This BCLA CLEAR report¹ explores the interactions between lens materials, care products and the tear film, looking at the biochemistry and compatibility of the various elements involved in successful contact lens wear.
Oxygen permeability
Contact lens materials have evolved over time from polymethyl methacrylate (PMMA) to 2-hydroxyethyl methacrylate (HEMA), to silicone hydrogel (SiHy) in the search for improved oxygen permeability. Silicone combines with oxygen in siloxane, allowing oxygen to pass through the polymer. The main issue with including silicone or fluorine in contact lens materials is that this causes hydrogel lenses to be more hydrophobic, affecting deposition onto the lens surface. Lysozyme and albumin tend to adsorb to these newer materials less than they do to HEMA, but cholesterol is more likely to form deposits on silicone hydrogel lenses. (figure 1). 2, 3
Relevance of oxygen transmission and contact lenses:
- Having no blood vessels, the cornea relies on oxygen from the air, dissolved into the tear film
- It is vital for corneal health that a contact lens allows oxygen to pass through
Wettability
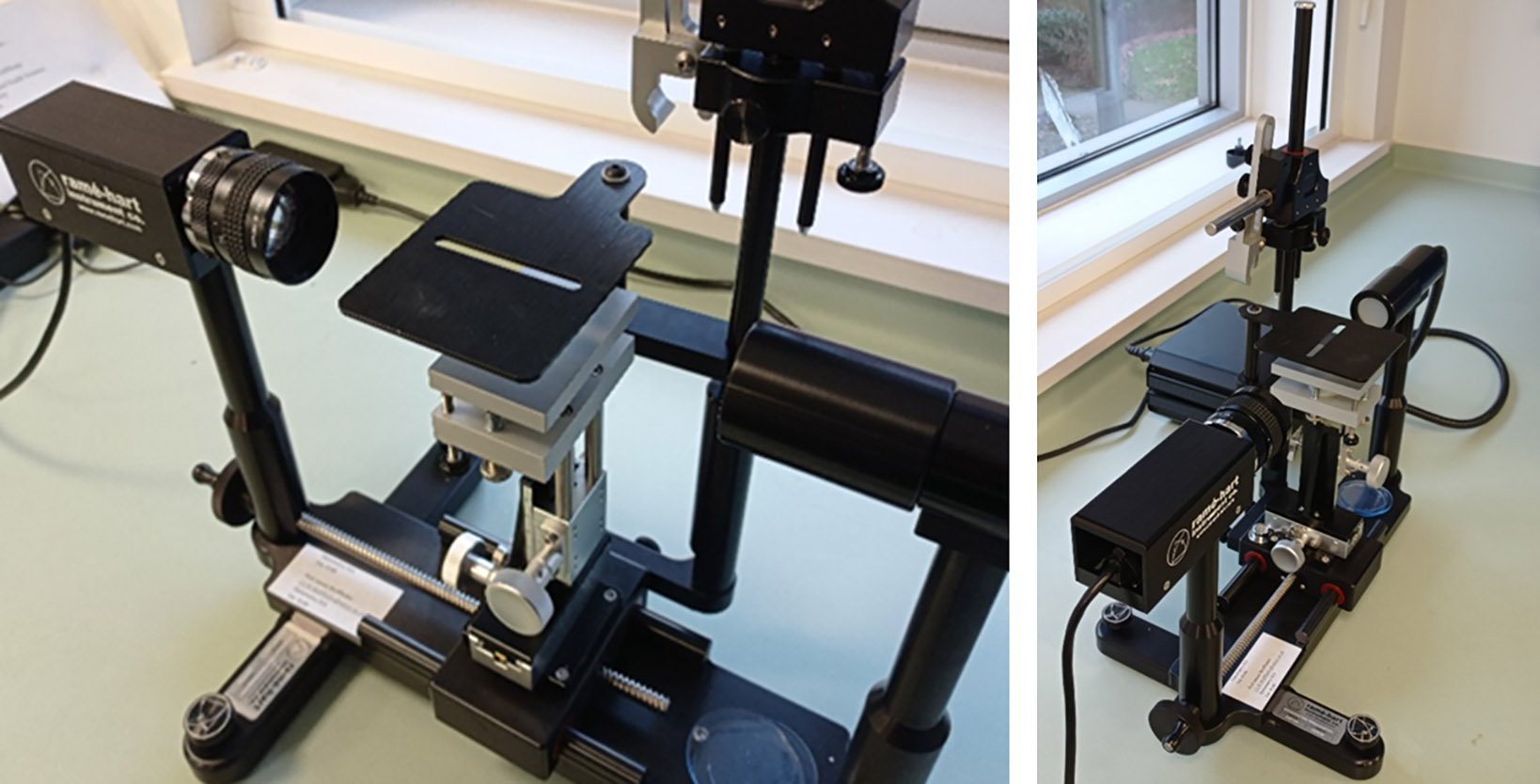
Wettability refers to the potential of a liquid to spread and maintain contact with a surface, thus wettability in this context refers to how much of the lens surface is covered by the tear film. The addition of other substances, either on the lens surface or in the associated liquid, will affect the wettability of the lens. Surfactants (surface active agents) lower the surface tension of a liquid, thereby increasing its ability to spread and penetrate. Factors affecting the wettability of a contact lens material include the chemical properties of the contact lens constituents, how it is manufactured (figure 2), what surface coatings are added and the inclusion of any wetting agents. The initial wettability of a reusable lens may change when exposed to lens care solutions and tear film components.
Figure 2: Reme-Hart contact angle goniometer is used to measure contact lens surface wettability using sessile drop or captive bubble technique
Wettability can be assessed in several ways in the laboratory using lenses which are unworn (in vitro) or worn (in vivo). One common way is to measure the contact angle of a droplet of liquid on a lens surface (figure 3).4
Figure 3: Diagram showing the contact angle (θ) of a liquid on surfaces: higher contact angles correspond to lower wettability and vice versa
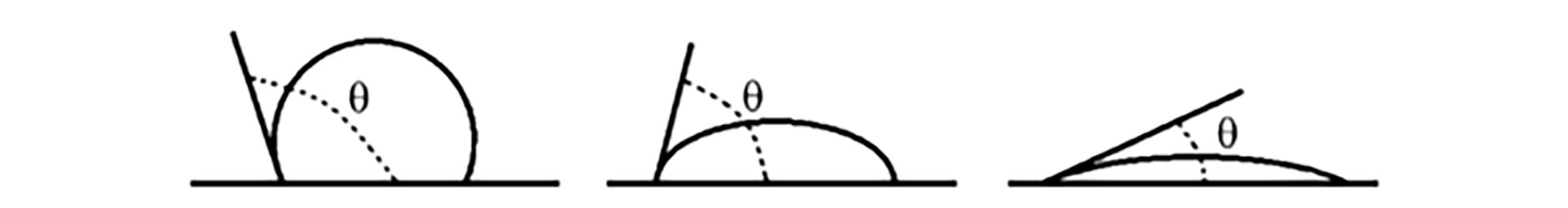
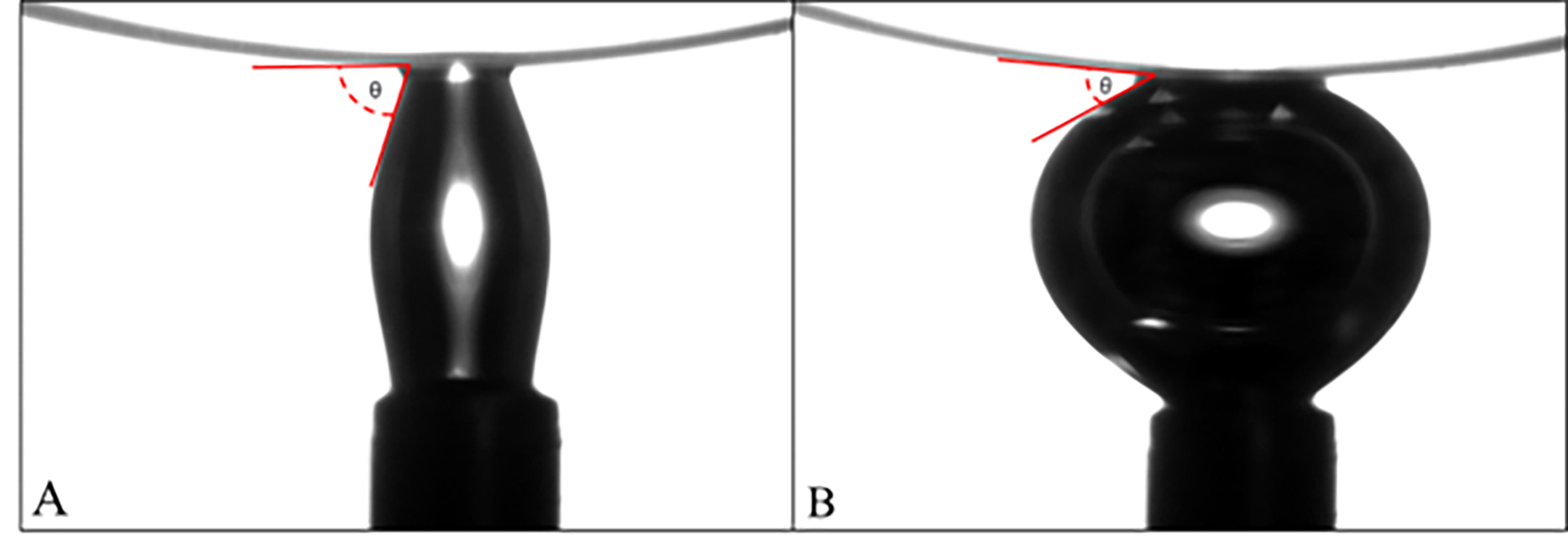
This can be done using sessile drop goniometry, where a droplet of liquid is placed on a solid surface, and the contact angle is measured by means of a digital camera and a goniometer. Alternatively, the captive bubble (figure 4) method requires the lens to be immersed in liquid and the shape of an air bubble injected beneath it is evaluated. It should be remembered that the solution in many blister packs for contact lenses contains agents to improve wettability and these agents are lost along with the solution as wettability is usually measured using saline or water.
Figure 4: Representative photograph of dynamic water captive bubble contact angle measurement technique. Contact angle assessment during A: advancing and B: receding type contact angle. Image from Dr Debarun Dutta, Optometry School, Aston University
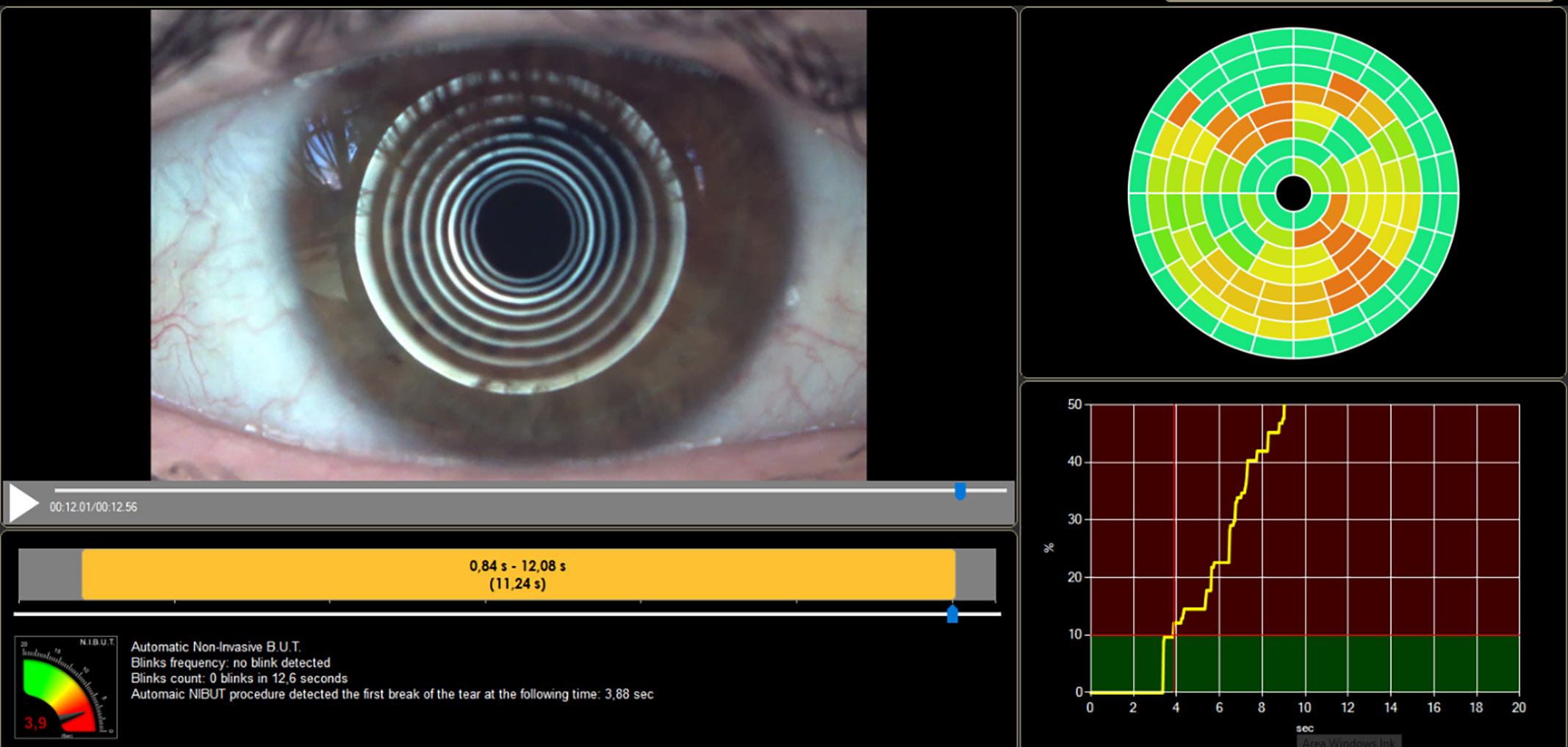
Assessment of the wettability of a contact lens on eye (in vivo) considers the ocular environment, including temperature, osmolarity and tear composition, which can all impact on the wettability of the lens surface. This can be indirectly evaluated by assessing the pre-lens tear film (PLTF) with slit lamp biomicroscopy, using specular reflection at high magnification, interferometry observation techniques and grading scales. Alternatively, the optical quality of the lens can be assessed as this is directly affected by the wettability of the lens surface. The most common method of assessing contact lens wettability is non-invasive break-up time (NIBUT, figure 5), which has the advantage of being available to practitioners in the clinic, covers a large amount of the lens surface and is largely unaffected by eye movements. However, this method is not very reproducible and measurements may vary between instruments.
Figure 5: Assessment of non-invasive tear break up time (NIBUT) using the Idra system
Tears are repelled from a hydrophobic surface but are retained on a hydrophilic surface. The relatively hydrophobic surface of silicone hydrogel lenses5 can be surface treated or copolymerised with other components, but during wear siloxane components can migrate to the surface, reducing wettability gained by these techniques. Wetting agents may alternatively be embedded into the contact lens material or gradually released from the lens during wear to improve the wearing experience.6
The relationship between lens wetting and comfort during contact lens wear is an important one to consider.
Contact lens wettability during wear can be maintained in several ways. Much has been written on various approaches to the subject, including changing the packaging solution in the blister pack, reviewing blink rate and offering exercises to improve it, the use of rewetting drops and the composition of such drops, and contact lens care solutions. However, neither rewetting drops nor lens care solutions have been shown to have a significant impact on lens wettability during wear, suggesting that the overriding factors may be the very fact of the lens being on eye, along with the individual’s tear film composition. In the absence of more data on this subject, eye care practitioners (ECPs) should continue to evaluate each patient’s situation independently regarding factors such as contact lens material, wetting drops and lens care solutions.
Relevance of wettability and contact lenses
- Wetting can be described as the ability of a liquid to spread out over a surface, maintaining contact with it.
- The wettability of a contact lens surface is greatly associated with its biocompatibililty and comfort on eye, and much work has been done to improve surface wetting of contact lens materials.
- Wettability of a contact lens material is important because a number of factors such as ocular physiology, comfort, deposit prevention and optical clarity depend on a moist lens surface.
Maintaining Clean Surfaces
The use of daily disposable contact lenses has increased dramatically in recent years, but reusable lenses still account for at least half of contact lenses used globally. About 70% to 90% of reusable lens wearers care for their lenses with multipurpose disinfecting solutions (MPDS), while the remainder predominantly use peroxide-based systems.
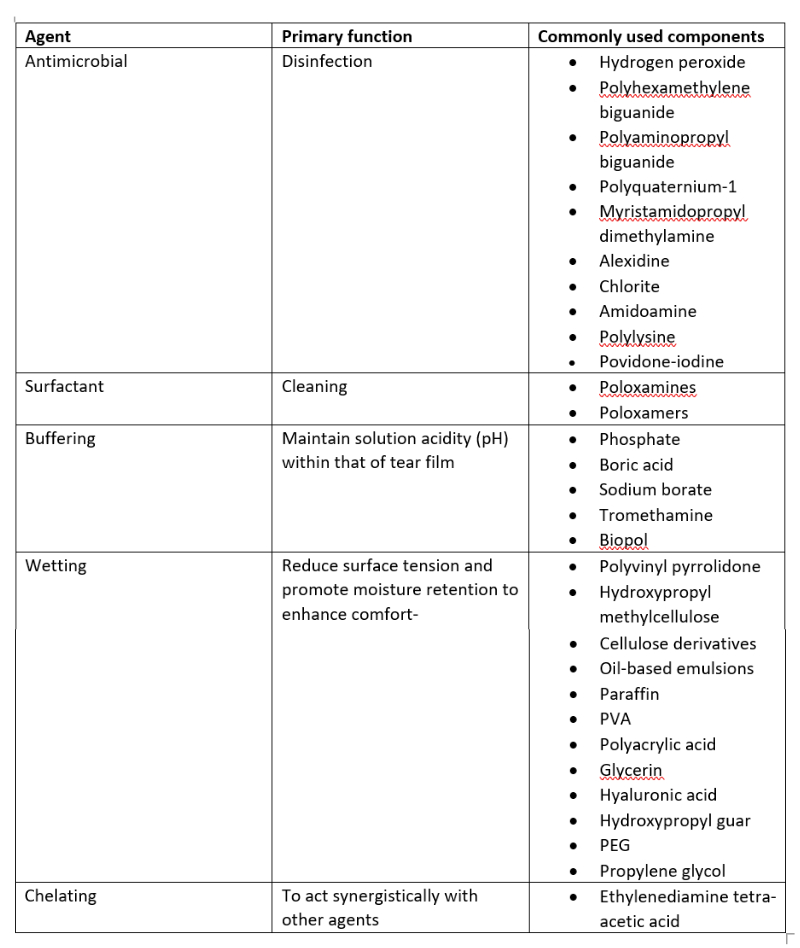
Balancing all the characteristics required of a lens care system is challenging, particularly when effective disinfecting is required without damage to ocular structures. A list of chemical agents typically used in contact lens solutions, along with their functions is shown in table 1.
Table 1: Chemical agents typically used in contact lens solutions, along with their functions
Most multipurpose solutions available on the market have passed the ISO 14729 stand-alone test, requiring the MPDS to reduce the numbers of standard bacterial strains and standard fungi strains by 3.0 log10 and 1.0 log10 respectively, within the recommended disinfection time (four to six hours depending on the solution). While these solutions are easy to use and have the advantage of continuous disinfecting activity due to the presence of a preservative, there can be a potential for corneal staining and such solutions may be less effective against microorganisms such as Acanthamoeba spp. Hydrogen peroxide solutions have the advantages of being potent and preservative-free once neutralised, but are relatively inefficient for long-term storage and highly toxic before neutralisation. Figure 6 reflects the array of solutions that might be acquired by the contact lens wearer without the knowledge of their ECP.
Figure 6: Different contact lens care systems available at Bangkok airport which may be purchased whilst travelling, usually with the contact lens wearer’s ECP being unaware of the products being used. Image from Neil Retallic

A surfactant in a contact lens solution acts as a cleaner or detergent, removing deposits, microorganisms and any other debris from the lens surface in a similar manner to handwashing with soap. A surfactant is both a surface cleaner and wetting agent, and therefore key to contact lens comfort.8,9
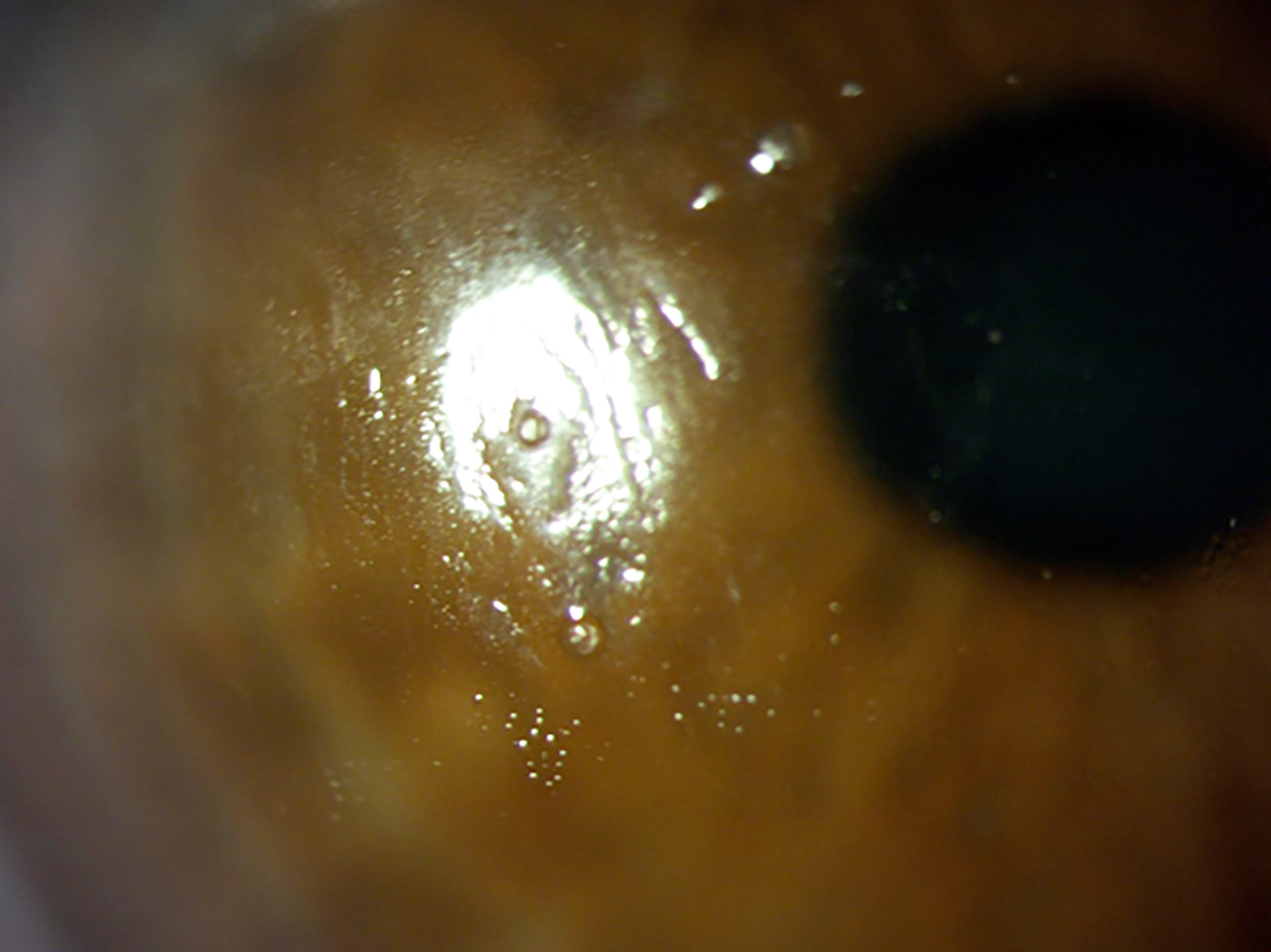
Manufacturers make use of different surfactants in multipurpose contact lens solutions, in differing quantities and combinations. Studies have shown differing levels of efficacy in removing various deposits from different lens types, including rigid corneal lenses (figure 7), which may be of assistance in helping ECPs to more effectively ‘match up’ lenses and solutions for their patients.
Figure 7: Deposits on a rigid corneal lens. Image from Dr Keyur Patel
The purpose of a chelating agent is to act synergistically with other components in the care solution, they react with metal ions to form stable, water-soluble metal complexes. They improve the efficacy of the disinfection components and help to remove tear film deposits, most commonly proteins.
Selecting the most appropriate lens care system for a contact lens patient may well help to reduce the likelihood of dropout of lens wear, and there are a number of factors to consider, including lens type, modality, cost and individual preference of both practitioner and patient. A solution might impact on ocular surface cells, causing discomfort, but it may also reduce lens friction caused by denatured protein, thereby improving comfort. However, studies have shown that the lens care system alone is not a significant factor in contact lens-related discomfort.10
Contact lens properties relationship to comfort
- Contact lens discomfort has been defined by the TFOS International Workshop as a condition characterised by episodic or persistent adverse ocular sensations related to lens wear, either with or without visual disturbance, resulting from reduced compatibility between the contact lens and the ocular environment, which can lead to decreased wearing time and discontinuation of contact lens wear.7
- In conclusion, any correlation between comfort and lens material, or links between comfort and wetting agents either in, or released from, contact lenses is unclear.8
Ideal characteristics of a contact lens care solution9
- Rapid and effective disinfection against a wide variety of pathogenic microorganisms
- No toxicity to ocular tissues
- Compatibility with all contact lens materials
- Simplicity of use
- Lens surface conditioning to enhance wettability and in-eye comfort
- Minimisation of deposition of tear film components
- Inexpensive to purchase
Effect of contact lenses on the tear film
There are over 1,000 proteins in the tear fluid11 and these can interact with contact lenses, causing causing deposition on the lens surface.
The TFOS Contact Lens Interactions with the Tear Film report concluded that the concentration of protein, lysozyme and lactoferrin in the tear film is probably unaffected by contact lenses and recommended further research on the effect of contact lens wear on other tear film components (figure 8). Similarly, although the ability of lipids to deposit on contact lenses is well-known, there is a lack of useful clinical analyses of this during lens wear.
Figure 8: Structure of the tear film and ocular surface (credit: BCLA)
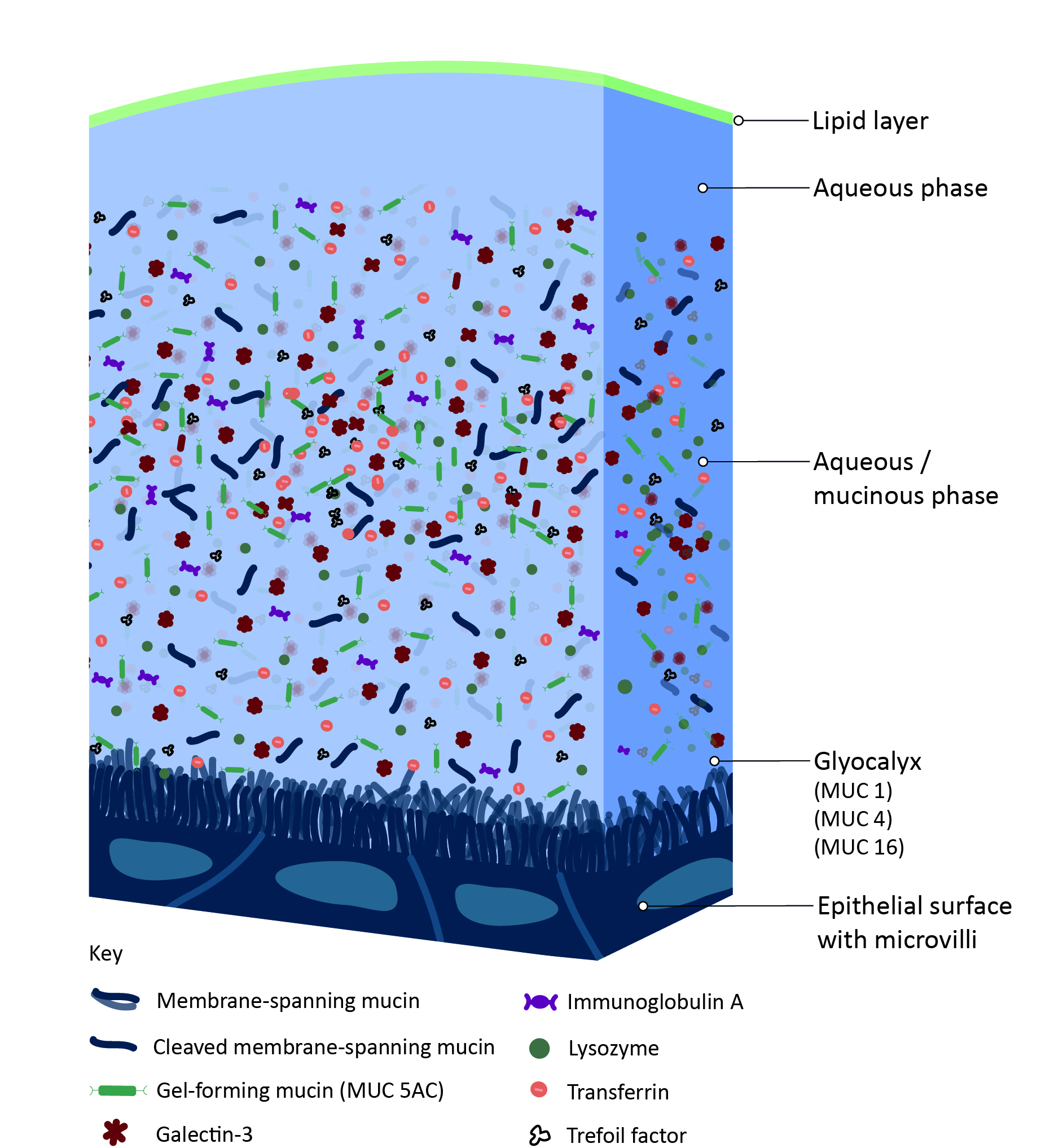
Tear film mucins are produced by goblet cells in the conjunctival epithelium, and both the density of these cells and their mucin secretion is reduced by contact lens wear, although this does not seem to impact on contact lens comfort.
The introduction of silicone hydrogel lenses brought greater oxygen permeability to contact lenses, but also more deposition of tear film components (figure 9). Manufacturers made modifications to lens surfaces to reduce this, and while the lenses appear to have better wettability and compatibility as a result, a link to improved comfort remains unclear.
Figure 9: Deposits and poor wettability on a silicone hydrogel reusable lens. Image from Dr Keyur Patel
Tear film supplements and drops were developed to assist in overcoming contact lens discomfort. In summary, many studies have examined the effect that contact lens wear has on the tear film and have found only a few associations between contact lens discomfort and tear film biochemistry. Patients exhibiting symptoms of discomfort may have differing concentrations of various tear film components, but it is uncertain whether these changes are causing the symptoms or merely coincidental. The comparison between various studies is made more challenging due to the use of different schemes classifying symptomatic and non-symptomatic lens wearers, different wear modalities, and lens care systems and materials. In addition, different biochemical techniques have been used in the studies and this also hampers accurate comparison.
Reduced deposition of proteins has been brought about with lens coatings of hyaluronic acid (HA) and polyethylene glycol (PEG), but rigorous clinical trials on this have yet to take place, and microbial binding to lenses has been reduced by antimicrobial coatings.
The impact of contact lenses on the tear film
- Studies have found that contact lenses can cause changes to the tear film
- Approaches to improve contact lens wettability, with the aim of improving comfort and biocompatibility includes lens surface modifications or/and adding wetting agents
- Although the exact relationship as to how these aspects link to tear film and contact lens comfort is still unclear
Summary
Surely, tear film is very important when considering the biocompatibility of lenses during wear. Further research is needed, however, as the exact role of the tear film and its possible alteration to improve biocompatibility and comfort is still unclear.
- The full report and supplementary information can be accessed at https://doi.org/10.1016/j.clae.2021.02.004
- The BCLA CLEAR Summary report is a short bite-size evidenced based practical guide for clinicians, bringing together the key findings from the report. Accessed via CLEAR (bcla.org.uk) .
- Listen to the BCLA podcast on this topic - https://podcasts.apple.com/br/podcast/bcla-clear-episode-8-contact-lens-wettability-cleaning/id1524673927?i=1000555210174
- The editors for this series are Neil Retallic and Dr Debarun Dutta.
Acknowledgements:
Acknowledgement and recognition to Mark Willcox, Nancy Keir, Vinod Maseedupally, Simin Masoudi, Alison McDermott, Rabia Mobeen, Christine Purslow, Jacinto Santodomingo-Rubido, Silvia Tavazzi, Fabrizio Zeri and Lyndon Jones who were the paper’s authors and the educational grants from Alcon and CooperVision.
The author would like to thank Professor Mark Willcox for reviewing of the article.
Original paper: Willcox M, Keir N, Maseedupally V, Masoudi S, McDermott A, Mobeen R, Purslow C, Santodomingo-Rubido J, Tavazzi S, Zeri F, Jones L. CLEAR - Contact lens wettability, cleaning, disinfection and interactions with tears. Contact Lens & Anterior Eye, 2021 Apr;44(2):157-191.
References
- Willcox M, Keir N, Maseedupally V, Masoudi S, McDermott A, Mobeen R, Purslow C, Santodomingo-Rubido J, Tavazzi S, Zeri F, Jones L. CLEAR - Contact lens wettability, cleaning, disinfection and interactions with tears. Contact Lens & Anterior Eye, 2021 Apr;44(2):157-191.
- Omali NB, Subbaraman LN, Coles-Brennan C, Fadli Z, Jones LW. Biological and clinical implications of lysozyme deposition on soft contact lenses. Optometry & Vision Science, 2015;92(7):750–7. https://doi.org/10.1097/OPX.0000000000000615.
- Walther H, Subbaraman L, Jones LW. In vitro cholesterol deposition on daily disposable contact lens materials. Optometry & Vision Science, 2016;93(1):36–41 https://doi.org/10.1097/OPX.0000000000000749
- Donaldson E, Alam W. Wettability. 1st ed. USA: Gulf Publishing Company; 2008.
- Keir N, Jones L. Wettability and silicone hydrogel lenses: a review. Eye & Contact Lens, 2013;39(1):100–8. https://doi.org/10.1097/ICL.0b013e31827d546e.
- Tighe BJ. A decade of silicone hydrogel development: surface properties, mechanical properties, and ocular compatibility. Eye & Contact Lens, 2013;39(1):4–12. https://doi.org/10.1097/ICL.0b013e318275452b.
- Nichols JJ, Willcox MD, Bron AJ, Belmonte C, Ciolino JB, Craig JP, et al. TheTFOS international workshop on contact lens discomfort: executive summary. Investigative Ophthalmology & Vision Science, 2013;54(11):TFOS7–13. https://doi.org/10.1167/iovs.13-13212.
- Jones L, Brennan NA, Gonzalez-Meijome J, Lally J, Maldonado-Codina C, Schmidt TA, et al. The TFOS international workshop on contact lens discomfort:report of the contact lens materials, design, and care subcommittee. Investigative Ophthalmology & Vision Science, 2013;54(11). https://doi.org/10.1167/iovs.13-13215.TFOS37-70.
- Jones L, Senchyna M. Soft contact lens solutions review: part 1 - components of modern care regimens. Optometry in Practice, 2007;8:45–56.
- Ramamoorthy P, Sinnott LT, Nichols JJ. Treatment, material, care, and patient-related factors in contact lens-related dry eye. Optometry & Vision Science, 2008;85(8):764–72. https://doi.org/10.1097/OPX.0b013e318181a91f.
- Zhou L, Zhao SZ, Koh SK, Chen L, Vaz C, Tanavde V, et al. In-depth analysis of the human tear proteome. J Proteomics 2012;75(13):3877–85. https://doi.org/10.1016/j.jprot.2012.04.053
