The second of in a quarterly series of online events, supported by Alcon, took place recently and looked at the topic of contact lens comfort. In the second of two reviews of this event (see here for Alcon talk #1), the focus is upon:
- The tear film
- Contact lens comfort
- The ‘ideal’ contact lens
- Contact lens discomfort (CLD)
The Tear Film
In any discussion of contact lenses and comfort, it is important to consider the basic principles of the tear film. Often, we are equipped with the fundamentals at university but it is easy to forget the details once in practice where we may be consumed by other pressing matters. It is important to revisit the structure of the tear film and understand the building blocks upon which innovations such as contact lenses are made.
Firstly then, what is the importance of the tear film? The tear film is responsible for a number of important functions:
- Regulates ocular hydration
- Nourishes the ocular surface
- Maintains optical quality
- Cleans the ocular surface
- Regulates the ocular surface pH
- Protects the eye from external threats, such as infection
The earlier concept of a three-layer model of the tear film (figure 1) is now widely accepted to be an oversimplification. Newer evidence suggests a two-layer concept consisting of a lipid layer and a muco-aqueous gel layer (figure 2).
Figure 1: Traditional three-layer model of the tear film

The lipid layer (figure 2a) is the thinnest layer, ranging from 15 to 157nm (average 42nm) in thickness. To put this into perspective, the thickness of a strand of human hair is approximately 80,000nm. Though it is the thinnest layer, it is arguably the most important one as it helps to stabilise the tear film by retarding evaporation. The lipid layer is mainly produced by the meibum and secreted from the lid margins. The blinking mechanism helps to spread this across the ocular surface.
Figure 2: (Left to right) Two-layer model. (a) Lipid layer. (b) Muco-aqueous gel layer
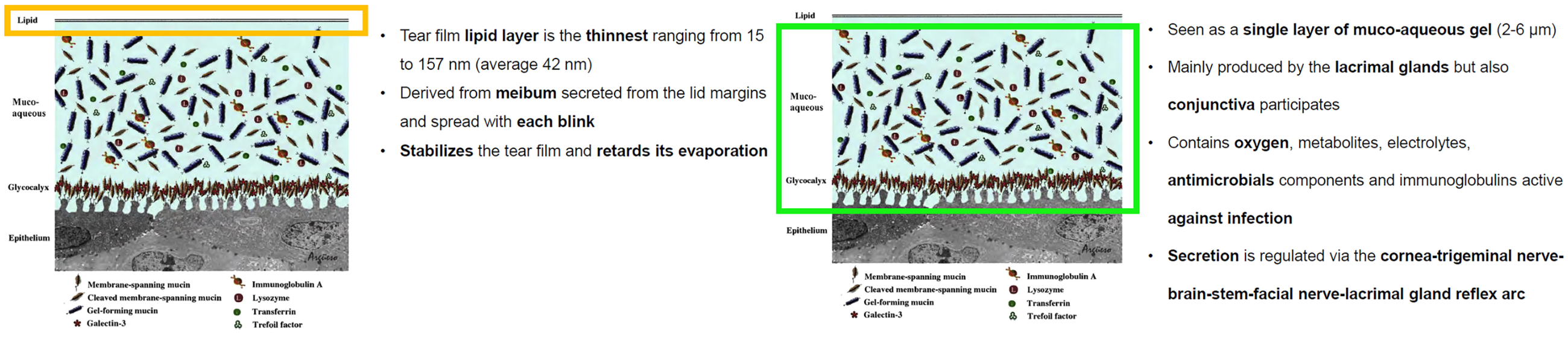
The second layer, collectively referred to as the muco-aqueous layer, acts as a single, dynamic unit and is mainly produced by the lacrimal glands, with the mucins produced by the conjunctiva (figure 2b). It acts to provide oxygen, metabolites, electrolytes, anti-microbials and immunoglobulins to the ocular tissue, washing away any debris. Secretion is regulated by the cornea-trigeminal nerve-brain-stem-facial nerve-lacrimal gland reflex arc.
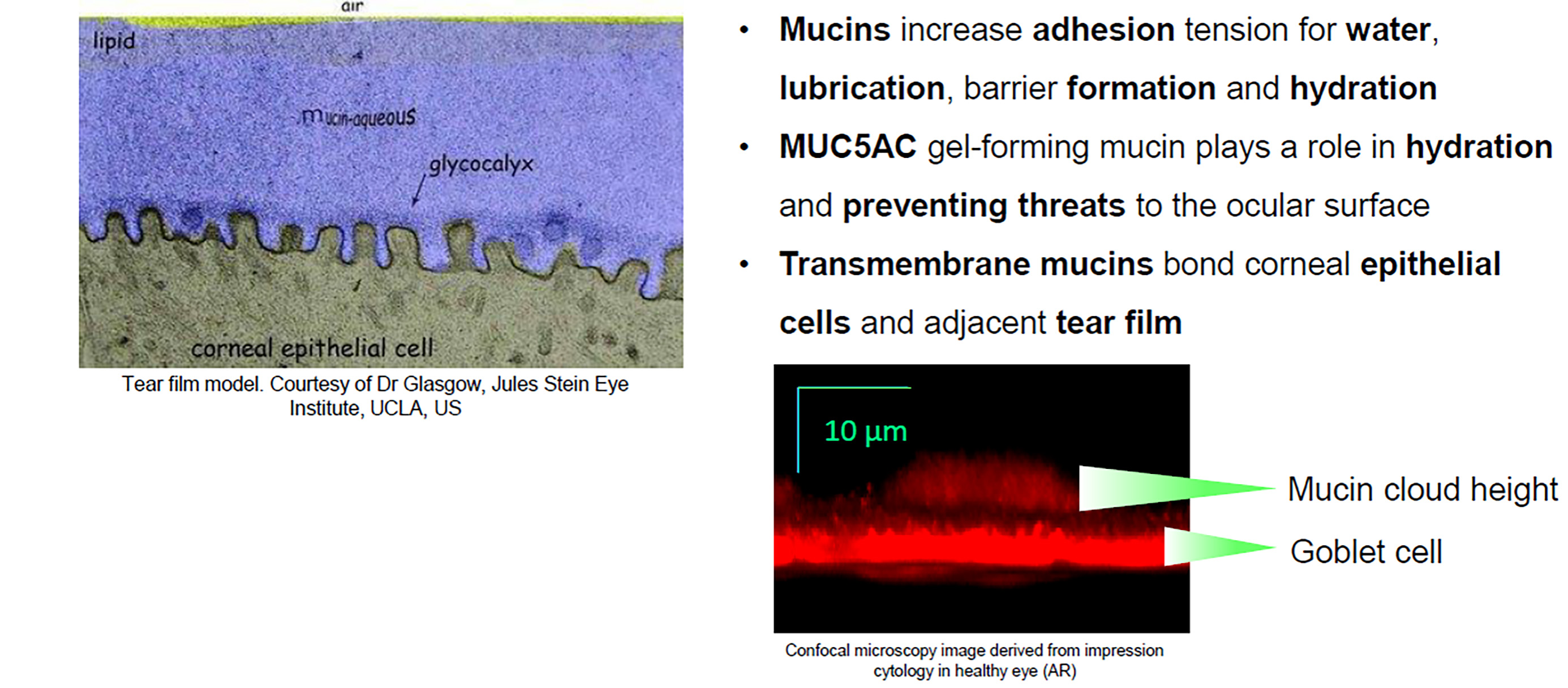
The mucins provide a dual function; increasing water adhesion tension to maintain lubrication, and to form a barrier to impede dehydration. The mucins can be divided into two types: MUC5AC gel-forming mucin, which play a role in hydration and preventing threats to the ocular surface, and transmembrane mucins, which help to bond corneal epithelial cells and the adjacent tear film (figure 3).
Figure 3: The role of mucins in the tear film
This structure of the tear film is disrupted by the insertion of a contact lens (figure 4). Contact lenses are 10x thicker than the tear film. The introduction of the contact lens splits the tear film into anterior and posterior components. Consequentially, there is a reduction of tear volume, a thinning of the lipid layer and increased evaporation, once lenses are inserted and sit in the tear film. There is also a higher chance to observe incomplete blinking and increased inter-blink interval.
Figure 4: The impact of a contact lens upon the tear film
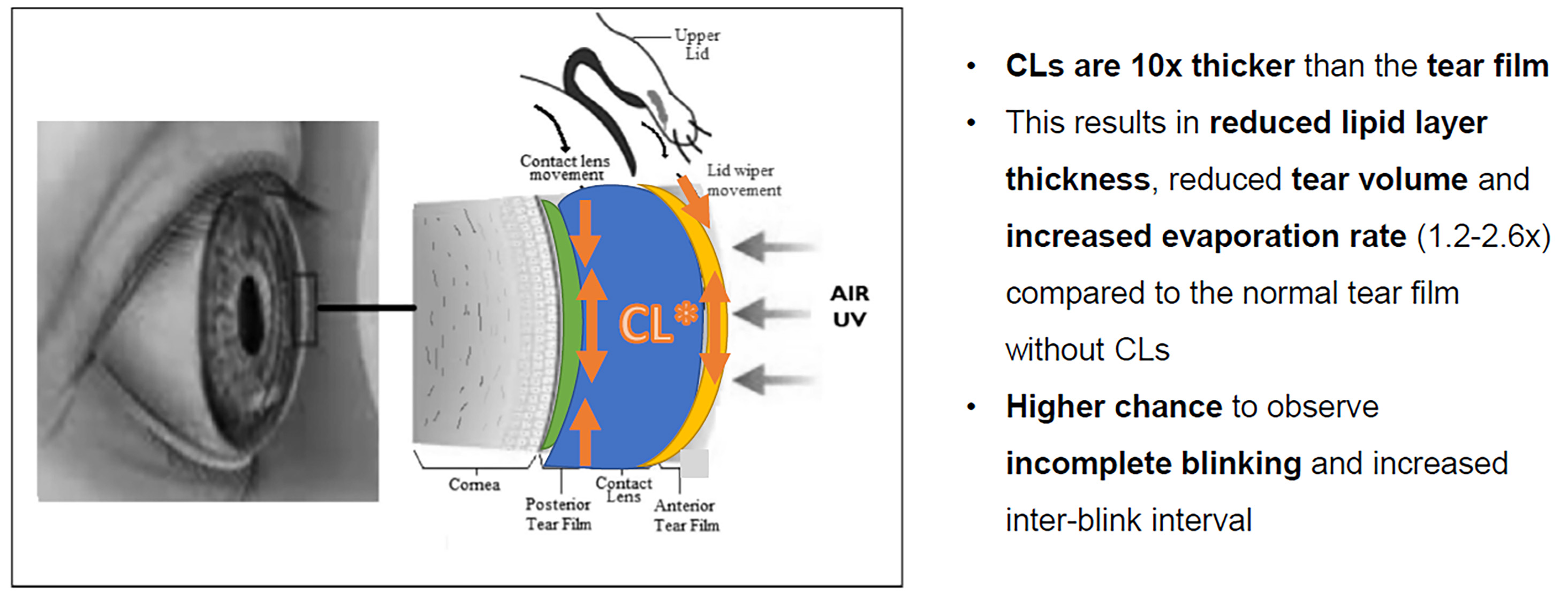
CLs wear may increase the risk of developing dry eye by up to three times. This is appreciable since there will be a reduction and delay of the tear exchange underneath the contact lens. There is a stagnation of tears beneath the contact lens and the possibility of the formation of mucin balls and staining.
The ‘Ideal’ Contact Lens
So, with the understanding that contact lenses can hinder the optimal tear film, is there an ‘ideal’ contact lens that would work in harmony with it?
Researchers have worked towards this idea for decades, balancing the different ideal properties required from a contact lens. At times, these properties can be at the compromise of each other. For example, a high Dk/t allows good oxygen transmissibility through the lens, but since there is a high concentration of silicone needed in the lens to achieve this, the lens can feel more rigid and so interfere with the comfort.
There are a number of factors to consider for the ‘ideal’ contact lens. These include:
- Modulus: Modulus refers to the flexibility or elasticity, in other words, how well does the lens retain its shape during handling. It depends on its material, thickness and diameter. Low modulus can result in difficult handling, whereas high modulus can result in poorer comfort.
- Tribology: Tribology refers to the interaction between surfaces in relative motion. Lubricity, friction and wettability are all essential components to this.
- Lubricity: Refers to the smoothness/slipperiness of one surface relative to another (ocular surface vs eyelids). We blink around 14,000 times per day and so the surfaces need to be able to glide over each other easily, without friction, to allow comfortable lens wear.
- Friction: The coefficient of friction is inversely correlated with contact lens comfort, and lower friction means better lubricity. When friction becomes an issue, it can lead to complications such as lid wiper epitheliopathy.
- Wettability: Refers to the degree of fluid distribution, coverage and maintenance over a contact lens. A smaller angle of contact allows better fluid distribution.
- Breathability: In order to avoid any metabolic complication, like corneal oedema, we want to offer more of those materials that are offering a high DK, to allow better oxygen transmissibility.
- All day comfort: We need to understand what the patient wants out of their contact lenses and help them to achieve comfortable wear during this time. However, patients also actively help to play a role in comfort, by being adherent to allow them to get the best out of their contact lenses.
- Stability: Stability of a contact lens can help with the vision. Referring back to the previous webinar on toric lenses, it is evident that superior vision will play a role in comfort, and where indicated, astigmatism of as low as 0.75DC should be offered a toric contact lens to optimise vision.
Considering all the aforementioned factors, and the need for a compromise between some of these factors, perhaps the best way to think about the ‘ideal contact lens’ is by considering what is ideal for that individual patient? No two patients are exactly the same, with the very same requirements and ocular environment.
Therefore, what may be the ideal lens for one patient, may in fact be the least desirable choice for another. Additionally, there may be a need for the patient to have a different lens for different activities, so that the ‘ideal’ lens is matched to the needs of each activity (for example, single vision daily disposables for running, but reusable multifocal lenses for work).
There are also a multitude of factors to consider when selecting the optimal lens for the patient. These include:
- Modality/desired wear times
- Allergies
- Pre-existing conditions
- Dry eye
- Meibomian gland dysfunction (MGD)
- Visual needs (astigmatism, presbyopia, keratoconus, high ametropia)
- Handling abilities/physical factors
- Age
- Environment
- Lifestyle/occupation/hobbies
Contact Lens Discomfort (CLD)
Contact lens discomfort is defined as follows: ‘Contact lens discomfort is a condition characterised by episodic or persistent adverse ocular sensations related to lens wear, either with or without visual disturbance, resulting from reduced compatibility between the contact lens and the ocular environment, which can lead to decreased wearing time and discontinuation of contact lens wear.’1
CLD is a very important issue for us as ECPs because we have up to 60% of symptomatic contact lens wearers, with peaks up to 90%. It appears from the evidence that soft contact lens materials have higher incidence rates of CLD compared to rigid corneal lenses. More frequently, such discomfort is reported from hydrogel materials rather than silicone hydrogels. CLD also appears more apparent in conventional silicone hydrogels compared to disposable silicone hydrogels. It is also reported more with toric lens wear than spherical lens wear.
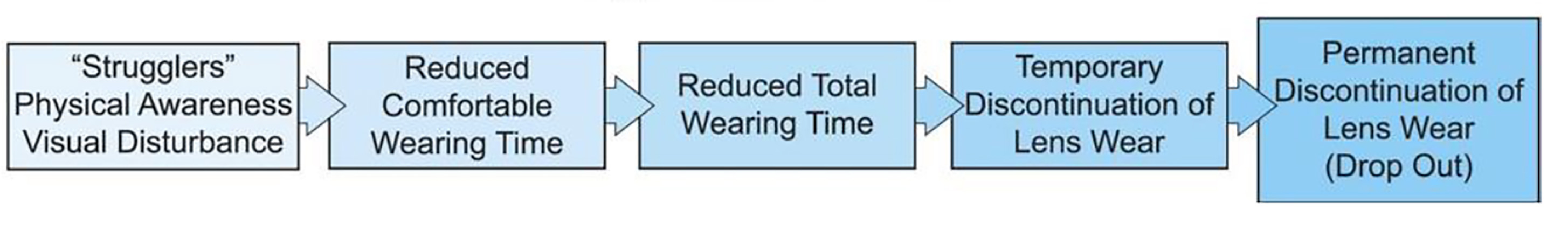
In terms of progression, CLD can be episodic and then turn into a persistent problem (figure 5). With persistence, the patient has a reduced comfortable wearing time and so reduces their total wear time of the lenses to compensate for this issue. This reduced wearing time can eventually lead to very rare contact lens use, and ultimately, discontinuation. Sometimes, we are unaware of these drop outs in our clinics until patients return for sight tests and the conversation around contact lenses is revisited.
Figure 5: Progression of contact lens discomfort
Risk Factors for CLD
The risk factors for CLD can be split into two typers:
- Contact lens-related factors
- Environmental factors
For the purposes of this review, we will only be focusing on the contact lens related risk factors.
Firstly, the choice of material can be a risk factor. Considering ocular surface interactions with different contact lens materials, on the whole, such interactions appear to be quite similar. The consideration should then be given to the lens surface and modulus. A surface with poor wettability and lubricity can contribute to CLD. A high modulus can also make the lens feel more rigid, and thus, lead to discomfort. As a result, during the last decade, the modulus of silicone hydrogel lenses has decreased significantly (1.400MPa to 0.025MPa).
The design of the contact lens can also play a role in CLD. Multifocal and toric lens designs appear to show higher incidence rates of CLD. The edge design is also another important factor to consider. Studies show that rounded edge designs offer less comfort due to a build-up of the conjunctiva at the edge of the lens.
The overall fit of the lens is also a factor to consider in CLD. The less mobile the lens on the eye, the better the comfort. Looser fitting promotes greater post-blink movement and smaller diameters reduce comfort. For monthly contact lenses, the findings are contradictory but switching to daily disposable lenses may be a beneficial solution.
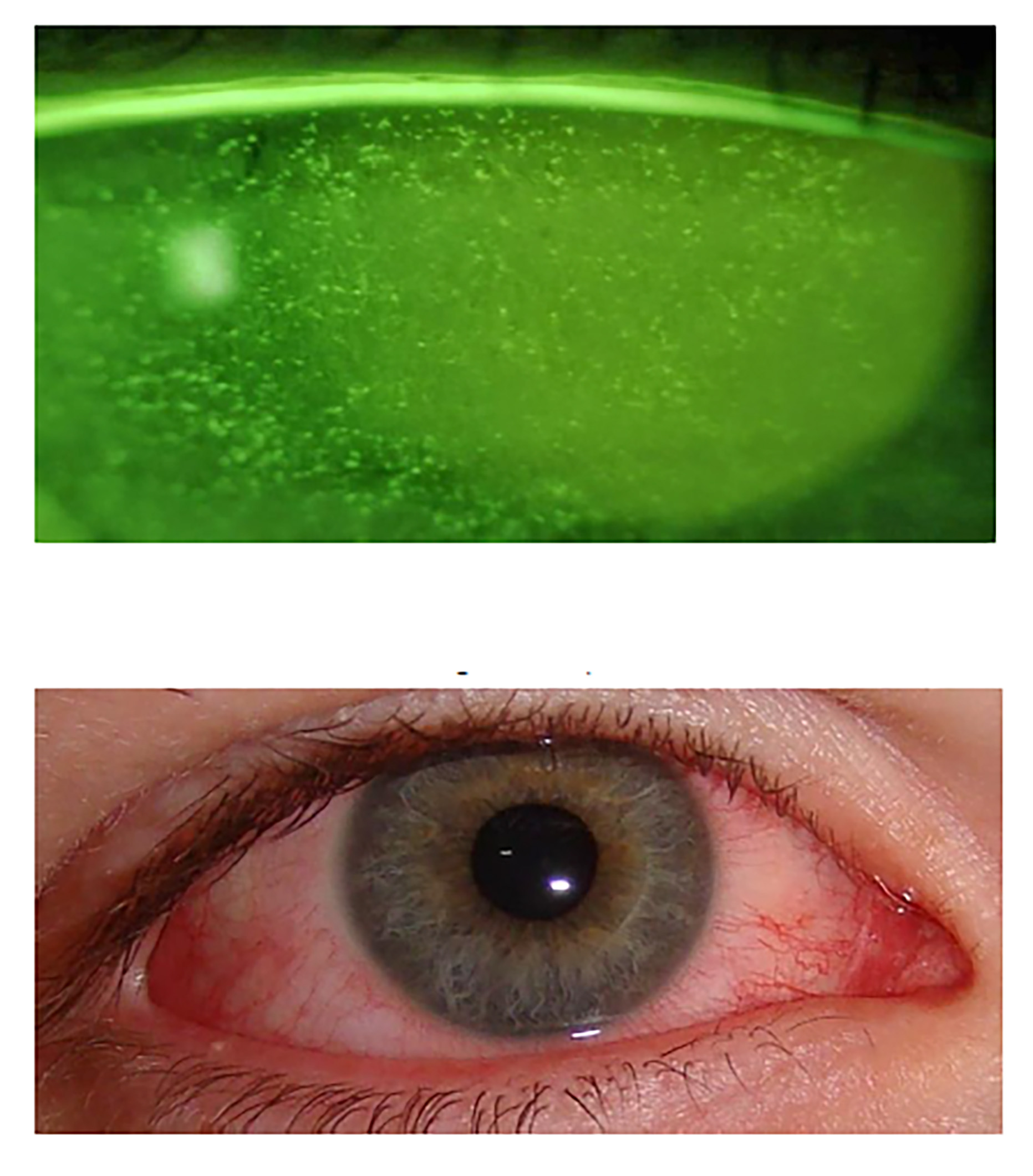
The lens care also needs to be taken into consideration. There is an obvious need to have safe, clean contact lenses. However, the cleaning solution can compromise the ocular surface (figure 6). There is some relation between PHMB-based contact lens maintenance solution and corneal staining, particularly with non-ionic, high water content hydrogel materials. There is also a risk to develop allergic interactions between contact lens deposits or the contact lens cleaning solution, and the ocular surface environment. For hydrogen-peroxide based cleaning solutions, the omission of the neutralising step can result in toxic keratopathy.
Figure 6: Solution-induced response due to use of a PHMB-base multipurpose solution; fluorescein staining (top) and diffuse hyperaemia (bottom)
- Dr Alberto Recchioni is a Research Fellow (optometry) at the University of Birmingham and Dr Sunayna Verma Mistry is Professional Education and Development Manager with Alcon.
- The next Alcon online event will take a look at dry eye disease and will be reviewed in the September Contact Lens Monthly.
- Alcon Talks in Optician Contact Lens Monthly 2023:
- March: Toric contact lenses
- June: Contact lens comfort
- September: Dry eye disease
- December: Multifocal contact lens options
References
- Willcox, MD, Argüeso, P, Georgiev, GA, Holopainen, JM, Laurie, GW, Millar, TJ, Papas, EB, Rolland, JP, Schmidt, TA, Stahl, U and Suarez, T, 2017. TFOS DEWS II tear film report. The ocular surface, 15(3), pp.366-403.
- King-Smith PE, Hinel EA, Nichols JJ. Application of a Novel Interferometric Method to Investigate the Relation between Lipid Layer Thickness and Tear Film Thinning. Investigative Ophthalmology and Visual Science. 2010;51(5):2418-23
