It is only as eye care professionals themselves become presbyopic that they realise for the first time the full implications of ‘old sight’ and the challenges associated with losing the ability to accommodate to focus objects clearly at near. As patients’ reading additions increase, for many occupations, including the optical professions, everyday work tasks become more and more difficult to satisfy with one, or even two pairs of spectacles.
Additionally, older patients exhibit increased prevalence of ocular and general health conditions that can impact on their ability to use a given optical appliance successfully. Older patients may be at higher risk of falling or may have issues with posture, balance, dizziness or any number of disabilities, and all patients are undergoing changing visual demands to cope with changes to their modern lifestyle.
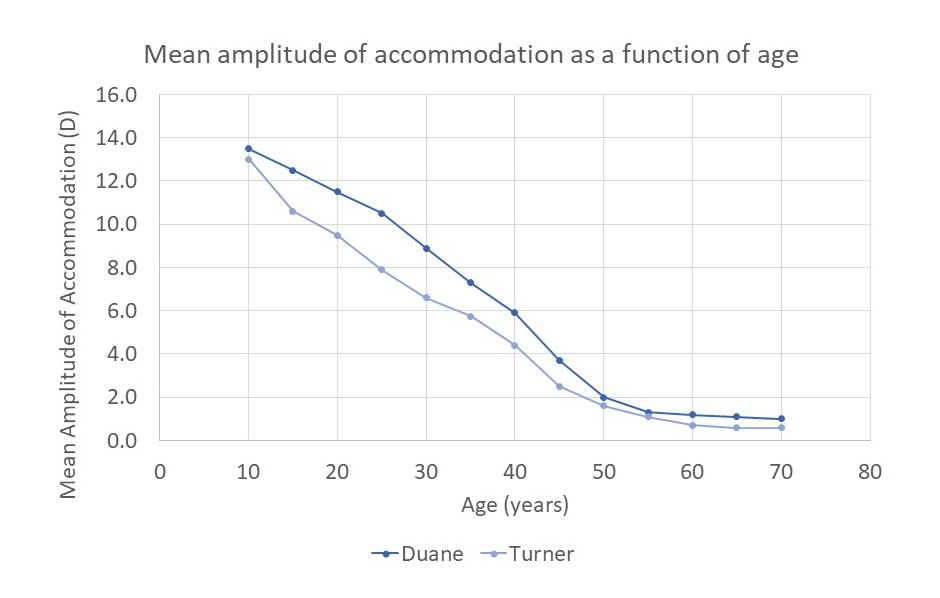
Figure 1: Results of research into amplitude of accommodation. Duane used the push-up method and Turner the push-out method
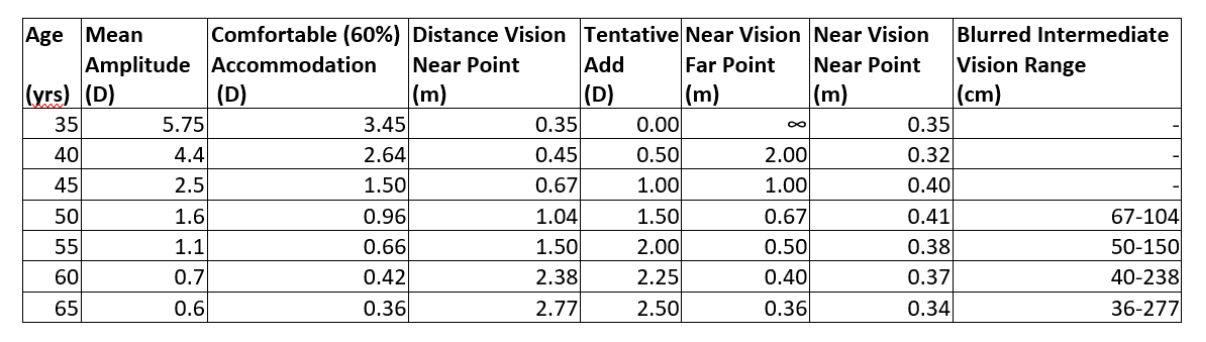 Table 1: Mean amplitude of accommodation as a function of age
Table 1: Mean amplitude of accommodation as a function of age
Patients who previously struggled to see the clock on the video recorder now struggle to spot the correct app on their smart TV, and even the very oldest patients are learning to adapt to an online world. The Covid-19 pandemic has further accelerated the process of digitisation, with many services simply no longer available except through online portals.
Tasks that require near or intermediate vision at or above head height become increasingly problematic as the reading addition increases and accommodation wanes, and even the most mundane intermediate task becomes impossible with either reading spectacles or traditional bifocals set up for distance and reading.
As people age, it becomes increasingly likely they will develop cataracts. This in itself can be a challenge, as it reduces contrast and causes light scatter. However, if we consider aphakia and pseudophakia as special cases of presbyopia, cataract surgery itself is now increasingly presenting challenging prescriptions. There is currently an obsession with leaving an eye approximately emmetropic following cataract surgery. However, patients who have previously lived with significant ametropia might often now be left significantly anisometropic following surgery. This can cause a host of practical and optical problems that could have been avoided if the lens implant had been calculated to leave the patient with approximately the same prescription as that to which they were accustomed. This is especially problematic if the second eye does not have a cataract, is not ready for surgery, cannot be operated upon, or is trapped in a long waiting list.
The three ‘A’s
The three ‘A’s are:
- Accommodation
- Addition
- Age
A patient’s age, accommodation and addition are all related, and although there are individual differences and also difference according to the type of refractive error (presbyopia occurring generally later in myopes and earlier in hyperopes relative to emmetropes) there are some useful rules of thumb to bear in mind. As mentioned in previous articles, a tentative reading addition is 0.50DS for every five years over the age of 35. So, a 40-year-old requires a +0.50DS add (which may or may not be worth prescribing), a 45-year-old a +1.00DS add, and so on up until the age of 60, where an addition of approximately +2.50DS is required. Above this age, the relationship no longer applies as higher adds are often a function of the need for magnification as deteriorating visual acuity and functional amplitude has reduced to a minimal value. A cursory analysis of practice management system data shows many patients in their 70s and 80s are happy with a +2.50DS add and that +2.25DS is a more accurate average for the add prescribed for 60-year-olds.
When dispensing presbyopes, it is vital to calculate the far point and near point of accommodation through both the distance and reading correction. It is essential to properly understand the visual issues in order to determine the best solution for the patient. If the prescribing clinician has not provided the amplitude of accommodation, or when the prescription is from elsewhere to the practice undertaking the dispense, then rules of thumb must be used and the accommodation estimated, unless dispensing opticians measure these values for themselves on the shop floor.
How much of their amplitude of accommodation a patient might be expected to be able to use comfortably when conducting prolonged near vision tasks is a matter of debate. Some authorities suggest half of the available accommodation and others cite two-thirds.
Table 1 has adopted Turner’s values from figure 1 and an assumption that 60% of available accommodation may be comfortably employed. This comfortable level is applied to both the distance vision and the near addition to determine the comfortable near point through the distance prescription for prolonged tasks and then, with the tentative add in place, the comfortable near point of accommodation. The near point of accommodation through the distance Rx is simply the reciprocal of the available comfortable accommodation. The far point for near vision is the reciprocal of the add and the near point, with the add in place, is determined by adding the accommodation to the add and taking the reciprocal.
It can be seen from table 1 that, once the average patient with expected tentative add reaches the age of 50 years, they enter a situation where their near point for distance is further away than the far point through their near prescription. So, there is an intermediate zone for which clear vision cannot be achieved comfortably for prolonged periods. This means that, by 55 years of age, our average patient cannot manage detailed intermediate tasks at all, even for short periods or spot tasks. For almost all patients, by the time they reach their 50s, they will benefit from an intermediate addition and progressive power lenses for general purpose use rather than bifocals or separate pairs.
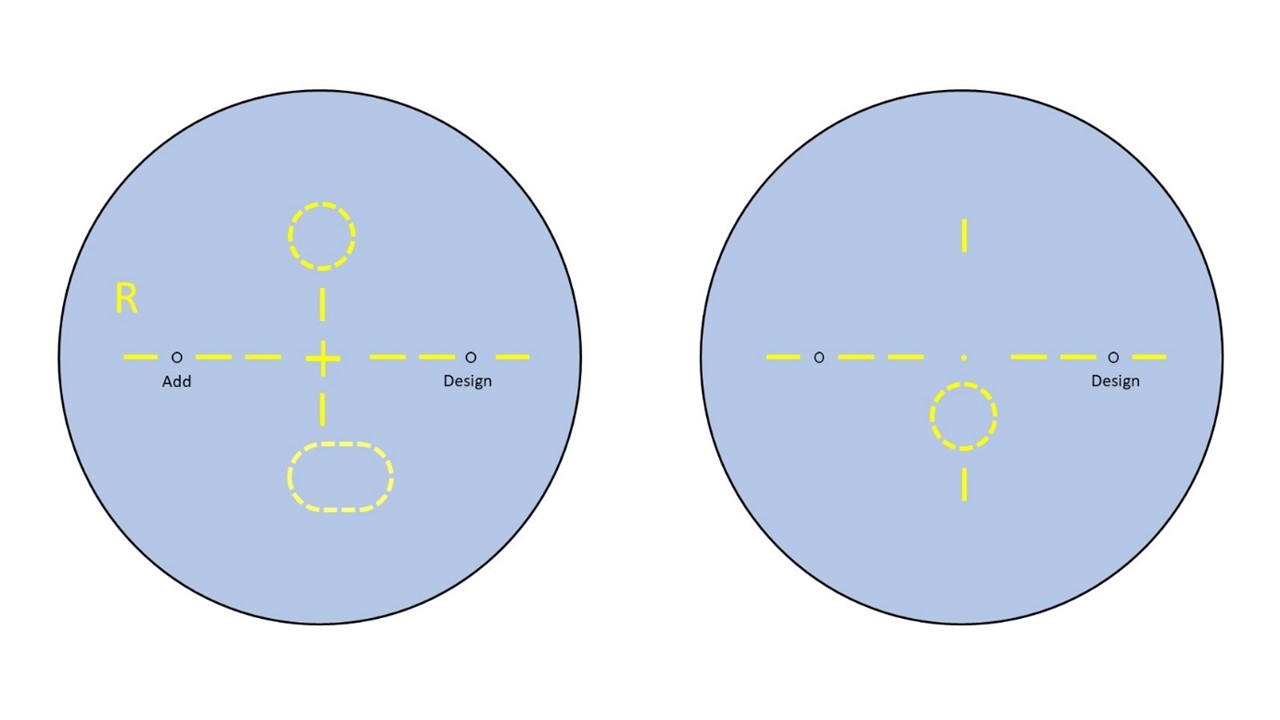
Figure 2: Asymmetric OPAL lens markings (left) compared to degressive lenses (right)
Non-tolerance to PPLs
Varifocals have become the most popular form of correction for presbyopia among patients who also require distance correction. However, they are not a panacea for all situations.
In the authors’ experience, practices report varifocal non-tolerance rates of between 0.25% and 20%. However, the latest research shows that most are due to inaccurate refraction,3 poor dispensing,4 or poor communication setting unrealistic expectations, rather than any fault on the part of the lenses themselves.
Almost all PPL lens manufacturer’s offer non-tolerance guarantees. However, most have a ‘fair usage’ policy, limiting claims to a realistic 1% of total PPLs dispensed, or utilise other interventions to manage total claims. These might include monitoring patient references and prescriptions to filter out occasions where the lenses have been reordered due to dispensing or lab error.
Genuine non-tolerance to progressive lenses is very low where the refraction and dispensing measurements are accurate and the centre of rotation condition is satisfied. However, patients with medical conditions that affect their balance or make them prone to spells of dizziness or nausea often struggle to adapt to PPLs. Emmetropic presbyopes, especially those who require a very wide intermediate zone in general use, are also significantly more likely to be non-tolerant, although this may, in part, be buyer’s remorse, given the vastly increased price relative to the ready-readers the patient is likely to have used previously.
Practitioners who are responsible for supervising many non-registered optical dispensing assistants may discover exceptionally high rates of ‘non-tolerance’ that turn out to be mainly due to dispensing error. Under these circumstances, manufacturers’ representatives are often prepared to provide dedicated staff training to improve the overall patient experience. Nevertheless, a large number of patients may be unnecessarily dissatisfied with their progressive lenses if the time is not taken to understand their visual needs based on accurate determination of the information in table 1 for each individual patient.
Anisometropia
Even a small difference in prescription between the two eyes can be a recipe for disaster with progressive power lenses, especially if the difference is in the vertical meridian. Anisometropia, inducing a vertical differential prismatic effect, is probably the major cause of genuine non-tolerance. In previous articles on binocular vision and prismatic effects,5-7 we have discussed the fact that most patients have a huge tolerance of horizontal prismatic effect, with fusional reserves of up to 20Δ base out and over 4Δ base is not uncommon. In the vertical meridian, however, tolerances are likely to be just 1Δ or less. This means that even small degrees of vertical anisometropia, ones that will not have presented a problem with a single vision lens correction and may not have presented a problem with a bifocal correction, will almost certainly cause problems with PPLs. To avoid vertical differential prismatic effects, single vision spectacle wearers can tilt their head or drop the spectacles down their nose to ensure they are looking at the optical centre and avoid vertical differential prismatic effect.
Bifocal wearers may have few ill effects from small degrees of anisometropia, especially with a judicious selection of segment drop by the dispensing optician. Take, for example, the following simple anisometropic prescription:
R. -3.00DS Add +2.00
L. -2.00DS Add +2.00
Remembering that differential prismatic effect is entirely due to the distance portion of the lens, if we place the distance optical centre at the segment top and assume the segment top position to be 6mm below pupil centre, then, when the eyes are in the primary position for distance, the patient will experience differential prism equal to 0.6Δ (base up in the right eye) for distance. When reading through the bifocal segment at a point 10mm below the primary position, 4mm below the segment top, then the patient would experience differential prismatic effect of 0.4Δ (base down in the right eye). Since both differentials are well within the 1Δ limit for vertical fusional reserves, the patient is highly likely to tolerate this without any need for resorting to slabbing off the right lens, dispensing odd-sized round segments (with the larger segment before the left eye), or some other method of compensating for differential prism.
Now, the same patient wearing PPLs will likely have a fitting cross at 4mm above the prism reference point where there should be no differential prismatic effect. The differential prism at distance will be 0.4Δ base up right eye; but now consider the near vision. In order to access the near prescription with PPLs, depending on the corridor length, the near zone is likely to be 15mm or more below the prism reference point. In this case, there would be 1.5Δ base down right eye at near, which most patients would not be able to tolerate and would complain of asthenopic symptoms, such as headaches or ‘pulling’ of their eyes, or intermittent or constant double vision. It should be borne in mind that slight diplopia may be described by a patient as blurred vision and a good diagnostic test is to ask the patient to describe their vision monocularly as well as binocularly.
Relatively similar moderate to high power cylinders at different oblique axes are a particularly potent source of non-tolerance that is almost never noticed by non-registered dispensing colleagues and rarely highlighted by optometrists as a potential source of vertical differential prismatic effect.
We have previously explored the concept of notional power,7 where FN = Fcyl sin2θ. A cylinder with an axis of 45º or 135º will contribute 50% of its power in the vertical meridian, whereas a cylinder axis of 30° or 150° contributes 75% of its power vertically, and so on.
Consider the following prescription:
R. -3.00 / -3.00 x 150 Add +2.00
L. -2.50 / -3.00 x 60 Add +2.00
This seemingly symmetrical correction hides some 2Δ or more (depending on the near vision point relative to the distance optical centre) of differential prism, base down right eye, which, if progressive lenses are required, would require slabbing off.
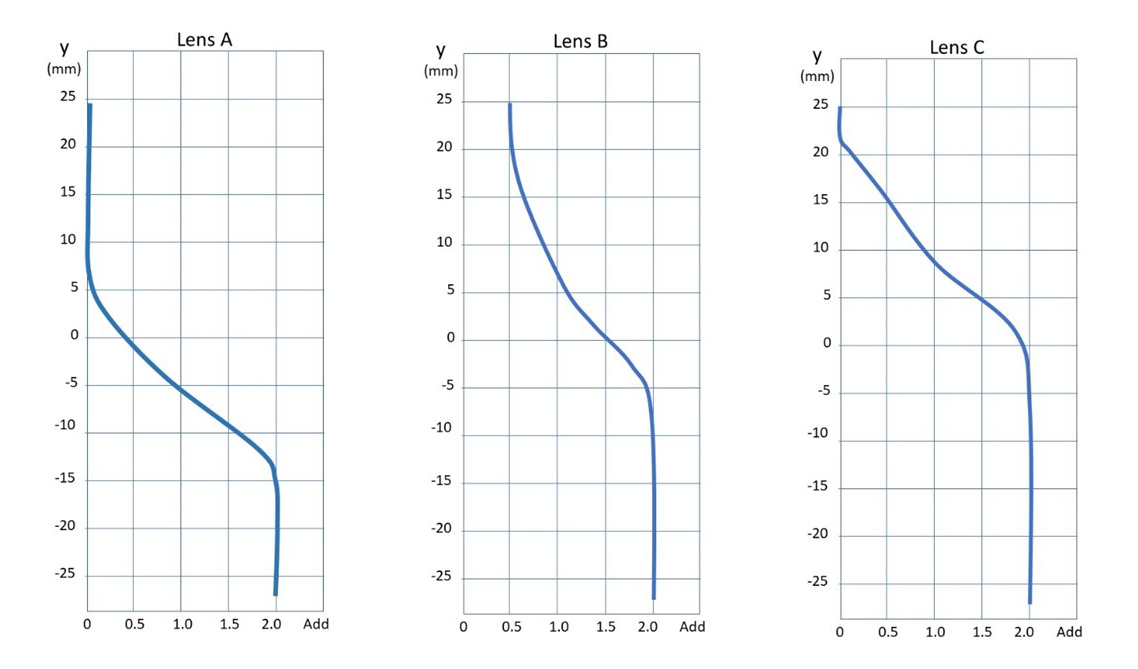
Figure 3: Power profiles for general purpose PPL and two OPALs
Limitations of PPLs
For patients with standard isometropic prescriptions, the major limitation of PPLs is the intermediate area being too small or too low for their individual circumstances and visual needs. It is important to realise that first-time presbyopes have few issues, due to the comparatively large reserve of accommodation enabling them to use the distance portion of the lens for intermediate tasks (as detailed in table 1). However, as patients reach their mid-fifties and their reading addition approaches +2.00DS, intermediate vision can be difficult. This may even be so with a lens specifically designed to provide intermediate vision over and above the vision provided by bifocals, as PPLs are. The need to raise the chin to view intermediate tasks can cause postural problems and associated neck, shoulder and back pain. Alternatively, in an attempt to see raised level digital screens clearly, PPL wearers may slouch, sliding down their chairs to facilitate a backward head tilt that allows comfortable sitting and clear intermediate vision. Look out for this in Microsoft Teams or Zoom meetings. This is less than satisfactory when intensive keyboard use is required.
Occupational single vision or bifocal lenses
A simple and highly effective solution to the problem of intermediate viewing at eye level is to dispense a pair of single vision intermediate spectacles whose far point lies just beyond the distance to the patient’s monitor. An intermediate prescription, incorporating a +1.50DS add, will allow clear vision up to its reciprocal distance 67cm away and the patient’s remaining accommodation will determine the near point. For patients in their 50s, this will probably give comfortable clear vision from 67cm to just under 50cm using comfortable levels of accommodation.
This is the principal solution to have been popularised by the Display Screen Equipment (DSE) regulations (www.hse.gov.uk/msd/dse/), despite there being several better options. It is unfortunate that the regulations stipulate that ‘employers only have to pay for glasses for DSE work if the test shows an employee needs special glasses prescribed for the distance the screen is viewed at. If an ordinary prescription is suitable, employers do not have to pay for glasses.’
In practice, the amount that employers contribute towards these spectacles means that only this basic appliance will be provided to most employees. The regulations have not kept up with available lens technology and designs or with the associated costs, despite display screens being a part of almost everybody’s working life. In fact, visual demands are arguably becoming greater with smaller laptop screens and multiple or extra-wide additional monitors becoming the norm for many workers.
A good option, often overlooked, is to dispense bifocal lenses with an intermediate correction at the top and near vision in the segment.
Occupational progressives and degressive lenses
Most advanced presbyopes will benefit from an additional pair of spectacles that provide intermediate and near vision adapted to their requirements. Broadly, the alternatives fit into two categories:
- Occupational progressive addition lenses (OPALs)
- Degressive lenses
Figure 2 shows the different styles of markings between OPALs and degressive lenses. OPALs are ordered in the same way as standard PPLs and have different designs for the right and left. Degressive lenses are ordered in the same way as single vision reading spectacles.
OPALs are manufactured using similar design principles to PPLs in that there are separate right and left designs with associated insets. They are ordered using distance mono-PDs, heights to pupil centre and the distance prescription. In some designs, the power is compensated by adding +0.50DS to the distance Rx to create a ‘room distance’ lens and correspondingly reducing the add by 0.50DS so that the near Rx remains correct. Adds are
available from 0.50 to 3.00DS or more, depending on the design.
Figure 3 shows diagrammatic representations of the power profiles for three lenses for the prescription Plano Add +2.00, for a conventional PPL (lens A) and for two OPALs. Lens A is plano from 5mm above the prism reference point (y=0) and the full near add is reached at around 13mm below. Lens B is a ‘room
distance’ occupational progressive, 0.50D at the top of the lens with a gradual increase in power almost immediately and the full near Rx reached at just over 5mm below. Lens C is an OPAL with a small DV area at the top of the lens.
Degressive lenses, also sometimes known as enhanced readers, are ordered using the near centration distance and near vision prescription and then stating the degression amount that the near Rx will be reduced by as the eye moves up towards the top of the lens.
Enhanced readers are technologically far less complex than OPALs, with right and left lenses of the same design, with no inset, and are often ordered like single vision lenses ‘on HCL’. However, this should be the facial HCL (the lower limbus) rather than the frame HCL to obtain best performance. It is important to check the different supplier fitting guidelines for their recommended heights. Common degressions are 0.75 and 1.25DS. However, depending on the manufacturer, 1.00, 1.50, 1.75 and even 2.25DS degressions are also available.
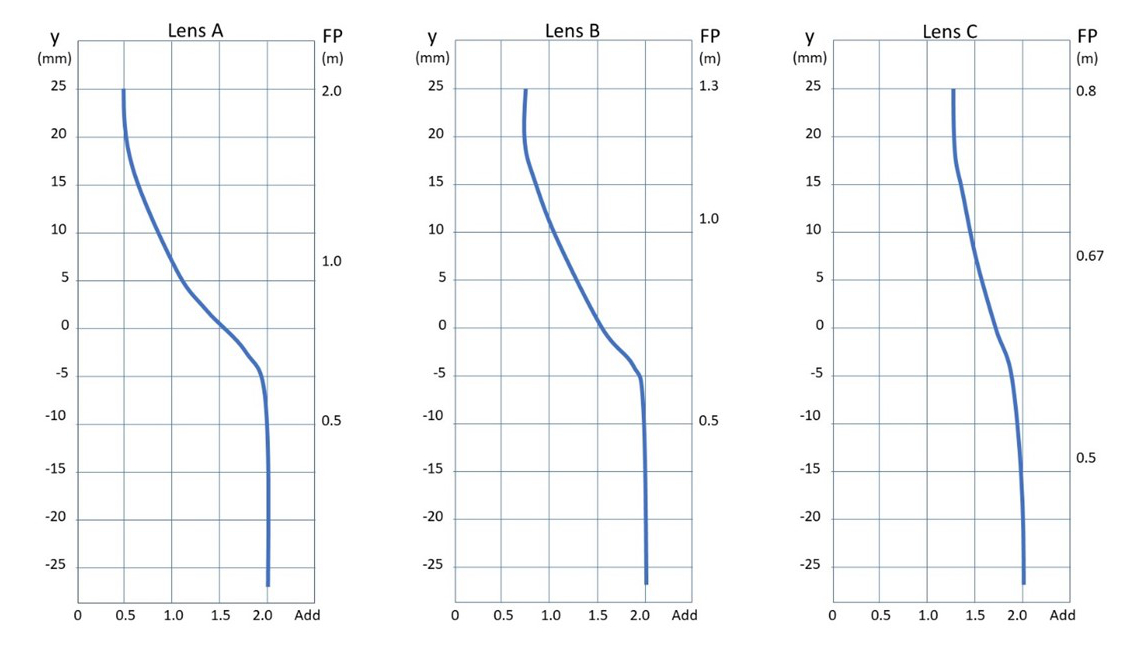
Figure 4: Power profiles for a room distance OPAL, and two degressive lenses
Figure 4 compares power profiles for a room distance OPAL (lens A, which is the same lens as lens B in figure 3) with enhanced reading lenses with 1.25DS (lens B) and 0.75DS (lens C) degressions. The y-axis represents the displacement from 0 (the optical centre or prism reference point), and the horizontal axis the add, or power assuming an emmetropic presbyope with a +2.00DS add. The righthand vertical axis shows the far point (the reciprocal of the add) at various points on the lens. Ignoring accommodation, it can be seen that the OPAL (lens A) has a range from 0.50 to 2m, lens B (1.25DS degression) is good from under 0.50m to 1.3m, and lens C (0.75DS degression) has the most limited range, from under 0.50m to 0.80m but is much better suited to using a digital screen at eye level (which approximates to 5mm above the optical centre).
Both enhanced readers and occupational progressives are dispensed not nearly as much as they should be in the UK. By routinely offering these lenses to patients who might benefit, it not only allows for valid consent to the purchase of PPLs but sets expectations of general purpose PPLs at a realistic level. Patients who find PPLs unsuited to prolonged intermediate use will return not to complain or demand a refund but to purchase the additional pair that were recommended as possibly being required at the outset.
Trifocals
A tiny minority of patients cannot tolerate progressive power lenses of any sort yet still require an intermediate correction. Although trifocals are little-used, they offer a great solution if a patient requires a single pair of spectacles for distance, intermediate and near but requires a wide intermediate zone and/or a periphery free from distortion. However, what lenses are available is constantly changing, not only because old designs are being discontinued but also because, in recent years, freeform lens technology has enabled new options to be developed to replace older designs.
In the authors’ experience, trifocal dispensing is demanding and best conducted by appointment so that sufficient time is available for accurate measurement. Key decisions for general purpose use include the intermediate portion to reading portion (IP/RP) ratio, the lens design, the depth of the intermediate portion and the fitting height of the intermediate segment.
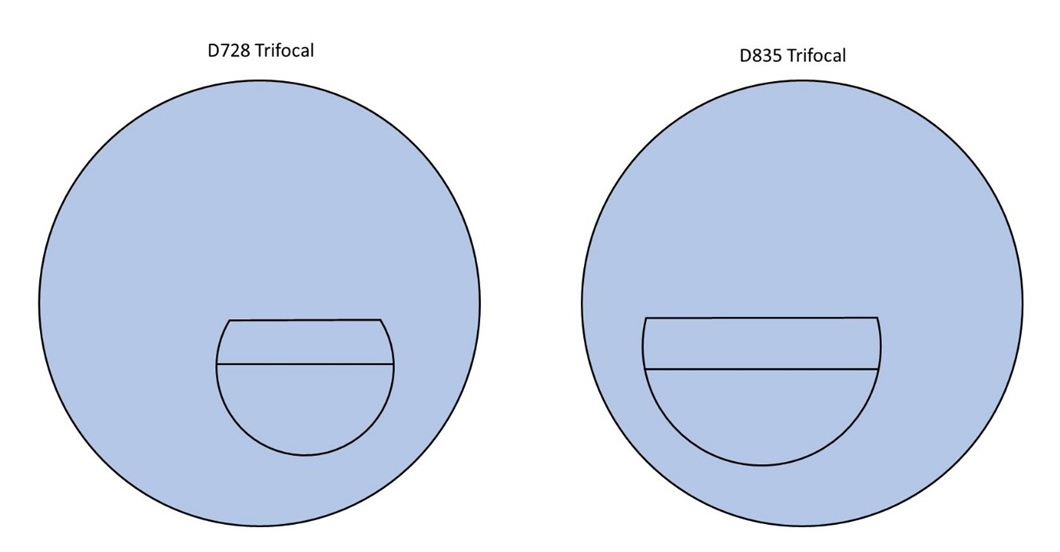
Figure 5: General purpose D segment trifocals
The IP/RP ratio is the intermediate addition divided by the near addition expressed as a percentage. General purpose trifocals, such as those shown in figure 5, are generally 50%. Sixty percent is a less common option, and 40% and 66% IP/RP ratios may also be available on one or two glass lenses.
It is important when ordering trifocals to be clear what is required. The lenses in figure 5 and the D1435 shown in figure 6 are recorded using a set format:
- D is the segment type
- The last two digits represent the segment width
- The number(s) in between indicate the intermediate segment depth
The D1435, therefore, has a 14mm deep intermediate portion and a 35mm wide D-seg. This lens is ideal for patients who predominantly require intermediate vision. Also in figure 6 is the ‘double D’ DD28, which is ideal for occupational use where the patient requires either intermediate or near vision both above and below their distance prescription. Electricians, plumbers, air conditioning engineers all have the type of occupation that benefits from this lens. It is worth noting here that there are also progressive lens options that fulfil this occupational requirement; double up and down progressives and ‘pilot’ progressives with a bifocal segment at the top.
The standard distance at the top, intermediate in the middle and near at the bottom configuration, suited to general purpose requirements, is available in E-line trifocals with 7mm, 8mm and 11mm intermediate depths. However, E-line trifocals are also available for those requiring near or intermediate vision above eye level as shown in figure 7.
Lens company Norville have long been the go-to supplier of trifocal lenses in the UK, and figures 8 and 9 show a selection of their currently available round segment lenses. The IRS invisible round segment up and down curve utilise freeform manufacturing to create another lens suited to those who need near or intermediate vision above head height. Three different styles of concentric round segment trifocals give options according to the balance required between intermediate and near.
For general purpose trifocals the default position for the top of the intermediate is 2mm above lower limbus. Up and down lenses should be fitted with the lower bifocal segment on lower limbus taking care to ensure the frame has sufficient height above to accommodate the top segment.
Figure 6: Special purpose trifocals Figure 7: Special purpose and general-purpose E-line trifocals
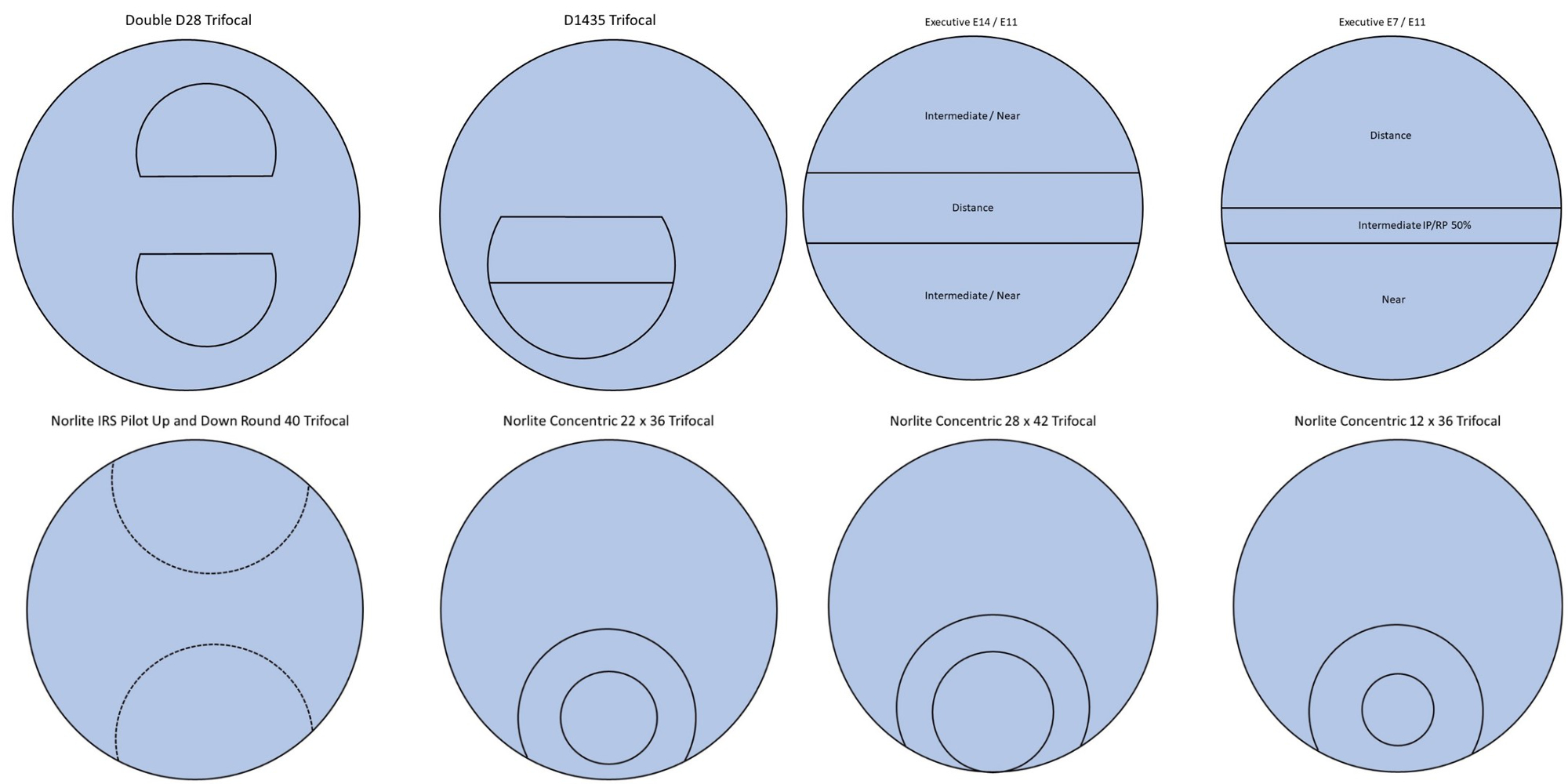
Figure 8: Special purpose and general-purpose round segment trifocals from Norville Figure 9: General-purpose concentric round segment trifocals from Norville
Conclusion
Progressive lenses offer a perfect solution to presbyopic patients in most situations, however advancing presbyopia and increasing reading additions place demands on visual requirements that often require additional or alternative solutions. Non-tolerance to PPLs can be reduced by considering anisometropia, especially ‘hidden’ differential prism due to oblique cylinders, and also in all kind of prescriptions setting expectations based on accurate understanding and communication of working distances relative to accommodation and addition, based on age-related averages where accurate data is not available. Occupational progressives and enhanced readers are an ideal accompaniment to PPLs. Trifocals are an alternative for patients who have special occupational requirements or need distortion free vision.
- Peter Black MBA FBDO FEAOO AFHEA is Course Lead for BSc (Hons) Ophthalmic Dispensing at the University of Central Lancashire, Preston, and is a practical examiner, practice assessor, exam script marker, board member and past president of the Association of British Dispensing Opticians.
- Tina Arbon Black BSc (Hons) FBDO CL is director of accredited CPD provider Orbita Black Limited, an ABDO practical examiner, practice assessor and exam script marker, and a distance learning tutor for ABDO College.
References available online at opticianonline.net.
