The BCLA CLEAR scleral publication provides a brief historical review of scleral lenses and an account of contemporary scleral lens practice including common indications and recommended terminology. The report illustrates in detail recent research on ocular surface shape, scleral lens fitting, on-eye evaluation, instrumentation, contact lens management, the importance of practitioner intercommunication and collaboration in a scleral lens practice. The paper also explores the potential future application of scleral lenses. This article follows a similar structure to the paper, with a focus on how to optimise patient outcomes in modern scleral lens practice.
Scleral Contact Lenses
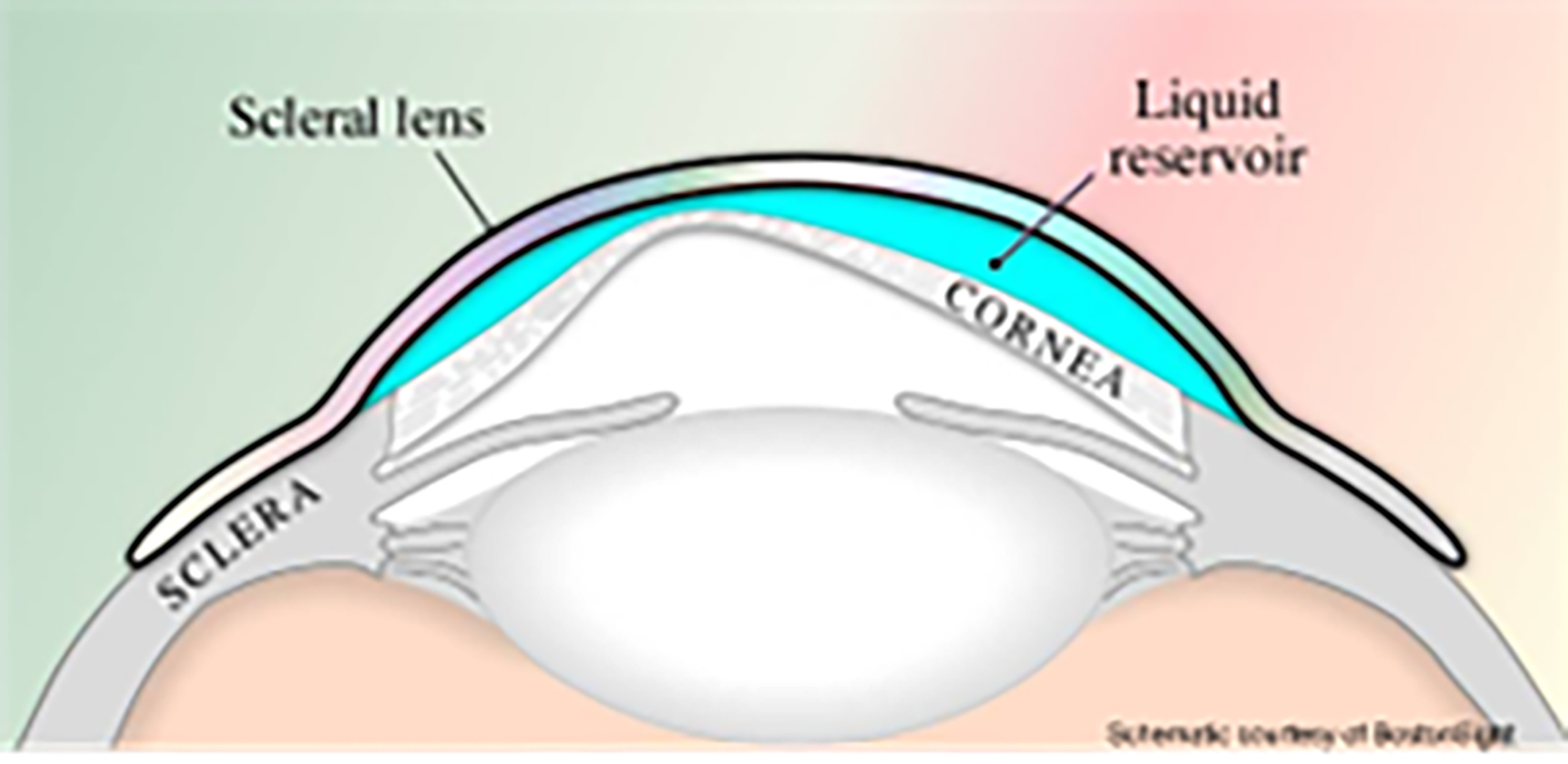
A scleral lens can be defined as a lens fitted to vault over the entire cornea, including the limbus, and lands on conjunctiva overlying the sclera (figure 1).
Scleral lenses fitting is gaining popularity and evolving as a stable platform for a range of optical applications including wavefront guided corrections, low vision aids and smart scleral lenses. Understanding on review of the literature how to apply an evidenced-based approach is key to success and discussed in this article.
Figure 1: Schematic representation of a scleral lens on eye
Scleral Lens Indications
Since the 1980s, indications for fitting scleral lens included the following:
- High ametropia: 44% of fits, primarily for aphakia and myopia
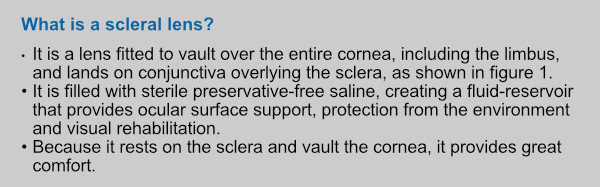
- Primary corneal ectasia: 32% of fits, for keratoconus, pellucid marginal degeneration and keratoglobus (figure 2)
- Post-penetrating keratoplasty: 12% of fits (figure 3)
- Ocular surface disease (7%)
Figure 2: Keracotonus

Modern scleral lens indications (and their percentage prevalence) are as follows:
- Primary corneal ectasia (53%)
- Ocular surface disease (18%)
- Post-penetrating keratoplasty (17%)
In addition to these, scleral lenses are also used to correct simple refractive errors, including presbyopia.
Figure 3: Post-penetrating keratoplasty
Scleral Lens Terminology
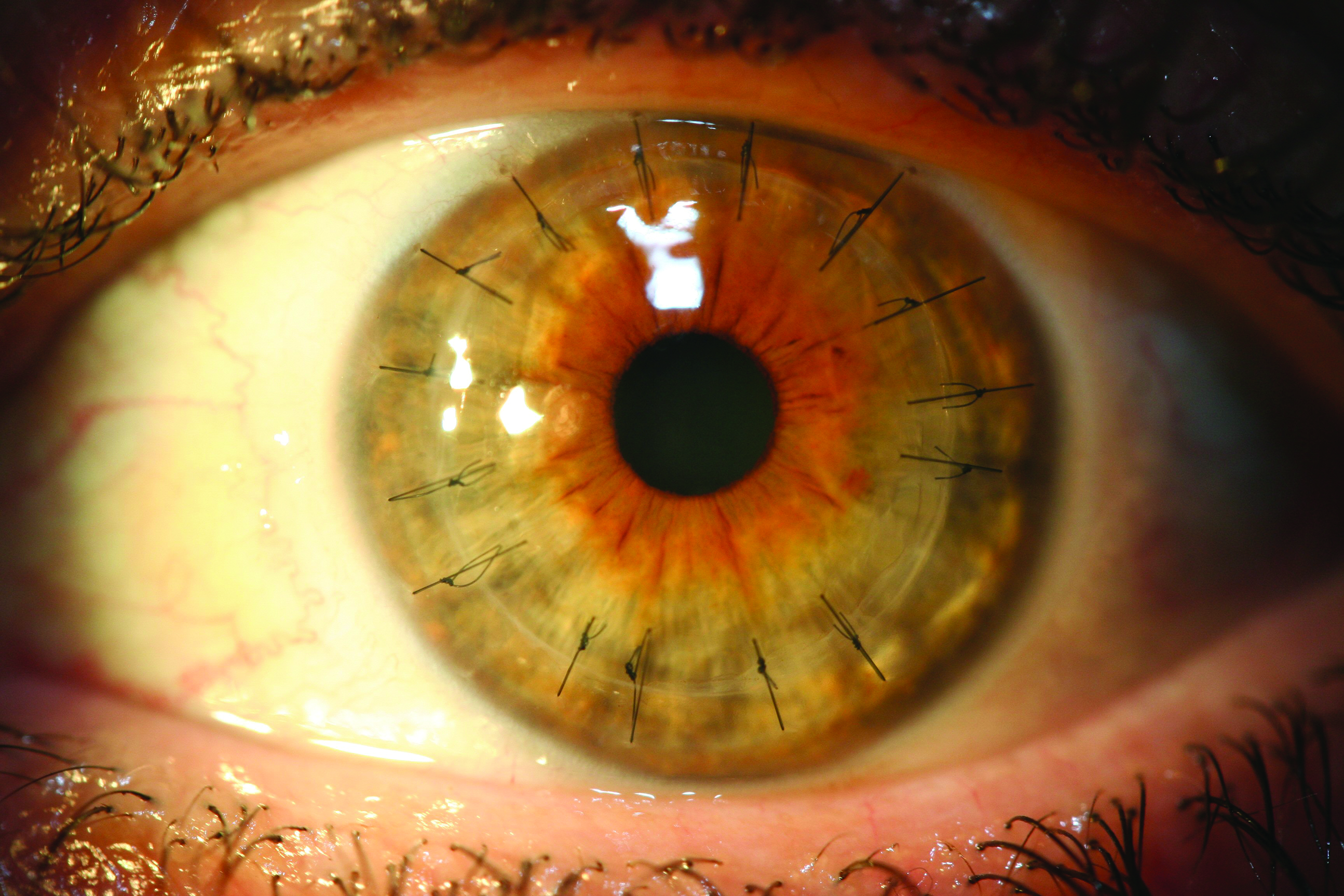
Scleral lenses have three zones as follows and as shown in figure 4 (Scleral lens zones; Image credit: Daddi Fadel):
- Optic zone: this houses the refractive correction of a scleral lens and can be customised similarly to rigid corneal lenses
- Transition zone; this connects the optic and landing zones and is often referred to as the limbal, peripheral, or intermediate zone
- Landing zone; this contacts the conjunctival tissue overlying the sclera and may be spherical, toric, quadrant, multi-meridian specific or completely customised based on an ocular impression
Ocular Surface Shape
Understanding of the ocular surface shape and elevation has contributed greatly to current knowledge about scleral lens design and fitting. Of particular importance is an understanding that back surface landing customisation improves fitting outcomes and also improves patient comfort, vision, increases wear time and enhances patient satisfaction.
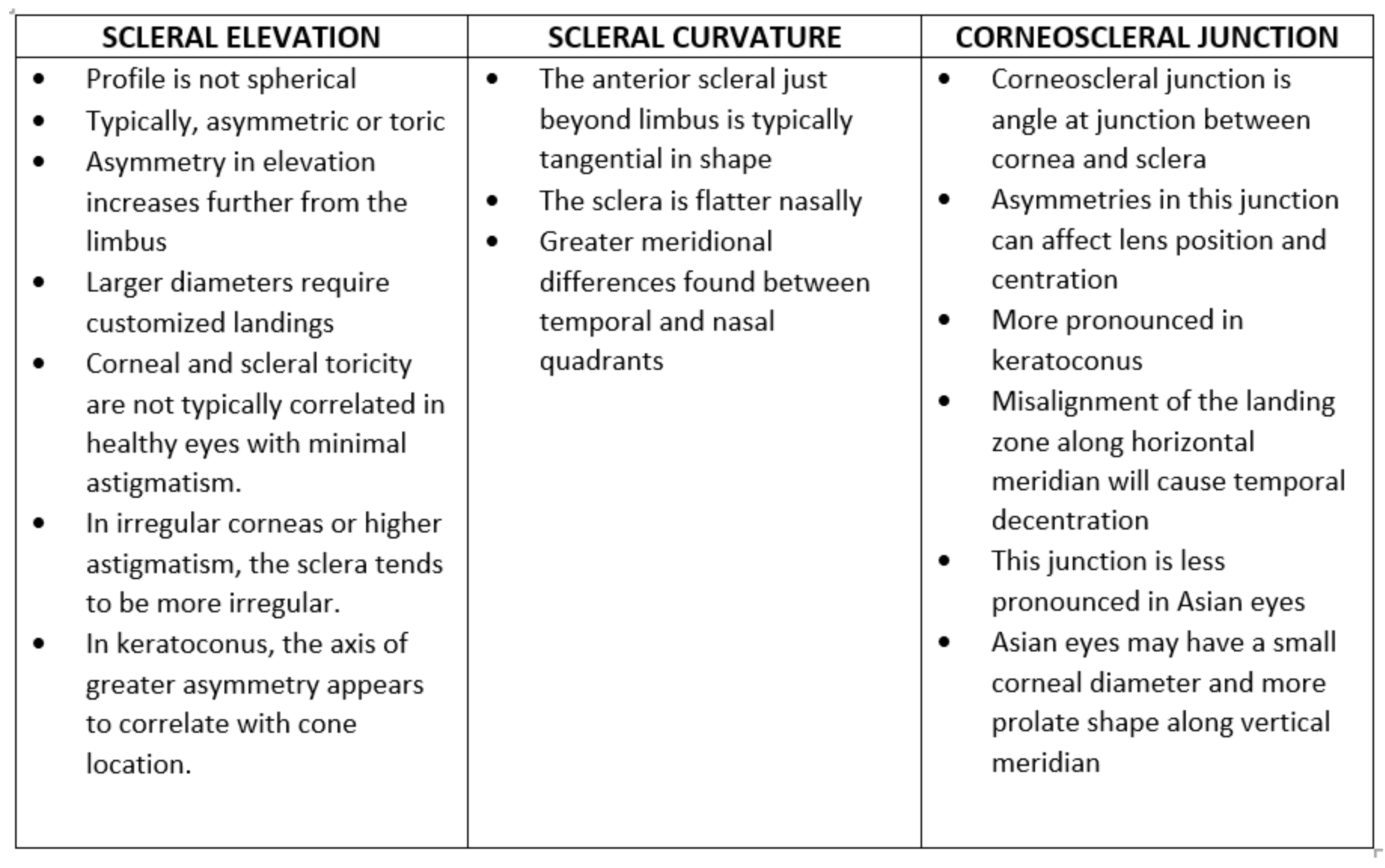
When it comes to ocular surface shape, three main areas to consider are:
- Scleral elevation
- Scleral curvature
- Corneoscleral junction
Key points about each of these are summarised in table 1:
Instrumentation
There are various tools and instruments that can help with ocular health assessment and monitoring, scleral lens fitting and troubleshooting. Most important are shown in figure 5 and are:
- Corneoscleral profilometers and topographers
- Optical coherence tomography
- Anterior segment photography
- Specular microscopy
Figure 5: Instrumentation helpful for scleral lens fitting and assessment. (Left to right) (a) Eaglet-Eye Eye Surface Profiler wide-field topography: (b) Anterior OCT to measure scleral lens clearance (image credit: Sophie Taylor-West)
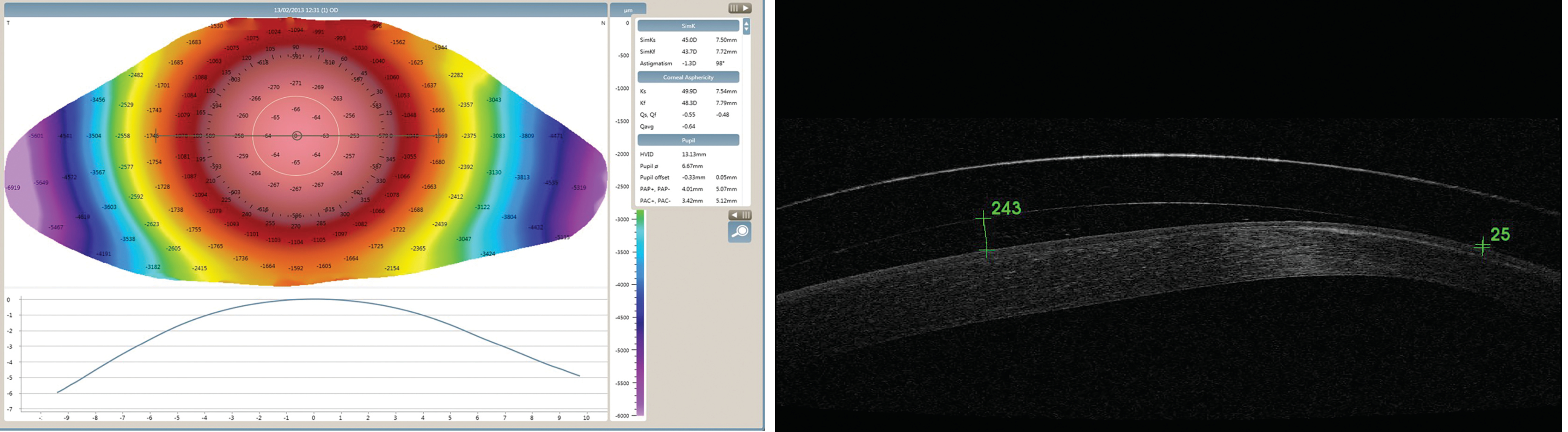
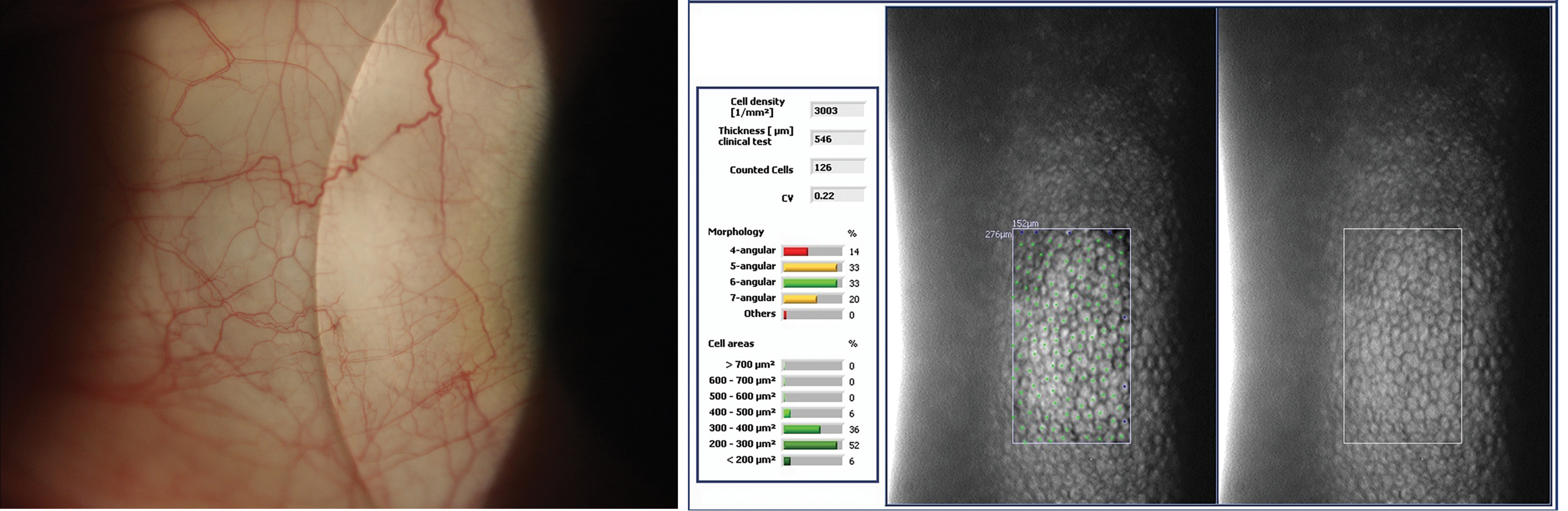
Figure 5: (Left to right) (c) Anterior segment photography of scleral lens blanching (image courtesy of Sophie Taylor-West): (d) Specular microscopy of endothelial cells
Optical coherence tomography is helpful in scleral lens fitting and troubleshooting, given the wide range of applications. From first trial lens identification, based on sagittal height at a specific chord diameter, to quantifying fluid reservoir thickness. The applications go beyond the fit, by also allowing the clinician to quantify response regarding corneal oedema, fluid reservoir debris and conjunctival tissue compression.
Anterior segment photography, via a camera coupled to a slit-lamp biomicroscope, is one of the most versatile tools to assess and monitor multiple areas of a scleral lens fitting journey. Not only is assessment and troubleshooting of the fit possible, but also assessment of the impact of the fit on the ocular health, monitoring disease progression or allowing improvements at the ocular surface (cornea, conjunctiva, lids) by objectively capturing images at different time points.
Specular microscopy utilises specular reflection to evaluate corneal endothelial cell morphology. This is especially useful when fitting grafted corneas or other compromised corneas with scleral lenses as it can provide insights regarding lens tolerance. Even when it has been reported that corneal endothelial morphology is influenced by short and long-term wear, there is no established threshold for specular microscopy metrics that would contraindicate lens wear.
Prescribing Scleral Lenses
There are various approaches to scleral lens fitting and lens prescribing. The main approaches and techniques are as follows:
- Empirical
- Impression-based
- Diagnostic
Empirical and impression-based fittings today rely on ocular surface elevation data to design the first pair of lenses, without necessarily applying a trial lens at the first visit. These techniques aim to reduce chair time with higher first fit success rates. Some practitioners may still require the application of trial lenses to obtain refractive data, but usually that can be obtained from previous rigid corneal lens data. If the conjunctival surface is negatively impacted from previous scleral lens wear, these techniques usually require cessation of lens wear for a few days, prior to any scan/impression acquisition.
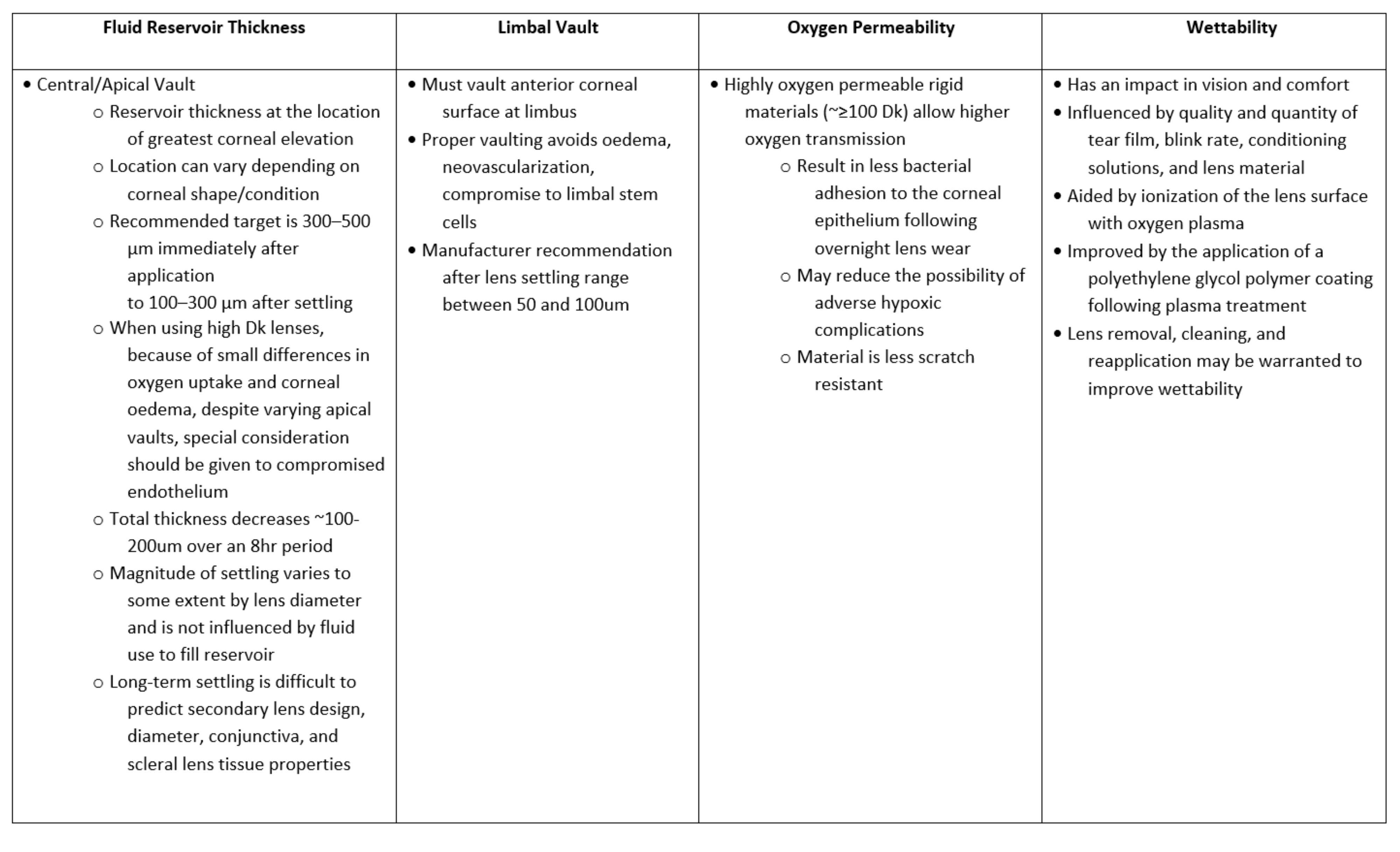
Despite the advent of new technologies, diagnostic lens fitting continues to be used by many clinicians. When using diagnostic lenses, the recommendation is to first focus on the lens diameter, then the sagittal height, and then the back surface profile. These are summarised in table 2:
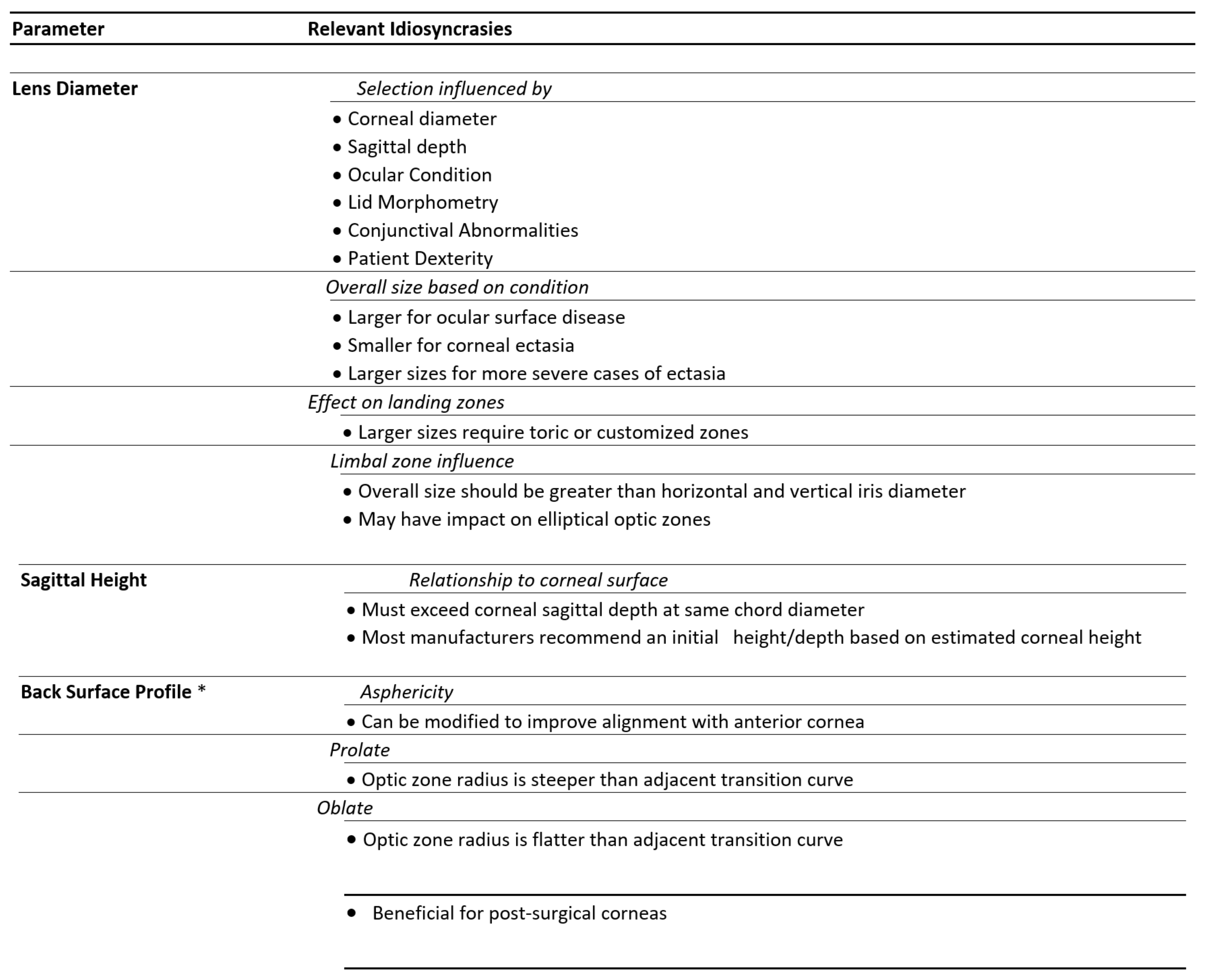
Beyond the parameters that are key for diagnostic lens fitting, there are other important fitting parameters that are important to take in consideration and these are outlined in table 3:
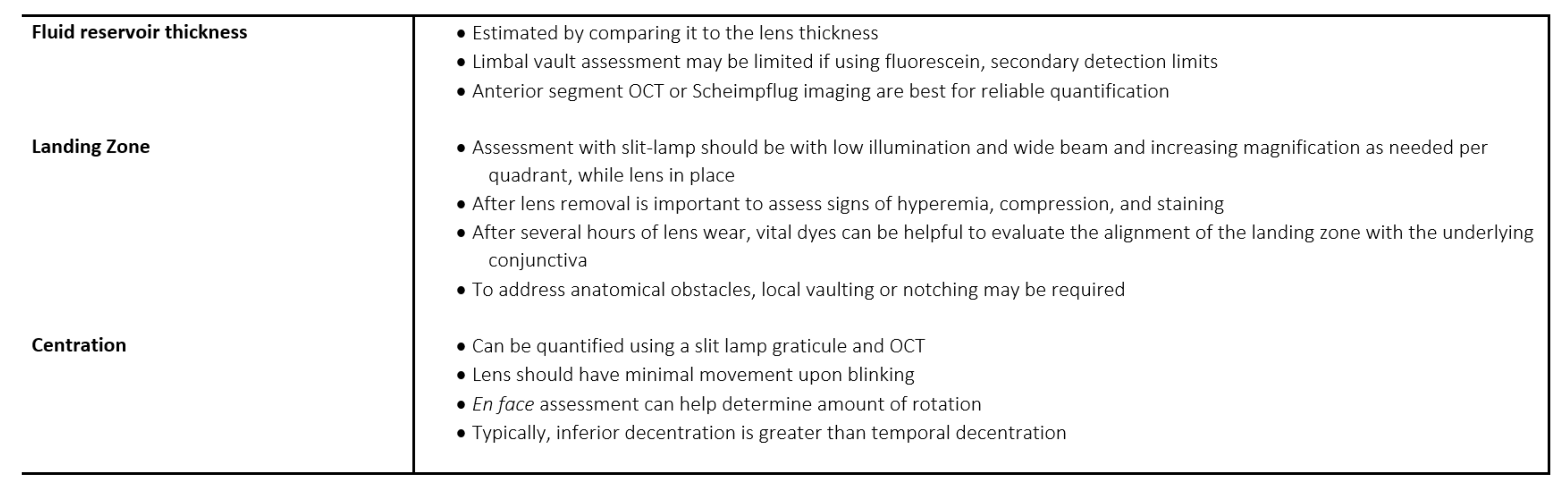
Scleral Lens Evaluation
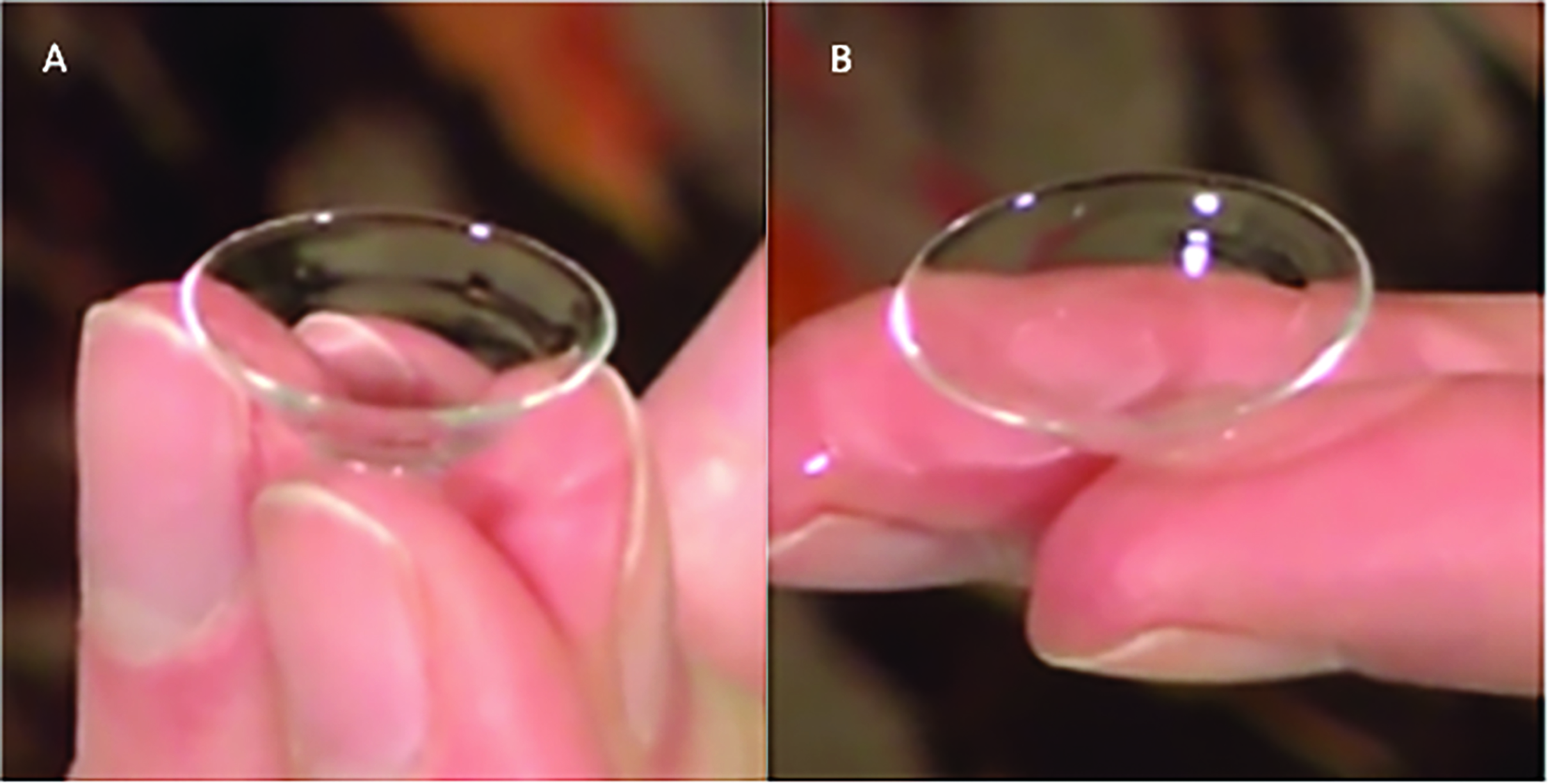
After lens application, it is recommended to confirm adequate placement, to check for bubbles (figure 6), and to assess the central vault. If bubbles are present even after correct re-application, a different diagnostic lens with more appropriate fluid reservoir thickness should be considered. When the lens is deemed to be appropriate, it is advisable to let the lens settle for about 30 minutes. After minimum settling, biomicroscopy assessment can be done in an ‘in-out’ approach to evaluate the fit from the lens centre to the edge.
Figure 6: Illustration of undesirable application bubble trapped in the fluid-reservoir compartment between the back surface of the scleral lens and the cornea. Image courtesy of BostonSight
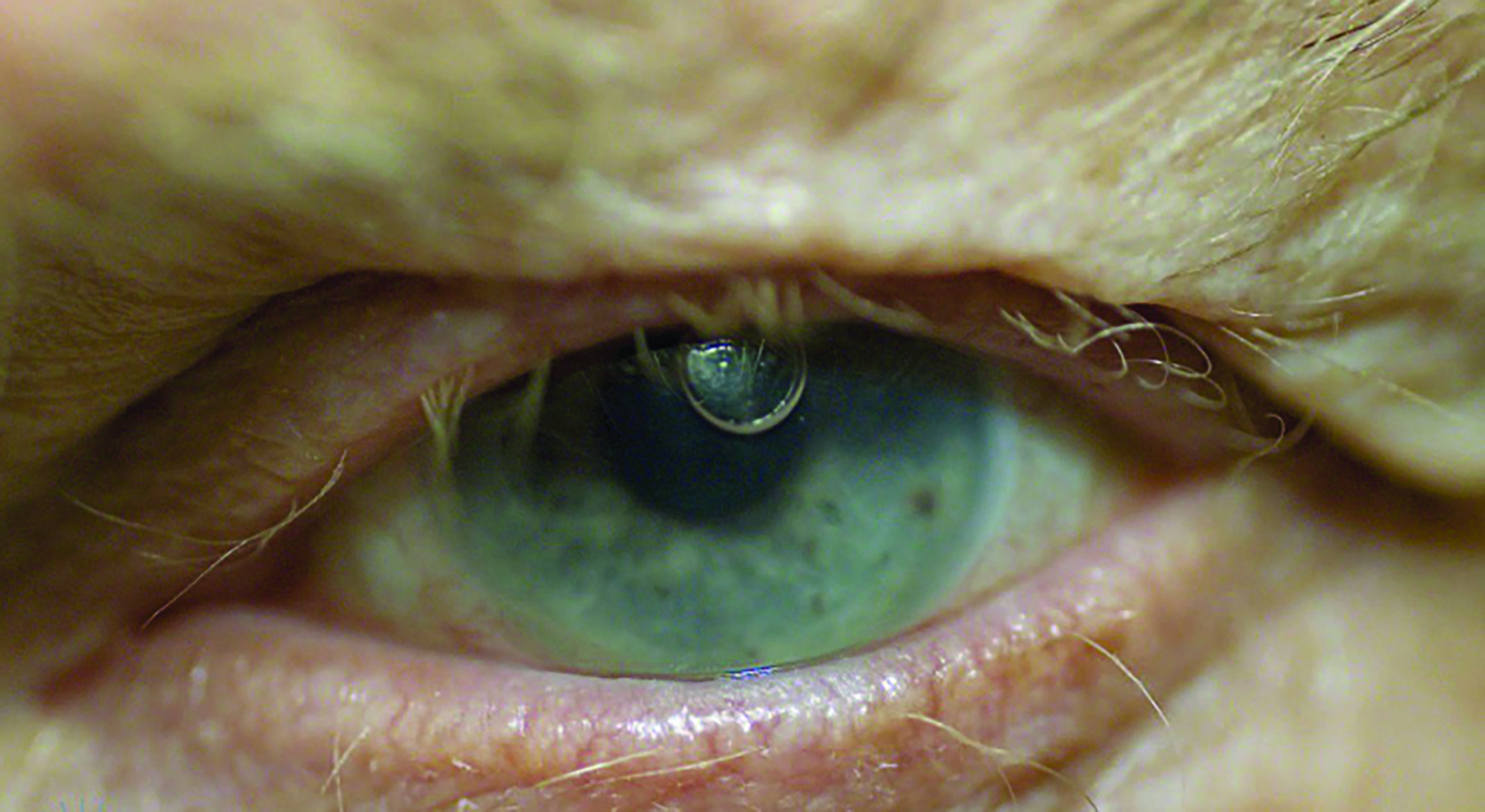
Table 4 summarises the evaluation of fitting parameters:
Scleral Lens Challenges
A number of post-fitting complications may impact successful wear and need to be addressed when they occur.
Figure 7: Two methods to hold a scleral lens for application without assistive devices. A: Tripod and B: Two-finger method. (From Scleral Lens Education Society; https://sclerallens.org/wp-content/uploads/2020/05/SLS-PATIENT-INFO-HANDOUT_02-11-2020-1.pdf)
Midday fogging
Fluid reservoir debris, otherwise known as midday fogging, is commonly encountered in 26 to 46% of patients. Midday fogging is currently managed by lens removal and reapplication, fitting modifications (improving landing zone alignment or reducing reservoir thickness), using a more viscous application fluid, and treating underlying ocular surface disease, such as blepharitis and MGD, allergies and dry eye disease.
Figure 8, scleral lens application assisted by holding scleral lens in a large suction cup/plunger. Picture courtesy of BostonSight:

Epithelial bogging
Corneal epithelial ‘bogging’ describes anterior corneal irregularities following scleral lens removal resulting in an uneven distribution of sodium fluorescein. Bogging is managed by daily, midday lens removal, rinsing, and reapplication and can otherwise be monitored.
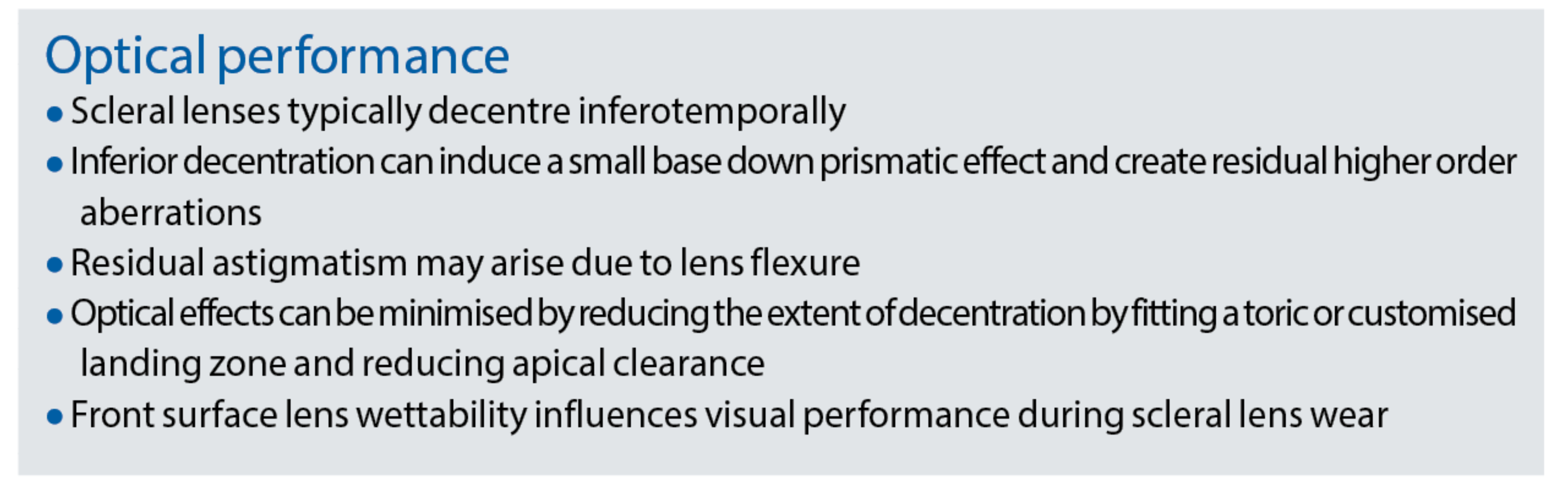
Optical considerations
Scleral lenses have been reported to have great visual rehabilitation benefits and potential, in both irregular cornea and ocular surface disease. For example, in a cohort of 422 keratoconus patients, when compared to corneal GP lenses, scleral lenses were shown to offer better vision and comfort.
Despite this, there are some fitting relationships that may have an impact on the lens optics and these need to be borne in mind by the clinician.
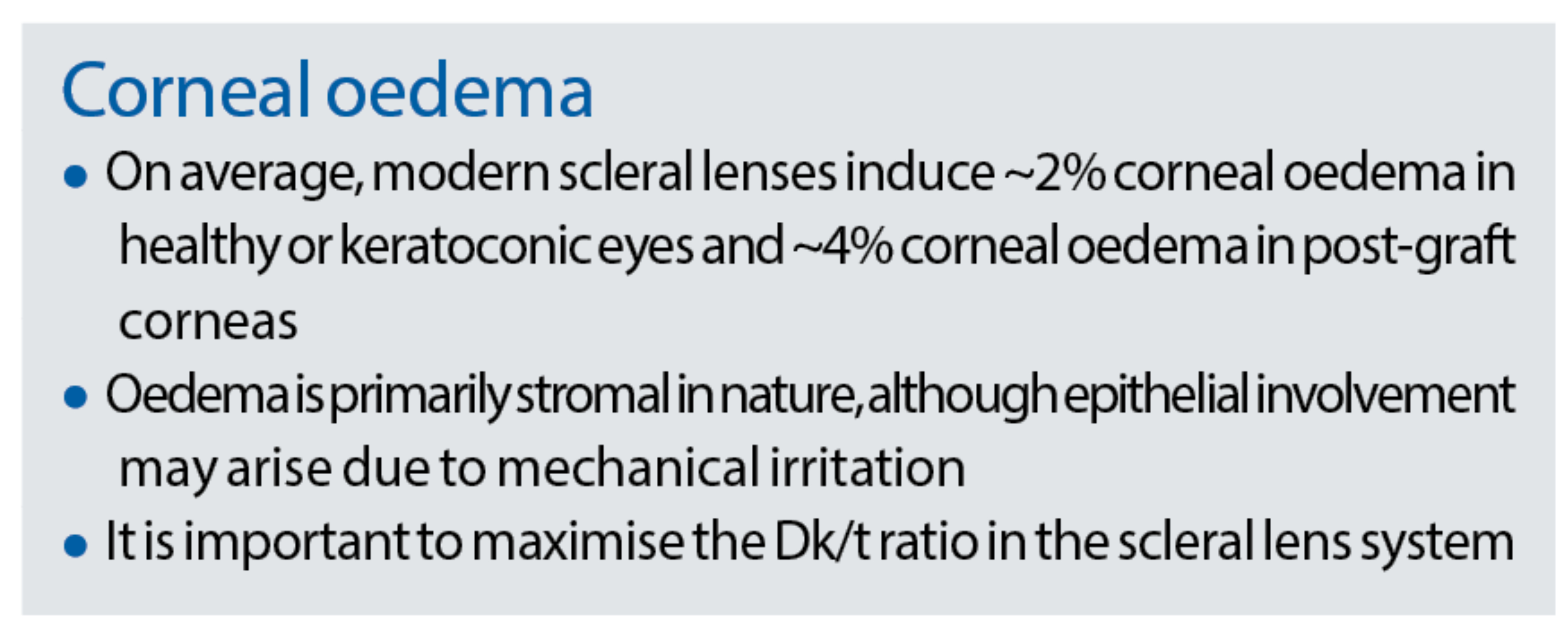
Corneal oedema
Gas permeable materials have evolved from rigid lens materials; from glass to PMMA to low Dk and then hyper-oxygen permeable rigid lens materials with a Dk of over 100. As a consequence, stromal oedema as a complication is found in fewer and fewer cases.
Conjunctival prolapse
Both compression and suction forces may contribute to conjunctival prolapse, defined as an elevation of the perilimbal conjunctival tissue that may encroach the limbus. This phenomenon is often benign and can be monitored, although long-term effects unknown. Usually, it occurs as a result of excessive clearance at the limbus and therefore reducing limbal clearance usually helps to resolve the problem.
Scleral Lens Application and Removal
Scleral lens handling is reported to be more difficult than rigid corneal lenses and is the primary reason for scleral lens drop-out. According to one study, challenges with scleral lenses handling was 63% compared to 40% in rigid corneal lens wearers.
Collaborative Care
As the scope of eye care practice continues to expand, sub-specialisation has become increasingly necessary and practical. Scleral lens practice is a sub-specialty requiring a specific skillset beyond the scope of primary eye care. Effective practitioner inter-communication and collaboration is critical for appropriate referrals, co-management and treatment outcomes for wearers.
Intra-optometric referrals
Intra-profession referrals are becoming more common based on increasing sub-specialties. In addition to the skillsets needed to analyse and modify scleral lenses, customised technology (such as corneoscleral topography and anterior segment OCT) may be required to provide the highest quality care. Managing patient’s expectations of the scleral lens fitting process, offering unique education and explaining the need for regular review, is important. Ensuring the practice is set up accordingly with a well-trained team and, at times, seeking advice or referral to more experienced colleagues may be beneficial.
Co-management
When fitting the practitioner should be knowledgeable about not only contact lens options, but also disease management strategies. In some situations, patients require co-management and collaboration to optimise outcomes for scleral lens wearers. Scleral lens practitioners may need to collaborate with various specialists, typically corneal specialists involved with the management of penetrating keratoplasty, glaucoma specialists and cataract specialists. Other specialists liaised with include oculoplastic, low vision and ocular oncology specialists.
A wide range of systemic diseases can present with ocular manifestations which are managed by scleral lens wear. Collaboration with medical specialties is sometimes required, such as rheumatologists, oncologists, endocrinologists and neurologists. The most common diseases to be managed with scleral lenses include:
- Ocular graft-versus-host disease (figure 9)
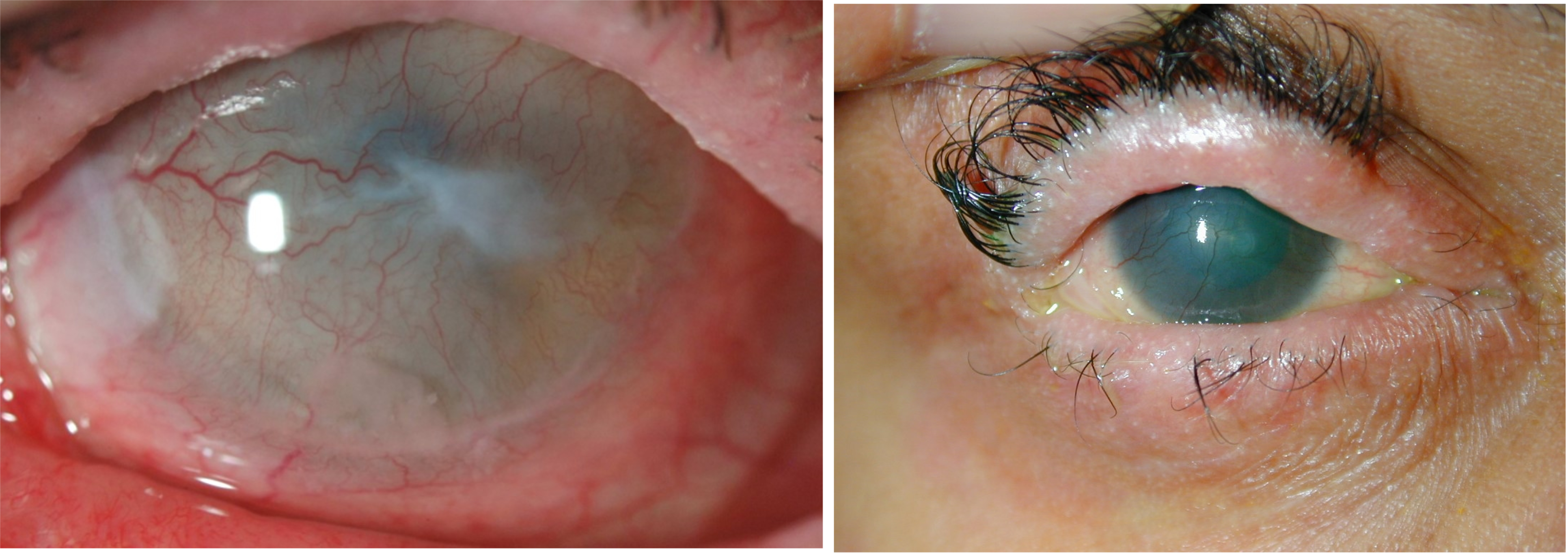
- Stevens-Johnson syndrome (figure 10)
- Sjögren’s Syndrome
Figure 9: Cornea showing signs of superficial keratitis and filamentary keratitis in graft-versus-host disease. (Image credit BostonSight)
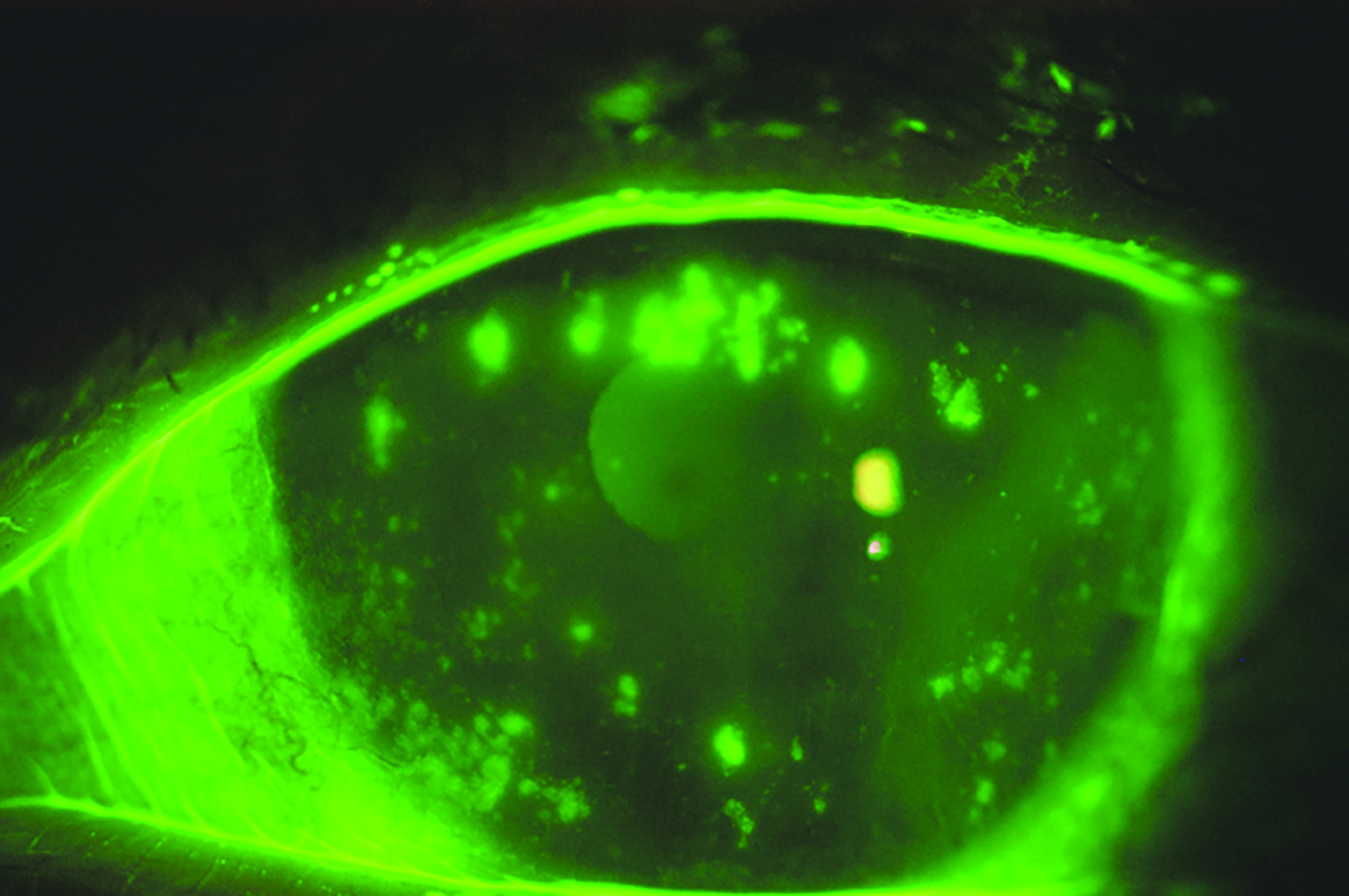
Figure 10: Two examples of Stevens-Johnson syndrome. (Images credit BostonSight (left) and Dr Dan Rosser (right))
Scleral Lens Platforms
Scleral lenses are currently being used as a stable platform for a range of optical applications including wavefront guided corrections and low vision aids.
Wavefront guided corrections. Although scleral lenses neutralise a significant proportion of anterior corneal optical anomalies, patients may still experience sub-optimal vision due to aberrations arising from the posterior corneal surface or the crystalline lens. To eliminate non-rotationally symmetric higher-order aberrations such as coma (which is common in keratoconus), a customised wavefront guided front surface design is required.
Low vision aids. A reflecting telescopic system embedded within a scleral lens can rapidly alternate between unmagnified and 3x magnification in response to controlled blinks and has potential applications in low vision rehabilitation. However, no in vivo data has been published to date.
Future direction
The BCLA CLEAR scleral lens review concludes by identifying several avenues where collaboration in patient care can improve outcomes, particularly in penetrating keratoplasty. Also covered alongside the use of scleral lenses as a platform for wavefront guided vision correction, largely due to the stability that scleral lenses provide, is their potential as smart devices, which might include biometric readers providing a simulated iris or augmented reality.
Conclusion
Various unique physiological responses may occur with scleral lenses. In general, they are safe with a low incidence of microbial keratitis when worn on a daily wear basis.
An understanding of scleral lens anatomy and ocular surface shape is necessary to optimise lens design, vision and comfort, and ocular physiology for each individual eye. Either empirical or diagnostic lens fitting can be performed; instrumentation can assist with scleral lens fitting and troubleshooting.
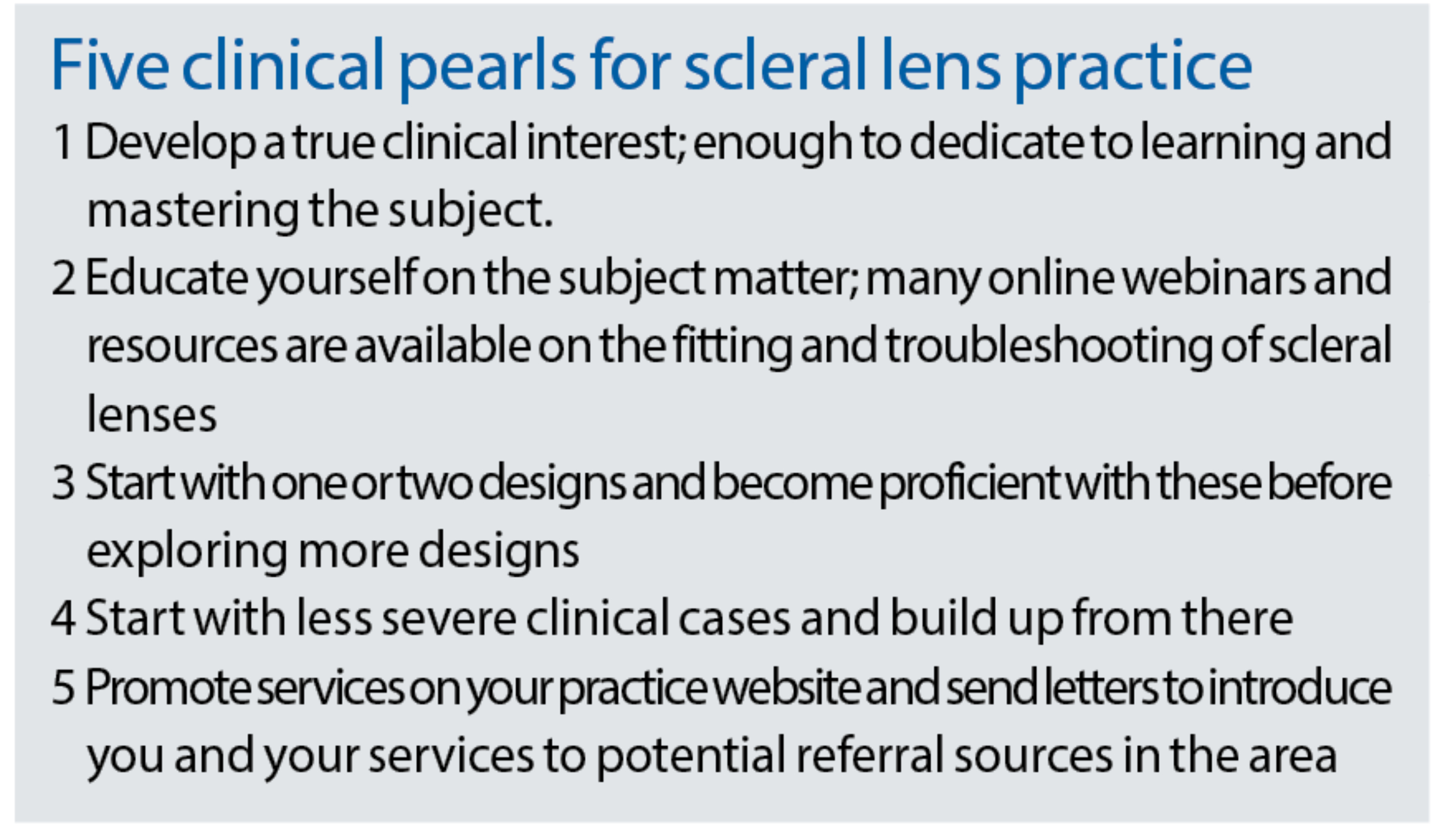
In summary, scleral lens fitting can be extremely rewarding and provide many benefits to the wearer beyond refractive correction alone. Following the clinical pearls and reviewing the latest published literature are a good starting point for those new to scleral lens work. Practitioner collaboration and intercommunication is essential in a scleral lens practice to maximizing success.
- Dr Melissa Barnett is a principal optometrist at the University of California, Davis Eye Center. She is Chair of the American Optometric Association Contact Lens and Cornea Section, a Fellow and Global Ambassador of the British Contact Lens Association, and is Past President of the Scleral Lens Education Society
- Dr Karen G Carrasquillo is Vice President of Clinical and Professional Affairs at BostonSight. In addition, she is an adjunct clinical professor at the New England College of Optometry, an adjunct clinical professor at the school of optometry, MCPHS University, Advisory Board member for the Gas Permeable Lens Institute (GPLI), Fellow of the American Academy of Optometry (FAAO), Fellow of the Educational Society of Scleral Lenses (FSLS), Fellow of the British Contact Lens Association (FBCLA), and Global Ambassador of the BCLA
•The full report and supplementary information can be accessed at: https://www.contactlensjournal.com/article/S1367-0484(21)00015-1/fulltext
•The BCLA CLEAR Summary report is a short bite-size evidenced based practical guide for clinicians, bringing together the key findings from the report. Accessed via CLEAR (bcla.org.uk)
•The editors for this series are Neil Retallic and Dr Debarun Dutta
Acknowledgements
Acknowledgement and recognition to Melissa Barnett, Claudine Courey, Daddi Fadel, Karen Lee, Langis Michaud, Giancarlo Montani, Eef van der Worp, Stephen Vincent, Maria Walker, Paramdeep Bilkhu and Philip Morgan who were the paper’s authors and the educational grants from Alcon and CooperVision.
Original paper
Barnett M, Courey C, Fadel D, Lee K, Michaud L, Montani G, van der Worp E, Vincent SJ, Walker M, Bilkhu P, Morgan PB. CLEAR - Scleral lenses. Contact Lens Anterior Eye, 44, 2021, 270-288
