In the past few years, the control of worsening myopia, with a view to slowing its predictable progression, has become a hot topic. Until recently a niche service, mainly offered by independent opticians, myopia management has suddenly become mainstream and is increasingly offered by virtually all practices in the UK, and now seems to also be firmly on the ophthalmology agenda.
Background
The surge in practitioner engagement with myopia management in the last couple of years is likely to be multifactorial. Coinciding with new product development there may well have been pent up demand caused by the Covid-19 pandemic as practices worked through backlogs of sight test1 and certainly some practices have woken up to the business opportunities that were previously being lost when prospective patients and their parents and siblings were forced to find another optician if their own would not help.2
However, the likelihood is the growth in myopia management has essentially been driven by the application of ethical and professional standards. GOC Standards of Practice (Standards 3.1, 3.1.4, 3.3 and 5.3) require registered opticians to ensure they gain valid consent and also to be evidence-based practitioners and professional bodies have been quick to support their members with appropriate guidance and consent templates to ensure patients have informed choice.3
Keep your knowledge and skills up to date.
5.3 Be aware of current good practice, taking into
account relevant developments in clinical research,
and apply this to the care you provide.
This means that all eye care professionals (ECPs) have a duty to keep abreast of the latest research, of which there is now plenty, and furthermore to inform patients of the likely progression of their myopia, any interventions that may slow its progression, and the potential consequences of the various options patients (and their carers) have open to them.
A surprising outcome from some of the research into myopia is that it would seem that patients may have been right all along; wearing standard single vision spectacles for the correction of myopia may indeed make your vision worse, at least relatively speaking.
But what choice does a -2.00DS myope have? Walk around in a blurred haze with a far point of clear vision of 50cm? Or correct their vision in the knowledge that their prescription will increase by 0.25 to 0.50DS at almost every regular sight test that follows until they have finished growing? The informed choice would appear to be to slow the progression of their myopia by choosing one or more of the options now available.
The prescribing of optical appliances to slow progressive myopia seems to come and go, in the UK at least, in the same way that frame styles are dictated by fashion. Nevertheless, the research base relating to slowing myopic progression now extends back decades, though until recently much of it was locked behind pay walls and would not have been subject to much scrutiny by the average registrant, especially dispensing opticians who generally have had no access to libraries of scientific journals.
These authors first joined the GOC register in the late 1980s, a time when ophthalmologists and optometrists frequently issued prescriptions and the then new GOS3 vouchers for bifocal lenses for the correction of ‘juvenile stress myopia’, usually with a +2.50DS reading-addition, and instructions to set the segment higher than would be normal for a presbyopic adult.
Dispensing opticians would normally dispense straight top D35 or D40 segments, or executive bifocals, with the segment top fitted at pupil centre or just below, to a well-fitting and deep frame that the patient could not look over the top of or see to read beneath the lower rim.
The evidence now suggests that both bifocal spectacles and progressive power lenses (PPLs) are effective to some degree in some patients at slowing the progression of myopia,4 however back then, as now, the General Ophthalmic Services (GOS) contract was ill-fitted to providing adequate funding since the treatments were judged to be experimental or unproven, and outside of hospital practice the treatment of progressive myopia was greatly reduced.
However, interest in myopia has never gone away, and has come to the fore in the last decade, as research evidence has been commercialised into viable, and more effective, solutions to slow myopic progression to a greater degree in a greater percentage of patients.
These solutions are more necessary than ever since myopia is reaching pandemic proportions with predictions that half of all people worldwide will be myopic by 2050, with closer to 100% in Far Eastern nations.
Ten percent are expected to have high myopia (standardised to spherical equivalent of -5.00D and greater – see author comment and later IMI notes on definitions) with consequences of serious pathology including retinal detachment, myopic maculopathy, glaucoma and cataract.5
Reducing myopic progression is clearly important to relieve the public health burden and improve quality of life for myopes, since slowing myopia by 1.00DS has been shown to reduce myopic maculopathy by 40%.6
Myopia is now generating more debate and research than ever before. There is clearly a link between genetic,7 environmental, and optical factors such as off axis refraction and the shape of the globe.8 Heritability of myopia is 60 to 80%,9 and it is known that a child of two myopes is much more likely to develop myopia than a child with only one myopic parent.10
Numerous articles relating to myopia progression and management have appeared in the optical journals in recent years, highlighting the role of relative peripheral refraction in stimulating axial eye growth, the effect of existing interventions, and reviewing evidence for pharmacological, spectacle and contact lens treatment options.
This article aims to provide an update on what has happened in the past year or so and consider the specific fitting criteria of myopia management spectacle lenses and the paediatric frames they are edged into.
The International Myopia Institute
After a meeting in 2015 between the World Health Organisation (WHO) and the Brien Holden Vision Institute (BHVI) on myopia and high myopia, the International Myopia Institute (IMI) was formed as the global burden of myopia and its sight threatening complications were clearly evident.
The IMI consists of experts from around the world who created a series of white papers and clinical summaries (free to access at myopiainstitute.org) to aid eye care practitioners, governments, educators and the general public understand myopia. The IMI has defined high myopia as ≤ -6.00DS using mathematically valid descriptors, meaning more myopic than -6.00D.11
The International Myopia Institute (IMI) exists to advance myopia research and education to prevent future blindness and is an excellent resource to stay up to date with the latest developments. The IMI publishes detailed data, and useful summaries of all interventions relating to myopia management including those that might be considered historical as well as those at the cutting edge of new research.
Spectacle Lenses
Single vision undercorrection
Under correction of myopes, giving rise to foveal myopic defocus potentially diminishing myopic progression, initially showed success in animal studies.12, 13
However, in humans, evidence is contradictory. Logan and Wolffsohn, in a systematic review found most evidence showed an increase in myopic progression compared to full correction.14 Current advice and guidance states that myopia should be fully corrected. It is worth mentioning here that the biggest cause of under or over-correction in patients with a high level of myopia is the routine failure of practitioners to measure and/or take into account a change in back vertex distance between what has been prescribed and the frame that is finally fitted.
Progressive power lenses
Gwiazda et al conducted a randomised clinical trial, which was completed by 462 children using Varilux comfort (+2.00DS addition) compared to single vision lenses.4 They achieved a reduction in myopic progression of 0.20D and axial length reduction 0.11mm although these results were not deemed clinically significant. The treatment effects of progressive power lenses (PPLs) have shown to be greatest in the initial six to 12 months, but diminish in later intervals. The reasons for this are unknown but it is thought this may be due to accommodation adaptation.15
Bifocals lenses
IMI data suggests executive bifocals with a 1.50DS addition are more effective than progressive power lenses. One group without prism and another incorporating 3∆ base in at near reduced myopic progression by 39% and 51% respectively over three years compared to single vision lenses. The prismatic lenses had a greater effect for children with lag of accommodation.16
Peripheral defocus (myopia control) lenses
All currently available spectacle lenses specifically marketed for the control of myopia progression utilise the mechanism of the peripheral defocus theory as the basis of lens designs. They adopt a simultaneous vision approach creating a clear foveal image as well as peripheral myopic defocus reducing the stimulus for eye growth.
Before moving to the several lens options now on the market, we will cover the frame fitting criteria, which all these lenses seem to have in common.
Frame selection for myopia control
With all spectacle lenses, vertical centration should take into account the centre of rotation condition so that the visual axis intersects the optical centre of the lens normally (at 90 degrees), so the optical axis and visual axis coincide and the oblique astigmatism aberration is minimised. In traditional progressive lenses, this is taken into account by the manufacturer.
This is why a pantoscopic tilt of nine or 10 degrees is recommended by manufacturers for the fitting cross to be aligned exactly on pupil centre.
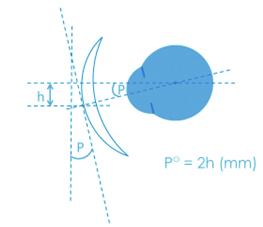
For single vision lenses, this requires measuring pantoscopic angle and heights to pupil centre and then compensating for tilt by dropping the optical centres 0.5mm for every degree of tilt (figure 1) to avoid the introduction of unwanted oblique astigmatism. Leaving the optical centres on pupil centre is a widely encountered error in ophthalmic dispensing practice and makes little or no difference in the majority of low powered lenses.
However, with all aspheric lenses and any lens over +/-5.00D, it is a common cause of unnecessary remakes, retests and refunds in optical practice.
Figure 1: Pantoscopic angle°
Experience tells us that the pantoscopic tilt in children is very much less than in adult patients, typically in the range of -4 to +6 degrees as opposed to +5 to +15 degrees in an adult. Frames must be designed to take into account a less developed bridge and naturally chubbier cheeks so that the frame can fit properly without resting on the cheeks.
Figure 2 shows how to measure pantoscopic tilt, in this case using a Zeiss pantoscopic tilt gauge. All major manufacturers offer such devices, and searching ‘free inclinometer’ in your smartphone’s app store will yield a host of suitable applications (such as the Velux windows app), yet many practices seem not to have this vital piece of equipment.
Figure 2: Measuring Pantoscopic angle

Tilt gauge instructions often say to remove the dummy lens in order to ensure a clean contact with the top and bottom rim and an accurate measurement, however in cases where the lens cannot be removed (rimless and supra styles) or combination frame designs where the top rim is much thicker than the bottom this is not appropriate, and care must be taken to ensure an equal gap at top and bottom of the lens as shown. It should be noted that, despite what can be found online, pantoscopic tilt is an ‘as worn’ measurement with the frame on the face and is not the same as angle of side.
The nature of all lenses designed specifically to control the progression of myopia is that there is a small central aperture that must be positioned very accurately with the optical centre on pupil centre in order that the area responsible for peripheral defocus is effective and the child retains a high level of visual acuity when the eye is in the primary position. It should be apparent therefore that when dispensing frames to be fitted with myopia control lenses the only pantoscopic angle that is appropriate is one of zero degrees.
Manufacturers offer centration tolerances of 1mm vertically and 0.5mm horizontally regardless of lens power which in effect means the pantoscopic tilt can be between -2 and +2 degrees with the optical centre (OC) on pupil centre. The frame selected in figure 2 is, of course, unsuitable since, once adjusted to a tilt of zero, there will be a large gap between the cheeks and bottom rim.
Additionally, the B measurement (vertical box height / lens depth) is important and also unlikely to be suitable in figure 2. The main point is that the frame should have as large a depth as possible so the child cannot look over the top rim or beneath the bottom rim to read. For example, Hoya recommend a B measurement of ≥ 25mm if a Hoya Miyosmart lens is to be dispensed.
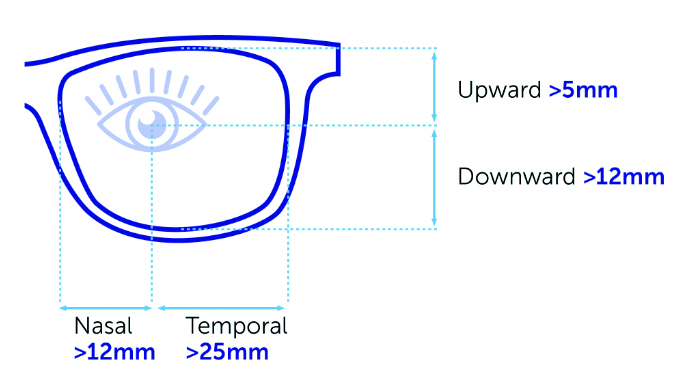
Understanding the differing lens designs is essential to ensure areas of peripheral defocus can be fully effective as, for example, the Norville My-Nor lens requires at least 12mm nasally and 25mm temporally from pupil centre, although a minimum eye size of 37mm is unlikely to be problematic (figure 3).
Figure 3: Minimum mounting dimensions for the My-Nor lenses
It is important that the child looks through the lenses for all visual tasks, and does not, for example, look below the bottom rim for close tasks, therefore it is important to select a frame that is sufficiently deep without touching the cheeks, and because of the fine tolerances involved, even in low powers it is important that the frame can be easily adjusted both for pantoscopic tilt and, ideally, vertical centration. Altering centre heights after manufacture would of course require adjustable nose pads, which can also be helpful in allowing adjustment of back vertex distance.
Regardless of lens power, back vertex distance is an important consideration and, as is the general rule for all dispensing, lenses should be fitted as close as possible to the eye without touching the eyelashes, with manufacturers stipulating 10mm or less as required.
The principle here is the same as for progressive lenses, where a keyhole effect is in operation and, whether this is the intermediate zone on a varifocal or, as here, the central zone on a myopia control lens, the closer the eye is to the key hole then the wider the field of view, and the easier the lens will be to use with less head movement required for optimum vision of objects that lie away from the primary direction of gaze.
Some frame suppliers have started to develop frame ranges specifically for myopia management, and some lens manufacturers offer complete package value pricing for specialist lens and frame combinations.
For example, Wolf Eyewear’s Wolf Cubs MY collection includes design features such as extra lens depth and joints positioned to give a flat pantoscopic tilt, as is required for Hoya Miyosmart lenses (figure 4), as well as a range of colours and sizes and optional clip-on sunglasses on some models. In the authors’ opinion, such frames, even if made from acetate rather than metal, would benefit from adjustable pads on arms, on at least some models.
Figure 4: Wolf Cubs MY frames are specifically designed for myopia management lenses
Myopia management lenses
Myopia management lenses will now be discussed, presented in alphabetical order.
Miyosmart (Hoya)
Miyosmart was launched in February 2021 in the UK, with data from a two-year double masked randomised controlled trial (RCT).17 Development of MiyoSmart was inspired by the defocus incorporated soft contact (DISC) lens, a simultaneous vision correction with central clear distance zone and a 50:50 ratio of (2.50DS) myopic defocus zones.18
Myopic progression was reduced by 58% when lenses were worn for at least seven hours, time worn or ‘dose’ of myopia management was linked to the effect. Providing this concept of simultaneous vision with myopic defocus was applied to spectacle lenses by defocus incorporated multiple segments (DIMS) technology as not everyone is suitable for contact lens wear.19
The lens has enjoyed meteoric growth, having recently reported the sale of 100 million lenses worldwide and, since then, there has been a three-year follow up study where results showed a sustained myopia control effect.20
This second study consisted of 128 children, those in the original DIMS group continued to wear the DIMS lens but children from a single vision control group were switched to the DIMS lens for a one-year period. Compared to the historical control group the DIMs lens showed a (mean difference) reduction in myopia progression of -0.18D and axial length of 0.08mm. The control-to-DIMS compared to the historical control showed reduction in myopia progression of -0.30D axial length of 0.12mm.
In June 2022, an abstract publication giving six-year results of data from 90 children, also showed that the children wearing DIMS lens throughout the six years (n=36) the DIMS lens maintained its effect of slowing myopia progression.21 Children that wore single vision lenses for the first two years (n=18) then switched to the DIMS lens until 3.5 to six years, at which point they stopped DIMS lens wear and exhibited faster myopic progression. At present, there is no specific research on this rebound effect after discontinuing Miyosmart.
Miyosmart is a simultaneous vision lens, consisting of a hexagonal 9.4mm clear central vision zone surrounded by a 33mm ring honeycomb treatment zone of micro-lens segments (lenslets) creating 3.50DS of myopic defocus (+3.50DS add) giving optical defocus in all regions of the lens and maintaining the 50:50 ratio of focus and defocus.21 Lenslets are very discreet, only visible if the lens is tilted and a light source used to show the multiple segments by reflection (figure 5).
Figure 5: Hoya MiyoSmart, showing defocus incorporated multiple segments (DIMS) lenslets

This lens design demands specific frame fitting criteria, and requires the selected frame to have a vertex distance of 10mm or less with a pantoscopic angle close to zero and face form angle no more than 5°. The frame needs a B size of more than 25mm with at least 12mm above the pupil ensuring a sufficient area of defocus. Lens centration measurements are taken in the same way as progressive lenses by locating the pupil centre the material polycarbonate, refractive index n = 1.59 with a multicoat.
At the time of writing, a Google search of spectacle lens suppliers for myopia control lenses shows that several small independent labs offer such products. However, on enquiry, it has transpired that in each case they are reselling the Hoya MiyoSmart lens.
MyCon (Rodenstock)
Rodenstock’s myopia management lens was launched in June 2023 and, at the time of writing, the authors have no experience of dispensing it. The lens is aimed at myopes between six and 14 years of age and, in terms of design philosophy, is closer to the Norville myopia control lenses than the offerings from Hoya, Essilor, Zeiss or SightGlass.
Rodenstock claim that, because myopia is a consequence of the eye being slightly too long, conventional single vision lenses can correct it but are not designed to slow it down. This is because light is projected behind the retina, causing some children’s eyes to grow excessively long and exacerbating short-sightedness.
With MyCon lenses, light is focused in front of the peripheral retina rather than behind it, thereby slowing eye-length growth. The areas that control myopia progression in a MyCon lens are located laterally (figure 6). This ensures that the visual acuity above and below is affected as little as possible.22
Figure 6: Defocus areas are located laterally in Rodenstock MyCon lenses
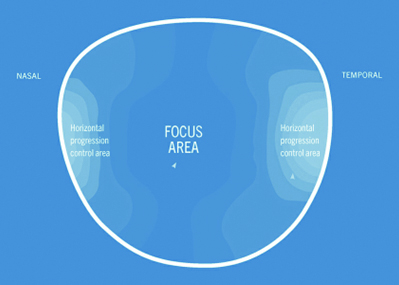
It is worth noting that being able to gaze downwards without moving one’s head can be much more comfortable for many patients, as we have found with progressive lens designs which are better accepted by people who are ‘eye movers’ as opposed to ‘head movers’ in the vertical meridian.
Fitting criteria are the same as other myopia management lenses; flat pantoscopic angle, mono-PDs and heights to pupil centre. Time will tell whether sceptical UK consumers see a con in MyCon; it is perhaps not the best of names.
My-Nor (Norville)
A recent feature in Optician (Myopia Guide, December 2022) discussed My-Nor and the comparative study where, on average, a 40% reduction in myopia progression was found. The study consisted of 94 children aged seven to 14 years split into two groups (a single vision group and a treatment group) over a period of five years.
This lens was launched in early 2022 and, uniquely, is available in a comprehensive range of indices (1.50 CR39, 1.53 Trivex, 1.60, 1.67 and 1.74), a wide power range (plano to -16.00DS) and has an asymmetric freeform back surface design with horizontal progression, creating relative peripheral myopic defocus in the horizontal meridian of +2.50DS at 25mm nasally and +2.00DS at 25mm temporally.
There is clear correction at the centre and horizontal peripheral defocus starts at 6mm nasally and 4mm temporally, recognising the need for convergence at near and intermediate distances. Vertically peripheral myopic defocus is achieved by positive spherical blur although it is a much smaller amount than in the horizontal meridian.
Once again, fitting criteria are important and lens centration measurements are taken in the same way as a progressive lens. However, when selecting a suitable frame, there must be least 5mm above pupil centre and 12mm below, a minimum boxed size of 37mm x 17mm to enable >25mm temporally and >12mm nasally from pupil centre.
On collection, explaining the lens design and location of the defocus areas is essential as well as the need to look centrally through the lenses. This will help the child to adapt more easily. Adaptation is usually within a day but can take up to two weeks. Correct frame fit is essential and, if there is any slip or the frame becomes out of alignment, the child and parent should be advised to return to the practice for adjustment.
This spectacle lens is a new addition to myopia management training and support is available from the manufacturer.
MyoCare and MyoCare S (Zeiss)
Having marketed myopia control lenses in East Asian markets for around 10 years, Zeiss only launched their new myopia management offering in the UK in June 2023. A fundamental difference to most other manufacturers is the offering of two different lenses depending on the age of the child. MyoCare is aimed at young children up to the age of nine, and MyoCare S at those myopes aged 10 and over (table 1).
Table 1: MyoCare and MyoCare S lens features
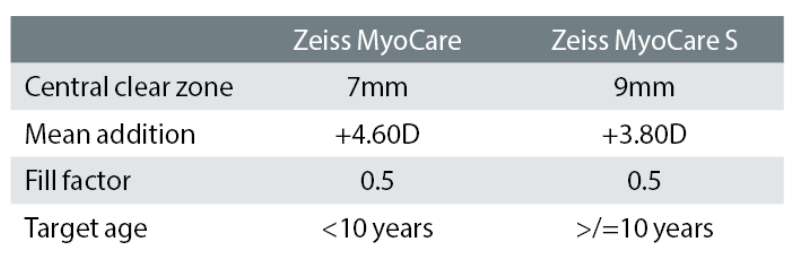
The CARE in MyoCare stands for ‘Cylindrical Annular Refractive Elements’, which are incorporated in the lenses to deliver a ‘stop signal’ to slow down the progression of axial elongation. The design consists of alternating defocus and correction zones in a ring-like pattern on the front surface, expanding towards the periphery of the lens.
Additionally, the freeform Zeiss ClearFocus design aims to remove the ‘growth signal’ through an optimised back surface delivering refractive correction as well as the intended myopic defocus in all directions of gaze. This optical design seems to be analogous to the diffractive simultaneous vision multifocal contact lenses that used to be available in the 1990s.
Zeiss claim to have stuck to optimum balance between myopia progression management and clear vision by having:
- A central zone small enough to establish an effective functional zone projecting myopic defocus on the near periphery close to the fovea
- A mean addition surface power to induce the intended relative myopic defocus
- A carefully selected fill factor (the ratio of the cylindrical defocusing elements to the whole of the periphery outside of the clear zone) to deliver high efficacy while preserving good wearability
At the time of writing, the authors are still awaiting delivery of first orders. However, the sample lenses provided obviously show poorer vision for distance through the periphery. This is not an issue when looking straight ahead, as the periphery is always blurred away from foveal fixation and, for other directions of gaze, can be overcome by setting expectations that more head movement will be required.
Time will tell whether children are comfortable with the experience of ensuring the intended myopic defocus are maintained for all gaze directions. This is important, not only for distinct viewing behaviours through the central clear zone when pursuing a focused task, but also for unintended gazes and saccades to the lens periphery.
Figure 7: Comparative mathematical simulation of spherical single vision lenses (in red) and MyoCare lenses (in blue)23
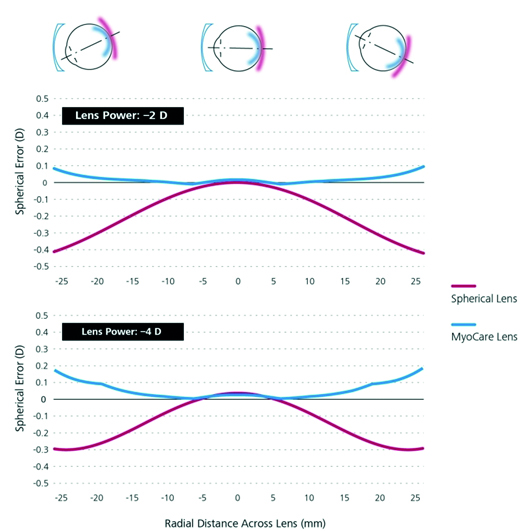
Additionally, the Zeiss ClearFocus design effectively minimises the induction of hyperopic defocus (figure 7) as opposed to typical spherical single vision lenses in a graph not dissimilar to the power profile of low base aspheric lenses compared to traditional point focal best form.23
Zeiss introduce a new measure of effectiveness in their clinical information called the emmetropic progression ratio. This aims to compare treated myopic eyes with the eyes of children who are exhibiting typical emmetropisation (figure 8). They claim ratios of 83% and 63% for 10 to 12 and seven to nine-year-olds, respectively.
Figure 8: Influence of Zeiss MyoCare on axial length growth over time23
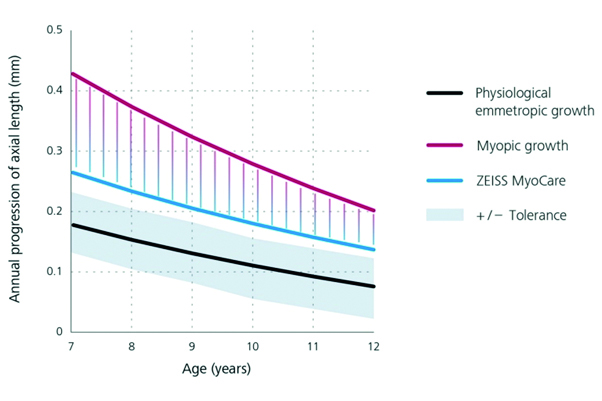
Although more challenging to understand, especially for patients, this measure at least gets away from some of the careless claims made in marketing materials from some suppliers of myopia management products, where it is said ‘myopia is reduced’ when what is meant is progression is not as advanced as it otherwise would be; myopia has still, in fact, increased.
Fitting criteria for Zeiss MyoCare are mono-PDs and heights to pupil centre while ensuring a deep frame with flat pantoscopic tilt and the lens comes with full UV protection as standard.
Stellest (Essilor)
The Stellest uses Highly Aspherical Lenslet Target (HALT) technology, consisting of a central single distance zone with aspherical lenslets spread on 11 concentric rings formed by contiguous aspherical lenslets having diameter of 1.1mm with a clear central zone of 9mm.
The design of the aspherical lenslets creates a volume of myopic defocus (VoMD), which ensure visual signals focus in front of the retina following the retinal profile reducing stimulus for eye growth.24
Two-year results have been published from a double masked randomised controlled trial based on 157 Chinese children who were divided into three groups, wearing lenses with highly aspherical lenslets (HAL), slightly aspherical lenslets (SAL) or single vision spectacle lenses (table 2).24
Table 2: Essilor Stellest lens two-year results24
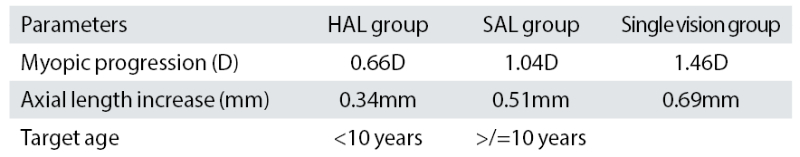
With full time wear, the study reported a dose-response relationship with HAL group efficacy at 0.99DD and 0.41mm for full time wearers. The best corrected visual acuity did not significantly differ at distance or near between the single vision group and those in either the HAL or SAL group, although, low contrast visual acuity and reading speed were reduced.
When fitting, lens centration measurements are again taken in the same way as progressive lenses with monocular centration and vertical heights. The centration point is the reference point, which is also used for prescription verification, and the lens material is Airwear polycarbonate (n = 1.59).
Vision DOT 0.2 lens (SightGlass)
SightGlass Vision was acquired and developed as a collaboration between Essilor-Luxottica and CooperVision but does not, at the time of writing, appear to be commercially available in the UK, despite having already been launched commercially in Far Eastern markets. Nonetheless, clinical trials have been widely publicised at conferences and it is expected it will be launched soon under the Nikon Lenswear brand in the UK (figure 9).25
Figure 9: The use of Diffusion Optics Technology to reduce contrast signalling at the retina
Diffusion Optics technology (DOT) uses microscopic diffusers applied to the lens surface to scatter the light reducing peripheral retinal contrast. Each diffuser is irregular in shape and translucent with a diameter of ≈ 0.14mm and height 0.2mm. There is a 5mm aperture outside, which the entire lens is integrated with microscopic diffusers in a Trivex lens material. Children aged six to 10 years, which is younger than other studies, wore assigned spectacles constantly (over 10 hours per day).
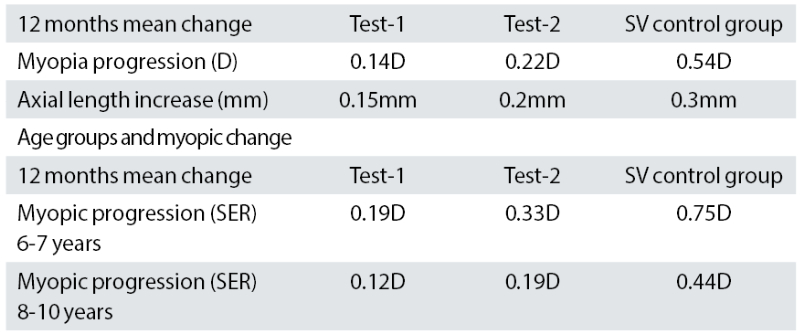
A multicentre (14 sites in North America) double-blind RCT published 12-month results. In the CYPRESS study, 32 subjects were randomised into three groups a single vision control group, test-1 marketed as DOT 0.2 0.365mm, test-2 0.240mm more closely spaced (table 3).
Results show a faster progression in the younger age group. When fitting, this lens design is also measured like a progressive lens.26
Table 3: Twelve-month results CYPRESS study26
Conclusion
While no intervention can provide a cure for myopia progression by reversing it or halting it completely, there are now a multitude of safe and effective spectacle and contact lens treatment options to slow the progression of myopia to around half of its typical expected rate through the creation of relative peripheral myopic defocus using products that are licenced / approved for this purpose.
For patients outside of the prescription ranges of the licenced products, other, less effective, alternatives exist, such as traditional bifocal or progressive spectacles and toric centre distance multifocal contact lenses. Where products and treatment strategies are used ‘off-licence’ for myopia management, ECPs should ensure full patient awareness that there is a lower rate of myopia progression reduction according to the evidence.
Being able to offer spectacle (and contact) lenses for the management of myopic progression provides an exciting opportunity for ECPs to prevent future sight loss and is a significant commercial opportunity. However, the mechanisms of myopia progression are still not fully understood so following the best available evidence is essential.
There is now an argument that all myopic children (and their guardians), as part of the process of gaining valid consent for the fitting of contact lenses or the dispensing of spectacles, must be told of the long-term implications of myopia.
Practices that do not offer myopia management solutions are therefore obliged to act in the best interest of their patients and refer them to practices that are able to assist if patients are interested in reducing their risk of blindness in the future.
- Peter Black MBA FBDO FEAOO AFHEA is Course Lead for BSc (Hons) Ophthalmic Dispensing at the University of Central Lancashire, Preston, and is a practical examiner, practice assessor, exam script marker, board member and past president of the Association of British Dispensing Opticians.
- Tina Arbon Black BSc (Hons) FBDO CL is director of accredited CPD provider Orbita Black Limited, an ABDO practical examiner, practice assessor and exam script marker, and a distance learning tutor for ABDO College.
References
- Visionary.org.uk. UK headed for pandemic vision crisis. 2021. [Online]. Available: https://www.visionary.org.uk/latest/uk-headed-for-pandemic-vision-crisis . [Accessed 22 June 2023].
- K. Young. Myopia management: education is key. 4 January 2023. [Online]. Available: https://www.aop.org.uk/ot/industry/eyewear-and-lenses/2023/01/04/myopia-management-education-is-key [Accessed 22 June 2023].
- British Contact Lens Association. Myopia management informed consent form. BCLA, 2023. [Online]. Available: https://www.bcla.org.uk/Public/Public/Member_Resources/Myopia-Management---Children.aspx [Accessed 22 June 2023].
- J. Gwiazda, L. Hyman, M. Hussein, D. Everett, T. T. Norton, D. Kurtz, M. C. Leske, R. Manny, W. Marsh-Tootle, M. Scheiman and The COMET Group. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Investigative Ophthalmology & Visual Science, vol. 44, pp. 1492-1500, April 2003.
- B. A. Holden, T. R. Fricke, D. A. Wilson, M. Jong, K. S. Naidoo, P. Sankaridurg, T. Y. Wong, T. J. Naduvilath and S. Resnikoff. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology, vol. 123, no. 5, pp. 1036-1042, May 2016.
- M. A. Bullimore and N. Brennan. Myopia control: Why each diopter matters. Optometry and Vision Science, May 2019.
- M. S. Tedja, A. Haarman, A. Meester-Smoor, J. Kapriro, D. A. Mackey, J. A. Guggenheim, C. J. Hammond, V. Verhoeven and C. Claver. IMI - Myopia genetics report. Investigative Ophthalmology & Visual Science, vol. 60, no. 3, 2019.
- D. I. Flitcroft. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Retinal and Eye Research, vol. 31, no. 6, pp. 622-660, 2012.
- Morgan and K. Rose. How genetic is school myopia? Retinal and Eye Research, vol. 24, no. 1, pp. 1-38, 2005.
- X. Zhang, X. Qu and X. Zhou. Association between parental myopia and the risk of myopia in a child. Experimental and Therapeutic Medicine, vol. 9, no. 6, pp. 2420-2428, 2015.
- Flitcroft DI et al. IMI – Defining and classifying myopia: A proposed set of standards for clinical and epidemiologic studies. Investigative Ophthalmology & Visual Science. 2019, vol. 60, no. 3,
- J. Wallman and J. Winawer. Homeostasis of eye growth and the question of myopia 2004. Neuron, vol. 43, no. 4, pp. 447-468, 2004.
- E. L. Smith and L. F. Hung. The Role of optical defocus in regulating refractive development in infant monkeys. Vision Research, vol. 39, no. 8, pp. 1415-1435., 1999.
- N. S. Logan and J. S. Wolffsohn. Role of un-correction, under-correction and over-correction of myopia as a strategy for slowing myopic progression. Clinical and Experimental Optometry, 2019, vol. 103, no. 2
- Li, SM et al. Studies using concentric ring bifocal and peripheral add multifocal contact lenses to slow the myopia progression in school-aged children: A meta-analysis., Ophthalmic and Physiological Optics, 2017, vol. 37, no. 1, pp. 57-59
- Huang PC et al. Protective behaviours of near work and time outdoors in myopia prevalence and progression in children: A 2 year prospective study. British Journal of Ophthalmology, 2020, vol. 104, pp. 956-961
- Lam CS et al. Defocus Incorporated Multiple Segments (DIMS) spectacle lenses slow myopia: A 2year randomised clinical trial. British Journal of Ophthalmology, 2020, vol. 104, pp. 363-368
- Harvey B. Managing with glasses. Optician, 20.12.2019, p31
- Kaymak H et al. Vision tests on spectacle lenses and contact lenses for optical myopia correction: a pilot study. BMJ Open Ophthalmology, 2022;7(1):e000971.
- Lam CS et al. Myopia control effect of defocus incorporated multiple segments (DIMS) spectacle lens in Chinese children: results of a 3-year follow-up study. British Journal of Ophthalmology, 2022;106(8):1110-1114DIMS
- Lam CSY et al. Long-term myopia control effect and safety in children wearing DIMS spectacle lenses for 6 years. Scientific Report, 2023 Apr 4;13(1):5475
- Rodenstock. Children’s spectacles – MyCon. Available at: www.rodenstock.com/uk/en/childrens-spectacles.html
- www.zeiss.co.uk/vision-care/eye-care-professionals/lenses/lenses-for-every-need/lenses-to-manage-myopia-progression-in-children
- Atchison DA et al. Relative peripheral hyperopia does not predict development and progression of myopia in children. Investigative Ophthalmology & Visual Science, 2015, vol. 56, pp. 6162-6170
- Optometry Times. New myopia control spectacle lens technology to be presented by sightglass vision. Available: www.optometrytimes.com/view/new-myopia-control-spectacle-lens-technology-to-be-presented-by-sightglass-vision-at-cooc
- Rappon J et al. Control of myopia using diffusion optics spectacle lenses: 12-month results of a randomised controlled, efficacy and safety study (CYPRESS), British Journal of Ophthalmology, 1 September 2022
