One characteristic of climate change is the number and complexity of ways in which nature and human society is being affected as a result of a much simpler reality; that the effect of increasing atmospheric concentrations of gases, such as carbon dioxide, is raising the planet’s temperature.
As the natural ecosystems of the planet become disrupted and the human population is increasingly exposed to extremes of environmental and associated social/economic pressures, there is invariably a toll taken upon the health of individuals and, as a consequence, upon health delivery systems. Within this context, the health of the human visual system is a specific focus where certain areas of concern, such as increased levels of ultraviolet radiation, neglected tropical diseases and air pollution, have been identified. It is this focus that this article takes.
The Ultraviolet Factor
There has been a well-documented link between exposure to ultraviolet radiation from sunlight and the incidence of cataracts.1 A specific historical focus has been provided by the depletion of ozone in the stratosphere caused by ozone-depleting substances, such as halocarbon refrigerants, solvents, propellants and foam blowing agents, and an associated increase in the prevalence of cataracts (figure 1).
Figure 1: There is a link between ozone depletion and the prevalence of cataract
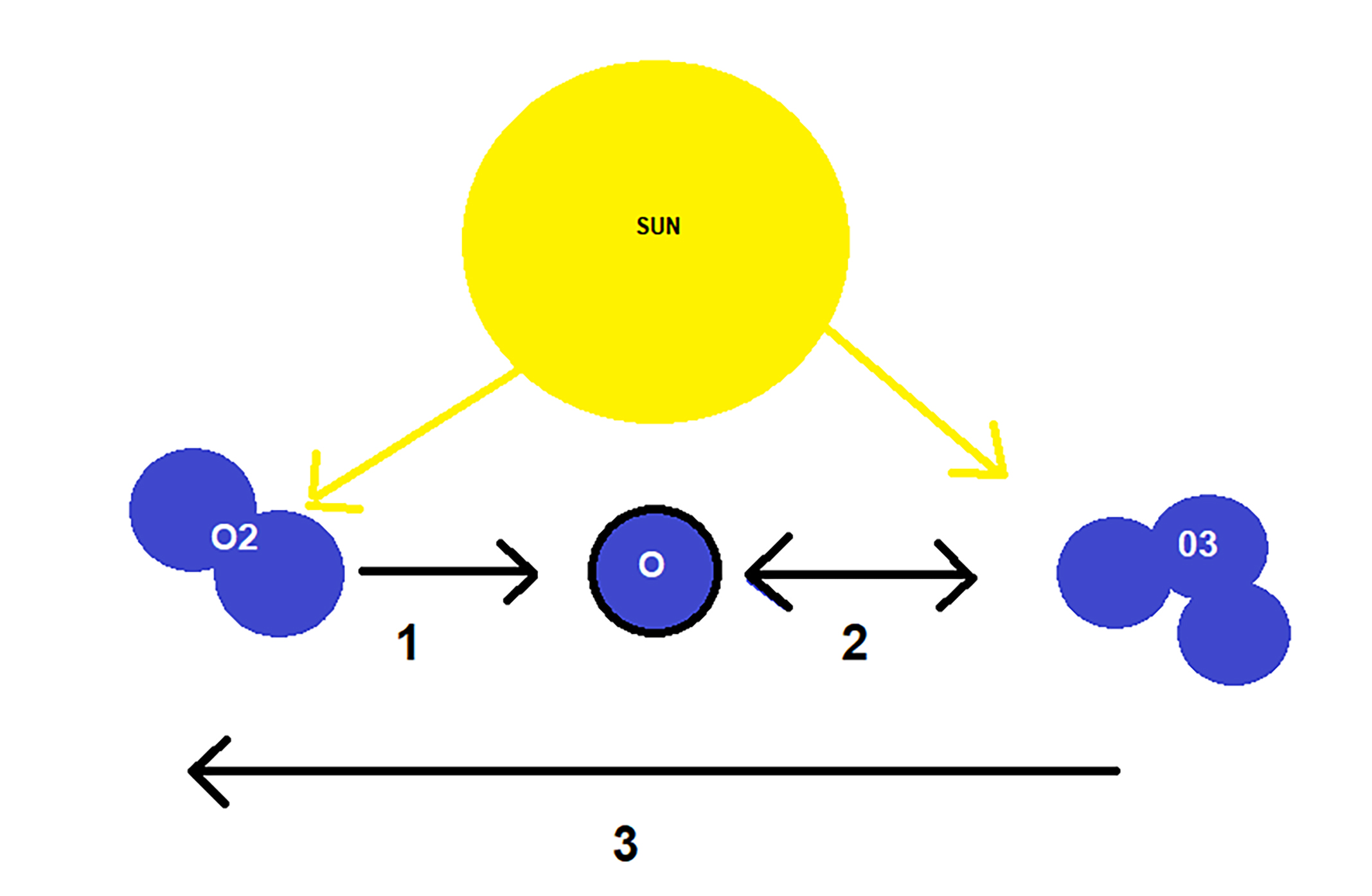
While the current levels of stratospheric ozone suggest a continued recovery towards those of the pre-1980 levels, largely driven by the 1987 United Nations Environment Programme (UNEP) Montreal Protocol, the role of climate change introduces degrees of uncertainty into this recovery process. One element of this level of uncertainty is that, with the accumulation of greenhouse gases in the atmosphere, the upper levels of the stratosphere are becoming colder. This favours the creation of polar stratospheric clouds in winter over the north and south poles. These clouds provide surfaces for the destruction of ozone when illuminated by sunlight with the return of the sun to either hemisphere in the spring. This triggers the destruction of ozone by a photochemical reaction resulting in the formation of ozone holes (figure 2). These areas of depletion are eventually restored by atmospheric circulation from near the equator.
Figure 2: The depletion of ozone by solar radiation. 1: Solar radiation breaks down the O2 molecule into its individual oxygen (O) atoms. This is a slow reaction. 2: Ozone is continually broken down by solar radiation (in a fast reaction) to release an oxygen atom which can reconvert another O2 molecule into ozone again. This rapid interconversion releases thermal energy to heat the atmosphere. 3: Some ozone or oxygen atoms slowly react with other trace elements, such as chlorine, and are lost
The units of atmospheric ozone are described in Dobson units, where 100 units is equivalent to a thickness of 1mm of ozone at standard atmospheric pressure. The unit is named after GMB Dobson (1889-1976) who undertook pioneering work while at University of Oxford to develop instruments to estimate ozone concentration from ground level observations of solar radiation. Thus, a Dobson value of 250 indicates that a vertical column of only 2.5mm of ozone at atmospheric pressure exists in a vertical column extending to the upper limits of the atmosphere.
Currently, it would appear that the reduction of ozone-depleting substances in the stratosphere is tipping the balance in favour of reducing average levels of ultraviolet exposure,2 though climate scientists are all too well aware that climate change could well disrupt this recovery process.
Extensive analysis has been undertaken of estimated historical atmospheric loading of ozone-depleting species as a result of volcanic eruptions by Brenna et al.3 While the variability of eruptions in terms of magnitude and extent of loading of the stratosphere with sulphur dioxide, chlorine and bromine compounds are variously identified, the worst case scenario of a high magnitude eruption involving significant halogen burden penetrating to the stratosphere would have the potential to result in a significant global ozone depletion; initially of up to 20%, and with a period of around 10 years for recovery. This recovery interval reflects the likely persistence of longer-lived halogen compounds in the stratosphere.
While such a future shock is unlikely, it is not altogether improbable. In fact, it is more likely with the melting of ice sheets which tend to suppress the expression of lava from deep crustal levels. Such a shock to the protective shield of stratospheric ozone would significantly and adversely impact upon diverse ecosystems, in addition to the known risks of ocular exposure. This area of environmental modelling is an important resource in assessing future climate trends.
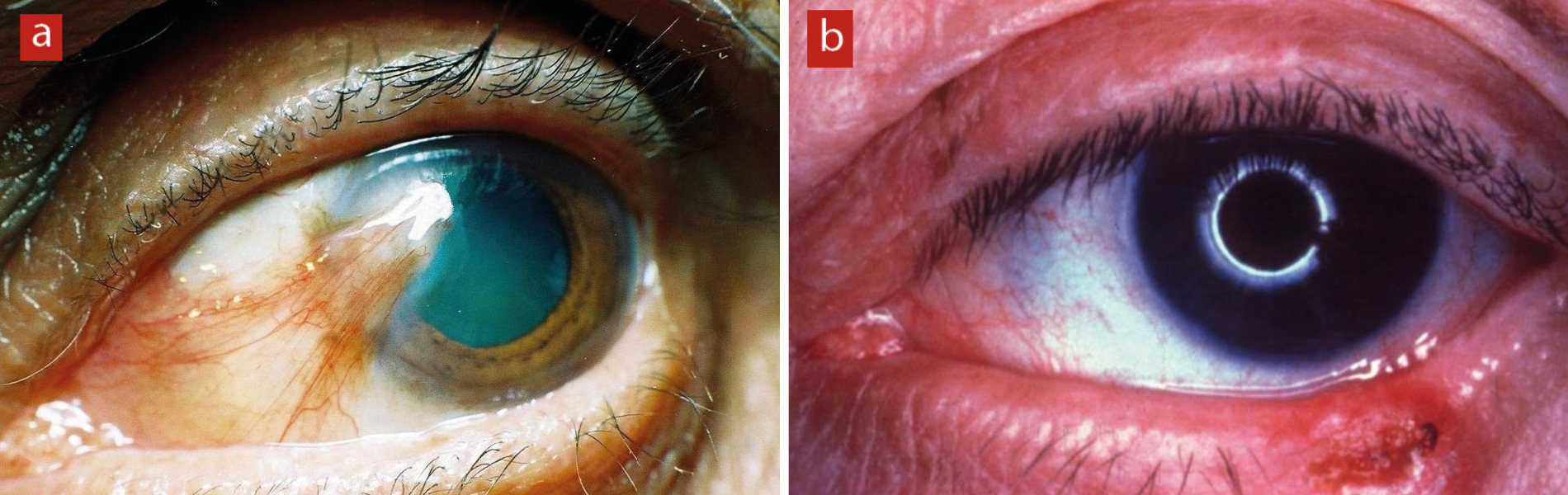
Within this picture of gradual ozone recovery, exposure to higher levels of ultraviolet radiation can be triggered by prolonged local weather events and by spending more time outdoors with increasing average temperatures.4 Alongside the increased incidence of cataracts from ultraviolet exposure, conditions such as photokeratitis, photo-conjunctivitis, pterygium, macular degeneration (in aphakes) and basal cell carcinoma are also associated with this increased UV exposure (figure 3).5
Figure 3: UV exposure is known to increase the risk of a variety of ocular conditions including (a) pterygium and (b) basal cell carcinoma
With the increased awareness of the risk of ultraviolet exposure, there is a greater focus on preventive measures regarding such exposure. Protection factors (E-SPF) have been developed that take into account both transmission components through a spectacle lens and also reflective components from the rear of the lens. The standard is intended to apply to clear prescription lenses, contact lenses and sunglasses (prescription or non-prescription). The use of such higher protective devices can be seen as both a general protective measure among the population and one especially relevant to areas of increasing ultraviolet exposure due to climate change.
It is important to recognise that younger age individuals are more prone to involvement of the retina with ultraviolet exposure (figure 4).7 Cullen describes the role of the United Nations Environmental Effects Panel in monitoring the role of stratospheric ozone in affecting levels of ultraviolet exposure of the human ocular system and stresses the ultraviolet risk will remain significant even with restoration of pre-industrial ozone levels.8
Figure 4: The retinas of younger patients have greater exposure to UV

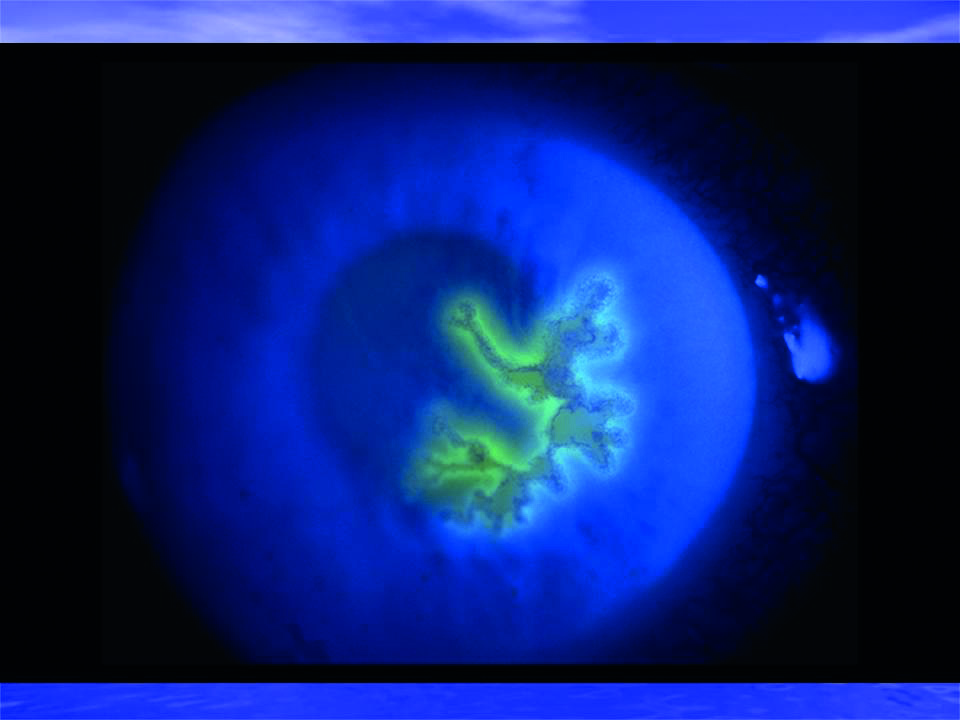
There is also some recognition that UVB radiation can interact with the immune system. Rooney et al have reported the effectiveness of sunscreen block to prevent the reactivation of the virus Herpes simplex (figure 5).9 On a more general note, Morrison et al have used animal studies to suggest that increasing levels of environmental exposure to ultraviolet radiation can adversely impact upon the effectiveness of more general immune responses in humans.10 This could potentially be a factor in the success of some vaccines within a given population.
Figure 5: Herpes simplex keratitis; reactivation may be triggered by UV
Neglected Tropical Diseases
Some important causes of sight loss in developing countries have multiple influences and their full eradication is increasingly thought to be adversely affected by the changes to the global climate. Two such conditions are described here.
Trachoma
According to the World Health Organisation, trachoma remains a health problem in 42 countries, with 125 million people remaining at risk of blindness due to trachoma and about 1.9 million people presently living with sight loss from the disease. The incidence of trachoma is a particularly distressing feature among the population of sub-Saharan Africa.
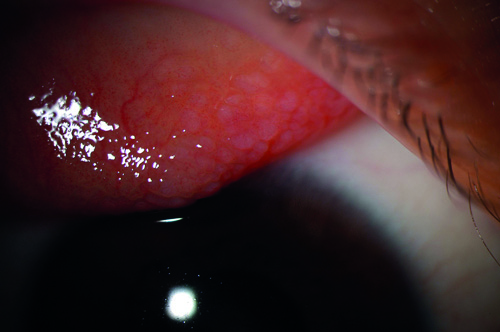
Table 1: Signs of trachoma29
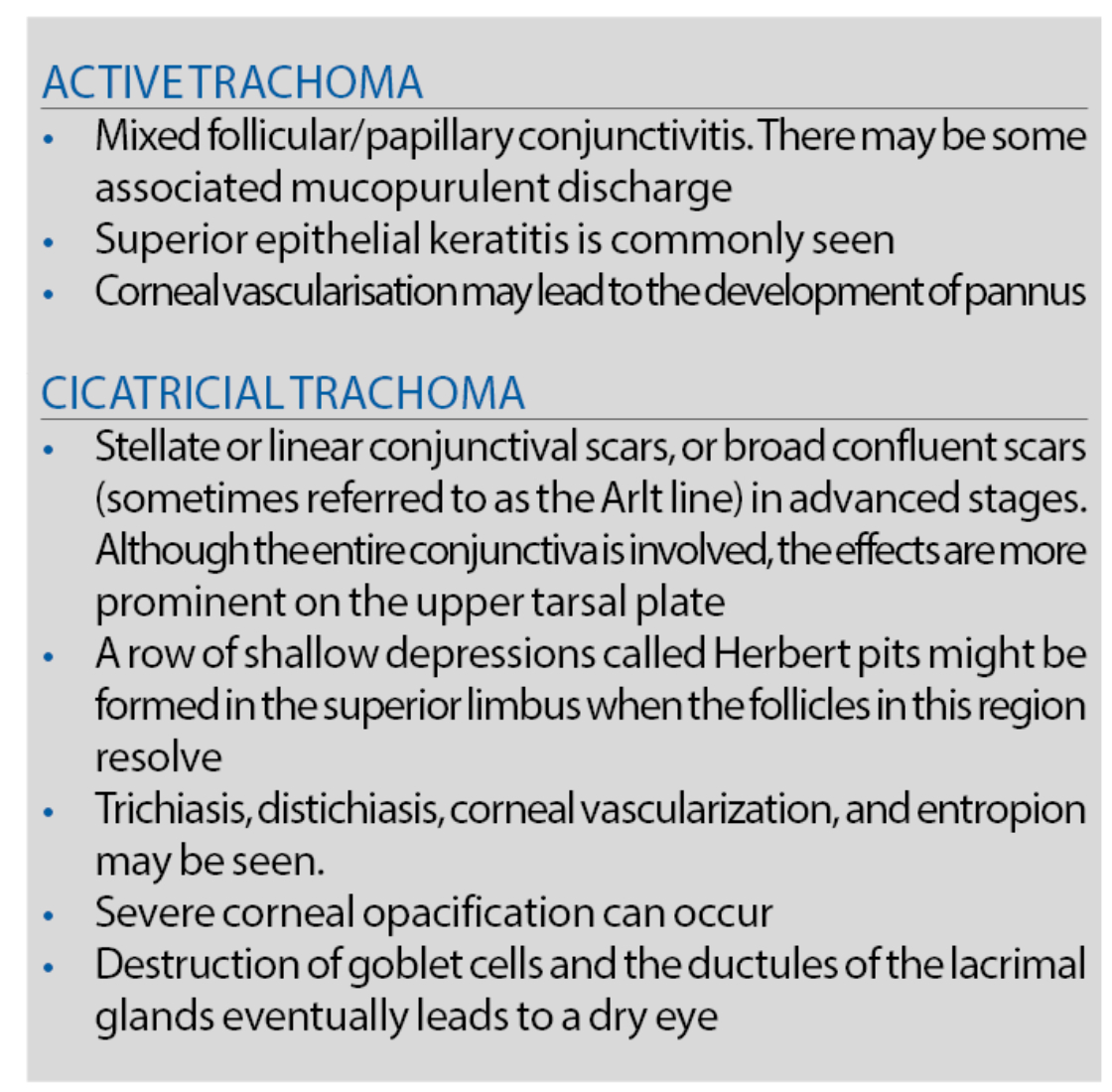
The condition presents as a bacterial infection caused by Chlamydia trachomatis, which is transmitted through both human contact and via the vector of specific species of flies. The condition is currently a focus of a World Health Organisation eradication initiative, with conditions of inadequate sanitation, scarcity of water, endemic poverty and social overcrowding presented as challenges in this programme. Following repeated episodes of infection, the eyelashes can become inverted so that they scratch the cornea, causing pain and resulting in permanent damage (figure 6 and table 1).
Figure 6: Corneal scarring caused by trachoma
The SAFE strategy has been widely adopted for treatment and control of trachoma, representing the following approach:
- Surgery
- Antibiotics: tetracycline ointment or azithromycin. The addition of azithromycin as a line of treatment follows evidence of its effectiveness.11
- Facial hygiene
- Environmental change
Numerous studies have been undertaken to identify the potential role of climate change as a factor in both the prevalence and management of the condition. A review by Ramesh et al of direct climatic parameters, however, offers no clear evidence of likely trends, though it is apparent that any deterioration of economic factors will have negative impacts on the prevalence and management of the condition.
Onchocerciasis
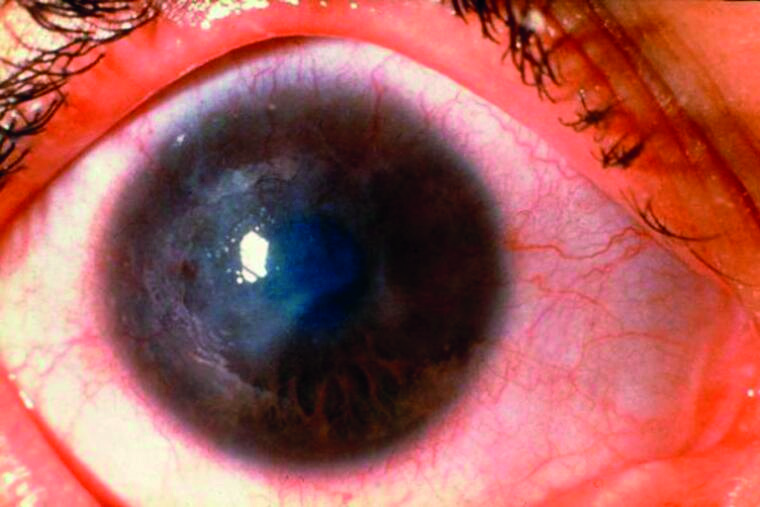
River blindness, or more properly onchocerciasis, is a disease of the tropics caused by the filarial nematode Onchocerca volvulus. The parasite is transmitted by Simulium flies, which breed in fast-flowing rivers. After transmission to a human host, infective-stage larvae mature into adult worms, which create millions of larvae that can penetrate the eye, causing visual impairment resulting ultimately in blindness (figure 7 and table 2). In 2017, it was estimated that at least 220 million people required preventive treatment and where 14.6 million of the infected patients already had skin disease and 1.15 million had vision loss. The programme to eradicate the infection began in earnest in around 1972 when, with a significant World Health Organisation programme, insecticide spraying targeting the Simulium flies was initiated in 11 West African countries. Around 1985, clinical trials indicated the effectiveness of a new anti-helminthic drug called ivermectin and, eventually, 12-monthly or six-monthly treatments with ivermectin became the main line of disease control rather than insecticide spraying. Ivermectin is freely donated to the eradication programme by Merck under the brand name of Mectizan.
Figure 7: The ocular effects of onchocerciasis include

Table 2: Signs and symptoms of onchocerciasis
While progress towards the eradication of Onchocerca volvulus gives the impression of a success story, caution has been advised by some observers13 who suggest that, while the prevalence of the infection has been significantly reduced, resistance to the main line drug could be increasing and there is the risk that existing medication programmes could suffer from neglect and complacency.
In the context of climate change, detailed assessments have been made of the likely impact of increased temperatures and variable rainfall in specific areas in West Africa.14 Model predictions project peaks of fly species in various sub-regions, with predicted temperature elevation due to climate change.
However, this is contradicted by field observations of falling insect populations, indicating that additional, as yet unknown, factors need to be included in such models. Monitoring of at-risk populations will continue to be required to control outbreaks to potential new territories.
A separate modelling exercise has been subsequently described by Cromwell et al.15 This aims to identify the priority area for population screening in Africa in an effort to identify those most likely to benefit from mass ivermectin administration as a further step towards eradication of the disease across Africa. Nuhman, however, has noted that the effective and final elimination of Onchocerca volvulus will only be achieved by the use of an effective vaccine against the infection.16 Identifying where this would best be introduced will require a well-resourced and managed long-term programme. In parallel, Gustavsen et al describes how a programme of eradication of the same parasite (Onchocerca volvulus) has been ongoing in South America. The aim is to finally deal with a smaller scale infestation that had resulted on a historical basis from slaves imported from West Africa.17 Successful elimination has already been achieved in Colombia, Ecuador, Mexico and Guatemala.
Health Costs
While one feature of attempts to assess the economic impact of climate change has been to look at factors such as storm/flood damage, lost agricultural production and so on, Echevarría-Lucas et al have assessed increased health provision costs in Southern Spain linked to increased incidence of eye disease.18 Links with climate change have thus been identified, for example, with raised incidence of retinal detachment associated with elevated temperatures19 and higher incidence of cataract operations through increased exposure to ultraviolet radiation (figure 8). The authors indicate that increase in eye diseases in Southern Spain associated with the effects of climate change is estimated to significantly increase direct healthcare costs.
Figure 8: Elevated temperature appears to increase the risk of retinal detachment

Air pollution and Climate Change in Eye Health
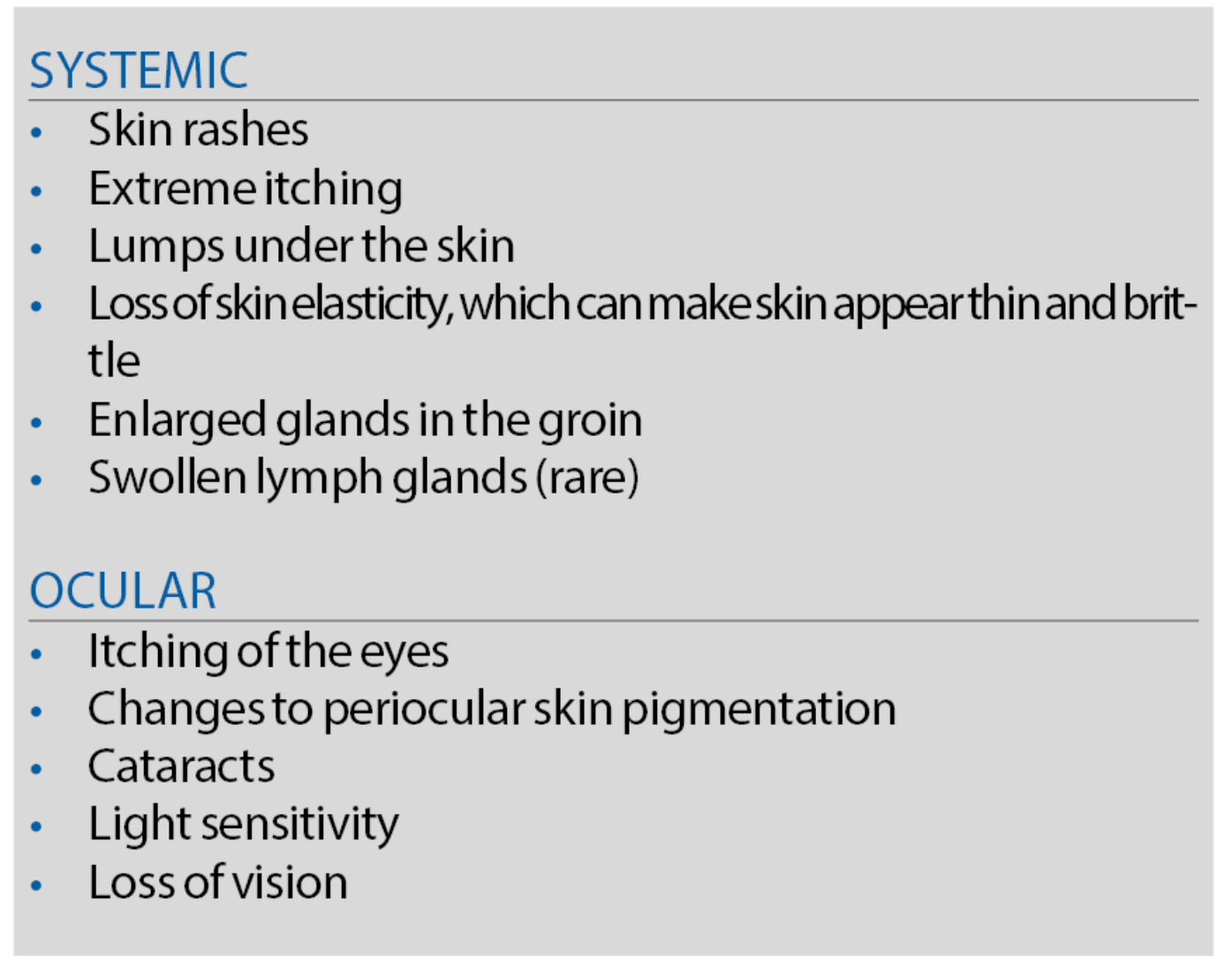
The general effects of climate change on air quality have been well described by Jacob and Winner.20 Hong et al have identified a link between levels of nitrogen dioxide (NO2), ozone (O3), and the incidence of allergic conjunctivitis (figure 9), but no correlation of the condition with particulate material, such as PM10 (particles less than 10µm in diameter) and PM2.5 (less than 2.5µm in diameter).21 Their specific research was based on an analysis of clinical presentations linked with detailed information of weather conditions and details of prevailing atmospheric pollution.
NO2 in an urban environment is most likely to originate from vehicle exhaust fumes and, initially, contain more nitric oxide (NO) than NO2. Once the NO is released into the atmosphere, it rapidly reacts with oxygen in the air to form NO2. Shin et al have also confirmed a positive link between exposure to PM10, NO2, as well as an association between atmospheric SO2 and cataract incidence.22 Chang et al also identified a link between ambient NO2 and carbon monoxide (CO) and as well as suggesting an increased risk for age-related macular degeneration.23 Miyazaki et al identified that the level of ambient air pollution (from such factors as NO2 and PM10) was significantly linked with the prevalence of ocular allergic diseases.24
Figure 9: Allergic conjunctivitis has been associated with levels of nitrogen dioxide and ozone in the atmosphere
There is an increasing focus upon assessing the effect of climate change on specific atmospheric pollutant levels, such as those of NO2 and ground ozone. Highly developed satellite monitoring systems, such as the Ozone Monitoring Instrument of the Aura satellite program operated by Nasa, have been developed to monitor NO2 levels. Lelieveld et al describe how trends in NO2 concentrations determined using this facility can be reliably linked to geopolitical factors, such as economic growth and pollution control measures.25 It would appear that, in this context, such factors are more significant than the regional out-workings of climate change. The adverse eye conditions associated with air pollution, however, pale into insignificance when compared with the associated excess deaths within an affected population.26
Planning for the Future
A significant element in coping successfully with climate change across diverse health sectors will be by ensuring the integrity of key supply chains. This was a lesson learned from the Covid-19 pandemic as described by Miller et al.27
While it is possible to look for subtle changes in the development of ocular diseases, nature can also present us with extreme adverse weather events, such as the recent floods in Pakistan.28 These events, now considered to be more likely due to climate change, damage national economies, disrupt effective healthcare systems and, at the same time, enable a range of waterborne diseases. Planning must, of course, address all immediate difficulties but a longer term principal goal must be to significantly reduce levels of greenhouse gases in the atmosphere.
- Dr Douglas Clarkson is a research fellow at the department of clinical physics and bio-engineering, Coventry and Warwickshire University Hospital Trust.
References
- Taylor HR. Ocular effects of UV-B exposure. Doc Ophthalmol, 1994-1995;88(3-4):285-93.
- Jaggernath J, Haslam D, Naidoo KS. Climate change: Impact of increased ultraviolet radiation and water changes on eye health. 2013 Health. 05. 921-930. 10.4236/health.2013.55122
- Brenna H, Kutterolf S, Krüger K. Global ozone depletion and increase of UV radiation caused by pre-industrial tropical volcanic eruptions. Science Reports 9, 9435 (2019). https://doi.org/10.1038/s41598-019-45630-0
- Laschewski G, Matzarakis A. Weather-Related Human Outdoor Behavior with Respect to Solar Ultraviolet Radiation Exposure in a Changing Climate. Atmosphere 2022, 13(8), 1183; https://doi.org/10.3390/atmos13081183
- Ivanov IV, Mappes T, Schaupp P, Lappe C, Wahl S. Ultraviolet radiation oxidative stress affects eye health First published: 30 March 2018 https://doi.org/10.1002/jbio.201700377Citations: 54
- Behar-Cohen F, Baillet G, de Ayguavives T, et al. Ultraviolet damage to the eye revisited: eye-sun protection factor (E-SPF), a new ultraviolet protection label for eyewear. Clinical Ophthalmology, 2014;8:87-104.
- Gaillard ER, Zheng L, Merriam JC, Dillon J. Age-related changes in the absorption characteristics of the primate lens. Investigative Ophthalmology and Vision Science, 2000 May;41(6):1454-9.
- Cullen, AP. Ozone depletion and solar ultraviolet radiation: ocular effects, a United Nations environment programme perspective. Eye & Contact Lens, 2011; 37(4), 185-190.
- Rooney JF, Bryson Y, Mannix ML, et al. Prevention of ultraviolet-light-induced herpes labialis by sunscreen. Lancet, 1991 Dec 7;338(8780):1419-22.
- Morison WL. Effects of ultraviolet radiation on the immune system in humans. Photochemistry and Photobiology, 1989 Oct;50(4):515-24.
- Bailey RL, Arullendran P, Whittle HC, Mabey DCW. Randomised controlled trial of single-dose azithromycin in treatment of trachoma. Lancet, 1993;342:453–6.
- Ramesh A, Kovats S, Haslam D, et al. The impact of climatic risk factors on the prevalence, distribution, and severity of acute and chronic trachoma. PLoS Neglected Tropical Disease, 2013 Nov 7;7(11):e2513. doi: 10.1371/journal.pntd.0002513. PMID: 24244768; PMCID: PMC3820701.
- Basáñez MG, Pion SD, Churcher TS, Breitling LP, Little MP, Boussinesq M. River blindness: a success story under threat? PLoS Medicine, 2006 Sep;3(9):e371. doi: 10.1371/journal.pmed.0030371. PMID: 17002504; PMCID: PMC1576321.
- Cheke RA, Basáñez MG, Perry M, et al. Potential effects of warmer worms and vectors on onchocerciasis transmission in West Africa. Philosophical Transcripts of the Royal Society, London, Biological Science, 2015 Apr 5;370(1665):20130559. doi: 10.1098/rstb.2013.0559.
- Cromwell EA, Osborne JCP, Unnasch TR, et al. Predicting the environmental suitability for onchocerciasis in Africa as an aid to elimination planning. 2021;PLoS Negl Trop Dis 15(7): e0008824. doi:10.1371/journal.pntd.0008824
- Nutman TB. Future directions for vaccine-related onchocerciasis research. Trends in Parasitology, 2002 Jun;18(6):237-9.
- Gustavsen K, Hopkins A, Sauerbrey M. Onchocerciasis in the Americas: from arrival to (near) elimination. Parasitic Vectors, 2011 Oct 25;4:205.
- Echevarría-Lucas L, Senciales-González JM, Medialdea-Hurtado ME, Rodrigo-Comino J. Impact of Climate Change on Eye Diseases and Associated Economical Costs. International Journal of Environment and Research in Public Health, 2021 Jul 5;18(13):7197.
- Auger N, Rhéaume MA, Bilodeau-Bertrand M, et al. 2017, Climate and the eye: Case-crossover analysis of retinal detachment after exposure to ambient heat. Environmental Research, 2017, 157, 103-109.
- Jacob, Daniel J, and Darrel A Winner. 2009. Effect of climate change on air quality. Atmospheric Environment 43(1): 51-63
- Hong J, Zhong T, Li H, et al. Ambient air pollution, weather changes, and outpatient visits for allergic conjunctivitis: a retrospective registry study. Science Reports, 2016 Apr 1;6:23858. doi: 10.1038/srep23858ence
- Shin J, Lee H, Kim H. Association between Exposure to Ambient Air Pollution and Age-Related Cataract: A Nationwide Population-Based Retrospective Cohort Study. International Journal of Environment and Research in Public Health, 2020, 17(24). doi:10.3390/ijerph17249231
- Chang KH, Hsu PY, Lin CJ, Lin CL, Juo SH, Liang CL. Traffic-related air pollutants increase the risk for age-related macular degeneration. Journal of Investigational Medicine, 2019 67(7), 1076-1081.
- Miyazaki D, Fukagawa K, Fukushima A, et al. Air pollution significantly associated with severe ocular allergic inflammatory diseases. Science Reports, 2019 9(1), 18205. doi:10.1038/s41598-019-54841-4
- Lelieveld J, Beirle S, Hörmann C, et al. Abrupt recent trend changes in atmospheric nitrogen dioxide over the Middle East. Science Advice, 2015 Aug 21;1(7):e1500498. doi:10.1126/sciadv.1500498.
- Vohra K, Marais EA, Bloss WJ, Schwartz J, Mickley LJ, Van Damme M, Clarisse L, Coheur PF. Rapid rise in premature mortality due to anthropogenic air pollution in fast-growing tropical cities from 2005 to 2018. Science Advice, 2022 Apr 8;8(14):eabm4435. doi: 10.1126/sciadv.abm4435.
- Miller FA, Young SB, Dobrow M, Shojania KG. Vulnerability of the medical product supply chain: the wake-up call of COVID-19. BMJ, 2021 Apr;30(4):331-335.
- Sarkar S, BMJ 2022; 378 doi: https://doi.org/10.1136/bmj.o2141
- Ahmad B, Patel BC. Trachoma. [Updated 2022 May 29]. https://www.ncbi.nlm.nih.gov/books/NBK559035/
