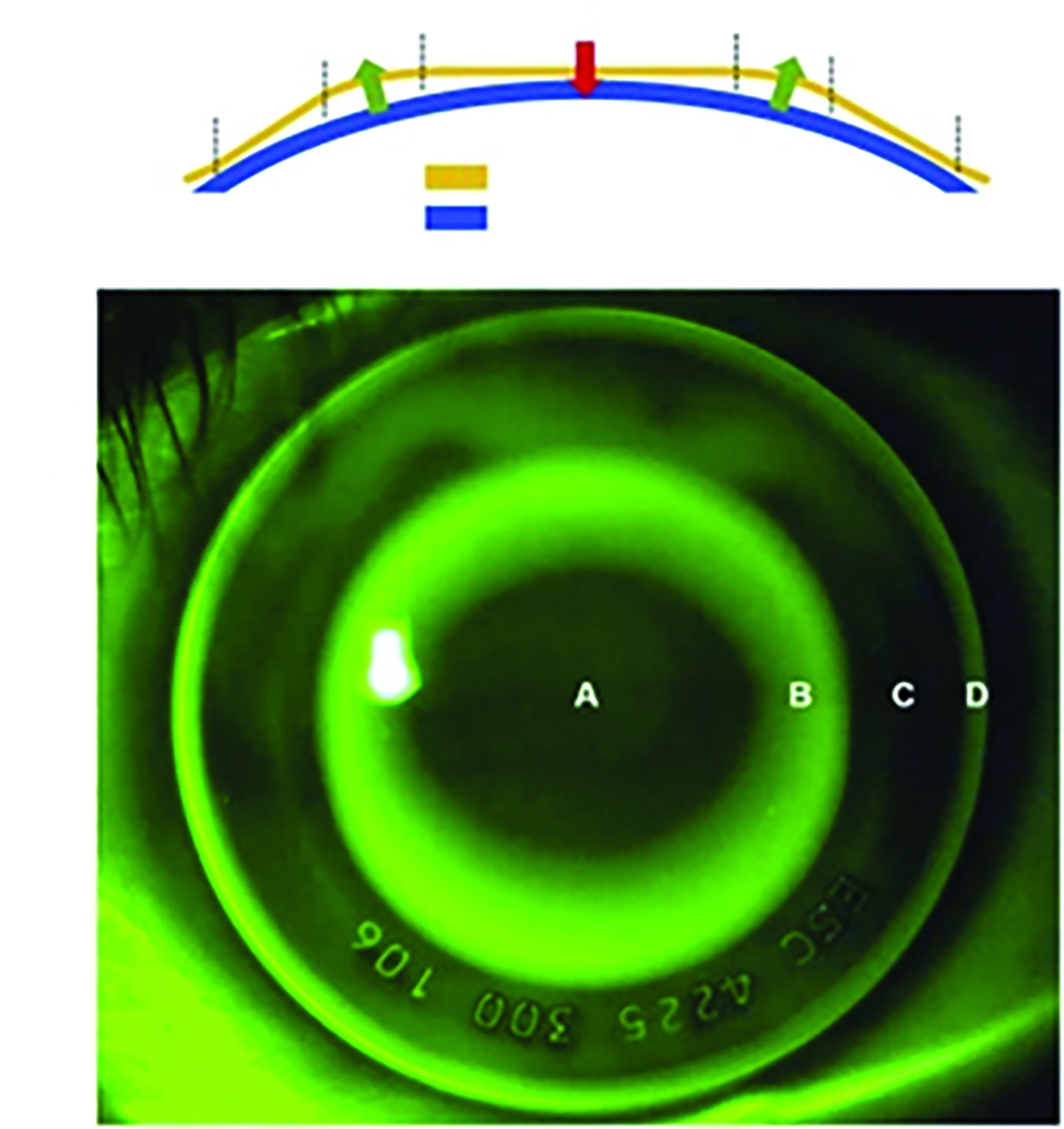
What Is Orthokeratology?
Orthokeratology (ortho-k) is the practice of redistributing the corneal tissue, using specialised reverse geometry rigid corneal lenses (RCLs), which are worn overnight. Through this process, it counteracts the wearers refractive error so that, on waking, it provides clear vision throughout the day, both with and without lenses in. The vision-related quality of life measures for ortho-k in adults is similar to other types of contact lenses (CLs), spectacles and even laser surgery.1
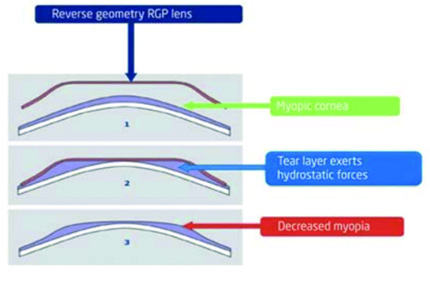
As in figure 1, rather than bending the cornea, an ortho-k lens causes displacement of epithelial cells through suction force in the tear film behind the lens, where epithelial cells ‘fill the gaps’ and are moulded to the same shape as the back surface of the reverse geometry lens. This is temporary, reversible and requires lens wear every night. The central cornea is also gently flattened with a conversely steepened mid-periphery to provide further refractive stability. The largest change in refraction occurs after the first night of wear, but it can take up to 10 nights of wear to achieve the new corneal curvature and thickness needed to fully correct any refractive error.2 If ortho-k is discontinued, a full reversal can take up to a few weeks.
Figure 1: How redistribution of the anterior corneal epithelium occurs in ortho-k
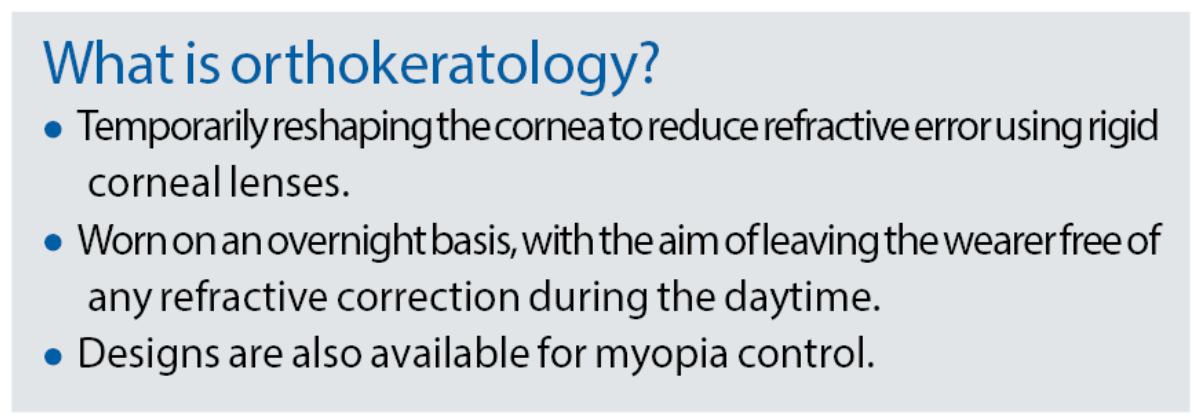
Most ortho-k lenses are custom-made and are therefore available in many different parameters. The parameters provided in this table provide a general range of lenses available from manufacturers and should not be considered an exhaustive list.
Orthokeratology Considerations
While ortho-k fitting is not limited to the correction of myopia, it is the primary refractive error managed in practice. Usually, licenced lenses can correct up to -6.00DS of myopia (table 1), though the best visual results are generally found in lenses up to -4.50DS. The design of a myopic ortho-k lens is shown in figure 2 with the corresponding fluorescein (NaFl) pattern, the design of the lens is then discussed in corresponding table 2.
Table 1: General parameters available in current approved ortho-k lenses (WTR = with-the-rule; ATR = against-the-rule)
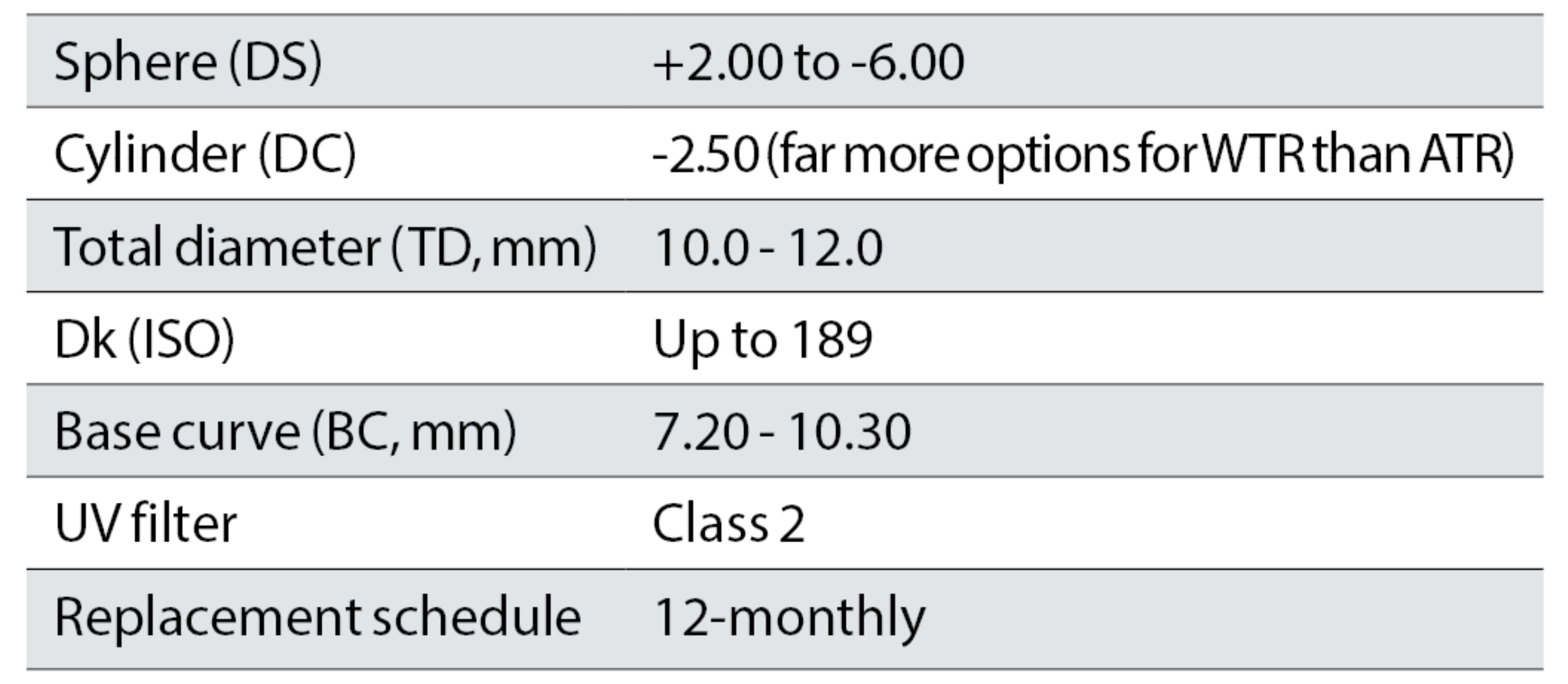
Figure 2: The design of a reverse-geometry ortho-k lens for myopia with corresponding fluorescein patten. (Image courtesy of BCLA CLEAR- Orthokeratology)
Ortho-k can be used for other refractive ametropias (see table 1). A patient may have an unstable or decentred fit with a spherical lens if there is corneal astigmatism present over 1.50DC, especially if the astigmatism is limbal-to-limbal. Here, a back surface toric design may need to be utilised, which can either have a central toric optic zone or a central spherical zone with a toric periphery. Correcting hyperopia is possible, though it is uncommonly used as the outcomes are less predictable and more variable, especially for refractive errors over +3.50DS. Ortho-k lenses can also correct presbyopia either by inducing a multifocal zonal effect or by way of monovision.
Table 2: Corresponding table to figure 2 showing the curves of a reverse geometry ortho-k lens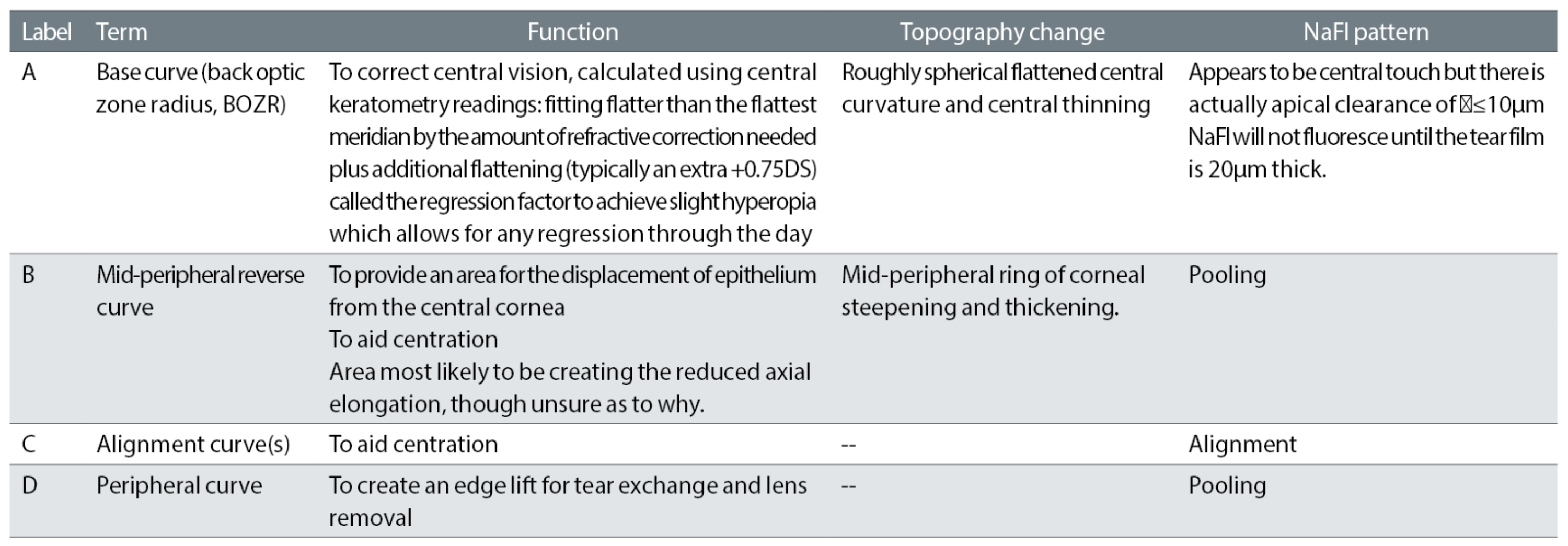
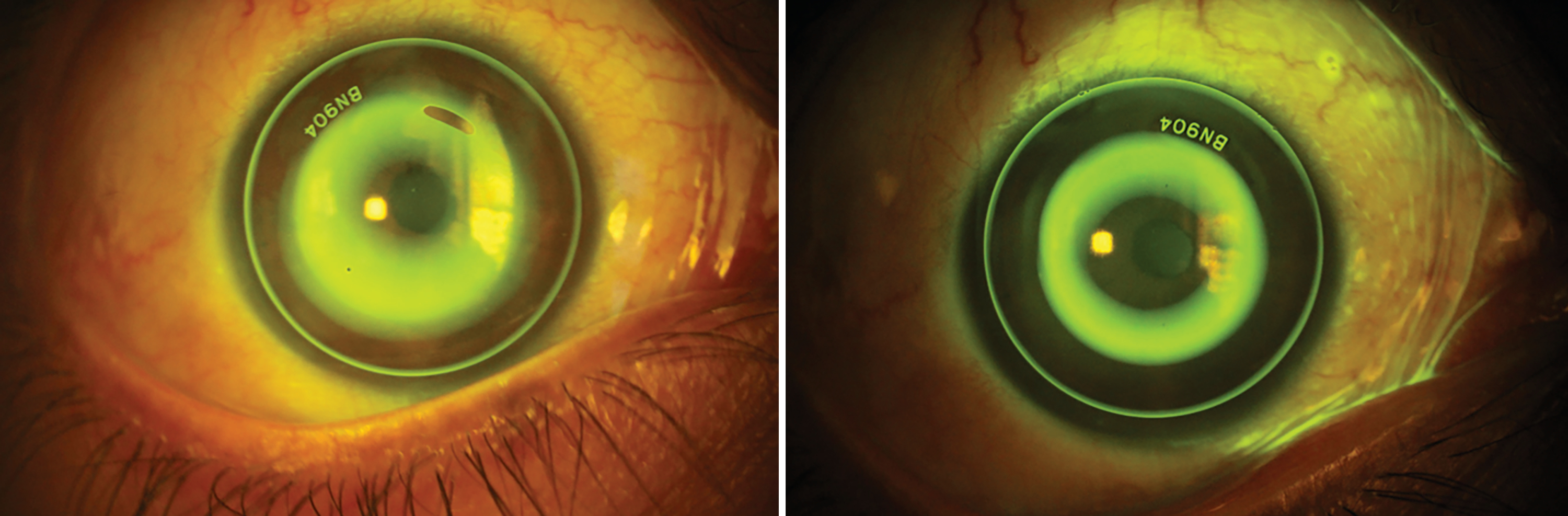
Figure 3 summarises the process for empirical fitting, which is becoming increasing popular as the most common approach to ortho-k lens fitting, rather than using a fitting set, while figure 4 shows fitting patterns.
Figure 3: The process for empirical fitting of an ortho-k lens
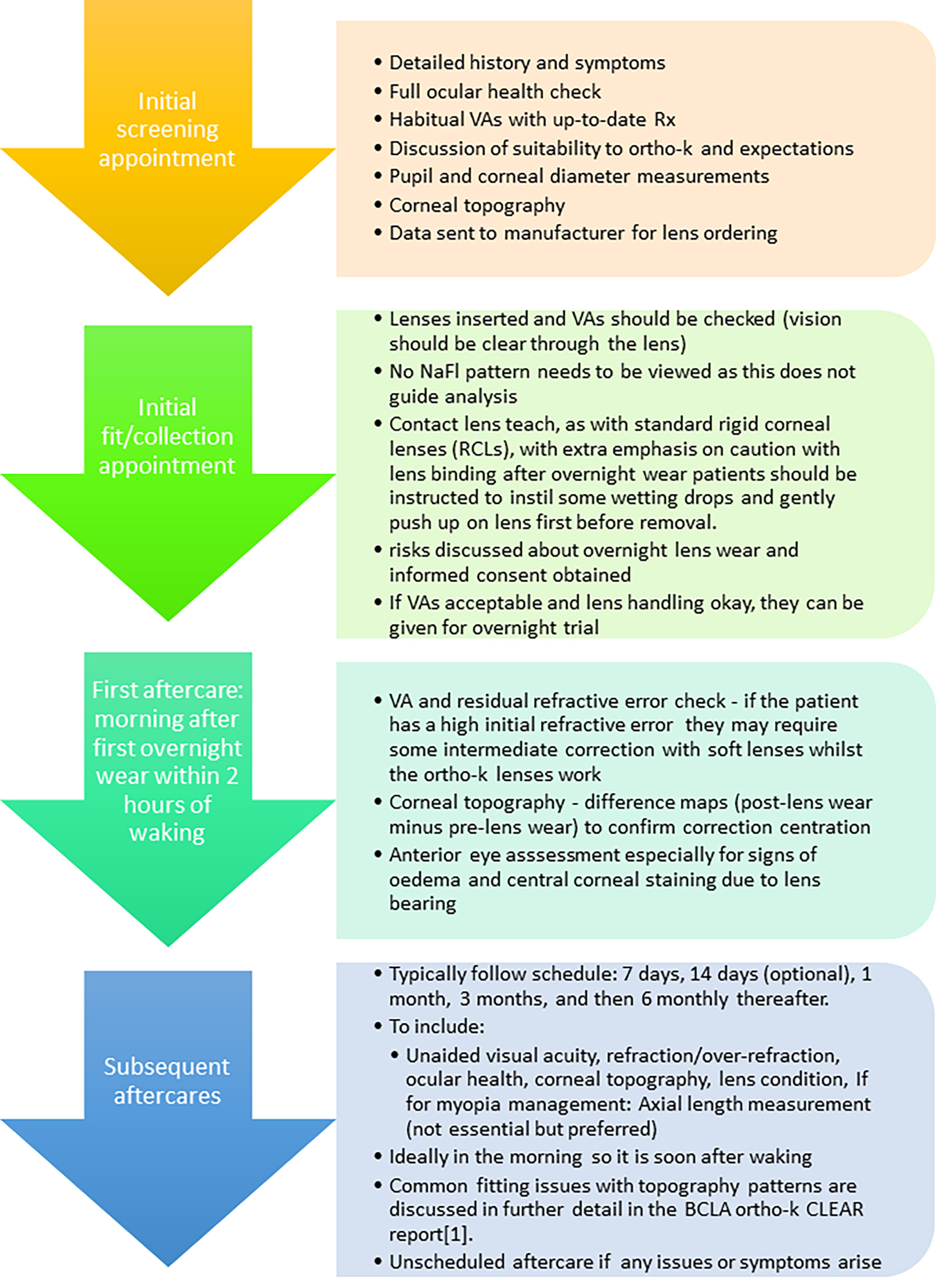
Figure 4a (left): Steep fit where the central area shows too much fluorescein, due to excessive apical clearance, associated with excessive sagittal height; 4B (right): A lower sagittal height and less apical clearance providing an acceptable fit. The central area shows a dark zone, the reverse zone has a ring of fluorescein, followed by the dark alignment curve and adequate edge lift at the peripheral curve. Images courtesy of Dr Patricia Flores
Orthokeratology For Myopia Control
Since the mid-2000s, there have been numerous studies providing evidence of a consistent myopia-slowing effect of orthokeratology in children. Major studies have found efficacy of ortho-k in reducing myopia progression by between 29 to 63%.1 This means that, while the myopia still progresses, it is at a slower rate than without any ortho-k treatment. Many of these studies were conducted in East Asia where the use of ortho-k is much higher than the rest of the world, so more ortho-k research in Western countries, which would be more relatable to Western populations, may be useful. Within Western countries, the proportion of ortho-k use is surprisingly low, contributing only 2% of global contact lens fits.3 This may be due to a lack of practitioner training and awareness, despite children wearing ortho-k for myopia responding more positively to most aspects of vision-related quality-of-life questionnaires when compared to other contact lens modalities.
Results so far have suggested that orthokeratology is more effective in younger age groups, most likely because this is where the fastest refractive progression occurs, hence the earlier the treatment is undertaken, the more benefit.
Some recent research, again in East Asian countries has been conducted into whether myopia management with ortho-k may be more effective as a combination treatment with atropine eye drops, though these are not currently an approved option within some markets, including the UK. A lower rate of eye growth was reported from children within the combination group than those just wearing ortho-k lenses during a time period of around one year,4 although more research is needed to understand long term effects.
There is a dispute over the mechanism for how ortho-k induces its myopia management effect, and some of the proposed theories are expanded on below.
Peripheral refraction
The most widely accepted theory of how this occurs is through the hyperopic peripheral defocus theory, shown in figure 5.
Figure 5: Diagram showing peripheral refraction curve of an eye corrected by a single vision lens and by a lens with plus power into the periphery. Image courtesy of Sophie Coverdale
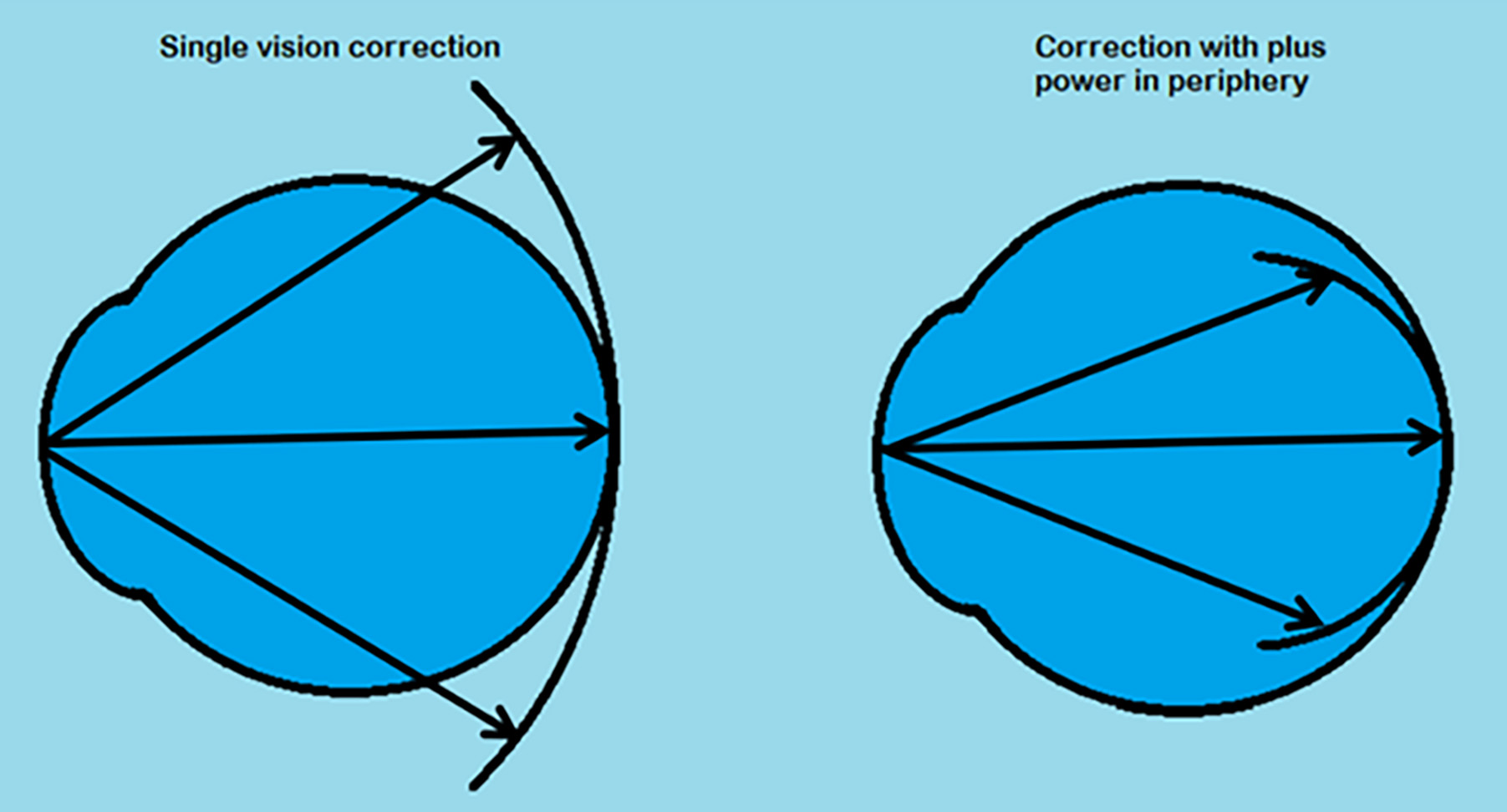
During standard single vision correction, the optics create an image shell with the centre focused on the fovea, while the peripheral image shell falls behind the retina. This peripheral hyperopic defocus has been presumed to stimulate axial (eye) elongation through local retinal mechanisms.5 In ortho-k however, altered optics from the steepened mid-periphery of the cornea create myopic defocus in the periphery, with the image shell falling in front of the retina. This can be linked to choroidal thickening, which has been associated with the control of axial length elongation.6 Further studies are needed to see if applying lenses to give a greater peripheral myopic defocus would be of benefit for improving the response of ortho-k for myopia management.
Higher order aberrations
Despite the potential degradation of vision due to elevated higher-order aberrations (HOAs) such as spherical aberration and coma, some longitudinal studies lasting at least a year have shown an association between the magnitude of these HOAs in children wearing ortho-k and a greater reduction in axial elongation.7 However, further evidence from randomised clinical trials are needed to see if slowing axial length elongation for myopia management can be improved by manipulating HOAs.
Pupil size
As pupil size would affect HOAs, accommodation response and peripheral refraction of the eye, it has been investigated as a factor that could affect the outcomes of ortho-k myopia management. Participants with larger pupils have been shown to have a slower axial growth than those with smaller pupils in the ortho-k wearing group of one study from Asia and another from Europe,1 and this may be one of the contributing factors as to the greater effect found in atropine combination studies with ortho-k, as it leads to a larger pupil.
Accommodation
Accommodation has been shown to be altered in ortho-k lens wear. A reduction in accommodative lag has been the most consistent accommodation change found within studies.8 Further studies are needed to confirm if this impact alters stimulation for axial growth and contributes to the global effects of myopia control in ortho-k.
Identifying the mechanism of myopia control is important as this would allow optimisation of the lens design for maximal myopia control efficacy. It would also be beneficial to research whether the same design would be applicable to every child or whether a tailored approach to ortho-k design could improve
efficacy.
Safety of Ortho-K
As with all contact lens fitting, safety of lenses are an important consideration and patients should be made aware of the risks and importance of hygiene and CL compliance to minimise these risks, especially the potential for serious corneal infection. Safety is especially important in ortho-k use because of the overnight wear and now the fitting to children for myopia control use. A summary of corneal findings can be found in table 3. For a more comprehensive overview of potential CL complications related to ortho-k wear, see the BCLA CLEAR complications report.9
Table 3: Corneal findings in ortho-k wear
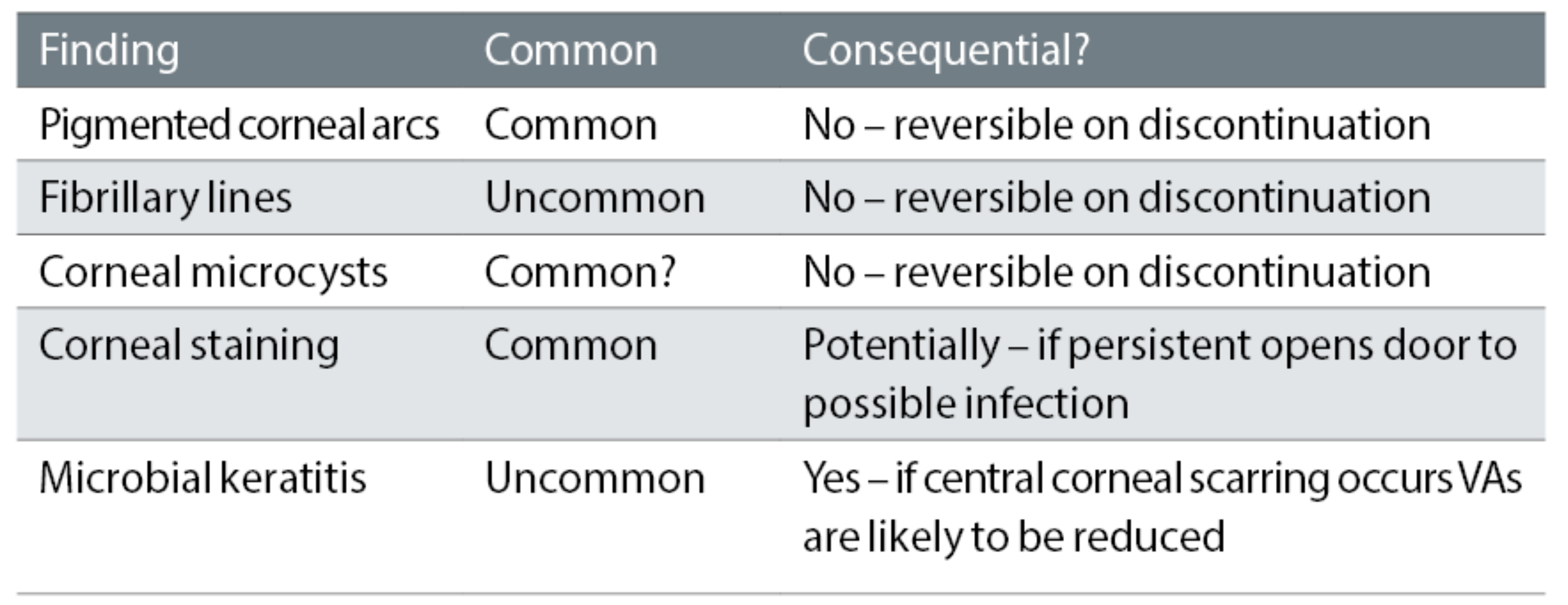
Identifying the incidence of adverse events in ortho-k use is difficult as it only accounts for a relatively small proportion of CL use, especially in Western countries. From the information available, adverse events appear uncommon and the majority are not sight threatening. A study in Spanish children found an incidence of adverse events at 13.3% of eyes per year.10 It has been found that adverse events are more prominent in those with higher refractive corrections rather than those with lower myopia.
Of all adverse events in children and adults, superficial corneal staining is the most common, which tends to appear in the central cornea, and normally worsens over the first few months of lens wear. If central corneal staining persists, this tends to be associated with lens binding, a common occurrence when a patient opens their eyes after sleeping, which can be minimised with common lubricating drops. Microbial keratitis (MK) is the most serious and possibly vision-threatening. Although exact figures are difficult because of the relatively low proportion of ortho-k wear, it is currently thought that the risk is marginally greater than those wearing a daily soft contact lens.11
Therefore, patients and caregivers should be made aware of this and alternative options discussed as appropriate. Reviews of published studies have found the trend of the most likely to get MK as young females of East Asian origin, with Pseudomonas aeruginosa as the primary infective microbe, followed by Acanthamoeba.12
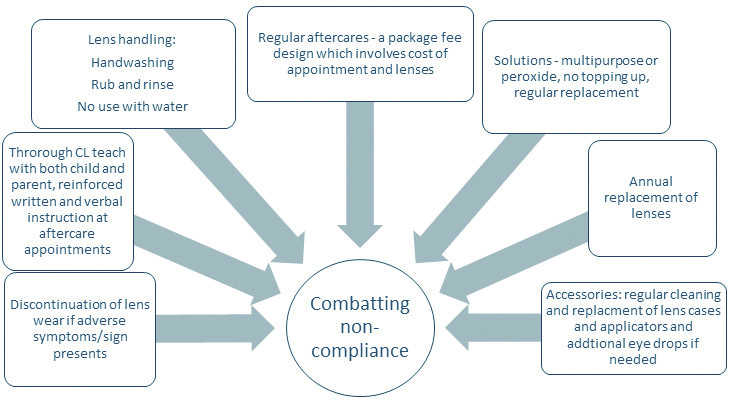
The main causal factor of serious adverse events in contact lens wear is non-compliance. Figure 7 shows ways to combatting non-compliance.
Figure 7: Methods of reducing non-compliance in orthokeratology
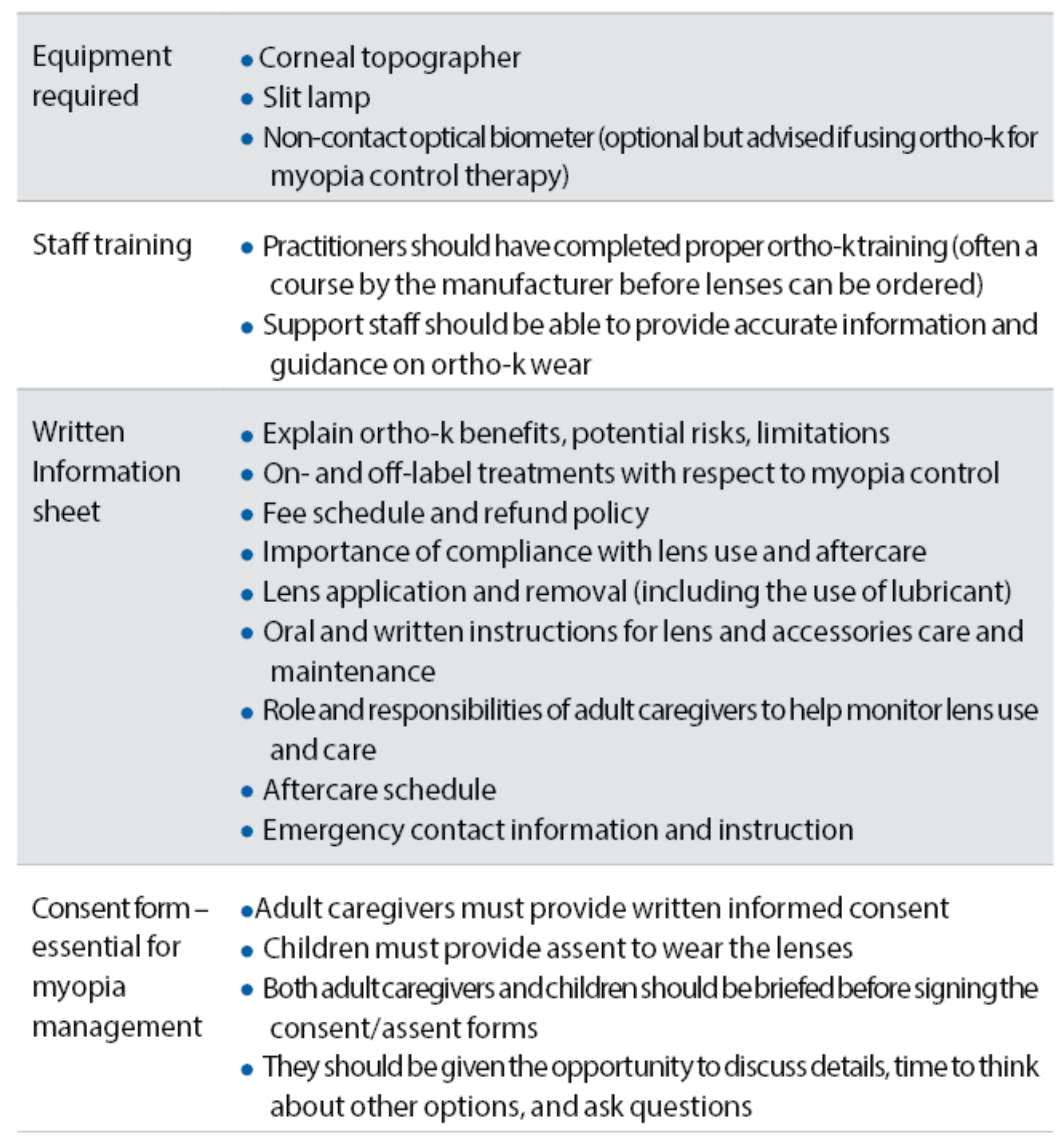
Relevance to clinical practice
An updated set of guidance on ortho-k fitting in practice can be seen in table 4, adapted from the recent BCLA CLEAR ortho-k paper.1 Informed consent is an important part of any ortho-k fitting, but especially relevant if the fitting is with an off-label lens, particularly aimed at myopia management.
Table 4: Considerations for ortho-k fitting in practice
There are additional factors to take into account when using ortho-k for myopia control. It is also down to the eye care practitioner (ECP) to monitor the efficacy of ortho-k in the myopia progression of the patient. If it is found that rapid progression is still occurring after at least six months, and not providing the level of control expected, then a different management option, or combined intervention (with spectacle lenses or atropine where possible) would be applicable. It has been found that across different ethnicities and the ages of six to 16 years, the average axial elongation over an initial two years of ortho-k treatment is 0.16mm/year.1 Therefore, if progression significantly exceeds this value, treatment should be reviewed and changed if deemed necessary.
While this is an average and provides a rough guideline, it is important to consider the rate of progression in the context of factors influencing progression such as age, ethnicity, initial refractive error and history of parental myopia. For example, an eight-year-old East Asian child with two myopic parents would be expected to have far higher progression rates than a 13-year-old Caucasian child with only one myopic parent.
If there is no knowledge of the current progression rate, then delaying the start of the intervention by three to six months to quantify progression has been proposed. This allows ECPs to identify fast progressors who would most benefit from early intervention, and provides a baseline to determine how effective the treatment is. It also allows the identification of slower progressors who may need a more tentative treatment plan. ECPs should also be careful when non-compliance is seen or adverse ocular effects such as poor lens fitting or consistent corneal staining is found.
In these cases, ortho-k should be stopped to minimise risk. Another important clinical task is to monitor progression after the patient ceases ortho-k treatment, looking for whether there is any evidence of a rebound phenomenon, where the patient rapidly progresses after ceasing treatment. If present, reinstating the intervention until progression is less likely, such as when the patient is older, is advised.
Conclusions
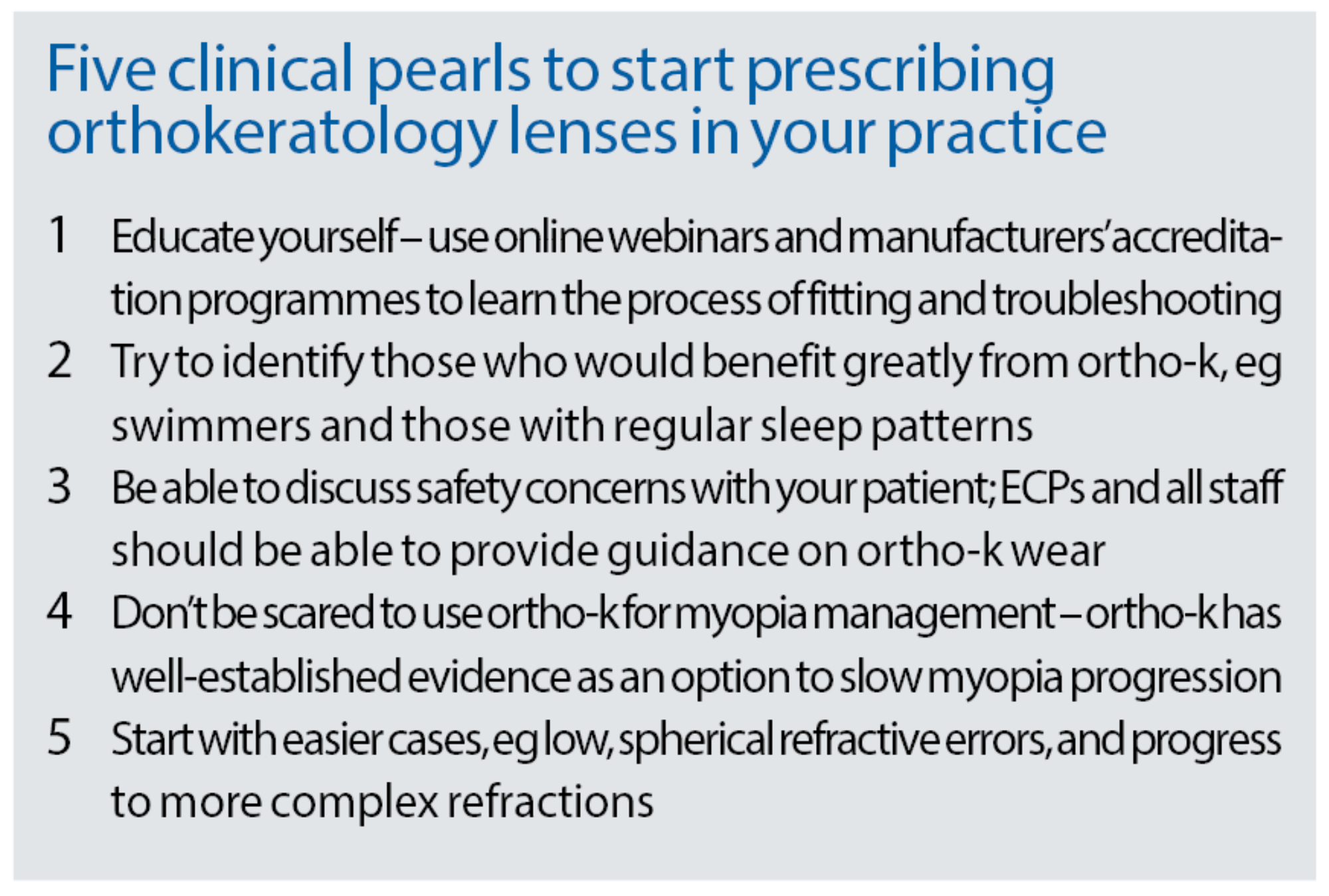
The practice of fitting ortho-k is still considered specialist to many ECPs, and barriers to it include the extra equipment needed and the increased initial chair time. Nevertheless, we may expect to see an increase in adoption and use now it has been proven an effective myopia management tool, though it also remains a viable option for regular refractive correction and is convenient for young patients even after myopia progression has ceased. Awareness of the principles and benefits of ortho-k is important, and this is an exciting evolving area, where future research will complement our understanding of best practice approaches.
- Dr Neema Ghobani Mojarrad is an optometrist and lecturer at the University of Bradford. He joined the university in 2019; since this time he has been a module leader for the contact lens undergraduate course. He is an editorial board member for the College of Optometrists Acuity magazine, and a member of the British and Irish University and College Contact Lens Educators (BUCCLE), which promotes collaboration and dissemination of evidence-based contact lens knowledge. His research interests include myopia development and management, contact lenses and applied myopia genetics, for which he won the 2021 Association of German Contact Lens Specialists and Optometrists (VDCO) Peter Abel prize.
- Sophie Coverdale is an Optometrist and Clinical Supervisor at the University of Bradford. She is a PhD Researcher in the field of myopia with interest in contact lenses including orthokeratology, and other myopia management options. She won the College of Optometrists Naylor Prize in 2019 for her final year dissertation at Cardiff University.
- The full report and supplementary information can be accessed at www.contactlensjournal.com/article/S1367-0484(21)00017-5/fulltext.
- The BCLA CLEAR Summary report is a short bite-size evidenced based practical guide for clinicians, bringing together the key findings from the report. Accessed via bcla.org.uk.
- The editors for this series are Neil Retallic and Dr Debarun Dutta.
Acknowledgements
Acknowledgement and recognition to Stephen Vincent, Pauline Cho, Ka Yin Chan, Daddi Fadel, Neema Ghorbani-Mojarrad, Jose Gonzalez-Meijome, Leah Johnson, Pauline Kang, Langis Michau, Patrick Simard, Lyndon Jones who were the paper’s authors and the educational grants from Alcon and CooperVision. The author would like to thank Stephen Vincent for kindly reviewing this article.
References
- Vincent SJ, Cho P, Chan KY, Fadel D, Ghorbani-Mojarrad N, González-Méijome JM, et al. BCLA CLEAR-Orthokeratology. Contact Lens and Anterior Eye 2021;44(2):240-69.
- Kang P, Swarbrick H. Time course of the effects of orthokeratology on peripheral refraction and corneal topography. Ophthalmic and Physiological Optics 2013;33(3):277-82.
- Morgan PB, Efron N, Woods CA, Santodomingo-Rubido J, International Contact Lens Prescribing Survey C. International survey of orthokeratology contact lens fitting. Contact Lens and Anterior Eye 2019;42(4):450-4.
- Tan Q, Ng ALK, Choy BNK, Cheng GPM, Woo VCP, Cho P. One-year results of 0.01% atropine with orthokeratology (AOK) study: a randomised clinical trial. Ophthalmic and Physiological Optics 2020;40(5):557-66.
- Smith Iii EL. The Charles F. Prentice award lecture 2010: a case for peripheral optical treatment strategies for myopia. Optometry and Vision Science 2011;88(9):1029.
- Li Z, Hu Y, Cui D, Long W, He M, Yang X. Change in subfoveal choroidal thickness secondary to orthokeratology and its cessation: a predictor for the change in axial length. Acta ophthalmologica 2019;97(3):e454-e9.Lau JK, Vincent SJ, Cheung S-W, Cho P. Higher-order aberrations and axial elongation in myopic children treated with orthokeratology. Investigative Ophthalmology & Visual Science 2020;61(2):22-.
- Batres L, Peruzzo S, Serramito M, Carracedo G. Accommodation response and spherical aberration during orthokeratology. Graefe’s Archive for Clinical and Experimental Ophthalmology 2020;258(1):117-27.
- Stapleton F, Bakkar M, Carnt N, Chalmers R, Vijay AK, Marasini S, et al. CLEAR - Contact lens complications. Cont Lens Anterior Eye 2021;44(2):330-67. https://doi.org/10.1016/j.clae.2021.02.010.
- Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutiérrez-Ortega R. Orthokeratology vs. spectacles: adverse events and discontinuations. Optometry and Vision Science 2012;89(8):1133-9.
- Hiraoka T, Sekine Y, Okamoto F, Mihashi T, Oshika T. Safety and efficacy following 10-years of overnight orthokeratology for myopia control. Ophthalmic and Physiological Optics 2018;38(3):281-9.
- Kam KW, Yung W, Li GKH, Chen LJ, Young AL. Infectious keratitis and orthokeratology lens use: a systematic review. Infection 2017;45(6):727-35.
