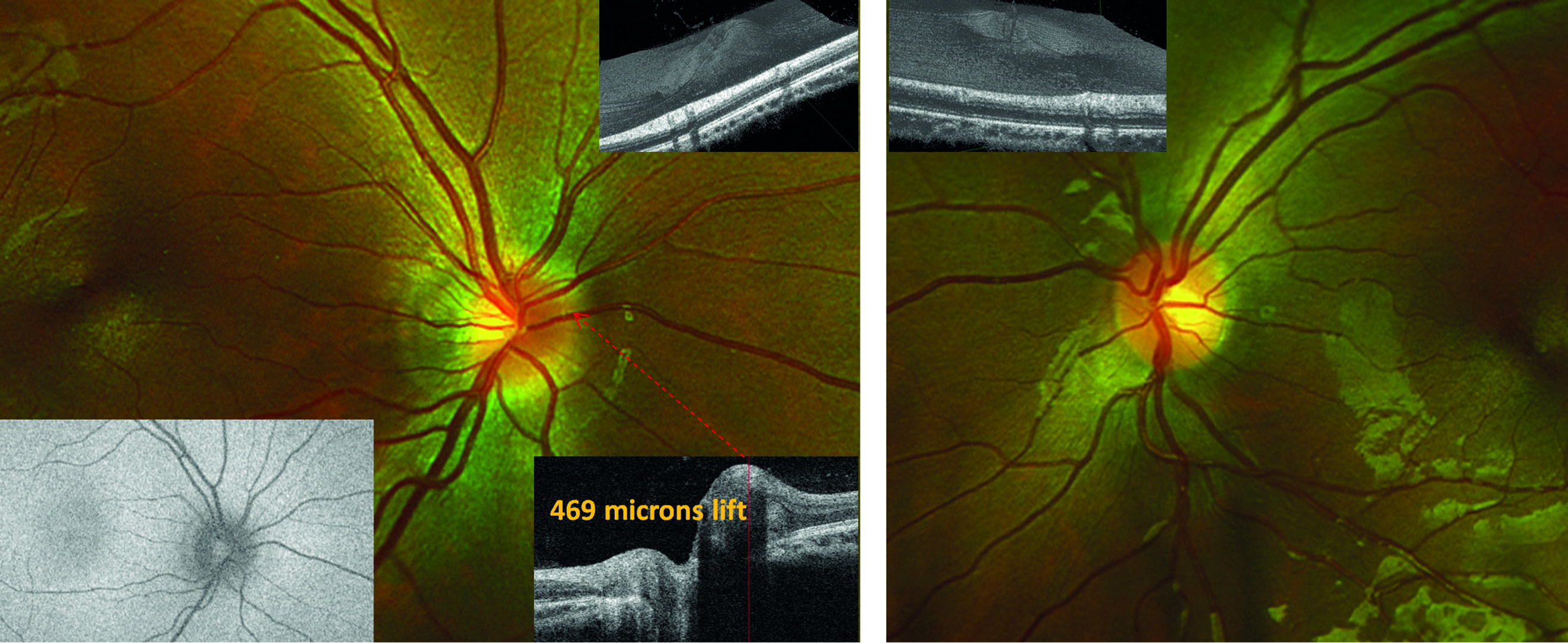 Figure 1: The right optic disc (main left) appears swollen nasally due to buried disc drusen. OCT (other insets) show elevated area. Autofluorescence (inset bottom left) shows no brightness indicative of drusen suggesting the drusen are yet to near the superficial tissue. The left disc (main right) appears normal
Figure 1: The right optic disc (main left) appears swollen nasally due to buried disc drusen. OCT (other insets) show elevated area. Autofluorescence (inset bottom left) shows no brightness indicative of drusen suggesting the drusen are yet to near the superficial tissue. The left disc (main right) appears normal
Management
In this case, there was no need for referral and the patient was to be monitored.
Discussion
Optic disc drusen are globular, often calcified, hyaline (glassy or translucent) bodies located within the optic nerve head. Drusen are relatively common, found in 1 to 2% of the population, and are thought to be inherited in an autosomal dominant pattern, though no specific gene has yet been found. The implied inheritance means it is advisable to screen siblings of any patient presenting with disc drusen.
Disc drusen are bilateral in 75% of cases, and the excrescence is more often seen on the nasal half of the disc. Drusen usually become visible after the age of 10, but sometimes appear at the surface at a younger age than this. Before this, they are buried and may give an appearance of papilloedema. At this stage, the drusen do not affect central vision so might easily be missed except, though compression of the retinal nerve fibres may result in a field defect. This abrupt, painless loss of peripheral vision may be detected with fields assessment of older patients and can mimic primary open angle glaucoma. A rare complication of disc drusen is the development of a choroidal neovascular membrane. Optic disc drusen have an association with angioid streaks in 25% of patients.
Case - Dry eye (Beth Ralph)
Patient booked in to the dry eye clinic.
Presentation
- Female, age 61
- Reason for contact; had spoken to GP at beginning of lockdown due to uncomfortable eyes. Had been recommended drops (name not known). Little used as ‘did not like them’
- Working from home due to Covid lockdown. Uses laptop seven to eight hours per day. Renovating property ready to move into – likely exposure to dust
- General health; menopausal, reports hot flushes for last seven to eight years. Asthma
- Medications; salbutamol inhaler as required
- History; seasonal allergic rhinitis but reports no symptoms at present
- CL wear – previous soft lens wear, lapsed c20 years ago due to poor comfort
Clinical findings
- Eyes still ‘uncomfortable,’ R worse than left
- Refraction
- • R; -3.50 (6/6 +2)
- • L; -4.00 (6/6 +2)
- • Add + 2.00 (N5 R&L)
- Slit-lamp with fluorescein
- Left (figure 2); complete blink, line of inferior desiccation stain, scattered temporal punctate stain, fluorescein break-up time five seconds
- Right (figure 3); incomplete blink, band of inferior desiccation stain, scattered temporal punctate stain, fluorescein break-up time four seconds
- Slit-lamp with white light (figure 4)
- Blepharitis crusting around lashes, R; grade 2, L; grade 1
- Inspissation of meibomian gland openings, R>L
Note; after further questioning to ascertain possible cause of R>L asymmetry of signs, patient revealed she is aware of rubbing the right eye more than the left, and prefers to sleep on her right side. Video capture confirmed that the lagophthalmos is only apparent on the right
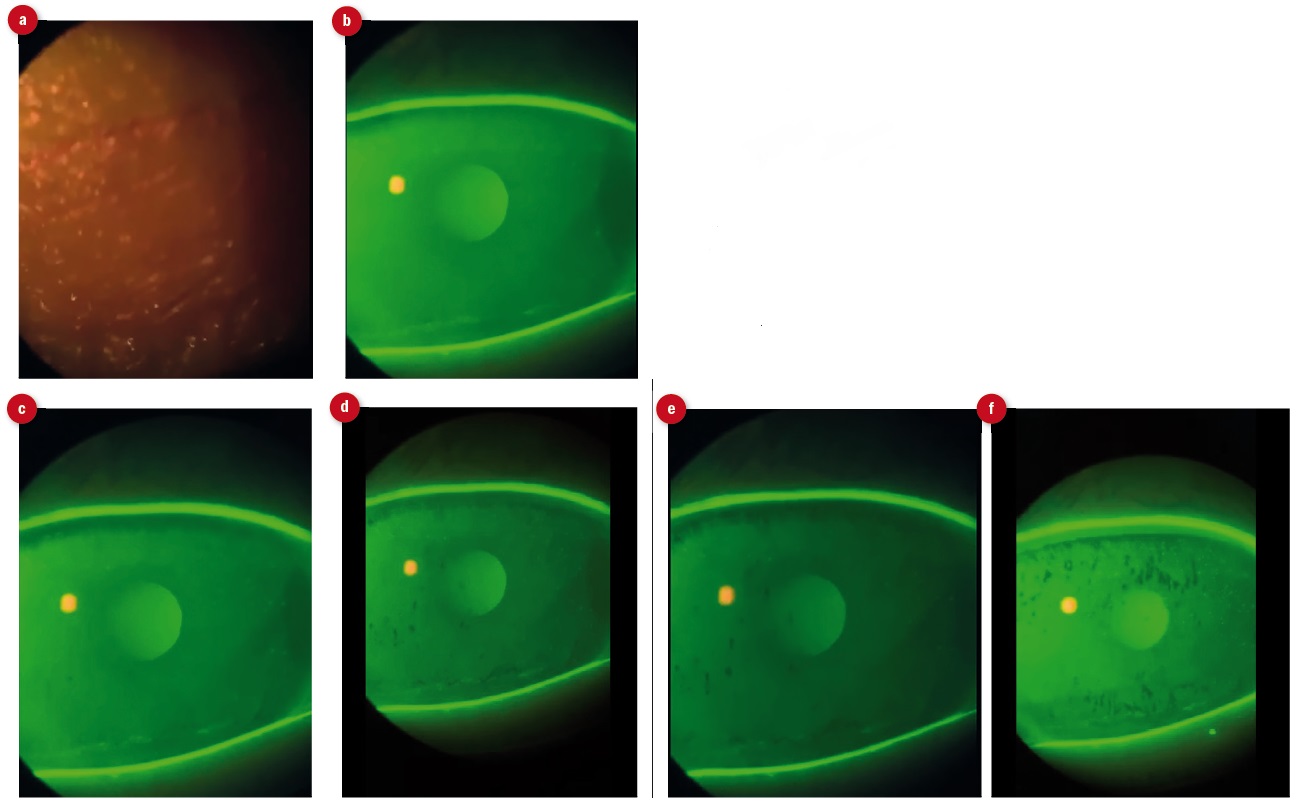 Figure 2: Stills from video of fluorescein break-up time for left eye. (a) initial blink, (b) three seconds and inferior desiccation visible, (c) five seconds and break up spots visible, (d) nine seconds, (e) 11 seconds and (f) 13 seconds
Figure 2: Stills from video of fluorescein break-up time for left eye. (a) initial blink, (b) three seconds and inferior desiccation visible, (c) five seconds and break up spots visible, (d) nine seconds, (e) 11 seconds and (f) 13 seconds
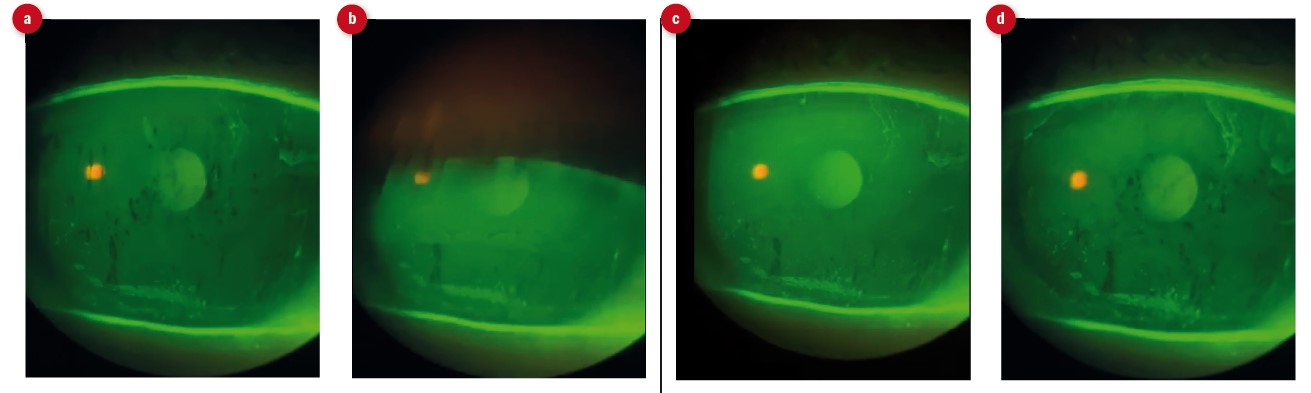 Figure 3: Stills from video of fluorescein break-up time for right eye. (a) pre-blink appearance showing multiple sites of break-up, greater inferior desiccation than left and scattered desiccation stain over cornea, (b) moment of maximum blink showing clear lagophthalmos, (c) tear break up at four seconds post-blink, (d) appearance eight seconds post-blink
Figure 3: Stills from video of fluorescein break-up time for right eye. (a) pre-blink appearance showing multiple sites of break-up, greater inferior desiccation than left and scattered desiccation stain over cornea, (b) moment of maximum blink showing clear lagophthalmos, (c) tear break up at four seconds post-blink, (d) appearance eight seconds post-blink
 Figure 4: (a) Right lower lid showing crusting of the lashes, irregular lid margin and whiteness of meibomian gland orifices due to inspissation. (b) Upper lid lash crusting
Figure 4: (a) Right lower lid showing crusting of the lashes, irregular lid margin and whiteness of meibomian gland orifices due to inspissation. (b) Upper lid lash crusting
Management
- Lid therapy; twice daily use of a warm compress (issued with Eye Doctor mask) followed by lid massage
- Eye lid cleaning; Blephasol Duo and pads to cleanse lids after lid heating and massage
- Tears; Theoloz duo gel (twice a day) or Theoloz Duo drops (every four hours) discussed. After previous experience and in-practice trial, patient preferred gel option preferred gel.
- Information given about safe computer use and blinking
- Review booked for one month.
- All images and video were taken using a smartphone (in this case, the iPhone 11) and a slit-lamp adaptor. The resolution of modern smartphone cameras is easily good enough to capture useful clinical signs as either stills or short videos
- The magnification of the slit-lamp may be complemented by that of the image either during capture or post-capture. Post-capture images may be further enhanced (for example, filters added or contrast enhanced) by image software included in standard software platforms
- Since the initial lockdown, there has been restricted access to many health care services, such as a GP, and eye care professionals are seeing an increase in the numbers reporting problems such as those seen here that can be dealt with by available ECPs
- Use of image capture equipment as shown here can help to reduce the duration of time spent in close proximity to a patient at the slit-lamp. The viewing screen on the smart phone can bee seen from some distance and capture may be set to operate by voice command or by a Bluetooth-linked remote-control button (as is supplied, for example, with the slit-lamp adaptor provided by Bond-Eye). Also, video capture can be viewed and measurements such as timings taken away from the patient and using accurate digital timings
It is essential to use the slit-lamp orange absorption filter (Wratten) along with the blue excitation filter to achieve the best image of any stain or fluorescence
Case study - Vascular disease co-morbidity
Presentation
A 61-year-old female, attended clinic in October last for a first low vision assessment on the recommendation of a member of the local Stroke Association support co-ordinator. Having, it seemed, suffered a stroke some two months previously, it was felt that her mention of ‘problems with her vision’ warranted a low vision assessment.
She attended today with her son as had some balance concerns, so was not confident on her own out of the home. This seemed, in part, related to a feeling that she was missing things ‘on the side’ though could not specify any particular area. She felt her vision was generally poor and was struggling to read.
She also relied on her son throughout the test as clearly had short term memory problems and was also somewhat confused and ague about her recent history. Existing pre-test notes were minimal, so a note was made to liaise with the Strokes Team and the GP after my assessment.
Assessment
Relevant clinical findings:
- After the stroke she had been aware of a ‘cloud’ in her right vision that, over the subsequent weeks, had evolved into ‘blotches’ and was currently hardly noticeable
- She was on anti-hypertensive medication only. Post-stroke, her blood pressure had been checked regularly and was within normal limits at last test.
- She was not a smoker.
- Distance static vision (she had no distance correction) was R 0.2 and L 0.1 logMAR (N6 R&L with +2.50D ready readers)
- Letter identification was good but scanning/reading was poor – she complained that letters were ‘jumbling’
- Refraction showed minimal spherical hyperopia and presbyopia
- Binocular status appeared orthophoric in all directions
- Concentration and fixation for tasks were poor throughout
- IOP was 14mmHg R&L at 14.00 with rebound tonometry (iCare)
Visual fields
- Gross perimetry suggested a superior right homonymous quadrant loss
- Humphrey C40 supported this, though fixation was poor (see figure 5 for simulated result). Loss appeared greater and less localised in the right eye
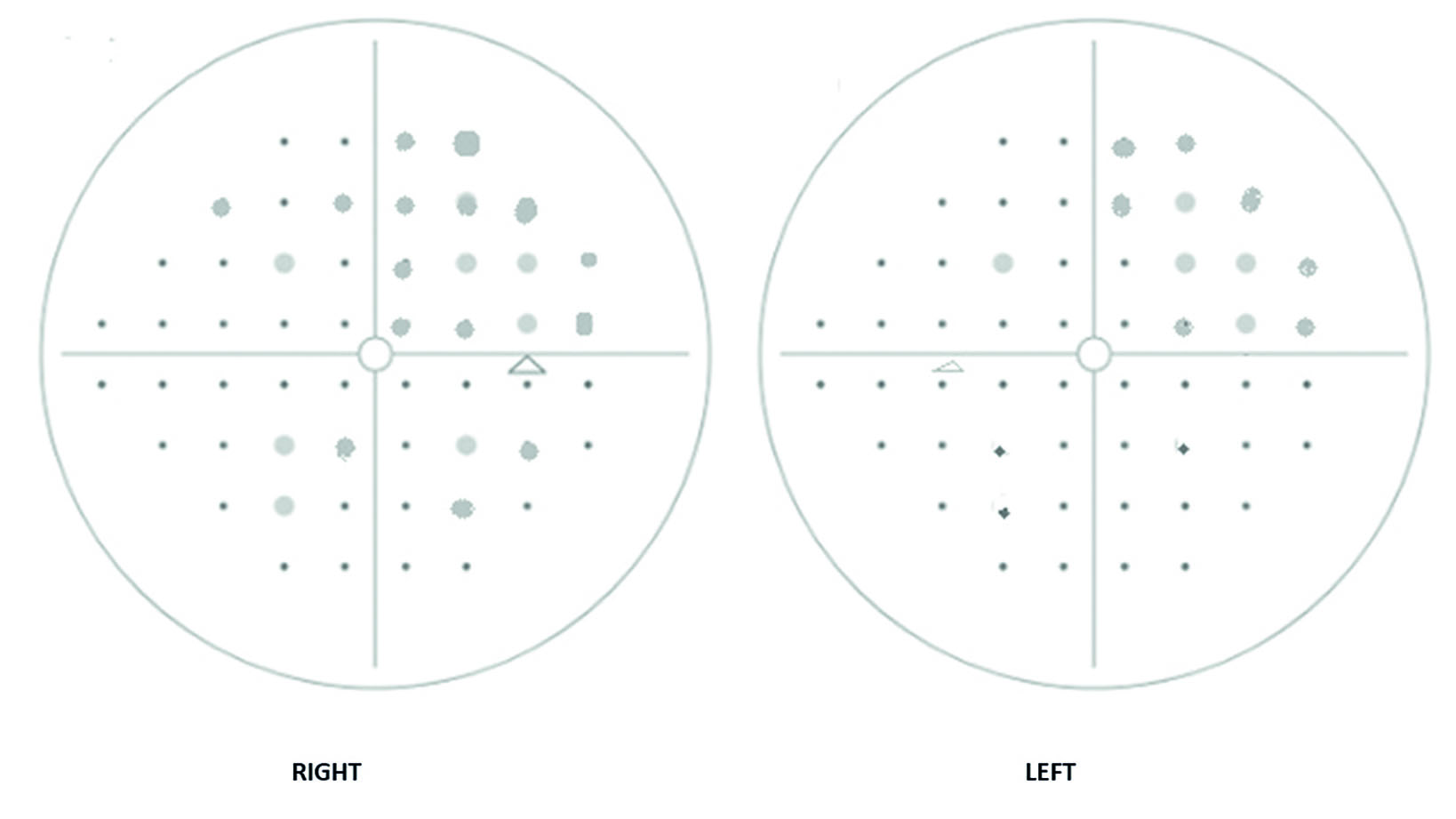 Figure 5: Simulated Humphrey C-40 results suggesting homonymous superior right quadrant loss and extended loss in the right eye
Figure 5: Simulated Humphrey C-40 results suggesting homonymous superior right quadrant loss and extended loss in the right eye
OCT/photography
- Despite poor fixation and some patient reluctance to be tested, retinal images (figures 6 and 7) and a 3D macula scan were obtained (figure 8, OCT scan quality not great alas)
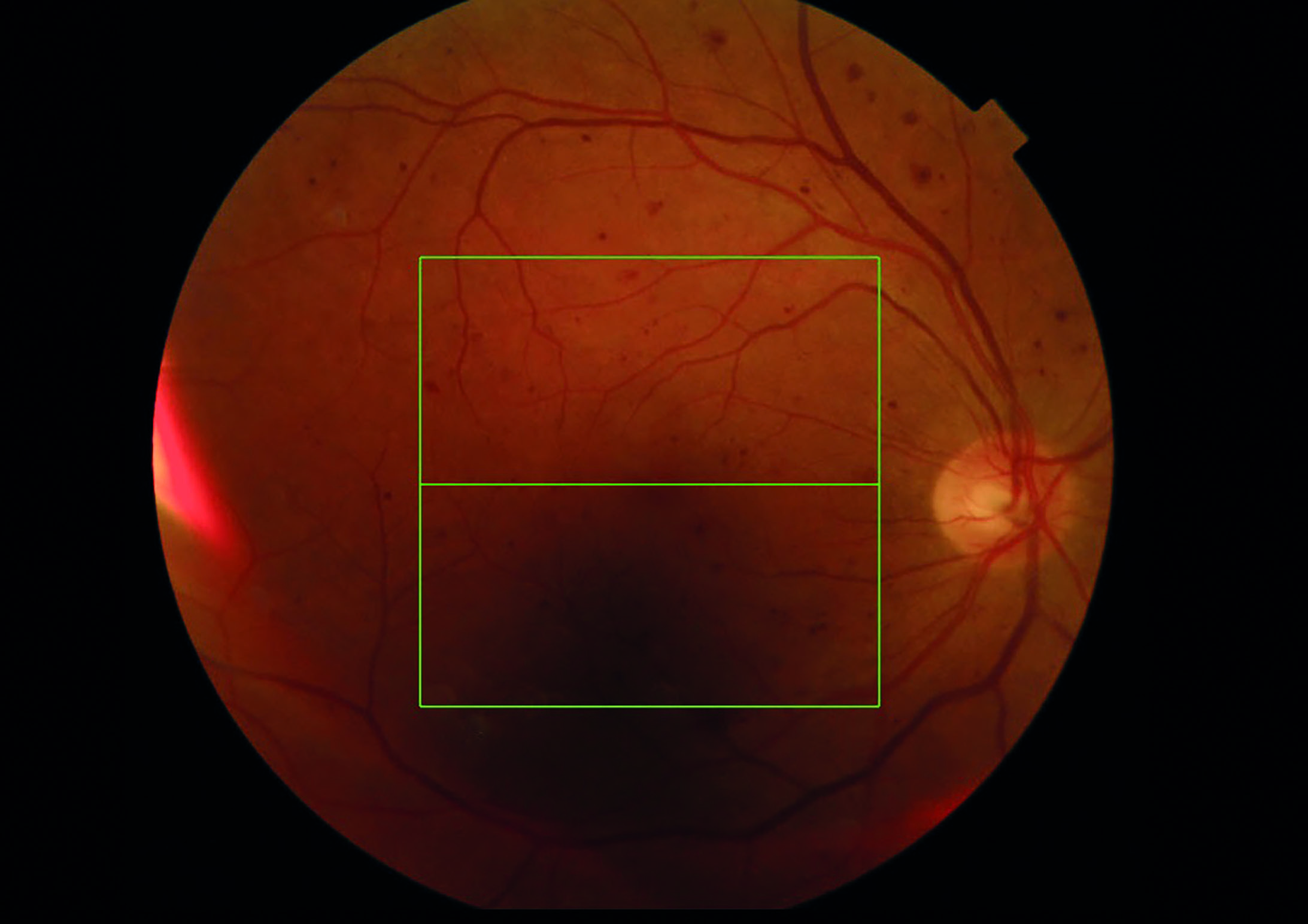 Figure 6: Right retinal image showing extensive ‘blot-like’ haemorrhaging indicative of a possible resolving central retinal vein occlusion
Figure 6: Right retinal image showing extensive ‘blot-like’ haemorrhaging indicative of a possible resolving central retinal vein occlusion
 Figure 7: Left fundus image with fewer haemorrhages but suggestive of previous hypertensive influence
Figure 7: Left fundus image with fewer haemorrhages but suggestive of previous hypertensive influence
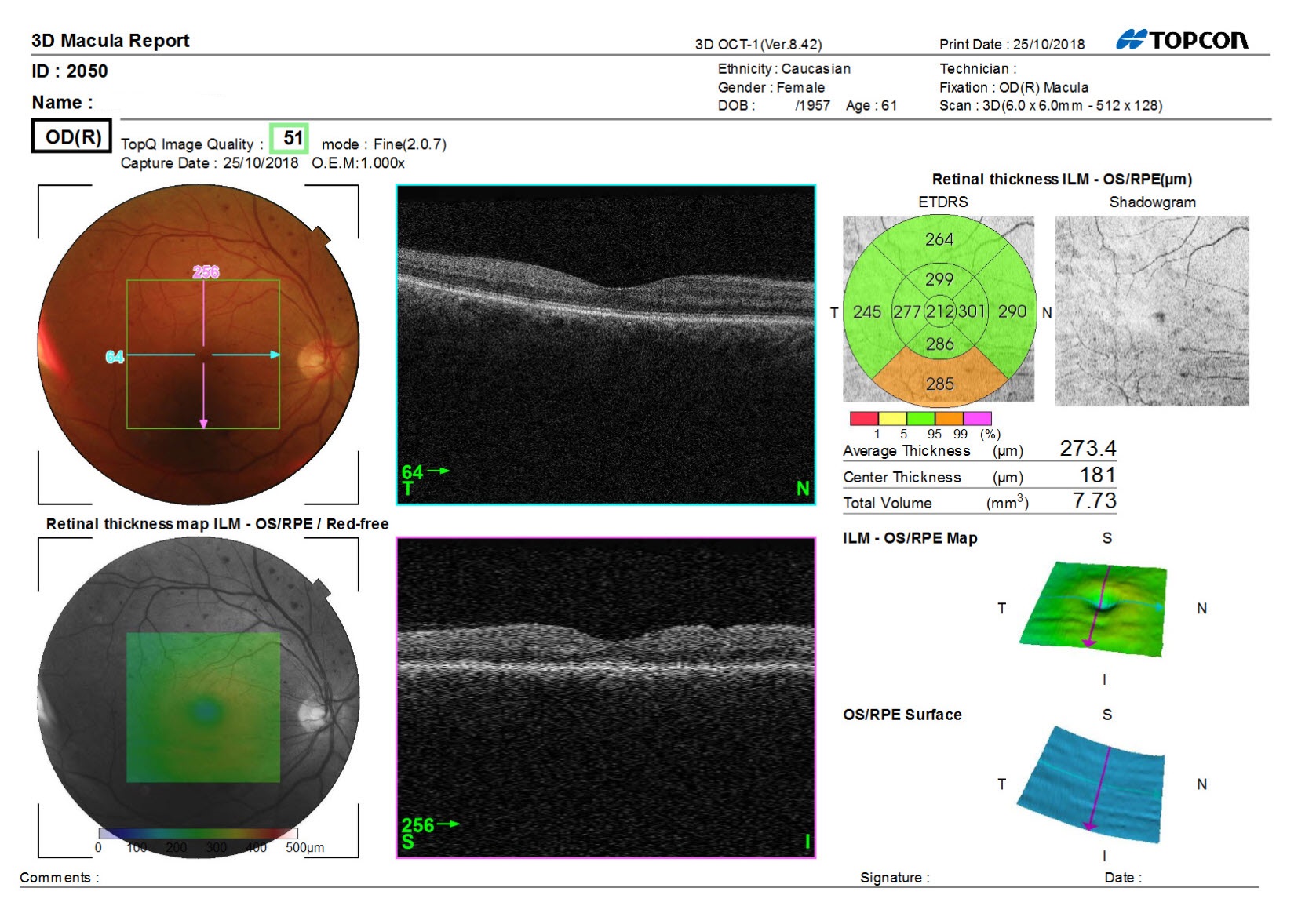 Figure 8: 3D macula scan of the right eye. Poor scan quality but no indication of significant macular oedema.
Figure 8: 3D macula scan of the right eye. Poor scan quality but no indication of significant macular oedema.
Management
There was some doubt as to whether this was the first post-stroke eye assessment. The retinal images both showed some residual signs of accelerated hypertension, primarily blot-like haemorrhages. There were no cotton wool spots nor signs of macular oedema, though the poor scan meant the thickness data was not reliable.
The right eye showed extensive widespread haemorrhagic changes which, when taken into account with the reported right visual symptoms, suggested a possible previous central retinal venous occlusion event now mainly resolved.
A referral was made to see ophthalmology as soon as possible (within two weeks) to review vascular patency, and confirm the field loss.
No aids or correction were issued at this stage as static acuity seemed acceptable. The main concerns to be addressed would be mobility, and also visual target association and interpretation which, it is hoped, will show some improvement before the next assessment after hospital review. Full records were sent to the stroke team and also the GP with an assumption that cardiovascular health status will be closely monitored over the period.
Discussion
Bilateral field loss respecting the vertical midline is likely where a cerebrovascular accident impacts upon the post-chiasmal visual pathway (here, likely the left inferior radiations). Problems of visual interpretation and assimilation imply parietal as well as temporal lobe involvement. This is important to establish for ongoing rehabilitation planning and time will tell how well the patient is able to adapt to their new visual world.
The likelihood of a concomitant retinal vascular incident should not be a surprise when one considers that the risk factors for stroke are likely also to be risk factors for retinal vascular occlusion.
Maintaining full communication with all other involved professionals (ophthalmology, GP, strokes team) is essential for ongoing care. It is quite possible for a patient to have had a stroke and be seen at a hospital and by sensory support teams, but without any ocular examination being undertaken until a referral to an optometrist is initiated.
Case - Asymmetric acuity (Sosena Tang)
Presentation
A four-year-old attended with their mother for their first eye exam. No problems reported but there is a family history of spectacle wear as children.
Assessment
Vision: R 6/9 L6/7.5 B6/9
Cover test D & N: orthophoria
Retinoscopy R +1.00DS L +1.50DS fluctuating reflex
NPC: to nose
Motility: full
Stereoacuity: 200’ Titmus test without Rx (figure 9)
 Figure 9: Titmus stereopsis test
Figure 9: Titmus stereopsis test
Management
Although the visions are borderline the presence of a possible prescription and unreliable retinoscopy and reduced stereoacuity would alert the practitioner that perhaps there is a bit more hypermetropia. In this case, a cycloplegic refraction would be recommended to rule out any more ametropia.
Discussion
Had the stereoacuity been better, perhaps 40’, it would indicate good accommodation and binocular single vision and less likelihood to finding uncorrected ametropia. An improved stereoacuity after the prescription was prescribed would give a good indication that it was helping the child’s near vision and binocularity.
Case - Presbyopia
A 42-year-old female patient appeared to show signs of incipient presbyopia (feelings of strain especially when using a tablet or smartphone in the evening – ‘for eBay’ – figure 10) along with digital eye strain (the same accompanied by grittiness and blurring on blink exclusive to screen viewing). She only recently had increased evening tablet use, which could be anything up to three hours at any one time. Typical working distance 50cm.
 Figure 10: Patient struggling with asthenopia
Figure 10: Patient struggling with asthenopia
She was anisometropic, had undergone spectacle and occlusion treatment when aged five to seven years, and had worn spectacles sporadically (‘for concentrating’) until aged 35 when she started wearing one-day silicone hydrogel lenses full time (R; +2.00 L; +3.00). Apart from the reported symptoms, vision and comfort were generally good with contact lenses and she was very resistant to the idea of spectacles. Health was good. Patient is a regular smoker of around 20 cigarettes a day.
Assessment
Refraction;
- R; +1.75DS (6/4)
- L; +3.00/ -0.50 x 90 (6/5)
- N5 (R and L) to 20cm
Cover test showed orthophoria at distance and near and near point of convergence was ‘to nose’.
There was evidence of significant tear instability, with conjunctival and corneal desiccation, irregular tear prism and a fluorescein tear break up averaging four to six seconds on repeat.
All other clinical findings were unremarkable relating to this case.
Management
The above prescription was ordered along with the +0.60DS addition option Eyezen lens.
- Frame chosen offered fitting heights of 23mm R&L (a minimum of 18mm is recommended)
- Mono CDs were R 31mm L 32mm
- Face form angle was four degrees (this must be a positive value)
- Pantoscopic angle was eight degrees (between eight and 12 is recommended)
- BVD was 8mm (8 to 10mm is ideal)
Discussion
A few points need to be considered. Prescribing the first reading addition may seem an easy choice but it is worth remembering that, in some cases, this may reduce the already existing ability to accommodate the required amount. A sudden increase in near digital task work can trigger symptoms and contribute to what is now established as the condition ‘digital eye strain’. Even though accommodation here (+5.00DS) should be adequate, a small addition along with advice regarding positioning and lighting should help with the visual symptoms. To be sure this would help it was absolutely essential to confirm the patient was orthophoric at near as any exophoria in a symptomatic patient may actually be made worse by the introduction of an addition.
Contact lens wear seemed to be exacerbating the impact of tear film disruption and evaporation and the patient is now fully aware of the need for regular breaks, improved blinking behaviours, hydration measures, and also that, as well as being linked to the other well-known concerns, smoking is bound to be aggravating the discomfort.
The use of a small addition spectacle lens offered an opportunity to encourage better visual stability in the evening, not only by removing contact lens influences altogether, but perhaps helping improve the pre-ocular humidity.
- Look out for more details on CPD case studies next week
