A multicentre study was undertaken recently to evaluate both practitioner and patient acceptability of a new one-day disposable silicone hydrogel contact lens; the sorafilcon A material Hoya One Day lens. This article describes the study and its results.
Background
Daily disposable contact lenses were introduced in 19871 and their greater convenience and other benefits,2 including adverse event rate below 1% per annum,3 have resulted in an increasing market share.4 A large international survey in 2013 concluded ‘The contact lens field appears to be heading toward a true single-use-only, disposable lens market.’4
Initially, soft contact lenses were made of hydrogel materials and some continue to be hydrogel including a leading brand, etafilcon A. In recent years, most major manufacturers, including the manufacturer of etafilcon A, have introduced new daily disposable brands made of silicone hydrogel materials. These have the advantage of higher oxygen transmissibility,2 although hydrogel and in particular etafilcon A has other advantages.1 It is accepted that some patients prefer hydrogel and some silicone hydrogel.5, 6 Differences in performance of different brands of silicone-hydrogel lenses have also been found.7
The most serious complication from contact lens wear is microbial keratitis.8 The risk of microbial keratitis has not been reduced in users of daily disposable and silicone hydrogel lenses, but microbial keratitis in daily disposable lens wear tends to be less severe than with reusable soft lenses.9
Sorafilcon A (Hoya One Day, henceforth referred to as sorafilcon) is a new daily disposable silicone hydrogel lens (8.60:14.20) manufactured by Hoya, a leading contact lens manufacturer in Japan. The aims of the present evaluation were to determine the acceptability of sorafilcon contact lenses for existing wearers of one-day disposable contact lenses in Hungary, Finland, Netherlands, and the UK. A randomised controlled trial design10 was considered, but a limitation of the strict experimental conditions in such trials is that the findings may not relate to everyday clinical practice (see Discussion).11 A more pragmatic evaluation11 was designed, one that closely replicates the in-practice conditions under which new brands of contact lenses are typically evaluated. A similar approach has been used in previous research.12
Real World Evaluation
Manufacturers of one-day lenses provide practitioners with free trial lenses, for patients wearing another brand to trial over a few days. Typically, just one appointment is required to check the fit and vision. The present evaluation builds on this simple approach. As noted above, the study is not a randomised controlled trial (RCT), where researchers must follow a fixed protocol for all tests and procedures, but is a more ‘real world’ evaluation of performance in typical clinical settings. Unlike an RCT, participating clinicians followed their normal clinical procedures. For example, the clinicians in the study were free to use their usual method of assessing ocular health, tear film and lens fit as the goal was not to impose an experimenter-driven protocol on participants. This means the study results are more likely to be applicable to everyday practice than an RCT as will be discussed later.
This evaluation conforms to the tenets of the Declaration of Helsinki and received ethics approval from the Institute of Optometry (UK) and local boards in Finland, Netherlands, and Hungary. The evaluation commenced after regulatory approval in Europe of the sorafilcon product. The evaluation was pre-registered at researchregistry.com (identifier 5367), and the funders and researchers agreed from the outset to publish the findings, regardless of outcome.
Participants
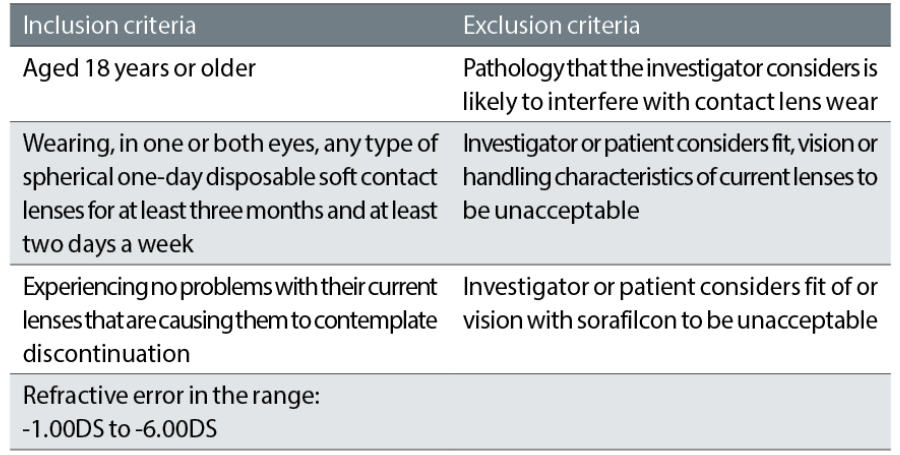
The goal was to evaluate 50 experienced wearers in each country. The selection criteria are detailed in table 1:
Outcome measures
The primary outcome measures were as follows:
- Patients’ self-reported satisfaction with vision
- Lens comfort
- Lens handling
- Willingness to change to sorafilcon
Secondary outcome measures were the investigators’ description of lens fit and vision compared with the participants’ usual lenses. These data were gathered using a practitioner questionnaire and a wearer questionnaire, using visual analogue scales (VAS).
Procedure
When suitable patients wearing spherical one-day lenses within the sorafilcon power range attended for a routine aftercare check, they were invited to participate. Consenting patients returned for an extra visit13 to check back vertex power (BVP) and to confirm that the vision and fit with sorafilcon lenses were acceptable. If so, were issued with 10 pairs of trial lenses.
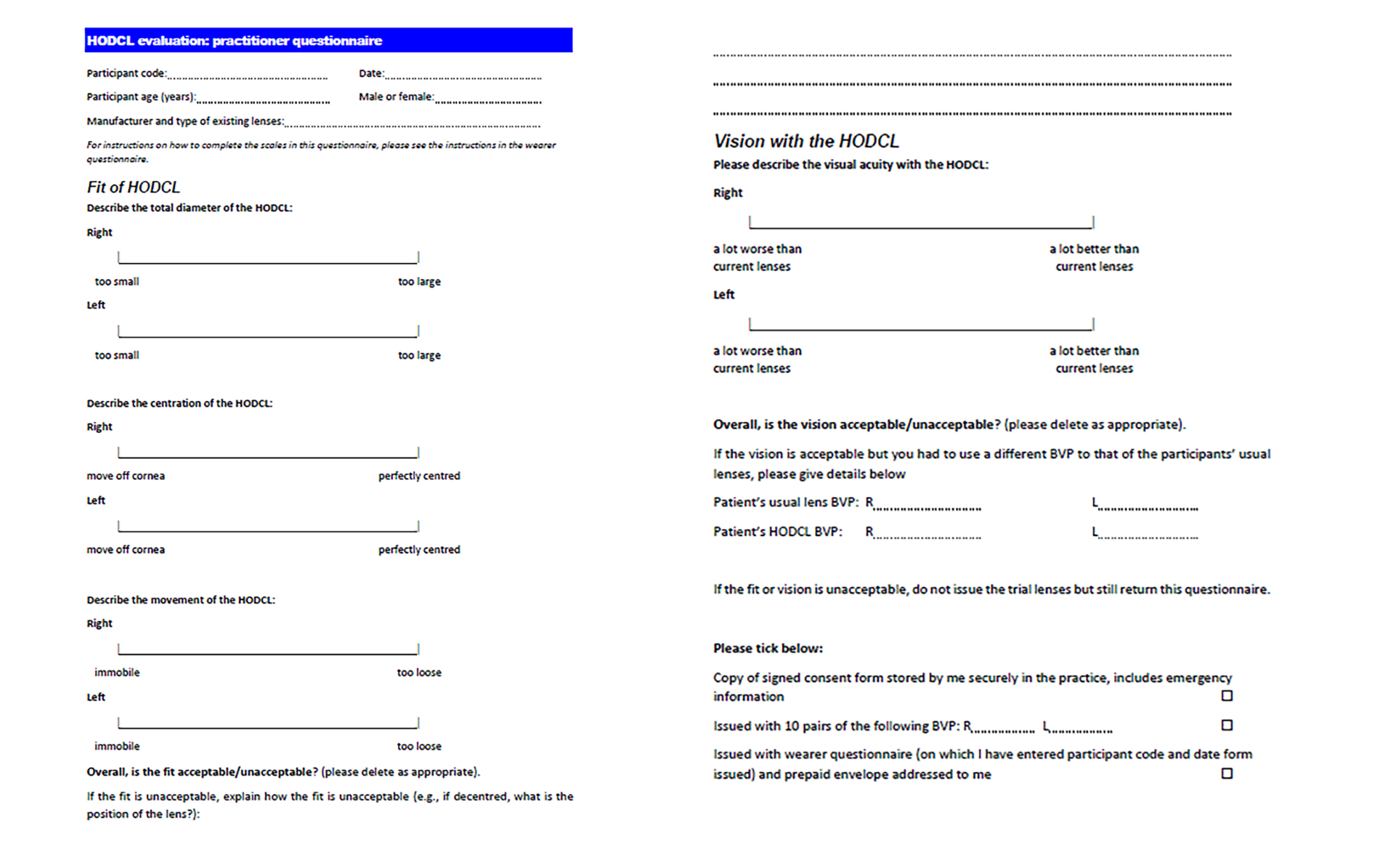
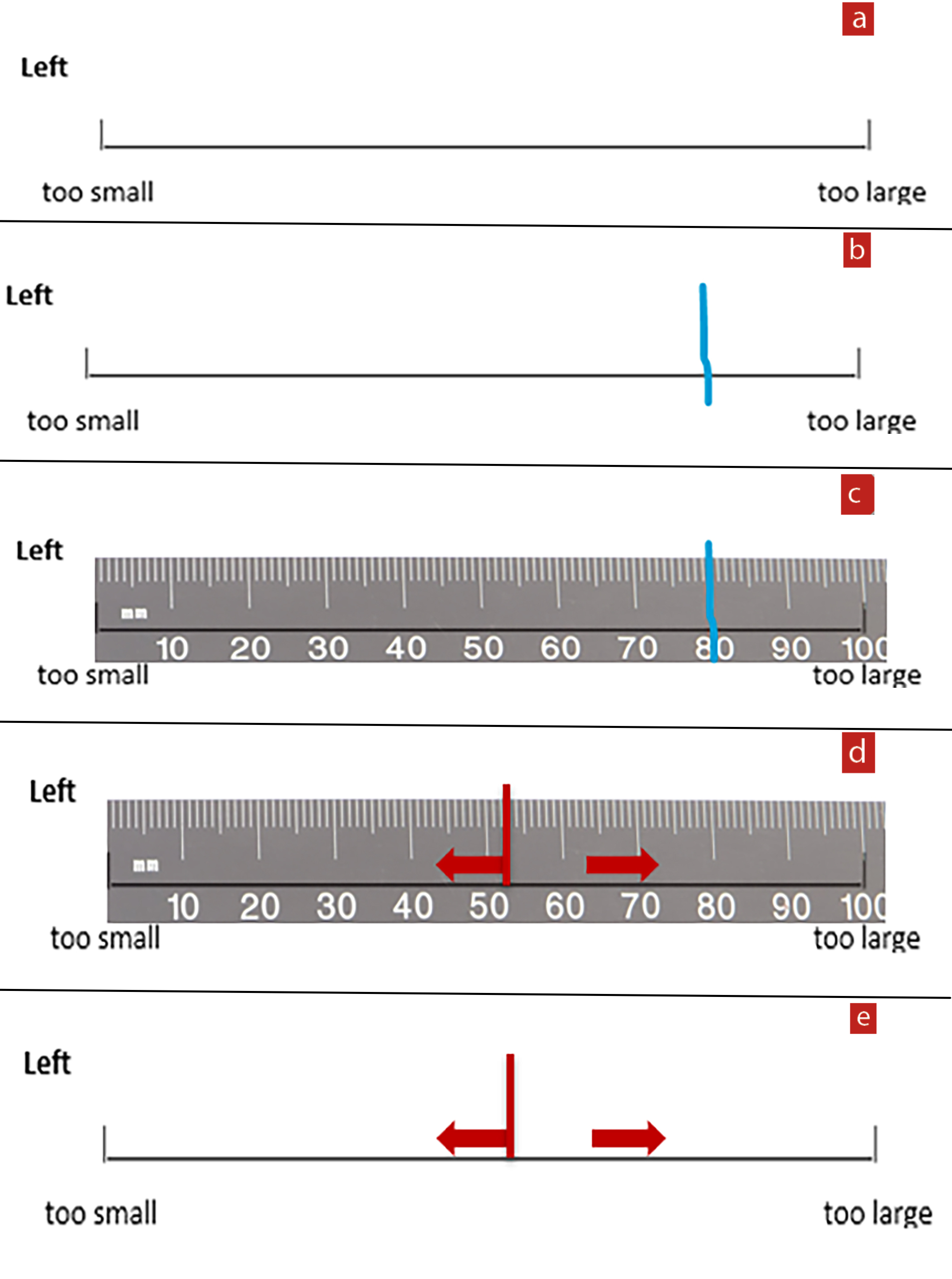
The investigator completed a brief practitioner questionnaire (figure 1) detailing habitual contact lenses, fit, vision, and back vertex power (BVP) of sorafilcon lenses. This questionnaire uses VAS (see below), and for vision compares performance with the habitually worn lenses. The questionnaire was designed to remove the need for standardizing methods of describing fit and vision and to be relevant to the everyday situation in clinical practice when a brand change is being considered.
Figure 1: Practitioner questionnaire. Sorafilcon A contact lenses are referred to in the study literature as HODCL (Hoya one-day contact lenses)
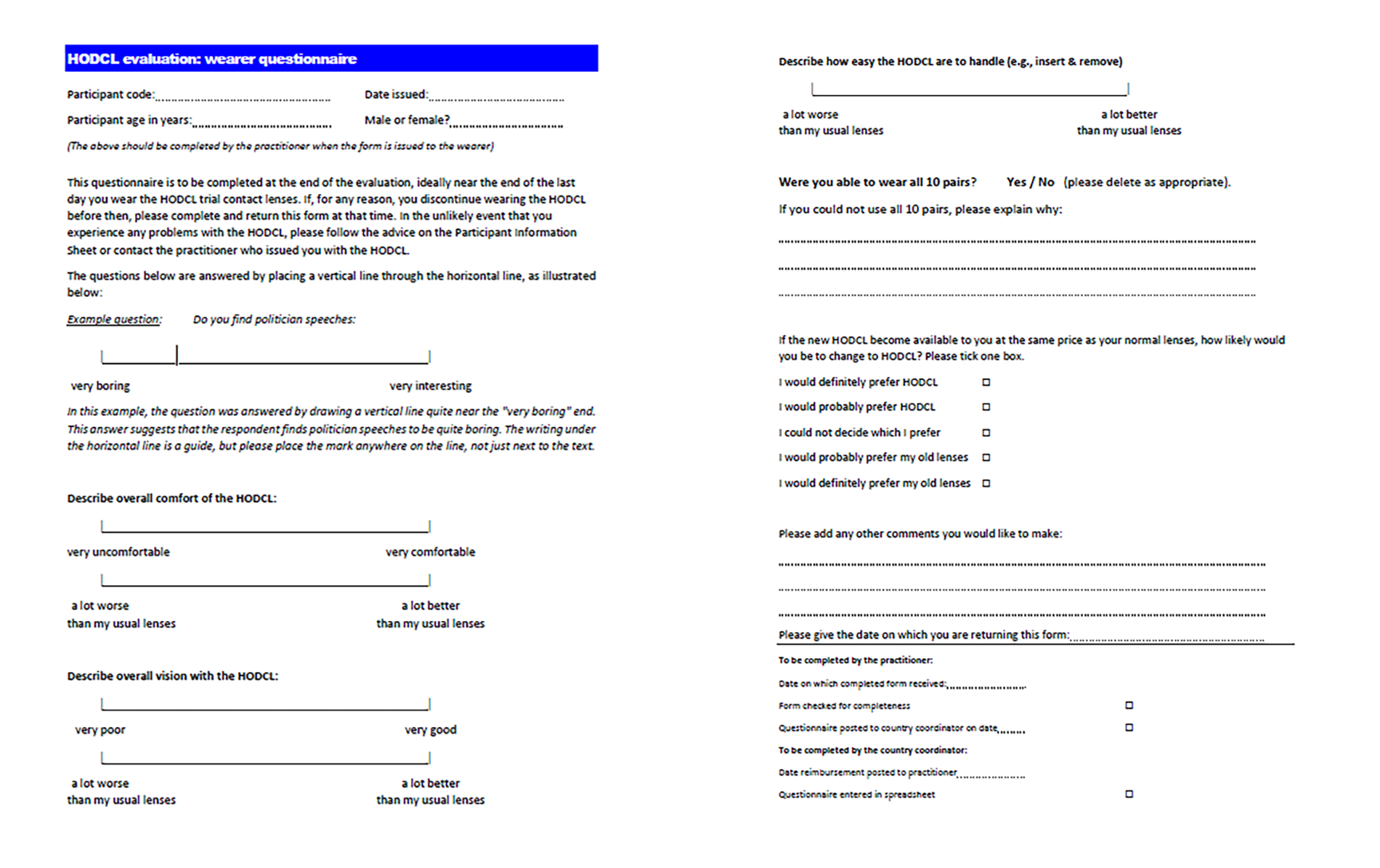
The investigator issued a wearer questionnaire (figure 2) for completion after 10 days, detailing patients’ perspective of lens performance (comfort, vision, handling) in absolute terms and compared with their existing lenses. A final question asks whether, if sorafilcon becomes available at the same price as the habitually worn lenses, participants would definitely prefer sorafilcon, probably prefer sorafilcon, could not decide, probably prefer habitual lenses, or definitely prefer habitual lenses. Additional comments are entered in a free text entry area.
An additional form was used to record any adverse events.
Figure 2: Wearer questionnaire. Sorafilcon A contact lenses are referred to in the study literature as HODCL (Hoya one-day contact lenses)
Statistical analysis
For all monocular variables, right and left eye data were highly correlated (Pearson r>0.75). Therefore, it was inappropriate to pool data,14-18 so left eye data were analysed. The primary goal of the evaluation was to provide descriptive statistics. Some inferential and comparative statistics are obtained, and the limitations of these are considered in the discussion section.
Results
General descriptive data
The experimental phase took place during the Covid-19 pandemic and the number of participants was restricted, particularly in countries with the most severe Covid lockdowns, to 51 from Hungary, 42 from Finland, 37 from Netherlands, and eight from UK; a total of 138. Participants were aged between 18 and 69 years (mean 34 years) and 61% were female.
One potential participant was excluded because they met one of the exclusion criteria; unacceptable lens fit. One non-serious adverse event occurred, for a patient who completed the evaluation but was found to have inferior corneal dense punctate staining. The patient had a history of similar episodes, attributed to dry eye, with habitual lenses (delefilcon A) and resumed wear of these with increased use of artificial tears.
Practitioner questionnaire
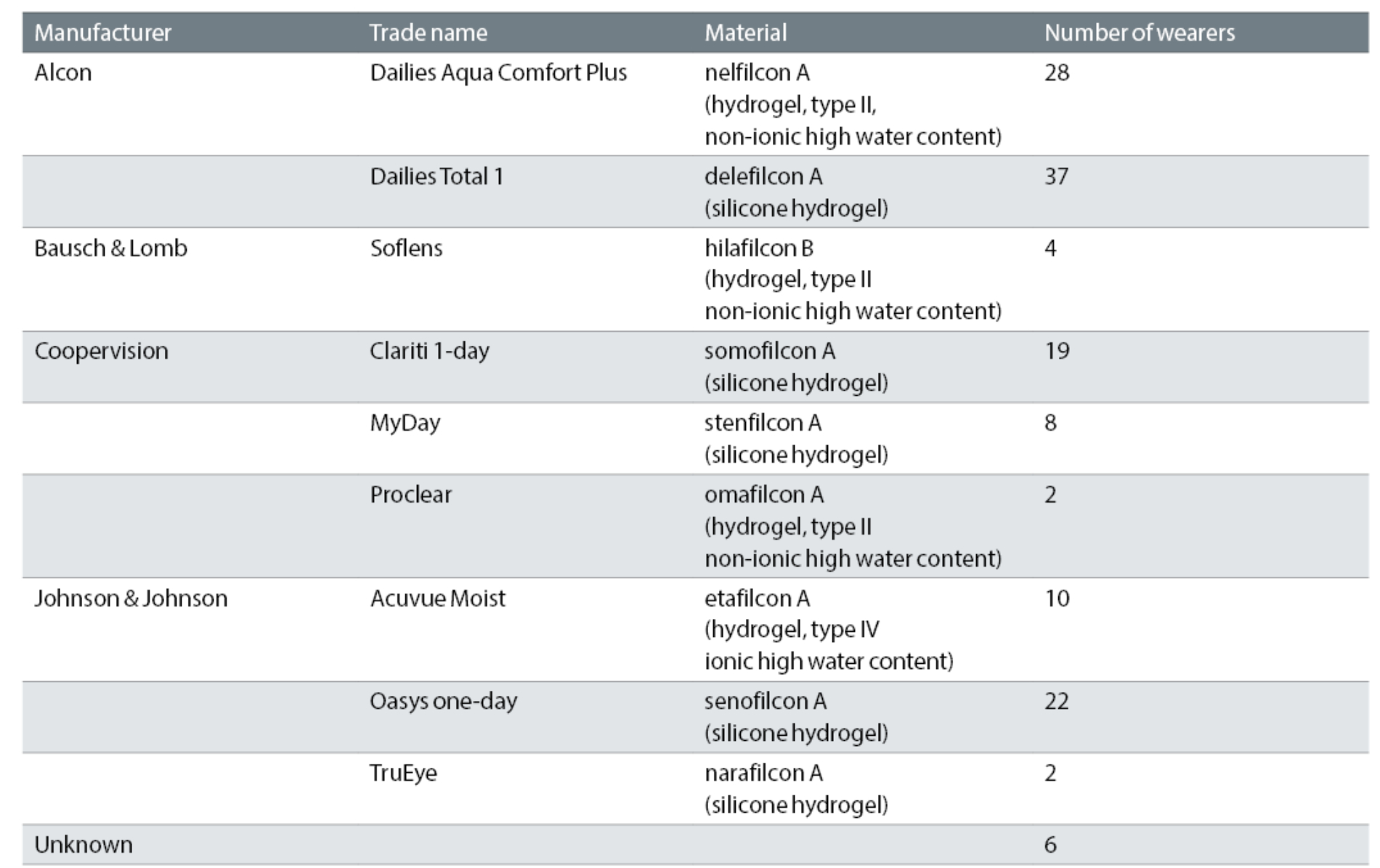
Habitually worn contact lenses are summarised in table 2.
VAS gradings were recorded on a 100mm line, with the position of the line bisection measured to provide scores from 0-100. The practitioner questionnaire (figure 1) asked for the fit to be graded on three pairs of VASs. The first pair were right and left eye gradings of the lens total diameter. The left end of the scale (0) contained the anchor comment, ‘too small’ and the right end (100), ‘too large’. The mean result (left eye data; see above) was close to the midpoint (52.5mm). The spread of the data was narrow (standard deviation 9.9mm), giving the range from 5th to 95th percentile 42.6-73.3mm. These data are illustrated in figure 3, which explains the method of presentation of the results used for other VAS data.
Figure 3: Example of VAS data from practitioner questionnaire. The blank VAS in (a) shows the task given to practitioners for grading lens diameter by placing a vertical line through the horizontal line. An example individual response is shown (b), where the respondent indicates (from the position of the blue line) that the lens diameter is larger than ideal. For each response, a ruler is applied as shown in (c) to convert the VAS result into a score, in this example 80. Data analysis involves calculating, from the results for all participants, the mean and range from the 5th to the 95th percentile. This is shown in (d) and (e)
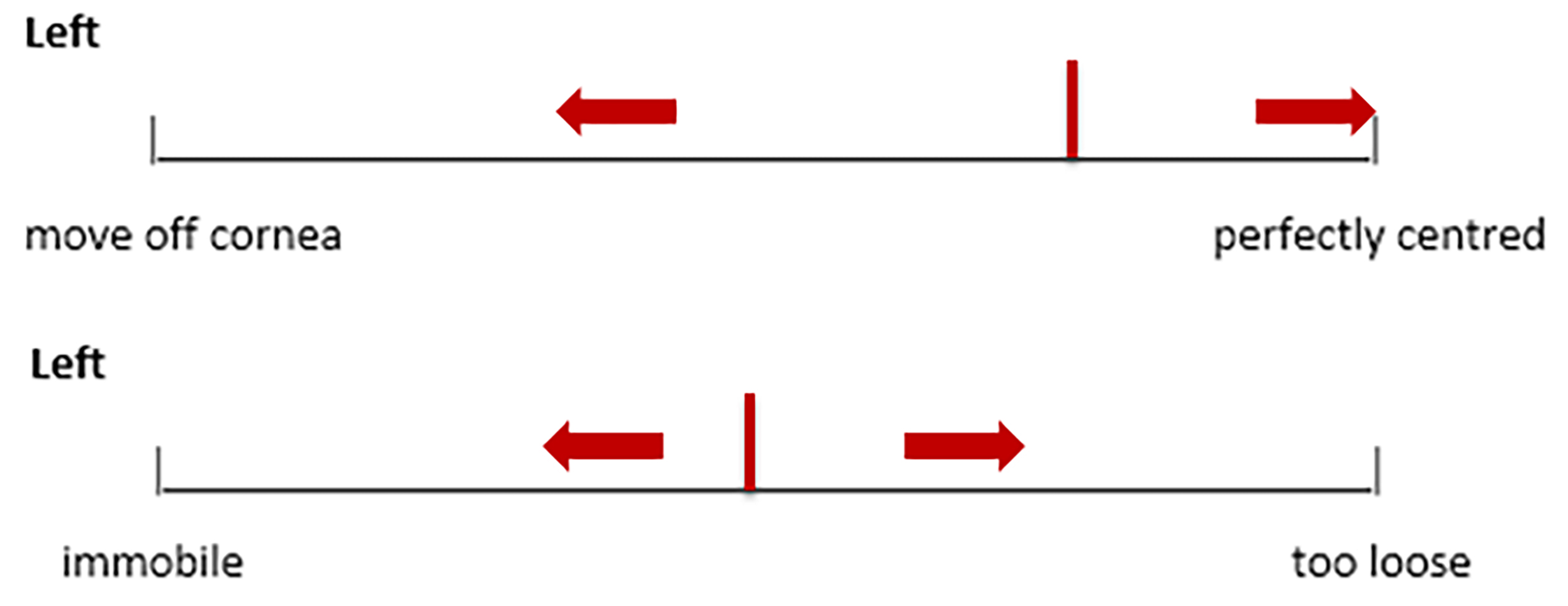
Summary statistics of mean and 5th to 95th percentile range are shown for the practitioner gradings of centration and movement of sorafilcon in figure 4. When practitioners were asked to state whether the fit of sorafilcon was acceptable or unacceptable, 96.4% said ‘acceptable’, 3.6% ‘unacceptable’. When the fit was judged unacceptable, practitioner explanations given were ‘left lens too temporal’, ‘decentred downwards’, ‘slipped down’ and ‘dry’.
Figure 4: Practitioner VAS results for centration and movement of sorafilcon. See figure 3 for explanation; the red line indicates the mean response and the arrows show the range from 5th to 95th percentile
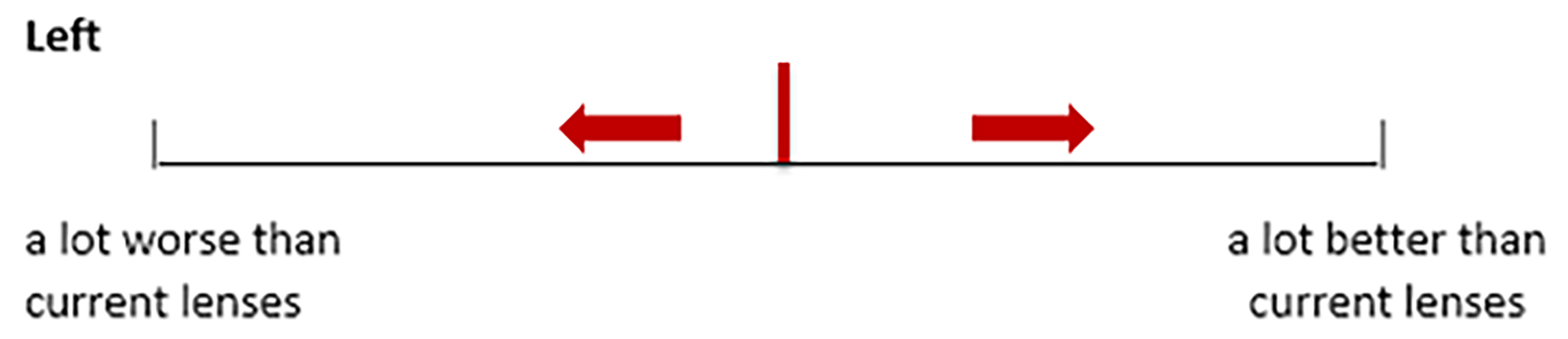
The VAS scales for grading vision asked practitioners, for each eye, to compare visual acuity with sorafilcon lenses to that with the habitual lenses. The results are summarised in figure 5. When asked whether they considered the vision acceptable or unacceptable, 98.5% considered it acceptable, 1.5% unacceptable.
Figure 5: Practitioner VAS results for visual acuity with sorafilcon. See figure 3 for explanation; the red line indicates the mean response and the arrows show the range from 5th to 95th percentile
There were only five participants (3.6%) who required a different BVP for sorafilcon, in every case requiring a less strong BVP than the habitual lenses, in most cases by 0.25DS.
Wearer questionnaire
Participants graded comfort and vision in two ways. First, in absolute terms (eg with a VAS that was anchored on the left (0) with ‘very uncomfortable’ and on the right (100) with ‘very comfortable’) and second relative to their habitual lenses. These results, and those for ease of lens handling, are summarised in figure 6.
Figure 6: Wearer VAS results for comfort, vision, and handling with sorafilcon. See figure 3 for explanation; the red line indicates the mean response and the arrows show the range from 5th to 95th percentile
For the gradings relative to habitually worn lenses, assuming the midpoint of the line represents equivalence between habitual and sorafilcon A lenses, the proportion of participants with a grading >50mm provides an indication of the proportion reporting superiority with sorafilcon (see discussion). This proportion is 60.9% for comfort, 73.9% for vision, and 72.5% for handling, all of which are statistically significant departures from the null hypothesis (2-tailed binomial test, p=0.013, p<0.001, p<0.001 respectively). These statistics rely on assumptions that the midpoint represents equivalence and that respondents are not biased to favour new lenses. These assumptions are addressed in the discussion section.
Eighty-eight percent of participants said they were able to wear all 10 pairs of sorafilcon trial lenses. Participants who could not wear all 10 pairs sometimes gave reasons that were logistical (eg lenses used too infrequently), but those relating to lens performance fell into two categories: dryness (four cases; 2.9%) and comfort (five cases; 3.6%).
Participants were asked, if sorafilcon lenses become available at the same price as their habitual lenses, how likely they would be to change to sorafilcon. The responses are given in table 3. These data can be summarised as 48.6% preferring sorafilcon, 26.8% preferring their habitual lenses, and 24.6% unable to choose. Looking at these data conservatively, approximately half of participants either did not express a preference or preferred their habitual lenses, with approximately half electing to change to sorafilcon. Just considering the 104 participants who expressed a preference, 64% preferred sorafilcon, which is statistically significantly higher than expected by chance (binomial test, 2-tailed, p=0.0042; see Discussion).
Table 3: Responses to question, how likely to change to sorafilcon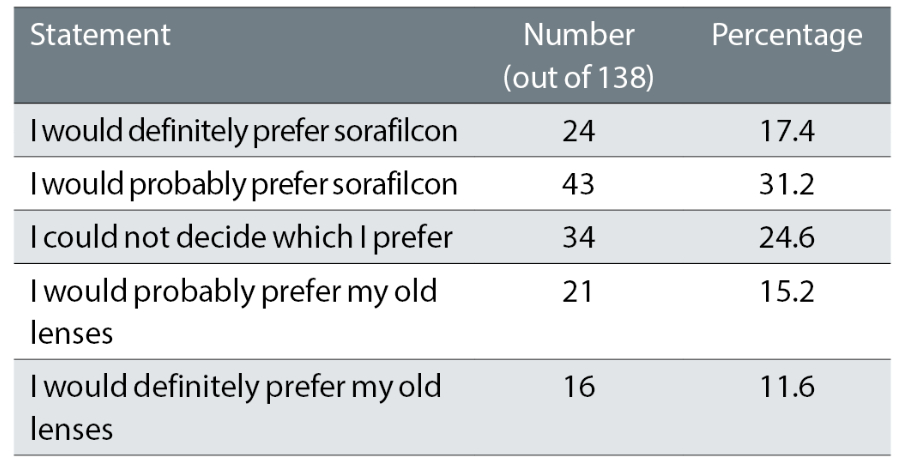
Participants were invited to add any other comments. Fewer than one third of participants made any comments. An attempt was made to classify the comments, but the number in each category was too low for meaningful analysis. For example, for comments relating to lens handling, four participants commented that they preferred sorafilcon to their previous lenses (each wore different habitual lenses), and three participants commented that they preferred the handling of their habitual lenses (each had different types of habitual lenses).
Habitual lens material-related analysis
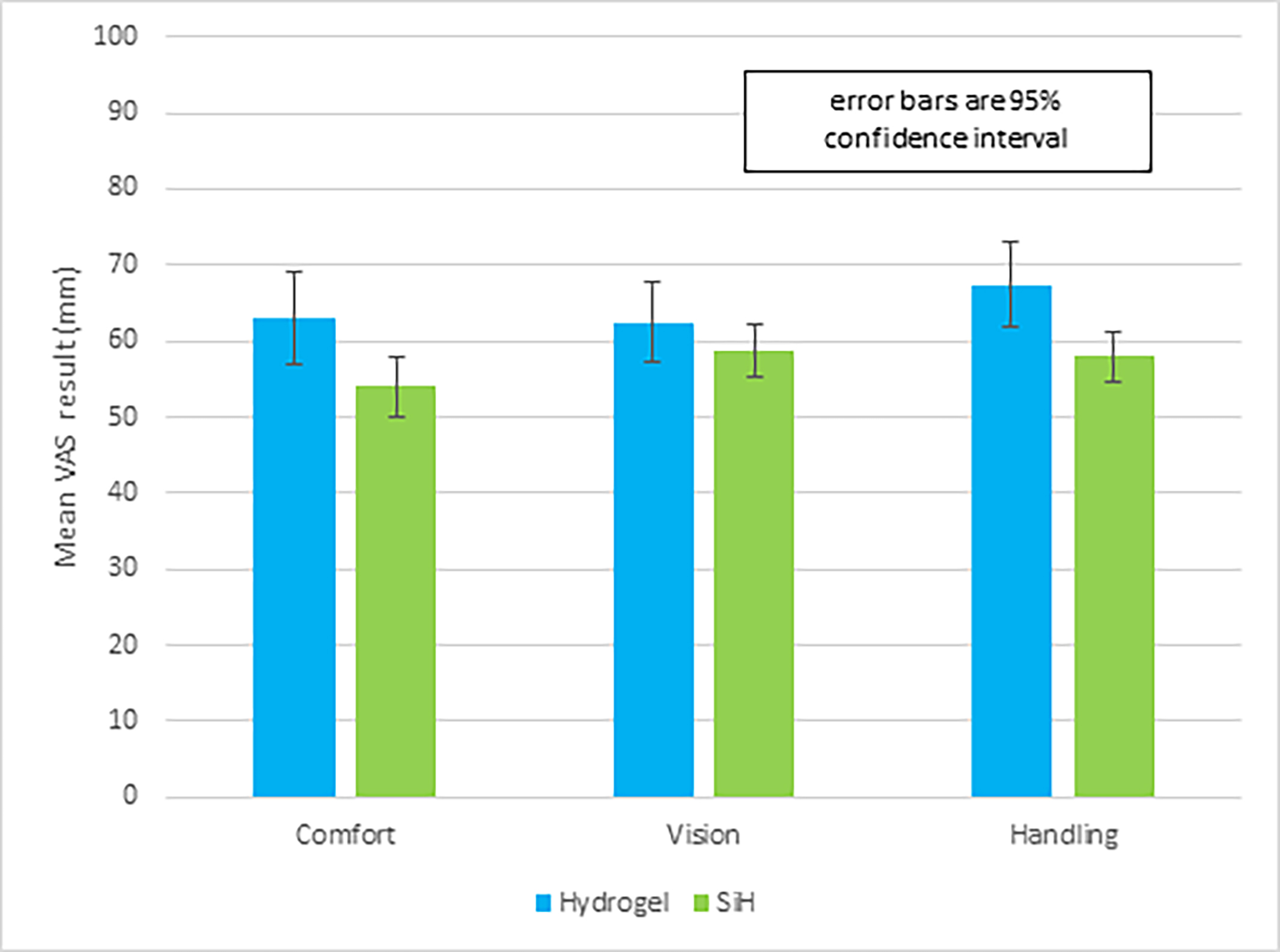
The key analyses above were repeated but comparing the 44 participants habitually wearing hydrogel lenses with the 88 habitually wearing silicone hydrogel (six participants were excluded because the type of lens they were habitually wearing was unknown). These analyses concentrated on the questionnaire items that compared performance with habitual lenses.
There were no significant differences between the hydrogel and silicone hydrogel lens wearers in age or ratio of sexes. Practitioners were slightly (t-test, p=0.05) more likely to grade the vision as better with sorafilcon than with old lenses for those whose habitual lenses were hydrogel (mean line bisection 56mm) than for those wearing silicone hydrogel lenses (mean line bisection 52mm).
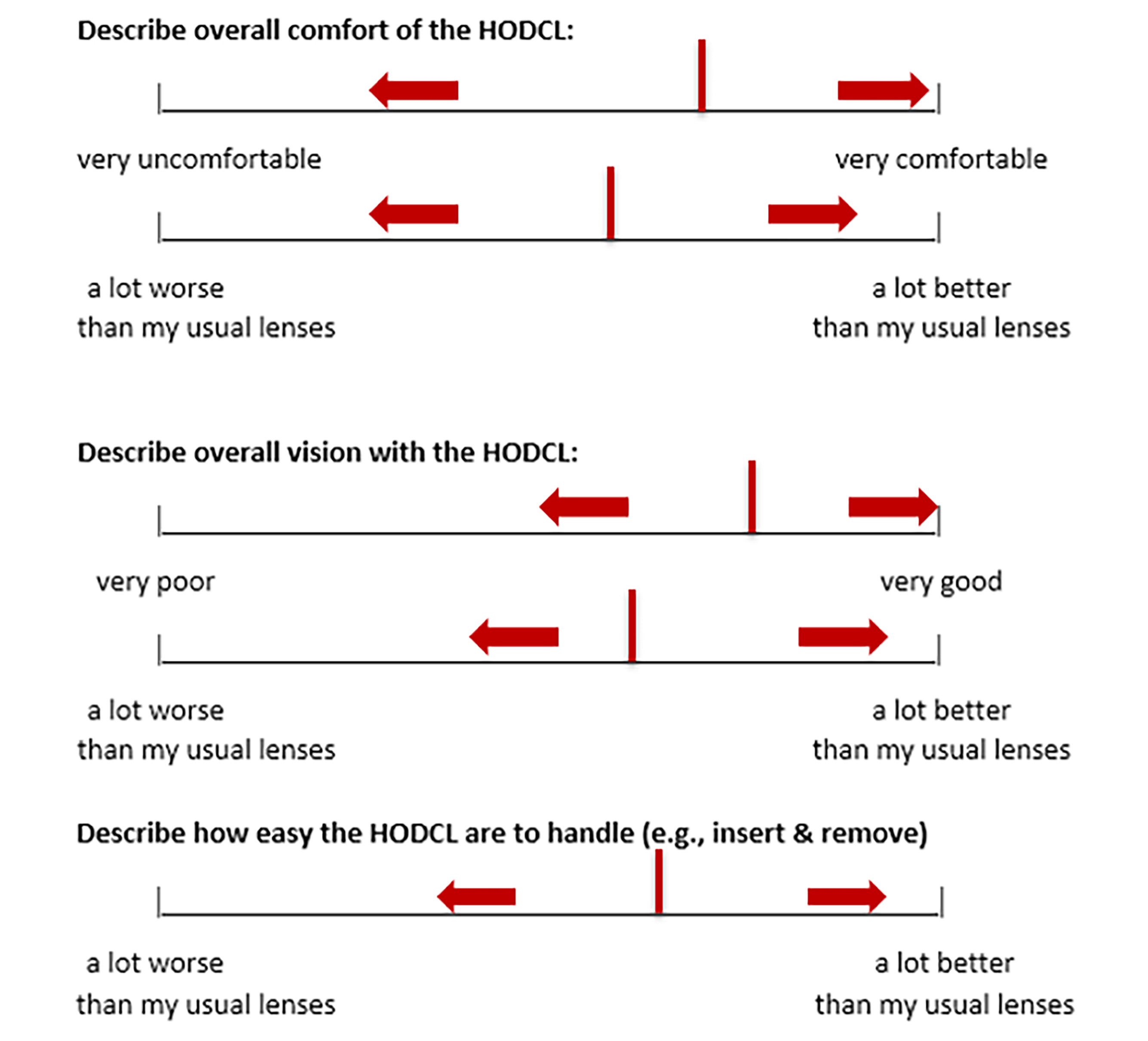
Considering the wearer questionnaires (figure 7), compared with those whose habitual lenses were silicone hydrogel, participants habitually wearing hydrogel lenses tended to report greater improvements in comfort (t-test, p=0.01) and handling (t-test, p=0.003). Wearers’ ratings of the difference in vision when changing to sorafilcon did not differ significantly between those who habitually wore hydrogel versus silicone hydrogel lenses (t-test, p=0.24).
Figure 7: VAS mean results for wearers’ comparison of sorafilcon with previous lenses, for the subgroups whose habitual lenses were hydrogel (N=44) or silicone hydrogel (N=88)
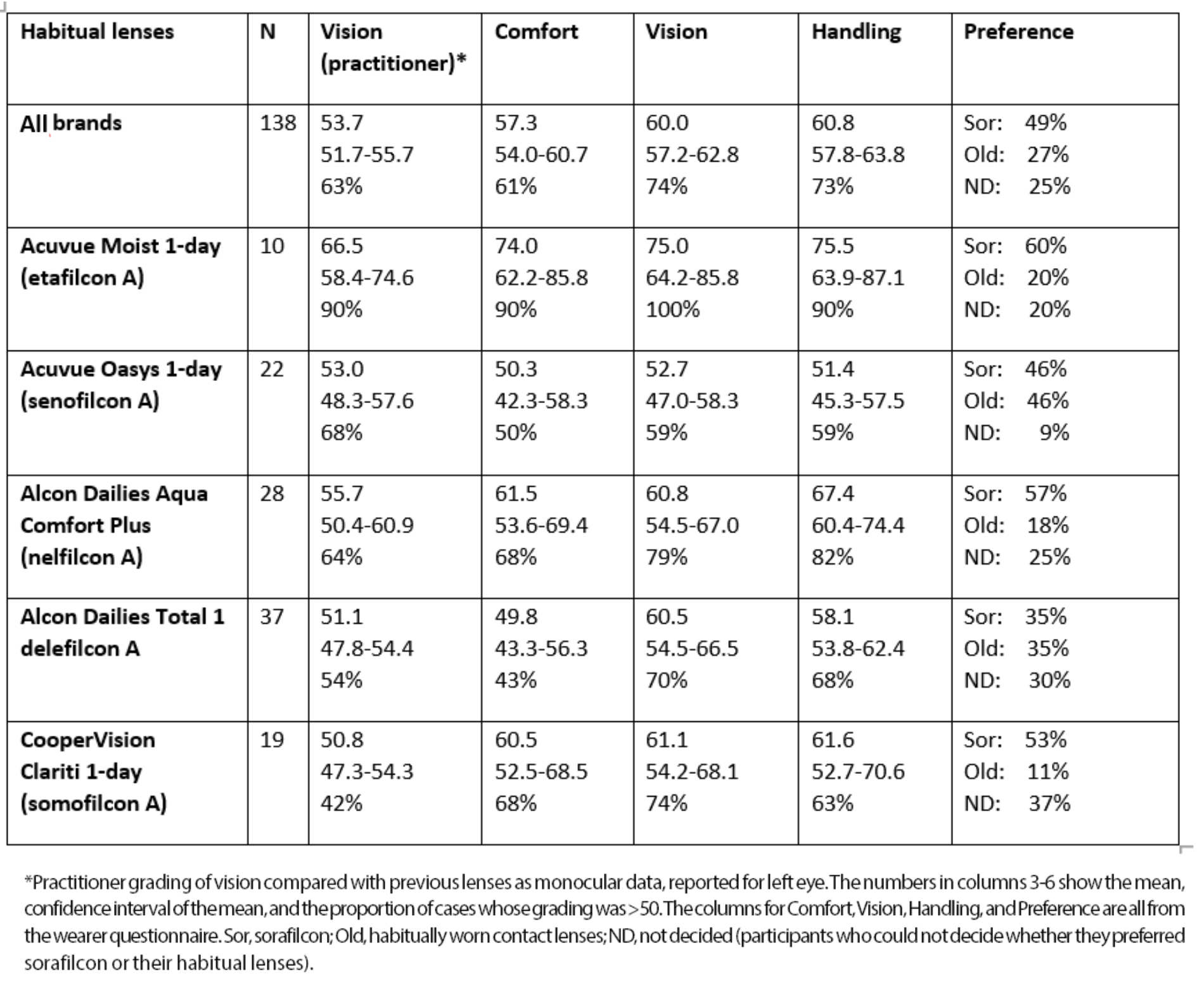
Habitual lens type-related analyses
The key analyses above were repeated but considering only participants who wore a particular brand of lens, for lens types with at least 10 wearers. These analyses concentrated on the questionnaire items that compared performance with sorafilcon with habitual lenses (table 4). For the participants who expressed an overall preference for either sorafilcon or their habitually worn lenses, the proportion preferring sorafilcon was significantly higher than chance (binomial test, 2-tailed) in the sub-groups wearing nelfilcon A (p=0.026) and somofilcon A (p=0.038), but not in sub-groups wearing other lens types. The low numbers wearing some lens types mean these analyses should be viewed with caution.
Table 4: Comparing sorafilcon lenses with main brands of habitual lenses
Discussion
Overview of results
VAS are widely used in healthcare sciences19 and one advantage, compared with Likert-type scales, is that respondents are not forced to categorise their responses, resulting in continuous variables rather than interval-level data.20 Papas and Schultz compared VAS with numerical rating scales (NRS) and found both approaches have strengths and weaknesses.21 A disadvantage of NRS is that participants have a tendency to round their responses.21 VAS have been widely used in vision science22-25 and contact lens research,26-28 to grade vision22 and ocular comfort.27, 28 The 100mm scale meant that a mean score of 50mm can be conceptualised as an equivalence of the statements anchoring each end of the scale.
In the practitioner questionnaire, an assessment of the fit of sorafilcon lenses is simplified to three parameters: total diameter, centration and movement. The VAS data for these parameters indicates that sorafilcon lenses were found to fit well (figures 3 and 4), confirmed by the overall judgement of the fit as acceptable in 96.4% of cases.
With several practitioners in four countries using different methods of testing and scoring visual acuity, a pragmatic approach was taken to the assessment of visual acuity. In practice, when clinicians contemplate changing a patient to a different brand of lens, the key question is how the new lenses compare with habitually worn lenses. Therefore, practitioners were asked to grade visual performance with sorafilcon lenses compared with habitually worn lenses. Practitioners judged the vision with sorafilcon lenses, on average, to be slightly better (mean line bisection 53.7mm) than the habitual lenses, with a narrow spread of data. The vision was considered acceptable in 98.5% of cases.
When changing to sorafilcon, a change of lens power was required in 4% of cases. This supports the clinical practice of clinicians checking the performance of a new lens type when it is proposed to change.29
The wearer questionnaire asked participants to grade comfort and vision in absolute terms and relative to their habitually worn lenses. For comfort, the mean absolute grading (69.7mm) was considerably to the right of (better than) the midpoint. This is supported by the grading relative to habitually worn lenses, with just over 60% of gradings exceeding 50mm, which may indicate that sorafilcon lenses were more comfortable than habitual lenses. The wearer perceptions of vision were more positive, with the absolute comparison mean 75.8mm and almost three-quarters of participants indicated vision exceeding that with their usual lenses. Most participants also graded lens handling with sorafilcon to be better than habitual lenses: line bisection (mean 60.8mm) was to the right of the midpoint of the line in 72.5% of cases.
A key question is whether participants would change to sorafilcon, if available at the same price as their habitual lenses (table 4). Nearly half prefer to change, although approximately one quarter prefer their habitual lenses and one quarter could not decide. This indicates, many patients prefer one lens brand, but the identity of that brand varies idiosyncratically. The most successful practitioners are likely to be those who access a wide range of brands and offer symptomatic patients, trials with alternative brands.
The use of binomial tests to assess the proportion of VAS gradings >50mm assumes that the midpoint represents equivalence and that respondents are not biased to favour new or old lenses. Although it seems intuitively reasonable that the centre point represents equivalence, it must be stressed that this is an assumption. In this regard, the inclusion of a central anchor on the line may have been helpful.30 Research investigating line bisection indicates that, in normal observers, there is a small (<1%) bias towards the left side of the midline, which would underestimate preference for sorafilcon.31 The question of whether participants were biased to favour new lenses would be influenced by a recency bias (favouring the most recently presented option) or primacy bias (favouring the first presented option). There is some evidence from research on taste tests that primacy bias predominates,32 at least in adults.33 Since the study is not an RCT, placebo effects may also be relevant.
The use of a binomial test to investigate participant preference also involves assumptions. First, it must be stressed that this comparison only considers those who expressed a preference, ignoring the 25% of participants who could not decide which they preferred. As noted above, if primacy bias outweighed recency bias this would decrease the likelihood of participants favouring sorafilcon, but if there is a placebo effect associated with trying a ‘new lens type’ this would create a bias in favour of sorafilcon. An RCT is required to control for these potential biases, although as noted above such a trial less closely resembles everyday clinical practice than the present design. Each type of study provides complimentary information and evidence from both approaches may help to fully inform clinicians.
The further analyses of habitual lens material and type are exploratory and preliminary. However, it is notable that for two modern silicone hydrogel materials (senofilcon A and delefilcon A), those who expressed a preference were evenly split between habitual lens type and sorafilcon. In contrast, those wearing other lens types were more likely to express a preference for sorafilcon than their habitual lenses.
Comparison with the literature
Papas and colleagues found that discomfort during contact lens wear is associated with the length of time lenses are on-eye, but not with the time of day when lenses are placed on-eye.28 The approach these researchers used, of sampling comfort at intervals throughout the day, is more thorough than that used here, but would not have been practical with the 138 participants in the present research.
Woods et al concluded that in studies of contact lens comfort, the sensitivity of comfort ratings is increased by concentrating on symptomatic wearers.27 The present research may have benefitted if it had concentrated on symptomatic patients, although it would have been more challenging to find 138 symptomatic wearers in contemporary contact lens practice. The design adopted in the present research is relevant for the situation when a different lens brand is being considered for patients who have minimal symptoms with their present lenses.
Inevitably, reports of research findings tend to emphasise the mean or typical result. However, the finding that for every VAS variable assessed, the range from 5th to 95th percentile response extends on both sides of the midpoint indicates that there are always exceptions to the trend identified by the mean result. Clinically, this is a reminder that every patient should be considered as an individual who may manifest a response that is contrary to the practitioner’s usual experience.
Strengths and limitations
Strengths of this study include the large sample size and multi-centre international design.
The use of an open-label, single-arm design,12 introduces both strengths and limitations. Double-masked RCTs are often described as the gold standard research for interventions,10, 34 but RCTs have their limitations.11, 35, 36 Indeed, Hill, the architect of the RCT, asserted ‘any belief that the controlled trial is the only way would mean not that the pendulum had swung too far but that it had come right off the hook’. For clinicians, an important limitation of RCTs is that the strictly controlled conditions depart from everyday clinical practice, and therefore the results may not apply to the clinical setting.37 From this perspective, the present study design may be more relevant to clinicians than an RCT. A clinician can predict that if a patient wearing a daily disposable contact lens is offered a trial with sorafilcon, there is a reasonable chance they will prefer sorafilcon.
A potential limitation of an unmasked evaluation is that participant expectation could influence results, for example via a placebo effect. Keir and colleagues note that masking is not feasible for most contact lens trials.38 They demonstrated that masking does not have a measurable impact on 0-100 ratings with daily disposable lenses, but can impact lens preference.38 The bias thus introduced was found to be in favour of the habitual manufacturer,38 although the authors cautioned their study did not provide strong evidence of such an effect.
A strength is that the present research included independent assessments of lens fit (practitioner) and of comfort (wearer). Wolffsohn and colleagues found that lens fit is not correlated with comfort.13
The wearing period of 10 days was selected as a balance, long enough for a reasonable trial and brief enough to allow recollection of experience with habitual lenses. Some studies have used longer periods (eg two weeks),12 others shorter (eg three days).7
Participants were given 10 pairs of free trial lenses to use and asked to complete and return the wearer questionnaire after 10 days’ wear. This reduces the risk of participants wearing a pair of lenses for more than one-day, which is known to be a non-compliance issue associated with reduced comfort.39 This could be a source of bias, increasing absolute estimates of comfort and inflating estimates of the sorafilcon lenses compared with habitual lenses.
Finally, a limitation of this study and indeed much contact lens research is that participants are recruited from clinics. This means that patients who use the internet40 and non-compliant wearers, who are more likely to have complications,3 may be under-represented.
Conclusions
In adults wearing a broad range of daily disposable contact lenses, a trial with sorafilcon lenses often leads to reports of improved vision, comfort and easier lens handling. The broad range of responses obtained for all variables measured highlights that each patient is an individual and may benefit from a trial with an alternative lens type.
The study was funded by Hoya Holdings and was undertaken by the HODCL team comprising:
- Bruce JW Evans BSc PhD FCOptom FAAO FEAOO FBCLA DipCLP DipOrth, Institute of Optometry, London, UK
- Timo Koljonen, BOptom, Lahden Silmäasema Oy, Finland
- Roy Houten, BOptom, Gijsen Optiek BV, The Netherlands
- Györgyi Munkácsi, MD, Szemlátomás Optika, Hungary
- Lilly Balla, Optometrist, Szemeszter Optika, Hungary
- Laszlo Reider, Optometrist, Reider Optika, Hungary
- Fabrizio Bonci MCOptom, Dr Acs Optika, Hungary
- Endre Viczay, Optometrist, Vicai Optika, Hungary
- Marc Ramaekers, Contact Lens Specialist, Gijsen Optiek BV, The Netherlands
- Monique Hanssen-Kelleter, Contact Lens Specialist, Gijsen Optiek BV, The Netherlands
- Claire O’Leary , BSc PhD MCOptom, Cole Martin Tregaskis Optometrists, UK
- Gábor Dózsa, TheFrogCompany, Hungary.
- Natalia Vlasak, MD, Hoya Vision Care, The Netherlands
References
- Efron N, Brennan NA, Chalmers RL, et al. Thirty years of ‘quiet eye’ with etafilcon A contact lenses. Contact Lens & Anterior Eye, 2020;43:285-297.
- Cho P, Boost MV. Daily disposable lenses: the better alternative. Contact Lens & Anterior Eye, 2013;36:4-12.
- Chalmers RL, Hickson-Curran SB, Keay L, Gleason WJ, Albright R. Rates of adverse events with hydrogel and silicone hydrogel daily disposable lenses in a large postmarket surveillance registry: the TEMPO Registry. Investigative Ophthalmology & Vision Science, 2015;56:654-663.
- Efron N, Morgan PB, Woods CA. International Contact Lens Prescribing Survey C. An international survey of daily disposable contact lens prescribing. Clinical and Experimental Optometry, 2013;96:58-64.
- Efron N, Brennan NA, Chalmers RL, et al. Authors’ Reply: ‘Thirty years of ‘quiet eye’ with etafilcon A contact lenses: Additional considerations’. Contact Lens & Anterior Eye, 2020, 43: 285-297
- Carnt N, Stapleton F. Thirty years of ‘quiet eye’ with etafilcon A contact lenses: Additional considerations. Contact Lens & Anterior Eye, 2020, 43: 285-297
- Varikooty J, Schulze MM, Dumbleton K, et al. Clinical performance of three silicone hydrogel daily disposable lenses. Optometry & Vision Science, 2015;92:301-311.
- Wu YT, Ho A, Naduvilath T, et al. The risk of vision loss in contact lens wear and following LASIK. Ophthalmic & Physiological Optics, 2020;40:241-248.
- Dart JK, Radford CF, Minassian D, Verma S, Stapleton F. Risk factors for microbial keratitis with contemporary contact lenses: a case-control study. Ophthalmology, 2008;115:1647-1654, 1654.
- Schulz KF, Altman DG, Moher D, Group C. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332.
- Patsopoulos NA. A pragmatic view on pragmatic trials. Dialogues in Clinical Neuroscience, 2011;13:217-224.
- Marx S, Lauenborg B, Kern JR. Performance evaluation of delefilcon a water gradient daily disposable contact lenses in first-time contact lens wearers. Contact Lens & Anterior Eye, 2018;41:335-341.
- Wolffsohn J, Hall L, Mroczkowska S, et al. The influence of end of day silicone hydrogel daily disposable contact lens fit on ocular comfort, physiology and lens wettability. Contact Lens & Anterior Eye, 2015;38:339-344.
- Armstrong RA. Statistical guidelines for the analysis of data obtained from one or both eyes. Ophthalmic & Physiological Optics, 2013;33:7-14.
- Cheng CY, Liu JH, Chiang SC, Chen SJ, Hsu WM. Statistics in ophthalmic research: two eyes, one eye or the mean? Zhonghua Yi. Xue. Za Zhi. (Taipei). 2000;63:885-892.
- Murdoch IE, Morris SS, Cousens SN. People and eyes: statistical approaches in ophthalmology. British Journal of Ophthalmology, 1998;82:971-973.
- Ray WA, O’Day DM. Statistical analysis of multi-eye data in ophthalmic research. Investigative Optometry & Vision Science, 1985;26:1186-1188.
- Lee CF, Cheng AC, Fong DY. Eyes or Subjects: Are Ophthalmic Randomized Controlled Trials Properly Designed and Analyzed? Ophthalmology. 2012.
- McCormack HM, Horne DJ, Sheather S. Clinical applications of visual analogue scales: a critical review. Psychology and Medicine, 1988;18:1007-1019.
- Reips UD, Funke F. Interval-level measurement with visual analogue scales in Internet-based research: VAS Generator. Behavioral Research Methods, 2008;40:699-704.
- Papas EB, Schultz BL. Repeatability and comparison of visual analogue and numerical rating scales in the assessment of visual quality. Ophthalmic & Physiological Optics, 1997;17:492-498.
- Pointer JS. A novel visual analogue scale (VAS) device: an instrument based on the VAS designed to quantify the subjective visual experience. Ophthalmic & Physiological Optics, 2004;24:181-185.
- Aakre BM, Doughty MJ. Are there differences between ‘visual symptoms’ and specific ocular symptoms associated with video display terminal (VDT) use? Contact Lens & Anterior Eye, 2007;30:174-182.
- Wahlberg M, Abdi S, Brautaset R. Treatment of accommodative insufficiency with plus lens reading addition: is +1.00 D better than +2.00 D? Strabismus, 2010;18:67-71.
- Kommerell G, Kromeier M, Scharff F, Bach M. Asthenopia, Associated Phoria, and Self-Selected Prism. Strabismus, 2015;23:51-65.
- Hiraoka T, Okamoto C, Ishii Y, et al. Patient satisfaction and clinical outcomes after overnight orthokeratology. Optometry & Vision Science, 2009;86:875-882.
- Woods CA, Bentley SA, Fonn D. Temporal changes in contact lens comfort over a day of wear. Ophthalmic & Physiological Optics, 2016;36:643-648.
- Papas EB, Chiem A, Zhang G, Mobeen R, Lee L. Temporal considerations in contact lens discomfort. Contact Lens & Anterior Eye, 2021;44:14-17.
- Gasson A, Morris J. Other soft lens fitting considerations. The Contact Lens Manual. A Practical Guide to Fitting, Fourth ed. Edinburgh: Elsevier; 2010:203-211.
- Paul-Dauphin A, Guillemin F, Virion JM, Briançon S. Bias and precision in visual analogue scales: a randomized controlled trial. American Journal of Epidemiology, 1999;150:1117-1127.
- Varnava A, McCarthy M, Beaumont JG. Line bisection in normal adults: direction of attentional bias for near and far space. Neuropsychologia, 2002;40:1372-1378.
- Dean ML. Presentation order effects in product taste tests. Journal of Psychology, 1980;105:107-110.
- Sumner E, DeAngelis E, Hyatt M, Goodman N, Kidd C. Cake or broccoli? Recency biases children’s verbal responses. PLoS One, 2019;14:e0217207.
- Rowe E, Evans BJW. Are commonplace optometric activities evidence-based? Optometry in Practice, 2018;18:207-218.
- Kaptchuk TJ. The double-blind, randomized, placebo-controlled trial: gold standard or golden calf? Journal of Clinical Epidemiology, 2001;54:541-549.
- Kaptchuk TJ. Powerful placebo: the dark side of the randomised controlled trial. Lancet, 1998;351:1722-1725.
- Sheikh A, Smeeth L, Ashcroft R. Randomised controlled trials in primary care: scope and application. British Journal of General Practice, 2002;52:746-751.
- Keir N, Luensmann D, Woods CA, Bergenske P, Fahmy M, Fonn D. Effect of Masking on Subjective Responses to Daily Disposable Contact Lenses. Optometry & Vision Science, 2016;93:828-835.
- Dumbleton KA, Richter D, Woods CA, et al. A multi-country assessment of compliance with daily disposable contact lens wear. Contact Lens & Anterior Eye, 2013;36:304-312.
- Stapleton F, Keay L, Edwards K, et al. The incidence of contact lens-related microbial keratitis in Australia. Ophthalmology, 2008;115:1655-1662.
