The first in a series of quarterly online events, supported by Alcon, took place recently. Dr Byki Huntjens, of City, University of London, delivered an interactive presentation covering the topic of toric contact lenses, a summary of which I present here (figure 1).
Alcon Talks in Optician Contact Lens Monthly 2023:
- March: Toric contact lenses
- June: Contact lens comfort
- September: Dry eye disease
- December: Multifocal contact lens options
Figure 1: Buki Anthony (left) introduces Dr Byki Huntjens
The session covered the following topics:
- Toric contact lens comfort
- Prevalence and the trends of astigmatism
- Criteria for fitting toric lenses
- The pros and cons of toric lens designs
- Tips and guidelines for fitting toric lenses to obtain and maintain optimal vision
Toric Contact Lens Comfort
The first topic of discussion was based around a well-known study by Dr Carole Maldonado and colleagues from the University of Manchester in 2021.1 This had investigated the association between comfort and vision in daily disposable, soft toric contact lenses. Results of this study indicate that greater subjective vision quality results in greater comfort scores, even though high and low contrast acuity was not statistically different between lenses. The take home message from this study is that toric contact lens comfort is directly related to subjective vision quality (figure 2).
Figure 2: The association between comfort and vision in daily disposable, soft toric contact lenses

This was an important point referred to throughout the presentation. Dr Huntjens explained: ‘We are so driven by numbers as eye care professionals (ECPs) but, in reality, patients are more concerned about their subjective vision quality. We should question ourselves; are we asking the right questions and performing the right tests to establish what the patient is really saying?’
Astigmatism Prevalence and Trends
Next, Dr Huntjens explored the prevalence of astigmatism and the factors that can influence this number. For example, if the definition is inclusive of even the lowest amount of astigmatism at 0.25DC, this will obviously result in higher prevalence rates than when the definition has a minimum threshold of 0.75DC. As ECPs, a 0.75DC is the lowest amount commonly taken to warrant soft toric lens fitting, so perhaps is a better representation.
It is also important to establish if data is based on one eye alone or consider both eyes. Equally, age is also a crucial factor in determining the prevalence rates of astigmatism. Aging can lead to changes within the crystalline lens, which can undoubtedly influence the level of astigmatism.
Lastly, regional differences can also influence prevalence rates. For example, the prevalence of astigmatism in Africa is about 11% whereas in the Americas, it is reported to be around 46%.2 Dr Huntjens referred to a recent meta-analysis conducted by Hashemi and colleagues.2 Using data from this study, the estimated global prevalence of astigmatism (defined as >0.50DC) is estimated to be around 40% among those over 30 years of age (figure 3). This study used over 122,000 participants in the analysis. If we then assume that the population wearing contact lenses is representative of the larger population requiring visual correction, you would expect approximately 40% of all our soft lens fits should be toric.
Figure 3: Prevalence of astigmatism in a sample of 122,0002
Delving into another study looking at prevalence rates of astigmatism, Dr Huntjens referenced Young and colleagues who studied a UK database of 11,624 spectacle prescriptions.3 They found that one in two patients have an astigmatism of 0.75DC or greater in at least one eye, and one in four in both eyes. Also, the prevalence of this level of astigmatism was found to be double in myopes compared to hyperopes (~32% vs ~16%).
The prevalence of ‘with-the rule’ astigmatism is slightly higher than ‘against-the-rule’, at around 33% versus 29%.3 Although oblique astigmatism is not very common, this can vary substantially with ethnicities. Referring to the International Contact Lens Prescribing Report from 2020, Dr Huntjens described the trends in the proportion of toric lenses out of all soft lens fittings between the year 2000 and 2020.4 For the 20 countries included in the report, it is apparent that five are lagging behind on toric lens fits; namely, Japan, Lithuania, Russia, Bulgaria and Taiwan (figure 4).
Figure 4: Toric lens fitting trends by nation from 2000 to 20204
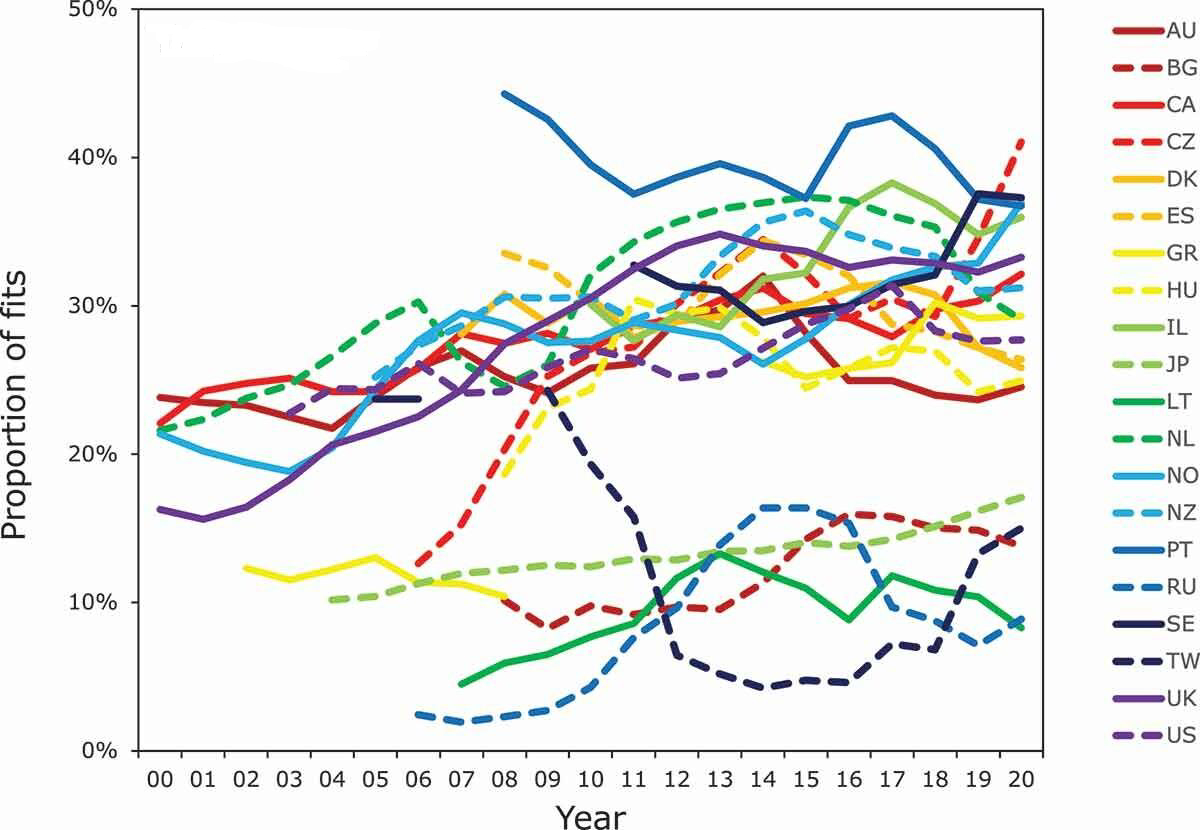
The results of this report show that soft toric fits represent, on average, around 28% of all soft lens fits. However, as mentioned earlier, the prevalence of clinically significant astigmatism was around 40%. So, in reality, we would expect to see this reflected in the number of soft toric fits, but this appears to be much lower.
Dr Huntjens proposed that the real figure may be even lower still, when looking at consumer data from different contact lens providers. She believes this may be in the region of around 10%. The variation in data may be due to the fact that the CL Prescribing Report4 collates information from ‘keen’ practitioners who work with contact lenses regularly. Overall, the percentage is quite low.
Criteria for Fitting Torics
Dr Huntjens continued: ‘Considering how so many parameters are now available for soft toric contact lenses in different wear modalities, major factors contributing to fitting habits, then the question that needs addressing is this; what is holding us back as ECPs?’
Level of astigmatism
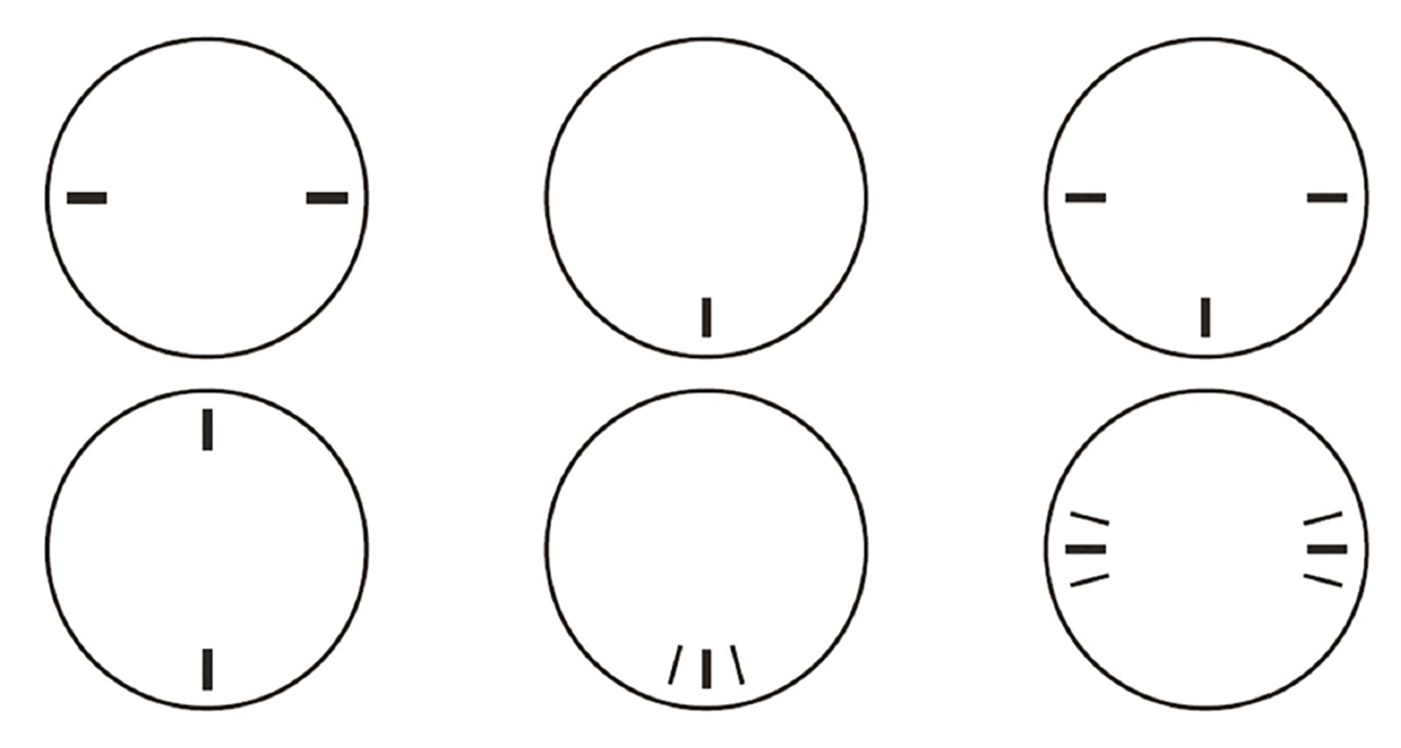
Obviously, each patient is different and should be assessed individually. The degree of astigmatism is very important, and so extra attention should be given to the subjective refraction, ensuring to take time on the Jackson cross-cyl to ensure an accurate result. An understanding of the visual impact the patient reports during the cross-cyl is crucial in this. This is due to the fact that some patients may be visually sensitive to even small changes, and so this needs to be factored in during soft toric fits. Any rotation or instability in patients with higher blur sensitivity will be picked up by them quite readily (figure 5).
Figure 5: Cross-cylinder testing may indicate a patient’s level of blur sensitivity and, therefore, tolerance to soft toric lenses

Dr Huntjens continued with this point as a possible reason underlying a common myth about astigmatism correction with contact lenses. ‘Aspheric designs do not successfully mask or correct astigmatism. Many years ago, soft lens materials were different, of a high modulus and resulting in thicker lenses.’ These may have allowed some masking of low levels of astigmatism; something, she explained, she was taught during her university time. However, this is not applicable nowadays with the materials and modalities currently available.
Axis selection
The next point of consideration was the cylinder axis. Dr Huntjens suggested that, when choosing a trial lens, it is best to prioritise matching the axis, then the cylinder power and finally the sphere power.
For a ‘with-the-rule’ astigmatism, you can round towards 180° and, for an ‘against-the-rule,’ you can round towards 90°. One must, of course, consider the nasal rotation that can occur with blinking. Although this is not a hard and fast rule, it is a suggestion which could provide toric fit success.
Ocular dominance
When a patient has a dominant eye, special consideration should be made to this eye, focusing on best visual acuity in this eye to support best comfort and vision overall.
Visual needs
The final point in the selection of a toric lens should be the visual needs of the patient. For example, do they need contact lenses for sport and, if so, what kind of sport? Is it one involving large head movements? If the latter is true, then there should be a particular focus on the rotational stability of the lens. It is important to think about what your patient wants, why they want contact lenses and what is important to them. This should be reassessed at the aftercare, as priorities and individual circumstances can change.
Listening to the visual needs of the patient is, therefore, very important. Equally important is the presence of eye strain. Eye strain has been shown to reduce when an astigmat is fitted with toric lenses, compared to best sphere equivalent lenses.
Initial observations
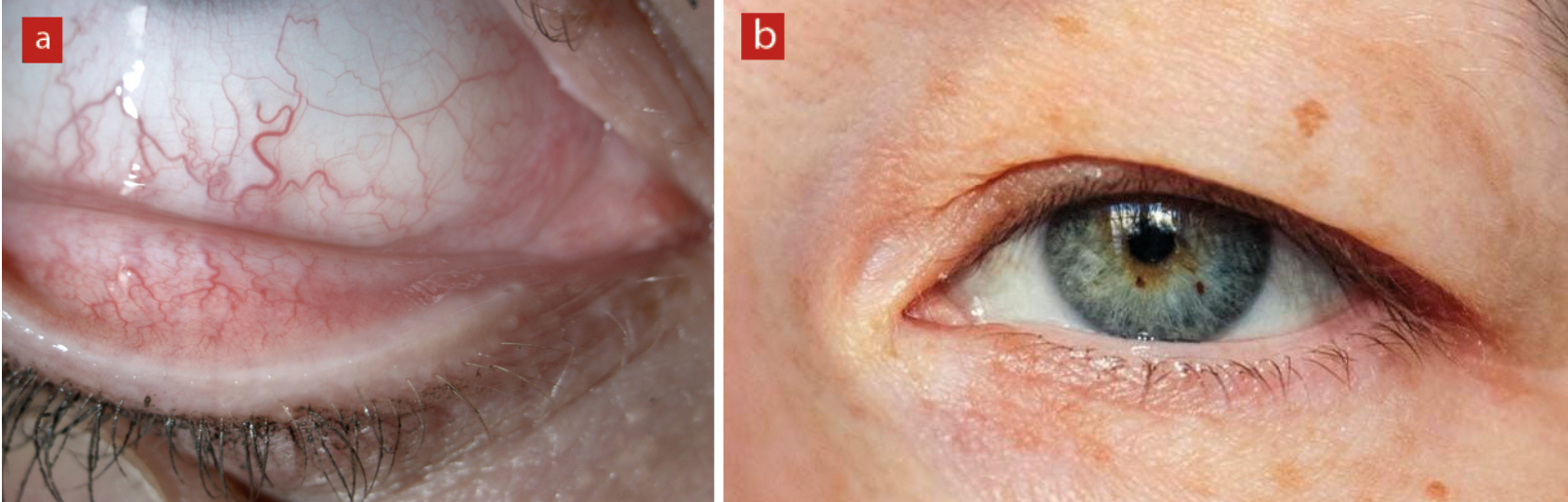
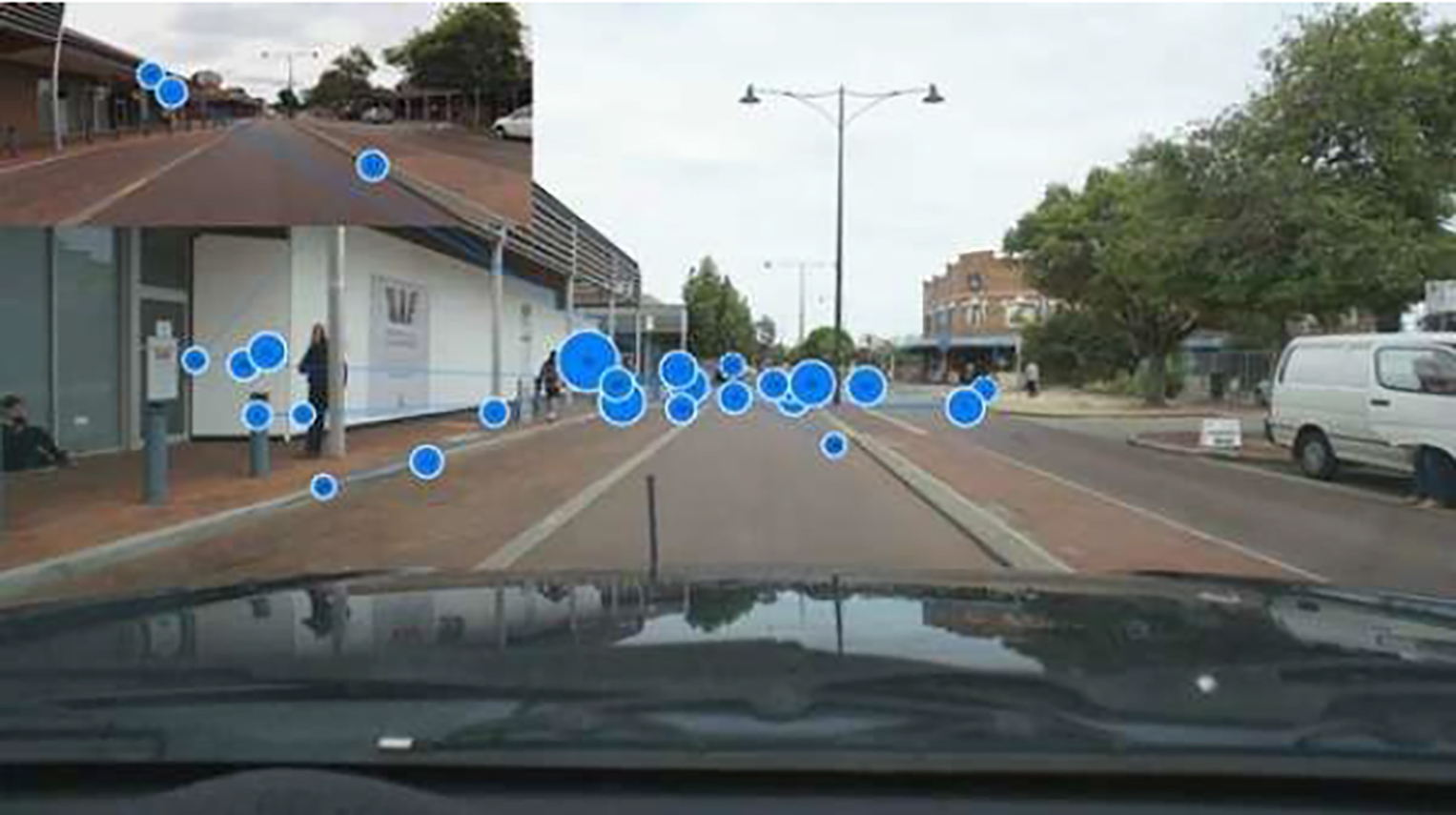
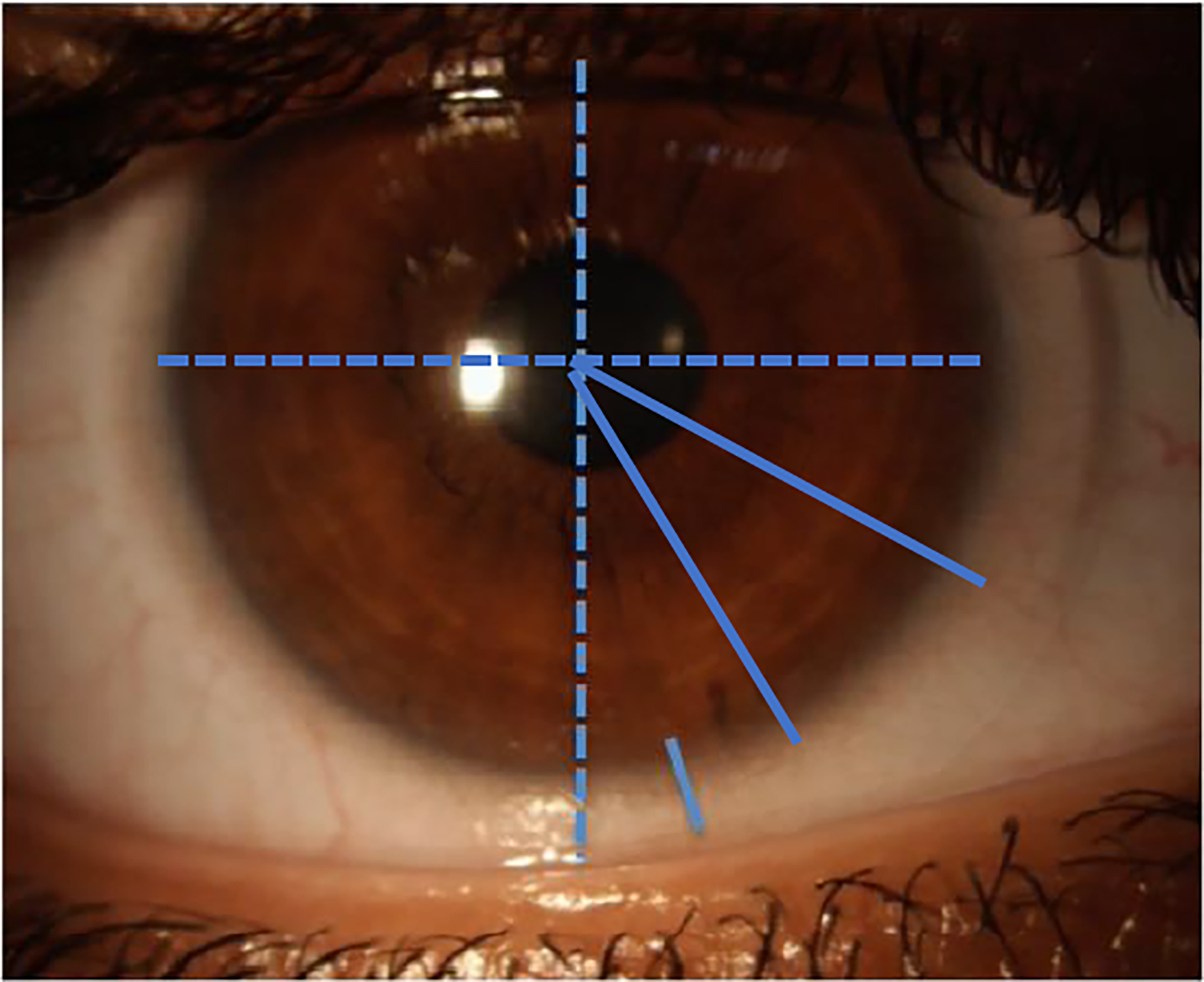
Dr Huntjens went on to explain the visual cues that ECPs can pick up on to further help with their examination and management. Signs such as excessive blinking, red and injected eyelid margins and lid tonicity can provide vital information about the presence of any lid margin or dry eye diseases, with the latter giving an indication on how the lens will fit (figure 6). The reason for this is that soft toric lens stabilisation methods rely on the pressure from the eyelids to maintain the axial alignment and stability in rotation.
Figure 6: Observations of (a) hyperaemia or (b) lid tonicity may help predict how well a toric lens rotates on eye
Stabilisation techniques
After the prevalence rates and fitting criteria were covered, Dr Huntjens directed the conversation to stabilisation techniques and their importance (figure 7).
Figure 7: Schematic representation of different toric lens stabilisation techniques. (a) Prism ballast. (b) Peri-ballast. (c) Modified prism/peri ballast (reversed prism). (d) Dual thin zone. (e) Accelerated stabilisation. Note; the blue shading represents thicker areas
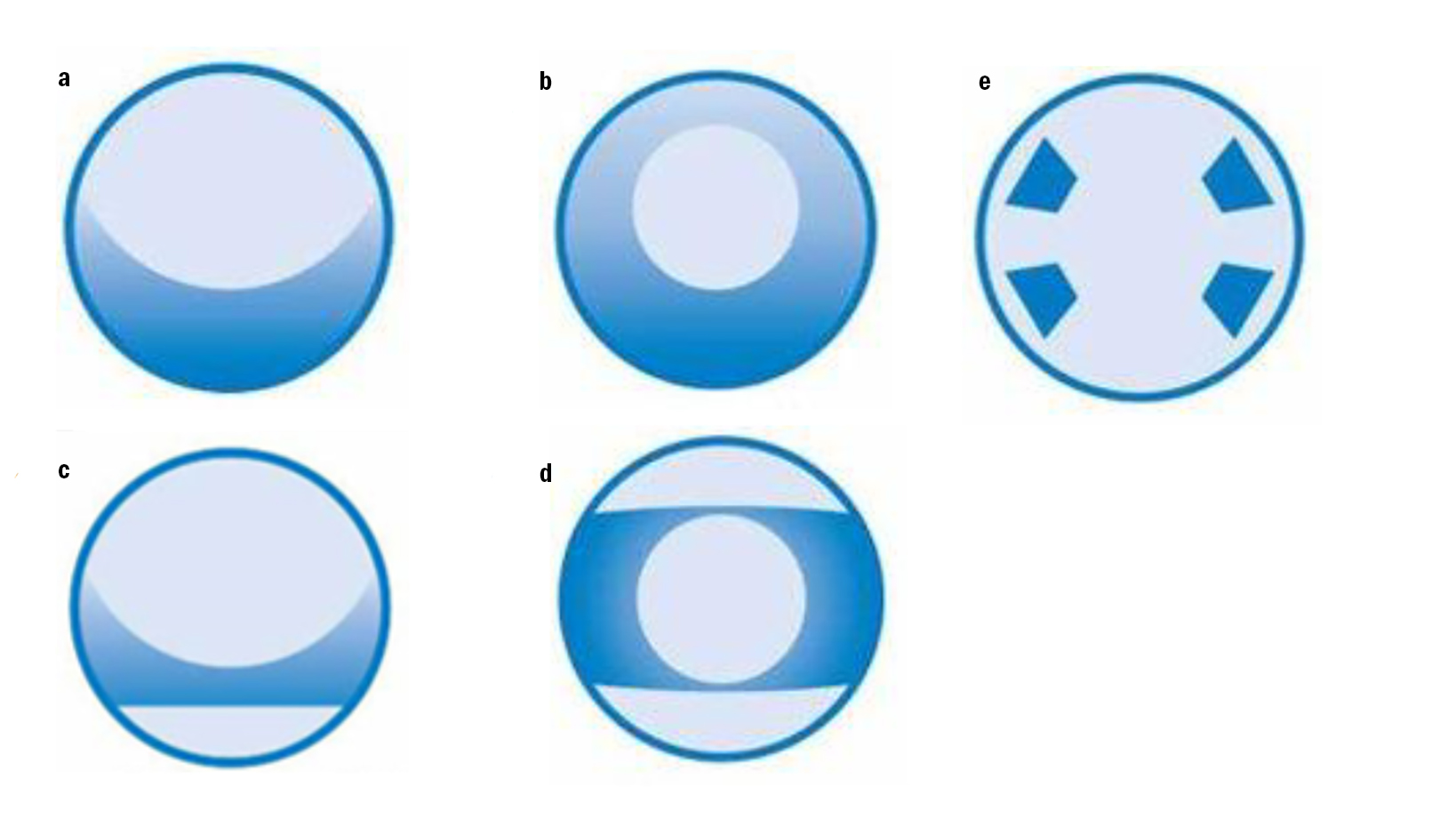
Prism ballast
Prism ballast design relies on vertical prism to orientate and stabilise the lens. In principle, there is a thicker profile at the bottom, towards the base, and the thinner portion is underneath the upper lid. This design squeezes the thicker portion of the lens towards the lower lid, an effect often described as ‘the watermelon seed principle’.
Such a design is quite traditional and there are some disadvantages to it. The thickness profile reduces oxygen transmissibility in specific areas. Also, prism ballast has been reported to cause discomfort in some patients due to the lid interaction.
Peri-ballast
The peri-ballast design follows a similar concept to prism ballast, but instead it is the superior portion of the lens which is thinned, producing a prism-like rotational stabilisation effect. An advantage of such designs is that they have been modified so the prism is restricted towards the lens periphery, allowing for central prism-free optics. Also, as these lenses are a little bit thinner, there is greater oxygen transmissibility.
Modified prism/peri ballast (reversed prism)
Modifications to the previous traditional designs have been made in order to develop both thinner and more comfortable lenses. These more recent designs have a thinner inferior lens periphery and therefore improved oxygen performance. Such modified designs are also known as reversed-prism design and the majority of disposable lenses employ this design.
Dynamic stabilisation
Dynamic stabilisation toric lens designs incorporate a thin zone at the top and at the bottom of the lens, which is covered by the eyelids. One example of dynamic stabilisation is the dual thin zone lens design.
The thicker part in the centre is squeezed between the lid margins. Unlike the prism-ballast and peri-ballast designs, which only use the superior lid for stabilisation, this technique employs both upper and lower lids for support.
At this point, Dr Huntjens referred back to the original points covered when considering toric fitting, highlighting that the tonicity of the eyelids will play an important role in these lens designs. For instance, if a patient has a weak lower lid, the dual thin zone design may not work as well. Apparently, the dual thin zone design is most successful when the thickness differential of the horizontal and vertical profile is the greatest. So, higher myopic prescriptions and also ‘against-the-rule’ cylinder corrections would work best because the wedge effect will be maximised. Conversely, such designs may work less well for lower prescriptions and oblique cylinder corrections, although Dr Huntjens explained that, personally, she has not experienced such difficulties.
The other dynamic stabilisation technique discussed was the accelerated stabilisation design. This also uses thickness differences across its profile, utilising both upper and lower eye lid movements to achieve rotational stability. With this design, there are four zones of stability, with the thicker profile placed in the mid-periphery of the lens. As such, this design aims to minimise lens rotation while maintaining minimal thickness under both lids.
Lens Design, Vision and Ocular Health
The conversation next turned towards the effects of the various different designs upon vision and ocular health.
Starting off with vision, Dr Huntjens discussed the impact that different designs have upon the optic zone. She used an image of different reusable lenses with a prescription of -3.00/-1.25 x 180 (figure 8). An accompanying image was used to help visualise the optic zone, which is typically 7.5mm in diameter.
Figure 8: (a) Different lens design profiles and their influence upon (b), a typical optic zone
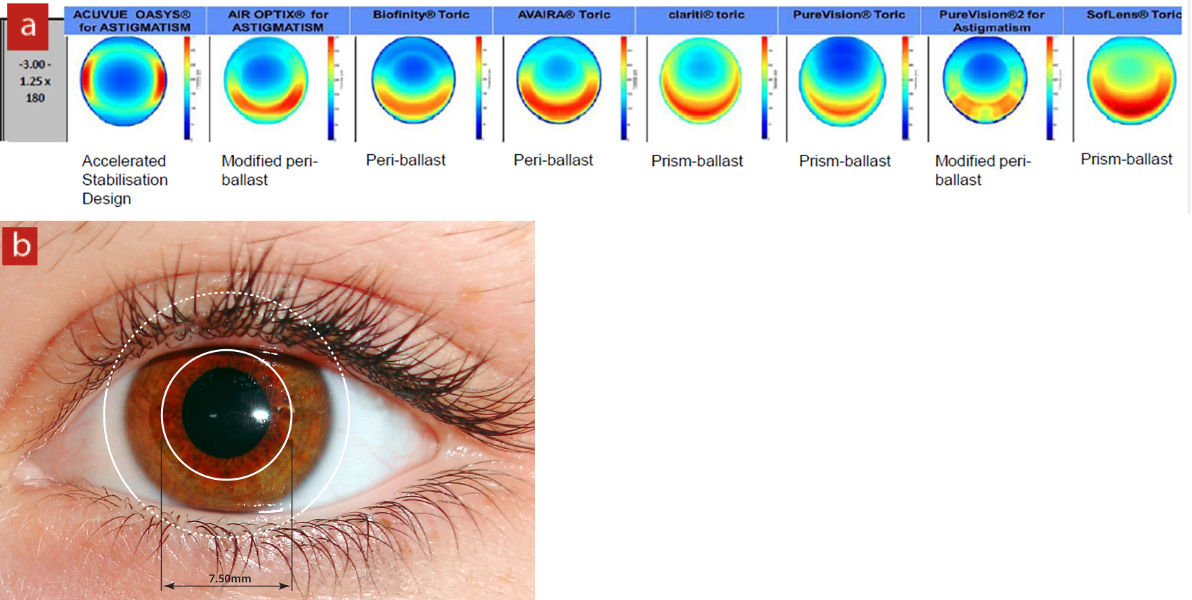
The lenses utilising the prism ballast and peri-ballast designs have vertical prism in the central optic zone. This is of particular interest for monocular astigmats fitted with soft toric lenses, or those wearing a mix of toric designs, since that vertical prism imbalance could create or even exacerbate disturbances in binocular vision function.
Practitioners should, therefore, be aware of not just lid tonicity, but also of any impact of design on the central optic zone. Consideration of this during lens selection will be particularly important when fitting monocular astigmats with pre-existing binocular vision anomalies.
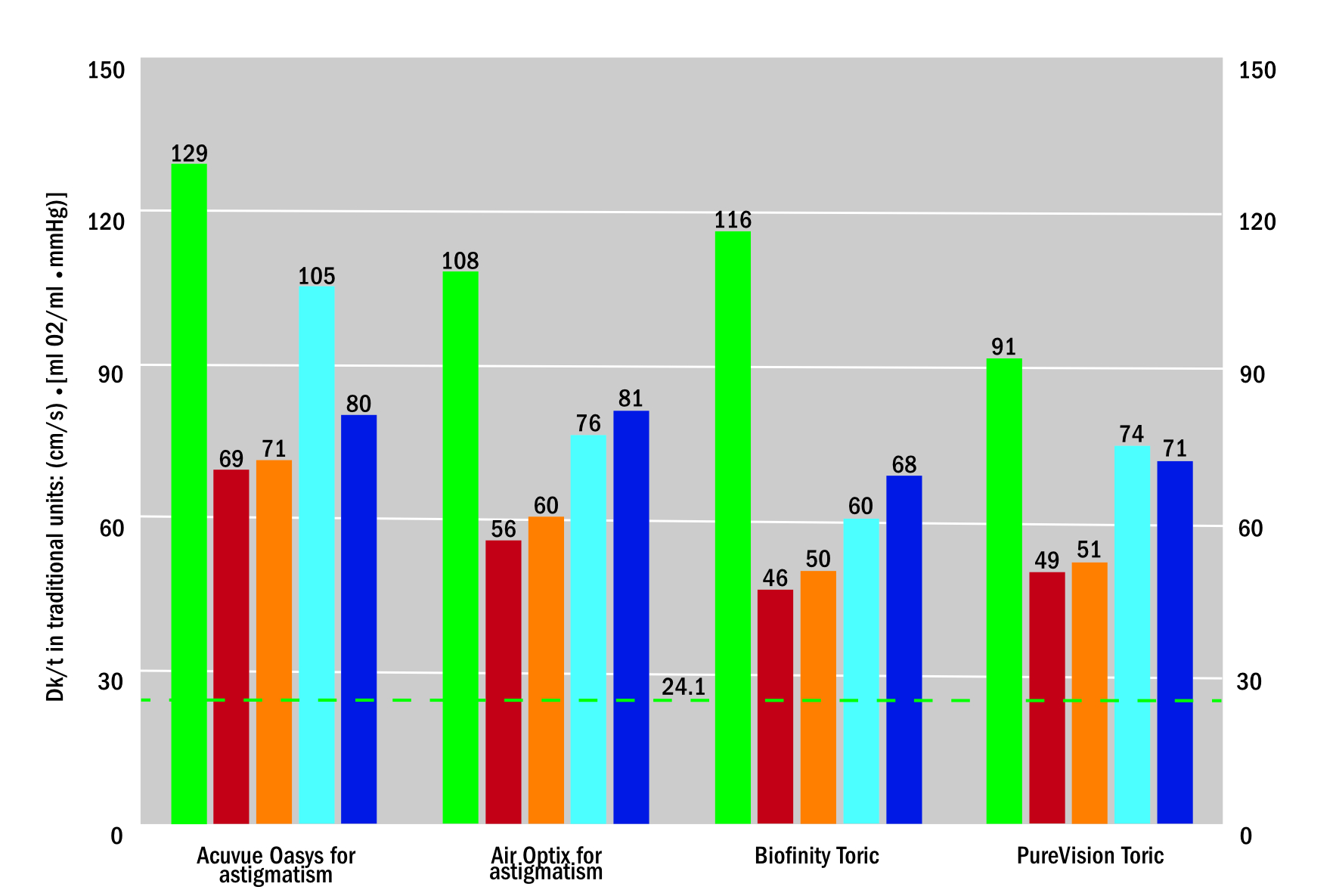
With regards to ocular health, it can be seen that the thickness profiles of toric lenses have an effect upon oxygen transmissibility. Figure 9 shows four different reusable toric lens designs which, despite sharing the same power and all thickness profiles being standardised, vary in inferior lens thickness. Thicker inferior lens profiles have less oxygen transmissibility in these regions.
Figure 9: Thickness profiles of various reusable toric contact lenses. Thicker areas (in red) will have reduced oxygen transmissibility
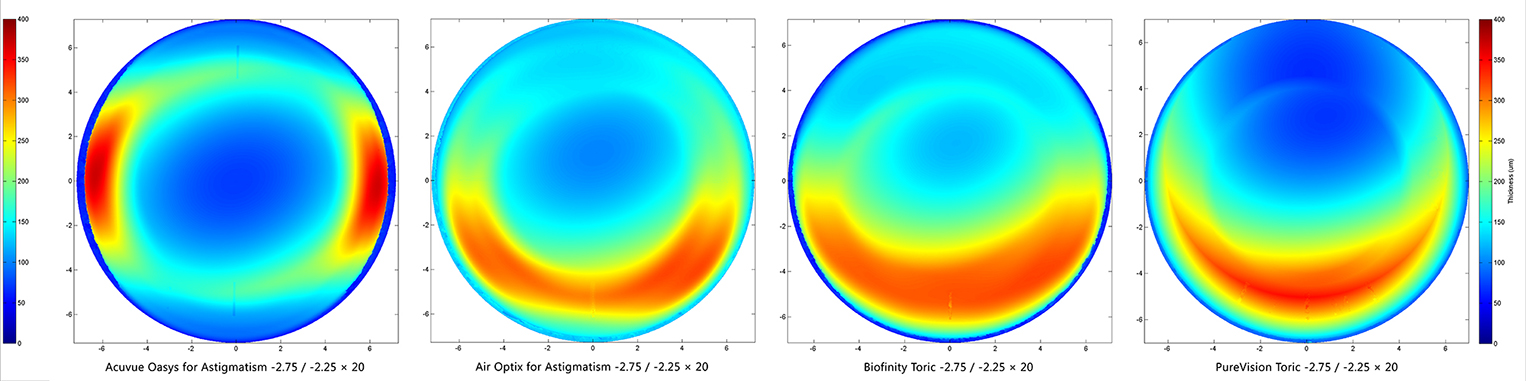
Dr Huntjens continued by comparing oxygen transmissibility profiles from two internal Alcon studies (figure 10). Surprisingly, there is less variation in reusable lenses than in daily disposables when it comes to oxygen transmission. Though reusables are a little bit thicker, Dr Huntjens explained she expected similar patterns in daily disposables. There is also some influence from centre thickness; for some lens designs, the thickness is evenly distributed, allowing a thinner central zone, while for others the thickness is displaced vertically; this could induce some prism.
Figure 10: Oxygen transmissibility profiles of a range of one day or reusable contact lens designs
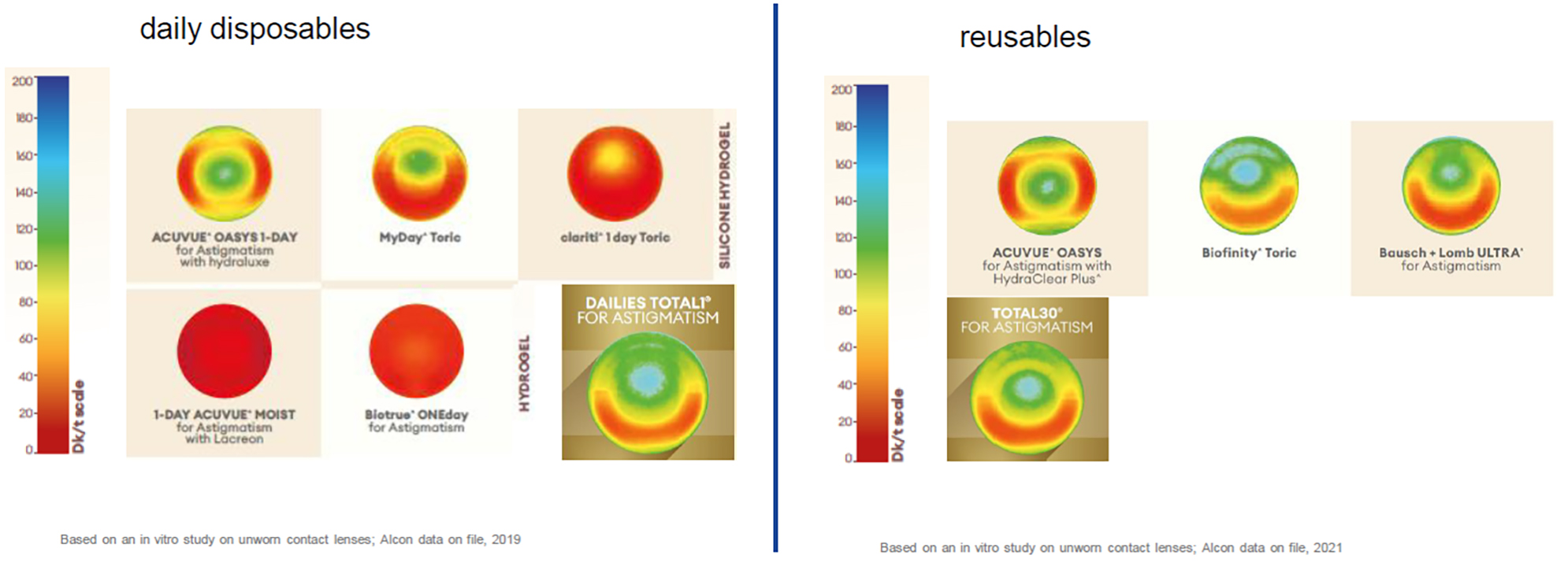
Consideration of the refractive power profile and its impact upon oxygen transmissibility (Dk/t) is important as there is a policy for lens manufacturers to state the Dk/t based on a -3.00DS reusable contact lens profile. Looking at figure 10, this does not provide clinicians with a useful indication of oxygen transmissibility, particularly for toric lenses, as it is quite evident that there is a big variation across the lens profile. The influence of refractive power upon transmissibility is nicely summarised in figure 11.
Figure 11: Oxygen transmission (Dk/t) within the central 7.50 mm of a range of soft toric lenses
Toric Contact Lens Fitting
The discussion now turned to the actual lens fitting. Dr Huntjens asked: ‘If we decide to fit a daily disposable lens, for example, and have established what design is best in that case; what are we doing with the prescription?’
As already discussed, a good, accurate subjective refraction is essential, as is paying attention to the patient and taking extra care during the Jackson cross-cyl measurement of astigmatism. Converting both principal meridians is also as important.
When choosing the best lens, it is important to select the lens based on cylinder axis first, then the power of the cylinder, and lastly the sphere power. There are some limitations as, typically, toric contact lens cylinder powers are only available in steps of half a dioptre. If the desired prescription falls between two powers, it is generally advised to select the lower cylinder power.
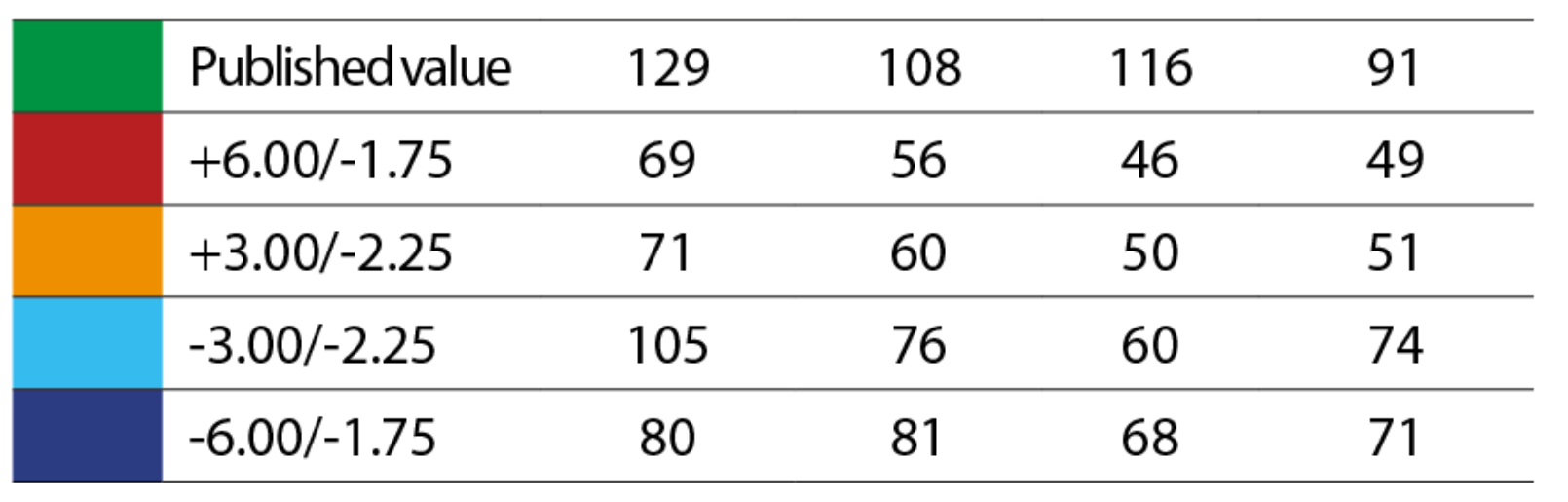
Once the lens is on the eye, assessing the fit is important. A lens that is too tight will not rotate properly and the astigmatic correction will not align across the desired meridian. It may rotate progressively as the lower lid spins it, but it may also become immobile completely (figure 12). So, a lens where the reference marks are a long way off from where they should be would be suspicious, particularly of a tight lens. With a loose lens, there may be a chance of it spinning around and decentring. A well-fitting lens should enable to stabilisation system to work while keeping the lens on axis.
Figure 12: How fit influences toric lens rotation
When assessing visual performance with toric lenses, it is important to not only assess vision in the straight-ahead direction, but also take into account how viewing takes place throughout the typical day of the patient. For example, when driving their car and changing lanes, the patient will be looking over the shoulders. Daily tasks require clear vision in different directions.
Dr Huntjens advised that, when checking rotational stability, patients should not only be asked to blink and look directly ahead to assess the rotation mark, but also to move the eyes to imitate movements that might be expected in real life. For example, looking up and to the side as if looking at the rear-view mirror when driving. Referring to an image of a driver’s view (figure 13), Dr Huntjens demonstrated the many different directions of gaze required when driving. Though the eyes are still facing in a forward direction, there is some deviation from the central fixation point. The same is true when playing many sports.
Figure 13: Different points of fixation showing changing direction of gaze when driving.
Next, the lens surface is an important concept to consider. Dr Huntjens explained how the first Purkinje image can reveal areas of drying out. If a person blinks a lot, this area will readily be replenished. However, for those who have lower blink rates, such drying on the surface will translate into subjective vision problems.
Another important point is to remember that ECPs are not trying to correct any misalignment of lens markings. These will always sit in the same place, even after making the appropriate cylinder axis changes. Clinicians manage the astigmatism of the lens, but do not manage the axis of rotation. Lens markings vary by manufacturer (figure 14), and there are a number of methods for measuring lens rotation (figure 15). For instance, some slit lamps have an in-built reticule that is calibrated in degrees.
Figure 14: Different manufacturers use different lens markings to show lens orientation
Unfortunately, many slit lamps used in eye care practice do not have this feature. Instead, the slit beam can be narrowed and rotated to align with the reference line. The axis can then be read off the slit lamp illumination system. Another method is to use sphero-cylindrical over-refraction, adding the lens prescription and over-refraction to an online calculator to figure out the final power. Such calculators are readily available from manufacturers.
Figure 15: Methods of measuring lens rotation. (L-R) (a) Slit-lamp reticule. (b) Slit-beam orientation alignment. (c) Trial frame and lenses
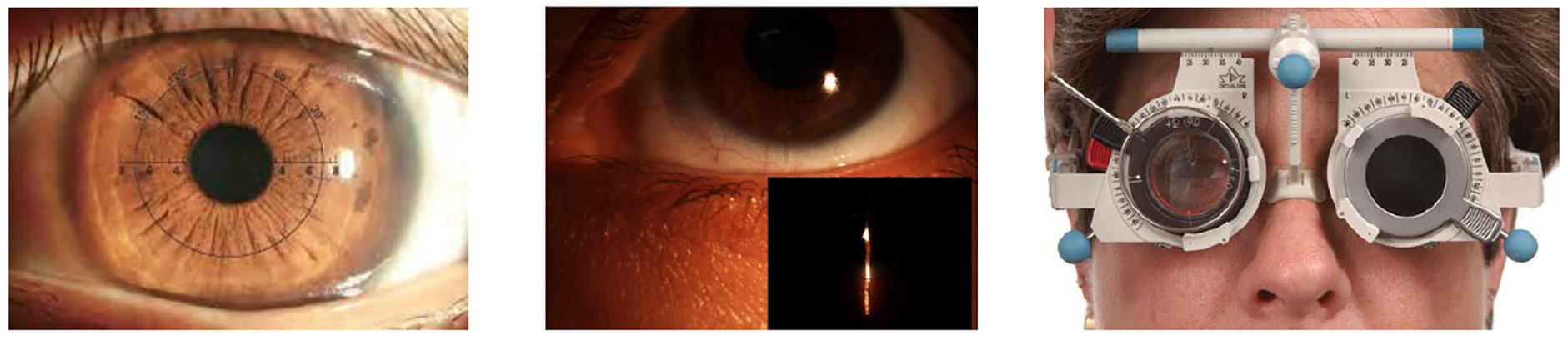
Alternatively, the trial contact lens power and over-refraction can be added into a trial frame and then neutralised with a focimeter. This technique is particularly helpful in cases of expensive custom lenses with high astigmatic powers.
The most common method appears to be use of ‘guesstimations’ in estimating the angle of rotation. Though students are educated on best practice, practitioners become good over time at estimating the angles without checking the slit lamp settings. Some manufacturers add extra reference lines on either side of the main marking which aids in this, and is helpful in establishing if a lens is 10 or 15 degrees out. A lot of disposable lenses come in axis intervals of 10 degrees so this can work quite nicely. If one thinks of a clock face, then each ‘hour’ will represent 30 degrees and, from there, smaller rotations may be estimated (figure 16).
Figure 16: Dividing the cornea into segments of a clockface helps with angle estimation. Three hours is 90 degrees, one hour 30 degrees, half of that 15 degrees
Dr Huntjens explained her personal preference to be two horizontal markings, as the slit beam will go through both orientation markings, so making it easier to see the rotation. There are some designs where the scribe mark is at 12 and 6 o’clock, but the marking at 12 o’clock can be redundant if the top lid is covering this.
When observing a lens with a 6 o’clock scribe mark, Dr Huntjens explained how it was possible to detect the presence of nasal rotation on blink. During the blink cycle, the closure of the lids proceeds from the outer canthus towards the inner canthus almost like a ‘zipper effect’. This movement is caused by the action of the lower lid, which will push a bit more nasally. The top lid, on the other hand, tends to travel down and then back up. This lid movement will push the lens from the bottom, up nasally, spinning the lens. Thus, some lenses do not necessarily rotate to the horizontal or vertical principal meridians but, instead, have a slight nasal rotation depending on lid tension. Dr Huntjens recommends looking for such rotation in practice, particularly when it is more than five degrees. This would suggest that the lens design is not correct for that patient and a different toric design should be chosen.
Final Power Calculation
The session concluded with a conversation about calculating the final prescription of the lens. It is well known that suboptimal vision or poor comfort can lead to contact lens dropout. Dr Huntjens discussed an example to illustrate this point, one which might present in practice when an online calculator is not available.
Consider you are fitting a soft toric contact lens of a -3.25 with a -1.25 at an axis of 30 and then a subjective over-refraction (OR) of a +0.75 with a -1.00 at 55.
Dr Huntjens recommends you add three lenses in a trial frame and then focimeter them. You start off with the sphere, which is the combination of the two spherical components, one from the toric lens and one from the subjective over-refraction, and you add them together. Then, add the cylinder from the contact lens and then the cyl from the subjective over-refraction, which should then be neutralised with the focimeter.
This is an efficient way to determine the prescription the patient needs before trying another diagnostic lens. You can even account for any rotation of the toric lens by adjusting the axis position. However, if such a method is not possible, Dr Huntjens recommends contacting the lens manufacturers for help.
And Finally…
Dr Huntjens finished off the webinar highlighting the great online calculators that are available to help with figuring out the final prescription and axis of the toric lens based on over-refraction and rotation. She continued: ‘There has never been a better time to be a contact lens wearer with astigmatism. There are so many options to choose from, and so it is vital we give our patients the best vision possible. Perhaps, the fitting is not as straightforward as a spherical fit. However, you will always pass failure on the way to success.’
- Buki Anthony MOptom Professional Education and Development Manager, UK and Ireland. Dr Byki Huntjens is a senior lecturer and Lead for Teaching Excellence in the School of Health representing optometry, City, University of London.
References
- Maldonado-Codina, C, Cornago, MN, Read, ML, Plowright, AJ, Vega, J, Orsborn, GN and Morgan, PB, 2021. The association of comfort and vision in soft toric contact lens wear. Contact Lens & Anterior Eye, 44(4), p.101387
- Hashemi, H, Fotouhi, A, Yekta, A, Pakzad, R, Ostadimoghaddam, H and Khabazkhoob, M, 2018. Global and regional estimates of prevalence of refractive errors: Systematic review and meta-analysis. Journal of Current Ophthalmology, 30(1), pp.3-22
- Young, G, Sulley, A and Hunt, C, 2011. Prevalence of astigmatism in relation to soft contact lens fitting. Eye & Contact Lens, 37(1), pp.20-25
- Morgan, PB and Efron, N, 2022. Global contact lens prescribing 2000-2020. Clinical and Experimental Optometry, 105(3), pp.298-312
