Clearly a ‘lifetime of contact lens (CL) wear’ is not intended to fully stretch from ‘cradle to grave’, but with modern CL materials and optical designs, it arguably covers a greater portion of that timespan than ever before. A patient who starts CL wear early in life with myopia management and continues through until they have reached advanced presbyopia could easily be wearing lenses for 50 years or more. However, it is well understood that when lens performance falls short, it can result in patients dropping out.1 So, what does it take to achieve many years of successful CL wear and how can the eye care professional (ECP) ensure they make the best use of available lens technology to meet the ever changing needs of wearers throughout their lives?
For committed CL wearers, the concept of wearing lenses over many years is not new, in fact the three authors of this article have a (somewhat frightening) combined experience of 110 years of successful CL wear, using a total of 26 different types of lenses over that time. Those lenses have included changes in the materials worn (including rigid to soft and hydrogel to silicone hydrogel), changes in replacement frequency (from unplanned replacement through to daily disposable) and updates to the vision correction required (from spherical to toric and, most recently, to monovision and multifocals).
This experience perfectly illustrates what long term CL wear entails; optimisation of the lens prescribed as both technology improves, and lifestyle and visual needs evolve. This is a key point to bear in mind when dealing with patients; a lifetime of CL wear is a dynamic rather than a static experience. There should be a broad acceptance of the fact that the patient will never remain in the first lens prescribed, but rather an expectation set by the ECP with their patient that the wearer is on a continual journey.
This article examines the considerations for soft CLs at various stages of a patient’s life and how to apply evidence-based fitting and practice to increase the chances of successful long term wear over many years.
Options Through the Ages
The early years
Outside of the need for medically necessary paediatric fitting, reports suggest that many ECPs feel the earliest children should be fit with CLs are in the early teen years,2,3 and to some extent this belief remains embedded with contemporary lenses, with ECPs in many areas of the world still only being comfortable fitting soft lenses to patients over 10 years of age.4 However, a child’s maturity, motivation, hygiene and parental support should all be more important factors than age when it comes to decisions about prescribing CLs.3
An interesting gap in the age at which children are deemed suitable for CLs was highlighted in a survey of 400 ECPs and 1,000 parents in six countries, with ECPs fitting from an average age of 9.1 years, but parents feeling comfortable with CL wear for their child at an average age of 11.7 years.5,6 This highlights a need to educate and support parents in their understanding when discussing options for their child. The comfort level of ECPs and parents to fit children at a much younger age with both rigid overnight orthokeratology and soft lenses with specific optical designs is particularly relevant given the proven capability of both options to slow the progression of myopia in pre-teens.7-11 Recent studies have demonstrated that lenses fit to this age group, including up to six years of hydrogel daily disposable wear, were successful, with minimal impact on ocular physiology.7,12-16
The teen years
In addition to the clinical need to offer myopia management, the value of fitting children (especially teenagers) with CLs has been clearly demonstrated. CL wear substantially improves quality of life scores for how both children and teens feel about their appearance and participation in activities, especially sports. They are more willing to try new activities, are more self-confident and exhibit greater satisfaction with their refractive correction.2,17-23 Previous studies have shown that children aged 11 to 14 are perfectly capable of following instructions to look after and care for their CLs and appear no less compliant with instructions than adults.16,24 The improvement in quality of life with CL wear and their levels of safety indicates that children can be routinely offered CLs as their main method of refractive error correction.
The ‘adult’ years
The years between secondary school and presbyopia are historically those years considered the prime ones to wear CLs. It is interesting to note that in a recent summary of 20 years of fit data from a global fitting survey, the average age of lens wearers was 30.8 ± 13.9 years for males and 32.5 ± 14.3 years for females,25 possibly suggesting that this is the age at which many people seek alternatives to their traditional spectacle vision correction and have the disposable income to be able to more easily afford this. It is during this period that probably the widest variety of lens materials, frequency of replacement and refractive correction options exist. So, where does the ECP begin with choosing the most appropriate design, lens material, frequency of replacement and where required, lens care product?
Some important initial considerations relate to cost, convenience and days per week of wear.26 A new young adult wearer who only wishes to wear lenses one to two days per week for sport or social events will likely opt for a daily disposable option, that will be convenient and inexpensive. A wearer who wants lenses to wear seven days per week along with seeking a convenient and easy regimen may also wish to opt for a daily disposable, but this will not be the case for all wearers, with many still finding great value and vision correction options with frequently replaced lenses. There is a wide choice of materials within the categories of frequently replaced and daily disposable. These broadly break down into hydrogel and silicone hydrogel materials, often with a range of options available, positioned from ‘entry level’ to ‘premium’ products, that offer different features and benefits that might best compliment the wearer’s lifestyle and needs.
Increasingly, the impact a product has on the environment in terms of its manufacture and ability to be recycled plays a role in the decision-making process for some patients. While daily disposable lenses logically appear to have more packaging and more frequent disposal than two-week or monthly lenses, once recycling schemes and lens care products are taken into account, the overall amount of waste from both replacement frequencies is low compared to overall household waste. They contribute just 0.20-0.26% of normal household waste per person per year in the UK, with full time wear of daily disposables generating 27% more waste than frequently replaced lens wear,27 and equivalent waste between replacement frequencies possible with part time wear of daily disposable CLs.
The 25 years or so between secondary school school and presbyopia is likely the time when most opportunities to change lens type to maximise comfort, optimise vision and help prevent drop-out occur. During this period, the most appropriate lens for the patient may change over time. This may mean a simple move from an initial economic option of a frequently replaced lens to the convenience of daily disposables. Comfort performance is important to optimise, especially given the potential for increased visual demands, use of digital devices, exposure to drying environments and long hours of wear that modern life often entails. Systemic health changes along with pregnancy may also impact CL comfort. As time passes, the wearer may notice their lenses are not as comfortable at the end of the day as they would like, presenting the opportunity for the ECP to recommend an alternative option, perhaps a more premium lens or newer technology or move to daily disposable if not already there.
What is important to recognise is that changes to comfort performance can be subtle, with a wearer not realising other options exist. Detailed questioning about the gap between total and comfortable wearing time helps to uncover suboptimal performance in this area.28 Ensuring vision is optimised is important too. Care should be taken to ensure an accurate over-refraction is performed using ±0.25D steps for all wearers at every CL check-up. Assessment of vision clarity and comfort with digital devices is also important to check, with some CL designs available designed to help alleviate the tiredness and dryness associated with digital eye strain. Patients benefit from having even low levels of astigmatism fully corrected with toric rather than spherical lenses,29,30 and with modern toric lenses as quick and easy to fit as spherical designs.31,32 The opportunity should always be taken to recommend toric lenses to patients with a little as 0.75D of astigmatism. A wide range of prescriptions are available in soft toric lenses for both daily disposable and frequently replaced lenses, with toric designs that provide clear and stable vision. Visual performance is correlated with comfort, with higher comfort scores associated with better vision,33 a fact that provides even more reasons to optimise vision for every CL wearer.
Lens performance and lifestyle demands need frequent discussion with the patient at every aftercare check. Every progress check is an opportunity to check in with the patient and confirm that the lenses the patient is currently wearing are performing at the highest level and providing the comfort, vision and convenience that satisfies the patient. Offering the latest technology for a patient to try often elicits a response from the patient along the lines of: ‘I didn’t actually know that my lens comfort was not as good as it could be without trying that new lens; now I know what good comfort really means.’
The later years
Between 2015 and 2050, the proportion of the world’s population over 60 years will nearly double, from 12% to 22%.34 Today’s presbyopes are more active than ever,35 and want to feel young and not be limited by their presbyopia. However, presbyopia brings with it many challenges for the CL wearer. While monovision may present an easier route to fitting, when wearers have experienced both this and multifocal CL correction, the latter is preferred.36
Historically, ECPs tended to steer away from fitting multifocal CLs as they were time consuming to fit and often the visual performance was lacking. However, modern multifocal soft CLs are easy to fit, with achievable high fit success rates when following the manufacturer’s fit guide for each lens design and provide excellent quality of vision.37-40 Accurate refraction of the presbyope is important in achieving that success, along with careful assessment of ocular dominance and optimisation of the CL prescription as required. Soft multifocal CLs are available in a wide variety of materials and frequency of replacement options, including daily disposable silicone hydrogels with frequently replaced toric multifocal correction available for astigmatic presbyopes too.
One important point to consider when fitting modern multifocal lenses are the significant number of studies that have demonstrated the most appropriate predictors of success include getting patients to undertake more ‘real-life’ tasks, such as reading a smartphone or using the lenses in their natural environment, rather than merely determining near and distance high contrast visual acuity in the consulting room at the fitting appointment.41-45 Visual performance metrics appear far better than visual acuity measures at predicting success and allowing the patient to use the lenses at home for several days will likely provide higher fit success than prescribing on visual acuity measures alone.
It seems clear that this improvement in the performance of multifocal lenses is being gradually acknowledged by ECPs, with the latest global fitting survey showing that 49% of presbyopes were fit with multifocal lenses, as compared with only 11% being fit with monovision.46 This compares with 41% and 12% respectively a decade ago.47
Fitting Trends
Given the considerations outlined above for CL recommendation throughout a patient’s life, what are ECPs actually fitting to today’s wearers and does it follow evidence-based practice as highlighted in the CLEAR report?48 It is interesting to consider that reusable disposable lenses were launched in 1986, the first hydrogel daily disposable lenses commercialised in 1995, the first silicone hydrogels in 1999 and the first daily disposable silicone hydrogels in 2008. Thus, in just over a 20-year period the landscape of available materials and modalities for ECPs changed enormously. Many tend to think that silicone hydrogel daily disposables are ‘new’, but they have been available for well over a decade and have a plethora of data on their use.54,60-65
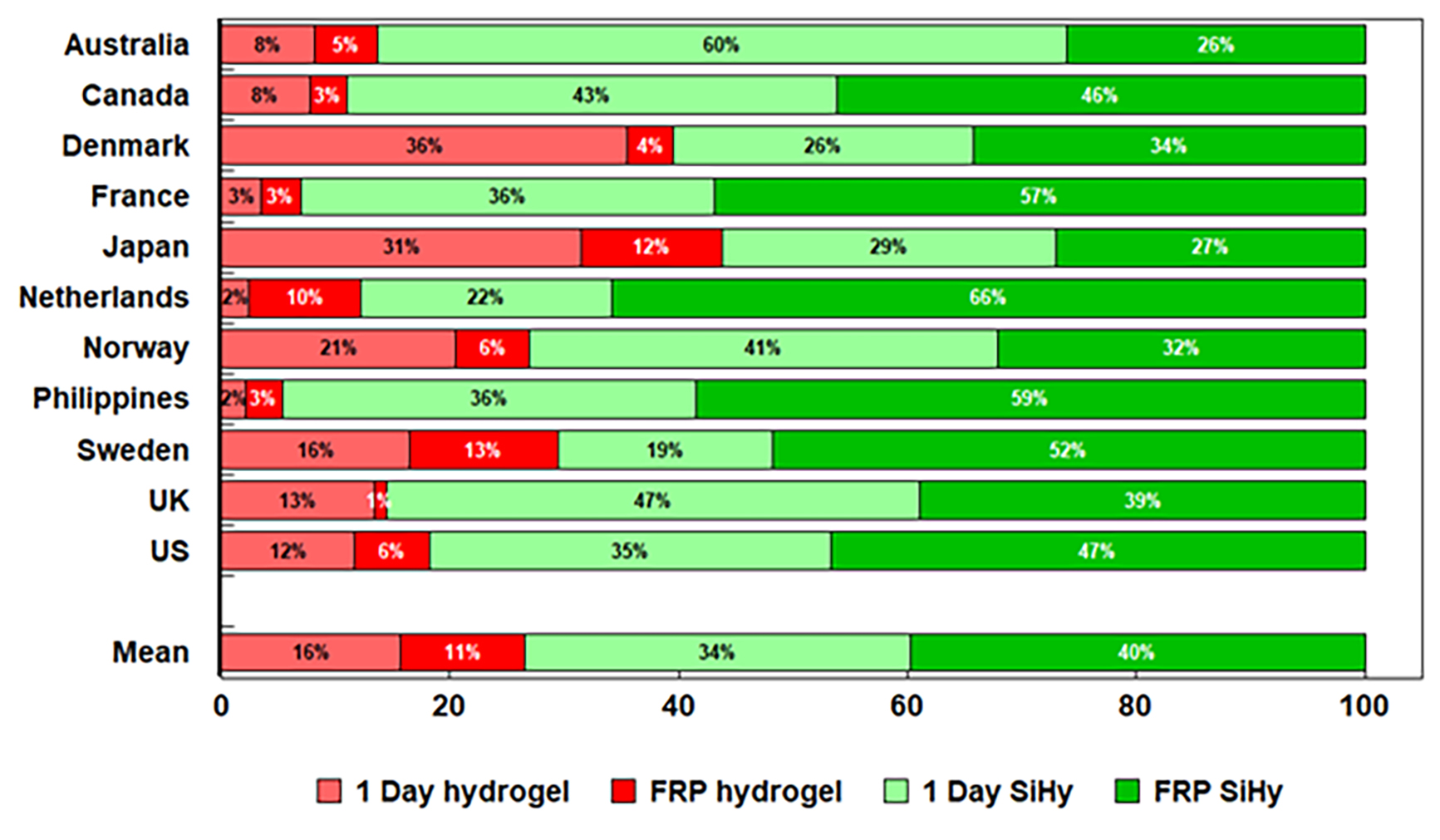
A snapshot of how this evolution in soft lens technology has impacted clinical practice can be found in the International CL Prescribing Report that is published annually,46 with the data from 20 years recently summarised in a new publication.25 Over the 28 countries surveyed and >14,000 fits reported in 2021, rigid lenses accounted for an average of 11% of all fits, with rigid orthokeratology accounting for a further 3%. Further analysis of the data provides some interesting trends for soft lens fits. Figure 1 provides data for 11 countries by frequency of soft lens replacement and figure 2 the relative proportions of reusable and daily disposable soft fits, broken down by hydrogel or silicone hydrogel material.
Figure 1: Soft lens replacement frequency, 202146
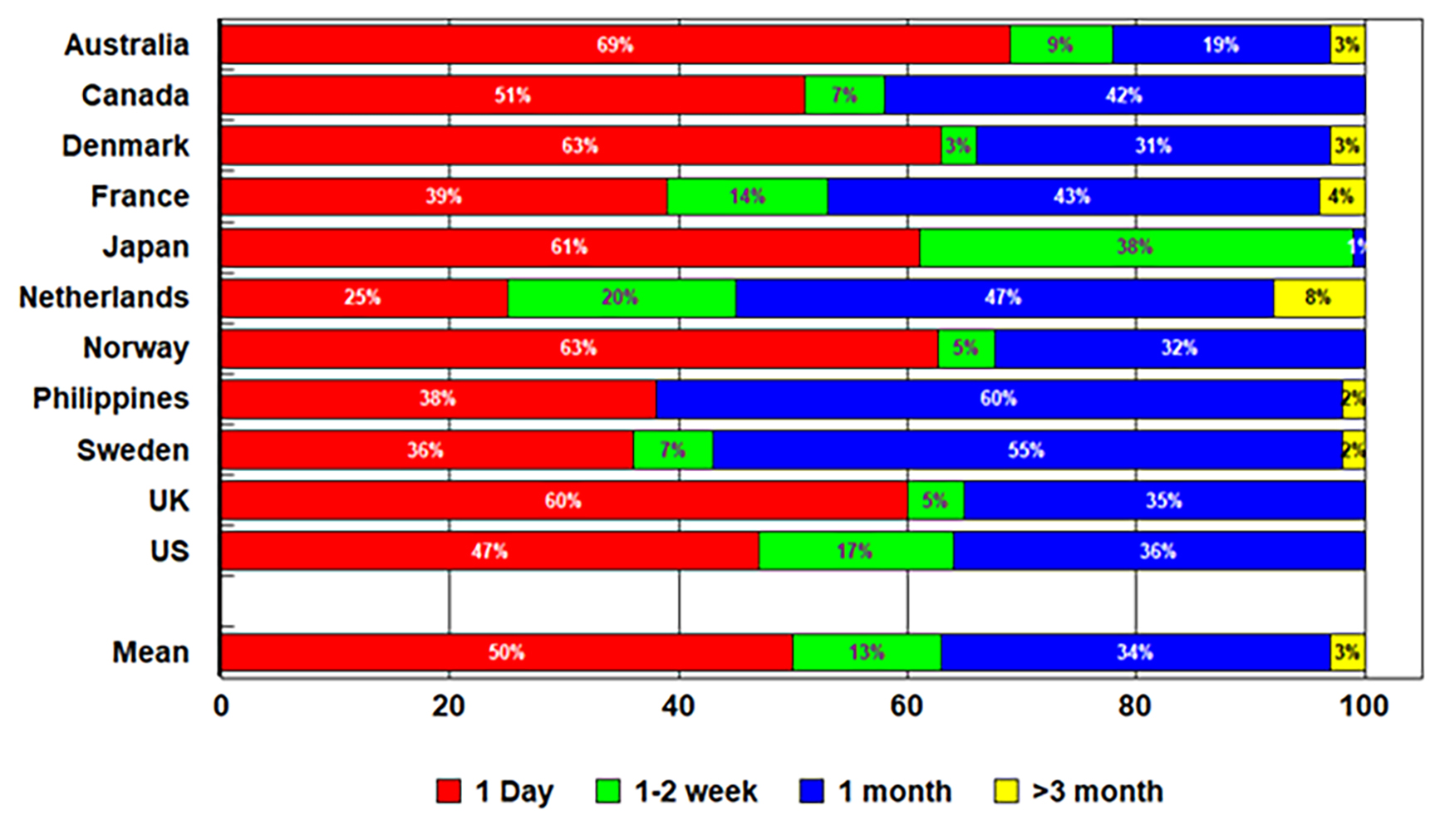
Figure 1 shows that on average, 50% of lenses fit are daily disposable, with just over one-third (34%) being replaced monthly. However, this differs widely between countries, with some (Australia) fitting over 2/3 with daily disposables and others (such as The Netherlands) only fitting 25%. This figure also shows the continued relevance of frequently replaced CLs, which continue to be used by 50% of wearers.
Figure 2 provides fascinating data on the continued usage of hydrogel materials, with an average of 27% of wearers still being fit with these materials (16% in daily disposables and 11% in reusable). Thus, despite the fact that silicone hydrogels have now been available for over 20 years, hydrogels still account for one-quarter of all fits. Once again, this does differ between countries, with some countries such as France and the Philippines having almost no hydrogel fits of any sort, but Japanese ECPs still fitting over 40% of its patients with hydrogel lenses.
Figure 2: Soft lens material type for daily disposable and frequent replacement (FRP) lenses, 202146
Putting it all together to achieve long-term wear
This article has reviewed patient needs and CL considerations by age, has highlighted the importance of evidence-based practice and summarised current fitting practices. How does this all come together to maximise success in patients’ long term?
To maintain CL wear over many years there are two distinct areas that must be considered: first, to address the key reasons patients drop out, and second, to ensure that the prescribed regimen helps to maintain healthy wear with minimal impact on ocular physiology over time.
Maintaining retention: comfort, vision and handling
Drop out from CL wear remains an issue, much of which is termed ‘silent drop out’, as the patient chooses to stop wearing lenses without discussing their concerns and seeking alternative solutions with their ECP first. A retrospective chart review of over five hundred patients new to CLs established a retention rate at 12 months of 74%.57 Of those who dropped out, the reason was not known for nearly one-third (32%) and for 71% of all dropouts no alternative lens or strategy had been tried. Where reasons were established for ceasing wear in this cohort of new wearers, the most common was poor vision, especially in toric and multifocal wearers, followed by discomfort and handling.57 For established wearers, dryness and discomfort remain the most common reasons given for drop out,66,67 with a pathway of reduced hours and days of wear leading to eventual drop out.68
Table 1: A proactive approach to identifying subjective suboptimal lens performance
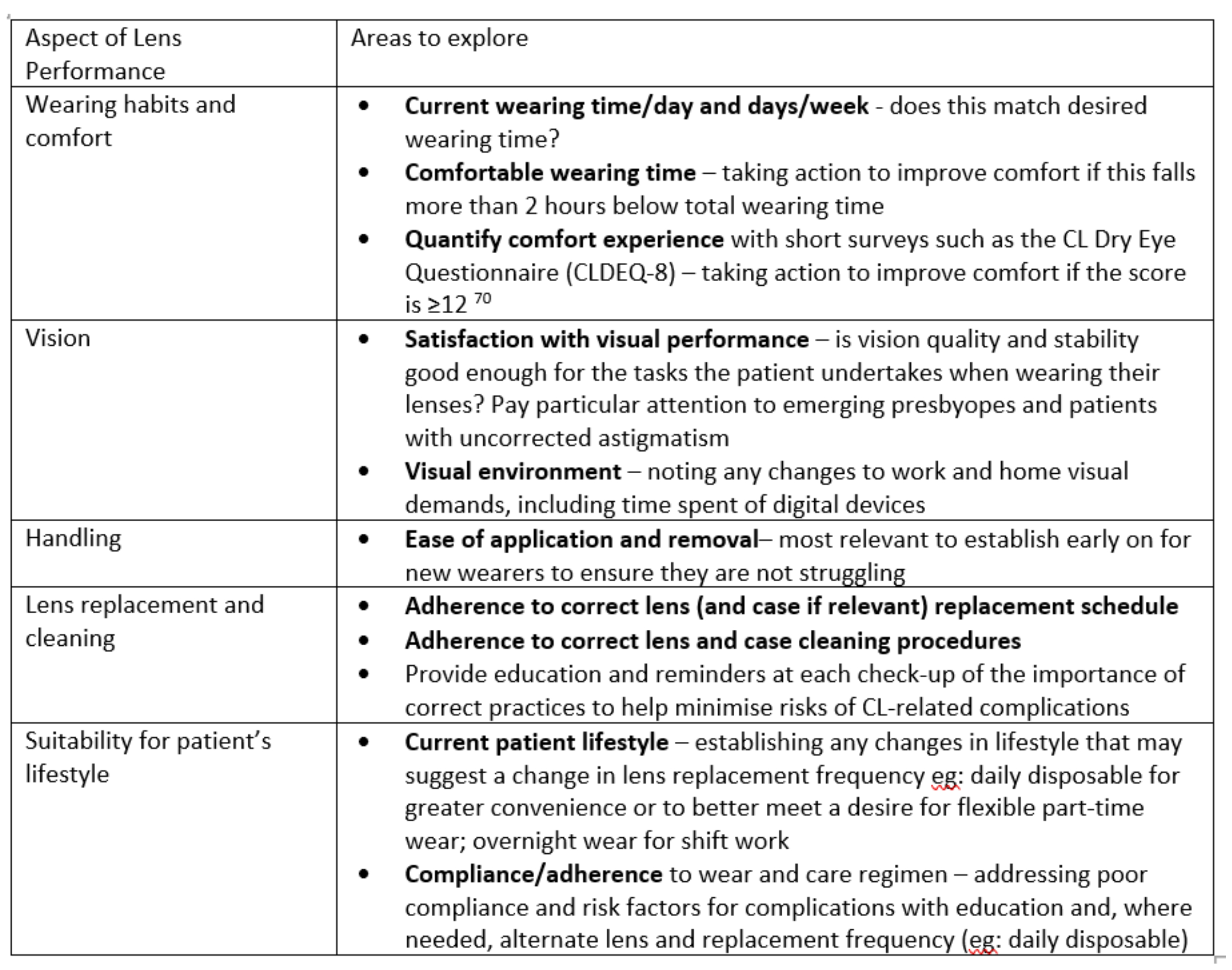
Recent correlation analysis on 55 adapted wearers revealed overall patient satisfaction was significantly correlated with handling, vision and comfort, with dissatisfaction with handling during lens application highlighted as potentially playing a major role in overall dissatisfaction with the CL.69 Given the evidence for how and why drop out occurs is clear, ECPs are well-placed to take a number of steps to proactively engage with their patients to address these issues early on, before they become too much for the patient to tolerate. This starts with exploring a number of areas of lens performance when taking history and symptoms at every aftercare (table 1), and ensuring the patient understands that their lens performance may change over time and there are other options they may be able to try.
Maintaining healthy CL wear throughout life
Oxygen considerations: Physiology and comfort with silicone hydrogels
As reported above, despite the fact that silicone hydrogel materials provide more oxygen to the eye, some 25% of new fits remain in hydrogels. Does this matter? Do all wearers need silicone hydrogel lenses to maintain a healthy cornea? Many studies have clearly demonstrated the improved physiological performance afforded by silicone hydrogels in certain wearers, including reduced limbal hyperaemia, reduced corneal swelling response and neovascular changes.71-74 The proportion of silicone hydrogels fit continue to grow, in both frequently replaced and daily disposable modalities.46
However, clinical evidence also exists that on a daily wear basis, hydrogels are able to provide oedema-free wear in many wearers and can provide good physiological performance for both children and adult wearers.16,75-78 It is also important to consider the design of the lens, as overall thickness profiles will impact oxygen transmission and thicker lens designs (such as that seen with certain toric or multifocal lenses) and higher prescriptions (especially in plus powered lenses) will have reduced oxygen transmission79,80 and may be better suited to being prescribed in silicone hydrogel materials.
In addition, there are differences in oxygen consumption between subjects, with marked differences in oedema responses between subjects when fitted with identical lenses and certain patients do need higher levels of oxygen delivery to prevent showing signs of hypoxia.81-83 A recent hypoxic model that took into consideration typical wearing patterns has predicted that when worn over an entire lifetime that silicone hydrogels result in a significantly lower oedema load to the cornea than hydrogel materials.84 So, for long term wear, over many years in adults, the additional oxygen delivery through silicone hydrogels induces a lower total level of hypoxia-induced corneal oedema response. The work in this model of long term wear of different materials seemingly echoing a message already well-accepted by the majority of ECPs, given the growth in use of this material over the past two decades.
Daily disposable lenses
As described above, daily disposable lenses continue to grow in terms of their fits to both new and existing wearers.46 Their convenience for busy lifestyles and ability to permit spectacle wearers to become ‘dual wearers’,85 using CLs on a part-time basis, remain major drivers for this growth. There are additional advantages to this replacement frequency too. With fewer steps in the daily routine compared to frequently replaced lenses that require cleaning and lens case care, it is easier for wearers to adhere to compliant practice with daily disposables. Daily disposable wearers are more likely to replace their lenses when advised to,86-88 have the lowest risk of inflammatory complications,49 avoid complications associated with lens cases and solutions,89-93 and report high levels of satisfaction.60,94
Physiology over time: What have we learned?
A recent review of 20 years of soft CL wear provides an assurance of what can be achieved if ECPs choose the appropriate lens materials and modality for their patients.95 Baseline ocular physiology data for 3,624 participants from the Brien Holden Vision Institute clinical trials database were retrospectively reviewed, from 1997 until now. Their data showed that while there have been changes over the past two decades in ocular physiological responses to CL wear, it appears that ocular health with current day CL wear is similar to no lens wear in most respects, demonstrating that modern lens materials and replacement options provide excellent options for patients compared with spectacle wear.95
Conclusion
With greater choice in CL technology, through designs, materials, replacement frequencies and prescription options, with increasing penetration of CL wear, and with young children starting lens wear earlier for myopia management, the need to wear them for many years over a substantial portion of a lifetime is becoming more common. It is important to set patient expectations from the outset. An informed patient is aware other options exist should their current lenses no longer meet their needs. A proactive ECP is motivated to carefully check all aspects of lens performance and their suitability for the patient’s lifestyle at every CL check.
Catching changes early enables solutions to be found, correcting sub-optimal comfort and vision, optimising healthy lens wear and ensuring the choice of lens best fits the lifestyle of the wearer. Contact lens wear itself can be constant for most wearers over the years, but expect change in prescription, lens design, material and replacement frequency over time to help maintain that. For ECPs, this practice is supported by an ever-growing choice of lens materials and optical designs, enabling a greater number of patients than ever before to be fitted with soft contact lenses. In many cases, the evidence suggests that moving forward there will be a growing number of wearers moving into silicone hydrogel daily disposables, helping to maximise comfort, compliance, convenience and minimise complications.
- Lyndon Jones is Director, Centre for Ocular Research & Education (CORE), School of Optometry and Vision Science, University of Waterloo, Waterloo, Ontario, Canada.
- Karen Walsh is Director, Global Professional Affairs 1 day & FRP lenses, CooperVision, Inc, and Anna Sulley is Director, Global Medical Affairs, CooperVision, Inc.
Disclosures: This article was funded by CooperVision, Inc.
References
- Pucker AD, Tichenor AA: A Review of Contact Lens Dropout. Clin Optom (Auckl) 2020; 12 85-94.
- Walline JJ, Gaume A, et al.: Benefits of contact lens wear for children and teens. Eye Contact Lens 2007; 33;6 Pt 1: 317-21.
- Sindt CW, Riley CM: Practitioner attitudes on children and contact lenses. Optometry 2011; 82;1: 44-5.
- Wolffsohn JS, Calossi A, et al.: Global trends in myopia management attitudes and strategies in clinical practice - 2019 Update. Cont Lens Anterior Eye 2020; 43;1: 9-17.
- Lumb E, Sulley A: Parent and practitioner opinions on myopia management – part 2. . Optician 2019; 219;8 (Aug 23): 26-28.
- Lumb E, Venezia C, et al.: Global survey on parent awareness and attitudes to myopia and its management. Contact Lens and Anterior Eye 2021; 44;1, Supplement 1: 13-14.
- Chamberlain P, Peixoto-de-Matos SC, et al.: A 3-year Randomized Clinical Trial of MiSight Lenses for Myopia Control. Optom Vis Sci 2019; 96;8: 556-567.
- Walline JJ, Walker MK, et al.: Effect of High Add Power, Medium Add Power, or Single-Vision Contact Lenses on Myopia Progression in Children: The BLINK Randomized Clinical Trial. JAMA 2020; 324;6: 571-580.
- Cho P, Cheung SW: Retardation of myopia in Orthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci 2012; 53;11: 7077-85.
- Bullimore MA, Richdale K: Myopia Control 2020: Where are we and where are we heading? Ophthalmic Physiol Opt 2020; 40;3: 254-270.
- Chamberlain P, Bradley A, et al.: Long-term Effect of Dual-Focus Contact Lenses on Myopia Progression in Children: A 6-year Multicentre Clinical Trial. Optom Vis Sci 2022; In press.
- Bullimore MA, Ritchey ER, et al.: The Risks and Benefits of Myopia Control. Ophthalmology 2021; 128;11: 1561-1579.
- Bullimore MA, Mirsayafov DS, et al.: Pediatric Microbial Keratitis With Overnight Orthokeratology in Russia. Eye Contact Lens 2021; 47;7: 420-425.
- Bullimore MA: The Safety of Soft Contact Lenses in Children. Optom Vis Sci 2017; 94;6: 638-646.
- Chalmers RL, McNally JJ, et al.: Adverse event rates in the retrospective cohort study of safety of paediatric soft contact lens wear: the ReCSS study. Ophthalmic Physiol Opt 2021; 41;1: 84-92.
- Woods J, Jones D, et al.: Ocular health of children wearing daily disposable contact lenses over a 6-year period. Cont Lens Anterior Eye 2021; 44;4: 101391.
- Walline JJ, Jones LA, et al.: Randomized trial of the effect of contact lens wear on self-perception in children. Optom Vis Sci 2009; 86;3: 222-32.
- Rah MJ, Walline JJ, et al.: Vision specific quality of life of pediatric contact lens wearers. Optom Vis Sci 2010; 87;8: 560-6.
- Pomeda AR, Perez-Sanchez B, et al.: MiSight Assessment Study Spain: A Comparison of Vision-Related Quality-of-Life Measures Between MiSight Contact Lenses and Single-Vision Spectacles. Eye Contact Lens 2018; 44 Suppl 2 S99-S104.
- Santodomingo-Rubido J, Villa-Collar C, et al.: Myopia control with orthokeratology contact lenses in Spain: a comparison of vision-related quality-of-life measures between orthokeratology contact lenses and single-vision spectacles. Eye Contact Lens 2013; 39;2: 153-7.
- Zhao F, Zhao G, et al.: Investigation of the Effect of Orthokeratology Lenses on Quality of Life and Behaviors of Children. Eye Contact Lens 2018; 44;5: 335-338.
- Yang B, Ma X, et al.: Vision-related quality of life of Chinese children undergoing orthokeratology treatment compared to single vision spectacles. Cont Lens Anterior Eye 2021; 44;4: 101350.
- Kandel H: Quality-of-life outcomes of long-term contact lens wear: A systematic review. Cont Lens Anterior Eye 2022; 45;1: 101521.
- Soni PS, Horner DG, et al.: Will young children comply and follow instructions to successfully wear soft contact lenses? CLAO J 1995; 21;2: 86-92.
- Morgan PB, Efron N: Global contact lens prescribing 2000-2020. Clin Exp Optom 2022 1-15.
- Efron N, Efron SE, et al.: A ‘cost-per-wear’ model based on contact lens replacement frequency. Clin Exp Optom 2010; 93;4: 253-60.
- Smith SL, Orsborn GN, et al.: An investigation into disposal and recycling options for daily disposable and monthly replacement soft contact lens modalities. Cont Lens Anterior Eye 2021 101435.
- Riley C, Young G, et al.: Prevalence of ocular surface symptoms, signs, and uncomfortable hours of wear in contact lens wearers: the effect of refitting with daily-wear silicone hydrogel lenses (senofilcon a). Eye Contact Lens 2006; 32;6: 281-6.
- Cho P, Cheung SW, et al.: Visual outcome of Soflens Daily Disposable and Soflens Daily Disposable for Astigmatism in subjects with low astigmatism. Clin Exp Optom 2012; 95;1: 43-7.
- Kruse A, Lofstrom T: How much visual benefit does an astigmat achieve being corrected with a toric correction? Int Contact Lens Clin 1996; 23;3/4: 59-65.
- Cox SM, Berntsen DA, et al.: Efficacy of Toric Contact Lenses in Fitting and Patient-Reported Outcomes in Contact Lens Wearers. Eye Contact Lens 2018; 44 Suppl 1 S296-S299.
- Morgan P, Smith S, et al.: Chair time required for the fitting of various soft contact lens designs. Optom Vis Sci 2021; 98 e-abstract 215062.
- Maldonado-Codina C, Navascues Cornago M, et al.: The association of comfort and vision in soft toric contact lens wear. Cont Lens Anterior Eye 2021; 44;4: 101387.
- World Health Organization: Ageing and health. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health 2021; Accessed 30 Mar 2022.
- Cohen A: Today’s older people really are ‘younger’ than in previous generations. https://www.fastcompany.com/90554646/todays-older-people-really-are-younger-than-in-previous-generations 2020; Accessed 30 Mar 2022.
- Richdale K, Mitchell GL, et al.: Comparison of multifocal and monovision soft contact lens corrections in patients with low-astigmatic presbyopia. Optom Vis Sci 2006; 83;5: 266-73.
- Sivardeen A, Laughton D, et al.: Randomized Crossover Trial of Silicone Hydrogel Presbyopic Contact Lenses. Optom Vis Sci 2016; 93;2: 141-9.
- Wolffsohn JS, Davies LN: Presbyopia: Effectiveness of correction strategies. Prog Retin Eye Res 2019; 68 124-143.
- Fogt JS, Weisenberger K, et al.: Visual performance with multifocal contact lenses and progressive addition spectacles. Cont Lens Anterior Eye 2021 101472.
- Walsh K, Jones L, et al.: Addressing common myths and misconceptions in soft contact lens practice. Clin Exp Optom 2021 1-15.
- Papas EB, Decenzo-Verbeten T, et al.: Utility of short-term evaluation of presbyopic contact lens performance. Eye Contact Lens 2009; 35;3: 144-8.
- Woods J, Woods C, et al.: Visual Performance of a Multifocal Contact Lens versus Monovision in Established Presbyopes. Optom Vis Sci 2015; 92;2: 175-82.
- Woods J, Woods CA, et al.: Early symptomatic presbyopes--what correction modality works best? Eye Contact Lens 2009; 35;5: 221-6.
- Diec J, Tilia D, et al.: Predicting Short-term Performance of Multifocal Contact Lenses. Eye Contact Lens 2017; 43;6: 340-345.
- Sivardeen A, Laughton D, et al.: Investigating the utility of clinical assessments to predict success with presbyopic contact lens correction. Cont Lens Anterior Eye 2016; 39;5: 322-30.
- Morgan P, Woods C, et al.: International Contact Lens Prescribing in 2021. Contact Lens Spectrum 2022; 37;1: 32-38.
- Morgan PB, Woods C, et al.: International contact lens prescribing in 2011. Contact Lens Spectrum 2012; 27;1: 26 - 31.
- Wolffsohn JS, Dumbleton K, et al.: CLEAR - Evidence-based contact lens practice. Cont Lens Anterior Eye 2021; 44;2: 368-397.
- Steele KR, Szczotka-Flynn L: Epidemiology of contact lens-induced infiltrates: an updated review. Clin Exp Optom 2017; 100;5: 473-481.
- Stapleton F, Bakkar M, et al.: CLEAR - Contact lens complications. Cont Lens Anterior Eye 2021; 44;2: 330-367.
- Szczotka-Flynn L, Jiang Y, et al.: Corneal inflammatory events with daily silicone hydrogel lens wear. Optom Vis Sci 2014; 91;1: 3-12.
- Cheung SW, Cho P, et al.: A comparative study of biweekly disposable contact lenses: silicone hydrogel versus hydrogel. Clin Exp Optom 2007; 90;2: 124-31.
- Fonn D, Dumbleton K: Dryness and discomfort with silicone hydrogel contact lenses. Eye Contact Lens 2003; 29;1 Suppl: S101-4; discussion S115-8, S192-4.
- Diec J, Tilia D, et al.: Comparison of Silicone Hydrogel and Hydrogel Daily Disposable Contact Lenses. Eye Contact Lens 2018; 44 Suppl 1 S167-S172.
- Lazon de la Jara P, Diec J, et al.: Measuring Daily Disposable Contact Lenses against Nonwearer Benchmarks. Optom Vis Sci 2018; 95;12: 1088-1095.
- Lazon de la Jara P, Papas E, et al.: Effect of lens care systems on the clinical performance of a contact lens. Optom Vis Sci 2013; 90;4: 344-50.
- Sulley A, Young G, et al.: Factors in the success of new contact lens wearers. Cont Lens Anterior Eye 2017; 40;1: 15-24.
- Sulley A, Young G, et al.: Retention Rates in New Contact Lens Wearers. Eye Contact Lens 2018; 44 Suppl 1 S273-S282.
- Efron N, Morgan PB: Rethinking contact lens aftercare. Clin Exp Optom 2017; 100;5: 411-431.
- Sulley A, Dumbleton K: Silicone hydrogel daily disposable benefits: The evidence. Cont Lens Anterior Eye 2020; 43;3: 298-307.
- Orsborn G, Dumbleton K: Eye care professionals’ perceptions of the benefits of daily disposable silicone hydrogel contact lenses. Cont Lens Anterior Eye 2019; 42;4: 373-379.
- Bishop MJ, Sun CK, et al.: Evaluation of daily disposable senofilcon A contact
