If we take just a moment to reflect that both tear production and quality are affected by the levels of sex hormones, it will come as no surprise that menopause and dry eye disease (DED) are closely linked. In fact, the shifts in levels of sex hormones in women will impact on tear film throughout their adult life; from the menstrual cycle to pregnancy, from the contraceptive pill to breast feeding, from peri-menopause to post-menopause. All women will experience at least some of these hormone changes and, consequently, may be impacted by dry eye symptoms.
It is suggested that approximately 61% of women who are peri-menopausal or menopausal suffer from dry eye disease. This number increases to 69% of women taking oestrogen-only hormone replacement therapy (HRT).1 Additionally, it has been found that the rate of DED in women over 50 years of age is almost double that in men.
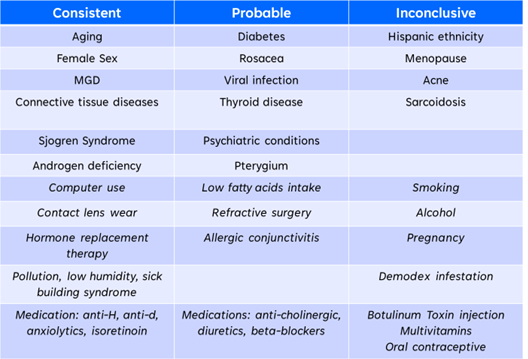
In the field of optometry, much work on DED has been carried out by the Tear Film and Ocular Surface Society (TFOS). In 2007, this multi-disciplinary world-wide group of experts published the TFOS Dry Eye Workshop (DEWS) report on DED and then, in 2017, DEWS II was published. However, if we look at the DEWS II report, we can see that, whilst both aging and female sex are consistently linked with DED, any link with menopause is thought to be inconclusive (table 1). It is worth noting that both androgen deficiency (one of the sex hormones) and HRT are both consistently linked with DED.
Table 1: Risk factors for dry eye disease as cited in the TFOS DEWS II
Hormonal Changes in Menopause
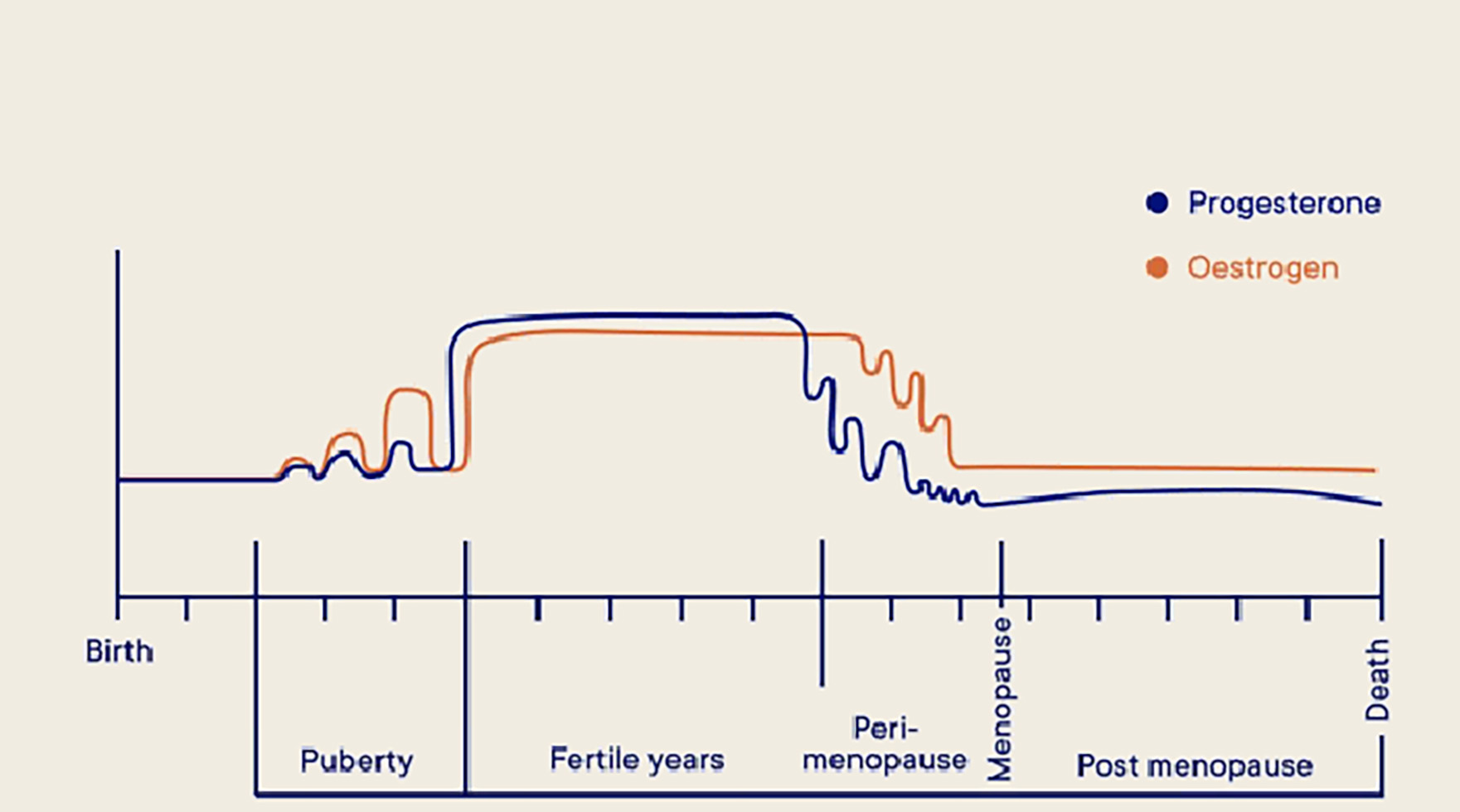
Women have both male and female sex hormones and levels of these sex hormones reduce dramatically during menopause (figure 1).
- Reduced levels of androgens; these are male sex hormones and include testosterone
- Reduced levels of oestrogen; these are female sex hormones
- Reduced levels of progesterone; these are female sex hormones and play a vital role in the menstrual cycle and pregnancy
Figure 1: There is a dramatic reduction in female hormone levels during menopause
Sex hormones affect both the production and the quality of all the tear film components; aqueous, lipid and mucin. Therefore, it is easy to see that drastically reduced levels of these hormones will inevitably affect the tear film. Some studies have found that post-menopausal women with severe evaporative dry eye have lower levels of both oestrogen and testosterone than women less affected by dry eye disease.2 However, other studies have also found increased levels of oestrogen and testosterone in patients with DED.3
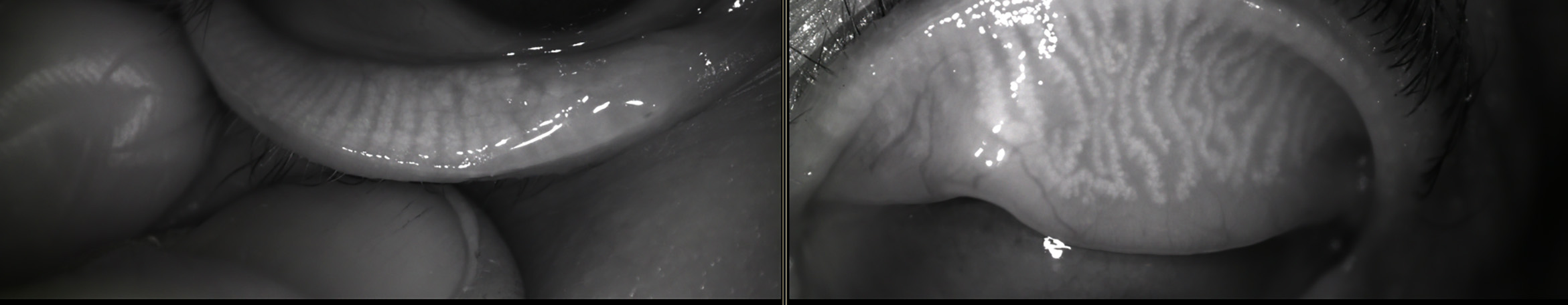
It has also been suggested that the increased levels of oestrogen and testosterone found in some women with dry eyes may be due to a feedback mechanism. Studies have observed that testosterone levels may increase as a result of meibomian gland loss in post-menopausal women (figure 2) while, in mouse models, testosterone has been seen to be protective against damage to meibomian glands.4 It is, therefore, possible that, paradoxically, levels of sex hormones increase, to combat the impact of DED.
Figure 2: Testosterone levels may increase as a result of meibomian gland loss in post-menopausal women
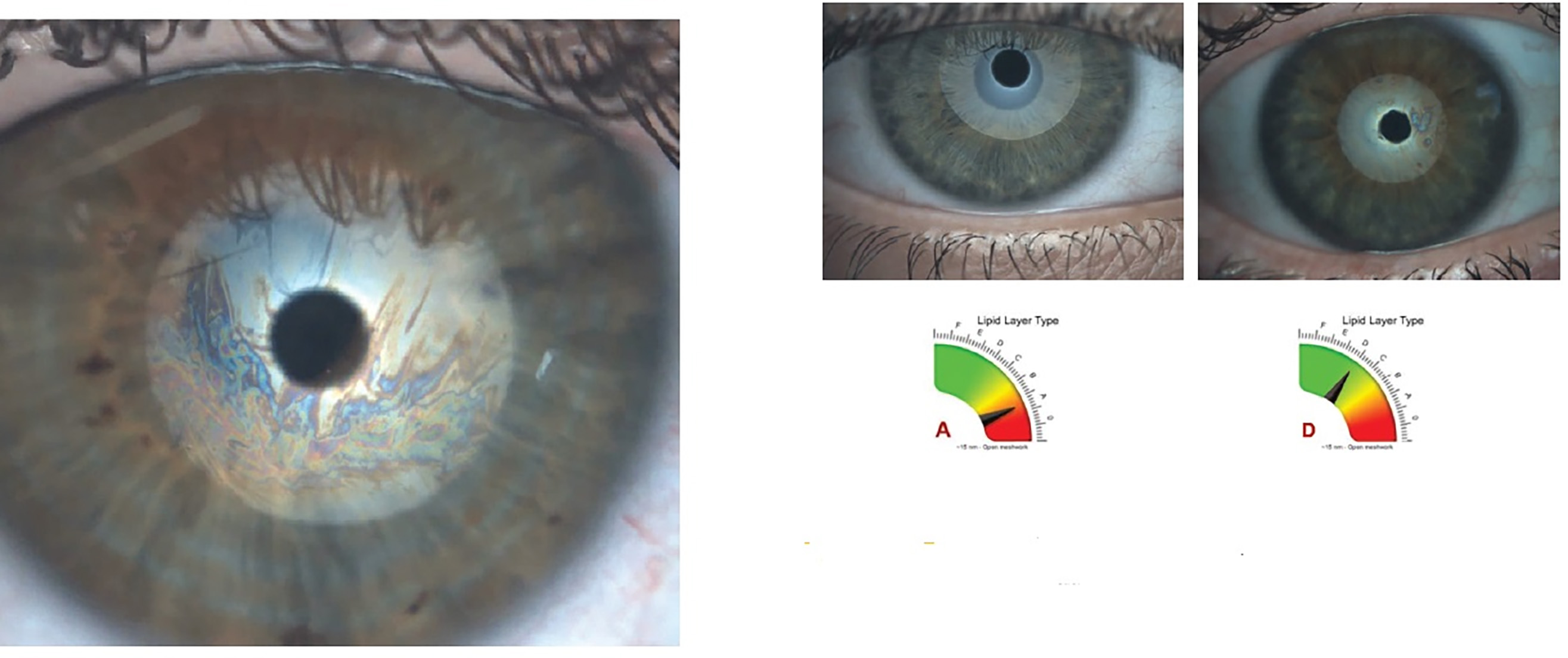
Sex steroid receptors have been found in the meibomian glands. Androgen binds with these receptors, and this results in both the synthesis and secretion of tear film lipids.5 However, oestrogen has been shown to cause a decrease in lipid production,6 and some researchers have suggested that increased levels of oestrogen may be a risk factor in DED (figure 3).
Figure 3: Oestrogen levels can influence the lipid layer of the tear film
The conflicting research shows that the relationship between sex hormone levels and clinical signs and symptoms of DED is a complex one. However, the balance of evidence supports the following:
- There is a reduction in the levels of sex hormones and this has a direct effect upon both production and quality of tears
- Mechanisms for effect are a combination of a reduction in hormone levels, changes in feedback mechanisms and shifts in receptor sensitivity
- There is an alteration in the homeostasis of the tear film which results in an increase in inflammation and DED
The overwhelming numbers of menopausal women who present with DED cannot be ignored and, as eye care professionals, we are in the perfect place to address this issue.
Effects of HRT on the Ocular Surface
Many thousands of women take HRT to combat the effects of menopause, around 15% of all women aged between 45 and 64 years (figure 4). HRT replaces the hormones lost through menopause and so, one might expect that it would improve signs and symptoms of DED. However, the largest cross-sectional study to date showed that long-term use of HRT actually increases the risk and severity of DED. Both high dose and duration resulted in an increase of dry eye symptoms in patients.7
Figure 4: The number of women taking HRT to combat the effects of the menopause is increasing in the UK
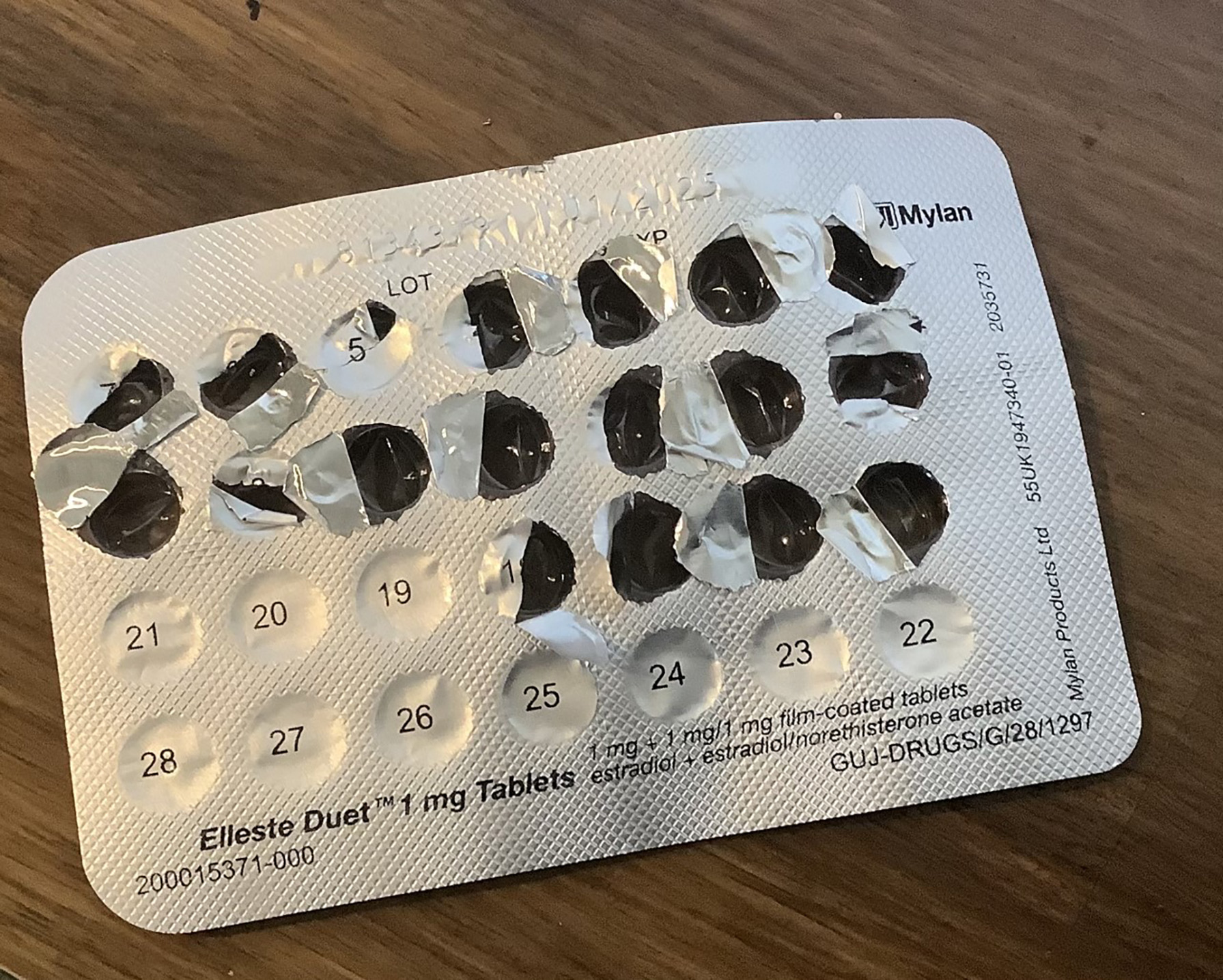
In one study, DED was found to be more common in patients taking oestrogen-only HRT than those taking a combination therapy.8 Each 3-year increase in duration of HRT resulted in a 15% increase in the risk of clinically diagnosed DED. In another study, a worsening in dry eye symptoms was also found in patients taking oestrogen-only HRT whilst an increase in tear secretion was found in patients on combination therapy.8
Once again, there is conflicting evidence regarding the impact of HRT on the ocular surface. However, the balance of evidence suggests that, whilst oestrogen-only HRT may increase the risk of DED over time, a combination therapy may improve symptoms. It is interesting to note that the DEWS II report lists HRT as one of the consistent risk factors for DED, whilst menopause is listed as an inconsistent risk factor (table 1).
Anti-Oestrogen Drugs and DED
Typically, anti-oestrogen drugs are used to treat and prevent oestrogen-positive breast tumours. The most commonly used drugs are:
- Tamoxifen
- Anastrozole
- Letrozole
It is interesting to note that these drugs are also sometimes used off-licence by body builders.
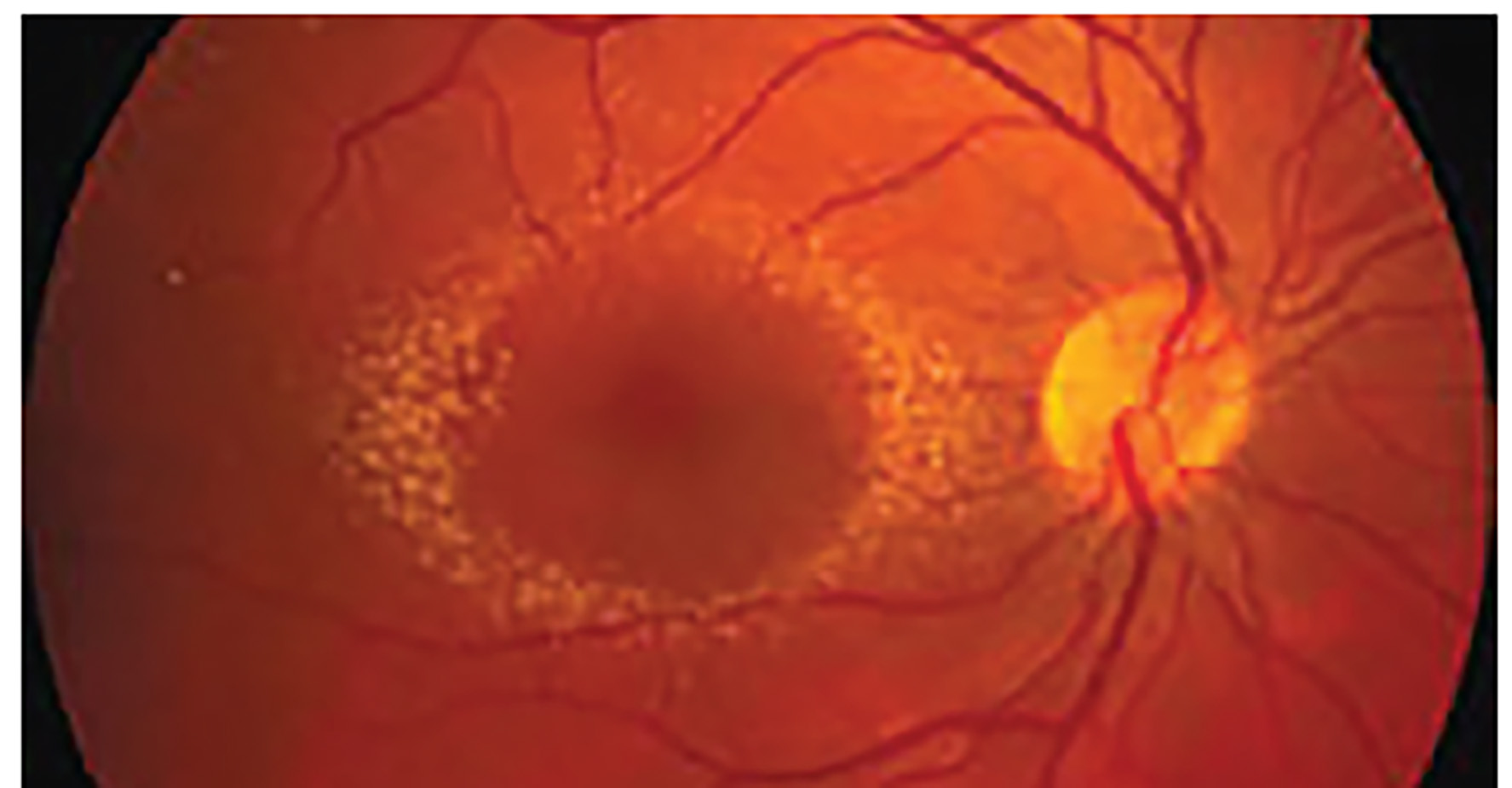
We have discussed the impact of reducing levels of sex hormones, particularly oestrogen, on tear quality and quantity, and so it will come as no surprise to find that these anti-oestrogen drugs bring about a similar effect upon the tear film as menopause. The author undertook a study of 1000 patients taking tamoxifen, as part of a research project to investigate ocular adverse reactions to tamoxifen. In addition, 100 patients were followed prospectively for five years. As well as both corneal and retinal changes found in some patients (figure 5), the prevalence of dry eye disease was found to be 7 times higher in the tamoxifen group than in the age-matched control group.9
Figure 5: Refractile crystals around the macula due to high dose tamoxifen
How to treat DED and maintain eye health in menopausal women
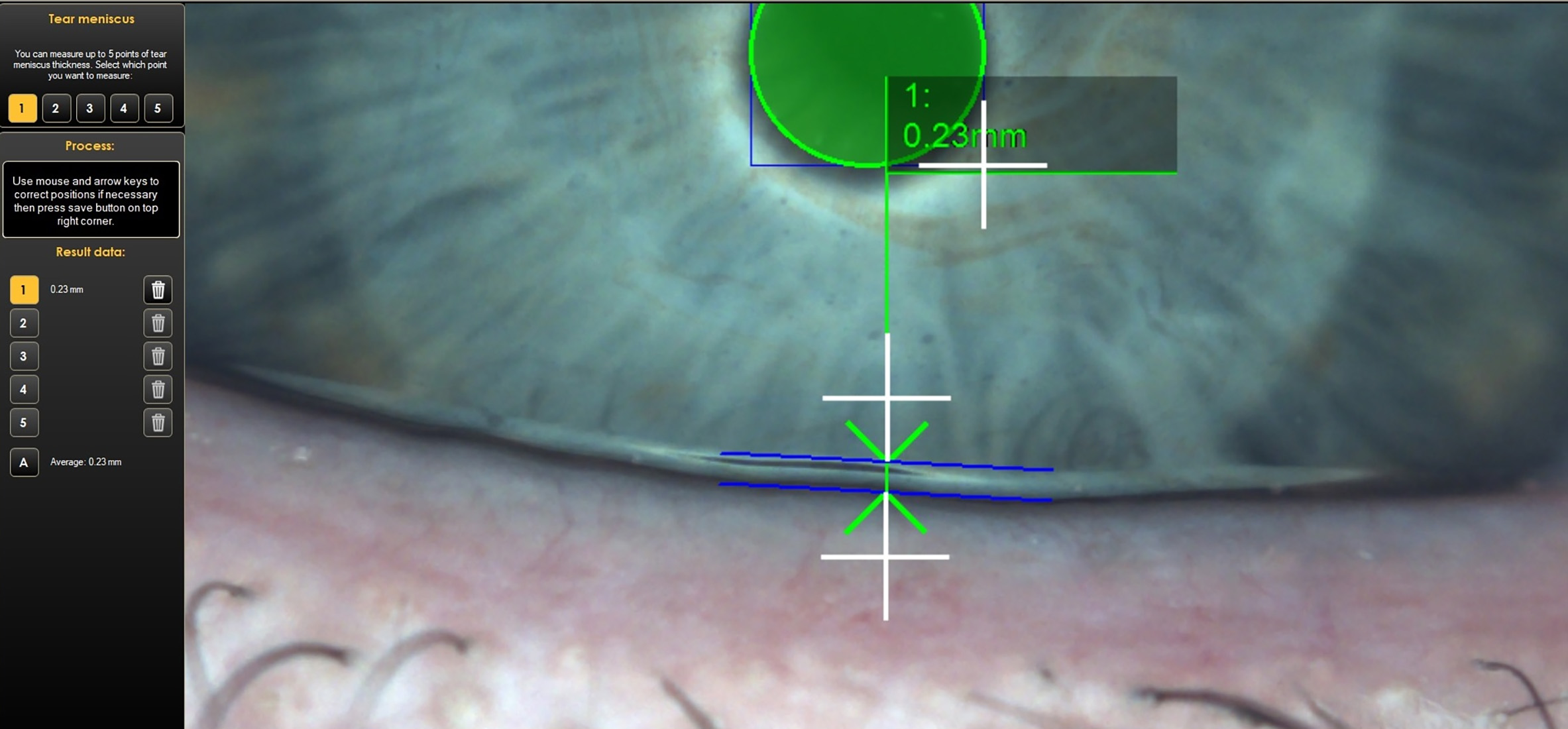
Key to managing DED in menopausal women is to maintain the integrity of the normal tear film (figure 6). This will require maintenance of a healthy lipid layer, by addressing any meibomian gland dysfunction (MGD, figure 7), and ensuring adequate aqueous volume (figure 8).
Figure 6: A healthy tear film
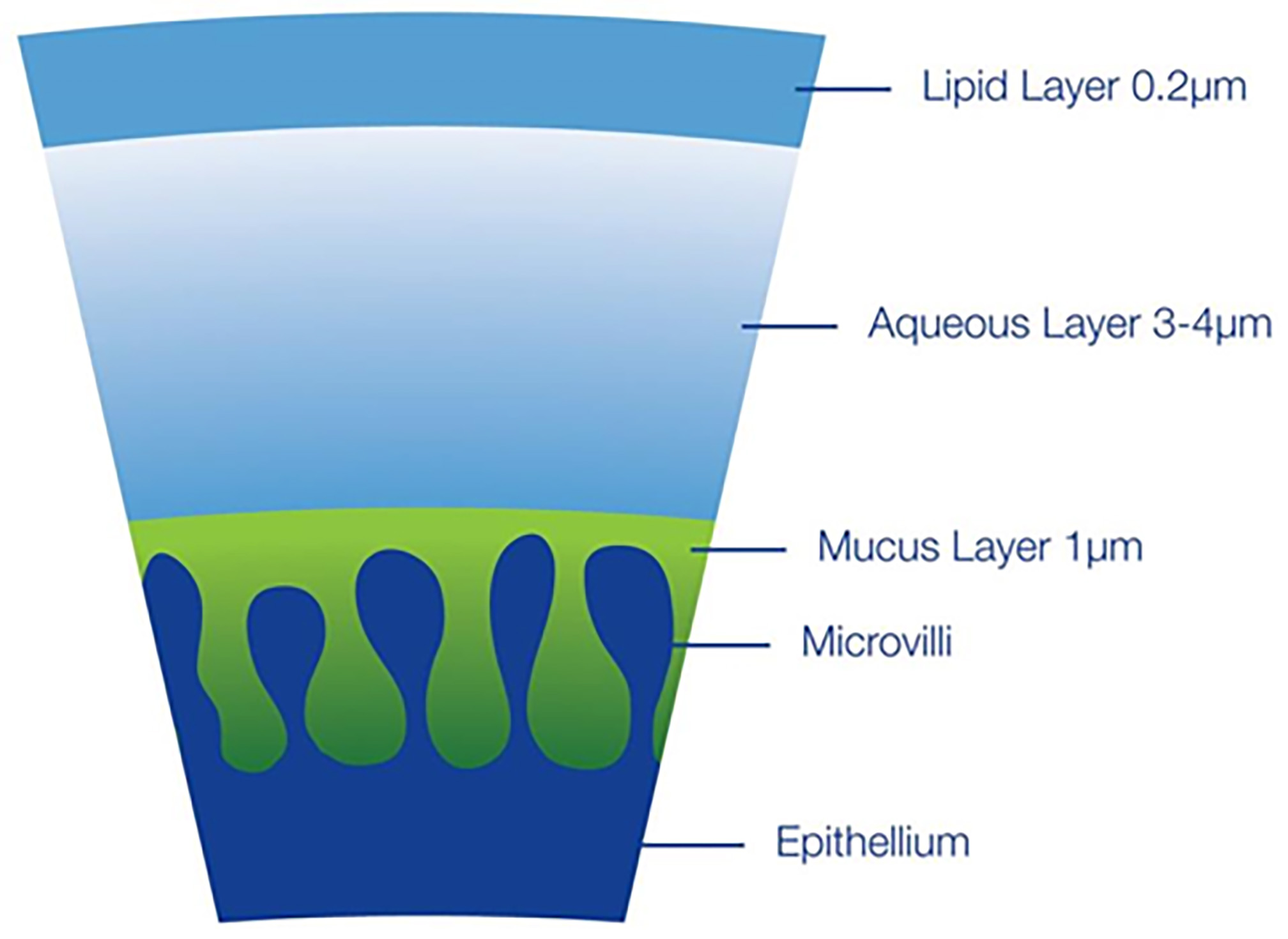
Figure 7: Meibomian gland dysfunction

It seems sensible to start with a simple routine to see if there is an improvement in both signs and symptoms. This can be augmented as needed.
- Lid hygiene
- reservative free artificial tear drops
- Preservative free artificial tear gel/ointment
- Omega-3/6 supplements and dietary advice
- Punctum plugs
- Meibomian gland expression
- IPL/Lipiflow
Let’s take a look at each of these in turn.
Figure 8: Aqueous volume may be assessed by measurement of the inferior tear prism height. A value of less than 0.2mm might suggest a low aqueous volume.
Lid Hygiene
It would be nice to think that the days of using a hot flannel followed by diluted baby shampoo on the tip of a cotton bud are over. However, patients still present with DED, having been told to do exactly this. To clean the lids, heat needs to be applied in a safe, sustained fashion. A heated eye mask is the perfect thing for this. Hot flannels lose their heat within seconds, whilst it is entirely possible to get the temperature too hot in the first moments against the eye lids. Proprietary eye masks reach a safe heat, which is maintained for around 10 minutes, allowing the meibomian glands to be warmed up, softening any sebum that has congealed and become stuck in the glands. Lid massage after the period of heat should be robust – it is worth demonstrating to the patient exactly where they should be applying some gentle pressure to encourage expression from the glands.
Cleaning the lids and lashes after the heat and massage is imperative and should be done using proprietary lid wipes or a lid cleaning solution with lint-free pads. Cotton wool and cotton buds contain lint that gets left behind in the lids and lashes, compounding the problem rather than alleviating it. Any solution of diluted baby shampoo affects the quality of the tear film, worsening the problem rather than improving it.
Good quality lid hygiene can improve MGD substantially, making a big difference to the secretion of lipid.
Preservative-free Topical Lubricants
Historically, benzalkonium chloride was the chemical preservative used to preserve multidose containers of artificial tear supplements. However, it has a detrimental effect upon the ocular surface, breaking down the tears and increasing dry eye symptoms. We want our patients to use their dry eye drops regularly and to be proactive in their use. Therefore, preservative-free preparations should always be recommended. It is also important to consider the ease of use for our patients. There are several delivery methods employed by pharmaceutical companies, each claiming ease of use to the patient. Experience suggests that different patients will find different methods work best for them. It is important to know how the delivery systems vary and to be able to suggest alternatives for our patients.
Experience shows that patients rarely use their drops regularly enough and so it is worth having a detailed conversation about regularity of use and the need to be proactive. If the patient always gets symptoms when staring at their computer screen, or undertaking a long drive, then it should be recommended that they use their drops before starting the activity.
Preservative-free Lubricant Gels
Many patients report waking during the night with dry eye symptoms and/or waking in the morning to find it difficult to open their eyes. Use of a more viscous artificial tear supplement at bedtime is the obvious way to alleviate these symptoms. It is important to explain to the patient that these gels and ointments may affect vision, however. Using them last thing before sleep is the best way to avoid vision problems.
In addition, lanolin or paraffin wax are commonly used in ointments and some patients may be allergic to one of these. Whilst gels are slightly less viscous, they do not contain these products, nor do they impact upon vision so much, and so may be a good option for our patients.
Omega-3/6 Supplements and Dietary Advice
Increasing levels of these oils in the diet has been shown by some studies to improve the quality of the tear film and ocular surface and many patients like to take a supplement for this. Typically, these are found in oily fish and so patients may choose simply to include more of these in their diet. However, vegans and vegetarians can find supplements containing these oils extracted from seaweed.
Punctum Plugs
Punctum plugs have been successfully used to reduce outflow of tears from the ocular surface for many years (figure 9). Generally, they are used as second line therapy, when lid hygiene and artificial tear supplements are not providing adequate relief from symptoms. Initially, a dissolvable plug is inserted into the punctum and this can last anything from 1 to 6 months. Over this period of time, the patient is able to assess whether there is a sustained improvement in symptoms. If so, permanent plugs may be inserted into the puncta and these can safely remain in place indefinitely.
Figure 9: A punctum plug recently inserted
Meibomian Gland Expression
Experience has taught me that patients often are not robust enough with expression of the meibomian glands during their lid hygiene. Therefore, you may wish to offer consulting room meibomian gland expression. In my practice, the patient would use a heat mask for the appropriate period of time, after which, they are seen by the optometrist to have the glands expressed in the consulting room. It has the advantage of the use of the slit lamp, enabling us a very clear view of how and where to express. As well as digital expression, using the finger tips, it is very useful to have some round end tipped tweezers and a round end/golf club spud. These blunt ended instruments allow safe and painless expression of the glands and subsequent cleaning of the eyelid margin by the optometrist. Recently, a heated mask that also massages the lids has been introduced (figure 10).
Figure 10: The Essilor Activa mask both heats and massages the lids
Intense Pulsed Light and Lipiflow Systems
Whilst these techniques are not listed as treatments for DED in the DEWS II report, many practices report great success with them. Intense pulsed light (IPL) uses pulsed light to treat DED caused by MGD in practice (figure 11). Lipiflow is an in-practice technique that uses heat and massage to treat MGD; an automated gland expression, as it were. Another option, recently introduced by Thea, is Blephasteam. This is a heated eye-mask worn by the patient to heat the glands to promote ease of meibomian gland expression (figure 12).
Figure 11: The Essilor TearStim intense pulsed light system

These techniques require investment by the practice to purchase the equipment as well as chair time with the optometrist and this will need to be reflected in the cost to the patient.
Figure 12: The Blephasteam system from Thea

Let’s Talk Menopause
Until recently, menopause was rarely discussed in public. However, celebrities such as Davina McCall and Gabby Logan have spoken very openly about their experience of menopause and have encouraged women to be more open about their own experience. In addition, companies are starting to take notice of menopausal symptoms with a view to supporting women through menopause. Hot flushes are just the tip of the iceberg when it comes to menopausal symptoms. Women may suffer depression, mood swings, lack of sex drive and memory issues, to name just a few of the typical symptoms driven by menopause. Historically, this was swept under the carpet and women have even been encouraged to leave their job due to menopausal symptoms rather than being encouraged to seek help to continue in their role.
As eye care professionals, we should be looking for and addressing any ocular symptoms of menopause in all women over 40 years of age. Symptoms may well start with peri-menopause and can continue for the rest of a woman’s life. Clearly, we need to adopt a sensitive approach; not every woman will have symptoms of DED relating to menopause. However, we should not shy away from the subject, simply because the symptoms are linked to menopause.
We talk to our patients already about age-related conditions, such as cataracts and AMD. We also discuss gender-related issues. again such as AMD. Therefore, it’s not a wild leap to discuss DED in terms of prevalence of those most likely to have symptoms of it. Most women will understand immediately, when told that their dry eye symptoms may be related to hormone changes; that peri-menopause, menopause or post-menopause may well be impacting the ocular surface. Very few women are aware that DED can be caused/exacerbated by menopause and all are relieved to have an explanation for their symptoms.
Historically, DED has been played down, especially by the medical profession. However, Quality of Life (QoL) questionnaires have revealed that patients with DED rate the impact of the disease on a par with severe angina; a telling indication of the impact that chronic health conditions like DED can have.
Menopause affects half of our population and so it’s imperative that we discuss eye conditions related with menopause with our patients. A better understanding of the condition can make it a lot easier for the patient to deal with it.
- Polly Dulley MPhil BSc(Hons) MCOptom is an optometrist in independent practice in Essex.
Useful resources
- https://rockmymenopause.com Rock My Menopause is the public-facing campaign of the Primary Care Women’s Health Forum (PCWHF), a group of 10,000 healthcare professionals with a special interest in women’s health. Their aim is to equip people with the expert menopause information and support they need to become more menopause aware.
- https://pcwhf.co.uk The Primary Care Women’s Health Forum (PCWHF) has its own site aimed at health professionals
- https://thebms.org.uk The website for The British Menopause Society (BMS), the specialist authority for menopause and post reproductive health in the UK, has a wealthy of useful information and statistics for health professionals
References
- Schaumberg DA, Sullivan DA, Buring JE, Dana MR. Prevalence of dry eye syndrome among US women. American Journal of Ophthalmology, 2003;136(2):318-26.
- Gagliano, C et al. Low levels of 17-β- oestradiol, oestrogen and testosterone correlate with severe evaporative dysfunctional tear syndrome in post-menopausal women: A case-control study. British Journal of Ophthalmology, 2014; 98:371-376.
- Ablamowicz AF, Nichols JJ, Nichols KK. Association between serum levels of testosterone and estradiol with meibomian gland assessments in postmenopausal women. Investigative Ophthalmology & Vision Science, 2016;57:295–300.
- Esmaeli B, Harvey JT, Hewlett B. Immunohistochemical evidence for estrogen receptors in meibomian glands. Ophthalmology, 2000;107:180–4.
- Suzuki T, Schirra F, Richards SM, Jensen RV, Sullivan DA. Estrogen and progesterone control of gene expression in the mouse meibomian gland. Investigative Ophthalmology & Vision Science, 2008;49:1797–808.
- Peck T, Olsakovsky L, Aggarwal S. dry eye syndrome in menopause and perimenopausal age group. Journal of Midlife Health, 2017; 8(2): 51–54.
- AlAwlaqi A, Hammadeh M. Examining the relationship between hormone therapy and dry-eye syndrome in postmenopausal women: A cross-sectional comparison study. Menopause, 2016;23:550–5.
- Schaumberg DA, Buring JE, Sullivan DA, Dana MR. Hormone replacement therapy and dry eye syndrome. JAMA, 2001;286:2114–9.
- Dulley P. Ocular adverse reactions to tamoxifen--a review. Ophthalmic & Physiological Optics. 1999; 19: 2-9.
