Many contact lens wearers with low to moderate astigmatism are left with a certain degree of astigmatism uncorrected despite the increasing improvements in soft toric lens manufacture. There are currently no reviews on whether soft toric contact lenses can provide better outcomes over soft spherical contact lenses in these individuals.
To assess the efficacy of soft toric lenses in comparison to soft spherical lenses for patients with low to moderate astigmatism (between -0.50 to -2.00DC), at the start of 2020, databases were searched for randomised trials comparing soft toric lenses to soft spherical lenses in subjects with low to moderate astigmatism. Primary outcomes included distance visual acuity, near visual acuity and contrast sensitivity. Secondary outcomes included participant reported outcomes, glare sensitivity, eye strain and lens fit details. The review follows the standard methodological procedures expected by the Cochrane Collaboration.
Astigmatism
Astigmatism is commonly defined as a refractive condition caused by meridional disparities in curvature, refractive index or alignment of the optical components of the eyes (more specifically the cornea and crystalline lens) along their principal meridians.1 In an astigmatic eye, incoming parallel light rays are focused at two distinct focal lines, which are generally perpendicular to one another.1
Likely causes of astigmatism include the following:
- Heredity2
- Eyelid morphology3
- Eyelid pressure4
- Extraocular muscle tension5
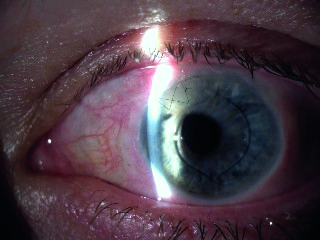
- Ocular surgery (figure 1)
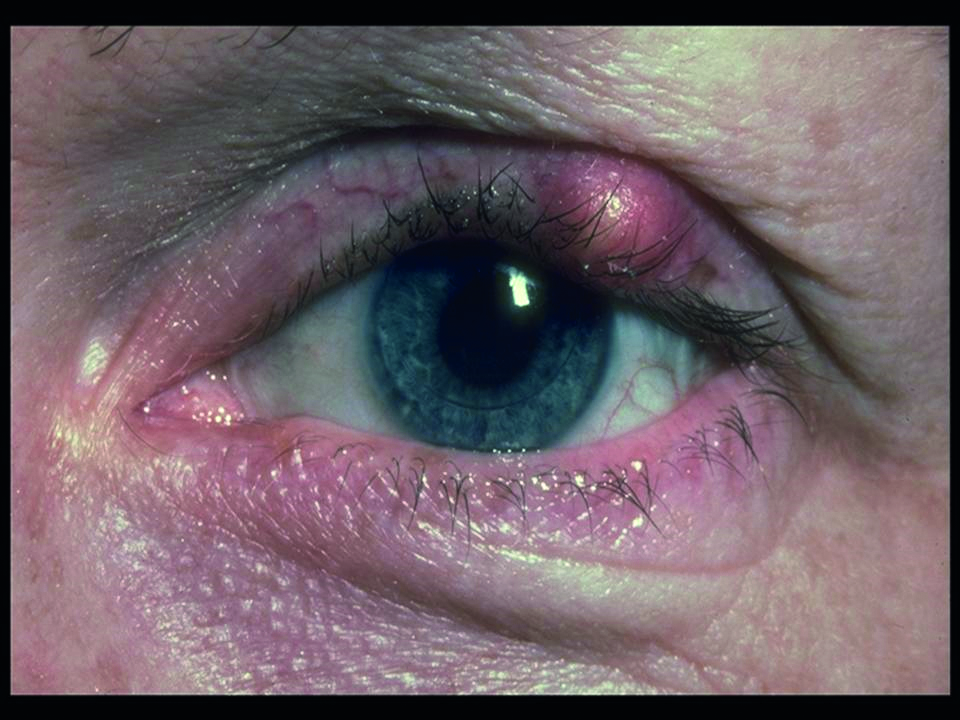
- Eye lid pathology3 (figure 2)
Since its discovery, several methods of correcting or treating astigmatism have developed. These include spectacles, toric contact lenses, laser eye surgery and refractive lens exchange.
Figure 1: Surgery can induce astigmatism
Prevalence of astigmatism
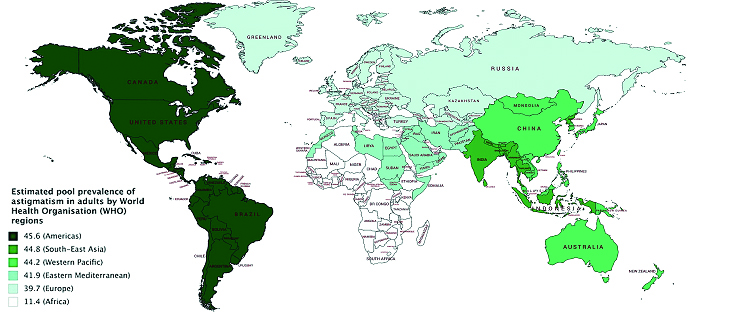
A review by Hashemi et al on the prevalence of refractive errors found that astigmatism is the most common refractive error among children and adults globally with 40.4% of adults having astigmatism ≥-0.50DC.6 Figure 3 demonstrates disparities in the estimated pool prevalence (EPP) of astigmatism between the WHO regions, with the highest EPP in the Americas (45.6%), and the lowest in Africa (11.4%). Closely behind, the Americas, South-east Asia and the Western Pacific follow with an EPP of 44.8% and 44.2% respectively.
Figure 2: A chalazion, an example of lid pathology that may induce astigmatism
Soft contact lenses
Soft contact lenses (SCLs) have become a fundamental method of correcting refractive errors, with around 125 million SCL wearers worldwide. Toric SCLs were developed in the 1970s,7 shortly after spherical SCLs were invented. During this time, many clinicians were required to be specialists in the soft toric lens field,8 as they were classed as difficult to fit due to problems with vision, comfort, rotation and manufacture.7, 9
Figure 3: Map showing estimated pool prevalence of astigmatism by World Health Organisation regions; adapted from Hashemi et al6
Conversely, toric SCLs have improved in design and production over the past 30 years making them easier to fit. This has been accompanied by an increase in toric SCL fits in the UK from 12 to 14% in the 1990s to 29% in 2008.9
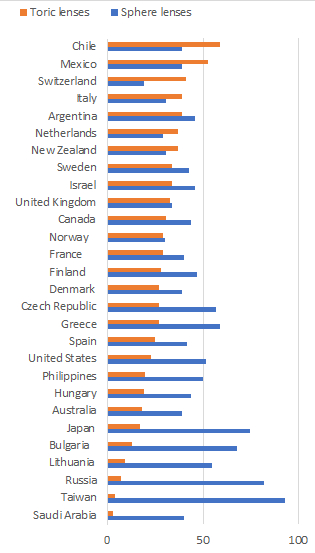
One UK study found around 47.4% of patients had clinically significant astigmatism (-0.75DC) in at least one eye and 24% in both eyes.10 In 2019, an international prescribing survey disclosed that only 32% of international SCL fits were toric lenses, with a slightly higher value of 33% in the UK (figure 4).11
Figure 4: Percentage of prescribed soft contact lenses that are sphere or toric for markets reporting greater than 100 soft lens fits in 201811
International prescribing patterns
Chile is the highest toric SCL prescriber, with 59% of prescribed fits being toric lenses (figure 4). This is 26% higher than the UK. Saudi Arabia prescribes the fewest toric contact lenses, with only 3% of prescribed lenses being toric. Saudi Arabia also prescribes a low number of spherical SCLs (40%), and this is attributable to a large majority of Saudi Arabia’s SCL prescriptions consisting of coloured lenses (55%). Taiwan is by far the highest sphere contact lens prescriber, with 93% of SCL prescriptions being sphere only, leaving only 4% of SCL prescribed as toric.11
Sphere or toric?
Soft sphere contact lenses are available in many different materials and they are obtainable in sphere-only powers for the correction of myopia and hyperopia. Soft toric lenses have been developed to correct the two meridional powers produced by astigmatism. The only problem with this is that SCLs have a tendency to rotate in the eye, which would be pointless in astigmatism error and has led to the development of stabilisation methods. Lenses are fitted using the spectacle prescription (back vertex adjusted where appropriate) and keratometry readings.
Design of systematic review
Astigmats are mostly over-represented among the soft contact lens dropouts and this is sometimes due to uncorrected astigmatism.10 Currently, there are no reviews on this topic and a systematic review is necessary to provide the best level of evidence to evaluate the effectiveness of toric and spherical SCLs in low to moderate astigmatism. The main aim of this systematic review is to appraise the current research on this topic and conclude whether toric SCLs are worth fitting over spherical SCLs in patients with low to moderate astigmatism.
Criteria for study inclusion
Types of studies
This review aimed to include randomised trials.
Types of participants
Trials to be included require participants who have low to moderate astigmatism ranging from -0.50DC to -2.00DC and are over the age of 18. Restrictions were not applied to gender or race.
Types of interventions
This review intended to included trials that compared any type of toric SCLs to spherical SCLs in either one or both eyes
Outcome measures
Primary outcome measures
- Distance and near visual acuities
- Contrast sensitivity
Secondary outcome measures
- Participant reported outcomes; including visual satisfaction, comfort of lenses and overall participant satisfaction.
- Any other important outcomes; these included glare, halos, and higher order aberrations
Adverse effects
This review aimed to state any adverse effects that had been reported in the studies.
Search methods
Electronic search
A literature search was conducted using the following databases:
- EBSCO Medline
- EBSCO CINAHL
- OVID Embase
- OVID AMED
- OVID Cochrane central register of controlled trials for related articles
The last database search took place on February 17, 2020. The following search terms were used in the EBSCO and OVID search: (‘astigmatism’ AND ‘toric’ AND ‘spherical’ AND ‘contact lenses’).
Other resources
The references published with the included articles were also searched for additional published articles not found within the literature search. There were no restrictions on language or the publication year.
Data collection and analysis
Selection of studies
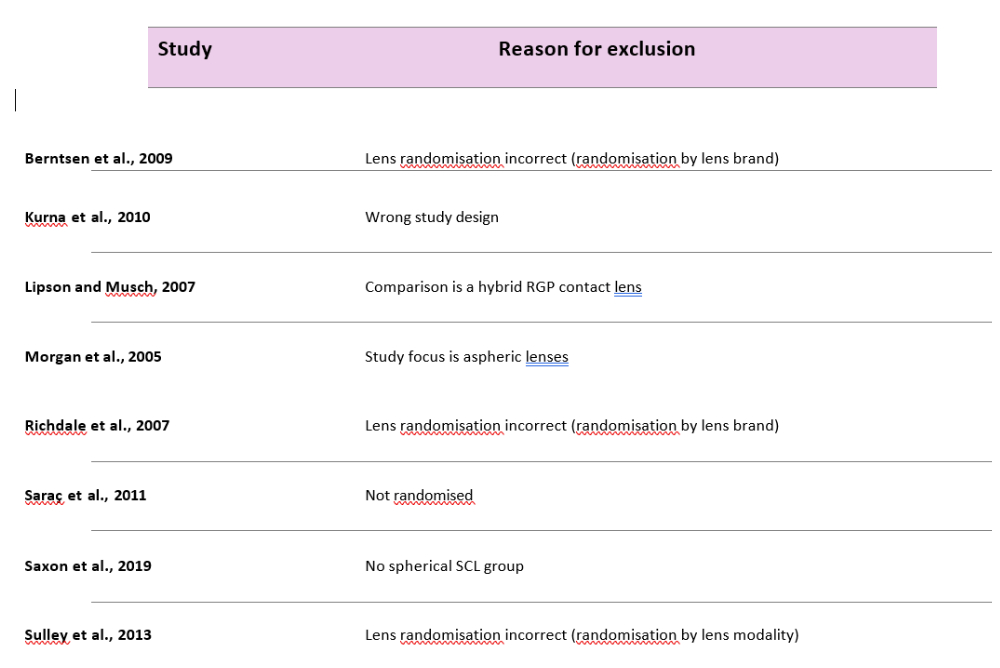
The abstracts and titles from the electronic search were independently screened by the author. Relevant full text article copies were retrieved and reasons for excluding articles at this phase were documented (table 2, below).
Data extraction and management
Covidence, a web-based software platform, was used to aid the production of this review and it was also used for data extraction. This data was then used in RevMan to conduct the data analysis.12
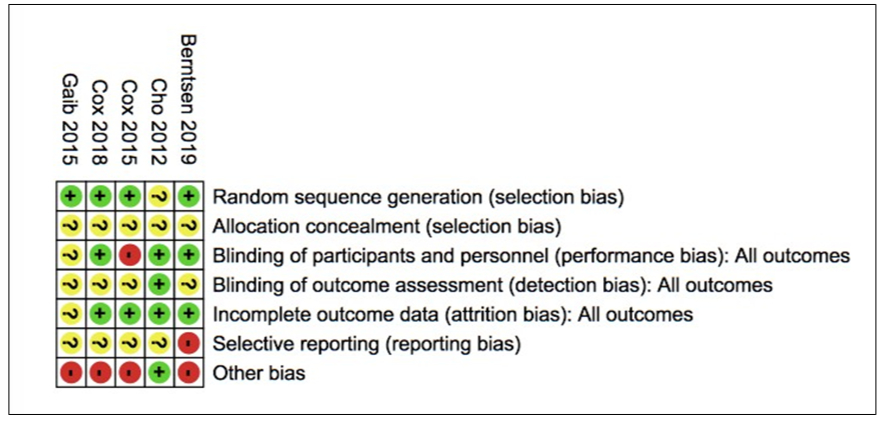
Assessment of risk of bias
This was undertaken using the Cochrane risk of bias tool. The Covidence inbuilt risk of bias tool was also used to assess the risk of bias of the studies and the risk of bias plots were produced in RevMan (figures 5 and 6).
Figure 5: Risk of bias graph representing the review author’s risk of bias judgements shown as a percentage across the included studies
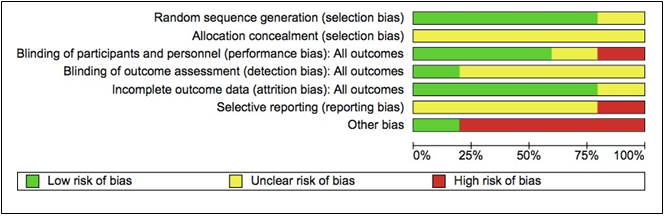
Figure 6: Risk of bias summary table representing the review author’s risk of bias judgements across the different domains for each individual study
Measurement of treatment effect
For continuous outcomes, the measure of the treatment effect was taken as the mean difference (MD) or standardised mean difference (SMD). The measurement of treatment effect for dichotomous outcomes was recorded as the risk ratio. All measurements of treatment effect included 95% confidence intervals.
Unit of analysis issues
This comparison could be applied to either one eye or both eyes and this has been indicated in the summary of characteristics. Where possible, this review has reported binocular results which better portray real visual performance.
Dealing with missing data
Missing data was recorded and assessed in the risk of bias ‘incomplete data’ domain (attrition bias) and any reasons behind the exclusions were documented in the characteristics of included studies table.
Assessment of heterogeneity
Heterogeneity was assessed in several ways, one of which was examining the direction and size of effects from forest plots. Heterogeneity was also assessed using the I2 statistic and values above 50% were considered as substantial heterogeneity.
Assessment of reporting bias
Funnel plots could not be presented in this study at this current time point as there are only a small number of studies included in this review.
Data synthesis
It was decided that the random effects model would be used in an analysis of three or more studies where appropriate. However, in studies of less than three, the fixed-effect model was used. In cases of substantial heterogeneity, it was decided that pooled data was not reported unless all the separate effect estimates were in favour of the same intervention.
Subgroup analysis and investigation of heterogeneity
Some studies (Berntsen et al, 2019 and Gaib and Vasudevan, 2015) recorded measurements at the fitting and again at a further follow-up. Appropriate subgroups were then collated and compared in RevMan.
Sensitivity analysis
This review did not include enough studies to conduct an appropriate sensitivity analysis. Additionally, only one study out of the five studies included was not rated as high risk for at least one of the risks of bias domains.
Results
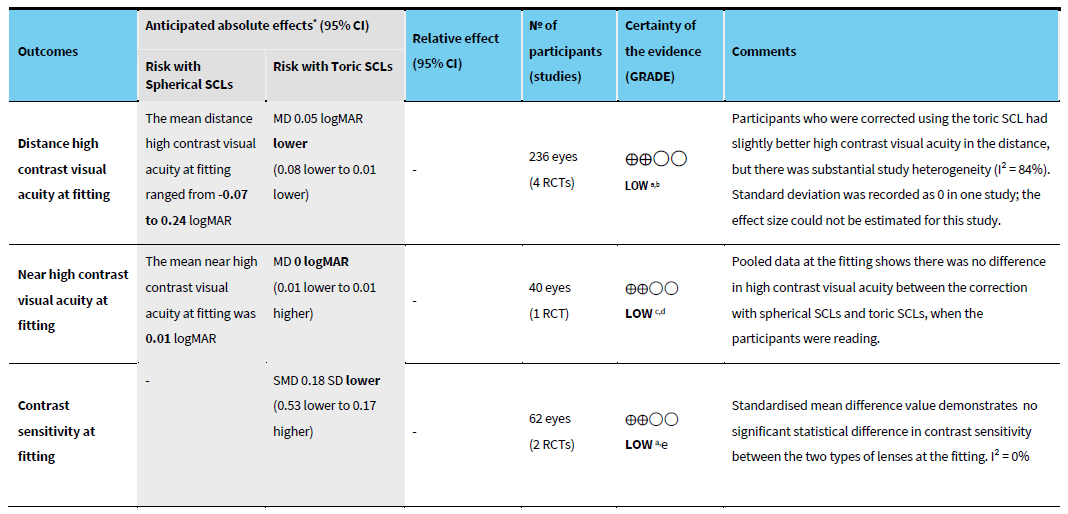
A summary of findings table (table 1) was created using the GRADEpro software and it provides the absolute and relative risks, as well as overall quality of the evidence for selected outcomes.
Table 1: Summary of results. *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI = Confidence interval; MD = Mean difference; SMD = Standardised mean difference; RR = Risk ratio; SCL = Soft contact lens
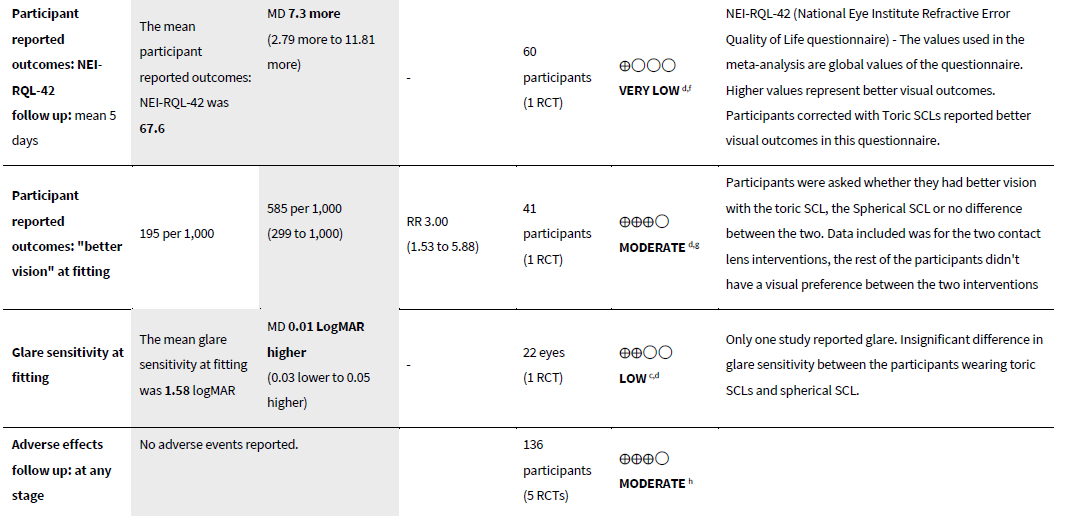
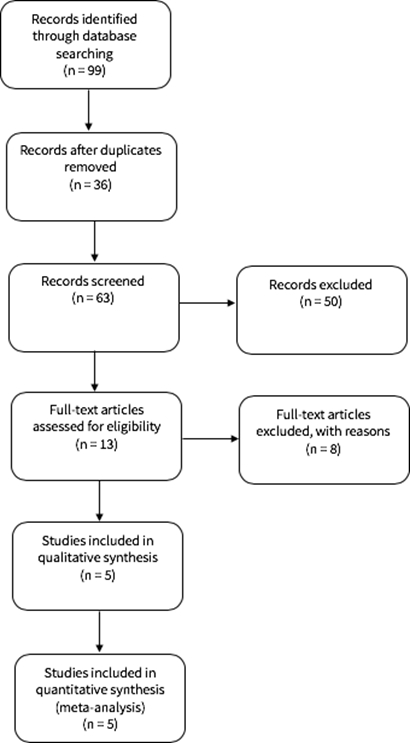
Electronic searches generated 99 articles (figure 7). Duplicated records were removed leaving 63 records to screen, of which 50 unrelated articles were excluded. Full text articles were obtained from 13 studies for further inspection, of which eight studies were excluded with reasons (see characteristics of excluded studies). The remaining five studies were included in this review for data synthesis.
Figure 7: Study flow diagram
Types of participants
In total, the five studies included 236 eyes of 136 participants with an age range between 19 and 40 years old. The majority of studies included habitual soft contact lens wearers only (Cox et al, 2015; Cox et al, 2018; Berntsen et al, 2019; Gaib and Vasudevan, 2015) and excluded any participants with presbyopia, ocular abnormalities, ocular infections and previous ocular surgeries. Astigmatism ranged between -0.75 to -2.00 with one study including astigmatism as low as -0.50DC (Gaib and Vasudevan, 2015. Refractive error ranged from +1.25 to -6.00 across the studies.
Interventions
All five studies compared toric SCLs to Spherical SCLs using a variety of branded lenses. Only one out of the five studies included monthly lenses (Gaib and Vasudevan, 2015), the rest were daily lenses:
- Cho et al, 2011: Bausch + Lomb for astigmatism Softlens vs Bausch + Lomb Softlens (spherical)
- Cox et al, 2015: Acuvue Moist for Astigmatism vs Acuvue moist (spherical)
- Cox et al, 2018 & Berntsen et al., 2019: Acuvue moist for astigmatism vs Acuvue moist (spherical)
- Gaib and Vasudevan, 2015: Intelliwave Aspheric toric SCL vs Air Optix aqua (Spherical)
Types of outcomes
The majority of the five studies reported high and low contrast visual acuity. The only one that did not report this outcome was Cox et al, 2018 but, as mentioned before, this study is linked to Berntsen et al, 2019, which did report these outcomes. High contrast visual acuity (HCVA) is usually measured with black letters on a white background (or vice versa), whereas low contrast visual acuity (LCVA) is measured with low contrast letters on a white background.
Low contrast visual acuity detects visual loss which is not captured in high contrast visual acuity methods.13 Berntsen et al, 2019 and Gaib and Vasudevan, 2015 reported these outcomes at fitting and follow up (follow up ranged from six hours to five days). Gaib and Vasudevan, 2015 was the only study that reported near high and low contrast visual acuities.
Contrast sensitivity was reported by two studies (Cox et al, 2015; Gaib and Vasudevan, 2015) but methods of measuring contrast sensitivity were very distinct. Cox et al, 2015 presented participants with 10 sets of three 1.84 logMAR letters and the contrast of those letters was decreased until at least two of the three letters could be read. Gaib and Vasudevan, 2015 measured contrast sensitivity using the CSV-1000 at four different spatial frequencies (3, 6, 12, 18). Contrast sensitivity for these two studies was combined by converting the logMAR letters used in Cox et al, 2015 into cycles per degree and pooling this data with results of a similar spatial frequency from Cox et al, 2015.
Standardised mean differences were used to pool these results due to these distinct methods of measuring contrast sensitivity. Participant reported outcomes were described across the studies but in a variety of forms. Questionnaires were used in Cho et al, 2011 to report whether participants felt the vision and comfort were ‘better’ in the toric or spherical lens (or no different). Gaib and Vasudevan, 2015 reported the participant’s subjective rating of vision of each lens type, on a scale of 1 to 10 (1 = worst, 10 = best). Cox et al, 2018 described the results of two types of questionnaires; National Eye Institute Refractive Error Quality of Life Instrument (NEI-RQL-42) and Convergence Insufficiency Symptom Survey (CISS). Higher values are considered as better for NEI-RQL-42 and lower values are considered as better for CISS.
Glare sensitivity was reported by Cox et al, 2015. Eye strain was measured using electromyography in Berntsen et al, 2019. The right eye of each participant was measured using electromyography techniques. These measurements translate as orbicularis oculi activity (or, more simply, eye strain). Other outcomes, such as lens fitting times, fitting success rates, and number of lenses required to fit each lens types, were reported by Cox et al, 2018.
The studies excluded from the review are listed in table 2, along with the reason for exclusion.
Allocation
Allocation was reported as unclear for all the studies. The majority of the studies did not report or describe any type of allocation concealment. However, Berntsen et al, 2019 and Cox et al, 2018 (linked studies) reported concealing methods such as packaging but did not go into further details. Therefore, these studies were reported as unclear risk.
Masking (performance and detection bias) and blinding
Blinding of participants was more prominent than blinding of outcome assessors across the studies. Three out of the five studies were reported as low performance bias (Berntsen et al, 2019; Cho et al, 2011: Cox et al, 2018). Cox et al, 2015 was reported as a high risk of performance bias as it was a single masked study and only particular outcome assessors were masked. Gaib and Vasudevan, 2015 was reported as unclear risk of performance bias as there was no reporting of participant masking. Only one study had a low risk of detection bias (Cho et al, 2011), the rest were unclear due to very poor masking/ blinding or no reporting.
Incomplete outcome data
Four out of five studies were assessed as having low attrition bias as all the participants that were included completed the trial. Gaib and Vasudevan, 2015 was graded as unclear attrition bias due to insufficient information on incomplete data.
Selective reporting
Reporting bias was graded as unclear in four out of five studies as trial registries or protocols were unavailable. Berntsen et al, 2019 had a trial registry, which had the same clinical trial registry ID as Cox et al, 2018. Berntsen et al, 2019 was reported as high risk of selective reporting as it reported eye strain as a secondary outcome; but the protocol listed this outcome as primary.
The re-ranking of outcomes carries a high risk of reporting bias. Cox et al, 2018 was graded as unclear risk of reporting bias as all the protocol outcomes were reported but some outcomes included in Cox et al, 2018 (such as the time required to fit lenses) were not included in the protocol. This is a minor source of selective reporting, which is why this study was reported as unclear. Although Cox et al, 2018 and Berntsen et al, 2019 originate from the same protocol, differences in the way these articles have been reported has led to separate risk of bias assessments.
Primary outcomes
Distance visual acuity
Four studies reported distance visual acuity (Cho et al, 2011; Berntsen et al, 2019; Gaib and Vasudevan, 2015; Cox et al, 2015). The majority of these studies measured distance visual acuity as high and low contrast visual acuity. Two studies measured visual acuity at fitting and at follow-up appointments (Berntsen et al, 2019 and Gaib and Vasudevan, 2015) and these results were presented as a separate sub-group (160 eyes in each intervention group).
Analysis of pooled data from four trials (Berntsen et al, 2019; Cho et al, 2011; Cox et al, 2015; Gaib and Vasudevan, 2015) reported an improvement HCDVA with toric lenses in comparison to spherical lenses at the fitting (MD -0.05 logMAR 95% CI -0.08, -0.01, 236 eyes in each intervention group). However, there was substantial heterogeneity (I2= 84%). At the follow up, the results are almost parallel to the fitting results as the MD was -0.05 logMAR (95% CI -0.09, -0.01). As before, there was substantial heterogeneity (I2= 83%), with very little CI overlap of the two studies. Nevertheless, the consensus from both subgroups is that toric lenses were favoured.
Analysis showed pooled results for LCDVA with three studies reporting results at the fitting (Berntsen et al, 2019; Gaib and Vasudevan, 2015; Cho et al, 2011; 214 eyes in each intervention group) and two of these studies further reporting results at the follow up (Berntsen et al, 2019 and Gaib and Vasudevan, 2015; 160 eyes in each intervention group). At the fitting and follow up, toric lenses were favoured (fitting MD -0.08 95% CI -0.10, - 0.06: Follow up MD -0.10 95% CI -0.12, -0.07). Heterogeneity was lower for LCDVA values than HCDVA, with I2 of 41% and 56% at the fitting and follow-up respectively.
Near visual acuity
Only one study reported this outcome (Gaib and Vasudevan, 2015; 40 eyes in each intervention group) and data was reported for the fitting and the follow-up six hours later. Gaib and Vasudevan, 2015 reported no difference in HCNVA at the fitting between the two interventions (MD 0 95% CI -0.01, 0.01). The follow-up results show a small improvement in HCNVA with toric SCLs (MD -0.01 95% CI -0.01, 0.00). Gaib and Vasudevan, 2015 also reported the LCNVA at the fitting (MD 0.00 95% CI -0.04, 0.04) and at the follow-up (0.00 MD 95% CI -0.04, 0.04). These results again show no difference between the two lens types and are exactly the same at the fitting and follow-up.
Contrast sensitivity
Contrast sensitivity was reported by two studies (Cox et al, 2015 and Gaib and Vasudevan, 2015) and the number of eyes included in total was 62 in each intervention. At the fitting, the standard mean difference (Std MD) was -0.18 Log CS (95% CI -0.53, 0.17). Gaib and Vasudevan, 2015 reported contrast sensitivity at the follow-up (six hours later) and a Std MD value of -0.11 [-0.55, 0.33] was calculated. The pooled result from this analysis shows that, although studies favoured the spherical SCL, there was no significant statistical difference in contrast sensitivity between the two types of lenses at both the fitting and follow-up. Heterogeneity calculated for the contrast sensitivity at the fitting was 0%.
Secondary outcomes
Participant reported outcomes: Visual and comfort preference
This was reported by Cho et al, 2011 and included 41 participants. Participants were asked to report whether they had better vision with the toric SCL, spherical SCL or no difference between the two. Overall, the participants preferred the toric SCL (RR 3.00, 95% CI 1.53, 5.88). The same study also reported whether participants preferred the comfort with the toric or spherical SCL, on insertion and 10 minutes after. Although the spherical lenses were preferred overall, there was no significant evidence for this preference in both subgroups (RR 0.64, 95% CI 0.27, 1.48) and 10 minutes later (RR 0.70, 95% CI 0.30, 1.66).
Participant reported outcomes: NEI-RQL-42 and CISS questionnaires
These questionnaires were carried out by Cox et al, 2018 and included 60 participants. Higher values are better for the NEI- RQL-42 and lower values are better for CISS. Global values were used for the NEI-RQL-42 questionnaire. Analysis demonstrated good outcomes when participants wore toric SCL (MD 7.30, 95% CI 2.79, 11.81). The CISS questionnaire revealed there is no evidence of significant differences between the two interventions (MD -2.20 95%CI -5.31, 0.91).
Participant reported outcomes: subjective rating of vision
This outcome was reported by Gaib and Vasudevan, 2015 and included 24 participants. Participants included were required to rate their vision for both interventions on a scale of 1 to 10 (1 = worst vision, 10 = best vision). No standard deviation values were included in the study and appropriate statistical analysis could not be carried out. However, the study reported a p-value >0.05, demonstrating no significant statistical difference between the two groups.
Electromyography: Eye strain
Berntsen et al, 2019 reported eye strain in 60 participants at the fitting and the follow-up. At the fitting, there was less eye strain with the toric lenses in comparison to the spherical lenses (MD -0.07, 95% CI -0.13, 0.00). However, at the follow up, there were no significant differences between toric and spherical SCLs (MD -0.04, 95% CI -0.10, 0.02).
Glare sensitivity
This outcome was reported by Cox et al, 2015 and included 11 participants. Mean difference value showed no significant difference in glare sensitivity across the two interventions (MD 0.01 95% CI -0.03, 0.05).
Lens fit details
Details of the lens fits were discussed in Cox et al, 2018. The success rate of fits is described as attaining an over refraction of plano in both eyes. Success rates were higher in those wearing toric SCLs in comparison to spherical SCLs (% difference = 5%). However, time required to fit lens (MD 1.20, 95% CI, -0.19, 2.59) and average number of contact lenses (MD 0.00, 95% CI -0.12, 0.12) required to fit SCL demonstrated no significant statistical differences between the groups.
Adverse effects
None of the studies reported any adverse effects.
Discussion
The results are summarised in table 1.
This review included five studies that included 136 participants (236 eyes). Four studies took place in the US and one study took place in China. Astigmatism ranged between -0.50DC to -2.00 DC and mostly included habitual contact lens wearers.
Participants ranged in age from 19 to 40 years old. Lens types were quite similar, with three studies using Acuvue moist lenses (Berntsen et al, 2019; Cox et al, 2018; Cox et al, 2015).
There is some evidence that toric SCLs can provide better distance visual outcomes in comparison to spherical SCLs. Distance high contrast visual acuity was shown to be slightly better in toric lenses, with an even higher improvement with low contrast acuity measurements. Results were almost equivalent at the follow-up. However, there were no significant differences found in HCNVA between the two lens types at the fitting, but there was a slight improvement with the toric SCLs at the follow up. Contrast and glare sensitivity measurements also showed no difference between the two lens types.
Participant reported outcomes were reported very differently across the studies and could not be analysed together. Overall, the visual preference of the participants tended to be the toric lenses and only one study reported no difference between the two-lens type when reporting subjective rating (Gaib and Vasudevan, 2015).
Participant reported comfort was only discussed by one study, which presented no significant differences between the two lenses at both insertion of the lens and 10 minutes later (Cho et al, 2011). The CISS questionnaire, carried out by Cox et al, 2018 revealed no significant differences in convergence insufficiency symptoms between the two lens types.
Eye strain was an interesting outcome investigated by Berntsen et al, 2019. Results at the fitting described higher eye strain with spherical lenses in comparison to toric lenses, whereas there were no significant differences found at the follow up. Lens fitting details did not demonstrate statistically significant findings between toric and spherical lenses.
Overall completeness and applicability of evidence
The evidence for this comparison cannot be considered as complete due to the small number of studies included and the majority of them were carried out in the US. This makes it difficult to apply the results of this study to different settings and countries. Although trial data was reported for every outcome, the majority of the analyses conducted were on single studies; which further questions the applicability of these outcomes. However, a majority of the main outcomes (distance visual acuity and contrast sensitivity) included at least two studies, which adds to their significance in comparison to other outcomes.
Quality of evidence
Quality of evidence is reviewed is the summary of findings table. All outcomes were downgraded due to risk of bias included within the studies.
Outcomes ranged in grading from low to moderate certainty, with most of the studies graded as low certainty. This means there is low certainty that the effect estimates are the actual true effect and further research may show different estimates of the true effect. Studies which only included one study were downgraded from imprecision. Only one outcome (distance high contrast visual acuity at fitting) was downgraded for high heterogeneity.
Potential bias in the review process
All the studies included in this review were crossover randomised trials, which can be problematic when incorporating into a review. This review evaluated the results of the studies as a parallel group trial in order to generate meaningful analyses. However, this can give rise to unit of analysis error causing some studies to be underweighted. Crossover trials also tend to include the carry over effect, which was not considered to be an issue in this review due to the type of intervention used. Where possible, binocular results were included, but results from Cox et al, 2015 did not implicitly state that results were binocular. In this case results were assumed to be binocular as the study had an interest in driving performance visual outcomes.
Agreements and disagreements with other studies or reviews
There are currently no reviews on the current subject according to the last electronic search. There have been a few studies that have directly compared toric and spherical SCLs. These include:
- Dabkowski et al;14 this non-randomised study compared visual acuity in participants wearing Durasoft (Ciba vision) toric and spherical soft contact lenses. Participants had astigmatism raging from -0.75 to -1.25. There was an improvement in visual acuity when participants were corrected with toric lenses and 71% of participants also had a subjective preference for the toric soft lenses over the spherical. Dabkowski et al found no difference in the contrast sensitivity between the two interventions. This study presents results very similar to this review.
- Richdale;7 Richdale and colleagues compared the visual acuity of participants with astigmatism ranging from -0.75- 2.00DC in a number of different lenses. They found that participants with low astigmatism gained 3.5 to 5 letters when wearing toric soft lenses in comparison to spherical soft lenses. They also found that participants with moderate astigmatism gained even more letters (8 to 12.5 letters) with the toric lenses in comparison to the spherical lenses. This study is in agreement with this review, although the improvement with toric lenses was substantially higher in Richdale.
Author conclusions
Implications for practice
This review highlights the subtle improvements with toric SCLs over spherical SCLs in distance visual performance, participant reported visual outcomes and eye strain, of participants with low-moderate astigmatism. This review also highlights the developments in soft toric lens manufacture, which has led to lenses that are easier to fit and better visual performance in comparison to years ago.
This review concludes that toric SCLs are recommended in individuals with low-moderate astigmatism as analyses have shown that toric SCLs are more likely to provide more benefits over spherical SCLs. Due to high heterogeneity, risk of bias and unit of analysis of some of the outcomes, results should be interpreted with some caution. Results from this review should be used to supplement current clinical fitting practices as well as patient preferences.
Implications for research
Further research is required for a more conclusive comparison of toric and spherical SCLs. There are no studies that investigate the long-term comparison of these lenses, which is important in fully understanding participant reported outcomes. Future trials would benefit from being more standardised by including a fundamental set of outcomes to ensure precise data pooling, which will lead to meaningful conclusions. There also needs to be a wide range of lens brands and types investigated so that evaluations can be more applicable.
- Danya Lahmami finished her prizewinning dissertation when she was a final year undergraduate at City University, London. She is now a resident optometrist working at Specsavers in West Thurrock, Essex.
- The author would like to thank Professor John Lawrenson for providing great support and guidance during the development of this review.
References
Studies included in this review:
- Berntsen, D., Cox, S., Bickle, K., Mathew, J., Powell, D., Seidman, S., Little, B., Lorenz, K. and Nichols, J., 2019. A randomized trial to evaluate the effect of toric versus spherical contact lenses on vision and eyestrain. Eye & Contact Lens: Science & Clinical Practice, 45(1), pp.28-33.
- Cho, P., Cheung, S. and Charm, J., 2011. Visual outcome of Soflens Daily Disposable and Soflens Daily Disposable for Astigmatism in subjects with low astigmatism. Clinical and Experimental Optometry, 95(1), pp.43-47.
- Cox, D., Banton, T., Record, S., Grabman, J. and Hawkins, R., 2015. Does correcting astigmatism with toric lenses improve driving performance? Optometry and Vision Science, 92(4), pp.404-411.
- Cox, S., Berntsen, D., Bickle, K., Mathew, J., Powell, D., Little, B., Lorenz, K. and Nichols, J., 2018. Efficacy of toric contact lenses in fitting and patient-reported outcomes in contact lens wearers. Eye & Contact Lens: Science & Clinical Practice, 44, pp.S296-S299.
- Gaib, S. and Vasudevan, B., 2015. Low toric soft contact lens acceptance study. Contact Lens and Anterior Eye, 38(3), pp.194- 198.
Studies excluded from this review:
- Berntsen, D., Merchea, M., Richdale, K., Mack, C. and Barr, J., 2009. Higher-order aberrations when wearing sphere and toric soft contact lenses. Optometry and Vision Science, 86(2), pp.115-122.
- Kurna, A and Şengör Tomris, 2010. Success rates in the correction of astigmatism with toric and spherical soft contact lens fittings. Clinical Ophthalmology, p.959.
- Lipson, M. and Musch, D., 2007. Synergeyes versus soft toric lenses: vision-related quality of life. Optometry and Vision Science, 84(7), pp.593-597.
- Morgan, P., Efron, S., Efron, N. and Hill, E., 2005. Inefficacy of aspheric soft contact lenses for the correction of low levels of astigmatism. Optometry and Vision Science, 82(9), pp.823- 828.
- Richdale, K., Berntsen, D., Mack, C., Merchea, M. And Barr, J., 2007. Visual acuity with spherical and toric soft contact lenses in low- to moderate-astigmatic eyes. Optometry and Vision Science, 84(10), pp.969-975.
- Saraç, Ö., Gürdal, C., Bilkay, H., Gökmen, S., Takmaz, T. and Can, İ., 2011. Effects of toric and soft spherical contact lenses on visual performance and wavefront aberrations in patients with low levels of astigmatism. Türk Oftalmoloji Dergisi, 41(1), pp.22-25.
- Saxon, J., Rah, M. and Reindel, W., 2019. Satisfaction of astigmatic patients with toric nesofilcon A contact lenses. Clinical Optometry, Volume 11, pp.1-10.
- Sulley, A., Young, G., Lorenz, K. and Hunt, C., 2013. Clinical evaluation of fitting toric soft contact lenses to current non- users. Ophthalmic and Physiological Optics, 33(2), pp.94-103.
General References
- Read, S., Vincent, S. and Collins, M., 2014. The visual and functional impacts of astigmatism and its clinical management. Ophthalmic and Physiological Optics, 34(3), pp.267-294
- Wixson, RJ., 1965. Refraction pedigrees. 2. The cornea. American Journal of Optometry, 1965;42(10):615–618
- Read, S., Collins, M. and Carney, L., 2007. A review of astigmatism and its possible genesis. Clinical and Experimental Optometry, 90(1), pp.5-19
- Gwiazda, J., Scheiman, M., Mohindra, I., Held, R. 1984. Astigmatism in children: changes in axis and amount from birth to six years. Investigative Ophthalmology & Vision Science. 1984;25(1):88–92
- Rowland, H. and Sayles, N., 1985. Photokeratometric and photorefractive measurements of astigmatism in infants and young children. Vision Research, 25(1), pp.73-81
- Hashemi, H., Fotouhi, A., Yekta, A., Pakzad, R., Ostadimoghaddam, H. and Khabazkhoob, M., 2018. Global and regional estimates of prevalence of refractive errors: Systematic review and meta-analysis. Journal of Current Ophthalmology, 30(1), pp.3-22
- Richdale, K., Berntsen, D., Mack, C., Merchea, M. And Barr, J., 2007. Visual acuity with spherical and toric soft contact lenses in low- to moderate-astigmatic eyes. Optometry and Vision Science, 84(10), pp.969-975
- Sulley, A., and Young, G. Soft torics; first choice for your astigmatic patients. Optician, 2011, 242; 6327: 24-30
- Morgan, P. and Efron, N., 2009. Prescribing soft contact lenses for astigmatism. Contact Lens and Anterior Eye, 32(2), pp.97-98
- Young, G., Sulley, A. and Hunt, C., 2011. Prevalence of astigmatism in relation to soft contact lens fitting. Eye & Contact Lens: Science & Clinical Practice, 37(1), pp.20-25
- Morgan, P. B., Woods, C. A., Tranoudis, I. O., Efron, N., Jones, L., Aighamdi, W., et al. (2019). International contact lens prescribing in 2018. Contact Lens Spectrum, 34(1), 26–32
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014
- Balcer, L., Raynowska, J., Nolan, R., Galetta, S., Kapoor, R., Benedict, R., Phillips, G., LaRocca, N., Hudson, L. and Rudick, R., 2017. Validity of low-contrast letter acuity as a visual performance outcome measure for multiple sclerosis. Multiple Sclerosis Journal, 23(5), pp.734-747
- Dabkowski, J., Roach, M. and Begley, C., 1992. Soft toric versus spherical contact lenses in myopes with low astigmatism. International Contact Lens Clinic, 19(11-12), pp.252-256
