Many patients experience problems with their new spectacles causing them to have to return to practices in the days and weeks immediately following initial collection. Of course, often these are simply issues of physical discomfort (for example, a tight-fitting frame) or the new spectacles either slipping down the nose or being misaligned such that a simple adjustment can ameliorate discomfort and restore visual performance.
However, commercial data shows that for a significant percentage of patients purchasing new spectacles, ranging from a minimum of around 1% or 2% to over 20% in a small minority of practices, dissatisfaction with the new spectacles is sufficient that the patient either requires a new pair of spectacles to be dispensed or demands a refund of the money they have paid. Many of these patients will also have had a second sight test before the spectacles are remade or refunded, yet in almost all cases this test is unnecessary.
In busy practices, unnecessary retests take the place of other consultations that would otherwise have resulted in income for the practice in the form of sight test fees and prescribed optical appliances. The authors estimate this to cost the UK optical sector around £40 million (around 1% of total sales) based on unnecessary retests contributing 2% of appointments and lost sales (assuming a typical average sales values and a conversion rate of 50%). In reality, the true cost is much higher once reputational damage to individuals, their employers and the sector as a whole is taken into account. Additionally, with sustainability and environmental concerns increasingly high on the agenda, unnecessary waste is seen by many as unforgivable in the light of climate change and micro-plastic pollution.
Given that most retests are unnecessary, it follows that patient dissatisfaction most often occurs as a result of poor dispensing, and commercial analysis of remakes and refunds shows that the overwhelming majority of patients who are dissatisfied with their spectacles are presbyopic and almost all of those are progressive lens wearers.
Setting Expectations
There is no doubt that part of the issue is poorly set expectations, especially in relation to supposedly ‘upgraded’ progressive power lenses. As part of gaining valid consent from a patient, it is not unusual to give an informed choice of three different options; ‘good, better, best.’ However, many people who dispense spectacles, especially those without formal higher education in ophthalmic dispensing, fail to realise that, for a ‘better’ lens to give improved visual performance, all other factors must remain equal.
A common way practices fall foul of this is when offering special deals on prescription sunglasses, such as free second pairs subject to a certain level of initial purchase. This kind of special offer often results in a premium quality progressive lens being dispensed for the everyday spectacles and a more basic lens for the sunglasses. Despite identical prescription and centration details, and quite often identical frames, a reduced intermediate and reading area and different levels of aberrational astigmatism are a certain recipe for dissatisfaction if a warning of relatively poor adaptation and/or visual performance has not been made at the time of dispensing.
It is relatively rare when patients choose new spectacles with progressive power lenses for all aspects of the prescription, centration and frame fit to remain the same, and many changes can have a detrimental effect on visual performance.
For example, in a high proportion of cases a presbyopic patient will require new spectacles because of an increased reading addition. This one change alone will cause an increase in both the level and extent of peripheral aberrational astigmatism with the result that the usable intermediate and reading areas will be reduced in a given lens design even if all other lens parameters remain the same. Effectively, as the add increases, a given lens design will become more ‘hard’ resulting in narrower visual zones and potentially more difficult wearing and adaptation characteristics. This makes it important to offer a higher quality alternative with the explanation that as the add increases the reading area will narrow and the only way to maintain reading width is to select a higher quality lens.
Setting expectations of a maintained or wider reading area is a common cause of complaint when expectations are not realised. This may be due to an increase in aberrational astigmatism, caused for example by an increase in actual prescribed cylinder, or it may be due to a change in fitting characteristics.
Vertex Distance
Although the Opticians Act and the associated GOC regulations (1984 Rule of Council on Sale and Supply of Optical Appliances) effectively make it a legal requirement in the UK to take British Standard 2738 relating to back vertex distance (BVD) into account, this only applies to prescriptions over +/-5.00DS in the highest principal meridian including the reading addition. Regardless of the Standard, all manufacturers’ fitting guidelines instruct practitioners to always take BVD into account whenever dispensing progressive power lenses regardless of the level of the refractive error. Personalised progressives are manufactured with compensated powers even in low powers. However, BVD is a critical factor to take into account even with non-personalised varifocals, and is perhaps the biggest cause of patient dissatisfaction (figure 1).
Patients who have paid to upgrade to a lens with a wider reading area are frequently disappointed if the frame selected fits with a larger BVD than their habitual spectacles. The corridor of a PPL can be considered like a keyhole, and obviously the closer the eye is to a keyhole the wider the field of view. Hence, if the frame vertex distance is increased in the new spectacles compared to the existing ones, then any gain in corridor width from a better quality design is potentially completely negated, despite what has been promised from the improved design, by the eye being further from the ‘keyhole’.
It really cannot be emphasised enough that spectacles should always be fitted as close to the eyes as possible regardless of power to maximise field of view especially with multifocal lenses.
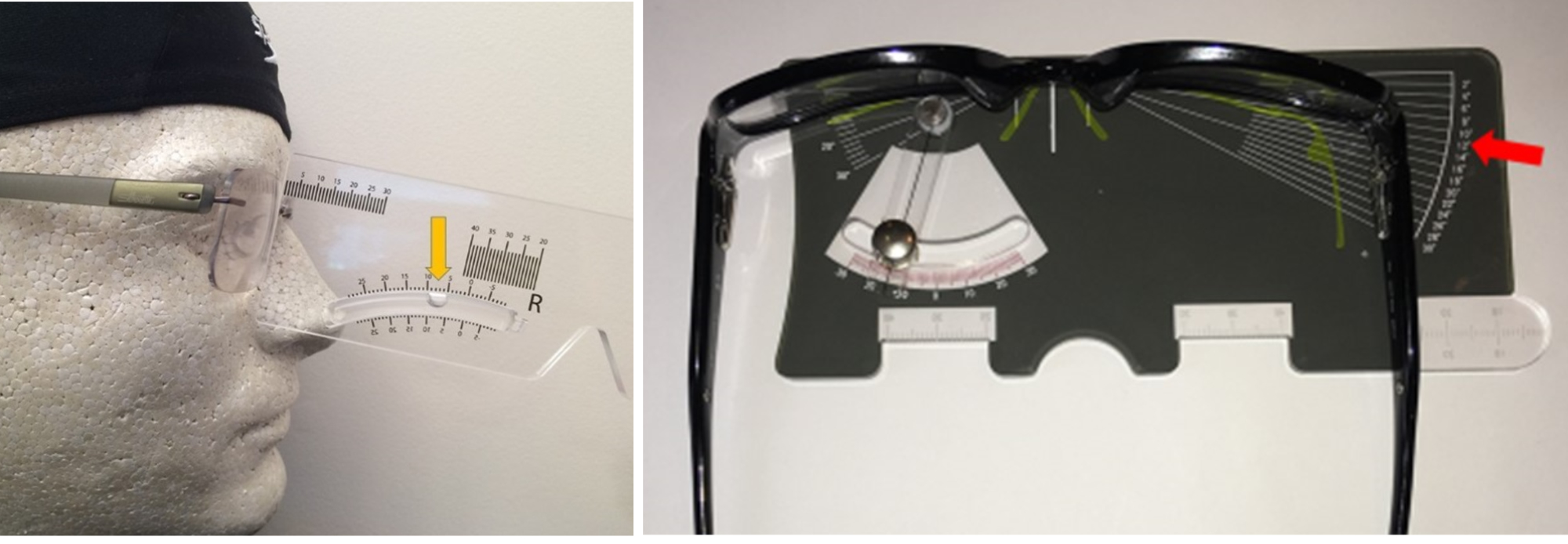
Figure 1: Manufacturers’ fitting guidelines instruct practitioners to always take BVD into account whenever dispensing progressive power lenses

Refractive Index and Abbe Number
Another area where there is potential to overpromise and under-deliver is in regards to lens material. Moderate and high prescriptions will always result in thinner lenses, all things being equal, if the refractive index of the lens is increased, however often the promised saving is often negated by a larger frame requiring more decentration and a larger uncut diameter. With high index and mid-index lenses any saving in thickness and weight comes at a cost of chromatic aberration as a result of reduced Abbe number. Transverse chromatic aberration is much more of a problem in progressive lenses, compared to single vision, due to the absolute necessity to use portions of the lens towards the lens periphery for near vision. Chromatic aberration is likely to cause problems even in quite low powers, once the additional prismatic effect due to the reading addition and the increased decentration due to corridor length are taken into account.
Pantoscopic Angle and Wrap
Lens manufacturers optimise their non-personalised progressive lenses for average values of pantoscopic tilt and face-form angle (wrap). Therefore, if a patient has worn lenses oriented according to the manufacturer’s fitting guidelines previously, and has now selected a frame that does not fit optimally in this regard, they are likely to experience compromised visual performance in each area of the lens yet again due to increased aberrational astigmatism. It is important to know the fitting parameters for your favoured brand as they all vary slightly. However, as a guide, pantoscopic tilt (figure 2) outside of the range 7 to 12 degrees, and wrap (figure 3) outside the range of 0-10 degrees are likely to cause a reduction in visual performance.
(Left to right) Figure 2 & 3: Measuring pantoscopic angle; measuring face-form angle, or wrap
It is important to select frames that fall within these parameters, and also ensure that these vital parameters can be adjusted as they may be affected by the glazing process, especially if the base curve has not been matched exactly to that of the frame/dummy lens. If the patient’s facial characteristics, or frame choice, mean the frame does not fall within recommended parameters then the patient must be informed that they should either select another frame, or opt for a personalised progressive lens to ensure visual expectations will be met.
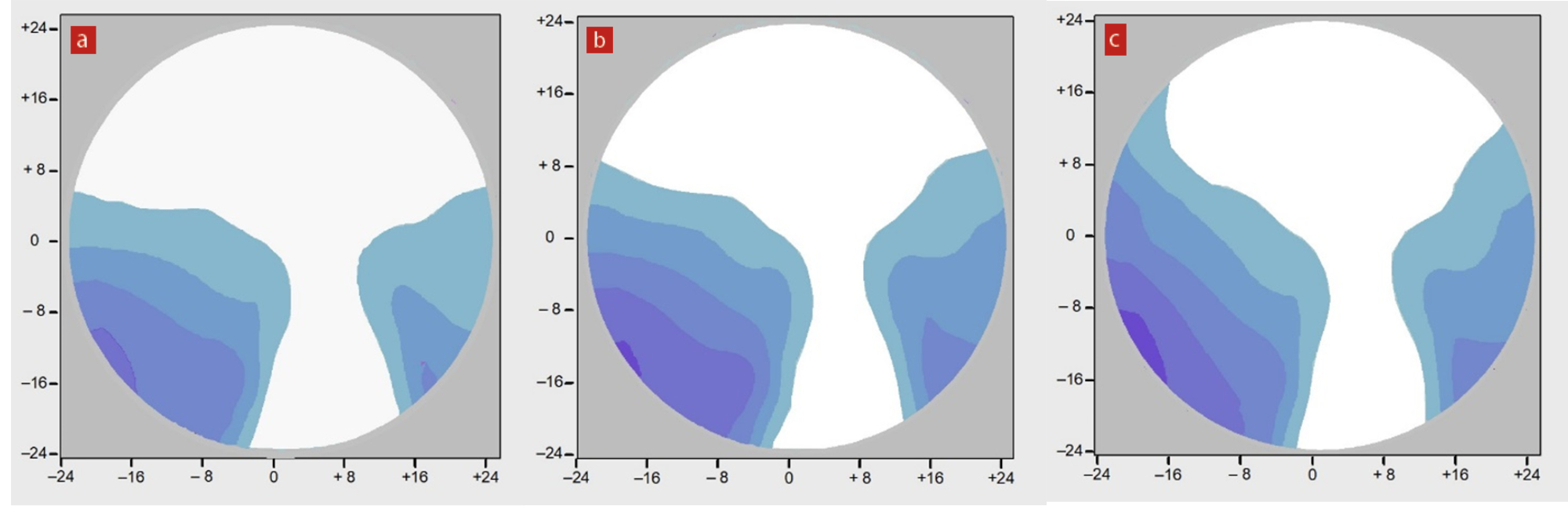
Patients with significant astigmatism, over ~0.75DC, especially if oblique, and patients with non-average characteristics such as narrow or wide inter-pupillary distance or prescribed prism will all achieve improved vision from personalised progressives (see figure 4). It is therefore also essential that practitioners can identify previous lenses from their markings to ensure patients who have previously worn individualised lenses are not unwittingly downgraded. Even the highest quality non-personalised PPL cannot compare to the performance of a personalised progressive.
Figure 4: Isocylinder plots for progressive power lenses at different pantoscopic angles. In all the following lenses the BVD is optimised at 9mm. (a) +5.00DS Add +2.00, Panto 9 degrees. (b) +5.00DS Add +2.00, Panto 3 degrees. (c) RE +3.00 / +2.00 x 90 Add +2.00, Panto 9 degrees. (d) RE +3.00 / +2.00 x 90 Add +2.00 Panto 3 degrees. (e) RE +3.00 / +2.00 x 90 Add +2.00 Panto 3 degrees; personalised progressive. Note the improved characteristics of the personalised progressive lens
Reading Spectacles
As a slight aside pantoscopic tilt and wrap are also significant causes of complaint with single vision spectacles used for near vision only by presbyopes. Vertical centration should be determined in the same way as for distance spectacles – heights to pupil centre in the primary position, dropped by 1mm for every 2 degrees of tilt so that the visual axis coincides with the optical axis of the lens. Horizontally however, since the near centration is inset from the primary position, highly wrapped frames should be avoided in favour of frames with little or no dihedral (face-form) angle. Occasionally it is necessary to apply a negative dihedral (anhedral) angle to ensure visual performance, however this is not usually cosmetically ideal with most frames unless the frame has been designed with near vision in mind as in the case of half-eyes.
Anisometropia
A difference in refractive error between the two eyes is a frequent cause of difficulty in presbyopic patients wearing bifocal, progressive or occupational lenses. Principally this is because anisometropia is not recognised as a problem either by the optometrist/ophthalmologist or dispensing optician/assistant. Anisometropia is also becoming increasingly common as ophthalmologists become obsessed with leaving patients without an Rx following cataract surgery. There seems to be no thought of the visual consequences of leaving the first eye plano when the second eye remains with significant refractive error, often for many years, rendering standard multifocal correction impossible due to the differential prismatic effects involved causing vertical diplopia at near.
Anisometropia may cause problems with aniseikonia (different retinal image sizes) however this is much less of a problem than is often thought. It is easy to see that if two eyes are axially myopic, a more myopic eye will have a longer axial length and therefore, given the reduced eye surface is a standard power, will produce a larger uncorrected retinal image. What is less understood is that since the more myopic eye requires a higher power lens that produces more minification overall the corrected retinal image size is reduced such that most patients do not experience aniseikonia.
Differential prismatic effects, however, are a significant issue for anisometropic patients and occur in all directions of gaze away from the (correctly positioned) optical centres. Differential prismatic effects cause misalignment of the visual axes and therefore diplopia, however this is so repugnant to the brain that it will work hard to alleviate the double vision. It should be remembered that the eyes can easily converge by very large amounts and so up to 20∆ of base out prism can be overcome in order to maintain binocular single vision, though comfortable tolerable levels, although significant will be much less. Divergence reserves are less substantial but are still of the order of 4∆ base in. Vertically, however, there is very little tolerance of differential prismatic effect, with any amount over 1∆ unlikely to be tolerated and therefore cause vertical diplopia. If the brain cannot induce the extraocular muscles to align the eyes and create binocular single vision, then the brain will typically ignore the image from one eye to restore a single image. So called suppression avoids the confusion of diplopia, but if it happens in the critical period of visual development in early childhood will lead to the visual pathway from the eye with the lower vision failing to develop – so called amblyopia.
Amblyopic presbyopes are often dispensed progressive lenses with the amblyopic eye requiring a balance lens and there is often a temptation to dispense a single vision balance lens. This in itself induces vertical differential prismatic effect, even if the patient is not anisometropic, because the PPL will incorporate prism thinning and the balance lens will not. It is therefore better in most cases to dispense a PPL as a balance lens if the patient’s visual acuities are within a few lines of each other and binocular stereoscopic vision is still in evidence.
PPL Case Study
A first time PPL wearer, aged 47, is dispensed a high-quality freeform PPL in a conventional (ie not personalised) design, back surface progressive, with a corridor length of 14mm and fitting height of 24mm.
R. +5.75 / -3.00 x 60 (6/5)
L. +5.25 / -2.50 x 135 (6/5)
Add +1.25 (N5).
On collection distance visual acuity is 6/5 binocularly. Near N5. Px returns after two weeks complaining that their eyes feel tired, especially after reading for long periods, and the vision with each eye monocularly for near is better than the vision with both eyes together when reading.
Possible solutions
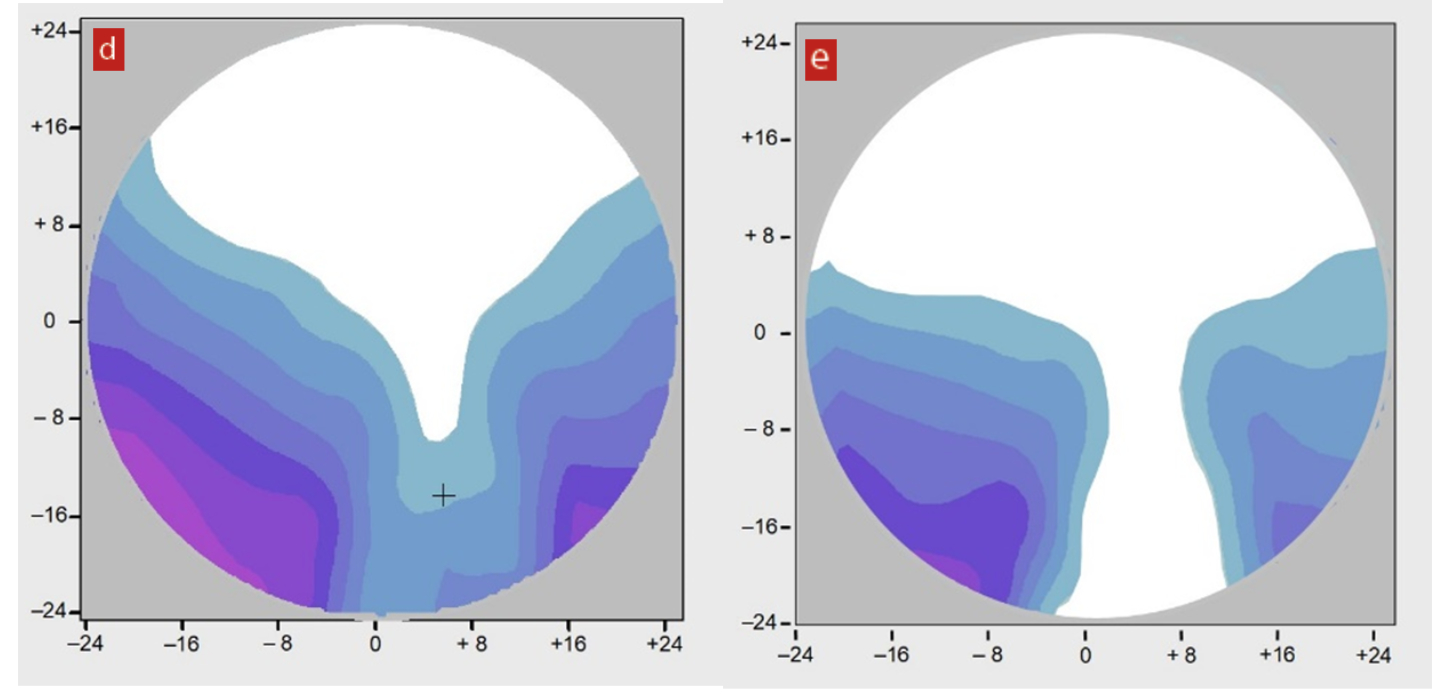
Assuming the spectacles were manufactured correctly and verified before collection then this could simply be a case of the frame needing realigning. If the frame is not sitting straight and say one fitting cross is now above pupil centre and the other below, then when looking down to read one eye might be looking through the full reading Rx and the other through an intermediate prescription. When viewed monocularly the correct head position can be assumed to see perfectly with each eye separately, however when using both eyes together this is not possible, and the patient will experience a blurred image and a clear image superimposed on top of each other, which the brain perceives as a blurred image as shown in image 9 in figure 5.
Figure 5: Articulating diplopia. In these diagrams, the red corresponds to the right eye view
It is likely, however, that the issue is more complex. Transposing the Rx makes it easier to visualise:
R. +2.75 / +3.00 x 150 Add +1.25
L. +2.75 / +2.50 x 45 Add +1.25
The spheres are the same, however the cylinders are of different powers and at differing levels of obliqueness. It is necessary to determine the notional power of the cylinders in the vertical meridian and then determine whether there is any significant differential prismatic effect.
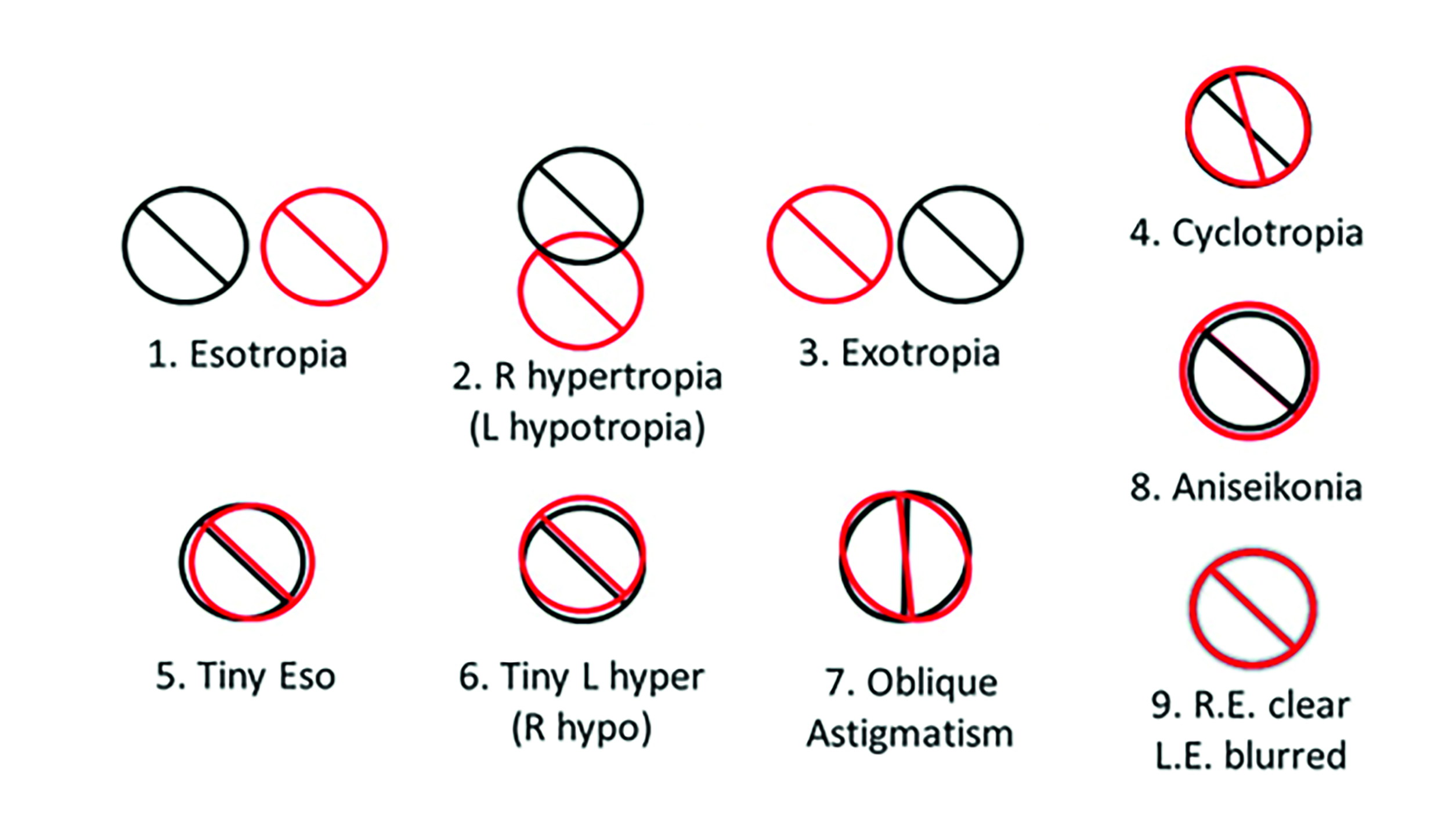
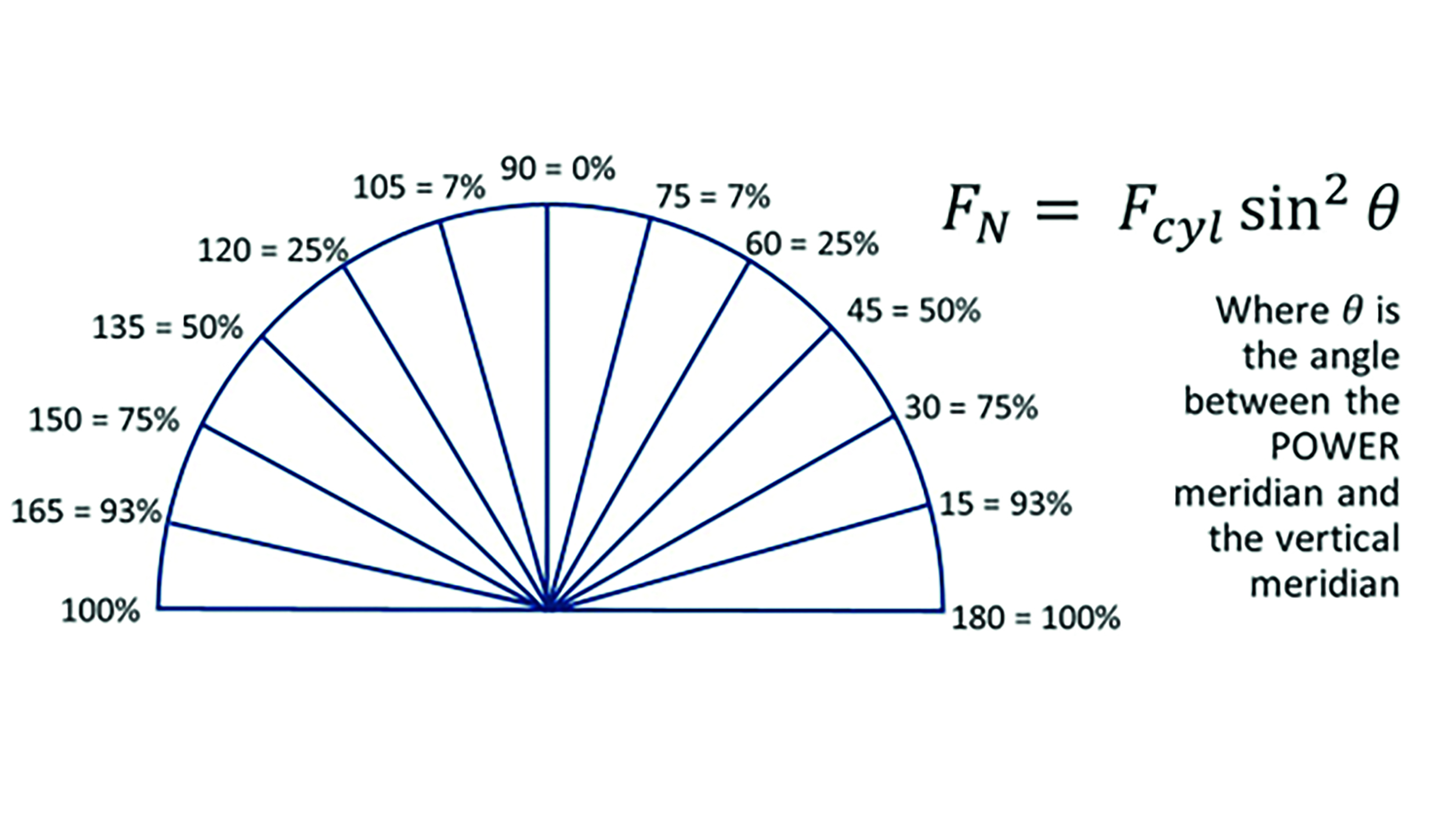
As shown in figure 6, the power meridian of the RE is 30 degrees from the vertical so it contributes three-quarters of the cylinder power in the vertical meridian +2.25D. The LE contributes half of the cylinder power in the vertical meridian, or +1.25D. There is a difference in the vertical meridian of +1.00D and this is likely to be the source of the blurred vision and eyestrain when reading.
With a corridor length of 14mm the patient will likely be using an area of the lens 15mm or more below the distance optical centre for near work. Hence there will be vertical differential prismatic effect at near of 1.5∆ or more, base up in the right eye. This being equivalent to 1.5∆, base down in the left eye, then the appropriate solution would be to slab off the left lens, removing 1.5∆ base down from the bottom half of the left lens. An alternative would be to use a semi-finished reverse slab-on lens for the right eye.
While significant diplopia is easy for patients to describe as ‘seeing double’, as indicated by illustrations 1, 2 and 3 in figure 5, small amounts of diplopia, where the two images are substantially overlapped, patients may not be able to articulate this as double vision as the visual effect is likely to be perceived as blurred vision by the patient. Images 4-9 in the figure illustrate some possible causes of slight diplopia that are likely to be described by the patient as blurriness. In this case, the vertical differential prismatic effect is above the generally accepted tolerance threshold of 1.0∆ and is likely to cause a break-down of binocular single vision some or all of the time equivalent to image 6 in figure 5.
Figure 6: Percentage power in the vertical meridian depending on vertical axis
Conclusions
Practices often have unacceptably high rates of dissatisfaction with progressive power lenses that are costly in both financial and reputational terms and could be reduced greatly by taking some simple steps to improve the quality of ophthalmic dispensing. These include following the manufacturers fitting guidance with regards to centration and always measuring pantoscopic angle and wrap to ensure they are within the recommended parameters. Where this is not possible or the patient requires a frame with non-standard tilt or wrap, then it is necessary to dispense a personalised progressive that can accommodate parameters outside the standard range.
Finally, practitioners should be vigilant for levels of anisometropia of 1.00D or more in the vertical meridian, especially where it is ‘hidden’ by subtle combinations of oblique cylinders, and particularly where the anisometropia has been recently induced by prescription changes including those induced following refractive surgery. Commercial data shows that retest rates in most practices with skilled staff are typically a little over 1%, and total dispensing errors that require remakes and refunds should be no more than 2-3% in practices with skilled dispensing practitioners. How does your practice compare?
- Peter Black MBA FBDO FEAOO AFHEA is Course Lead for BSc (Hons) Ophthalmic Dispensing at the University of Central Lancashire, Preston, and is a practical examiner, practice assessor, exam script marker, board member and past president of the Association of British Dispensing Opticians.
- Tina Arbon Black BSc (Hons) FBDO CL is director of accredited CPD provider Orbita Black Limited, an ABDO practical examiner, practice assessor and exam script marker, and a distance learning tutor for ABDO College.
