The progressive nature of myopia, that children who become myopic at a young age will become more myopic as they grow, has been understood for many years and eye care practitioners (ECPs), academics and researchers have been interested in the possibility of slowing or halting the progression of myopia for at least four decades.
Background
The authors qualified in the 1980s when E-line no-jump bifocal spectacle lenses were routinely prescribed by progressive ophthalmic opticians and hospital eye departments, most often with a +2.50 add, seg heights measured to pupil centre, in order to slow the progression of ‘juvenile stress myopia’. Unfortunately, the NHS, at least as far as optics is concerned, does not see itself as a means of funding long-term experiments or treatments that may or may not be successful, so the practice of dispensing bifocal spectacles to children (except those with convergence excess) all but ceased for many years.
However, in other markets and in academic circles, interest in managing the progression of myopia did not abate, and has undergone a resurgence in the recent past as it has become clear that myopia worldwide is reaching epidemic proportions. Myopia is predicted to have prevalence of 50% worldwide by 2050 with one in 10 having high myopia (standardised to spherical equivalent of -5.00D and greater). High myopia dramatically increases the risk of serious sight threatening pathology, retinal detachment, myopic maculopathy, cataract and glaucoma.1 It is evident that reducing myopic progression is likely to improve quality of life for myopes and reduce the public health burden. Slowing myopia such that the final prescription is even 1.00D less can reduce the incidence of myopic maculopathy by 40%.2
In the past few years, a number of optical appliances and medical interventions have been introduced that claim to be able to treat myopia progression. The General Optical Council Standards of Practice for Optometrists and Dispensing Opticians place a number of obligations on registrants (figure 1) to stay abreast of the latest developments and communicate these effectively to patients. It is vital, if patients (or parents/carers) are to be given informed choice, and opticians are to obtain patients’ valid consent when dispensing spectacles or fitting contact lenses, that they are apprised of the most up-to-date research evidence and are able to outline the absolute and relative risks, and likely outcomes, of the various alternative treatments and lifestyle adjustments that have been shown to be beneficial.
Figure 1: GOC Standards of Practice relating to professional responsibility
Discussion of risk factors
For any disease, understanding the risk factors is essential for prevention and the development of treatments as well as determining public health policies. The more complex aetiology of myopia having both genetic, environmental, and visual components means the development of treatments and preventative interventions are considerably more challenging as linking a clear causal connection with a defined mechanism is difficult.
Randomised controlled trials (RCTs) are considered the gold standard for establishing cause and effect but are very expensive and often not ethical, so evidence is often from longitudinal observational studies. The two major controllable risk factors for myopia identified by the International Myopia Institute (IMI) are restricted access to education and limited time outdoors.3 There is a professional responsibility for optometrists and dispensing opticians to be able to hold discussions with patients and answer questions related to myopia risk factors.
Time spent outdoors
By increasing time spent outdoors the onset of myopia can be delayed but whether it slows progression of already myopic eyes is questionable.1 The suggested mechanism being the release of dopamine from the retina stimulated by brighter daylight conditions that acts as an inhibitor for eye growth.
Using elevated ambient light levels in classrooms has been shown to have a protective effect against myopia4 with one study going a step further using the concept of a ‘bright classroom’ whereby construction consisted of glass walls and ceilings to increase light exposure and intensity. This approach clearly presents significant cost implications.5 Taking a different approach, a recent multi-centre RCT using low-level red-light therapy (650nm) to bring light straight to the retina for myopia control achieved promising results.6
Discussions with patients should include explaining the protective effect of increasing time spent outdoors since children spending less than two hours per day outside are significantly more likely to develop incident myopia than children who spend more than three hours per day. This (free) treatment is sometimes hard to persuade parents and patients of, since the evidence suggests an increase of approximately 76 minutes per day on average is what would be needed to give a 50% reduction in incident myopia7 and an hour per day yields a 45% reduction. This may be easier said than done, especially during the winter months when daylight hours are short.
Additionally, although some of the studies referenced mention ‘bright daylight’ others are not clear whether ‘time outdoors’ means time during daylight hours, or whether outdoor distance vision tasks, such as playing football under floodlights in the evening or walking the dog under street lighting, also counts.
That said, outdoor exercise has the added advantage of improving a child’s physical and mental health and even when a myopia management treatment is prescribed patients and parents should be advised that the effect of time outdoors is still of benefit and must be encouraged in order to maximise the efficacy of any given treatment. Advice on lighting while inside should also be discussed as this is something often overlooked.
Education
Evidence supporting a causal association between more education and more myopia is consistent,1 especially when considered alongside results using Mendelian randomisation analyses that each year of additional education is associated with a more myopic refractive error of -0.27DS,8 although it is hard to say whether this is also due to less time outdoors. The mechanism for this risk remains unclear, near work may be a factor9 particularly when working distances are very short (≤20cm) and reading is continuous (≤45minutes).10
Advising the importance of regular sight tests for children should also not be overlooked, a recent study of children in Essex found only 34.3% of patients under 16 years old had a sight test over an 18-month period.11
Parental myopia
The IMI clinical management report suggest a threefold increased risk of developing myopia for children with two myopic parents compared with children who have no myopic parents. There is differing evidence presented on the odds ratio for parental myopia as a risk factor and readers should be aware when reviewing this evidence that environmental factors like time outdoors and education can act as confounders influencing results. The effect of parental myopia has often been used to infer evidence of a genetic link but may be more based on a shared lifestyle where the environment is more predisposed to myopia.
It is important that optometrists and dispensing opticians critically appraise research in particular looking at sample groups, ethnicity, duration of the study and measurement methods used.
Predicting Myopia Onset and Progression (PreMO): an evidence-based risk indicator for eye care practitioners is a useful aid when discussing myopia that uses a traffic light system to indicate a child’s risk of developing myopia and for children that are already myopic their risk of myopic progression.
Definitions and classifications
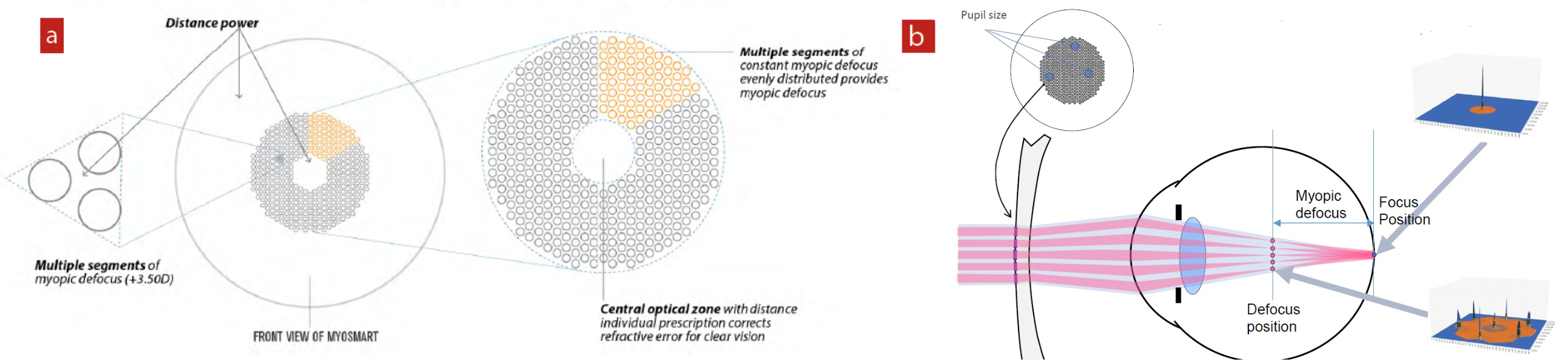
Table 1 summarises the terminology and the proposed general and quantitative thresholds for myopia proposed by the Interventions for Controlling Myopia Onset and Progression Report from the International Myopia Institute (IMI).12
Table 1: IMI definitions and classifications of myopia12 (note: high myopia defined as ≤ -6.00D using mathematically valid descriptors, meaning more myopic than -6.00D)
The DREAM study13 followed myopia progression until age 25 years in 2,555 European children finding children that were -3.00DS or worse before age 10 years all developed high myopia. Those adults with high myopia were the faster progressors during childhood. Clearly, early childhood is the opportune time for myopia management interventions particularly for children who are at risk of developing high myopia. The IMI identified the term pre-myopia shown in (table 1) and the CLEERE study found that children with a refraction of less than +0.75DS of hyperopia at six years of age have an increased risk of developing myopia.14
Current thinking
A striking feature of all the recent myopia studies is the remarkable consistency in the myopia progression in the control groups of children wearing standard single vision spectacle lenses. Annual progression rates average -0.50DS to -0.75DS and are consistent with in practice experience that primary school age myopic children, tested every six months, tend to experience a -0.25DS or -0.50DS change at every sight test. The aim of myopia management is, obviously, to reduce this myopic progression and a plethora of optical and non-optical interventions are currently under investigation with new treatments being launched every few months in the past few years.
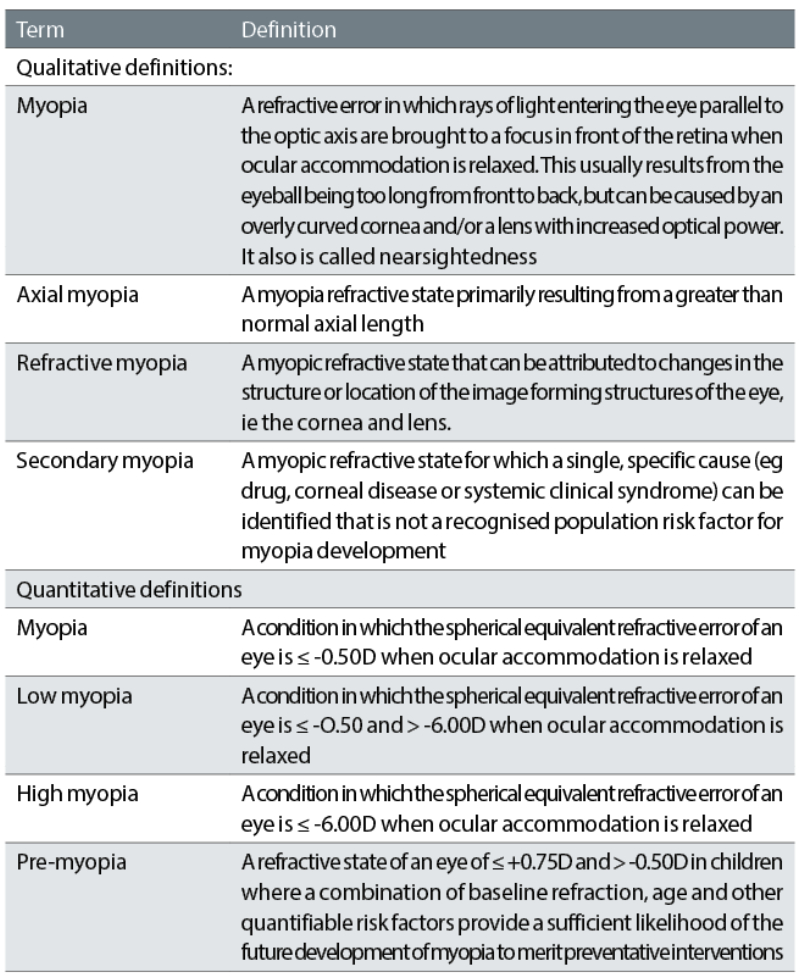
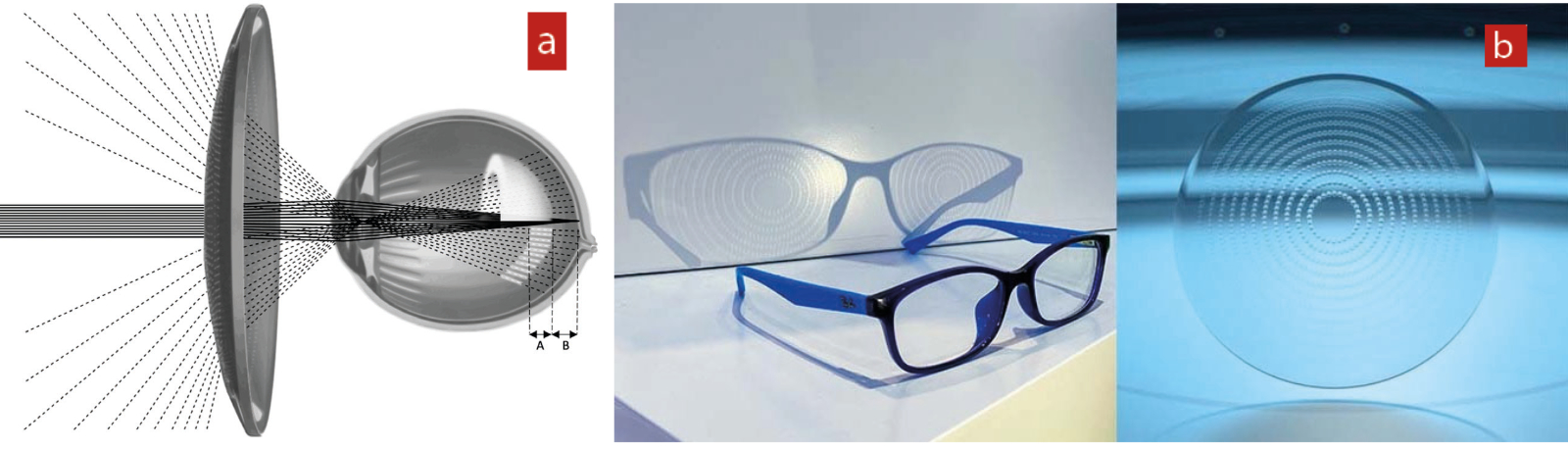
The theory upon which current successful optical interventions to reduce myopia progression are based is the peripheral defocus theory where the peripheral retinal refraction is considered to play a significant role in driving eye growth.16-18 Current optical interventions simultaneously present a clear foveal image as well as at the same time creating a myopic defocus image shell in the peripheral retina (figure 2).
Figure 2: Peripheral myopic defocus
Relative peripheral hyperopia was observed one year before myopia onset in white children and three years before in Asian children supporting the theory that relative peripheral hyperopia is a driver not an effect of myopia.18
Current spectacle lens designs
Hoya Miyosmart lens
Hoya’s lens was the first specialist myopia management spectacle lens to launch in the UK and has been subject to a number of studies to date with increasing longitudinal data demonstrating its benefit. It is a sign of the rapid changes in this field that four years’ data is considered significant.
Lens design
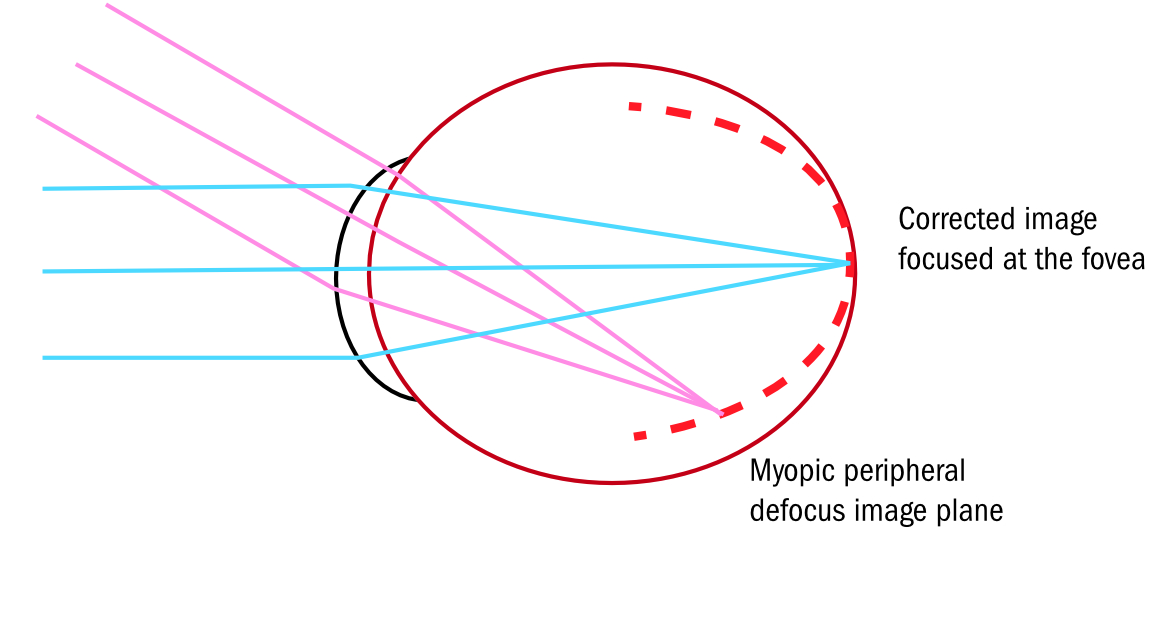
Miyosmart provides simultaneous clear foveal vision with peripheral retinal myopic defocus to slow eye growth by defocus incorporated multiple segments (DIMS).19
A simultaneous vision spectacle lens with a 9mm hexagonal central distance zone surrounded by a ring of micro lens segments (lenslets), which creates 3.50D of myopic defocus (+3.50D Add) and maintains a 50:50 ratio of focus and defocus. Lenslets are discreet, only visible if the lens is tilted and a light source used to show the multiple segments by reflection (figure 3).
Figure 3: The design of the Defocus Incorporated Multiple Segments (DIMS) spectacle lens. (a) The distribution of the defocusing lenslets. (b) the creation of the defocus zone. (c) The appearance of the lens

Evidence
Lam et al19 first published results form a two-year, double-masked RCT of Chinese children aged eight to 13 years; primary outcome measurements cycloplegic refraction (spherical equivalent refraction, SER) and axial length, the greatest effect was seen in the first six months but over the two-year trial the mean myopic progression in the DIMS group was -0.41DS and -0.85DS in the control single vision group. The mean changes in axial length were 0.21mm in the DIMS group and 0.55mm in the single vision group.
A total of 21.5% of children wearing the DIMS lens had no myopia progression over two years compared to 7.4% in the single vision control group. Constant wear of spectacles was achieved in both subject groups (around 15 hours).
There was no significant differences in visual function of children wearing the DIMS lens compared to those wearing single vision lenses although it was accepted that further studies were required covering a longer time period.20 Changes in the relative peripheral refraction (RPR) between the two groups were observed with the single vision group showing an increase in hyperopic RPR but for the children in the DIMS group there was no significant change suggesting a more uniform slower eye growth.21
Lam et al 202222 published three-year results of the children who had worn the DIMS lens as part of the previous trial continued to wear DIMS and the children in the single vision control group switched to wearing the DIMS lens. The mean annual progression in the original DIMS group was -0.18D and 0.10mm, the control-to-DIMS group showing -0.30D and 0.12mm.
Lens fitting
Lenses are measured in the same way as progressive lenses locating the position of monocular centration distances and vertical pupil heights. The frame needs to have a B size of more than 25mm with at least 12mm above pupil the ideal vertex distance is 10mm or less having a pantoscopic angle close to zero and a face form angle no more than 5°.
Essilor Stellest lens: Lens design
The Stellest lens by Essilor also uses the peripheral defocus theory with Highly Aspherical Lenslet Target (HALT) technology, having a central distance zone with aspherical lenslets 1.1mm in diameter spread on 11 concentric rings. Lenslet geometry has been calculated to generate a volume of myopic defocus (VoMD) placing visual signals in front of the retina following the retinal profile.23
Figure 4: (a) Lens providing volume of myopic defocus (VoMD) (white shell) in front of the retina through 11 concentric rings of contiguous lenslets, where A=depth of VoMD and B=distance from the retina. (b) Appearance of the lens23
Evidence
A two-year double-masked RCT with 170 children aged eight to 13 years and myopia between -0.75D to -4.50D subjects wore spectacle lenses with highly aspherical lensets (HAL) slightly aspherical lenslets (SAL) or single vision lenses.23 The VoMD is described in the study as instead of creating focus on two surfaces the aspherical lenses deviate light in a non-linear way creating a three-dimensional quantity of light in front of the retina. Primary outcome measurements from cycloplegic refraction SER, and axial length.
The results after one year with mean progression -0.81D in the single vision group, -0.48D in the SAL group and -0.27D in the HAL group. The two-year results showed progression slowed by 0.80D and axial length by 0.35mm in the HAL lenses, SAL lenses myopic progression 0.42D and axial length 0.18mm and for single vision lenses the fastest progression was 1.46D and axial length 0.69mm.24
The Stellest lens adopts the HAL design, which has shown to cause no significant change to visual acuity and reading speed at high contrast compared to single vision lenses although at low contrast reading speed and visual acuity were slightly reduced.25
Lens fitting
Again these lenses are measured in the same way as progressive lenses on pupil centre with monocular centration distances and vertical heights. The frame should fit flat with pantoscopic tilt kept to a minimum to avoid oblique aberrations.
SightGlass Vision DOT lenses
Use Diffusion Optics Technology having a central clear 5mm aperture surrounded by multiple dots, microscopic diffusers applied to the lens surface that scatter light and reduce peripheral retinal contrast. Each microscopic diffuser is translucent and irregularly shaped with a diameter of 0.14mm and height 0.2mm.
The mechanism for this design is that high contrast signals received by the retinal photoreceptors induce eye growth and low contrast signals slow eye growth.
The CYPRESS study,26 a 36-month double-blind multicentre RCT with three study groups (a single vision control group and two investigational groups with different densities of diffusers). The spacing between the diffusers was 0.365mm (test 1 – marketed as DOT 0.2) and 0.240mm (test 2). The SightGlass DOT 0.2 lens reduced myopia progression by 50% and the other test lens by 33%.
Current contact lens designs
MiSight 1 day
MiSight 1 day (CooperVision) a Dual focus soft daily disposable contact lens with a central distance correction zone (3.36mm) surrounded by a treatment zone creating 2.00D myopic defocus zone (+2.00DS Add) this alternating pattern is then repeated. The mechanism for this design is the peripheral defocus theory.
Evidence
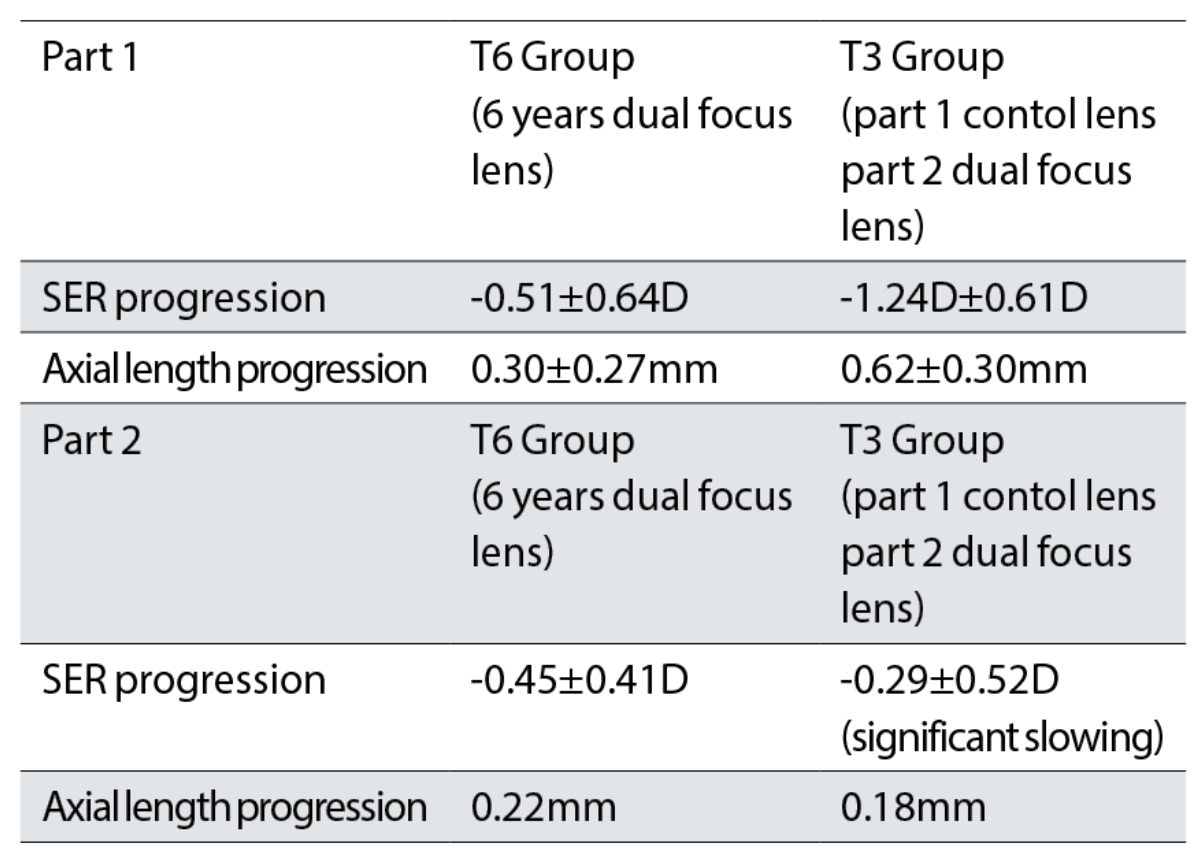
Chamberlain et al27 are responsible for the longest running continuous myopia management study spanning six years. This study began as a multicentre double-blind RCT; Part 1 with children aged eight to 12 years and Part 2 children aged 11 to 15 years, but those in the control group wearing Proclear lenses moved to the MiSight lens meaning there was no longer a control group for comparison and analysis of efficacy. T6 group children who had received six years of the MiSight treatment lens and T3 group, children who had been in the control group but switched to MiSight receiving three years of the treatment lens.
Over six years, the T6 group progressed an average of -0.92±0.87DS and the T3 group progressed an average of -1.55±0.81DS. The study highlights that, in the T6 group, 23% of eyes showed no clinically meaningful change in SER over a six-year period. The results are summarised in table 2.
Table 2: Three and six-year results for spherical equivalent error (SER) and axial length progression with the MiSight 1 day dual focus lens27
Interestingly, results from a two-year parallel group MiSight Assessment Study Spain (MASS)28 found lower efficacy results; 39.32% reduction in myopic progression and 36.04% reduced axial elongation. Recently, it was found that more time spent outdoors was the only differentiating factor between children taking part in the MASS study, as those children spending more than three to four hours per week outdoors did experience a greater effect from the treatment.29 This highlights just how important increasing time outdoors can be for myopic children.
Rebound effect
Rebound effect has been an issue of concern with atropine and orthokeratology myopia management interventions, but cessation of Misight 1 day lens over a one year period found no rebound effect.30 This concurs with the opinion that intervention by altering retinal image profile is a more natural, less invasive, approach and unlikely to produce rebound effects.31
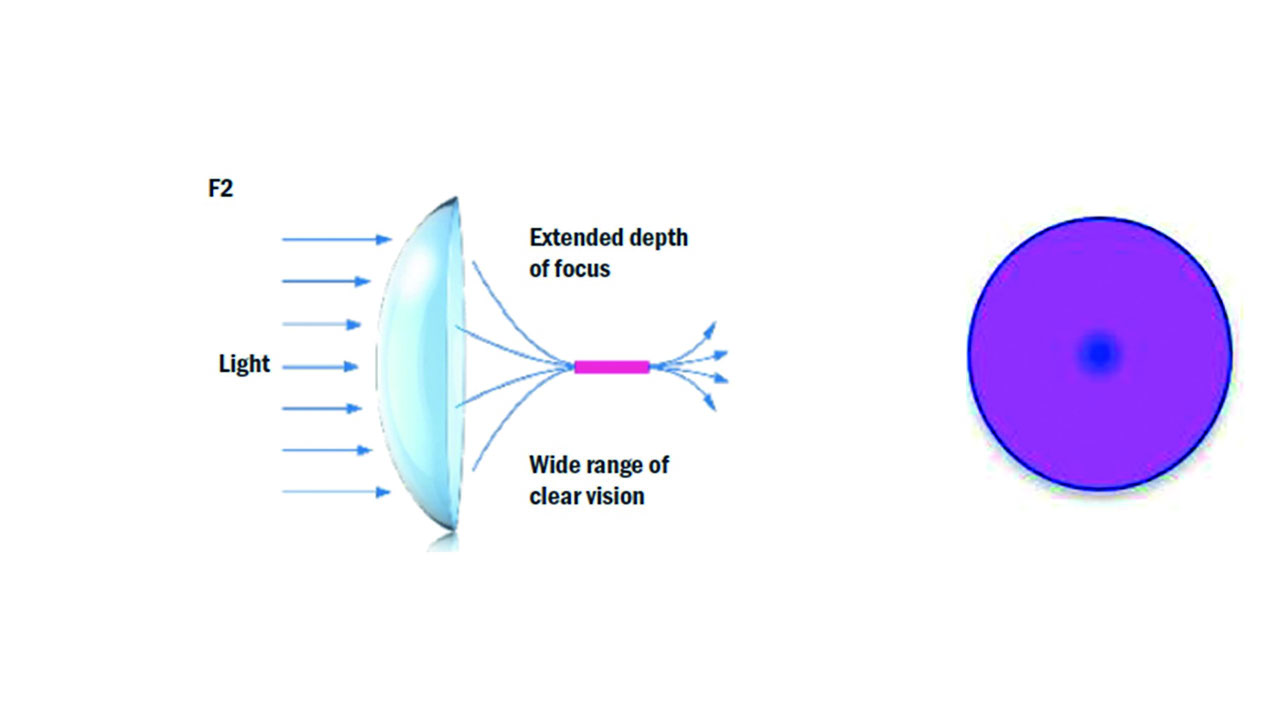
Naturalvue 1-day Multifocal Contact Lens (NVMF)
The mechanism upon which theses lenses are based is the peripheral defocus theory. The extended depth of focus (centre distance) simultaneous vision multifocal contact lens uses Neurofocus Optics Technology (patented aspheric design) rapidly increasing relative plus power from central zone inducing a virtual pinhole effect, the smooth power distribution arising from the nonconical aspheric surface design (figure 5).32
Figure 5: Aspheric design extended depth of focus lens (left) with a rapidly increasing relative plus power from the central zone (right) inducing a virtual pinhole effect
Evidence
The supporting evidence for this lens is from retrospective case series analysis this research methodology does not use a separate control group like RCT making efficacy assessment difficult as well as comparison to other available products.33 It does, however, provide real world evidence and the study itself acknowledges it lacks the rigour compared to RCTs.
There were 32 children aged six to nine years that took part in the study and data for each eye was analysed separately. The duration the lenses were worn varied from six to 25 months, 10.94 months being the average, but eight (25%) of the children only wore the lenses for six months and two children (6.2%) for 24 months, daily wearing time were not specified.
For 75% of children, myopic progression stopped, 6.25% experienced a regression, and 90.6% of children showed a ≥70% reduction in myopic progression.
There are a lot of percentages, which can be confusing, and the annualised progression rates were calculated from measurements at the initial visit, but it is not clear if cycloplegic refraction was used and axial length measurements were not taken.
Further results came from 153 children (mean age 12 years) followed from six months to almost five years for whom an approximate figure of 0.90DS was given as a decrease in myopic progression.34 There was also a subset of 36 children where axial length was measured, which showed a change from the baseline of approximately 0.10mm growth per year of wearing NVMF. This was not a publication of a full study, so detailed scrutiny was not possible.
Case studies provide real world evidence and RCTs are a very expensive exercise to undertake, this lens clearly worked for patients taking part in this research study, but care needs to be taken interpreting the results particularly regarding efficacy, which should be considered alongside the limitations of this study methodology.
In 2022, Menicon began marketing the Naturalvue daily disposable lens under the Bloom brand. Bloom Day is part of a range of myopia management products that currently includes Bloom Night, Menicon’s orthokeratology offering for myopia management.
Orthokeratology
Orthokeratology (ortho-k) lenses have been fitted for several decades offering patient’s daytime freedom from spectacles but are also an effective option for myopia management. The lens design (reverse geometry) creates a steepening in the mid peripheral corneal zone inducing myopic defocus, which, as a mechanism for myopia management, applies the peripheral defocus theory (figure 6).
Figure 6: Fluorescein profile of an orthokeratology lens
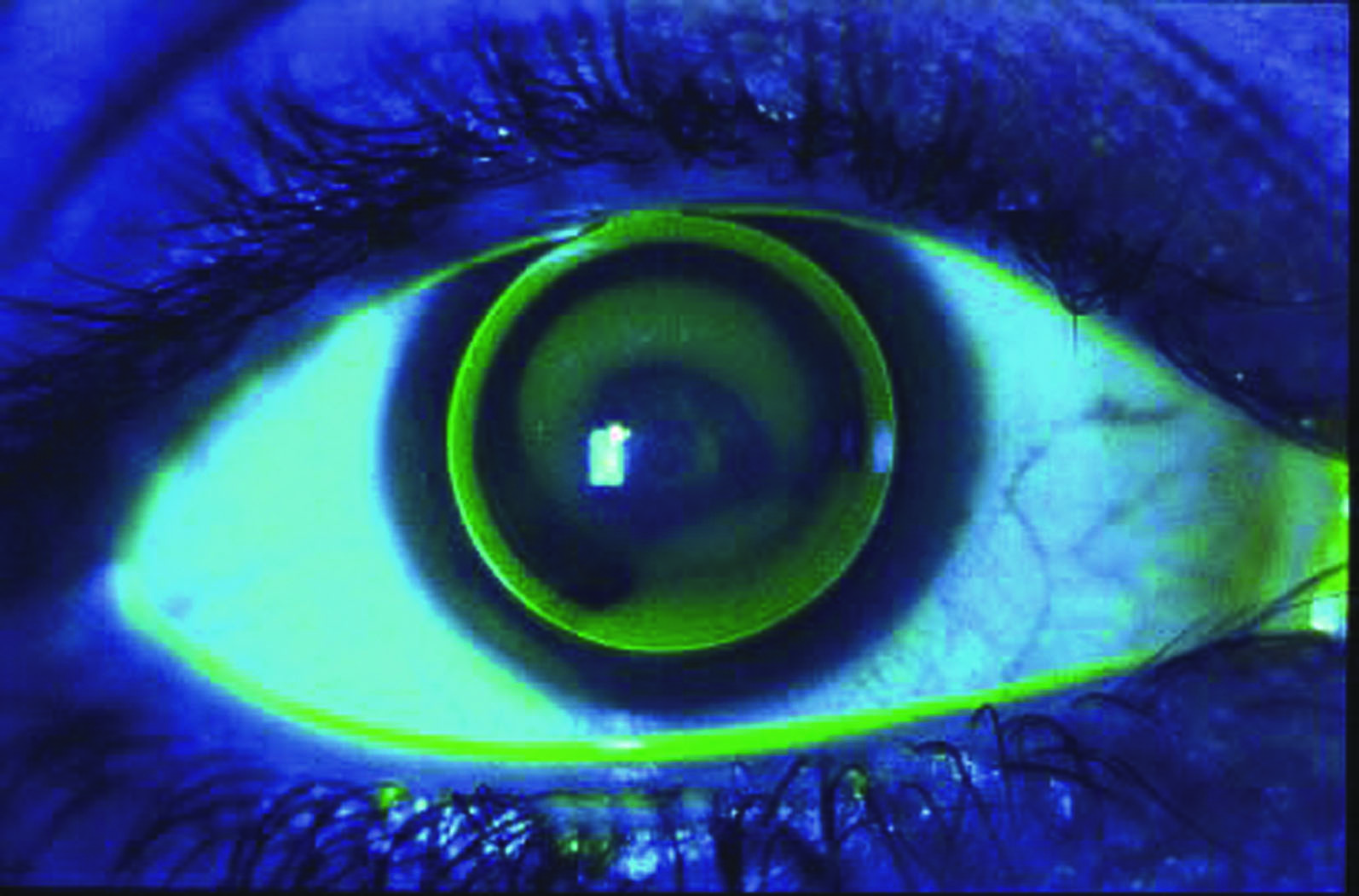
Understanding corneal topography is essential for this type of lens design as it requires exact specialist fitting. Efficacy for lens as an option for myopia management from (Sun et al 2015)35 meta-analysis showed change in axial length in the ortho-k lens group was 0.27mm equating to an approximate 45% reduction in myopic progression.
The risk of microbial keratitis is similar to other overnight wear lenses approximately 13.9 per 10,000 patient years of wear.36 Rebound effects on cessation of wearing orthokeratology lenses have been observed37 although, there is a lack of robust comparable data.
Pharmacological intervention
The use of atropine is currently not licenced in the UK but looking at published evidence from the ATOM1 study,38 which showed atropine with a concentration of 1% produced a 77% reduction in myopic progression over two years but a considerable rebound effect was observed after a one-year cessation period. Considering the side effects and rebound effect lower concentrations have been studied.
The two-year LAMP study phase three report39 compared concentrations of 0.05%, 0.025% and 0.01% atropine, with 0.05% offering better treatment efficacy compared to 0.01% (figure 7).
Figure 7: Low dose atropine, yet to be made available in the UK

Questions still remain regarding the cellular and pharmacological process, optimum concentration, treatment duration, drug holidays, safety of long-term use and whether the sclera, choroid, or retina location impedes myopic progression.40
Conclusions
Armed with the knowledge that myopia progresses at fairly predictable rates, and that becoming myopic at a young age is highly likely to lead to the patient being highly myopic as an adult, it is important that ECPs communicate this to patients/parents and apprise them of the risks before offering an optical correction. Although the absolute risk of sight threatening conditions relating to myopia remain low the relative increase in risk dramatically increases in high myopia and the biggest predictor of high myopia is the incidence of myopia at a young age.
To gain valid consent from the parent of a young myope the information given must include reference to available optical appliances beyond standard single vision spectacles or contact lenses. Practices that do not offer myopia management solutions of the types mentioned here have a duty to inform the patient of these options and refer the patient to another practitioner if they are not able to provide these themselves.
ECPs should not prejudge the patient’s ability to afford these options but should present a range of suitable options and allow the parent/guardian to decide for themselves. ECPs should also keep data on their myopia management interventions and volunteer for studies when possible – with robust evidence it is conceivable that GOS vouchers may be increased to fund myopia management lenses in the future.
With new entrants to the market the range of available options is increasing and while myopia control contact lenses should form part of the informed choice for all myopic children, spectacles are still required as a back-up and myopia control lenses should naturally be offered alongside conventional spectacle lenses and the patient/parent allowed to decide for themselves based on the information provided. ECPs who are new to myopia management are also strongly recommended to complete the manufacturer’s CPD accredited training programmes before embarking upon supply, and finally to adhere to the recommended fitting guidelines for both contact lens and spectacle lens alternatives.
- Peter Black MBA FBDO FEAOO AFHEA is Course Lead for BSc (Hons) Ophthalmic Dispensing at the University of Central Lancashire, Preston, and is a practical examiner, practice assessor, exam script marker, board member and past president of the Association of British Dispensing Opticians.
- Tina Arbon Black BSc (Hons) FBDO CL is director of accredited CPD provider Orbita Black Limited, an ABDO practical examiner, practice assessor and exam script marker, and a distance learning tutor for ABDO College.
References
- Holden BA, Fricke RF, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-1042. Available from: https://www.sciencedirect.com/science/article/pii/S0161642016000257
- Bullimore MA, Brennan NA. Myopia Control: Why Each Diopter Matters. Optometry and Visual Science. 2019; Available from: https://www.researchgate.net/profile/Mark_Bullimore/publication/333266680_Myopia_Control_Why_Each_Diopter_Matters/links/5e91c7704585150839d2b02a/Myopia-Control-Why-Each-Diopter-Matters.pdf
- Morgan IG, Wu P, Ostrin LA, Willem J, Tideman L, Yam JC, et al. IMI risk Factors for Myopia. Investigative Ophthalmology & Visual Science. 2021;62(5): 3. Available from: https://doi.org/10.1167/iovs.62.5.3
- Hua W, Jin J, Wu A, Yang J, Jiang X, Gao G, et al. Elevated light levels in schools have a protective effect on myopia. Ophthalmic and Physiological Optics. 2015;35(3):252-262. Available from: https://doi.org/10.1111/opo.12207
- Zhou Z, Chen T, Wang M, Jin L, Zhao Y, Chen S, et al. Pilot study of a novel classroom designed to prevent myopia by increasing children’s exposure to outdoor light. PLOS ONE. 2017; 2(7):1-16. Available from: https://doi.org/10.1371/journal.pone.0181772
- Jiang Y, Zhu Z, Tan X, Kong X, Zhong H, Zhang J, et al. Effect of Repeated Low-Level Red-Light therapy for Myopia Control in Children: A multicenter randomised controlled trial. Ophthalmology. 2022;129(5): 509-519. Available from: https://commonslibrary.parliament.uk/research-briefings/cbp-7375/https://doi.org/10.1016/j.ophtha.2021.11.023
- Xiong S, Sanderidurg P, Naduvilath, Zang J, Zhu J, Lv M. et al. Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmologica. 2017;95(6): 551-556. Available from: https://doi.org/10.1111/aos.13403
- Mountjoy E, Davies N, Plotnikov D, Smith GD, Rodriguez S, Williams CE, et al. Education and myopia: assessing the direction of causality by mendelian randomisation. BMJ. 2018; 361. Available from: https://doi.org/10.1136/bmj.k2022
- Huang P, Hsiao Y, Tsai C, Tsai D, Chen C, Chien C, et al. Protective behaviours of near work and time outdoors in myopia prevalence and progression in myopic children: a 2 year prospective population study, Br J Ophthalmology. 2019;104(7):956-961. Available from: http://old.medlib.am/aknabujutyun/(2)_956.full.pdf
- Li SM, Li SY, Kang M, Zhou Y, Liu L, Li H, et al. Near work Related Parameters and Myopia in Chinese Children: the Anyang Childhood Eye Study. PLOS ONE. 2015; 10(8). Available from: https://doi.org/10.1371/journal.pone.0134514
- Swystun A, Davey C. Exploring the effect of optometrist practice type on NHS funded sight test outcome. Journal of Optometry. 2021;14(1):69-77. Available from: https://doi.org/10.1016/j.optom.2020.03.008
- Flitcroft DI, He M, Jonas JB, Jong M, Naidoo K, Ohno-Matsui, et al. IMI – Defining and Classifying Myopia: A Proposed Set of Standards for Clinical and Epidemiologic Studies. Investigative Ophthalmology & Visual Science. 2019;60(3). Available from: https://iovs.arvojournals.org/article.aspx?articleid=2727312
- Polling JR, Klaver C, Willem J. Myopia progression from wearing first glasses to adult age: the DREAM Study. British Journal of Ophthalmology. 2020; 106:820-824. Available from: https://bjo.bmj.com/content/106/6/820
- Zadnik K, Sinnott LT, Cotter SA, Jones-Jordan LA, Kleinstein RN, Manny RE, et al. Prediction of Juvenile-Onset Myopia. Jama Ophthalmology. 2015;133(6): 683-689. Available from: https://jamanetwork.com/journals/jamaophthalmology/fullarticle/2206339
- Flitcroft DI. The Complex Interactions of Retinal, Optical and Environmental Factors in Myopia Aetiology. Retinal and Eye Research. 2012;31(6): 622-660.Available from: https://www.sciencedirect.com/science/article/pii/S1350946212000444?via%3Dihub
- Wallman J, Winawer J. Homeostasis of Eye Growth and the Question of Myopia. Neuron. 2004; 43(4): 447-468. Available form: https://www.sciencedirect.com/science/article/pii/S0896627304004933
- Diether S, Schaeffel F. Local Changes in Eye Growth Induced by Imposed Local Refractive Error Despite Active Accommodation. Vision Research. 1997; 37(6): 659-668. Available from: https://www.sciencedirect.com/science/article/pii/S0042698996002246
- Mutti DO, Hayes JR, Mitchell LG, Jones LA, Moeschberger ML, Cotter SA, Kleinstein RN, Manny RE, Twelker D, Zadnik K. Refractive Error, Axial Length and Relative Peripheral Refractive Error Before and After the Onset of Myopia. Investigative Ophthalmology & Visual Science. 2007;48(6):2510-2519. Available from: https://iovs.arvojournals.org/article.aspx?articleid=2164126
- Lam CS, Tang WC, Tse DY, Lee RP, Chun RK, Hasegawa K, Qi H, Hatanaka T. Defocus Incorporated Multiple Segments (DIMS) spectacle Lenses Slow Myopia: A 2year Randomised Clinical Trial. British Journal of Ophthalmology. 2020;104: 363-368. Available from: https://bjo.bmj.com/content/104/3/363.full
- Lam CS, Tang WC, Qi H, Radhakrishnan, Hasegawa K, To CH, Charman WN. Effect of Defocus Incorporated Multiple Segments Spectacle Lens Wear on Visual Function in Myopic Chinese Children. Translational Vision Science & Technology. 2020;9(9). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7442864/
- Zhang HY, Lam CS, Tang WC, Leung M, To CH. Defocus Incorporated Multiple Segments Spectacle Lenses Changed The Relative Peripheral Retinal Refraction: A 2-Year Randomised Clinical Trial. Investigative Ophthalmology & Visual Science. 2020; 61(5). Available fom: https://iovs.arvojournals.org/article.aspx?articleid=2766259
- Lam CS, Tang WC, Lee PH, Zhang HZ, Hasegawa K, To CH. Myopia control effect of defocus incorporated multiple segments (DIMS) spectacle lens in Chinese children: results of a 3-year follow-up study. British Journal of Ophthalmology. 2022;106: 1110-1114. Available from: https://bjo.bmj.com/content/106/8/1110#F2
- Bao J, Yang A, Huang Y, Li X, Pan Y, Ding C, et al. One-year myopia efficacy of spectacle lenses with aspherical lenslets. British Journal of Ophthalmology. 2021;0: 1-6. Available from: https://bjo.bmj.com/content/106/8/1171.full
- Bao J, Huang Y, Li X, Yang A, Lim EW, Spiegel D, et al. Myopia control with spectacle lenses with aspherical lenslets: a 2-year randomised clinical trial. Investigative Ophthalmology & Visual Science. 2021; 62(8). Available from: https://iovs.arvojournals.org/article.aspx?articleid=2775676
- Gao Y, Lim EW, Yang A, Drobe B, Bullimore. The impact of spectacle lenses for myopia control on visual function. Ophthalmic and Physiological Optics. 2021;41(6): 1320-1331. Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/opo.12878
- Rappon J, Chung C, Young G, Hunt C, Neitz M, Chalberg. Control of myopia using diffusion optics spectacle lenses: 12 month results of a randomised controlled, efficacy and safety study (CYPRESS). British Journal of Ophthalmology. 2021;0:1-7. Available from: https://bjo.bmj.com/content/bjophthalmol/early/2022/08/31/bjo-2021-321005.full.pdf
- Chamberlain P, Bradley A, Arumugam B, Hammond D, McNally J, Logan N, et al. Long-term Effect of Dual -Focus contact Lenses on Myopia Progression in Children: a 6-year Multicenter clinical Trial. Optometry and Vision Science. 2022;99(3): 204-212. Available from: https://journals.lww.com/optvissci/Fulltext/2022/03000/Long_term_Effect_of_Dual_focus_Contact_Lenses_on.2.aspx
- Ruiz-Pomeda A, Perez-Sanchez B, Valls S, Prieto-Garrido, Gutierrez-Ortega, Villa-Collar C. MiSight Assessment Study Spain (MASS). A 2-year randomised clinical trial. Graefe’s Archive for Clinical and Experimental Ophthalmology. 2018; 256:1011-1021. Available from: https://link.springer.com/article/10.1007/s00417-018-3906-z
- Parieto-Garrido FL, Verdejo JL, Villa-Collar C, Ruiz-Pomeda A. Predicting factors for progression of the myopia in the Misight assessment study Spain (MASS). Journal of Optometry.2022;15(1): 78-87. Available From: https://www.sciencedirect.com/science/article/pii/S1888429620301278
- Ruiz-Pomeda A, Prieto-Garrido FL, Verdejo JL, Villa-Collar C. Rebound Effect in the Misight Assessment Study Spain (MASS). Current Eye Research. 2021; 46. Available from: https://www.tandfonline.com/doi/full/10.1080/02713683.2021.1878227?scroll=top&needAccess=true
- Holden B, Sankaridurg P, Smith E, Aller Jong M, He M. Myopia, an underrated global challenge to vision: where the current data takes us on control. Eye. 2013; 28:1420146. Available from: https://www.nature.com/articles/eye2013256
- Griffin RA. Multifocal Ophthalmic Lens With Induced Aperture. US6474814 (Patent) 2002. Available from: https://patents.google.com/patent/US6474814B1/en
- Cooper J, O’connor B, Watanabe R, Fuerst R, Berger S, Eisenberg, Dillehay SM. Case Series Analysis of Myopic Progression with a Unique Extended Depth of Focus Multifocal Contact Lens. Eye & Contact Lens. 2018;44(5):16-24. Available from: https://journals.lww.com/claojournal/Fulltext/2018/09000/Case_Series_Analysis_of_Myopic_Progression_Control.14.aspx
- Review of Myopia Management. New Clinical Evidence through Five Years: NaturalVue Multifocal. Available from: https://reviewofmm.com/new-clinical-evidence-through-five-years-naturalvue-multifocal/
- Sun Y, Xu F, Zhang T, Liu M, Wang D, Chen Y, et al. Orthokeratology to control myopia progression: A Meta-Analysis. PLOS ONE. 2017;10(4). Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0124535
- Bullimore M, Sinnott L, Jones-Jordan L. The Risk of Microbial Keratitis With Overnight Corneal Reshaping Lenses. Optometry and Vision Science. 2013;90(9):937-944.Available from: https://journals.lww.com/optvissci/Abstract/2013/09000/The_Risk_of_Microbial_Keratitis_With_Overnight.6.aspx
- Cho P, Cheung SW. Discontinuation of Orthokeratology on Eyeball Elongation (DOEE). Contact Lens and Anterior Eye. 2017; 40(2):82-87. Available from: https://www.sciencedirect.com/science/article/pii/S1367048416301916
- Chua WH, Balakrishnan V, Chan YH, Tong L, Ling Y, Quah BL, Tan D. Atropine for the Treatment of Childhood Myopia. Ophthalmology. 2006;113(12):2285-2291. Available from: https://www.sciencedirect.com/science/article/pii/S0161642006007597
- Yam J, Zhang XJ, Zhang Y, Wang YM, Tang SM, Li FF, et al. Three-Year Clinical Trial of Low-concentrations Atropine for Myopia Progression (LAMP) Study: Continuous Versus Washout: Phase 3 Report. Ophthalmology. 2022;129(3): 308-321. Available from: https://www.sciencedirect.com/science/article/pii/S0161642021007454
- Chierigo A, Desideri LD, Traverso CE, Vagge A. The role of Atropine in Preventing Myopia Progression: An update. Pharmaceutics. 2022; 14(5). Available from: https://www.mdpi.com/1999-4923/14/5/900/htm
