Cerebral visual impairment (CVI) is one of the leading causes of visual impairment (VI) in the paediatric population in Western countries.1, 2 The increase of CVI is thought to be related to the higher survival rate of pre-term children.3, 4 This complex condition leads to visual dysfunction, affecting what a child can see and how they use their vision effectively for learning and development. Early intervention is essential in order to compensate for their visual dysfunction.5, 6
However, it appears that many children with CVI are living with this condition without this being identified.7, 8 This is, in part, due to unfamiliarity with the condition among healthcare and education professionals.9
Due to the complex nature of this condition, it can be difficult and daunting for professionals to engage with it. This article provides an overview of what is understood about CVI as well as its prevalence. Subsequent articles will cover the impact of CVI on learning and development, how it is diagnosed and managed and what the impact is of timely interventions.
Definition of CVI
Some authors assume a diagnosis of CVI by exclusion, whereby CVI is considered if the visual problems cannot be explained by ocular or anterior pathway pathology (for example, Sakki et al10). Others prefer a diagnosis founded on conceptual inclusion, based on ‘functional visual processing, rather than anatomical landmarks.’11 Lueck and Dutton12 provide the following definition, which will be used to describe CVI in this article and the remaining in the series:
“CVI is a term that describes deficiency in the functions of vision, due to damage or malfunction of visual pathways and visual centres in the brain (specifically those behind the lateral geniculate bodies), including the optic radiations, the occipital cortex and the visual associative areas, which may be accentuated by associated disorders of the control of eye movements.”
Visual pathways
The process of ‘seeing’ commences with visual input through our eyes. The visual information is processed at different stages, including the retina and optic nerves, before it reaches the occipital cortex for basic processing of information about visual fields, visual acuity, contrast sensitivity, colour vision and movement.4
However, in order to make sense of the visual world, further processing is required. The two main visual processing pathways are the ventral and the dorsal stream, also referred to as the ‘what’ and the ‘where’ pathways or networks (figure 1).13 These networks are inter-linked to create a holistic visual representation of the environment. The ventral stream network runs from the occipital lobe to the temporal lobe and is primarily responsible for recognition. It contains the ‘visual library’ for faces, places and objects.14
Figure 1: Ventral and dorsal streams
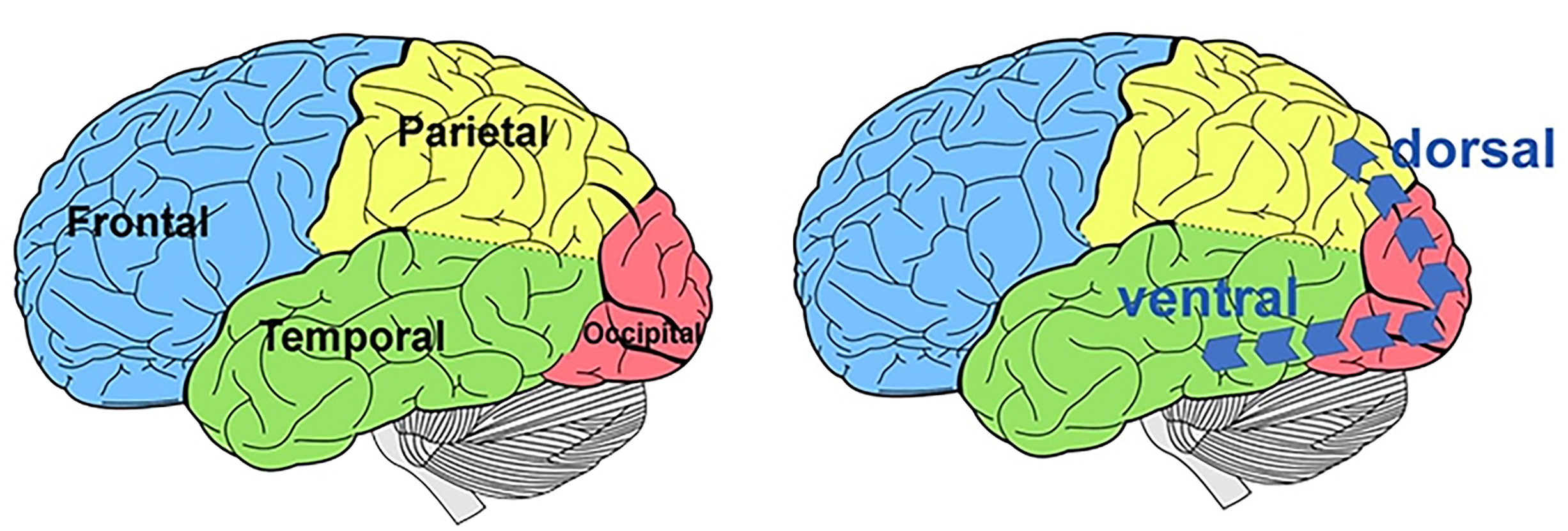
The dorsal stream network refers to the pathway from the occipital lobe to the parietal lobe and is responsible for spatial orientation, visually guided reach and attention.4 It provides a real-time representation of the visual surroundings.14
Visual dysfunctions in CVI
In ventral stream dysfunction, the ‘visual library’ is incomplete. This results in impairment of instant recognition of objects, faces and places. When a person is confronted with a real-time image, a match cannot be found with a stored image in the ‘visual library’ and the image is not recognised.4
Dorsal stream dysfunction hinders the automatic mapping of our surroundings, which can lead to anxiety and stress in busy and unfamiliar places.15 Children typically find it more difficult to function in cluttered or crowded environments and may experience ‘melt-downs’. Other children avoid these environments or withdraw.16
Table 1 provides an overview of common ventral and dorsal dysfunctions.
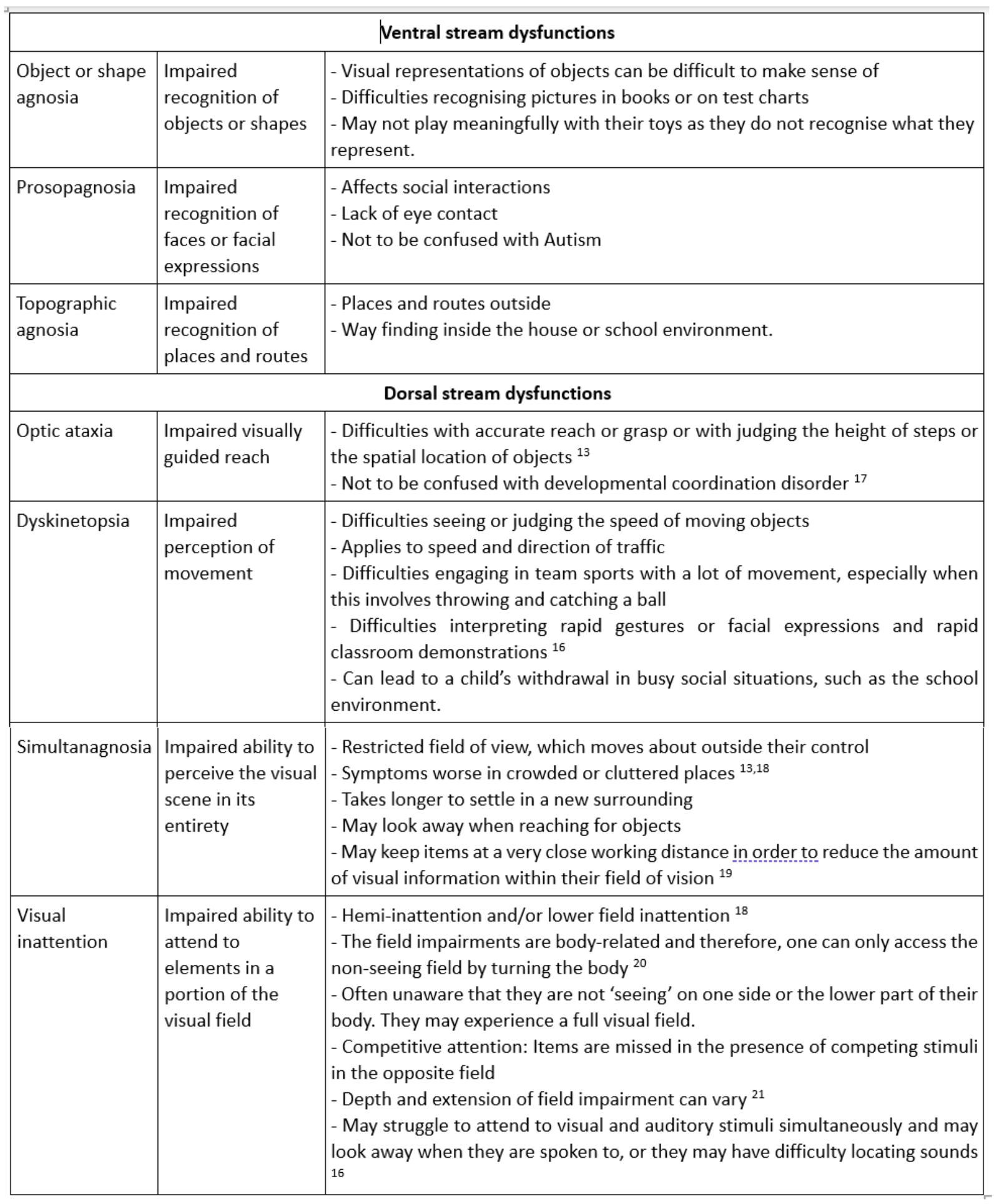
Figure 2 shows a representation of competitive attention and figure 3 shows a lower field impairment.
Figure 2: Competitive inattention. (a) Normal view. (b) Left side missing. (c) Right side missing

Figure 3: (a) Normal view. (b) View with lower field loss

Visual behaviours
It is common for children with CVI to display different behavioural features, depending on the specific underlying visual dysfunction. In some cases, children are given behavioural labels, such as autistic spectrum disorder (ASD) or attention deficit hyper-activity disorder (ADHD). The underlying cause of the behaviours and perceived difficulties is not always identified in these children, despite the fact that brain networks and functions in the visual area of the brain are often involved in these conditions.22-25
It is important to consider the inter-relationship between ASD, intellectual disability and CVI and to understand the mechanisms underpinning certain behaviours, so that appropriate adaptive strategies can be offered.26-30 Sonksen and Dale linked the development of social, language and motor skills with vision in early childhood.31 Lueck and Dutton explain that a number of behavioural characteristics in ADHD, dyslexia and ASD overlap with those of CVI.12
For example, difficulties in sustaining attention are a feature of ADHD, but can also be a result of dorsal stream dysfunction, visual field defects, simultanagnosia or visual fatigue.12 Poor spelling is a feature of dyslexia, but can also be due to simultanagnosia, dorsal stream dysfunction or visual field defects.12 Social impairment, failure to understand facial expressions and lack of eye contact are distinguishing features of ASD, but can also be related to low visual acuities, delayed visual maturation, prosopagnosia, dyskinetopsia, simultanagnosia or dorsal stream dysfunction.12
Children with behavioural labels often receive additional support for learning. However, as Williams et al pointed out, these children are usually not receiving vision-based support, despite the presence of vision-related problems. This was thought to be due to a lack of awareness or other competing problems. Some children with CVI-related visual dysfunction cope reasonably well in school, but struggle at home in terms of behaviour and emotional conduct.32 Processing visual information is slowed down and leads to fatigue and fluctuating performance at school and at home.33
The impact of CVI on learning and development will be further discussed in a later article. The next section provides an overview of the prevalence of CVI in the UK with particular focus on the prevalence within schools.
Estimating the prevalence of ocular visual impairment (OVI) and CVI in children
Historically, the leading cause of visual impairment in children has been ocular pathology. However, in more recent years, CVI, has become more common in children and this is now considered to be one of the leading causes of paediatric sight impairment in Western countries.1, 2, 34-38 Rahi et al pointed out that there are significant challenges in estimating the prevalence of childhood visual impairment.35 First of all, the definition of visual impairment varies between countries and between studies.
Secondly, it is difficult to achieve sufficiently large and representative populations of affected children. Children who have not received a diagnosis or who have opted out of certification for vision impairment are not represented in statistics derived from sight impairment registers. Studies that record the causes of sight loss in a particular clinical setting are likely to be biased as these clinics may not give a true representation of the population.
While it is not possible to generate precise statistics about childhood visual impairment causes and trends, studies concerning statistics about paediatric visual impairment provide valuable insight into the current situation.
Prevalence of CVI in population and clinical studies
A UK population-based observational study among children under the age of 18 who were newly diagnosed with visual impairment or blindness (using WHO criteria) in 2015-16 revealed that 48% of children had disorders of the brain or visual pathways.1 An earlier study in the UK reported on children under 16 who were newly diagnosed with severe sight impairment in the year 2000.34 In this study, 48% of children with severe sight impairment (using WHO criteria) had disorders of the brain or visual pathways as one of the contributing factors.
Bunce et al reported an increasing trend of CVI among children with visual impairment in England and Wales. In 2014/2015, disorders of the cortex/brain, malignant neoplasms (excluding the eye), disorders of the optic nerve/visual pathways and congenital anomalies of the brain/nervous system accounted for 26% of children certified for sight impairment or blindness, excluding multiple causes.2
The most common cause of sight loss among children attending a Dutch institute for low vision has consistently been reported as CVI in the period of 1998-2009, with 27.2% in 2009.36 In New Zealand, CVI accounted for 31.5% of children with visual impairment (using WHO criteria) enrolled with the Blind and Low Vision Education Network.37 Huo et al stated a prevalence of CVI of 2.4% in a large retrospective study among children attending a paediatric outpatient clinic in the USA.39
Prevalence of CVI in schools
In recent years, interest in CVI has increased and a number of studies have been undertaken to gain insight into the prevalence of CVI within schools, particularly among children with additional support needs.
In a study by Williams et al,32 3.4% of children attending mainstream schools had at least one CVI-related vision problem and 1.1% had more than one CVI-related vision problem, based on Gordon Dutton’s five questions (see table 2). The use of question inventories for screening, diagnosing and management of CVI will be discussed in more detail in a future article.
Table 2: Dutton and Bax40 identified five questions from a longer question inventory, which could serve as a rapid clinical method of identifying children who warrant more detailed evaluation
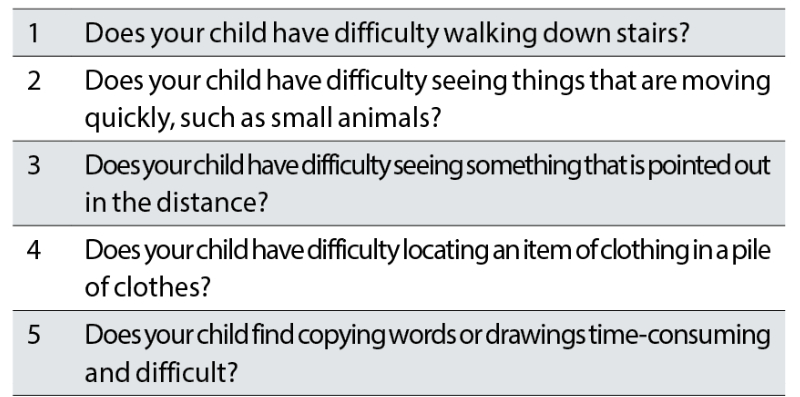
Here, it is important to understand that, although these statistics are striking, one has to bear in mind that Dutton and Bax recommend a cut-off for a potential CVI diagnosis when three out of five questions are answered with ‘often’ or ‘always’.40 Gorrie et al validated the five questions as a potential screening tool, using this ‘three out of five’ cut-off.41 The study by Williams et al does not report what percentage of children had three or more CVI-related vision problems, but it does demonstrate that CVI-related visual dysfunction is common among primary school children. Furthermore, they reported a higher rate of CVI-related vision problems in children who received additional educational support.
A study by Black et al reported that 23.5% of children in a special education school presented with a crowding deficit and/or evidence of visual processing difficulties, most of which were previously unknown to the parents and educators.42 This is in keeping with other studies, which showed a relationship between CVI and learning disability and neurodevelopmental conditions.8, 26-30, 32, 41, 43
Reason for increase of CVI in paediatric population
The increased prevalence of CVI is thought to be related to the increased survival rate of extremely premature infants and improved outcomes for those with other causes of brain injury.3, 4 At the same time, prevention and treatment for ocular conditions has improved and therefore, the proportion of children with OVI has reduced.16
Premature birth is associated with increased risk of developing CVI.44-47 Grey and white matter volume can be altered in these children.47 Periventricular white matter damage, or leukomalacia is commonly seen in children with cerebral palsy,48 children with low birth weight and ex-preterm children,44 and often leads to visual processing dysfunction, sometimes with preservation of normal visual acuity. Periventricular leukomalacia is associated with hypoxia (lack of oxygen) and ischaemia (lack of blood supply) at 24-34 weeks gestation.49
Focal damage is more common in children born after 34 weeks. In these children, hypoxic ischaemic encephalopathy can lead to damage to deep grey matter, hippocampus, brainstem and thalamus regions.50 The extent and location of damage determines the severity and presentation of the visual dysfunction.40 Perinatal hypoxia is the most common cause of childhood CVI. Other causes are hydrocephalus, infections, hypoglycaemia, traumatic brain injury, stroke and genetic conditions.39, 45, 50-53
Conclusion
In summary, CVI is a common cause of paediatric vision impairment, particularly among children with additional support needs and children with perinatal complications and deserves the attention of eye care professionals. Although optometrists and dispensing opticians are not expected to diagnose CVI, familiarity with the condition can aid in identifying children who require onward referral for further investigation of potential CVI.
The next article will provide an overview of approaches and investigations for the purpose of diagnosing CVI in children.
- Cirta Tooth is a specialist low vision optometrist, working in both private practice and the hospital eye service.
References
- Teoh, LJ, Solebo, AL and Rahi, JS on behalf of the British Childhood Visual Impairment Study Interest Group. 2021. Visual impairment, severe visual impairment and blindness in children in Britain (BCVIS2): a national observational study. Lancet Child and Adolescent Health 5(3), pp. 190-200
- Bunce, C, Zekite, A, Wormald, R and Bowman, R. 2017. Is there evidence that the yearly numbers of children newly certified with sight impairment in England and Wales has increased between 1999/2000 and 2014/2015? A cross-sectional study. British Medical Journal Open 7(9), e016888
- Kozeis, N. 2010. Brain visual impairment in childhood: Mini review. Hippokratia 14(4), pp. 249-251
- Philip, SS and Dutton, GN. 2014. Identifying and characterising cerebral visual impairment in children: a review. Clinical and Experimental Optometry 97(3), pp. 196-208
- Jimenez-Gomez, A, Fisher, KS, Zhang, KX, Liu, C, Sun, Q and Shah, VS. 2022. Longitudinal neurological analysis of moderate and severe cerebral visual impairment. Frontiers of Human Neuroscience 16. 772353
- Lam, FC, Lovett, F and Dutton, GN. 2010. Cerebral visual impairment in children: a longitudinal case study of functional outcomes beyond the visual acuities. Journal of Visual Impairment and Blindness 104(10), pp. 625-635
- Jackel, B, Wilson, M and Hartmann, E. 2010. A survey of parents of children with cortical or cerebral visual impairment. Journal of Visual Impairment and Blindness 104(10)
- Donaldson, L and Karas, M. 2020. Optometric care of children with significant learning disabilities. Optometry in Practice 21(3). C-100559
- Pilling, RF, & Ravenscroft, J. (2022). Cerebral visual impairment and educational support in the United Kingdom: Understanding thresholds for providing support. British Journal of Visual Impairment, 0(0). https://doi.org/10.1177/02646196221143315
- Sakki, HEA, Dale, NJ, Sargent, J, Perez-Roche, T and Bowman, R. 2018. Is there consensus in defining childhood cerebral visual impairment? A systematic review of terminology and definitions. British Journal of Ophthalmology 102(4), pp.424-432
- Boot, FH, Pel, JJM, van de Steen, J and Evenhuis, HM. 2010. Cerebral visual impairment: which perceptive visual dysfunctions can be expected in children with brain damage? A systematic review. Research in Developmental Disabilities 31, pp. 1149-1159
- Lueck, AH and Dutton, GN. 2015. Vision and the brain. New York: ABF Press, American Foundation for the Blind, page 13
- Dutton, G. N. 2009. ‘Dorsal stream dysfunction’ and ‘dorsal stream dysfunction plus’: a potential classification for perceptual visual impairment in the context of cerebral visual impairment? Developmental Medicine and Child Neurology 51(3), pp. 168-172
- Zihl, J and Dutton, GN. 2015. Cerebral visual impairment in children. Wien: Springer-Verlag
- McDowell, N. and Budd, J. 2018. The perspectives of teachers and paraeducators on the relationship between classroom clutter and learning experiences for students with CVI. Journal of Visual Impairment and Blindness 112(3), pp. 248-260
- Lueck, A, Dutton, G and Chokron, S. 2019. Profiling children with cerebral visual impairment using multiple methods of assessment to aid in differential diagnosis. Seminars in Pediatric Neurology 31, pp. 5-14
- Chokron, S and Dutton, GN. 2016. Impact of cerebral visual impairments on motor skills: implications for developmental coordination disorders. Frontiers in Psychology 7, 1471
- Dutton, GN et al. 2004. Association of binocular lower visual field impairment, impaired simultaneous perception, disordered visually guided motion and inaccurate saccades in children with cerebral visual dysfunction: a retrospective observational study. Eye 18, pp. 27-34
- Swift, SH, Davidson, RC and Weems, LJ. 2008. Cortical visual impairment in children: presentation, intervention and prognosis in educational settings. Teaching Exceptional Children Plus 4(5), 14065727
- Zihl, J and Dutton, GN. 2015. Cerebral visual impairment in children. Wien: Springer-Verlag, pages 94, 198-200
- Jacobson, L, Flodmarl, O, and Martin, L. 2006. Visual field defects in prematurely born patients with white matter damage of immaturity: a multiple-case study. Acta Ophthalmologica Scandinavica 3, pp. 357-362
- Martineau, J, Cochin, S, Magne, R and Barthelemy, C. 2008. Impaired cortical activation in autistic children: Is the mirror neuron system involved? International Journal of Psychophysiology 68(1), pp.35-40
- Manouilenko, I, et al. 2013. Autistic traits, ADHD symptoms, neurological soft signs and regional cerebral blood flow in adults with autism spectrum disorders. Research in Autism Spectrum Disorders 7(5), pp. 566-578
- Bu, X, et al. 2020. Exploring white matter functional networks in children with attention deficit/hyperactivity disorder. Brain Communications 2(2). doi:10.1093/braincomms/fcaa113
- Keehn, RJJ, et al. 2021. Underconnectivity between visual and salience networks and links with sensory abnormalities in autism spectrum disorders. Journal of the American Academy of Child and Adolescent Psychiatry 60(2), pp. 274-285
- Fazzi, E, Micheletti, S, Galli J, Rossi, A, Gitti, F and Molinaro, A. 2019. Autism in children with cerebral and peripheral visual impairment: Fact or artifact? Seminars in Pediatric Neurology 31, pp. 57-67
- Chokron, S, Kovarski, K, Zalla, T and Dutton, GN. 2020. The inter-relationships between cerebral visual impairment, autism and intellectual disability. Neuroscience and Biobehavioural Reviews 114, pp. 201-210
- Hay, I, Dutton, GN, Biggar, S, Ibrahim, H and Assheton, D. 2020. Exploratory study of dorsal visual stream dysfunction in autism; A case series. Research in Autism Spectrum Disorders 69. doi: 10.1016/j.rasd.2019.101456
- Chokron, S, Kovarski, K and Dutton, GN. 2021. Cortical visual impairments and learning disabilities. Frontiers in Human Neuroscience 15. doi: 10.3389/fnhum.2021.713316
- Kovarski, K. et al. 2021. Emotional face recognition in autism and in cerebral visual impairments: In search for specificity. Journal of Neuropsychology 15(2), pp. 235-252
- Sonksen, P. M. and Dale, N. 2002. Visual impairment in infancy: impact on neurodevelopmental and neurobiological processes. Developmental Medicine and Child Neurology 44, pp. 782-791
- Williams, C, et al. 2021. Cerebral visual impairment-related vision problems in primary school children: a cross-sectional survey. Developmental Medicine and Child Neurology 63(6), pp. 683-689
- McKillop, E, Bennett, D, McDaid, G, Holland, B, Smith, G, Spowart, K and Dutton, G. 2006. Problems experienced by children with cognitive visual dysfunction due to cerebral visual impairment- and the approaches which parents have adopted to deal with these problems. The British Journal of Visual Impairment 24(3), pp. 121-127
- Rahi, JS, Cable, N, and British Childhood Visual Impairment Study Group. 2003. Severe visual impairment and blindness in children in the UK. Lancet 362, pp. 1359–1365
- Rahi, JS. 2007. Childhood blindness: a UK epidemiological perspective. Eye 21, pp. 1249–1253
- Boonstra, N, Limburg, H, Tijmes, N, van Genderen, M, Schuil, J and van Nispen, R. 2012. Changes in causes of low vision between 1998 and 2009 in a Dutch population of children. Acta Ophthalmologica 90, pp. 277-286
- Chong, C-F, McGhee, CNJ and Dai, SH. 2019. Causes of childhood low vision and blindness in New Zealand. Clinical and Experimental Ophthalmology 47, pp. 165-170
- Sahli, E, Kiziltunc, PB and Idil, A. 2021. Visual habilitation in young children with visual impairment. Child Care Health and Development 48(3), pp. 378-386
- Huo, R, Burden, SK, Hoyt, CS and Good WV. 1999. Chronic cortical visual impairment in children: aetiology, prognosis, and associated neurological deficits. British Journal of Ophthalmology 83, pp. 670-675
- Dutton, GN and Bax, M. 2010. Visual Impairment in children due to damage to the brain. London: Mac Keith Press
- Gorrie, F, Goodall, K, Rush, R and Ravenscroft, J. 2019. Towards population screening for cerebral visual impairment: Validity of the Five Questions and the CVI Questionnaire. Plos One 14(3). e0214290
- Black, SA, et al. 2019. In-school eyecare in special education settings has measurable benefits for children’s vision and behaviour. Plos One 14(8), e0220480
- Hokken, MJ, Krabbendam, E, van de Zee, YJ and Kooiker, MJG. 2022. Visual selective attention and visual search performance in children with CVI, ADHD, and dyslexia: a scoping review. Child Neuropsychology. doi: 10.1080/09297049.2022.2057940
- Macintyre-Béon, C, et al. 2013. Cerebral visual dysfunction in prematurely born children attending mainstream school. Documenta Ophthalmologica 127, pp. 89-102
- Khetpal, V and Donahue, SP. 2007. Cortical visual impairment: etiology, associated findings, and prognosis in a tertiary care setting. Journal of the American Association for Pediatric Ophthalmology and Strabismus 11(3), pp. 235-239
- Hård, A-L, Aring, E and Hellström, A. 2004. Subnormal visual perception in school-aged ex-preterm patients in a paediatric eye clinic. Eye 18, pp. 628-634
- Schmitz-Koep, B, et al. 2021. Grey and white matter volume changes after preterm birth: A meta-analytic approach. Journal of Personalized Medicine 11. 868
- Lanzi, G, et al. 1998. Cerebral visual impairment in periventricular leukomalacia. Neuropediatrics 29(3), pp. 145-150
- Pavlova, MA and Krägeloh-Mann, I. 2013. Limitations on the developing preterm brain: impact of periventricular white matter lesions on brain connectivity and cognition. Brain 136, pp. 998-1011
- Pehere, N, Chougule, P and Dutton, GN. 2018. Cerebral visual impairment in children: Causes and associated ophthalmological problems. Indian Journal of Ophthalmology 66, pp. 812-815
- Bosch, DGM et al. 2016. Novel genetic causes for cerebral visual impairment. European Journal of Human Genetics 24, pp. 660-665
- Kabakus, N, Yilmaz, T, Balci, TA, Kamisli, O, Kamisli, S and Yildirim, H. 2005. Cortical visual impairment secondary to hypoglycemia Neuro-Ophthalmology 29, pp. 27-31
- Bennett, CR, Bauer, CM, Bailin, ES and Merabet, LB. 2020. Neuroplasticity in cerebral visual impairment (CVI): assessing functional vision and the neurophysiological correlates of dorsal stream dysfunction. Neuroscience and Behavioral Reviews 109, pp. 171-181
