In the past few years, there has been increased interest about populations with special requirements, including autism. Although autistic people can have a co-occuring learning disability, autism is not a learning disability itself. This is likely to be a common misconception and can lead to autistic people being poorly understood and incorrectly supported. Research has reported healthcare professionals lack knowledge about autism and have limited autism-related resources.1-3
Although eye care providers (ECPs) have access to resources to improve accessibility for autistic children and autistic people with learning disabilities4 there is nothing that is tailored to autistic adults who do not have learning disabilities. The College of Optometrists has recently produced guidance on seeing autistic patients,5 but this is largely based on research concerning autistic children and around what would take place in the testing room. Additionally, although research has investigated eye conditions in autistic children, many of whom also had a learning disability, none has focused on autistic adults.6
It is evident that autistic adults without learning disabilities have received poor attention from current research and also when it comes to resource provision. Therefore, as ECPs, how can we be guided on what we should be aware of, or pay particular attention to when seeing autistic adult patients? Is it appropriate to assume that autistic adults will have similar experiences to autistic children or those with learning disabilities?
New emergent research has tried to address the lack of focus on autistic adults without learning disabilities.7,8 The aim of this series is to introduce this knowledge to ECPs to equip them with an understanding of adult autism and vision. What are the visual sensory experiences that autistic adults can be susceptible to? How do these impact their daily lives? This is an important area to appreciate because visual sensory experiences could affect the course of an eye examination and influence autistic adults’ visual symptoms. Thereafter, the series will explore the barriers that autistic adults face when accessing eye care and how accessibility could be improved with easy-to-implement adaptations.
What is autism?
Autism is a lifelong neurodevelopmental condition, affecting social interaction, communication and behaviour; see table 1 for some typical examples. Impairments in these areas have stressful and negative impacts on the day-to-day living of autistic people.9,10 Globally, the prevalence of autism is about 0.6%.11 In the UK, approximately 1.1% of adults12 and 1.57% of children13 are diagnosed as autistic, although these figures are probably inaccurate due to under-diagnosis in adults,14 females15 and ethnic minority groups.16 There appears to be a gender imbalance, with up to four times more males diagnosed as autistic than females.17,18 Around one-third of autistic people also have a learning disability.19
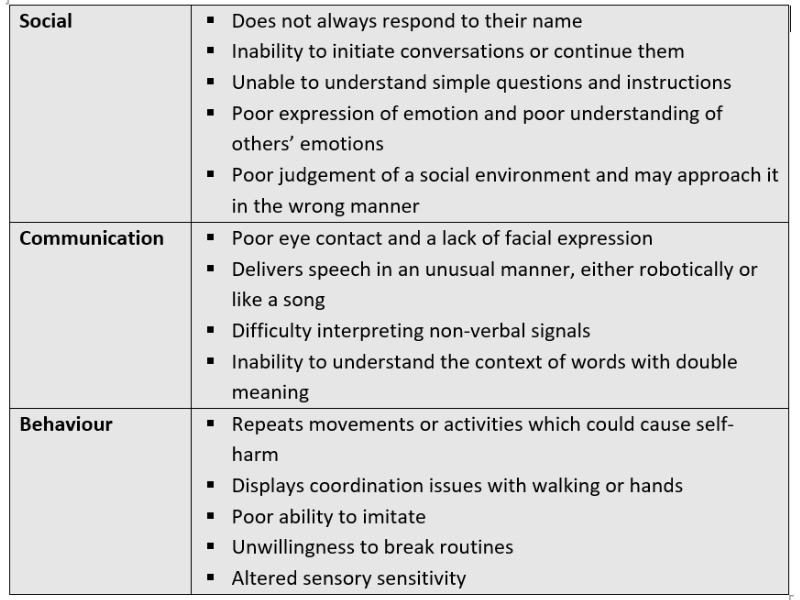
Table 1: Examples of the social, communication and behavioural challenges that autistic people can experience21
The UK diagnostic criteria for autism are laid out in the International Statistical Classification of Diseases (ICD-11)20 and Diagnostic and Statistical Manual of Mental Disorders (DSM-5)21 (figure 1). In summary, these are:
- Impaired social communication and interaction
- Restricted or repetitive patterns of behaviour
- Symptoms must be present in the early developmental period but not necessarily fully manifest
- A clinically significant impairment of social ability, occupational capability or in another area of function
- Impairments cannot be better explained by intellectual disability or global developmental delay
Autism diagnosis centres in the UK use various methods to assess the likelihood of an individual being autistic, including questionnaires, interviews, and consultations by a multidisciplinary team. However, the National Autistic Society22 highlights that if a diagnosis of adult autism is made by these centres then they do not always go on to offer future support or follow-ups. It is autistic people with learning disabilities who are more likely to receive support.23
Figure 1: The UK diagnostic criteria for autism are laid out in the ICD-11 and DSM-5
Autism and Sensory Experiences
The majority of autistic people have altered sensory sensitivity,24,25 meaning they experience sensory stimuli differently to non-autistic people. They can be hyper- or hypo-sensitive to sensory stimuli. Hypersensitivity describes an excessive response to sensory stimuli, such as:
- Visually focusing on fine details in an object rather than the object as a whole
- Intolerance to the feel of particular textures or types of clothing
- Finding the tastes of certain foods overpowering, and therefore developing a restricted diet
- An inability to cope with certain scents, for example strong perfumes
- Difficulty ignoring background noise
Hyposensitivity describes an obviously dampened response to sensory stimuli, for example:
- An inability to visually detect some features of objects
- An ability to tolerate more pain that usually expected
- A liking for extreme tasting foods, such as very spicy food
- Failure to notice strong smells
- Gaining pleasure from loud noises
Additionally, autistic people can display sensory seeking behaviours such as excessive touching of object edges or fascination with reflections.26
Altered sensory sensitivity largely takes the form of hypersensitivity for autistic individuals.27 Assessment of altered sensory sensitivity can be grouped into five key methods:
- Questionnaires
- Psychophysical assessment
- Direct behavioural observation
- Interviewing techniques
- Neuroimaging28
Research has shown the degree of altered sensory sensitivity increases with the severity of autism29 but not age.30,31 Importantly, sensory issues are lifelong,32 affects each sense33,34 as well as multisensory processing.35,36 The impact of these can vary from stressful to pleasant, depending on the nature of the experience produced.37,38 Unsurprisingly, a recent review39 has found meaningful links between sensory sensitivities and fear and anxiety; particularly, there is a potential bi-directional relationship between sensory sensitivity and anxiety.
Autism and Visual Sensory Experiences
Vision is often thought of as the dominant human sense; a recent survey study40 found that 75% of non-autistic adults (67/91) feared losing their sight the most. Vision plays a major role in the simplest of tasks, such as activities of daily living.41 The importance of vision can be easily underestimated by individuals who do not experience any visual issues.
Various studies have used questionnaires,27 interviews38,42 and focus groups37 to investigate general sensory sensitivity in autistic adults, mentioning some visual experiences. Although we can get a feel for the variety of autistic visual sensory experiences from these studies, it is unlikely that they have revealed the full extent. This is because studies have not focused on vision. Identifying this gap and the need for a holistic understanding, more recent qualitative research by Parmar et al7 has focused solely on autistic adults’ visual sensory experiences, with an aim to characterise these in detail alongside associated impacts and coping strategies.
It is important for ECPs to have an understanding of autistic visual sensory experiences because these can influence how comfortable an autistic person may feel in the optometric practice and during the eye examination, their presenting visual symptoms, their ability to undergo eye tests and how they visually manage on a daily basis. Appreciating these factors can allow ECPs to consider how their services could be better adapted for autistic people, deliberate the likelihood of presenting visual symptoms being linked to visual sensory experiences, or the impact of visual sensory experiences on autistic people, which may otherwise be less influential for non-autistic people. The following sections discuss our current understanding of autistic visual experiences, the impact these have on daily living and coping strategies that autistic adults employ.
Features of autistic visual experiences
Autistic adults can experience a variety of visual hypersensitivities, but these vary from person to person depending on how sensitive they are to visual inputs.7,43 Therefore, a blanket assumption cannot be made about autistic visual sensory experiences. Nevertheless, it is important to have an all-round awareness of the challenges or advantages that an autistic person could face.
A commonly reported autistic experience is hypersensitivity to different aspects of lighting.7,37,38 43-45 Brightly lit environments, and flickering or artificial lighting can trigger discomfort. Particularly, strip and spotlights can be challenging because they are concentrated light sources, as opposed to diffuse lighting (figure 2). Furthermore, rapid changes in intensity or type of lighting (eg moving from a naturally lit to artificially lit environment) can be problematic.37 Visual clutter combined with lots of movement in the visual field cause difficulty for autistic adults who are hypersensitive to visual motion;7 interestingly, cognitive studies have found autistic people to have altered perception of motion.46,48 Impressions of environments, objects and food can be strongly influenced by likes and dislikes for particular colours. Bright, vibrant colours can be troublesome for autistic people because of visual hypersensitivity.7,37,48 In Parmar et al,7 participants described bright colours as causing ‘…toddler screaming levels of irritation’ and said, ‘...if it had any bright colours then I would just avoid that room.’
Figure 2: Spotlights can be challenging for autistic people

Due to altered sensory processing, autistic adults can pay more attention to fine details (‘local information’) rather than the overall impression of an object or environment (‘global information’).7, 26, 49-51 Cognitive theories that have attempted to explain this altered processing are the Weak Central Coherence theory,52 Enhanced Perceptual Function theory53 and Predictive Coding.54 As a result, they notice details that non-autistic people may overlook, such as minute details in pictures or patterns in data.
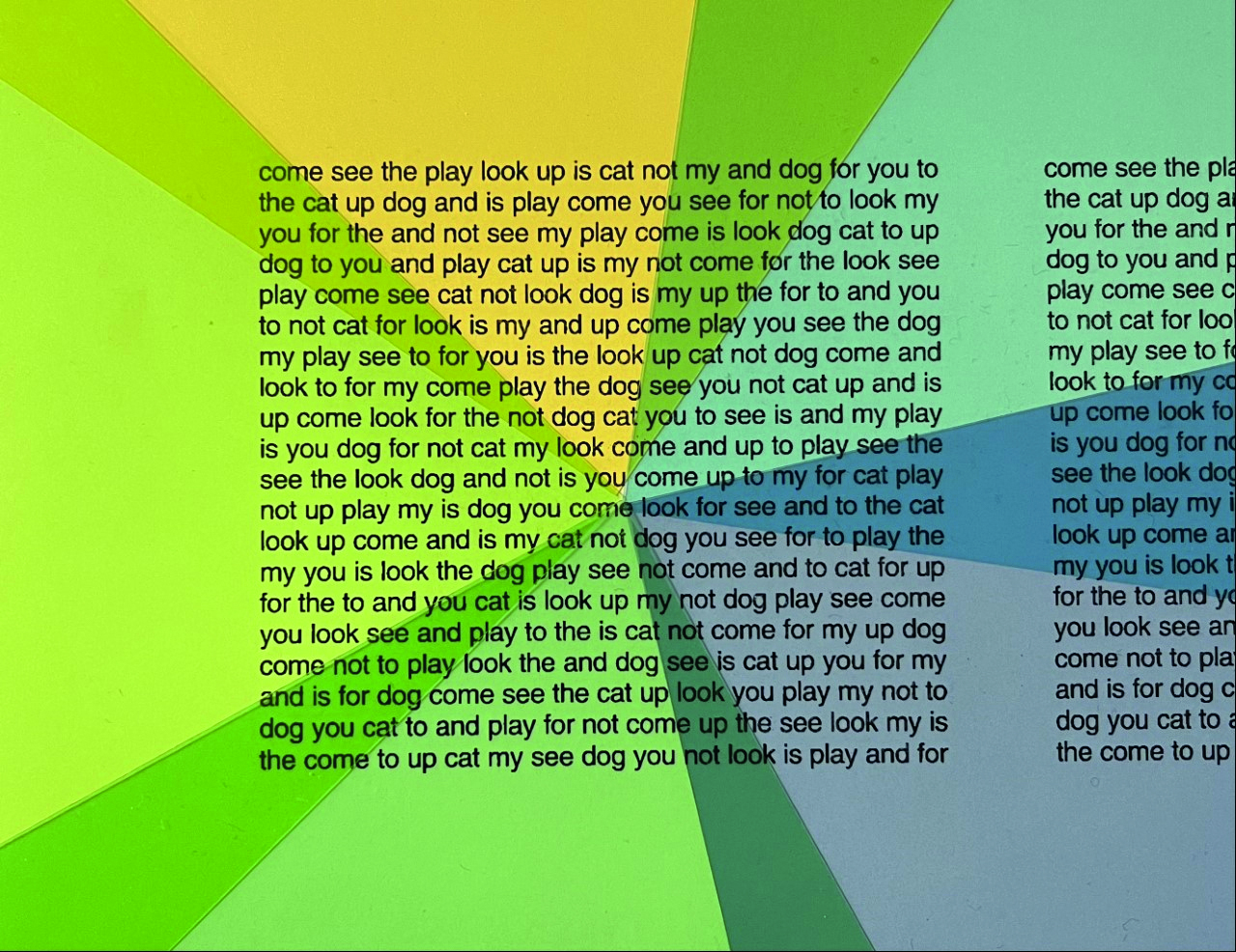
Originally described by Olive Meares55 and Helen Irlen,56 visual stress (also termed ‘Meares-Irlen syndrome’, ‘pattern glare’ and ‘scotopic sensitivity’) is a perceptual disorder caused by repetitive high-contrast patterns.57 Autistic adults have reported visual experiences that overlap with key symptoms of visual stress, including flickering, fading and discomfort when viewing repetitive patterns.7,37 Although visual stress is commonly associated with reading, autistic adults have largely described it as a wider issue impacting different aspects of daily life, such as the effect of the pattern created by items on a shelf or striped carpets at the entrance of shops (figure 3).7, 37
Figure 3: With autism, visual stress may be caused by many things, such as the pattern created by striped carpets at the entrance of shops

In addition to visual sensory experiences, autistic adults have suggested issues associated with eye movements. Multiple lab-based studies have investigated this in autistic individuals. These have found that their ability to initiate saccades and engage/disengage from targets to be comparable to non-autistic people.59 On the other hand, autistic people make faster eye movements during predictable saccades58 and exhibit poor eye tracking of moving objects, impaired ability to stop saccades and reduced accuracy of saccades.
Subjectively, autistic adults have reported difficulties suggestive of issues with eye tracking, visually locating objects and ocular muscle balance: ‘My eye tracking is a bit weird. I think I don’t look at... the thing I’m intending to look at sometimes or following it correctly.’7 It is possible that impairments with eye movements contribute to autistic visual sensory experiences, but this is yet to be thoroughly investigated. From an ECPs perspective, ensuring a comprehensive eye examination for autistic patients is important to rule out any optometric symptoms that may contribute to visual experiences. Studies with autistic children have revealed a higher likelihood of significant refractive errors and binocular vision anomalies (e.g., strabismus and amblyopia) compared to non-autistic controls.6
The impacts of autistic visual sensory experiences
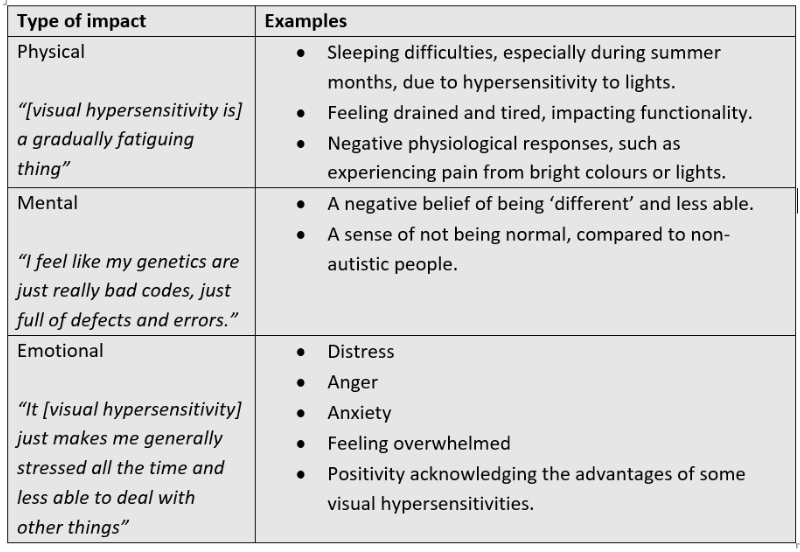
Visual sensory experiences have multiple impacts on the day-to-day living of autistic adults. They face largely negative effects on personal wellbeing. Table 2 gives examples of how autistic visual sensory experiences affect physical, mental and emotional wellbeing, adapted from Parmar et al.7
Visual sensory experiences can hinder tasks in daily life,7 and it would not be unreasonable to speculate that they contribute to poorer daily living skills that are exhibited by autistic individuals.60, 61 In particular, activities requiring concentration, such as cooking or crafting, are less enjoyable and in fact can be overwhelming. Many a time, visual sensory experiences contribute to a larger multisensory issue for autistic adults.7 They can have difficulty visiting public places, for example supermarkets and hospitals, and using public transport, subsequently avoiding them. In such environments, autistic adults experience different visual sensory issues (e.g., bright colours, uncomfortable lighting and lots of visual motion) together with multisensory challenges (e.g., lots of noise and strong smells):
“...it’s a multi-level thing... I mean hard, easy to clean floors, which means every person stepping around is bang, bang, bang... You’ve got people moving around randomly. You’ve got the bright lights... and you’ve got all the people talking simultaneously.”7
Table 2: Examples of the physical, mental and emotional impacts of visual sensory experiences on autistic adults.7 Quotes are taken from Parmar et al7
Distraction has been suggested to be the main impact of visual sensory experiences.7 Studies have shown autistic individuals to have difficulties ignoring irrelevant sensory information,38, 62, 63 and impaired attention,30 which is closely linked to distraction. Explanations for the former include autistic people having a greater perceptual capacity (i.e., they can process relatively more sensory information before irrelevant input is filtered out)64 and enhanced sensory sensitivity,30 both of which are positively correlated to each other.65 Parmar et al’s7 participants described difficulty with attending just to their central vision. In fact, autistic people have to make a conscious effort to ignore stimuli in the peripheral field.7 Having to do this can be tiring and result in autistic adults feeling frustrated and angry. On the other hand, some autistic adults used visual distractions to fully occupy their attention, preventing distractions from other stimuli: ‘...so I can ignore the sounds and the visual stimulus of people talking, I focus as firmly as I can on what I’m reading.’7
A good example of the practical implications of distractions is driving difficulties for autistic adults. Research has shown that autistic people display more problematic driving behaviours and are less likely to pay attention to relevant visual information when driving.67 Subjectively, autistic people have said bright headlights, visual clutter and redundant objects in the visual field can make them feel overwhelmed and struggle to focus where required. As a result, this population may avoid driving.7 Of course, these visual issues will contribute to other reported driving concerns displayed by autistic people: poor motor coordination, speed control, adaptability to unexpected situations and ability to stay in lane.68
Autistic visual sensory experiences can have positive aspects too. It has been noted that when sensory experiences, or the associated anxieties, are under control then they can be enjoyable.69 Autistic adults may take advantage of their visual hypersensitivity to fine detail, being able to spot patterns in data analysis or features in environments, which non-autistic people may overlook.7 While brightly lit environments and vibrant colours have largely been reported to cause negative experiences,7, 37-38 for some they can be pleasant and stimulating.43 For example, dull days can leave autistic adults feeling sad and depressed: ‘I always feel my best on a bright, sunny day. I like rooms to be brightly lit...’43
Overall, the impact of visual sensory experiences is situation-dependent and can have both positive and negative implications for autistic adults. This was well described by a participant in Parmar et al’s study:7
“...seeing details is a double-edged sword. On the one hand you could get overwhelmed with all the detail. But at the same time, it also means ... When I’m painting, I can see far more detail than other people can see. I can spot things that other people miss.”
Attempts to manage autistic visual sensory experiences
Few studies have attempted to investigate autistic adults’ coping strategies for sensory experiences.37, 38, 69 Of these, only Parmar et al7 have focused on vision, but it appears that some coping mechanisms are not exclusive to a particular sense. Agreeing with the vision-related results of Parmar et al,7 Smith and Sharp38 found the impact of general sensory issues can be controlled with moderating factors: reducing sensory inputs, reducing stimuli intensity (e.g., dimmer lights or quieter sounds), being able to predict the environment (such as knowing the types of sensory stimuli) and the autistic person being calm. In situations where autistic adults have ineffective or undetermined coping strategies, they just try to cope as best as possible.7 As a result, they may experience increasing sensory overload leading to greater negative emotions such as distress.
Coming to visual sensory issues, autistic adults try to practically overcome these using different strategies. Autistic adults can experience sensory overload because of excessive visual information. Consequently, they avoid visually cluttered places (e.g., public places at peak time and social gatherings), or visit the same supermarkets as they would know where items are usually kept.7 However, avoiding social events can put autistic people at risk of appearing uncooperative or awkward.
Next, simple light alterations in artificially lit environments help some autistic people cope with visual sensory issues.7 The colour temperature of lighting can influence visual comfort, with natural light easing visual sensory symptoms and warmer light feeling more comfortable. In general, lowering light levels may improve visual performance: ‘...I can see very well in low light.’7
Specific to eyewear, autistic adults can find their spectacle frames to be a distraction, especially if they are bold and very visible in their field of view. Options to manage this include rimless spectacles or larger, subtle frames, which are less visible.7 Considering the difficulties autistic adults may have with bright lights, it would not be unreasonable to suggest sunglasses or photochromic lenses to be useful. But, these seem to only be a partial solution because the artificial darkening can be disconcerting and make one feel detached from reality. This emphasises the struggle that visually sensitive autistic people face in balancing optimal conditions for good vision with managed sensory issues.
Autistic adults have mixed views on the impacts of coloured filters (overlays and lenses).7 For some with pattern sensitivity issues, coloured filters noticeably improve reading, quality of vision and ability to interpret facial expressions: ‘...[without coloured lenses] I never saw the social world, I never saw people, never saw expression...’7 For others, they provide no perceivable benefit. Coloured filters are prescribed in optometric practices (figure 4) as per a standardised protocol to manage visual stress, and can be found here. However, they are now being promoted as a management option for autistic behaviours (read more here).
Figure 4: Coloured overlays used for visual stress (image courtesy of Dr Catherine Porter)
The suggested link between autism and coloured filters may be based on the extremely beneficial effects of coloured lenses reported in two personal stories from autistic individuals70, 71 and a case report on one autistic child,72 but this represents very low quality evidence for a routine intervention. Studies with autistic children have suggested mixed effects on reading speed,72-74 improved ability to interpret facial expressions,75 and enhanced control of behaviour, coordination and personal space.72, 76
Yet some of these studies have poor control of placebo effect and bias, and there is restricted generalisability due to limited participant numbers. As Ludlow et al76 point out, further work is needed to find out whether the effect of coloured filters would be ‘worthwhile and long-lasting’ as a clinical intervention for autism. It is important to highlight that symptoms of visual stress overlap with those of other ophthalmic anomalies, for example, uncorrected refractive error, convergence insufficiency and cataract.77, 79 Therefore, optometrists should thoroughly assess and manage these prior to recommending coloured filters.80
Key messages
Autistic adults can experience a variety of visual symptoms (the majority being sensory), which vary between individuals and cause considerable discomfort for some. These symptoms can occur alone or contribute to larger multisensory experiences. Although it could be argued that non-autistic people may experience similar visual experiences, it is the impact that seems greater for autistic people. This has driven some autistic people to access unregulated management options, such as tinted lenses, which claim to have a calming effect in this population.
Visual symptoms cause or contribute to mostly negative impacts on daily activities. Autistic people try to control the effects of visual experiences but with limited success. It is possible that some visual experiences are linked to more basic ophthalmic anomalies, although this requires further investigation.
Optometrists should thoroughly assess and manage these to prevent resultant symptoms contributing to autistic visual sensory experiences.
- Dr Ketan Parmar PhD MSci(optom) is a research optometrist at Eurolens Research, and Optometry Clinical Tutor for the undergraduate Optometry degree programme at The University of Manchester.
References
- Calleja S, Islam FMA, Kingsley J, McDonald R. Healthcare access for autistic adults: A systematic review. Medicine. 2020;99(29):e20899-e.
- Mason D, Ingham B, Urbanowicz A, Michael C, Birtles H, Woodbury-Smith M, et al. A systematic review of what barriers and facilitators prevent and enable physical healthcare services access for autistic adults. Journal of Autism And Developmental Disorders. 2019;49(8):3387-400.
- Morris R, Greenblatt A, Saini M. Healthcare providers’ experiences with autism: a scoping review. Journal of Autism and Developmental Disorders. 2019;49(6):2374-88.
- SeeAbility. Resources. 2019. [Available from: https://www.seeability.org/resources?resource_specialism=52. Accessed: 3rd October 2021]
- The College of Optometrists. Examining patients with autism. 2021. [Available from: https://guidance.college-optometrists.org/guidance-contents/knowledge-skills-and-performance-domain/examining-patients-with-autism/?action=generate-pdf&domain=1§ion=2508. Accessed: 7th September 2021]
- Gowen E, Porter C, Baimbridge P, Hanratty K, Pelham J, Dickinson C. Optometric and orthoptic findings in autism: a review and guidelines for working effectively with autistic adult patients during an optometric examination. Optometry in Practice. 2017;18(3):145-54.
- Parmar KR, Porter CS, Dickinson CM, Pelham J, Baimbridge P, Gowen E. Visual sensory experiences from the viewpoint of autistic adults. Frontiers in Psychology. 2021;12.
- Parmar KR, Porter CS, Dickinson CM, Pelham J, Baimbridge P, Gowen E. Autism-friendly eyecare: Developing recommendations for service providers based on the experiences of autistic adults. Ophthalmic and Physiological Optics. 2022.
- Oakley B, Loth E, Murphy DG. Autism and mood disorders. International Review of Psychiatry. 2021;33(3):280-99.
- Uljarevié M, Katsos N, Hudry K, Gibson JL. Practitioner Review: Multilingualism and neurodevelopmental disorders - an overview of recent research and discussion of clinical implications. Journal of Child Psychology and Psychiatry. 2016;57(11):1205-17.
- Elsabbagh M, Divan G, Koh YJ, Kim YS, Kauchali S, Marcín C, et al. Global prevalence of autism and other pervasive developmental disorders. Autism Research. 2012;5(3):160-79.
- Brugha T, Cooper S, McManus S, Purdon S, Smith J, Scott F, et al. Estimating the prevalence of autism spectrum conditions in adults: extending the 2007 adult psychiatric morbity survey. 2012. [Available from: http://www.wecommunities.org/MyNurChat/archive/LDdownloads/Est_Prev_Autism_Spec_Cond_in_Adults_Report.pdf. Accessed: 14th march 2022]
- Taylor B, Jick H, Maclaughlin D. Prevalence and incidence rates of autism in the UK: time trend from 2004-2010 in children aged eight years. BMJ Open. 2013;3(10):e003219-e.
- Kapp SK, Gillespie-Lynch K, Sherman LE, Hutman T. Deficit, difference, or both? Autism and neurodiversity. Developmental Psychology. 2013;49(1):59-71.
- Hull L, Petrides KV, Mandy W. The female autism phenotype and camouflaging: a narrative review. Review Journal of Autism and Developmental Disorders. 2020;7(4):306-17.
- Hussein AM, Pellicano E, Crane L. Understanding and awareness of autism among Somali parents living in the United Kingdom. Autism. 2019;23(6):1408-18.
- Loomes R, Hull L, Mandy WPL. What Is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. Journal of the American Academy of Child & Adolescent Psychiatry. 2017;56(6):466-74.
- Fombonne E. Epidemiology of pervasive developmental disorders. Paediatric Research. 2009;65(6):591-8.
- Lemmi V, Knapp M, Rahan I. The autism dividend: reaping the rewards of better investment. London: National Autism Project, 2017.
- World Health Organization. International Statistical Classification of Diseases Revision 11. Geneva: World Health Organization, 2021.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington: American Psychiatric Association; 2013.
- National Autistic Society. Post-diagnosis support - a guide for autistic adults. 2020. [Available from: https://www.autism.org.uk/advice-and-guidance/topics/diagnosis/post-diagnosis-support/autistic-adults. Accessed: 4th january 2022]
- National Audit Office. Supporting people with autism through adulthood. 2009. [Available from: https://www.nao.org.uk/report/supporting-people-with-autism-through-adulthood/. Accessed: 4th October 2021]
- Green D, Chandler S, Charman T, Simonoff E, Baird G. Brief report: DSM-5 sensory behaviours in children with and without an autism spectrum disorder. Journal of Autism and Developmental Disorders. 2016;46(11):3597-606.
- Kientz M, Dunn W. A Comparison of the Performance of Children With and Without Autism on the Sensory Profile. The American Journal of Occupational Therapy. 1997;51(7):
530-7. - Simmons D, Robertson A, McKay L, Toal E, McAleer P, Pollick F. Vision in autism spectrum disorders. Vision Research. 2009;49(22):2705-39.
- Ben-Sasson A, Gal E, Fluss R, Katz-Zetler N, Cermak SA. Update of a meta-analysis of sensory symptoms in ASD: A new decade of research. Journal of Autism and Developmental Disorders. 2019;49(12):4974-96.
- DuBois D, Lymer E, Gibson BE, Desarkar P, Nalder E. Assessing sensory processing dysfunction in adults and adolescents with autism spectrum disorder: a scoping review. Brain Sciences. 2017;7(8):108.
- Robertson AE, Simmons DR. The relationship between sensory sensitivity and autistic traits in the general population. Journal of Autism and Developmental Disorders. 2013;43(4):775-84.
- Liss M, Saulnier C, Fein D, Kinsbourne M. Sensory and attention abnormalities in autistic spectrum disorders. Autism. 2006;10(2):155-72.
- Kern J, Trivedi M, Garver C, Grannemann B, Andrews A, Savla J, et al. The pattern of sensory processing abnormalities in autism. Autism. 2006;10(5):480-94.
- Crane L, Goddard L, Pring L. Sensory processing in adults with autism spectrum disorders. Autism. 2009;13(3):215-28.
- Baum SH, Stevenson RA, Wallace MT. Behavioral, perceptual, and neural alterations in sensory and multisensory function in autism spectrum disorder. Progress in neurobiology. 2015;134:140-60.
- Clery H, Andersson F, Bonnet-Brilhault F, Philippe A, Wicker B, Gomot M. fMRI investigation of visual change detection in adults with autism. NeuroImage: Clinical. 2013;2:303-12.
- Beker S, Foxe JJ, Molholm S. Ripe for solution: Delayed development of multisensory processing in autism and its remediation. Neuroscience & Biobehavioral Reviews. 2018;84:182-92.
- Marco EJ, Hinkley LB, Hill SS, Nagarajan SS. Sensory processing in autism: a review of neurophysiologic findings. Pediatric research. 2011;69(8):48-54.
- Robertson AE, Simmons DR. The Sensory Experiences of Adults with Autism Spectrum Disorder: A Qualitative Analysis. Perception. 2015;44(5):569-86.
- Smith RS, Sharp J. Fascination and isolation: A grounded theory exploration of unusual sensory experiences in adults with Asperger syndrome. Journal of Autism and Developmental Disorders. 2013;43(4):891-910.
- Muskett A, Radtke S, White S, Ollendick T. Autism spectrum disorder and specific phobia: The role of sensory sensitivity: Brief review. Journal of Autism and Developmental Disorders. 2019;6(3):289-93.
- Hutmacher F. Why is there so much more research on vision than on any other sensory modality? Frontiers in Psychology. 2019;10.
- Kempen GIJM, Ballemans J, Ranchor AV, van Rens GHMB, Zijlstra GAR. The impact of low vision on activities of daily living, symptoms of depression, feelings of anxiety and social support in community-living older adults seeking vision rehabilitation services. Quality of Life Research. 2012;21(8):1405-11.
- Kirby AV, Dickie VA, Baranek GT. Sensory experiences of children with autism spectrum disorder: In their own words. Autism. 2015;19(3):316-26.
- Robledo J, Donnellan A, Strandt-Conroy K. An exploration of sensory and movement differences from the perspective of individuals with autism. Frontiers in Integrative Neuroscience. 2012;6.
- Bogdashina O. Different sensory experiences – different perceptual worlds. In: Sensory perceptual issues in autism. London: Jessica Kingsley, 2003.
- Leekam S, Nieto C, Libby S, Wing L, Gould J. Describing the Sensory Abnormalities of Children and Adults with Autism. Journal of Autism and Developmental Disorders. 2007;37(5):894-910.
- Van der Hallen R, Evers K, Brewaeys K, Van den Noortgate W, Wagemans J. Global processing takes time: A meta-analysis on local–global visual processing in ASD. Psychological Bulletin. 2015;141(3):549.
- Todorova GK, Hatton REM, Pollick FE. Biological motion perception in autism spectrum disorder: a meta-analysis. Molecular Autism. 2019;10(1):49.
- Robertson A. Sensory experiences of individuals with Autism Spectrum Disorder and autistic traits: a mixed methods approach. University of Glasgow; 2012.
- Kabatas E, Ozer P, Ertugrul G, Kurtul B, Bodur S, Alan B. Initial ophthalmic findings in turkish children with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2015;45(8):2578-81.
- Rinehart N, Bradshaw J, Moss S, Brereton A, Tonge B. Atypical interference of local detail on global processing in high-functioning autism and Asperger’s disorder. The Journal of Child Psychology and Psychiatry and Allied Disciplines. 2000;41(6):769-78.
- Plaisted K, Swettenham J, Rees L. Children with autism show local precedence in a divided attention task and global precedence in a selective attention task. The Journal of Child Psychology and Psychiatry and Allied Disciplines. 1999;40(5):733-42.
- Happé F, Frith U. The weak coherence account: Detail-focused cognitive style in autism spectrum disorders. Journal of Autism and Developmental Disorders. 2006;36(1):5-25.
- Mottron L, Dawson M, Soulières I, Hubert B, Burack J. Enhanced perceptual functioning in autism: an update, and eight principles of autistic perception. Journal of Autism and Developmental Disorders. 2006;36(1):27-43.
- Friston K. Predictive coding, precision and synchrony. Cognitive Neuroscience. 2012;3(3-4):238-9.
- Meares O. Figure/ground, brightness contrast, and reading disabilities. Visible Language. 1980;14(1):13-29.
- Irlen H. Reading by the colours. New York: Avery; 1991.
- Evans BJ, Stephenson SJ. The pattern glare test: a review and determination of normative values. Ophthalmic & Physiological Optics. 2008;28(4):295-309.
- Kovarski K, Siwiaszczyk M, Malvy J, Batty M, Latinus M. Faster eye movements in children with autism spectrum disorder. Autism research. 2019;12(2):212-24.
- Johnson BP, Lum JAG, Rinehart NJ, Fielding J. Ocular motor disturbances in autism spectrum disorders: Systematic review and comprehensive meta-analysis. Neuroscience & Biobehavioral Reviews. 2016;69:260-79.
- Bal VH, Kim S-H, Cheong D, Lord C. Daily living skills in individuals with autism spectrum disorder from 2 to 21 years of age. Autism. 2015;19(7):774-84.
- Smith LE, Maenner MJ, Seltzer MM. Developmental trajectories in adolescents and adults with autism: The case of daily living skills. Journal of the American Academy of Child & Adolescent Psychiatry. 2012;51(6):622-31.
- Adams NC, Jarrold C. Inhibition in autism: Children with autism have difficulty inhibiting irrelevant distractors but not prepotent responses. Journal of Autism and Developmental Disorders. 2012;42(6):1052-63.
- Christ SE, Kester LE, Bodner KE, Miles JH. Evidence for selective inhibitory impairment in individuals with autism spectrum disorder. Neuropsychology. 2011;25(6):690-701.
- Remington A, Swettenham J, Campbell R, Coleman M. Selective attention and perceptual load in autism spectrum disorder. Psychological Science. 2009;20(11):1388-93.
- Brinkert J, Remington A. Making sense of the perceptual capacities in autistic and non-autistic adults. Autism. 2020;24(7):1795-804.
- Mottron L, Mineau S, Martel G, Bernier CS-C, Berthiaume C, Dawson M, et al. Lateral glances toward moving stimuli among young children with autism: Early regulation of locally oriented perception? Development and Psychopathology. 2007;19(1):23-36.
- Daly BP, Nicholls EG, Patrick KE, Brinckman DD, Schultheis MT. Driving behaviors in adults with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2014;44(12):3119-28.
- Classen S, Monahan M, Hernandez S. Indicators of simulated driving skills in adolescents with autism spectrum disorder. The Open Journal of Occupational Therapy. 2013;1(4):2.
- Jones RSP, Quigney C, Huws JC. First-hand accounts of sensory perceptual experiences in autism: a qualitative analysis. Journal of Intellectual & Developmental Disability. 2003;28(2):112-21.
- White BB, White MS. Autism from the inside. Medical Hypotheses. 1987;24(3):223-9.
- Williams D. Like colour to the blind. London: Jessica Kingsley Publishers Ltd; 1999.
- Ludlow AK, Wilkins AJ. Case report: color as a therapeutic intervention. Journal of Autism and Developmental Disorders. 2009;39(5):815-8.
- Ludlow A, Wilkins A, Heaton P. Colored overlays enhance visual perceptual performance in children with autism spectrum disorders. Research in Autism Spectrum Disorders. 2008;2(3):498-515.
- Fong KNK, Ma WY, Pang HK, Tang PPK, Law LLF. Immediate effects of coloured overlays on the reading performance of preschool children with an autism spectrum disorder using eye tracking. Research in Developmental Disabilities. 2019;89:141-8.
- Whitaker L, Jones C, Wilkins A, Roberson D. Judging the intensity of emotional expression in faces: the effects of colored tints on individuals with autism spectrum disorder. Autism Research. 2016;9(4):450-9.
- Ludlow AK, Giannadou A, Franklin A, Allen PM, Simmons DR, Wilkins AJ. The possible use of precision tinted lenses to improve social cognition in children with autism spectrum disorders. Vision Research. 2020;170:53-9.
- Evans BJ. The need for optometric investigation in suspected Meares-Irlen syndrome or visual stress. Ophthalmic & Physiological Optics. 2005;25(4):363-70.
- Wilkins A, Allen PM, Monger LJ, Gilchrist JM. Visual stress and dyslexia for the practicing optometrist. Optometry in Practice. 2016;17(2):103-12.
- Evans BJ, Allen PM. A systematic review of controlled trials on visual stress using intuitive overlays or the intuitive colorimeter. Journal of Optometry. 2016;9(4):205-18.
- The College of Optometrists. Precision Tinted Lenses. 2022. [Available from: https://www.college-optometrists.org/clinical-guidance/using-evidence-in-practice/precision-tinted-lenses. Accessed: 13th June 2022]
